Abstract
Objective:
The purpose of this study was to compare the clinical outcomes between patients with a valgus or varus deformity undergoing minimally invasive total knee arthroplasty through the medial approach.
Methods:
The patients were classified into 2 groups according to the preoperative femorotibial angle measured on an anteroposterior long leg roentgenogram. The valgus group comprised of 26 knees in 21 patients with a femorotibial angle <170° (163.5 ± 5.7), and the varus group comprised of 24 knees in 21 patients with a femorotibial angle >190° (195.9 ± 5.5). The following background variables were compared between the groups: age at the time of the operation, sex, causative disease, preoperative femoral mechanical–anatomical angle, and postoperative knee range of motion, Knee Society score, femorotibial angle, and implant position.
Results:
There were significant differences between the valgus and varus groups in the age (68.0 ± 6.9 vs 75.8 ± 6.2 years), percentage of males (23.8% vs 0%), percentage with rheumatoid arthritis (61.9% vs 4.8%), and preoperative femoral mechanical–anatomical angle (6.2 ± 1.0° vs 7.4 ± 2.1°). Clinical outcome variables of postoperative femorotibial angle (173.1 ± 3.9° vs 175.2 ± 1.6°) and α angle (96.6 ± 3.1° vs 95.0 ± 1.9°) also differed.
Conclusion:
It was assumed that over-valgus resection of the femur is a contributory factor to residual valgus alignment. However, knee range of motion and Knee Society score did not differ between the groups. We suggest that minimally invasive total knee arthroplasty through the medial approach is one of the treatment options for patients with valgus deformity.
Keywords: Femoral Mechanical‒Anatomical Angle, Medial Approach, Minimally Invasive Total Knee Arthroplasty, Pie Crust Technique, Posterior-Stabilized Implant, Valgus Deformity
INTRODUCTION
Minimally invasive total knee arthroplasty (MIS TKA) has several advantages compared with the conventional TKA, such as less postoperative pain, smaller skin incision, and earlier recovery of quadriceps muscle strength, knee range of motion (ROM), and the ability to walk [1-4]. However, therearesome concernsabout MIS TKAbecauseof the high complication rates (e.g., delayed wound healing or skin necrosis), malpositioning of the implant, learning curve for surgeons, and similar midterm results as for the conventional TKA [5-8]. We regularly performed MIS TKA through the medial approach in both varus and valgus knees. A number of valgus knees were observed to have complex abnormalities in the soft tissue and bone, including medial collateral ligament laxity, lateral capsular and ligament contracture, rotational deformity and osseous deficiency of the femoral condyle or tibia plateau, or patellar maltracking. A proper lateral soft tissue release was emphasized in addition to correcting the osseous alignment and positioning the articular surface when performing TKA for valgus knees [9-11]. However, it is sometimes difficult to reach the lateral structures and to ensure correct soft tissue balance through the medial approach.
The purpose of this study was to compare the variables such as patient background and clinical outcomes between the patients with a valgus or varus knee undergoing a MIS TKA through the medial approach.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board (No.15R-146). All patients received information regarding the purpose, and informed consent was obtained from all patients. We have treated 151 knees in our institutions from 2008 to 2013, and retrospectively reviewed 42 patients (50 knees) who had relatively severe valgus or varus deformities.
Characteristics of Patients
The patients were classified into 2 groups based on the preoperative femorotibial angle (FTA) measured on an anteroposterior long leg roentgenogram. The valgus group comprised 21 patients (26 knees) with an FTA <170° (163.5 ± 5.7°), and the varus group comprised of 21 patients (24 knees) with an FTA >190° (195.9 ± 5.5°). The mean follow-up period was 32.9 ± 16.0 and 26.0 ± 10.7 months, respectively.
