Abstract
Adenovirus (AdV) can cause severe pneumonia in non-immunocompromised host, but limited data exist on the distinctive characteristics of AdV pneumonia in non-immunocompromised patients. We evaluated distinctive clinico-laboratory and radiological characteristics and outcomes of AdV pneumonia (n = 179), compared with non-AdV pneumonia (n = 188) in Korean military personnel between 2012 and 2016. AdV pneumonia patients had a higher rate of consolidation with ground-glass opacity (101/152) in lobar distribution (89/152) on computed tomography (CT) (P < 0.001). Laboratory findings showed a higher incidence of unusual blood profiles such as leukopenia (55/179, P < 0.001) or thrombocytopenia (100/179, P < 0.001). The patients had more systemic symptoms such as myalgia (82/179, P = 0.001) or diarrhea (23/179, P < 0.001), compared with non-AdV pneumonia patients. Bacterial co-infection was identified in 28.5% of AdV pneumonia. Most of the AdV isolates typed (69/72, 95.8%) were AdV-55. Patients with a pneumonia severity index ≥ class III were more commonly observed in AdV pneumonia patients compared with non-AdV pneumonia patients (11.2% vs. 2.1%, P < 0.001), and time to clinical stabilization from admission was longer in the AdV pneumonia patients compared with the non-AdV pneumonia patients (3.8 vs. 2.6 days, P < 0.001). Mechanical ventilation (n = 6) was only required in AdV pneumonia patients, one of whom died due to AdV-55. Our data showed that AdV pneumonia in non-immunocompromised patients had distinct characteristics and most of the isolates typed in our study were AdV-55. It is suggested that AdV-55 is an important pathogen of pneumonia in Korean military personnel.
Keywords: Adenovirus, Consolidation, Pneumonia, Thrombocytopenia
Graphical Abstract

INTRODUCTION
Adenoviruses (AdV) are non-enveloped, double-stranded DNA viruses that can cause diseases of the respiratory tract, and gastrointestinal and ocular systems (1). It is well-known that AdV respiratory tract infections are usually mild and self-limiting in a non-immunocompromised host, in contrast with immunocompromised hosts, in whom AdV infection can be fatal (2,3,4). Since the fatal case of AdV pneumonia in a healthy adult was described in the 1960s (5), severe disease caused by AdV has been reported among non-immunocompromised adults, especially in vulnerable populations, such as military recruits and residents of health care facilities (6,7,8,9). Recent studies have also described fatal cases of severe AdV pneumonia caused by particular serotypes, which provide insight into emerging, highly virulent serotypes, even in non-immunocompromised patients (10,11,12,13,14).
In the Armed Forces Capital Hospital, the largest military referral center in Korea, the number of community acquired pneumonia (CAP) patients, admitted with varying severities of disease, has increased annually; among these cases, the AdV isolation rates have been steadily increasing over recent years and fatal cases have been reported since 2012 (15-17). Thus, physicians have tried to identify the causative respiratory viral agents at an early stage to produce favorable outcomes, with these efforts, we have recently reported clinical data on the outcome of administration of antiviral agents, and factors predictive of respiratory failure in AdV pneumonia (16,17).
However, there is limited data on the distinctive characteristics of AdV pneumonia in non-immunocompromised patients, which could help a physician to determine a diagnostic or treatment strategy during early presentation. Therefore, in the present study, we evaluated the characteristics of AdV-associated vs. non-AdV pneumonia cases among Korean military personnel between 2012 and 2016, and additionally described the characteristics of the AdV pneumonia caused by the serotype of AdV-55 which was most commonly isolated type.
MATERIALS AND METHODS
Study subjects
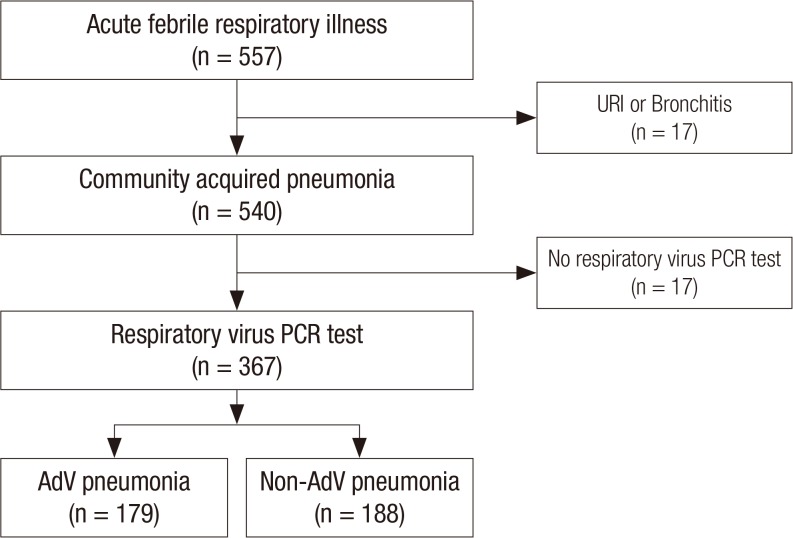
We reviewed the medical records of 557 consecutive adult patients who were admitted with acute febrile respiratory illness, between July 2012 and January 2016, to the Armed Forces Capital Hospital, Korea. All patients were serving in the military service and were non-immunocompromised with negative human immunodeficiency virus infection tests. Of these patients, those with upper respiratory tract infection (URI) or bronchitis (n = 17), and those who did not undergo a respiratory virus polymerase chain reaction (PCR) test (n = 173), were excluded. Consequently, 367 patients with CAP were included in the analysis; of these, 179 with AdV pneumonia and 188 with non-AdV pneumonia were identified and included in the analysis (Fig. 1).
Fig. 1.
Patients included in the study analysis.
