Abstract
This study examined the impact of a selective anxiety prevention program for offspring of clinically anxious parents on three domains of child functioning: 1) social, 2) familial, and 3) emotional/behavioral. Dyads were randomized into either the Coping and Promoting Strength program (CAPS; n=70) or Information Monitoring (IM; n=66) comparison group. Multi-informant assessments were conducted at baseline, post intervention, and 6 and 12 months follow-ups. Random effects mixed models under the linear growth modeling (LGM) framework was used to assess the impact of CAPS on growth trajectories. Over time, children in the CAPS group had significantly lower anxiety, anxious/depressed symptoms, and lower total behavior problems (parent report), compared to children in IM group. The intervention did not impact other domains assessed (e.g., social functioning), which may be due to “floor effects” on these measures. Longitudinal follow-up data is needed to provide valuable information about this high risk population.
Keywords: Prevention, Child anxiety, High risk
Introduction
Anxiety disorders are the most common mental health problem in children, with an average prevalence rate of 10% [1 - 3]. Youth who suffer with an anxiety disorder typically have impairment in multiple domains of daily functioning. These domains include social (e.g., less peer acceptance, limited pro-social behaviors, more victimization) [4] and familial functioning (e.g., impaired relationships with parents and siblings) [5]. Anxious youth also experience high levels of distress, distorted cognitions, and deficits in self-concept and quality of life [6]. Youth with anxiety disorders are also likely to struggle with co-occurring internalizing and externalizing disorders/symptoms which can further impair important aspects of functioning [7]. Subthreshold anxiety is also clinically relevant, associated with functional impairment and when present at an early age, often continues to manifest into adulthood [8-10]
The high prevalence and negative consequences of excessive anxiety highlight the need for effective prevention programs. Addressing this need, a growing body of research has accumulated showing that anxiety prevention programs are promising. Two recent meta-analyses examined the effectiveness of preventive interventions for lowering anxiety symptoms. Fisak et al. (2011) [11] examined 35 studies evaluating preventive interventions for anxiety. The interventions varied in duration (e.g., the number of sessions across programs ranged from 1-31) and the majority was delivered in schools using a classroom or group format. Effect sizes for the reduction of anxiety symptoms at post-intervention ranged between d = −0.22 to 1.65, with a weighted overall effect size of d = 0.18. In the second meta-analysis, Teubert and Pinquart (2011) [12] examined 65 studies that reported on preventive interventions for both anxiety and depression and reported similar effect sizes for reduction of anxiety symptoms which ranged from −0.74 to 2.14 with a weighted mean effect size of Hedges g = 0.22 at the post evaluation and g = 0.19 at follow-up (8.2 months on average). The large range in effect sizes could be attributed to significant heterogeneity in sample size, program characteristics, target population, and publication bias [11]. Although anxiety prevention programs produce statistically small effect sizes since there tends to be less room for improvement in the short-term, given the potential long-term consequences associated with anxiety disorders, even small effect sizes have public health relevance when applied across the population [13].
While these meta-analyses found prevention programs reduced anxiety symptoms, whether they impact other important aspects of functioning (referred to hereafter as “spillover effects”) is a critical question. Answering this question will help us understand the broader impact of preventive interventions and other possible applications. To date, few studies have examined spillover effects of anxiety prevention programs. The current study addresses this knowledge gap. Among studies that have examined spillover effects, data are inconsistent. For instance, Dadds et al. (1997) [14] examined the effectiveness of a version of the Coping Koala: Prevention program (a 10 week school-based cognitive behavioral group intervention) in a sample of 128 children (7-14 years old) and found the intervention did not impact general behavior problems (as measured by the Child Behavior Checklist completed by parents) or parenting behaviors. In contrast, Siu (2007) [15] and Essau et al., (2012) [16] both found spillover effects for the FRIENDS program (a school-based 10 session intervention) on various measures of social, familial, and emotional functioning.
The current study adds to this literature by presenting multi-informant data (i.e., parent and child) on the effects of an anxiety prevention program on 1) social functioning (e.g., friendship quality), 2) family functioning, (e.g., interparental conflict, stress and sibling relationship quality), and 3) child emotional and behavioral functioning (e.g., internalizing, externalizing, and total behavior problems).
The intervention, Coping and Promoting Strength (CAPS), is a family-based selective anxiety prevention program targeting the offspring of clinically anxious parents. A description and rationale for this intervention has been published [17]. In the recently published efficacy trial of CAPS [18], 136 families were randomized equally to CAPS (n= 70) or an information monitoring control group (IM; n = 66). Primary outcomes were assessed at post intervention (or 9 weeks after randomization) and again at a 6 and 12 month follow-up by independent evaluators. Findings at the 12 month follow-up, indicated that 5% of the children who received CAPS developed an anxiety disorder, compared to 31% of children in the IM control group. Youth in IM, compared to CAPS, also had higher levels of anxiety symptoms (ADIS-Clinician Severity Rating [CSR]) based on the diagnostic interview at the one-year follow-up. Baseline child anxiety severity was a significant moderator. Significant mediators included parent psychopathology and parental modeling of anxiety [18]. In the present study, we hypothesized that, compared to children in the IM group, children in CAPS would show significantly greater improvements on all measures of functioning assessed.
Methods
Participants
One hundred and thirty-six dyads of clinically anxious parents and their non-anxious children were recruited using various methods of advertisement in the community. Children were 6 – 13 years old; m = 8.69 (SD = 1.8); 44.1% male, and 84.6% were Caucasian (6.6% were Black, 4.4% Latino, 2.9% Asian and 1.5% identified as “other”). Regarding family income, 78.7% reported earning over $80,000.00 per year. None of the children had medical or psychiatric conditions contraindicating the study intervention (e.g., suicidality) based on clinical interview nor were they currently receiving treatment for problematic anxiety. All parents had a current DSM-IV primary diagnosis of an anxiety disorder based on the Client Anxiety Disorders Interview Schedule for DSM-IV (ADIS) [19]. For the present study, at least one biological parent was required, there were no restrictions regarding family composition, and comorbid non-anxiety disorders were allowed for parents but had to be lower in severity than anxiety as determined by the ADIS - CSR [19]. Overall, 107 mothers and 29 fathers completed study questionnaires and diagnostic interviews. Additional enrollment criteria and sample characteristics are available elsewhere [18].
