Abstract
Introduction
The traditional methods in displaced tibial plateau fractures use metallic instrumentation. “Balloon-tibioplasty” is a novel minimally invasive technique.
Purpose
Use of the balloon-tibioplasty show an improvement of the reduction compared to traditional methods.
Patients and methods
We enrolled 28 patients who presented with a depression fracture of external tibial plateau divided into two treatment groups: balloon-tibioplasty (group I) and “traditional” reduction technique (group II).
Results
Balloon-tibioplasty is a minimally invasive treatment for tibial plateau fracture.
Discussion
Balloon-tibioplasty appears to have several advantages over traditional reduction techniques.
Conclusion
Balloon-tibioplasty represents an improved and accurate modality for restoration of articular congruence.
Keywords: Tibial plateau fracture, Tibioplasty, Intra-articular fracture, Fixation technique
1. Introduction
Depressed external tibial plateau fractures can be difficult to treat and current reduction techniques often lead to poor results. The commonly encountered fracture patterns are split with depression and pure lateral depression fractures, the later seen predominantly in older patient with osteoporotic bone.1 With increasing osteoporosis, low energy falls are resulting in more fractures especially in the weak metaphyseal location of long bones. Tibial plateau fractures constitute 1% of all fractures and 8% of fractures in the elderly.2 The mechanism usually involves a varus or valgus load with an axial force. Soft tissue injury is very common especially in high energy open fractures. Surgical treatment is usually halted until soft tissue swelling subsides and local skin conditions improve. Surgical incisions made through injured and damaged soft tissues about the knee have high complication rates. Non-operative treatment is indicated for non-displaced or minimally displaced fractures in patients with osteoporosis. This requires partial weight bearing in either a cast or hinged fracture brace. Operative indications include depressed fragments greater than 10 mm or instability >10° in a fully extended knee.2 Open fractures with an associated compartment syndrome is another indication for surgery. The treatment of choice for this type of fractures is considered to be open reduction and internal fixation.3 Restoration of the joint surface and tibial alignment is the goals of surgery. This is usually accomplished with buttress plating with subchondral rafting screws. Many authors suggest to avoid the use of cannulated screws without plate especially in comminuted fractures with important articular defect.4 Depressed articular fragments can be elevated using a metal tamp and filling the defect with bone graft filler. Other authors have also incorporated knee arthroscopy to aid in the reduction of the articular fragment. Surgery of tibial plateau fractures is not without complications in patients who are older with multiple co-morbidities. This may result in worsening the defect and even articular penetration as the surface of the impact is small and the force applied is uneven. Borrowing from the successful vertebral kyphoplasty technique, we used an inflatable balloon as a tamp, to reduce a depressed tibial plateau fracture. This gave us the advantage of reducing the bone window to a drill hole while simultaneously increasing the area of force transmission, resulting in easy and satisfactory fracture reduction and minimal trauma, minimizing wound complications to the tenuous skin around the knee.
2. Methods
We reported clinical and radiological results of randomized multicentric trial performed 3 year ago at Orthopedic Department of Sassari, Orthopedic Department of Schio and Orthopedic Department of Oristano. Between June 2011 and January 2013, 28 patients (21 males and 7 females) with post-traumatic external tibial plateau fractures were randomized to fracture reduction using balloon tibioplasty (group I) or “traditional” surgical techniques (group II). In order to pilot this study, the investigators have decided to recruit 14 patients into each arm of the trial. The diagnosis of external tibial plateau fracture was made on AP and lateral X-rays, according to the current guidelines. CT scan was used to localize the injury and assess the topography of the fracture, classify it, and quantify it. According to the Schatzker classification, patients were classified into type II (n = 3) and type III (n = 25). Inclusion criteria were isolated, depressed or split depressed fracture of the external tibial condyle where the decision for operative fixation has been made by the on call team; patients aged 18–80 years; patients willing to give informed consent. The patient and trial statistician were blinded from the treatment method received. 14 patients (9 males and 5 females) with average age of 67.3 years (23.4–74.7 years) underwent surgical treatment using a minimally invasive technique consisting of an inflatable bone tamp for the reduction of the depression (KyphX® Inflatable Bone Tamp Kyphon, Sunnyvale, CA); 13 patients with a contained depressed fracture with no involvement of the lateral cortex underwent tibioplasty alone without any fixation device; one patient, previously underwent surgery with two cannulated screws, showed persistent comminuted fracture of the external tibial condyle (Fig. 1); in this case cannulated screws were removed and tibioplasty with lateral proximal tibial buttress plate fixation (Synthes, Paoli, Pennsylvania) was performed immediately below the compressed tibial plateau (Fig. 2). 14 patients (12 males and 2 females) with average age of 64.5 years (21.2–72.5 years) underwent traditional reduction technique and fixation using cannulated screws (4 cases) and buttress plates (10 cases).