URI = upper respiratory tract infection, PCR = polymerase chain reaction, AdV = adenovirus.
The diagnosis of AdV pneumonia was considered confirmed when the following findings were present: 1) acute lower respiratory symptoms; 2) definite infiltration on radiography or computed tomography (CT); and 3) evidence of AdV infection identified by a respiratory virus PCR test from lower respiratory specimens including sputum or bronchoalveolar lavage fluid. When specimens sampled from the lower respiratory tract were considered inadequate, specimens from the upper respiratory tract, including nasopharyngeal or oropharyngeal swabs, were obtained (16,17).
The serotype of AdV-positive specimens was evaluated in some patients. Before June 2014, serotype analysis was performed only in severe cases based on the attending physician's decision (16). Between December 2014 and March 2015, because the number of CAP patients had increased and more severe patients with unusual blood profiles such as leukopenia or thrombocytopenia were referred to the Armed Forces Capital Hospital (Fig. 2), serotype analysis was more frequently performed cooperated by the Armed Forces Medical Command (17). During the same period, serotype analysis was also performed in some outpatients without pneumonia but who had severe symptoms based on the attending physician's decision. The present study included previously published data on patients with AdV pneumonia treated at the Armed Forces Capital Hospital (15,16,17).
Fig. 2.
Time trend of patient number with leukopenia (A) and thrombocytopenia (B) among admitted patients with CAP (patient number per 3 months) (n = 540).
CAP = community acquired pneumonia.
Patient management and data collection
Patients who had persistent symptoms, or who deteriorated despite appropriate empirical antibiotics for 2–3 days, and/or who had unusual blood profiles including leukopenia or thrombocytopenia, were suspected of having atypical causative agents and underwent etiological investigations. Etiologies were evaluated in blood, sputum, bronchoalveolar lavage fluids, nasopharyngeal or oropharyngeal secretions, and urine using microbiological culture for bacteria; a multiplex real-time PCR test for bacterial agents including Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae, and Chlamydia pneumoniae; a multiplex real-time PCR test for respiratory viruses; and a urinary antigen test for S. pneumoniae or Legionella pneumophila . Antiviral therapy with cidofovir was applied in some severe patients (3,16). The serotype of human-AdV-positive samples was investigated by sequencing the partial hexon genomic region (16,17).
Statistical analysis
Data are shown as means ± standard deviation (SD) for continuous variables and as numbers and percentages for categorical variables. Data were compared using a two-sample t-test for continuous variables, and by χ2 or Fisher's exact test for categorical variables. Statistical analyses were performed using PASW software (ver. 18.0; SPSS Inc., Chicago, IL, USA) and a two-sided P value < 0.05 was considered to indicate statistical significance.
Ethics statement
The Institutional Review Board of the Armed Forces Medical Command and Armed Forces Capital Hospital approved this study and permitted the review and publication of patient records (AFMC-16-IRB-037). The requirement for informed consent by individual patients was waived given the retrospective nature of the study.
RESULTS
Comparisons of clinical characteristics between AdV and non-AdV pneumonia
We compared clinical characteristics between the AdV and non-AdV pneumonia patients (Table 1). Most patients were previously healthy males with a mean age of 22 years, and a minority of patients had underlying conditions such as asthma (n = 3), bronchiectasis (n = 3), tuberculosis (n = 2), or congenital cystic malformation (n = 1). All patients presented with clinical symptoms or signs, and AdV pneumonia patients had higher rates of sore throat, myalgia, and diarrhea. Patients with AdV pneumonia were more likely to have clinical instabilities, defined as fever (≥ 38.3°C), dyspnea (≥ modified Medical Research Council [mMRC] II), tachypnea (> 30 breaths/min), tachycardia (> 100 beats/min), oxygen requirement, and inability to eat, compared with patients with non-AdV pneumonia (18). Patients with pneumonia severity index ≥ class III were more commonly observed in the AdV pneumonia. The time from symptom onset to hospital admission tended to be longer in the AdV pneumonia patient group than in the non-AdV pneumonia patient group; however, there was no significant difference between the 2 groups.
Table 1. Comparisons of clinical characteristics between AdV and non-AdV pneumonia.