Intervention Conditions
Coping and Promoting Strength (CAPS)
Briefly, CAPS targeted offspring of anxious parents because familial aggregation studies have established that anxious parents are more likely to have anxious children [20] and these high risk youth also have a number of anxiety-related impairments (e.g., social, family and emotional/behavioral domains) [21]. A family-based model was used because parental psychopathology, parenting behaviors, and parent-child interactions have all been implicated in the etiology of pediatric anxiety disorders [22]. The CAPS intervention combined strategies from family-based cognitive behavior therapy (CBT) for anxiety disorders; interventions for offspring of depressed parents; and the ‘transfer of control’ intervention model for clinically anxious youth [23]. CAPS consisted of 8 weekly, 60 minute sessions and 3 optional monthly booster sessions. Each individual family met with a trained therapist. The intervention (described in Ginsburg, 2009) [17] targeted theory-driven modifiable child and parent anxiety risk factors through the acquisition of CBT skills. Children were taught to reduce anxiety by practicing relaxation strategies, behavioral exposure, cognitive restructuring, and problem solving. Parents were taught to reduce anxiety-promoting parenting behaviors by modeling adaptive coping, reducing accommodation, and decreasing overcontrol, overprotection, and hostility.
Information-Monitoring Condition (IM)
Dyads randomized to the IM condition were provided with a 36 page brochure published by the National Institute of Mental Health (2009) [24]. The brochure contained information related to anxiety disorders and the various treatments available. The publication did not include information about the anxiety reductions strategies that were included in the CAPS program. Measures of Spillover Effects
Social Measures
Friendship Quality Questionnaire
[25] is a 40-item child report measure that assesses children's perceptions of various qualitative aspects of their very best friendship. The measure has 6 factors (in addition to a total score): Validation and Caring, Conflict and Betrayal, Conflict Resolution, Help and Guidance, Companionship and Recreation, Intimate Exchange [26]. This study used the 10 item Validation and Caring subscale. For each item, children rate on a 1 (not at all true) to 5 (really true) scale the extent to which a particular quality was characteristic of their friendship (e.g., “_____ makes me feel good about my ideas,” “_____ and I always tell each other about our problems.”). Mean scores range from 0 – 5, higher scores indicate higher levels of friendship quality. At baseline this sample had a Cronbach's alpha of .90.
Friendship Questionnaire
[17] was created by study staff with the purpose of measuring the extent to which children are rejected or neglected by their peers. Parents and children individually completed the questionnaire by endorsing whether the child has experienced (yes/no) six troubling social situations (e.g., being teased, ignored, laughed at by peers). Scores range from 0 to 6 with higher scores indicating higher levels of peer rejection/neglect. Cronbach's alphas for parent and child measures for this sample were .68 and .72, respectively.
Family Measures
Parenting Stress Index
Short Form (PSI/SF) [27] is a 36 item parent-completed measure assesses parenting stress. Each item is rated on a 5 point Likert-type scale with a range of 1 (strongly disagree) to 5 (strongly agree). For this study, we examined the PSI Parent-Child Dysfunctional Interaction and Difficult Child subscales. The Dysfunctional Interaction subscale assesses parent's perception of their children's behavior during their interactions (e.g., “My child is not able to do as much as I expected”). The Difficult Child subscale surveys the parent's view of the child's temperament, defiance, noncompliance, and demandingness (e.g., “My child makes more demands on me than most children”). Each subscale consists of 12 items and subscales scores may range from 12 to 60. Higher scores indicate greater levels of dysfunction or difficulty. Cronbach's alpha coefficients for this sample were .80 for the Parent-Child Dysfunctional Interaction subscale scores and .85 for the Difficult Child subscale scores at baseline.
Sibling Relationships- Parent and Child
(SR) is a 22-item questionnaire comprised of items from the Sibling Relationships Questionnaire (SRQ) [28] and the Sibling Inventory of Behavior (SIB) [29]. Parents and children independently completed the questionnaire. Subscales included the Companionship/Involvement (e.g., “My sibling likes playing with me”) (6 items) and Conflict/Aggression subscales (e.g., “My sibling teases or annoys me”) (5 items). Items are rated on a 1 to 5 scale and are summed to yield a total score ranging from 6 to 30 and 5 to 25, respectively. Higher scores indicate better companionship and more conflict. Eighty study children had a sibling. Children enrolled in the study without any siblings did not complete the questionnaire. At baseline the Cronbach's alpha coefficients for this sample were .86 for both the Companionship/Involvement and Conflict/Aggression child subscales and .89 and .85 for the parent subscales.
Children's Perception of Interparental Conflict
Scale (CPIC) [30] is a 51-item scale that measures children's perception of interparental conflict. For this study, we examined the conflict frequency (e.g., “they may not think I know, but parents argue a lot”) and perceived threat (e.g., “get scared when my parents argue”) subscales. Each 6-item child-competed subscale is rated on a 3 point Likert-type scale including 1 (True), 2 (Sort of True) or 3 (False). Scores range from 6 to 18 with higher scores indicating lower perceived frequency of interparental conflict or lower perceived threat. At baseline, Cronbach's alpha for frequency and perceived threat subscales for this sample were .80 and .83, respectively.
Child Emotional and Behavioral Measures
The Child Behavior Checklist for Ages 6-18
(CBCL/6-18) [31] is one of the most widely used parent-report measures of psychopathology and includes 20 competence items. For this study, only the 113 specific behavioral/emotional items were used. Each item is rated on a 3 point scale including 0 (Not True) to 2 (Very True or Often True). Total scores range from 0 to 226, with a higher score indicating more behavior problems. In the present study, the Total Problems scale and 4 subscales were examined including: Withdrawn/Depressed, Anxious/Depressed, Social Problems and Attention Problems. The CBCL demonstrates excellent test-retest reliability and discriminates well between referred and non-referred samples [31]. This sample's Cronbach's alphas for the Withdrawn/Depressed, Anxious/Depressed, Social Problems, Attention Problems subscales and Total Problems scale were .76, .83, .70, .81 and .93, respectively.
Screen for Child Anxiety Related Emotional Disorders
(SCARED) [32]. The SCARED is a 41-item questionnaire measure of pediatric anxiety that has been demonstrated to differentiate between clinically anxious and non-anxious psychiatrically ill youth [32]. The parent and child each completed their own version of the SCARED. Parents and children individually respond to items describing the degree to which statements are true about their child/themselves using a 3-point Likert-type scale: 0 (not true or hardly ever true) to 2 (very true or often true). Total scores range from 0-82, with a clinical cut-off of 25 for children and parents. Higher scores reflected higher levels of anxiety. For this study we used the parent and child SCARED total scores. Cronbach's alphas for SCARED parent and child report were .91 and .89, respectively. The psychometric properties of this measure are favorable [33].
Self-Perception Profile for Children
[34] is a 36 item, child-report measure. In the current study, only the six item Global Self-Worth subscale was used. Each item contains opposing sides to a statement (e.g., Some kids like the kind of person they are BUT Other kids often wish they were someone else). Children select the side which they best identify with and then how true that statement is for them. Each item is scored on a one to four point scale 1 (Really true of me; low self-worth statement) to 4 (Really true of me; high self-worth statement) and subscale scores range from 0 – 24. Higher scores indicate a higher global self-worth. Cronbach's alpha for this subscale with the current sample was .73.