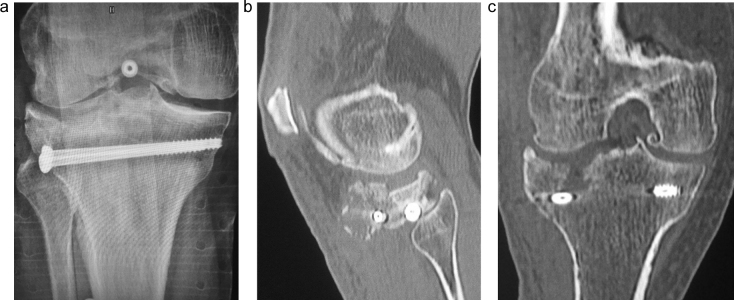
Fig. 1.
Anteroposterior postoperative radiograph showing depressed external tibial plateau fixed by two cannulated screws (a). Postoperative CT scans on sagittal (b) and coronal (c) views showing lateral split with important articular defect.
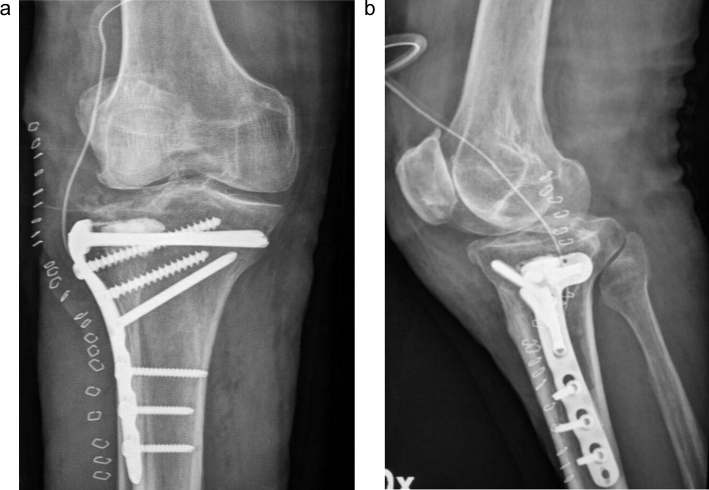
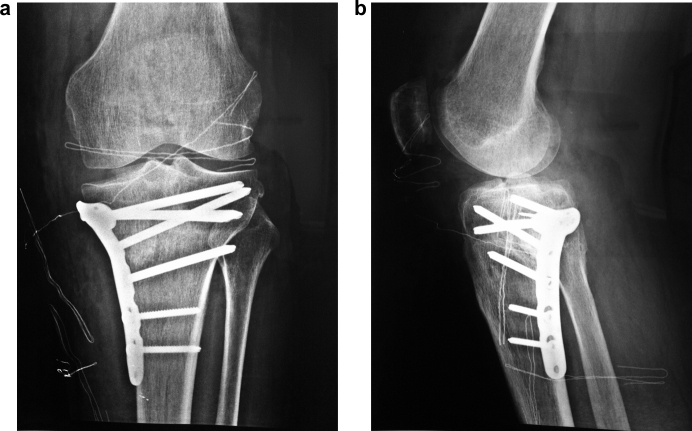
Fig. 2.
Anteroposterior (a) and lateral (b) postoperative radiographs after fracture reduction by balloon-guided inflation tibioplasty and plating.