| Characteristics | Total (n = 367) | AdV (n = 179) | Non-AdV (n = 188) | P value |
|---|---|---|---|---|
| Age, yr | 22.0 ± 3.1 | 21.0 ± 2.1 | 22.0 ± 3.7 | 0.014 |
| Sex (male) | 367 (100.0) | 179 (100.0) | 188 (100.0) | NA |
| BMI, kg/m2 | 23.4 ± 3.8 | 23.7 ± 4.5 | 23.0 ± 2.7 | 0.056 |
| Smoking | < 0.001 | |||
| Never smoker | 301 (82.0) | 143 (79.9) | 158 (84.0) | |
| Ex-smoker | 49 (13.4) | 20 (11.2) | 29 (15.5) | |
| Current smoker | 17 (4.6) | 16 (8.9) | 1 (0.5) | |
| Underlying condition | 0.061 | |||
| Asthma | 3 (0.8) | 1 (0.6) | 2 (1.1) | |
| Bronchiectasis | 3 (0.8) | 2 (1.1) | 1 (0.5) | |
| Previous history of tuberculosis | 2 (0.5) | 2 (1.1) | - | |
| Congenital cystic malformation | 1 (0.3) | - | 1 (0.5) | |
| Grave's disease | 1 (0.3) | 1 (0.6) | - | |
| Irritable bowel syndrome | 1 (0.3) | 1 (0.6) | - | |
| Presenting symptoms or signs | ||||
| Cough | 296 (80.7) | 150 (83.3) | 146 (77.7) | 0.148 |
| Sputum | 214 (58.3) | 111 (62.0) | 103 (54.8) | 0.170 |
| Sore throat | 99 (27.0) | 69 (38.5) | 30 (16.0) | < 0.001 |
| Myalgia | 137 (37.3) | 82 (45.8) | 55 (29.3) | 0.001 |
| Diarrhea | 24 (6.5) | 23 (12.8) | 1 (0.5) | < 0.001 |
| Initial clinical instability | ||||
| Fever (≥ 38.3℃) | 304 (82.8) | 169 (94.4) | 135 (71.8) | < 0.001 |
| Dyspnea (> mMRC scale II) | 91 (24.8) | 65 (36.3) | 26 (13.8) | < 0.001 |
| Tachypnea (> 30 breaths/min) | 30 (8.2) | 27 (15.1) | 3 (1.6) | < 0.001 |
| Tachycardia (> 100 beats/min) | 85 (23.2) | 44 (24.6) | 41 (21.8) | 0.539 |
| Need for oxygen application | 150 (40.9) | 95 (53.1) | 55 (29.3) | < 0.001 |
| Need for vasopressor | 16 (4.4) | 14 (7.8) | 2 (1.1) | 0.002 |
| Inability to eat | 53 (14.4) | 40 (22.3) | 13 (6.9) | < 0.001 |
| Initial SpO2 on room air, % | 95.0 ± 3.1 | 95.0 ± 3.3 | 96.0 ± 2.7 | 0.025 |
| Pneumonia severity index (≥ class III) | 24 (6.5) | 20 (11.2) | 4 (2.1) | < 0.001 |
| Time from symptom onset to admission, day | 8.8 ± 3.7 | 9.1 ± 3.7 | 8.4 ± 3.6 | 0.103 |
Data are shown as mean ± standard deviation or number (%).
AdV = adenovirus, BMI = body mass index, mMRC = modified Medical Research Council, NA = not applicable, SpO2 = stands for peripheral capillary oxygen.
Comparisons of laboratory findings between AdV and non-AdV pneumonia
We compared the laboratory findings between the AdV and non-AdV pneumonia patients (Table 2). The white blood cell (WBC) count and platelet count in AdV pneumonia patients were lower than those of non-AdV pneumonia patients, and leukopenia and thrombocytopenia were more commonly observed in AdV pneumonia patients (all P < 0.001). Pleural fluid analyses were performed in eight AdV pneumonia patients and all had lymphocyte-dominant exudates and elevated adenosine deaminase levels (≥ 40 IU/L), and there was no evidence of mycobacterial infection in all pleural fluid analysis.
Table 2. Comparisons of laboratory findings between AdV and non-AdV pneumonia.
| Characteristics | Total (n = 367) | AdV (n = 179) | Non-AdV (n = 188) | P value |
|---|---|---|---|---|
| Inflammatory markers | ||||
| WBC count, /µL | 7,255.0 ± 4,343.2 | 5,936.0 ± 4,321.6 | 8,510.0 ± 3,986.6 | < 0.001 |
| Neutrophil, % | 71.8 ± 11.8 | 69.9 ± 11.7 | 73.8 ± 11.7 | 0.002 |
| Lymphocyte, % | 18.7 ± 9.4 | 21.0 ± 9.9 | 16.2 ± 8.3 | < 0.001 |
| Neutrophil-lymphocyte count ratio | 5.6 ± 4.9 | 4.7 ± 4.1 | 6.5 ± 5.6 | 0.001 |
| Leukocytosis | 64 (17.4) | 17 (9.5) | 47 (25.0) | < 0.001 |
| Leukopenia (< 4,000/µL) | 62 (16.9) | 55 (30.7) | 7 (3.7) | < 0.001 |
| Platelet count (× 103/µL) | 180.0 ± 66.5 | 150.0 ± 55.6 | 209.0 ± 63.2 | < 0.001 |
| Thrombocytopenia (< 150,000/µL) | 126 (34.3) | 100 (55.9) | 26 (13.8) | < 0.001 |
| C-reactive protein, mg/dL | 9.2 ± 5.7 | 8.9 ± 5.2 | 9.6 ± 6.1 | 0.264 |
| Pleural fluid analysis | 9 | 8 | 1 | |
| Lymphocyte dominant exudate | 8/9 | 8/8 | 0/1 | |
| WBC count, /µL | 2,032.0 ± 2,030.6 | 1,943.0 ± 2,151.7 | 2,750 (NA) | |
| Neutrophil, % | 7.4 ± 10.8 | 4.6 ± 7.2 | 41.0 (NA) | |
| Lymphocyte, % | 35.0 ± 12.5 | 34.3 ± 13.2 | 30.0 (NA) | |
| Adenosine deaminase (≥ 40 IU/L) | 9/9 | 8/8 | 1/1 | |
| Positive respiratory virus PCR test | 202/367 | 179/179 | 23/188 | < 0.001 |
| Viral agents | 0.001 | |||
| AdV | 166 | 166 | - | |
| Rhinovirus | 15 | - | 15 | |
| Influenza A virus | 5 | - | 5 | |
| Metapneumovirus | 2 | - | 2 | |
| Enterovirus | 1 | - | 1 | |
| AdV + rhinovirus | 10 | 10 | - | |
| AdV + parainfluenza virus | 2 | 2 | - | |
| AdV + enterovirus | 1 | 1 | - | |
| Serotype of AdV | NA | |||
| AdV-55 | NA | 69/72 | NA | |
| AdV-4 | NA | 3/72 | NA | |
| Positive specimen for AdV PCR | NA | |||
| Sputum | 121/263 | 121/123 | 0/140 | |
| Nasopharyngeal or oropharyngeal swab | 86/146 | 86/89 | 0/57 | |
| Positive microbiological test | 105/313 | 47/165 | 58/148 | 0.001 |
| Bacterial agents | < 0.001 | |||
| S. pneumoniae | 15 | 8 | 7 | |
| H. influenzae | 16 | 11 | 5 | |
| M. pneumoniae | 23 | 5 | 18 | |
| C. pneumoniae | 1 | - | 1 | |
| P. aeruginosa | 1 | - | 1 | |
| K. pneumoniae | 2 | - | 2 | |
| S. pneumoniae + H. influenzae | 26 | 21 | 5 | |
| S. pneumoniae + M. pneumoniae | 11 | - | 11 | |
| H. influenzae + M. pneumoniae | 3 | 1 | 2 | |
| S. pneumoniae + H. influenzae + M. pneumoniae | 7 | 1 | 6 | |
| Positive specimen for microbiological test | NA | |||
| Sputum + urinary antigen test | 98/284 | 44/151 | 54/133 | |
| Blood, serology test | 17/127 | 6/71 | 11/56 | |
| Blood, bacteremia | 1/252 | 0/145 | 1/107 |
Data are shown as mean ± standard deviation or number (%). Neutrophil (%) and lymphocyte (%) data were missing in 35 cases (29 in non-AdV and 6 in AdV). C-reactive protein (mg/dL) data was missing in 36 cases. Positive specimen for microbiological test; sputum for PCR test and gram stain/culture, urinary antigen test for S. pneumoniae or L. pneumophila, and serology tests for M. pneumoniae or C. pneumoniae.