Parental Anxiety Measure
Anxiety Disorders Interview Schedule for DSM-IV
(ADIS) [35]. Parental diagnostic status was assessed using the ADIS, a semi-structured interview that is considered the best diagnostic instrument for adult anxiety disorders and is widely used in anxiety disorders treatment research. The ADIS has demonstrated good internal consistency and inter-rater reliability [36]. The interview assesses a broad range of DSM-IV disorders and screens for other disorders such as psychosis, substance abuse. Clinical Severity Ratings (CSR) are generated for each diagnosis (range = 0-8; a 4 is required to make a diagnosis). At baseline, parents mean total CSR score on their primary anxiety disorder was 5.6 with a standard deviation of 0.9
Procedure
Families were recruited for a study on the prevention of childhood anxiety disorders using a variety of advertisement platforms including local newspaper and radio as well as community flyers and mailings to local psychologists and psychiatrists. Interested families called study staff and completed a phone screen designed to assess preliminary study inclusion criteria. Families who passed the phone screen (i.e., child was within age range and had no psychiatric disorder or current treatment) completed an in-person baseline evaluation and, if eligible, were randomized to CAPS or IM (1:1 ratio, derived via randomization.com). Families were asked to complete a post evaluation (conducted approximately 9 weeks after randomization) as well as a 6 and 12 month follow-up visit. During each evaluation, families completed the battery of questionnaires described above. The Client ADIS and ADIS-C/P [37, 19] were also administered by an independent evaluator to determine parent and child diagnostic status respectively. Parents provided written informed consent for their own and their child's participation in the study. All children also provided informed assent. The study was approved and conducted in compliance with Institutional Review Board guidelines. See Ginsburg et al., (2015) [18] for a full description of the study procedures.
Statistical Analysis Plan
Chi-square and t-tests were conducted to examine differences between participants at baseline in the CAPS and IM groups on demographic and clinical variables. An intent-to-treat approach with the original 136 children was employed in examining intervention effects. Mplus (v. 7) [38] was utilized, using full-information maximum likelihood estimation [39] to handle missing data. Random effects mixed models under the linear growth modeling (LGM) framework was used to assess the impact of the CAPS on growth trajectories. Child age, gender, race, and family income were included in the models as controlling variables. We hypothesized that the slopes of trajectories would be significantly lower for the problem behavior or dysfunction variables (e.g., CBCL total problems, SCARED) and higher for the high functioning variables (e.g., global self-worth). One-tailed test was used. To adjust for multiple tests of the same domain of measures (e.g., family measures, child emotional and behavioral measures), the false discovery rate (FDR) [40], which controls for the expected proportion of false positives among all significant hypotheses, was applied. We interpreted effects as reliable if the FDR was ≤ .10. Following the formula suggested by Feingold (2009) [41], we calculated the model estimated effect sizes on Cohen's d associated with the difference between the CAPS and IM groups at the end of the study, adjusting for baseline differences. Lastly, differences between the CAPS and IM groups at each time point after the intervention were compared using analysis of covariance (ANCOVA), adjusting for the baseline scores, child age, gender, race, and family income.
Results
Baseline Group Comparisons and Descriptive Statistics
Chi –square and t tests revealed no differences between the participants in the CAPS group and participants in the IM group in terms of child age, gender, race or family income. There were also no baseline group differences on any clinical outcome measures (see Table 1) or on parent anxiety severity between the CAPS (M= 5.69 SD=0.79) or IM (M=5.59 SD=1.02 groups; t(134)= 0.607, p =0.545.
Table 1.
Descriptive statistics for each dependent variable by group at each time-point.
| Baseline Evaluation | Post Evaluation | 6 month follow-up | 12 month follow-up | |||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | ||||||||
| Treatment group | CAPS | IM | CAPS | IM | CAPS | IM | CAPS | IM |
| Social Measures | ||||||||
| Friendship Questions Parent- Total | 1.10 (1.59) | 1.53 (1.46) | 0.52 (0.97) | 0.85 (1.36) | 0.82 (1.11) | 0.64 (1.02) | 0.98 (1.53) | 1.12 (1.39) |
