Abstract
Antibiotic resistance is steadily rising worldwide. Respiratory tract infections (RTIs) are common indications, mostly imprudent, for antibiotic prescriptions in outpatient setting. In Korea, antibiotic prescription rate for RTIs is still high. As physician visit and antibiotic prescribing are influenced by patient's perceptions and beliefs, we aimed to explore the general public's perspectives and practices toward RTIs and to develop the ‘RTI clinical iceberg.’ A cross-sectional survey was conducted in Wonju Severance Christian Hospital (WSCH) among 550 adults attending outpatient departments during January 2016. Differences in distributions between groups were examined using two-tailed Pearson χ2 test. Using the Andersen's behavioral model as a conceptual framework, we constructed logistic regression models to assess factors associated with physician visit. Of 547 participants with complete questionnaires, 62.9% reported having experienced an RTI in the previous six months; 59.3% visited a physician for the illness, most commonly because the symptoms were severe or prolonged, and approximately 16% of them expected an antibiotic prescription from the visit. Perceptions of symptoms severity, the need factor, most strongly influenced physician visit. Predisposing and enabling factors such as inappropriate expectations for antibiotic for a sore throat or having national health insurance also influenced physician visit. Almost all participants who reported asking for an antibiotic were prescribed one, with a 37.1% non-adherence rate. Conclusively, public education on self-care for RTI symptoms that addresses their main concerns may reduce physician visits. Improving physician-patient relationship and informing patients about the lack of antibiotic benefit for most RTIs may also reduce antibiotic prescriptions.
Keywords: Antibiotics, Respiratory Tract Infections, Expectations, Physician Visit, Attitudes, Practices, Adherence, South Korea
Graphical Abstract
INTRODUCTION
Antibiotic resistance is a serious global concern with steady rise that has reduced the effectiveness of current treatments for common infectious diseases (1). While overuse of antibiotics accelerates the emergence of resistance, prudent lower use slows down this trend (2,3). Acute respiratory tract infections (RTIs) are the most common illnesses experienced worldwide (4), accounting for numerous visits to physicians and imprudent prescriptions of antibiotics (2). As these infections are largely viral and self-limiting, antibiotics offer little benefit for these conditions (5,6). Globally, concerted efforts targeting both clinicians and the public have been implemented in order to reduce the antibiotic prescription rate and expectations for antibiotics in RTIs (7,8).
In Korea, antibiotic resistance rates are particularly high (9,10). Thus, various and relatively effective health policies have been implemented to promote the prudent use of antibiotics, particularly for acute RTIs. These policies include separation of prescribing from dispensing, public educational campaigns, and public disclosure of physicians' antibiotic prescriptions (11,12,13). Despite a significant decrease in the past decade, the antibiotic prescription rate in Korea remains higher than the rates in other developed countries (14). In addition, there is a steady upward trend for total consumption of antibiotics, with significantly higher rates in outpatient settings (15). Furthermore, despite public educational campaigns, the general public still has misconceptions and poor attitudes toward antibiotic efficacy and use (16).
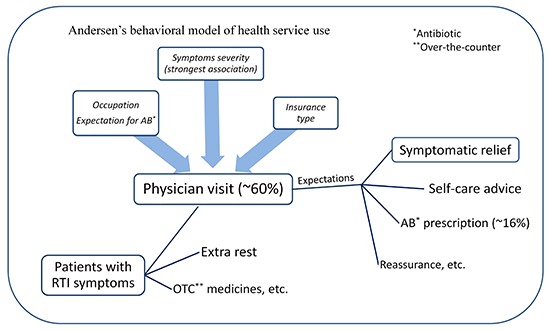
Multifaceted coordinated interventions that facilitate behavior change in both patients and clinicians are generally more successful in addressing the problem of imprudent antibiotic prescriptions (17). However, little is known about the Korean general public's expectations for consultations and antibiotics in RTIs (18). As improved understanding of individual patient's perspective and his/her journey through an RTI illness can help physicians make better shared decisions and develop multifaceted interventions (19), we aimed to develop a description of the components of the ‘RTI clinical iceberg’ (20) by exploring the practices, expectations, and adherence of the general public toward RTIs and antibiotics. Furthermore, the Andersen's behavioral model of healthcare utilization (21) was used as the conceptual framework to identify factors associated with intention to visit a physician. The model suggests that healthcare utilization is influenced by three main decision components: predisposing factors (including socio-demographic characteristics and health/disease knowledge and attitudes), enabling factors (including family and community resources, accessibility, and availability), and need factors as the most immediate cause of healthcare use (including perceived/evaluated health status and severity of symptoms). This model may help better explain different health-seeking behaviors.
MATERIALS AND METHODS
Study setting and design
This facility-based cross-sectional study surveyed individuals visiting Wonju Severance Christian Hospital (WSCH) during January 2016. The survey formed part of a larger comparative study performed in January and February 2016 between two cities in Korea and Iran in terms of knowledge, attitudes, and practices of the general public towards antibiotic use and RTIs.
WSCH, located in Wonju city, is the largest hospital in Gangwon province, Korea. It is a general hospital and the final step for all patients referred from across the province. As Gangwon province has been reported to have the highest rate (48.9% in 2012) (22) of antibiotic prescription for acute RTIs, WSCH was chosen to represent various socioeconomic backgrounds within the province.
A cross-sectional interview study using a validated structured questionnaire was conducted among the general public (patients and companions) attending outpatient departments at WSCH. Research assistants collected data. To maintain the quality of data collection and standardization, all interviewers were thoroughly trained. In addition, supervisors frequently controlled the process and quality of data collection.
Study population and sampling
Attendees of WSCH were defined as the study unit. There were three inclusion criteria: 1) adult (≥ 18 years of age); 2) having used antibiotics (self-medication or been prescribed in outpatient setting) in the past year; and 3) living in Gangwon province. The participants were selected using convenience sampling, trying to include different age groups and both sexes.