Post-operative care included 6 weeks non-weight-bearing, with early active mobilization of the knee, managed by a standard physiotherapy rehabilitation regime. All patients used a walker for ambulatory assistance the first week following the procedure and received rigorous physiotherapy achieving full range of motion by the second week and progressing to full weight bearing by the end of the third week on swimming pool for 6 weeks at least. At the final follow up, functional outcome (pain, walking capacity, extension lag, range of motion, and stability) was evaluated using the Rasmussen score system.5 The maximum score for each item was 6. A total score of 28–36 was considered as excellent, 20–27 as good, 10–20 as fair, and 6–10 as poor. CT scan was performed post-operatively on day of surgery and analyzed for residual depression (Table 1).
Table 1.
Evaluation index according Rasmussen scoring system.
| Rasmussen scoring systema | Score | Group I (n = 14) | Group II (n = 14) |
|---|---|---|---|
| Pain | |||
| • No pain | 6 | 10 | 8 |
| • Occasional pain, bad weather pain | 5 | 3 | 2 |
| • Throbbing pain in certain position | 4 | 1 | 2 |
| • Constant pain after activity | 2 | 0 | 2 |
| • Pain at rest | 0 | 0 | 0 |
| Walking capacity | |||
| • Normal | 6 | 11 | 10 |
| • Can walk outdoor for at least 1 h | 4 | 3 | 2 |
| • Can walk outdoor for 15 min | 2 | 0 | 2 |
| • Can walk indoor only | 1 | 0 | 0 |
| • Wheelchair bound/bedridden | 0 | 0 | 0 |
| Extension lag | |||
| • Normal | 6 | 13 | 10 |
| • 0°–10° | 4 | 1 | 3 |
| • >10° | 2 | 0 | 1 |
| Range of motion | |||
| • ≥140° | 6 | 13 | 10 |
| • ≥120° | 5 | 1 | 2 |
| • ≥90° | 4 | 0 | 2 |
| • ≥60° | 2 | 0 | 0 |
| • ≥30° | 1 | 0 | 0 |
| • 0° | 0 | 0 | 0 |
| Stability | |||
| • Normal in extension and 20° flexion | 6 | 13 | 10 |
| • Instability in 20° flexion | 5 | 1 | 2 |
| • Instability in 10° extension | 4 | 0 | 1 |
| • Instability in >10° extension | 2 | 0 | 1 |
Scores of 28–36 indicate excellent, 20–27 good, 10–20 fair, and 6–10 poor.
2.1. Surgical procedure
2.1.1. Tibioplasty (group I)
The optimal position for balloon placement was predetermined using fluoroscopy.6 Under spinal anesthesia, a clinical stability test was applied, which did not reveal any ligamentous injury. The fractures were identified in both the AP and lateral planes using fluoroscopy. The osteointroducer with a trocar tip, was inserted through the medial tibial cortex just underneath the depressed fragment (Fig. 3). We started slowly inflating the balloon with contrast solution, without any radiographic evidence of balloon asymmetry, indicative of malpositioning. We then fully inflated the balloon to approximately 200 psi. Using live fluoroscopy, we were able to see a gradual elevation of the fragment until it looked anatomically reduced on a true AP fluoroscopic view. This was also confirmed on a lateral fluoroscopic view. Nevertheless, if a reduction defect persists, the balloon can be deflated, repositioned, and re-inflated to reduce the persistent compression. When adequate reduction was achieved, the balloon was deflated and withdrawn.7 The cavity formed by the balloon is secured by the compression of the cancellous bone and thus allows use of calcium phosphate cement filler, which has better mechanical stability.8 We injected calcium phosphate cement through the trocar, filling the balloon-created cavity of the external tibial plateau and augmenting the fracture (Fig. 4). The volume of the cement was determined by the volume of the contrast solution used with the balloon (3.5 cc.) and the injection was carefully done under fluoroscopy, to avoid excessive cement overflow into the tibial medullary cavity. The final reduction was radiologically verified.
Fig. 3.