| Friendship Questions Child- Total | 1.34 (1.64) | 1.50 (1.74) | 0.69 (1.76) | 0.81 (1.08) | 1.18 (1.76) | 1.47 (2.28) | 0.57 (1.25) | 0.42 (.74) |
| Friendship Quality – Child | 4.43 (.59) | 4.23 (.82) | 4.47 (.49) | 4.18 (.82) | 4.45 (.60 | 4.32 (.63) | 4.49 (.50) | 4.50 (.52) |
|
Family Measures | ||||||||
| PSI Dysfunction | 21.47 (6.08) | 21.20 (7.87) | 19.63 (5.17) | 20.11 (5.99) | 18.17 (5.42) | 20.24 (6.72) | 19.32 (5.42) | 19.17 (6.09) |
| PSI Difficult child | 29.82 (7.62) | 30.13 (7.94) | 27.61 (7.75) | 28.29 (7.89) | 25.97 (8.15) | 27.3 (8.04) | 26.32 (7.42) | 26.83 (8.04) |
| CPIC - Frequency of Conflict | 13.72 (3.04) | 13.88 (2.92) | 14.69 (2.47) | 14.23 (3.12) | 15.12 (2.71) | 14.70 (2.81) | 15.30 (2.38) | 14.62 (2.88) |
| CPIC- Perceived Threat | 14.68 (3.57) | 14.59 (3.12) | 15.48 (3.03) | 15.37 (2.98) | 15.70 (3.01) | 15.36 (2.90) | 15.40 (3.39) | 15.82 (2.33) |
| SR - Comp/Involvement– Child | 16.56 (6.03) | 17.38 (5.85) | 18.03 (6.02) | 18.19 (6.56) | 19.49 (5.22) | 17.94 (6.85) | 18.66 (5.57) | 17.88 (5.80) |
| SR - Conflict/aggression– Child | 15.26 (5.04) | 15.23 (5.86) | 14.88 (4.18) | 13.78 (5.21) | 13.48 (5.41) | 13.71 (5.34) | 13.32 (4.84) | 13.38 (4.13) |
| SR - Comp/Involvement - Parent | 20.80 (5.05) | 22.26 (4.04) | 21.21 (5.07) | 21.92 (4.55) | 22.06 (4.42) | 21.11 (5.08) | 20.66 (4.66) | 22.51 (4.47) |
| SR - Conflict/aggression - Parent | 15.46 (3.87) | 14.41 (3.51) | 14.33 (2.97) | 14.00 (3.18) | 13.45 (3.31) | 14.00 (3.66) | 14.32 (2.93) | 13.72 (3.45) |
|
Child Emotional and Behavioral Measures | ||||||||
| CBCL- Total Problems | 29.97 (18.99) | 32.50 (19.08) | 22.65 (16.44) | 26.05 (15.66) | 16.81 (10.79) | 26.08 (19.64) | 18.74 (15.99) | 22.84 (16.92) |
| CBCL- Withdrawn/depressed | 1.49 (2.06) | 1.67 (2.10) | 1.04 (1.37) | 1.36 (1.73) | 0.87 (1.38) | 1.08 (1.40) | 0.98 (1.50) | 1.30 (1.55) |
| CBCL- Anxious/depressed | 6.01 (4.73) | 6.34 (4.35) | 4.67 (3.37) | 5.20 (3.87) | 3.79 (3.39) | 5.04 (4.20) | 3.49 (3.10) | 4.26 (3.83) |
| CBCL – Social Problems | 2.80 (2.86)) | 2.83 (2.69) | 2.29 (2.44) | 2.09 (2.38) | 1.43 (1.95) | 1.78 (2.01) | 2.11 (2.38) | 1.80 (2.19) |
| CBCL – Attention Problems | 3.75 (3.18) | 4.64 (4.03) | 3.05 (2.92) | 3.98 (3.23) | 2.06 (2.24) | 4.28 (3.90) | 2.56 (2.92) | 3.59 (3.79) |
| Harter- Global Self-Worth | 3.49 (.48) | 3.55 (.46) | 3.65 (.37) | 3.67 (.45) | 3.74 (.45) | 3.67 (.44) | 3.67 (.45) | 3.71 (.40) |
| SCARED Child Total | 19.84 (11.42) | 17.92 (11.11) | 14.21 (10.75) | 12.07 (9.19) | 11.84 (9.93) | 10.88 (8.27) | 13.15 (11.92) | 12.57 (10.37) |
| SCARED Parent Total | 18.45 (11.53) | 17.15 (10.95) | 13.69 (3.31) | 16.14 (10.16) | 12.76 (8.60) | 16.70 (13.33) | 11.98 (9.56) | 14.40 (11.82) |
-Bolded numbers indicate significant differences between CAPS and IM groups at the indicated time point
Social Domain
Table 2 shows the differences of the growth trajectories (i.e., linear slopes) between the two conditions and the corresponding p-value, FDR p-value, and the model estimated effect size. No significant differences were found for the Friendship Questionnaire (Parent and Child report) and Friendship Quality Questionnaire (child report).
Table 2.
Comparison of the Growth Rates between the CAPS and IM Groups
| Statistics | Unstandardized Growth trajectory Difference B(SE) | P value | FDR P value | Model Estimated Effect Size on Cohen's d |
|---|---|---|---|---|
| Social Measures | ||||
| Friendship Questions Parent- Total | .02(.03) | .26 | .46 | .23 |
| Friendship Questions Child- Total | .01(.07) | .46 | .46 | .08 |
| Friendship Quality - Child | −.003(.01) | .40 | .46 | −.06 |
| CPIC- Frequency | .09(.06) | .07 | .24 | .42 |
| CPIC – Perceived threat | −.01(.07) | .47 | .47 | −.04 |
| PSI Dysfunction | −.10(.13) | .22 | .35 | −.20 |
| PSI Difficult child | −.21(.16) | .09 | .24 | −.38 |
| SR- Comp/Involvement - Parent | −.19(.09) | .02 | .16 | −.58 |
| SR - Conflict/Aggression - Parent | .02(.08) | .43 | .47 | .08 |
| SR - Comp/Involvement – Child | .16(.14) | .13 | .26 | .38 |
| SR - Conflict/Aggression - Child | −.06(.12) | .32 | .43 | −.15 |
| CBCL- Total Problems | −.78(.28) | .003** | .02 | −.65 |
| CBCL- Withdrawn/depressed | −.04(.03) | .10 | .16 | −.27 |
| CBCL- Anxious/depressed | −.24(.12) | .02* | .08 | −.74 |
| CBCL – Social Problems | −.02(.05) | .33 | .39 | −.10 |
| CBCL – Attention Problems | −.10(.07) | .07 | .14 | −.39 |
| Harter- Global Self-Worth | 0.003(.01) | .39 | .39 | .09 |
| SCARED Child Total | −.08(.26) | .38 | .39 | −.10 |
| SCARED Parent Total | −.43(.24) | .03* | .08 | −.54 |
Family Domain
Based on the FDR p-values, the LGMs of the PSI, CPIC and child report on the SR subscales showed no significant differences of the growth trajectories (see Table 2).