In consideration of the larger concurrent comparative study and the sample size formula for hypothesis testing for two population proportions, it was necessary to sample 550 individuals in each field for a margin of error of 0.05 at a 95% confidence interval (CI). A 5%–6% expected rate of incomplete response was also considered.
Where = 1.96, = 1.28 for 90% power, p1 = proportion in one population, p2 = proportion in the other population, q1 = 1 − p1, q2 = 1 − p2, = average of p1 and p2, = average of q1 and q2; the minimum effect size (p1 − p2) considered to be significant was 0.1.
Survey questionnaire
The questionnaire was developed mostly from previous studies with similar objectives (16,20,23), so that face and content validity were assured. However, the questions were also assessed and slightly rephrased according to the study objectives by a pharmacist and a physician with clinical expertise. Additionally, the questionnaire was pre-tested in a pilot study and amended before being used for the interviews. It was first developed in English and then translated into Korean.
The questionnaire consisted of two main parts: 1) the interviewer-administered part had three sub-sections: (a) practice of antibiotic use, (b) knowledge and attitudes towards antibiotic use and antibiotic resistance, and (c) management of RTIs; and 2) the self-administered part assessed ten socio-demographic characteristics of the participants. The questionnaire consisted of both closed questions (multiple-choice, Likert scale) and one open question.
In sub-section (a), participants were asked about their practice of asking a doctor to prescribe antibiotics for any condition in the past year, if any, and the result, as well as their practice of taking antibiotics as prescribed in the past year. In sub-section (b), participants were then asked to rate (from strongly agree to strongly disagree) a number of statements about antibiotic efficacy and indications. They were also asked to share their opinions on the problem of antibiotics side effects. In sub-section (c), participants were asked about their expectations of being prescribed antibiotics if they visit a doctor with different RTI symptoms, and their perceptions of antibiotics effectiveness for different RTI symptoms. Then, they were asked whether they had had sore throat, cold, cough, or flu symptoms in the past six months; how the symptoms of recent RTI affected their general health; the actions they took as a result; and their reasons and expectations for consultation in case they had visited a doctor for their most recent RTI.
In the self-administered questionnaire, the socio-demographic characteristics of the participants, including sex, age, education level, marital status, occupation, and average monthly income quintiles were recorded. Participants also answered questions about type of health insurance, self-rated health, and history of chronic disease. The questions regarding education level, occupation, income quintiles, and type of health insurance were taken from the Community Health Survey in Korea (24).
Statistical methods
Data were entered into Epi Info, version 7 (Centers for Disease Control and Prevention, Atlanta, GA, USA) (25). Data management and all analyses were performed using IBM SPSS Statistics for Windows, version 20.0 (IBM, Armonk, NY, USA) (26). We checked the database for missing values and monotonous answers. Knowledge and attitude answers were coded as either correct or incorrect; responses of ‘Strongly agree’ and ‘Agree’ were coded as ‘Agree,’ and responses of ‘Strongly disagree’ and ‘Disagree’ were coded as ‘Disagree,’ and ‘Don't know/No opinion’ responses were considered incorrect responses. Descriptive measures included percentages and corresponding 95% CIs or means ± standard deviation (SD), as appropriate. Differences in distribution between groups were examined using two-tailed Pearson χ2 tests. All variables were then considered for bivariate logistic regression models. Those with P < 0.2 in the crude models were included in the multivariate logistic regression analyses, where physician visit was the dependent variable and three sets of factors (predisposing, enabling, and needs) were included in the final model in separate blocks. A P < 0.05 was considered statistically significant in the adjusted model.
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board of Yonsei University Wonju College of Medicine (Approval No. YWMR-15-0-063). All participants were informed about the survey purpose and provided verbal consent at the beginning of the survey. They were also read a statement about their voluntary participation. As the interview was rather long, participants were given a small remuneration with completion of the questionnaire. They were able to quit the interview at any time. No personal identifiers were included in the database.
RESULTS
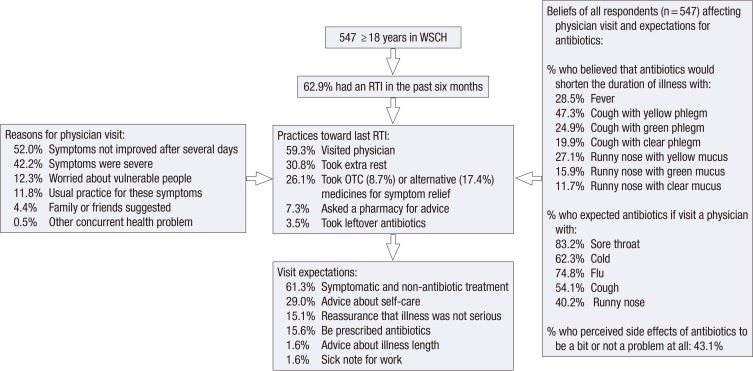
Of all consumers surveyed, 547 completed the survey (response rate 99.5%). Of them, 344 (62.9% [95% CI, 58.7%–66.9%]) reported RTI symptoms in the past six months (Fig. 1); these symptoms included cold (68.6%), sore throat (36.9%), cough (27.6%), and flu symptoms (7.0%); with cough, runny or stuffy nose, throat pain, body aches, and fever as the main complaints.
Fig. 1.
The RTI journey of patients: their practices, reasons for physician visit, expectations, beliefs, and attitudes.
RTI = respiratory tract infection, WSCH = Wonju Severance Christian Hospital, OTC = over-the-counter.