Intraoperative picture showing percutaneous technique of balloon-guided inflation tibioplasty with minimal-invasive incisions for medial-to-lateral Jamshidi trocars.
Fig. 4.

Intraoperative fluoroscopic view of the “standard” technique of percutaneous balloon-guided inflation tibioplasty.
2.1.2. “Traditional” reduction technique (group II)
For this technique, a small cortical window is made in the metaphyseal bone and a metal tamp used to manually elevate the depression. Once an acceptable reduction has been achieved, bone substitute is inserted in the void left by the elevation of the depressed fragment, and internal fixation is performed to support the now congruent joint.
3. Results
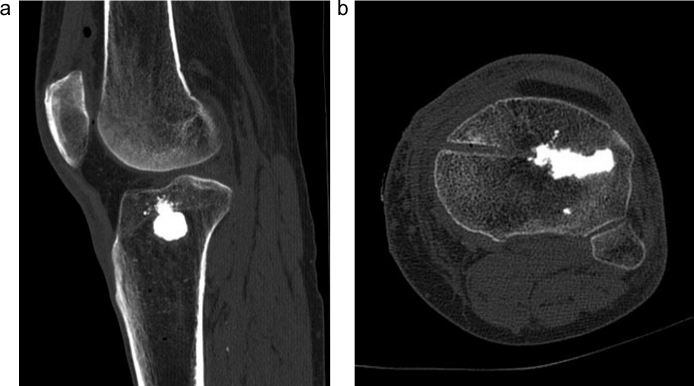
Clinical and radiographic results differ for the two groups. The mean Rasmussen score was lower in 14 patients of group II (26.1 vs. 28.9, p < 0.001 independent sample t test). In the group I CT scan achieved the first postoperative day showed the recovery of about 75% of the area of the tibial lateral plateau joint surface (Fig. 5). Radiograph at 6 weeks demonstrated a maintained anatomic articular reduction (Fig. 6). All patients were allowed to progressively increase weight-bearing status to weight bearing as tolerated by 10 weeks. They had an excellent long-term outcome and were free of symptoms with full active range of motion of knee (0°–140°) at 3 months. All patients were last seen for a scheduled 1-year follow-up (14 months postoperatively), at which point final radiographs demonstrated a maintained long-term reduction and fixation. Patient underwent tibioplasty and plate fixation regained stability of knee to a varus and valgus stress in both full extension and 30 degrees of flexion.
Fig. 5.
Sagittal (a) and axial (b) postoperative CT scans showing a good restore of joint surface after tibioplasty.
Fig. 6.

Anteroposterior radiograph after 6-weeks balloon-guided inflation tibioplasty procedure.
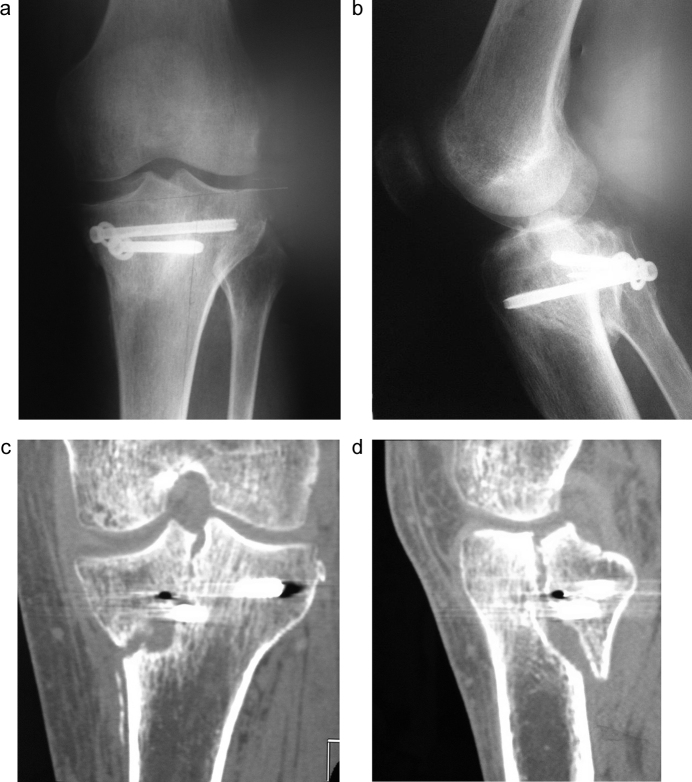
In the group II CT scan achieved the first postoperative day showed the recovery of about 70% of the area of the tibial lateral plateau joint surface with some articular bone free fragments. Radiographs achieved after 6 weeks showed a loss of reduction with subsidence of tibial fragment in one patient underwent anatomical reduction and stabilization by percutaneous cannulated screws (Fig. 7); this patient underwent reoperation achieving good result by reduction and stabilization of fracture using plate and screws (Fig. 8).