Child Emotional and Behavioral Domain
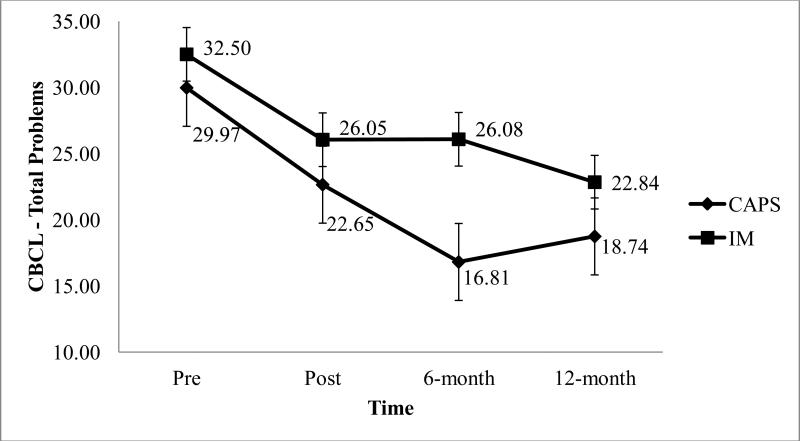
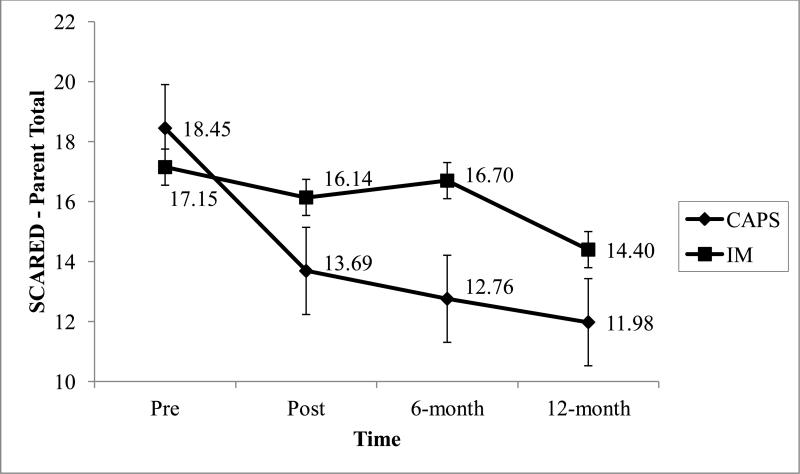
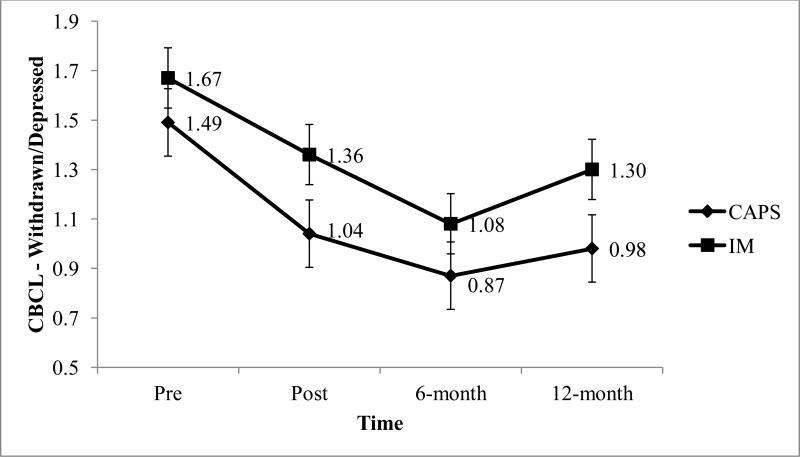
As shown on Table 2, there were three significant differences on the growth trajectories that had a FDR ≤ .10. Over time, children who received CAPS had significantly lower CBCL total problems (B = − 0.78, SEB = 0.28; adjusted Cohen's d = −.65), CBCL anxious and depressed problems (B = − 0.24, SEB = 0.12; adjusted Cohen's d = −.74), and Parent SCARED (B = − 0.43, SEB = 0.24; adjusted Cohen's d = −.54) compared to children in the IM condition. The adjusted mean scores and ANCOVA results for CBCL-Total Problems, CBCL-Anxious/Depressed Problems, and Parent report of SCARED at each of the post intervention assessments are presented in Table 3. Figures 1-3 illustrate the changes over time across groups for these three variables, respectively, using the observed means.
Table 3.
Adjusted Mean Scores and ANCOVA Results for CBCL-Total Problems, CBCL-Anxious/Depressed Problems, and Parent report of SCARED
| Time Point | Adjusted Estimated Means | Program Main Effect | t-Statistics | Cohen's d at the meana | |||
|---|---|---|---|---|---|---|---|
| CAPS | IM | Effect | P value | ||||
| CBCL-total | Post-intervention | 22.77 | 26.30 | −3.53(1.92) | −1.84 | .03 | −.31 |
| 6-month follow-up | 17.38 | 26.15 | −8.77(2.24) | −3.92 | <.001 | −.68 | |
| 12-month follow-up | 18.34 | 24.69 | −6.34(2.15) | −2.95 | <.001 | −.51 | |
| CBCL-Anxious/depressed | Post-intervention | 4.65 | 5.20 | −,55(.48) | −1.14 | .26 | −.20 |
| 6-month follow-up | 3.90 | 5.22 | −1.32(.54) | −2.44 | .01 | −.42 | |
| 12-month follow-up | 3.47 | 4.53 | −1.05(.55) | −1.91 | .03 | −.33 | |
| SCARED-Parent Report | Post-intervention | 13.14 | 16.85 | −3.71(129) | −2.87 | .002 | .50 |
| 6-month follow-up | 12.96 | 18.58 | −5.62(1.92) | −2.93 | .002 | −.51 | |
| 12-month follow-up | 11.59 | 15.58 | −3.99(1.76) | −2.26 | .01 | −.39 | |
Abbreviations: Cohen's d of the main effect, representing the effect size for baseline symptom scores were at the mean.
Figure 1.
Changes on the CBCL – Total Problems over time for the Coping and Promoting Strengths (CAPS) and Information Monitoring (IM) groups.
Figure 3.
Changes on the SCARED - Parent Version total score over time for the Coping and Promoting Strengths (CAPS) and Information Monitoring (IM) groups.
Discussion
The current study examined whether the Coping and Promoting Strength (CAPS) program, a preventive intervention designed to reduce current anxiety symptoms and prevent the onset of anxiety disorders in offspring of anxious parents, had an impact on three domains of child functioning. These domains included: 1) social functioning, 2) family functioning and 3) child emotional and behavioral problems. Findings indicated that youth receiving the CAPS intervention had lower anxiety symptoms and fewer total behavior problems (as reported by parents) over the course of the 14-month assessment period, compared to youth in the monitoring only condition. Contrary to the hypotheses, the program's benefits did not extend to the social or family measures that were assessed in this study.
The current study aimed to examine the impact of CAPS on children's social functioning, as anxiety has been associated with social impairments [42-44]. According to parent and child report, the intervention did not appear to have an impact on children's or parents’ perceptions of peer rejection or neglect (e.g., being teased by peers, not picked to be on a team) or children's relationship with their best friend (e.g., my best friend sticks up for me). Although the negative impact of elevated anxiety on children's social lives is well documented, Teubert and Pinquart, (2011) [12] reported mixed levels of effect sizes regarding prevention studies effects on social competence (−.08 to .15). Moreover, parents may struggle to accurately report on the quality of their children's friendships and social lives. Similar to other domains examined in this study, children's scores on the social impairment scales were low and likely in the normal range, again restricting room for scores to move over the course of the study.
With respect to the interventions impact on family functioning, across all post intervention time points, findings indicated that the intervention had no superior impact on the family functioning variables assessed compared to the control condition, and children in both groups did not show significant changes over time. Similar to children's emotional functioning most scores on the family measures (such as the PSI) were in the normal range. Therefore, score ranges for both groups are representative of a normal sample and likely had little room to improve. The sibling relationship and inter-parental conflict subscales do not have established cut offs, however scores from both groups indicated consistently low levels of sibling difficulties and inter-parental conflict at each time point.