Surgical Techniques
All patients were given general and epidural anesthesia, which showed beneficial effects such as postoperative analgesia and decreased risk of deep vein thrombosis by increasing blood flow to the lower extremity because of the sympathetic nerve block [12]. Tourniquets were not applied. The mini-subvastus approach was used in 45 knees, and the mini-parapatellar approach was used in 5 knees without eversion of the patella. The MIS Quad-Sparing instrumentation (Zimmer Biomet Holdings Inc., Warsaw, IN, USA) was used when cutting the femur and tibia from the medial side [13, 14]. The posterior cruciate ligament (PCL) was sacrificed, and the patella was resurfaced in all cases. In the coronal plane, the bone resection angle was set 6° valgus to the anatomical axis using an intramedullary rod for the femur and perpendicular using the extramedullary guide for the tibia. In the sagittal plane, the bone resection angle was set parallel to the distal anterior cortex for the femur and at a 7° posterior slope to the mechanical axis for the tibia. In the axial plane, the bone resection angle was set 3° externally rotated to the posterior condylar line for the femur. When the posterior condylar line was not apparent because of a bony defect of the lateral posterior condyle, as observed occasionally in the valgus knees, we referred to Whiteside’s line and set the bone resection angle perpendicular to this line. The rotation in the axial plane of the tibia was controlled by checking the whole lower limb alignment after a trial of the implanted component that was adapted to the medial one-third of the tibial tuberosity. Lateral soft tissue release was performed according to the “pie crust” technique until medial–lateral balance was achieved [15]. We implanted the NexGen® Legacy Posterior-Stabilized Flex (Zimmer®) knees and fixed the bearing inserts using bone cement in all cases. A constrained-type implant was not used in any patient. Fig. (1) shows sample preoperative and postoperative radiographs of a 72-year-old female patient with rheumatoid arthritis.
Fig. (1).
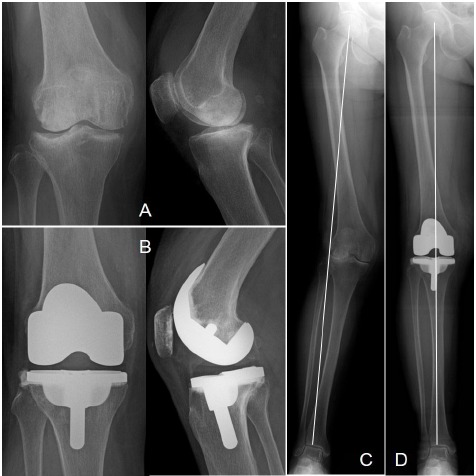
A 72-year-old female patient with rheumatoid arthritis underwent minimally invasive total knee arthroplasty through the medial approach (A, B). The femorotibial angle was corrected from 162° to 174° (C, D), the knee range of motion improved from 120°/–20° to 125°/–5° for flexion and extension, respectively, and the Knee Society score improved from 45 to 84.
On postoperative day 2, the intraarticular drain was removed, and the patients began exercise according to the rehabilitation protocol. When patients were able to walk independently with a T-cane, they were permitted to be discharged from the hospital.
Evaluation Items
We compared the following background variables between the 2 groups: age at the time of the operation, sex, causative disease, body mass index (BMI), preoperative femoral mechanical–anatomical (FMA) angle, knee range of motion (ROM), and Knee Society score (KSS). We also compared clinical outcomes such as operation time, skin incision length, and the postoperative ROM, KSS, FTA, and implant positioning in the coronal plane. The α and β angles were measured according to the method reported by Ewald [16].
Statistical Analyses
Statistical analyses were performed using IBM SPSS Statistics software (v. 22; IBM, Armonk, NY, USA). Variables were compared between the 2 groups using the Mann–Whitney U test or Student t test, and a p value <0.05 was considered significant.
RESULTS
The valgus group was significantly younger at the time of the operation (68.0 ± 6.9 year-old) with higher percentages of male (24%) and rheumatoid arthritis (RA) patients (38%) and had a smaller preoperative FMA angle (6.2 ± 1.0°) compared with the varus group. There was a trend toward a lower BMI (24.4 ± 4.0 kg/m2) in the valgus group. There were no significant differences in the ROM and KSS (Table 1).
Table 1.