Fig. 7.
Postoperative anteroposterior (a) and lateral (b) radiographs showing a good restore of articular surface after percutaneous cannulated screw fixation of postero-medial tibial plateau split fracture. Coronal (c) and sagittal (d) CT scans achieved 2 weeks after surgery showed a loss of reduction of fracture.
Fig. 8.
Postoperative anteroposterior (a) and lateral (b) radiographs after plate positioning.
4. Discussion
Reduction of the articular surface in displaced tibial plateau fractures is still challenging and may result in joint incongruence, leading to post-traumatic arthritis. Anatomic reduction of impacted articular fractures should be the goal of any treating surgeon.9 Tibial plateau fractures with depression are predominantly seen in elderly people and for this reason their treatment must take into account the fragility and osteoporosis of the bones treated. Conventional treatment options call for the use of metallic instruments for the reduction of the depression, which in osteoporotic bone may result in further damage of the articular surface and joint incongruence or even joint penetration. We instead, used a new technique for the reduction, balloon tibioplasty, borrowed from spinal surgery. The technique is already in use apart from kyphoplasty surgery, in maxillofacial surgery, and has recently been used for other areas such as acetabular fractures, cuboid fractures, distal radius, calcaneus, and lately tibial plateau fractures. It has already been proven both in laboratory as well as clinically to be superior to conventional methods, the only drawback being the higher cost due to the disposable instruments.10 The balloon offers the advantage of being minimally invasive and creating a symmetric, contained defect to hold a bone filler for subchondral support.11 The absence of muscular damage reduces postoperative pain and facilitates rehabilitation. The anterior point of introduction under the fracture site is made by an avascular window,12 limiting risks of infection and scarring problems and preserving the blood supply to the periosteum. The balloon allows access to the posterior compressions while eliminating the neurological and vascular risks of a conventional approach. In the presence of lateral wall fracture is need to associate plate fixation to warranty the joint stability and to permit fast recovery. Use of modern fluoroscopy and arthroscopic techniques has resulted in a tendency to avoid open plating of the lateral plateau in favor of percutaneous fixation of the fracture.13
This is especially applicable to split fractures of the lateral plateau, the so-called Schatzker type-I injury. Without severe depression of the joint, this fracture, when displaced, is usually treated by anatomical reduction and stabilization. Most clinical studies of fractures of the lateral plateau have described open reduction and plating of displaced injuries.14
Earlier studies suggested that plating provided the most secure fixation of injuries to the lateral tibial plateau, especially in osteoporotic bone.15
5. Conclusions
We presented our experience in the surgical treatment of depressed external tibial plateau fractures by two different approaches. We founded the balloon tibioplasty technique to be easily applicable and effective in reducing the depression as well as minimally invasive. We achieved excellent results without any complication during or after the operation. The risks of wound complications were minimized do to the small stab incision used to place the trocar. The technique therefore appears to be a promising alternative to standard reduction options for this type of fracture, leading to better results and lesser surgical trauma. With proper patient selection with specific fractures patterns, this new minimally invasive tibioplasty technique is a good alternative to the conventional technique using a bone tamp in the treatment of tibial plateau fractures. It provides anatomical reduction of the fracture in a gentle and progressive manner and mechanical stability allowing early rehabilitation and more fast weight-bearing. In the presence of longitudinal external tibial condyle fracture is advisable to associate fixation using plate and screws that are more stable on weight-bearing than single cannulated screws.