The absence of group differences on these measures was unexpected for several reasons. First, parental anxiety-and elevated levels of child anxiety have been found to negatively impact family functioning [45-48]. Second, the intervention specifically targeted family interactions and parenting behaviors and included two individual parent sessions dedicated to reducing anxiety-promoting parenting behaviors. Third, anxiety treatment studies have found positive “spillover effect” to parents and family functioning [49-52], though other prevention studies have failed to find this effect [53]. We speculate that one reason for the null finding may be that these families, with children with subclinical anxiety had not yet experienced the impairment documented in families with a child who has an anxiety disorder [54]. Moreover, while some children did develop a disorder by the 12 month follow-up [18], perhaps the impact of anxiety on family interactions had not yet become prominent as these youth were “caught” early in the course of their illness. In order to further enhance the impact of the intervention on family functioning it may be that additional parent sessions are needed. Finally, examining additional aspects of family functioning (e.g., family accommodation) might be needed to detect the intervention's impact.
The most robust finding in this study was the positive effect of the intervention on reducing anxiety symptoms and total behavior problems. Youth who received the intervention were less likely to exhibit symptoms of anxiety such as feeling shy, nervous and/or scared and were less likely to be disobedient at home or act impulsively, compared to youth in the comparison condition. Specifically, children who received CAPS showed significantly larger reductions in anxious/depressed, anxiety and total behavior problems from baseline to the one year follow-up compared to children who were in the IM condition (corresponding to a between groups effect sizes of −.74, −.54, and −.65, respectively, on Cohen's d at one year follow-up).
These effect sizes are larger than most reported in meta-analyses of anxiety prevention studies which revealed an average effect size of .05 at 12 month follow-up for prevention interventions on anxiety symptoms (the range was d = −0.74 to 2.14) [55,11-12]. The effect sizes from CAPS were also favorable when compared to similar (e.g., study design, child age, number of sessions) cognitive behavioral prevention interventions (d = .17-.49) [14, 56 and 16]. Although according to parent report there was a significant intervention effect on anxiety symptoms (SCARED total score), child report did not result in the same effect. This finding is in accordance with the literature, as parents and children agreement on anxiety symptoms is low [57-61].
The positive impact on anxiety and behavior problems was expected as the intervention specifically targeted the core symptoms of anxiety including avoidant behavior, cognitive distortions, and physiological arousal. Specifically, CAPS modules included psychoeducation about the signs of anxiety, strategies for facing one's fears systematically through behavioral exposures, relaxation techniques, cognitive restructuring, and problem solving. Interestingly, the largest reduction in anxiety and overall problems occurred around the 6 month follow-up time point. These reductions, while still partially present, are not as strong by the 12 month follow-up. This pattern of finding suggests that booster sessions (which occurred in the CAPS group only prior to but not after the 6 month follow-up) may be warranted and may have bolstered the interventions impact at the 6 month time point. Alternatively, by the 6 month time point, participants may have had continued time to implement the skills and conduct exposures across situations in effect improving upon already realized gains. This is consistent with the aims of the intervention, which included skills that were intended to be implemented over time. The later worsening of symptoms at the 12 month follow-up could represent the natural waxing and waning of anxiety symptoms.
In contrast to the intervention's impact on anxiety symptoms and general behavior problems, the CAPS intervention did not affect other aspects of child emotional or behavioral functioning such as withdrawn/depressed symptoms (e.g., underactive, slow moving, or lacks energy), feelings of self-worth (e.g., feeling unhappy with oneself) or problems with attention (e.g., difficulty concentrating, unable to sustain attention). This finding is similar to studies examining other selective and universal anxiety prevention programs using similar methodology, samples and measures – many of which have also failed to find intervention spillover effects [14, 53].
Reasons for the non-significant impact of the intervention on these other areas of child behavioral and emotional functioning may be due to the restricted range of scores and related low statistical power, or that children's scores on these measures at each time point were, in general, within the “normal” range, suggesting a floor effect. Taken together, while CAPS was successful in reducing anxiety and overall behavior problems, additional intervention strategies or a more intensive focus on other domains may be needed to extend the impact of the intervention to other areas of emotional and behavioral functioning, where needed.
Limitations
While considering the strengths of the design, it is important to note several study limitations. The sample was predominantly Caucasian and from a high socioeconomic background. Individuals were also high functioning, looking for help with child anxiety prevention (rather than treatment and screened/excluded for the presence of an anxiety disorder) and willing to be involved in a research study as volunteers. These factors restrict the generalizability of findings. The limited age range of this sample and short duration of follow-up assessment (one year) did not allow children to be studied through stressful developmental risk periods (e.g., school transitions). Considering the chronicity of anxiety, a longer follow-up assessment window could provide additional insight into the fluctuation of anxiety symptoms over important life milestones. The measures used to assess outcomes were also limited both in scope and informant. Specially, social measures focused entirely on friends and friendship quality and lacked many other social components (e.g., quality of interactions with peers, behavior in public). The reliance on parent and child report is also noteworthy and future studies should incorporate more objective measures of functioning (e.g., teacher data, peer nominations, visits to the school nurse).
Future directions of anxiety prevention research should focus on recruiting larger and more diverse samples. This would allow for comparisons within and across different age and ethnic/racial groups. One way to address this could include multi-site projects with varying demographic makeups. For example, older children may have more complex and dynamic peer and family relationships [62]. Therefore one might expect to see larger changes on family and social measures. Similarly, as low socio economic status is a predictor of higher levels of anxiety symptoms and impairment [20], a more financially diverse sample may experience larger changes in functional outcomes after receiving the intervention.
Summary and Conclusions
The Child Anxiety Prevention Study examined the efficacy of a selective family-based anxiety prevention intervention, relative to an Information Monitoring control. The current study reported on the intervention's impact on children's social, familial and behavioral and emotional functioning. Across these domains, the intervention was successful in reducing anxiety severity and total behavior problems (both based on parent report) but did not impact other domains examined (social and family), which may be due to “floor effects” on these measures.
Figure 2.
Changes on the CBCL – Withdrawn/depressed subscale over time for the Coping and Promoting Strengths (CAPS) and Information Monitoring (IM) groups.
Acknowledgments
This study was supported by a NIMH grant (R01 MH077312) awarded to Dr. Golda Ginsburg by the National Institute of Mental Health.