Practices toward the most recent RTI symptoms
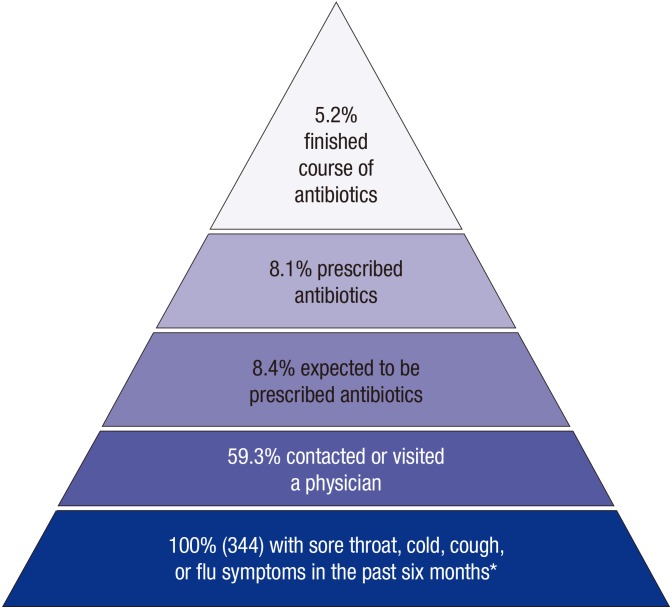
Of the 344 adults with recent RTI symptoms, more than half reported visiting a physician (59.3%; 95% CI, 53.9%–64.5%) (Fig. 2), 30.8% took extra rest, 26.1% reported taking over-the-counter (OTC) medicines or alternative treatments (including home remedies) to relieve their symptoms, 7.3% asked for advice at a pharmacy, and 3.5% self-medicated with leftover antibiotics (Fig. 1). Simply waiting for symptoms to resolve and drinking more water were among the other actions mentioned.
Fig. 2.
The respiratory tract infection (RTI) clinical iceberg.
*The denominator for all percentages is 344.
Reasons for visiting a physician
Of the 204 participants who had visited a physician for their recent RTI, 42.2% reported symptom severity as the reason for their visit, 52.0% reported that symptoms had not improved after several days, 12.3% visited a physician because they worried about infecting others, particularly children and the elderly, and 11.8% because they usually visited a physician for those symptoms (Fig. 1). There was also an attitude among some of the participants that ‘early treatment is better’; they were considered to be patients with high consultation behavior who usually visit a physician for minor symptoms.
Effect of socio-demographic characteristics on physician visit
Of those with an RTI in the past six months, middle-aged/elderly women were more likely to have visited a physician (P = 0.023). However, women who were students or had occupations other than employment were significantly less likely to visit a physician (P = 0.036). There was a similar trend for all participants in terms of occupation. Further, married participants were marginally more likely to visit a physician. There were no significant differences by sex, education level, family income level, or health insurance type (Table 1).
Table 1. Characteristics of study participants with an RTI in the past six months by physician visit; total and stratified by sex.
| Characteristics | Physician visit | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||||||
| Did not visit (n = 140) | Visited (n = 204) | Total (n = 344) | P value | Did not visit (n = 53) | Visited (n = 80) | Total (n = 133) | P value | Did not visit (n = 87) | Visited (n = 124) | Total (n = 211) | P value | |
| Sex | 0.822 | NA | NA | |||||||||
| Male | 53 (39.8) | 80 (60.2) | 133 (38.7) | |||||||||
| Female | 87 (41.2) | 124 (58.8) | 211 (61.3) | |||||||||
| Age, yr | 0.388 | 0.601 | 0.023 | |||||||||
| ≤ 24 | 13 (56.5) | 10 (43.5) | 23 (6.7) | 3 (27.3) | 8 (72.7) | 11 (8.3) | 10 (83.3) | 2 (16.7) | 12 (5.7) | |||
| 25–39 | 25 (41.0) | 36 (59.0) | 61 (17.7) | 10 (50.0) | 10 (50.0) | 20 (15.0) | 15 (36.6) | 26 (63.4) | 41 (19.4) | |||
| 40–59 | 54 (37.5) | 90 (62.5) | 144 (41.9) | 16 (36.4) | 28 (63.6) | 44 (33.1) | 38 (38.0) | 62 (62.0) | 100 (47.4) | |||
| ≥ 60 | 48 (41.4) | 68 (58.6) | 116 (33.7) | 24 (41.4) | 34 (58.6) | 58 (43.6) | 24 (41.4) | 34 (58.6) | 58 (27.5) | |||
| Education level | 0.746 | 0.864 | 0.417 | |||||||||
| < High school | 34 (38.6) | 54 (61.4) | 88 (25.6) | 14 (40.0) | 21 (60.0) | 35 (26.3) | 20 (37.7) | 33 (62.3) | 53 (25.1) | |||
| High school | 55 (43.3) | 72 (56.7) | 127 (36.9) | 17 (37.0) | 29 (63.0) | 46 (34.6) | 38 (46.9) | 43 (53.1) | 81 (38.4) | |||
| University | 51 (39.5) | 78 (60.5) | 129 (37.5) | 22 (42.3) | 30 (57.7) | 52 (39.1) | 29 (37.7) | 48 (62.3) | 77 (36.5) | |||
| Marital status | 0.071 | 0.386 | 0.101 | |||||||||
| Married | 104 (38.2) | 168 (61.8) | 272 (79.1) | 39 (37.9) | 64 (62.1) | 103 (77.4) | 65 (38.5) | 104 (61.5) | 169 (80.1) | |||
| Others | 36 (50.0) | 36 (50.0) | 72 (20.9) | 14 (46.7) | 16 (53.3) | 30 (22.6) | 22 (52.4) | 20 (47.6) | 42 (19.9) | |||
| Occupation | 0.071 | 0.792 | 0.036 | |||||||||
| Employed | 72 (38.5) | 115 (61.5) | 187 (54.4) | 34 (39.1) | 53 (60.9) | 87 (65.4) | 38 (38.0) | 62 (62.0) | 100 (47.4) | |||
| Unemployed/retired/housewife/man | 55 (40.1) | 82 (59.9) | 137 (39.8) | 14 (38.9) | 22 (61.1) | 36 (27.1) | 41 (40.6) | 60 (59.4) | 101 (47.9) | |||
| Student/other | 13 (65.0) | 7 (35.0) | 20 (5.8) | 5 (50.0) | 5 (50.0) | 10 (7.5) | 8 (80.0) | 2 (20.0) | 10 (4.7) | |||