AdV = adenovirus, WBC = white blood cell, PCR = polymerase chain reaction, NA = not applicable, S. pneumoniae = Streptococcus pneumoniae, H. influenzae = Haemophilus influenzae, M. pneumoniae = Mycoplasma pneumoniae, C. pneumoniae = Chlamydia pneumoniae, P. aeruginosa = Pseudomonas aeruginosa, K. pneumoniae = Klebsiella pneumoniae, L. pneumophila = Legionella pneumophila.
In total, 13 of the 179 (7.3%) AdV pneumonia patients had co-infections with respiratory viruses other than AdV, such as rhinovirus (n = 10), parainfluenza virus (n = 2), and enterovirus (n = 1). Most of the isolates typed (69/72, 95.8%) were AdV-55. More than two-thirds (121/179, 67.6%) of AdV pneumonia patients had positive AdV PCR sputum specimens. Bacterial agents were more commonly identified (58/148, 39.2%) in the non-AdV pneumonia patients (P = 0.001), of whom one had pneumococcal bacteremia. Interestingly, in the AdV pneumonia patients, co-infection with bacterial agents, such as S. pneumoniae followed by H. influenzae and M. pneumoniae, was not uncommon (47/165, 28.5%).
During the study period, PCR tests of nasopharyngeal or oropharyngeal secretions for respiratory viruses were performed in some outpatients without evidence of pneumonia on chest radiography, but who had severe upper respiratory symptoms; 49 patients were confirmed to have AdV infection. A serotype analysis was also performed and AdV-55 (n = 46, 94.0%) was the most commonly identified serotype, followed by AdV-6 (n = 1, 2%), AdV-5 (n = 1, 2%), and AdV-1 (n = 1, 2%).
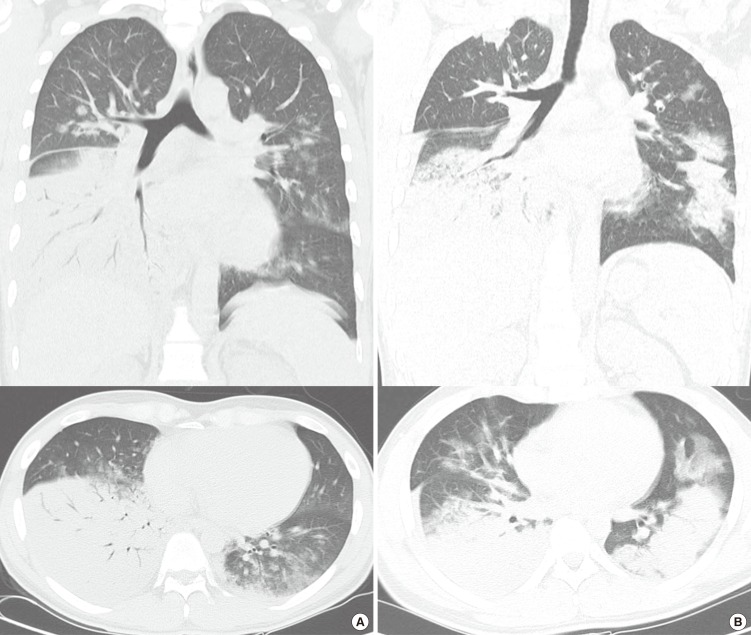
Comparisons of initial chest CT findings between AdV and non-AdV pneumonia
Of the study patients, initial chest CT images were available in 292 patients (Table 3). Notably, approximately 60% of AdV pneumonia patients had consolidation with ground-glass opacity patterns in lobar distribution (Fig. 3), which represented a higher frequency compared with that in the non-AdV pneumonia patients (both, P < 0.001). The mainly involved lobe in the 2 groups tended to differ; however, lower lobe involvement (left, right, and both lower lobe) was commonly observed in both AdV and non-AdV pneumonia patients.