References
- 1.Costello EJ, Egger HL, Angold A. Developmental epidemiology of anxiety disorders. In: Ollendick TH, March JS, editors. Phobic and Anxiety Disorders in Children and Adolescents: A Clinician's Guide to Effective Psychosocial and Pharmacological Interventions. Oxford University Press; New York: 2004. pp. 61–91. [Google Scholar]
- 2.Costello EJ, Egger HL, Angold A. The developmental epidemiology of anxiety disorders: phenomenology, prevalence, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2005;14:631–648. doi: 10.1016/j.chc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Velting ON, Setzer NJ, Albano AM. Anxiety disorders. In: Marsh DT, Fristad MA, editors. Handbook of Serious Emotional Disturbance in Children and Adolescents. Wiley; Hoboken: 2002. pp. 204–227. [Google Scholar]
- 4.Erath SA, Flanagan KS, Bierman KL. Social anxiety and peer relations in early adolescence: behavioral and cognitive factors. J Abnorm Child Psychol. 2007;35:405–416. doi: 10.1007/s10802-007-9099-2. [DOI] [PubMed] [Google Scholar]
- 5.Hudson JL, Rapee RM. Parent-child interactions in clinically anxious children and their siblings. J Clin Child Adolesc Psychol. 2002;31:548–555. doi: 10.1207/S15374424JCCP3104_13. [DOI] [PubMed] [Google Scholar]
- 6.Mendlowicz MV, Stein MB. Quality of life in individuals with anxiety disorders. Am J Psychiatry. 2014;157:669–682. doi: 10.1176/appi.ajp.157.5.669. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Capps L, Sigman M, Sena R, Heoker B, Whalen C. Fear, anxiety and perceived control in children of agoraphobic parents. J Child Psychol Psychiatr. 1996;37:445–452. doi: 10.1111/j.1469-7610.1996.tb01425.x. [DOI] [PubMed] [Google Scholar]
- 9.Whaley SE, Pinto A, Sigman M. Characterizing interactions between anxious mothers and their children. J Consult Clin Psychol. 1999;67:826. doi: 10.1037//0022-006x.67.6.826. [DOI] [PubMed] [Google Scholar]
- 10.Woodruff-Borden J, Morrow C, Bourland S, Cambron S. The behavior of anxious parents: examining mechanisms of transmission of anxiety from parent to child. J Clin Child Adolesc Psychol. 2002;31:364–374. doi: 10.1207/S15374424JCCP3103_08. [DOI] [PubMed] [Google Scholar]
- 11.Fisak BJ, Richard D, Mann A. The prevention of child and adolescent anxiety: a meta-analytic review. Prev Sci. 2011 doi: 10.1007/s11121-011-0210-0. [DOI] [PubMed] [Google Scholar]
- 12.Teubert D, Pinquart M. A meta-analytic review on the prevention of symptoms of anxiety in children and adolescents. J Anxiety Disord. 2011;25:1046–1059. [Google Scholar]
- 13.Rapee RM, Kennedy S, Ingram M, Edwards S, Sweeney L. Prevention and early intervention of anxiety disorders in inhibited preschool children. J Consult Clin Psych. 2005;73(3):488. doi: 10.1037/0022-006X.73.3.488. [DOI] [PubMed] [Google Scholar]
- 14.Dadds MR, Spence SH, Holland DE, Barrett PM, Laurens KR. Prevention and Early Intervention for Anxiety disorders: A controlled trial. J Consult Clin Psychol. 1997;65:627–635. doi: 10.1037//0022-006x.65.4.627. [DOI] [PubMed] [Google Scholar]
- 15.Siu AFY. Using FRIENDS to combat internalizing problems among primary school children in Hong Kong. J Cogn Behav Psychother. 2007;7:11–26. [Google Scholar]
- 16.Essau CA, Conradt J, Sasagawa S, Ollendick TH. Prevention of anxiety symptoms in children: results from a universal school-based trial. Behav Ther. 2012;43:450–564. doi: 10.1016/j.beth.2011.08.003. doi: 10.1016/j.beth.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Ginsburg G. The Child Anxiety Prevention Study: Intervention Model and Primary Outcomes. J Consult Clin Psychol. 2009;77:580–5887. doi: 10.1037/a0014486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ginsburg GS, Drake KL, Tein JY, Teetsel R, Riddle MA. Preventing the Onset of Anxiety Disorders in Offspring of Anxious Parents: A Randomized Controlled Trial of a Family-based Intervention. Am J Psychiatry. 2015 doi: 10.1176/appi.ajp.2015.14091178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown TA, Dinardo P, Barlow DH. Anxiety Disorders Interview Schedule Lifetime Version (ADIS-IV-L): Specimen Set (Includes Clinician Manual and 1 ADIS-IV-L Client Interview Schedule) Graywind Publications Inc.; Boulder: 1994. [Google Scholar]
- 20.Beidel DC, Turner SM. At risk for anxiety: I. Psychopathology in the offspring of anxious parents. J Am Acad Child Adolesc Psychiatry. 1997;36:918–924. doi: 10.1097/00004583-199707000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Manassis K, Hood J. Individual and familial predictors of impairment in childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry. 1998;37:428–434. doi: 10.1097/00004583-199804000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Ginsburg GS, Siqueland L, Masia-Warner C, Hedtke KA. Anxiety disorders in children: Family matters. Cogn Behav Pract. 2005;11:28–43. [Google Scholar]
- 23.Ginsburg GS, Silverman WK, Kurtines WK. Family Involvement in treating children with phobic and anxiety disorders: A look ahead. Clin Psychol Rev. 1995;15:457–473. [Google Scholar]
- 24.National Institute of Mental Health . Anxiety Disorders [brochure] National Institutes of Health; Bethesda: 2009. [Google Scholar]
- 25.Parker JG, Asher SR. Friendship and friendship quality in middle childhood: Links with peer group acceptance and feelings of loneliness and social dissatisfaction. Dev Psychol. 1993;29:611–621. [Google Scholar]
- 26.Nangle DW, Erdley CA, Newman JE, Mason CA, Carpenter EM. Popularity, friendship quantity, and friendship quality: Interactive influences on children's loneliness and depression. J Clin Child Adolesc Psychol. 2003;32:546–555. doi: 10.1207/S15374424JCCP3204_7. [DOI] [PubMed] [Google Scholar]
- 27.Abidin RR. In: Parenting Stress Index Manual. 3rd ed Lutz FL, editor. Psychological Assessment Resources Inc.; Odessa: 1995. [Google Scholar]
- 28.Furman W, Buhrmester D. Children's perceptions of the personal relationships in their social networks. Dev Psychol. 1985;21:1016–1024. doi: 10.1037/0012-1649.21.6.1016. [Google Scholar]
- 29.Volling BL, Blandon AY. Positive indicators of sibling relationship quality: The Sibling Inventory of Behavior. In: Lippman LH, editor. What do children need to flourish: Conceptualizing and measuring indicators of positive development. New York. Springer Science + Business Media; 2005. pp. 203–219. [Google Scholar]