| Family income* | 0.952 | 0.779 | 0.768 | |||||||||
| ≤ 100 | 16 (40.0) | 24 (60.0) | 40 (11.6) | 6 (37.5) | 10 (62.5) | 16 (12.0) | 10 (41.7) | 14 (58.3) | 24 (11.4) | |||
| 100–200 | 19 (38.0) | 31 (62.0) | 50 (14.5) | 11 (39.3) | 17 (60.7) | 28 (21.1) | 8 (36.4) | 14 (63.6) | 22 (10.4) | |||
| 200–300 | 31 (42.5) | 42 (57.5) | 73 (21.2) | 13 (50.0) | 13 (50.0) | 26 (19.6) | 18 (38.3) | 29 (61.7) | 47 (22.3) | |||
| 300–400 | 32 (43.8) | 41 (56.2) | 73 (21.2) | 7 (31.8) | 15 (68.2) | 22 (16.5) | 25 (49.0) | 26 (51.0) | 51 (24.2) | |||
| ≥ 400 | 42 (38.9) | 66 (61.1) | 108 (31.4) | 16 (39.0) | 25 (61.0) | 41 (30.8) | 26 (38.8) | 41 (61.2) | 67 (31.8) | |||
| Insurance type | 0.141 | 0.545 | 0.164 | |||||||||
| NHI | 56 (36.4) | 98 (63.6) | 154 (44.8) | 23 (37.1) | 39 (62.9) | 62 (46.6) | 33 (35.9) | 59 (64.1) | 92 (43.6) | |||
| Private/Medicaid | 84 (44.2) | 106 (55.8) | 190 (55.2) | 30 (39.8) | 41 (57.7) | 71 (53.4) | 54 (45.4) | 65 (54.6) | 119 (56.4) | |||
| Self-rated health | 0.733 | 0.970 | 0.475 | |||||||||
| Good | 46 (38.7) | 73 (61.3) | 119 (34.6) | 18 (40.9) | 26 (59.1) | 44 (33.1) | 28 (37.3) | 47 (62.7) | 75 (35.5) | |||
| Fair | 74 (42.8) | 99 (57.2) | 173 (50.3) | 28 (38.9) | 44 (61.1) | 72 (54.1) | 46 (45.5) | 55 (54.5) | 101 (47.9) | |||
| Poor | 20 (38.5) | 32 (61.5) | 52 (15.1) | 7 (41.2) | 10 (58.8) | 17 (12.8) | 13 (37.1) | 22 (62.9) | 35 (16.6) | |||
| Chronic disease | 0.860 | 0.749 | 0.942 | |||||||||
| Yes | 57 (40.1) | 83 (41.1) | 142 (41.3) | 25 (38.5) | 40 (61.5) | 65 (48.9) | 32 (41.6) | 45 (58.4) | 77 (36.5) | |||
| No | 83 (59.9) | 119 (58.9) | 202 (58.7) | 28 (41.2) | 40 (58.8) | 68 (51.1) | 55 (41.0) | 79 (59.0) | 134 63.5) | |||
Values are presented as number (%).
RTI = respiratory tract infection, NHI = National Health Insurance.
*Income quintiles adopted from Community Health Survey 2013 (24) for monthly average; unit is 10,000 KRW.
Effect of perceptions, beliefs, and attitudes on physician visit
Survey participants whose health was severely affected by their recent RTI illness were more likely to have visited a physician (73.0%), compared to those who were moderately (51.9%) or mildly (24.1%) affected (P for trend < 0.001). No participant reported not being affected at all. Further sub-analyses showed that middle-aged women were marginally more likely to report being severely affected by their recent RTI illness (age groups: ≤ 24 years, 25.0%; 25–39 years, 61.0%; 40–59 years, 50.0%; ≥ 60 years, 36.2%; P = 0.062). Likewise, women with higher education levels were significantly more likely to report being severely affected than those with lower education levels (education level: less than high school, 37.7%; high school completed, 46.9%; university, 53.2%; P for trend = 0.014). Intriguingly, there were no notable differences by sex or chronic disease history.
Of all 547 participants surveyed, 37.5% believed that antibiotics work on most coughs and colds, 60.9% that antibiotics can kill viruses, and 58.3% that common cold is cured more quickly with antibiotics. Of the 344 survey participants with RTI in the past six months, those who had a sensible view and disagreed that ‘common cold is cured more quickly with antibiotics’ were marginally less likely to visit a physician (51.9% of those with correct response vs. 62.7% of those with incorrect response; P = 0.057) (Table 2).
Table 2. Relationship between perceptions and beliefs of participants with an RTI in the past six months and physician visit.
| Characteristics | Physician visit | |||
|---|---|---|---|---|
| Did not visit (n = 140) | Visited (n = 204) | Total (n = 344) | P value | |
| Symptoms severity | < 0.001 | |||
| Severe | 43 (27.0) | 116 (73.0) | 159 (46.2) | |
| Moderate | 75 (48.1) | 81 (51.9) | 156 (45.3) | |
| Mild | 22 (75.9) | 7 (24.1) | 29 (8.4) | |
| Antibiotic effectiveness | 0.240 | |||
| Cough/runny nose with sputum | 115 (39.4) | 177 (60.6) | 292 (84.9) | |
| Other symptoms | 25 (48.1) | 27 (51.9) | 52 (15.1) | |
| Antibiotic side effects | 0.157 | |||
| Not or a bit of a problem | 74 (44.6) | 92 (55.4) | 166 (48.3) | |
| Moderate or major problem | 66 (37.1) | 112 (62.9) | 178 (51.7) | |
Values are presented as number (%).
RTI = respiratory tract infection.