Table 3. Comparisons of initial chest CT findings between AdV and non-AdV pneumonia.
| Characteristics | Total (n = 292) | AdV (n = 152) | Non-AdV (n = 140) | P value |
|---|---|---|---|---|
| Dominant pattern | < 0.001 | |||
| Consolidation + ground glass opacity | 144 (49.3) | 101 (66.5) | 43 (30.7) | |
| Consolidation | 131 (44.9) | 42 (27.6) | 89 (63.6) | |
| Ground-glass opacity | 5 (1.7) | 4 (2.6) | 1 (0.7) | |
| Nodular lesions | 12 (4.1) | 5 (3.3) | 7 (5.0) | |
| Distribution | < 0.001 | |||
| Lobar | 141 (48.2) | 89 (58.5) | 52 (37.1) | |
| Peribronchovascular | 53 (18.2) | 19 (12.5) | 34 (24.3) | |
| Focal | 50 (17.1) | 24 (15.8) | 26 (18.6) | |
| Patchy | 26 (8.9) | 3 (2.0) | 23 (16.4) | |
| Multifocal | 18 (6.2) | 14 (9.2) | 4 (2.9) | |
| Diffuse | 4 (1.4) | 3 (2.0) | 1 (0.7). | |
| Mainly involved lobe | 0.005 | |||
| Left lower lobe | 102 (35.0) | 63 (41.3) | 39 (28.0) | |
| Right lower lobe | 63 (21.7) | 27 (17.8) | 36 (25.7) | |
| Both lower lobe | 18 (6.2) | 10 (6.6) | 8 (5.7) | |
| Left upper lobe | 34 (11.6) | 18 (11.8) | 16 (11.4) | |
| Right upper lobe | 29 (9.9) | 19 (12.5) | 10 (7.1) | |
| Both upper lobe | 1 (0.3) | 1 (0.7) | - | |
| Right middle lobe | 20 (6.8) | 3 (2.0) | 17 (12.1) | |
| Right middle and lower lobe | 10 (3.4) | 3 (2.0) | 7 (5.0) | |
| Left upper and lower lobe | 8 (2.7) | 3 (2.0) | 5 (3.6) | |
| Whole lobes | 7 (2.4) | 5 (3.3) | 2 (1.4) | |
| Bilateral | 104 (35.6) | 54 (35.5) | 50 (35.7) | 0.999 |
| Pleural effusion | 87 (29.8) | 49 (32.2) | 38 (27.1) | 0.371 |
Data are shown as number (%).
AdV = adenovirus, CT = computed tomography.
Fig. 3.
Chest CT findings in 2 AdV pneumonia patients. Chest CT shows prominent consolidation in the right lower lobe with an air bronchogram and bilateral patchy ground glass opacities (A and B).
CT = computed tomography, AdV = adenovirus.
Comparisons of treatment outcomes between AdV and non-AdV pneumonia
Of the 367 study patients, 324 who had detailed medical records during hospitalization were included in the final outcome analysis (Table 4). All 324 patients received empirical antibiotics: a 3rd-generation cephalosporin plus an azalide was the most common treatment (n = 133, 41.1%), followed by respiratory quinolone (n = 75, 23.2%). Cidofovir was administered in 34 AdV pneumonia patients and adjuvant intravenous immunoglobulin (IVIG) was also administered in 14 AdV pneumonia patients. Mechanical ventilation (n = 6) and extracorporeal membrane oxygenation (ECMO) support (n = 1) were needed only in AdV pneumonia patients.
Table 4. Comparisons of treatment outcomes between AdV and non-AdV pneumonia.
| Characteristics | Total (n = 324) | AdV (n = 166) | Non-AdV (n = 158) | P value |
|---|---|---|---|---|
| Treatment regimens | < 0.001 | |||
| Initial empirical antibiotics | ||||
| Amoxicillin and clavulanate | 5 (1.5) | 4 (2.4) | 1 (0.6) | |
| 3rd-cephalosporin + azalide | 133 (41.1) | 47 (28.4) | 86 (54.5) | |
| 3rd-cephalosporin + respiratory quinolone | 1 (0.3) | - | 1 (0.6) | |
| Respiratory quinolone | 75 (23.2) | 45 (27.1) | 30 (19.0) | |
| Piperacillin/tazobactam | 22 (6.8) | 16 (9.6) | 6 (3.8) | |
| Piperacillin/tazobactam + azalide | 3 (0.9) | - | 3 (1.9) | |
| Piperacillin/tazobactam + respiratory quinolone | 82 (25.3) | 52 (31.3) | 30 (19.0) | |
| Carbapenem | 3 (0.9) | 2 (1.2) | 1 (0.6) | |
| Antiviral agents (cidofovir, 5 mg/kg/week) | 34 (20.5) | - | NA | |
| No. of cidofovir administration | ||||
| 1 | - | 29/34 | - | |
| 2 | - | 5/34 | - | |
| Adjuvant IVIG | 16 (4.9) | 14 (8.4) | 2 (1.3) | 0.002 |
| High flow nasal cannula | 13 (4.0) | 8 (4.8) | 5 (3.2) | 0.575 |
| Mechanical ventilation | 6 (1.9) | 6 (3.6) | - | 0.03 |
| ECMO | 1 (0.3) | 1 (0.6) | - | 0.999 |
| Respiratory failure during hospitalization | 50 (15.4) | 37 (22.3) | 13 (8.2) | 0.001 |
| Initial respiratory failure | 34 (10.5) | 23 (13.9) | 11 (7.0) | |
| Progressed to respiratory failure | 16 (4.9) | 14 (8.4) | 2 (1.3) | |
| Time to overall clinical stabilization from admission, day | 3.3 ± 2.5 | 3.8 ± 2.8 | 2.6 ± 1.9 | < 0.001 |
| Death | 1 (0.3) | 1 (0.6) | 0.999 |
Data are shown as mean ± standard deviation or number (%).
AdV = adenovirus, CT = computed tomography, ECMO = extracorporeal membrane oxygenation, IVIG = intravenous immunoglobulin, NA = not applicable.