Conflicts of interest
The authors have none to declare.
References
- 1.Schatzker J., Tile M. Springer Verlag; Berlin, Germany: 2005. The Rationale of Operative Fracture Care. [Google Scholar]
- 2.Watson J.T., Schatzker J. Tibial plateau fractures. In: Browner B.D., editor. Skeletal Trauma: Basic Science, Management, and Reconstruction. 3rd ed. Saunders; Philadelphia, PA: 2003. pp. 2047–2130. [Google Scholar]
- 3.Moore T.M., Patzakis M.J., Harvey J.P. Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. J Orthop Trauma. 1987;1(2):97–119. [PubMed] [Google Scholar]
- 4.Denny L.D., Keating E.M., Engelhardt J.A., Saha S. A comparison of fixation techniques in tibial plateau fractures. Orthop Trans. 1984;10:388–389. [Google Scholar]
- 5.Rasmussen P.S. Tibial condylar fractures. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973;55(October (7)):1331–1350. [PubMed] [Google Scholar]
- 6.Hegenscheid K., Puls R., Rosenberg C. Imaging strategies for knee injuries. Radiologue. 2012;52(11):980–986. doi: 10.1007/s00117-012-2411-3. [DOI] [PubMed] [Google Scholar]
- 7.Boisrenoult P., Bricteux S., Beaufils P., Hardy P. Screws versus screw-plate fixation of type 2 Schatzker fractures of the lateral tibial plateau. Cadaver biomechanical study. Arthroscopy French Society, Rev Chir Orthop Reparatrice Appar Mot. 2000;86(November (7)):707–711. [PubMed] [Google Scholar]
- 8.Jaeblon T. Polymethylmethacrylate: properties and contemporary uses in orthopaedics. J Am Acad Orthop Surg. 2010;18(May (5)):297–305. doi: 10.5435/00124635-201005000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Pizanis A., Garcia P., Pohlemann T., Burkhardt M. Balloon tibioplasty: a useful tool for reduction of tibial plateau depression fractures. J Orthop Trauma. 2012;26(July (7)):e88–e93. doi: 10.1097/BOT.0b013e31823a8dc8. [DOI] [PubMed] [Google Scholar]
- 10.Werner C.M., Scheyerer M.J., Schmitt J., Wanner G.A., Simmen H.P. Minimally invasive balloon-assisted reduction and internal fixation of tibial plateau fractures. Unfallchirurg. 2012;115(12):1126–1132. doi: 10.1007/s00113-012-2245-5. [DOI] [PubMed] [Google Scholar]
- 11.Broome B., Mauffrey C., Statton J., Voor M., Seligson D. Inflation osteoplasty: in vitro evaluation of a new technique for reducing depressed intra-articular fractures of the tibial plateau and distal radius. J Orthop Traumatol. 2012;13(June (2)):89–95. doi: 10.1007/s10195-012-0185-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hannouche D., Duparc F., Beaufils P. The arterial vascularization of the lateral tibial condyle: anatomy and surgical applications. Surg Radiol Anat. 2006;28(1):38–45. doi: 10.1007/s00276-005-0044-1. [DOI] [PubMed] [Google Scholar]
- 13.Koval K.J., Polatsch D., Kummer F.J., Cheng D., Zuckerman J.D. Split fractures of the lateral tibial plateau: evaluation of three fixation methods. J Orthop Trauma. 1996;10:304–308. doi: 10.1097/00005131-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Segal D., Mallik A.R., Wetzler M.J., Franchi A.V., Whitelaw G.P. Early weight bearing of lateral tibial plateau fractures. Clin Orthop. 1993;294:232–237. [PubMed] [Google Scholar]
- 15.Toolan B.C., Koval K.J., Kummer F.J., Sanders R., Zuckerman J.D. Vertical shear fractures of the medial malleolus: a biomechanical study of five internal fixation techniques. Foot Ankle Int. 1994;15:483–489. doi: 10.1177/107110079401500905. [DOI] [PubMed] [Google Scholar]