We found that 83.2% of all participants would expect a physician to prescribe an antibiotic if they visited him for a sore throat, 74.8% for flu symptoms, 62.3% for a cold, 54.1% for a cough, and 40.2% for a runny nose. Of the 344 survey participants with RTI in the past six months, 97.7% (n = 336) reported that they would expect a physician to prescribe an antibiotic if they visit him for an RTI. However, they were more likely to visit a physician for their recent RTI if they reported that they would expect a physician to prescribe an antibiotic for a sore throat (61.6% vs. 47.3%; P = 0.048). This association was even stronger for female participants (61.4% vs. 40.7; P = 0.042). A similar trend was also observed for male participants who said they would expect a physician to prescribe an antibiotic for a cold (66.3% vs. 44.7%; P = 0.022). Nevertheless, expectation for antibiotics for cough, flu symptoms or runny nose had no effect on physician visit rate.
On the other hand, beliefs that any type of cough with phlegm or runny nose would improve more quickly with antibiotics had no effect on decision to visit a physician (60.6% of those who believed vs. 51.9% of those who did not believe). More participants believed that antibiotics would improve an illness more quickly if the phlegm or mucus were colored yellow than if they were colored green or colorless (Fig. 1).
Of all individuals surveyed, 43.1% answered that antibiotic side effects were not or only a bit of a problem; while 30.7% and 21.8% believed they were a moderate and major problem, respectively. Among those with RTI symptoms in the past six months, the proportions of individuals who visited a physician did not differ significantly whether they believed the side effects of antibiotics were a moderate or major problem (62.9%), or not or only a bit of a problem (55.4%) (Table 2). However, women who perceived antibiotic side effects to be a moderate or major problem were less likely to expect a physician to prescribe antibiotics for a cough (50.9% vs. 64.2%; P = 0.051).
Multivariate analyses of factors associated with physician visit
Physician visits were modeled using multivariate logistic regression (Table 3). In the final model, occupation and expectation for antibiotic for a sore throat were marginally and significantly contributing predisposing factors, respectively. Employed participants were nearly three times more likely to had visited a physician for their recent RTI compared to students and other occupations (adjusted odds ratios [AOR], 2.75; 95% CI, 0.86–9.02; P = 0.087). Patients who had unreasonable expectations for antibiotic prescription were two times more likely to visit a physician for their recent RTI (AOR, 2.20; 95% CI, 1.15–4.21; P = 0.020) compared to those with sensible attitudes. Among enabling factors, patients with National Health Insurance (NHI) were more likely to visit a physician than those with government subsidy (Medicaid) or private insurance (AOR, 1.78; 95% CI, 1.06–2.90; P = 0.029). Severity of symptoms, as the only need factor, strongly and significantly influenced the decision to visit a physician; those who perceived symptoms as moderate or severe had 3.5 to 10 times higher likelihood than those with mild symptoms (AOR, 3.53; 95% CI, 1.32–8.87; P = 0.010; AOR, 9.88; 95% CI, 3.66–25.75; P < 0.001, respectively).
Table 3. Logistic regression analyses on visiting a physician for the most recent RTI using the Andersen's model (n = 344).
| Variables | Category | Crude OR (95% CI)* | AOR (95% CI)† |
|---|---|---|---|
| Predisposing factors | |||
| Socio-demographics | |||
| Age, yr | ≤ 24 | 0.54 (0.22–1.34) | 1.03 (0.28–3.26) |
| 25–39 | 1.02 (0.54–1.91) | 1.00 (0.44–1.92) | |
| 40–59 | 1.18 (0.71–1.94) | 1.24 (0.69–2.25) | |
| ≥ 60 | 1.00 | 1.00 | |
| Marital status | Married | 0.62 (0.37–1.04)‡ | 0.97 (0.47–1.97) |
| Others | 1.00 | 1.00 | |
| Occupation | Employed | 2.97 (1.13–7.79) | 2.75 (0.86–9.0.2)‡ |
| Unemployed/retired/houseman/wife | 2.77 (1.04–7.38) | 2.53 (0.73–8.03) | |
| Student/other | 1.00 | 1.00 | |
| Knowledge and attitude | |||
| Common colds are cured more quickly with antibiotics | Incorrect answer | 1.56 (0.99–2.48) | 1.43 (0.85–2.40) |
| Correct answer | 1.00 | 1.00 | |
| Antibiotics side effects | Not or a bit of a problem | 0.73 (0.48–1.13) | 0.73 (0.45–1.17) |
| Moderate or major problem | 1.00 | 1.00 | |
| Expect antibiotic if visit a physician for sore throat | Yes | 1.79 (1.00–3.20) | 2.20 (1.15–4.21)§ |
| No | 1.00 | 1.00 | |
| Enabling factors | |||
| Health insurance type | NHI | 1.39 (0.90–2.14) | 1.78 (1.06–2.90)§ |
| Private/Medicaid | 1.00 | 1.00 | |
| Need factors | |||
| Severity of symptoms | Severe | 8.48 (3.38–21.27) | 9.88 (3.66–25.75)‖ |
| Moderate | 3.39 (1.37–8.40) | 3.53 (1.32–8.87)§ | |
| Mild | 1.00 | 1.00 | |
| Hosmer and Lemeshow test | - | Non-significant (P = 0.745) | |
| Overall prediction, % | - | 69.3 | |
| Nagelkerke pseudo-R2 | - | 0.189 |
RTI = respiratory tract infection, OR = odds ratio, CI = confidence interval, AOR = adjusted odds ratio, NHI = National Health Insurance.
*This column shows ORs for those variables significant at P < 0.2 in crude models; †Adjusted for all significant variables from crude models simultaneously; ‡P < 0.1; §P < 0.05; ‖P < 0.001.
Visit expectations
Of these 204 participants, 15.6% (95% CI, 11.79%–20.43%) had expected an antibiotic prescription (8.4% of those with RTI symptoms [Fig. 2]), 61.3% expected non-antibiotic medicines for their symptoms, 29.0% and 1.6%, respectively, expected advice about self-care and illness duration, 15.1% expected reassurance and prevention of a more serious illness, and 1.6% expected a sick note for work.