- 30.Grych JH, Seid M, Fincham FD. Assessing marital conflict from the child's perspective: The Children's Perception of Interparental Conflict Scale. Child Dev. 1992;63:558–572. doi: 10.1111/j.1467-8624.1992.tb01646.x. [DOI] [PubMed] [Google Scholar]
- 31.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. University of Vermont; Burlington: 2001. [Google Scholar]
- 32.Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 33.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 34.Harter S. Manual for the Self-Perception Profile for Children. University of Denver; Denver: 1985. [Google Scholar]
- 35.Brown TA, DiNardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV. Graywind Publications; New York: 1994. [Google Scholar]
- 36.Di Nardo P, Moras K, Barlow D. Reliability of DSM-III-R anxiety disorder categories: Using the Anxiety Disorders Interview Schedule-Revised (ADIS-R). Arch Gen Psychiatry. 1993;50:251–256. doi: 10.1001/archpsyc.1993.01820160009001. [DOI] [PubMed] [Google Scholar]
- 37.Silverman WK, Albano AM. The anxiety disorders interview schedule for DSM-IV – child and parent versions. Psychological Corporation; San Antonio: 1996. [Google Scholar]
- 38.Muthén LK, Muthén BO. Mplus User's Guide. Seventh Edition Muthén & Muthén; Los Angeles, CA: 1998-2012. [Google Scholar]
- 39.Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling: Issues and Techniques. Lawrence Erlbaum Associates; Mahwah, NJ: 1996. [Google Scholar]
- 40.Benjamini Y, Hochberg Y. On the adaptive control of the false discovery rate in multiple testing with independent statistics. J Educ Behav Stat. 2000;25:60–83. [Google Scholar]
- 41.Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ginsburg GS, La Greca AM, Silverman WK. Social anxiety in children with anxiety disorders: relation with social and emotional functioning. J Abnorm Child Psychol. 1998;26:175–185. doi: 10.1023/a:1022668101048. [DOI] [PubMed] [Google Scholar]
- 43.Strauss CC, Frame CL, Forehand R. Psychosocial impairment associated with anxiety in children. J Clin Child Psychol. 1987;16:235–239. [Google Scholar]
- 44.Essau CA, Conradt J, Petermann F. Frequency, comorbidity, and psychosocial impairment of anxiety disorders in German adolescents. J Anxiety Disord. 2000;14:263–279. doi: 10.1016/s0887-6185(99)00039-0. [DOI] [PubMed] [Google Scholar]
- 45.Bögels SM, van Oostern A, Muris P, Smulders D. Familial correlates of social anxiety in children and adolescents. Behav Res Ther. 2001;39:273–287. doi: 10.1016/s0005-7967(00)00005-x. [DOI] [PubMed] [Google Scholar]
- 46.Nomura Y, Wickramaratne PJ, Warner V, Mufson L, Weissman MM. Family Discord, Parental Depression, and Psychopathology in Offspring: Ten-Year Follow-up. J Am Acad Child and Adolesc Psychiatry. 2002;41:402–409. doi: 10.1097/00004583-200204000-00012. [DOI] [PubMed] [Google Scholar]
- 47.Kiliç EZ, Özgüven HD, Sayil I. The psychological effects of parental mental health on children experiencing disaster: the experience of Bolu earthquake in Turkey. Fam Process. 2003;42:485–495. doi: 10.1111/j.1545-5300.2003.00485.x. [DOI] [PubMed] [Google Scholar]
- 48.Katz LF, Low SM. Marital violence, co-parenting, and family-level processes in relation to children's adjustment. J Fam Psychol. 2004;18:372–382. doi: 10.1037/0893-3200.18.2.372. [DOI] [PubMed] [Google Scholar]
- 49.Kendall PC. Child and Adolescent Therapy: Cognitive Behavioral Procedures. Guilford Press; New York: 2012. [Google Scholar]
- 50.Hudson JL, Rapee RM. Familial and social environments in the etiology and maintenance of anxiety disorders. In: Antony MM, Stein MB, editors. Oxford Handbook of Anxiety and Related Disorders. Oxford University Press; New York: 2009. pp. 173–189. [Google Scholar]
- 51.Silverman WK, Kurtines WM, Jaccard J, Pina AA. Directionality of change in youth anxiety treatment involving parents: an initial examination. J Consult Clin Psychol. 2009;77:474–485. doi: 10.1037/a0015761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Keeton CP, Ginsburg GS, Drake KL, Sakolsky D, Kendall PC, Birmaher B. Benefits of Child-focused Anxiety Treatments for Parents and Family Functioning. Depress Anxiety. 2013;30:865–872. doi: 10.1002/da.22055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dadds MR, Roth JH. Prevention of anxiety disorders: Results of a universal trial with young children. J Child Fam Stud. 2008;17:320–335. [Google Scholar]
- 54.Kisely S, Scott A, Denney J, Simon G. Duration of untreated symptoms in common mental disorders: association with outcomes International study. Br J Psychiatry. 2006;189:79–80. doi: 10.1192/bjp.bp.105.019869. [DOI] [PubMed] [Google Scholar]
- 55.Neil AL, Christensen Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin Psychol Rev. 2009;29:208–215. doi: 10.1016/j.cpr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 56.Balle M, Tortella-Feliu M. Efficacy of a brief school-based program for selective prevention of childhood anxiety. Anxiety Stress Coping. 2010;23:71–85. doi: 10.1080/10615800802590652. [DOI] [PubMed] [Google Scholar]
- 57.Choudhury MS, Pimentel SS, Kendall PC. Childhood anxiety disorders: parent-child (dis)agreement using a structured interview for the DSM-IV. J Am Acad Child Adolesc Psychiatry. 2003;42:957–964. doi: 10.1097/01.CHI.0000046898.27264.A2. [DOI] [PubMed] [Google Scholar]
- 58.Comer JS, Kendall PC. A symptom-level examination of parent–child agreement in the diagnosis of anxious youths. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(7):878–886. doi: 10.1097/01.chi.0000125092.35109.c5. [DOI] [PubMed] [Google Scholar]
- 59.DiBartolo PM, Albano AM, Barlow DH, Heimberg RG. Crossinformant agreement in the assessment of social phobia in youth. J Abnorm Child Psychol. 1998;26:213–220. doi: 10.1023/a:1022624318795. [DOI] [PubMed] [Google Scholar]
- 60.Grills AE, Ollendick TH. Issues in parent–child agreement: the case of structured diagnostic interviews. Clin Child Fam Psychol Rev. 2002;5:57–83. doi: 10.1023/a:1014573708569. [DOI] [PubMed] [Google Scholar]
- 61.Rubio-Stipec M, Canino GJ, Shrout P, Dulcan M, Freeman D, Bravo M. Psychometric properties of parents and children as informants in child psychiatry epidemiology with the Spanish Diagnostic Interview Schedule for Children (DISC. 2). J Abnorm Child Psychol. 1994;22:703–720. doi: 10.1007/BF02171997. [DOI] [PubMed] [Google Scholar]
- 62.La Greca AM, Lopez N. Social anxiety among adolescents: Linkages with peer relations and friendships. J Abnorm Child Psychol. 1998;26:83–94. doi: 10.1023/a:1022684520514. [DOI] [PubMed] [Google Scholar]