Respiratory failure, defined as partial pressure of arterial oxygen/fraction of inspired oxygen (FiO2) ratio ≤ 300 with or without tachypnea, occurred more commonly in AdV pneumonia patients than in non-AdV pneumonia patients (P = 0.001). Of the 37 AdV pneumonia patients who had respiratory failure, 23 had initial respiratory failure at the time of admission and 14 progressed to respiratory failure during hospitalization. Time to overall clinical stabilization from admission was significantly longer in the AdV pneumonia patients than in the non-AdV pneumonia patients (mean 3.8 vs. 2.6 days, P < 0.001).
Characteristics and outcomes of 69 patients with AdV-55 pneumonia
Because there are only limited data on the characteristics of AdV pneumonia caused by serotype AdV-55 and there has been concern about the highly virulent serotypes (13), we described the characteristics and outcomes of the 69 patients with AdV-55 pneumonia (Table 5), given that most of the isolates typed in our study were AdV-55. Of the 69 patients with AdV-55 pneumonia, 42 (60.9%) required oxygen, 8 (11.6%) needed a vasopressor, and 13 (18.8%) had pneumonia severity index ≥ class III. Also, leukopenia (n = 24, 34.8%) and thrombocytopenia (n = 39, 56.5%) were commonly observed. Five (7.2%) patients had co-infections with other respiratory viruses such as rhinovirus or enterovirus, and bacterial agents were identified in 30.4% of patients. Most patients (40/63, 63.5%) had consolidation with ground-glass opacity patterns on chest CT. More than a third of patients (n = 24, 34.8%) had respiratory failure, and one patient with AdV-55 pneumonia died of respiratory failure and massive hemorrhagic infarction.
Table 5. Characteristics and outcomes of 69 patients with AdV-55 pneumonia.
| Characteristics | No. (%) of patients |
|---|---|
| Presenting symptoms or signs | |
| Cough | 62 (89.9) |
| Sputum | 36 (52.2) |
| Sore throat | 30 (43.5) |
| Myalgia | 30 (43.5) |
| Diarrhea | 10 (14.5) |
| Initial clinical instability | |
| Fever (≥ 38.3℃) | 67 (97.1) |
| Dyspnea (> mMRC scale II) | 33 (47.8) |
| Tachypnea (> 30 breaths/min) | 17 (24.6) |
| Tachycardia (> 100 beats/min) | 17 (24.6) |
| Need for oxygen application | 42 (60.9) |
| Need for vasopressor | 8 (11.6) |
| Inability to eat | 23 (33.3) |
| Initial SpO2 on room air, % | 95.0 ± 2.9 |
| Initial PaO2/FiO2 ratio | 298.3 ± 82.1 |
| Pneumonia severity index (≥ class III) | 13 (18.8) |
| Inflammatory markers | |
| Leukopenia (< 4,000/μL) | 24 (34.8) |
| Thrombocytopenia (< 150,000/μL) | 39 (56.5) |
| Other viral agents | 5 (7.2) |
| AdV + rhinovirus | 4 (5.8) |
| AdV + enterovirus | 1 (1.4) |
| Positive microbiological test | 21 (30.4) |
| S. pneumoniae | 4 (5.8) |
| H. influenzae | 4 (5.8) |
| M. pneumoniae | 1 (1.4) |
| S. pneumoniae + H. influenzae | 11 (15.9) |
| S. pneumoniae + H. influenzae + M. pneumoniae | 1 (1.4) |
| Chest CT findings (n = 63) | |
| Consolidation + ground-glass opacity pattern | 40/63 (63.5) |
| Lobar distribution | 39/63 (61.9) |
| Bilateral | 29/63 (46.0) |
| Pleural effusion | 26/63 (41.3) |
| High flow nasal cannula | 2 (2.9) |
| Mechanical ventilation | 6 (8.7) |
| ECMO | 1 (1.4) |
| Respiratory failure during hospitalization | 24 (34.8) |
| Initial respiratory failure | 16 (23.2) |
| Progressed to respiratory failure | 8 (11.6) |
| Time to overall clinical stabilization from admission, day | 4.3 ± 3.7 |
| Death | 1 (1.4) |
Data are shown as mean ± standard deviation or number (%). Initial PaO2/FiO2 ratios were missing in 42 cases.
AdV = adenovirus, CT = computed tomography, S. pneumoniae = Streptococcus pneumoniae, H. influenzae = Haemophilus influenzae, M. pneumoniae = Mycoplasma pneumoniae, ECMO = extracorporeal membrane oxygenation, mMRC = modified Medical Research Council, SpO2 = stands for peripheral capillary oxygen, PaO2 = partial pressure of arterial oxygen, FiO2 = fraction of inspired oxygen.
DISCUSSION
One of the most noticeable findings in our study was that AdV pneumonia in previously healthy young adults had distinctive clinico-laboratory and radiological findings compared with non-AdV pneumonia patients. In our study conducted in Korean military personnel, AdV pneumonia patients were more likely to have consolidation with ground-glass opacity in lobar distribution, not uncommonly accompanied by cytopenic blood profiles including leukopenia or thrombocytopenia, and systemic symptoms including myalgia or diarrhea. Studies on the clinical features of AdV pneumonia in non-immunocompromised patients that support our data have consistently been reported (7,12,19,20). For example, in a study that reported 6 cases of severe AdV pneumonia that occurred in a psychiatric care facility, most patients (5/6, 83.3%) had dense lower lobe consolidation on chest radiographs and all patients had a transient fall in WBC and platelet counts in the course of the disease (7). In another study, which compared the characteristics between AdV-55 and other AdV serotypes among 48 AdV pneumonia patients, approximately half of them had consolidation on chest radiographs and only 12.5% had elevated WBC counts (12). In an additional study, which evaluated 115 CT findings of 93 viral and 23 bacterial pneumonia cases, AdV tended to have characteristic imaging results, most of which (7/10, 70%) showed multifocal consolidation or ground-glass opacity (21). However, there is still a lack of data on the detailed clinico-radiological features of AdV pneumonia, especially in non-immunocompromised patients; thus in this context, our data may have clinical significance because it provides suggestive findings of AdV pneumonia, which could help physicians to determine further diagnostic or treatment strategies at the time of presentation of pneumonia.