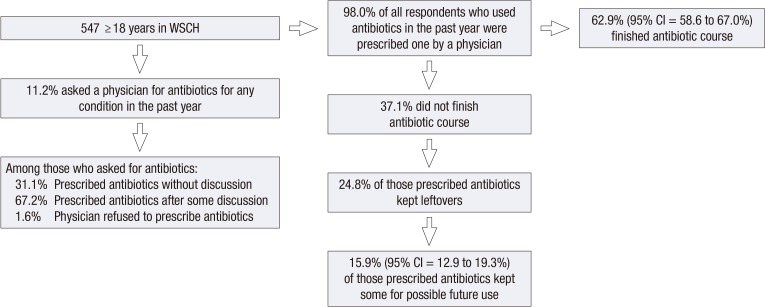
Asking for antibiotics and adherence
Of the 61 (11.2%) participants who reported asking a physician for antibiotics in the past year, only 1.6% were refused, 67.2% were prescribed antibiotics after some discussion, and 31.2% without any discussion about their illness. Of the 536 (98.0%) participants who used prescribed antibiotics in the past year, 37.1% did not finish the full course, 24.8% did not finish the course and kept some, and 15.9% mentioned that they kept their leftovers for possible future use (Fig. 3).
Fig. 3.
Practices reported by all 547 participants regarding antibiotic use in the past year.
WSCH = Wonju Severance Christian Hospital, CI = confidence interval.
DISCUSSION
This was a descriptive study to illustrate the components of RTI clinical iceberg and to identify factors associated with physician visit among the Korean general public. Most RTIs are self-limiting and the symptoms can improve with rest and OTC medicines. Yet, RTIs often result in unnecessary visits to primary care and imprudent antibiotic prescriptions (27). Considering our findings, it seems that physician visit and consultation is the first choice for the Korean general public in case of RTIs, with a consulting rate of 59.3%. The second and third choices are taking extra rest and OTC or alternative medicines. These are similar to the results of a Korean study (18) in which most of participants preferred visiting a physician in case of RTIs. However, our findings are far different from an English perspective, where the trend was quite the opposite (20). This may partly be due to lack of public awareness about the usual course of RTIs and ways to self-manage the symptoms. It may also be due to the broken health care system of Korea as described by Lee et al. (28), where patients have free access to various healthcare providers at different levels.
Specific groups of patients seem more inclined to visit a physician for an RTI; for example, older patients, those with misperceptions about the benefits of consulting a physician and/or antibiotics effectiveness, or those who perceive their symptoms as serious (20,29). In line with these studies and considering the Andersen's behavioral model, our findings suggest considerable contribution of predisposing, enabling, and need factors.
Employed participants were marginally more likely to visit a physician for their recent RTI; this may reflect their effort to avoid missing work and consequent earnings loss. They may also be urged more by others to visit a physician. In addition, participants who expected an antibiotic prescription for a sore throat were significantly more likely to visit a physician for their recent RTI. This may be due to their previous experiences in which they received an antibiotic prescription during a physician visit for a sore throat, entering the vicious cycle of “medicalization of illness” (30) where patients perceive a sore throat more severely and believe that only a physician visit and antibiotics could be effective.
Having NHI increased the likelihood of physician visit in the current study. NHI is a wage-based contributory insurance program that covers almost all Koreans. Those preferring increased coverage can also obtain private insurance. And the poor are covered by a government-subsidized assistance program (Medicaid) that offers increased coverage compared to that of NHI. Our finding is in contrast with one study from Korea (31), which reported higher healthcare utilization in patients with Medicaid. Sub-analyses could partly explain this discrepancy, as those with NHI had less sensible views regarding antibiotic effectiveness (data not shown).
Similar to the results of previous studies (20,29), severity of symptoms as the need factor had the strongest impact on decision to visit a physician. Patients' appraisal of symptoms and the way they respond to them form what is known as ‘illness behavior.’ Individuals behave differently according to their socio-demographic, cultural, and health status backgrounds (29,32). In our study, middle-aged women or women with higher levels of education were more likely to perceive the symptoms more severe.
As expected, this survey showed that the general public indeed visited physicians for symptomatic relief, advice about self-care, reassurance, and time to recovery. This is in line with previous studies where patients with acute RTIs had similar expectations from physician visit (20,33). Interactive educational leaflets with information specific to RTI symptoms and usual course of illness have been shown to be effective to address such concerns, to promote patient-physician relationships, and to reduce physician visits (34). There also seems to be a mild pressure on physicians to prescribe antibiotics as it formed only about 16% of all expectations among the participants with recent RTI.
Patient expectations for antibiotic treatment and physician perceptions of these expectations have been shown to significantly increase the likelihood of antibiotic prescription contrary to clinical guidelines in Korea (35,36). Similarly, our study showed that almost all participants who asked a physician for antibiotics in the past year were prescribed one, with one-third being prescribed without any discussion during the consultation. A strategy that may help reduce this expectation and demand is delayed antibiotic prescribing (37); this strategy encourages both patient and physician to come to an agreement and reduces the volume of antibiotics prescribed. While it is commonly practiced in the UK (20), Korea clinical guidelines recommend it mainly for acute otitis media in children.
We also found that the general public considers symptoms such as cough and runny nose with discolored sputum more likely to benefit from antibiotic treatment, although clinical evidence does not support it. Previous studies have shown that such symptoms and beliefs in antibiotic effectiveness for them are associated with higher physician visit rates and more frequently prescribed antibiotics (20,38). Our findings imply an opportunity to educate Korean patients to make their expectations for antibiotics more realistic.
In this study, adherence to the antibiotic regimen was about 63%, which is lower than what reported in a previous Korean study (18) and a meta-analysis on misuse of antibiotics in the community (39). The most common reasons for non-adherence were when the patients began to feel better or when the adverse effects occurred. Non-adherence itself is the main reason for leftover antibiotics and subsequent self-medication with antibiotics (39).
We have some limitations in this research. The survey participants were recruited opportunistically at the WSCH; thus, the sample is not representative of Gangwon province overall, nor can the findings be generalized to the whole Korea population. However, we could assess responses from various socio-demographic backgrounds. In addition, convenience sampling may have introduced selection bias. Nevertheless, the aim of this study was to provide insight into the Korean general population's journey through RTI illnesses. As the study was retrospective, there may inevitably be recall bias about antibiotic use or recent RTI. In addition, those affected more severely may have recalled the details better. Finally, as with all questionnaire studies, there might have been a social desirability bias whereby participants provided answers they considered to be more favorable to others.
In conclusion, antibiotic prescribing for RTIs is a complex issue and physicians should consider both the individual and the society needs in order to minimize the emergence of antibiotic resistance. This RTI clinical iceberg may help improve the quality of prescribing decisions. There seems to be an opportunity for Korean physicians to provide more information on illness course and duration, as well as advice on symptomatic relief of RTIs. They should discuss more often about the positives and negatives of antibiotic use for RTIs, delay prescribing, explain the importance of full adherence to antibiotic regimen as prescribed, and address the improper emphasis that patients place on discolored sputum and nasal discharge in order to come to an evidence-based shared decision.
ACKNOWLEDGMENT
The authors would like to thank Community Health Surveyors of Yonsei University, Jeong-Soon Yoo, Namsook Kim, Mun-Ja Lee, Hyo-Sin Kim, and Yeongsook Hwang for their technical assistance for this study.
Footnotes
Funding: This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2016S1A5B8925203); and 2015 Korean Community Health Survey, funded by the Korea Centers for Disease Control and Prevention, Gangwon province and 7 Districts (Hoengseong, Hongcheon, Jeongseon, Pyeongchang, Taebaek, Wonju, and Yeongwol) in Korea.
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Freidoony L, Kim CB, Haghani H. Data curation: Freidoony L, Kim CB, Park MB. Funding acquisition: Kim CB. Investigation: Freidoony L. Writing - original draft: Freidoony L. Writing - review & editing: Kim CB, Haghani H, Chang SJ, Kim SH, Koh SB.
References
- 1.Laxminarayan R, Duse A, Wattal C, Zaidi AK, Wertheim HF, Sumpradit N, Vlieghe E, Hara GL, Gould IM, Goossens H, et al. Antibiotic resistance-the need for global solutions. Lancet Infect Dis. 2013;13:1057–1098. doi: 10.1016/S1473-3099(13)70318-9. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. The evolving threat of antimicrobial resistance: options for action [Internet] [accessed on 26 May 2016]. Available at http://apps.who.int/iris/bitstream/10665/44812/1/9789241503181_eng.pdf.
- 3.Butler CC, Dunstan F, Heginbothom M, Mason B, Roberts Z, Hillier S, Howe R, Palmer S, Howard A. Containing antibiotic resistance: decreased antibiotic-resistant coliform urinary tract infections with reduction in antibiotic prescribing by general practices. Br J Gen Pract. 2007;57:785–792. [PMC free article] [PubMed] [Google Scholar]
- 4.Monto AS. Epidemiology of viral respiratory infections. Am J Med. 2002;112(Suppl 6A):4S–12S. doi: 10.1016/s0002-9343(01)01058-0. [DOI] [PubMed] [Google Scholar]
- 5.Arroll B. Antibiotics for upper respiratory tract infections: an overview of Cochrane reviews. Respir Med. 2005;99:255–261. doi: 10.1016/j.rmed.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Smith SM, Fahey T, Smucny J, Becker LA. Antibiotics for acute bronchitis. Cochrane Database Syst Rev. 2014:CD000245. doi: 10.1002/14651858.CD000245.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Earnshaw S, Mancarella G, Mendez A, Todorova B, Magiorakos AP, Possenti E, Stryk M, Gilbro S, Goossens H, Albiger B, et al. European antibiotic awareness day: a five-year perspective of Europe-wide actions to promote prudent use of antibiotics. Euro Surveill. 2014;19:20928. doi: 10.2807/1560-7917.es2014.19.41.20928. [DOI] [PubMed] [Google Scholar]
- 8.Kim B, Kim J, Kim SW, Pai H. A Survey of antimicrobial stewardship programs in Korea, 2015. J Korean Med Sci. 2016;31:1553–1559. doi: 10.3346/jkms.2016.31.10.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee K, Yong D, Jeong SH, Chong Y. Multidrug-resistant Acinetobacter spp.: increasingly problematic nosocomial pathogens. Yonsei Med J. 2011;52:879–891. doi: 10.3349/ymj.2011.52.6.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song JH, Joo EJ. The crisis of antimicrobial resistance: current status and future strategies. J Korean Med Assoc. 2010;53:999–1005. [Google Scholar]
- 11.Kwon K, Hwang IG, Kwak HS, Park JS, Kim MG, Lee G. Administration of National Antimicrobial Resistance Experts and Public Campaign Activities. Seoul: Korea Food & Drug Administration; 2006. [Google Scholar]
- 12.Yun JM, Shin DW, Hwang SS, Cho J, Nam YS, Kim JH, Cho BL. Effect of public disclosure on antibiotic prescription rate for upper respiratory tract infections. JAMA Intern Med. 2015;175:445–447. doi: 10.1001/jamainternmed.2014.6569. [DOI] [PubMed] [Google Scholar]
- 13.Chung DR, Song JH, The Korean Society of Infectious Diseases National campaign for appropriate antibiotic use in Korea. Infect Chemother. 2012;44:164–167. [Google Scholar]
- 14.Kim BN. Overview of antibiotic use in Korea. Infect Chemother. 2012;44:250–262. [Google Scholar]