In recent years, concerns regarding the highly virulent serotype have increased and studies have reported fatal cases caused by specific AdV serotypes such as AdV-3, -7, -11, -14, and -55 (10,11,13,14,16,17,19), especially in relatively vulnerable populations such as military personnel. Among Korean military personnel, 6 patients with severe AdV pneumonia caused by AdV-55 were first identified between 2012 and 2014 (16); other severe pneumonia cases associated with AdV-55 have been identified. Interestingly, during the same period, 5 fatal cases of AdV pneumonia caused by AdV-55—with 80% mortality rate—were reported in China (13), which also highlights the emerging highly virulent AdV pathogens. An outbreak of AdV respiratory infection including severe pneumonia was also reported in Chinese military trainees and efforts have been made to identify the immunological profiles of patients with AdV-55 pneumonia (9), which may partly help to identify those more vulnerable to developing severe disease and to develop a treatment strategy. In our study, because approximately one third of the 69 patients with pneumonia caused by AdV-55 had respiratory failure (one of whom died), one might consider AdV-55 as a virulent pathogen. However, given that we could not compare AdV-55 with other AdV serotypes and most of the isolates typed in outpatients without pneumonia during the study period were also AdV-55, our data imply that AdV-55 is not always associated with severe respiratory disease, although it can cause fatal pneumonia, even in non-immunocompromised patients. Regarding these points, no accurate data exist and further well-designed studies of the serotype and host vulnerabilities are required.
In our study, bacterial co-infections in AdV pneumonia patients were identified in 28.5% (47/165) of patients, and S. pneumoniae, H. influenzae, and M. pneumoniae were commonly identified. It is generally known that bacterial co-infection is associated with up to 40% of viral respiratory infections, and is an important contributor to morbidity in pneumonia (22,23,24). Regarding bacterial co-infections associated with AdV infection, one recent study has described elevated serum procalcitonin levels (> 0.5 ng/mL), suggesting the possibility of bacterial co-infection in 4 of 12 AdV pneumonia patients (12). However, there are no accurate data on the incidence, clinical implications, or pathogenesis of bacterial co-infections associated with AdV respiratory infections. In this context, our data may provide significant information on the incidence and bacterial types, but further studies are needed.
Our study had several limitations. First, because our study was conducted at a military hospital, our cohort was not representative of the general population in terms of age, gender, or underlying condition. Thus, our data cannot be applied to mild or severely immunocompromised patients. Second, not all of the isolated AdV samples underwent serologic analysis; thus, inflammatory responses to different AdV serotypes should be evaluated. Third, because of the retrospective design, the possible effects of unidentified bacterial or viral co-infections on the clinical characteristics of pneumonia cannot be excluded. Lastly, there is a possibility that some AdV pneumonia patients might not have been included in our characteristics analysis because not all CAP patients underwent PCR tests for respiratory viruses and a relatively large numbers of CAP patients (n = 173, Fig. 1) was excluded from the analysis.
In conclusion, our data showed that AdV pneumonia in non-immunocompromised patients had distinct characteristics and most of the isolates typed in our study were AdV-55, which suggested that AdV-55 is an important pathogen for pneumonia. However, further surveillance is needed because limited data exist.
Footnotes
DISCLOSURE: The authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conceptualization: Yoon H, Jhun BW, Yoo H. Data curation: Yoon H, Jhun BW, Kim H, Yoo H, Park SB. Supervision: Yoon H, Jhun BW, Kim H, Yoo H, Park SB. Writing - original draft: Yoon H, Jhun BW. Writing - review & editing: Yoon H, Jhun BW.
References
- 1.Lynch JP, 3rd, Fishbein M, Echavarria M. Adenovirus. Semin Respir Crit Care Med. 2011;32:494–511. doi: 10.1055/s-0031-1283287. [DOI] [PubMed] [Google Scholar]
- 2.Simsir A, Greenebaum E, Nuovo G, Schulman LL. Late fatal adenovirus pneumonitis in a lung transplant recipient. Transplantation. 1998;65:592–594. doi: 10.1097/00007890-199802270-00027. [DOI] [PubMed] [Google Scholar]
- 3.Doan ML, Mallory GB, Kaplan SL, Dishop MK, Schecter MG, McKenzie ED, Heinle JS, Elidemir O. Treatment of adenovirus pneumonia with cidofovir in pediatric lung transplant recipients. J Heart Lung Transplant. 2007;26:883–889. doi: 10.1016/j.healun.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 4.Mayeur N, Srairi M, Tetu L, Guilbeau Frugier C, Fourcade O, Dahan M. Lethal hemorrhagic alveolitis after adenovirus pneumonia in a lung transplant recipient. Heart Lung. 2012;41:401–403. doi: 10.1016/j.hrtlng.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Levin S, Dietrich J, Guillory J. Fatal nonbacterial pneumonia associated with adenovirus type 4. Occurrence in an adult. JAMA. 1967;201:975–977. [PubMed] [Google Scholar]
- 6.Tate JE, Bunning ML, Lott L, Lu X, Su J, Metzgar D, Brosch L, Panozzo CA, Marconi VC, Faix DJ, et al. Outbreak of severe respiratory disease associated with emergent human adenovirus serotype 14 at a US air force training facility in 2007. J Infect Dis. 2009;199:1419–1426. doi: 10.1086/598520. [DOI] [PubMed] [Google Scholar]
- 7.Klinger JR, Sanchez MP, Curtin LA, Durkin M, Matyas B. Multiple cases of life-threatening adenovirus pneumonia in a mental health care center. Am J Respir Crit Care Med. 1998;157:645–649. doi: 10.1164/ajrccm.157.2.9608057. [DOI] [PubMed] [Google Scholar]
- 8.Ryu JS, Cho JH, Han HS, Jung MH, Yoon YH, Song ES, Lee JY, Kim SY, Lee KW, Kwak SM, et al. Acute respiratory distress syndrome induced by adenovirus in an otherwise healthy woman. Yonsei Med J. 2003;44:732–735. doi: 10.3349/ymj.2003.44.4.732. [DOI] [PubMed] [Google Scholar]
- 9.Chen WW, Nie WM, Xu W, Xie YX, Tu B, Zhao P, Qin EQ, Zhang YH, Zhang X, Li WG, et al. Cross-sectional study of the relationship of peripheral blood cell profiles with severity of infection by adenovirus type 55. BMC Infect Dis. 2014;14:147. doi: 10.1186/1471-2334-14-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lewis PF, Schmidt MA, Lu X, Erdman DD, Campbell M, Thomas A, Cieslak PR, Grenz LD, Tsaknardis L, Gleaves C, et al. A community-based outbreak of severe respiratory illness caused by human adenovirus serotype 14. J Infect Dis. 2009;199:1427–1434. doi: 10.1086/598521. [DOI] [PubMed] [Google Scholar]
- 11.Gu L, Liu Z, Li X, Qu J, Guan W, Liu Y, Song S, Yu X, Cao B. Severe community-acquired pneumonia caused by adenovirus type 11 in immunocompetent adults in Beijing. J Clin Virol. 2012;54:295–301. doi: 10.1016/j.jcv.2012.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cao B, Huang GH, Pu ZH, Qu JX, Yu XM, Zhu Z, Dong JP, Gao Y, Zhang YX, Li XH, et al. Emergence of community-acquired adenovirus type 55 as a cause of community-onset pneumonia. Chest. 2014;145:79–86. doi: 10.1378/chest.13-1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun B, He H, Wang Z, Qu J, Li X, Ban C, Wan J, Cao B, Tong Z, Wang C. Emergent severe acute respiratory distress syndrome caused by adenovirus type 55 in immunocompetent adults in 2013: a prospective observational study. Crit Care. 2014;18:456. doi: 10.1186/s13054-014-0456-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scott MK, Chommanard C, Lu X, Appelgate D, Grenz L, Schneider E, Gerber SI, Erdman DD, Thomas A. Human adenovirus associated with severe respiratory infection, Oregon, USA, 2013-2014. Emerg Infect Dis. 2016;22:1044–1051. doi: 10.3201/eid2206.151898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heo JY, Lee JE, Kim HK, Choe KW. Acute lower respiratory tract infections in soldiers, South Korea, April 2011-March 2012. Emerg Infect Dis. 2014;20:875–877. doi: 10.3201/eid2005.131692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim SJ, Kim K, Park SB, Hong DJ, Jhun BW. Outcomes of early administration of cidofovir in non-immunocompromised patients with severe adenovirus pneumonia. PLoS One. 2015;10:e0122642. doi: 10.1371/journal.pone.0122642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoon H, Jhun BW, Kim SJ, Kim K. Clinical characteristics and factors predicting respiratory failure in adenovirus pneumonia. Respirology. 2016;21:1243–1250. doi: 10.1111/resp.12828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Halm EA, Fine MJ, Marrie TJ, Coley CM, Kapoor WN, Obrosky DS, Singer DE. Time to clinical stability in patients hospitalized with community-acquired pneumonia: implications for practice guidelines. JAMA. 1998;279:1452–1457. doi: 10.1001/jama.279.18.1452. [DOI] [PubMed] [Google Scholar]
- 19.Barker JH, Luby JP, Sean Dalley A, Bartek WM, Burns DK, Erdman DD. Fatal type 3 adenoviral pneumonia in immunocompetent adult identical twins. Clin Infect Dis. 2003;37:e142–6. doi: 10.1086/379127. [DOI] [PubMed] [Google Scholar]
- 20.Hakim FA, Tleyjeh IM. Severe adenovirus pneumonia in immunocompetent adults: a case report and review of the literature. Eur J Clin Microbiol Infect Dis. 2008;27:153–158. doi: 10.1007/s10096-007-0416-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miller WT, Jr, Mickus TJ, Barbosa E, Jr, Mullin C, Van Deerlin VM, Shiley KT. CT of viral lower respiratory tract infections in adults: comparison among viral organisms and between viral and bacterial infections. AJR Am J Roentgenol. 2011;197:1088–1095. doi: 10.2214/AJR.11.6501. [DOI] [PubMed] [Google Scholar]
- 22.Falsey AR, Becker KL, Swinburne AJ, Nylen ES, Formica MA, Hennessey PA, Criddle MM, Peterson DR, Baran A, Walsh EE. Bacterial complications of respiratory tract viral illness: a comprehensive evaluation. J Infect Dis. 2013;208:432–441. doi: 10.1093/infdis/jit190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cillóniz C, Ewig S, Menéndez R, Ferrer M, Polverino E, Reyes S, Gabarrús A, Marcos MA, Cordoba J, Mensa J, et al. Bacterial co-infection with H1N1 infection in patients admitted with community acquired pneumonia. J Infect. 2012;65:223–230. doi: 10.1016/j.jinf.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morens DM, Taubenberger JK, Fauci AS. Predominant role of bacterial pneumonia as a cause of death in pandemic influenza: implications for pandemic influenza preparedness. J Infect Dis. 2008;198:962–970. doi: 10.1086/591708. [DOI] [PMC free article] [PubMed] [Google Scholar]