- 15.Yoon YK, Park GC, An H, Chun BC, Sohn JW, Kim MJ. Trends of antibiotic consumption in Korea according to national reimbursement data (2008–2012): a population-based epidemiologic study. Medicine (Baltimore) 2015;94:e2100. doi: 10.1097/MD.0000000000002100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim SS, Moon S, Kim EJ. Public knowledge and attitudes regarding antibiotic use in South Korea. J Korean Acad Nurs. 2011;41:742–749. doi: 10.4040/jkan.2011.41.6.742. [DOI] [PubMed] [Google Scholar]
- 17.Agency for Healthcare Research and Quality (US) Improving antibiotic prescribing for uncomplicated acute respiratory tract infections [Internet] [Accessed 10 May 2016]. Available at https://www.effectivehealthcare.ahrq.gov/ehc/products/561/2112/antibiotics-respiratory-infection-report-160128.pdf. [PubMed]
- 18.Kim JS, Park HN, Cho EM, Park WM, Lee SH, Lee HS, Lee SH. Patient knowledge of upper respiratory infections an unnecessary utilization of antibiotics. J Korean Acad Fam Med. 2001;22:200–211. [Google Scholar]
- 19.Coxeter P, Del Mar CB, McGregor L, Beller EM, Hoffmann TC. Interventions to facilitate shared decision making to address antibiotic use for acute respiratory infections in primary care. Cochrane Database Syst Rev. 2015:CD010907. doi: 10.1002/14651858.CD010907.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McNulty CA, Nichols T, French DP, Joshi P, Butler CC. Expectations for consultations and antibiotics for respiratory tract infection in primary care: the RTI clinical iceberg. Br J Gen Pract. 2013;63:e429–36. doi: 10.3399/bjgp13X669149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 2005;83:1–24. [PubMed] [Google Scholar]
- 22.Health Insurance Review & Assessment Service (KR) Comprehensive Quality Report of National Health Insurance 2012. Seoul: Health Insurance Review & Assessment Service; 2013. [Google Scholar]
- 23.Wun YT, Lam TP, Lam KF, Ho PL, Yung WH. The public’s perspectives on antibiotic resistance and abuse among Chinese in Hong Kong. Pharmacoepidemiol Drug Saf. 2013;22:241–249. doi: 10.1002/pds.3339. [DOI] [PubMed] [Google Scholar]
- 24.Korea Centers for Disease Control and Prevention. Community Health Survey 2008-2014: Community Health Statistics at a Glance. Cheongju: Korea Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 25.Dean AG, Arner TG, Sunki GG, Friedman R, Lantinga M, Sangam S, Zubieta JC, Sullivan KM, Brendel KA, Gao Z, et al. Epi Info™, a Database and Statistics Program for Public Health Professionals. Atlanta, GA: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 26.IBM Corp. (US) IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp.; 2011. [Google Scholar]
- 27.Renati S, Linder JA. Necessity of office visits for acute respiratory infections in primary care. Fam Pract. 2016;33:312–317. doi: 10.1093/fampra/cmw019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee JY, Jo MW, Yoo WS, Kim HJ, Eun SJ. Evidence of a broken healthcare delivery system in Korea: unnecessary hospital outpatient utilization among patients with a single chronic disease without complications. J Korean Med Sci. 2014;29:1590–1596. doi: 10.3346/jkms.2014.29.12.1590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Duijn HJ, Kuyvenhoven MM, Schellevis FG, Verheij TJ. Illness behaviour and antibiotic prescription in patients with respiratory tract symptoms. Br J Gen Pract. 2007;57:561–568. [PMC free article] [PubMed] [Google Scholar]
- 30.Little P, Gould C, Williamson I, Warner G, Gantley M, Kinmonth AL. Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics. BMJ. 1997;315:350–352. doi: 10.1136/bmj.315.7104.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Suh HS, Kang HY, Kim J, Shin E. Effect of health insurance type on health care utilization in patients with hypertension: a national health insurance database study in Korea. BMC Health Serv Res. 2014;14:570–581. doi: 10.1186/s12913-014-0570-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hordijk PM, Broekhuizen BD, Butler CC, Coenen S, Godycki-Cwirko M, Goossens H, Hood K, Smith R, van Vugt SF, Little P, et al. Illness perception and related behaviour in lower respiratory tract infections—a European study. Fam Pract. 2015;32:152–158. doi: 10.1093/fampra/cmu075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Driel ML, De Sutter A, Deveugele M, Peersman W, Butler CC, De Meyere M, De Maeseneer J, Christiaens T. Are sore throat patients who hope for antibiotics actually asking for pain relief? Ann Fam Med. 2006;4:494–499. doi: 10.1370/afm.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andrews T, Thompson M, Buckley DI, Heneghan C, Deyo R, Redmond N, Lucas PJ, Blair PS, Hay AD. Interventions to influence consulting and antibiotic use for acute respiratory tract infections in children: a systematic review and meta-analysis. PLoS One. 2012;7:e30334. doi: 10.1371/journal.pone.0030334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jang SN, Kim NS. Understanding the culture of antibiotics prescribing of primary physicians for acute upper respiratory infection. J Korean Acad Fam Med. 2004;25:901–907. [Google Scholar]
- 36.Cho HJ, Hong SJ, Park S. Knowledge and beliefs of primary care physicians, pharmacists, and parents on antibiotic use for the pediatric common cold. Soc Sci Med. 2004;58:623–629. doi: 10.1016/s0277-9536(03)00231-4. [DOI] [PubMed] [Google Scholar]
- 37.McCullough AR, Glasziou PP. Delayed antibiotic prescribing strategies--time to implement? JAMA Intern Med. 2016;176:29–30. doi: 10.1001/jamainternmed.2015.7095. [DOI] [PubMed] [Google Scholar]
- 38.Butler CC, Kelly MJ, Hood K, Schaberg T, Melbye H, Serra-Prat M, Blasi F, Little P, Verheij T, Mölstad S, et al. Antibiotic prescribing for discoloured sputum in acute cough/lower respiratory tract infection. Eur Respir J. 2011;38:119–125. doi: 10.1183/09031936.00133910. [DOI] [PubMed] [Google Scholar]
- 39.Kardas P, Devine S, Golembesky A, Roberts C. A systematic review and meta-analysis of misuse of antibiotic therapies in the community. Int J Antimicrob Agents. 2005;26:106–113. doi: 10.1016/j.ijantimicag.2005.04.017. [DOI] [PubMed] [Google Scholar]