Preoperative data.
| Valgus group | Varus group | p value | |
|---|---|---|---|
| Age (years) | 68.0 ± 6.9 | 75.8 ± 6.2 | <0.05 |
| Sex (male/female) | 5/16 | 0/21 | <0.05 |
| Diagnosis (OA/RA) | 8/13 | 20/1 | <0.05 |
| BMI (kg/m2) FMA angle |
24.4 ± 4.0 6.2 ± 1.0° |
26.5 ± 4.4 7.4 ± 2.1° |
0.09 <0.05 |
| Knee ROM (flexion) (extension) |
101.9 ± 19.6° –15.2 ± 12.8° |
100.0 ± 17.3° –13.1 ± 9.9° |
0.72 0.52 |
| KSS | 35.5 ± 15.9 | 33.2 ± 13.6 | 0.59 |
The clinical outcomes in the valgus group included smaller postoperative FTA (173.1 ± 3.9°) and larger α angle (96.6 ± 3.1°) compared with the varus group, but there were no significant differences in the operation time, skin incision, ROM, KSS, and β angle (Table 2).
Table 2.
Perioperative and postoperative data.
| Valgus group | Varus group | p value | |
|---|---|---|---|
| Operation time (minutes) | 154.3 ± 32.4 | 151.0 ± 22.4 | 0.67 |
| Skin incision (cm) | 11.0 ± 1.7 | 10.2 ± 1.9 | 0.14 |
| Knee ROM (flexion) (extension) |
114.6 ± 15.9° –3.6 ± 7.3° |
116.7 ± 15.4° –0.5 ± 1.5° |
0.66 0.06 |
| KSS | 82.0 ± 11.5 | 85.9 ± 1.9 | 0.19 |
| FTA | 173.1 ± 3.9° | 175.2 ± 1.6° | <0.05 |
| Component position α angle β angle |
96.6 ± 3.1° 89.2 ± 3.9° |
95.0 ± 1.9° 89.9 ± 2.2° |
<0.05 0.43 |
DISCUSSION
Chou et al. compared 83 TKAs in the valgus knees in 83 patients with 1084 TKAs in the varus knees in 949 patients and reported younger preoperative mean age and lower BMI (65.0 ± 8.1 years and 26.9 ± 7.4 kg/m2, respectively) in the valgus group [17]. They suggested that the higher percentages of RA (25.3%) and male (74.7%) patients in the valgus group were the main reason for the differences between the groups. In our study, the percentages of RA (61.9%) and male (23.8%) patients were higher and lower, respectively, than in the study by Chou et al., but the mean age (68.0 ± 6.9 years) and BMI (24.4 ± 4.0 kg/m2) were similar to their values. There might be differences in the pathology between the valgus and varus groups. There were also anatomical differences such as the preoperative FMA angle, which was significantly smaller in the valgus group (6.2 ± 1.0°) than in the varus group (7.4 ± 2.1°).
Several authors have noted a similar pattern for the FMA angle. Jingjit et al. reported FMA angles of 6.85° and 5.28° in patients with varus and valgus deformity, respectively [18]. Curtin et al. reported a mean FMA angle of 5.35°, with a wide range of 1° to 10°, and showed that nearly 10% of patients had an FMA angle >7° or <3°. They concluded that routine reliance on a single fixed femoral resection angle could result in malalignment in 10% of patients [19]. Deakin et al. reported a wide distribution of the FMA angle in an osteoarthritic population, with a mean of 5.7° ± 1.2°, and showed that the median FMA angle was larger for the severe varus group (7°) and smaller for the moderate to severe valgus group (5°) compared with the moderate varus or mild valgus group (6°). They concluded that, for severe varus deformities, a femoral cut of 6° or 7° would be within ± 1° of perpendicular to the mechanical axis for 83% and 78% of patients, respectively. However, for the moderate to severe valgus deformities, a femoral cut of 6° would be within this limit for only 52% of patients, and a cut of 5° would be within this limit for 88% of patients [20]. The femoral resection angle was routinely fixed at 6°.
In this study, a postoperative FTA within the neutral alignment (172–177°) was achieved in 21 knees (83%) for the varus group but in 17 knees (65%) for the valgus group. For the other 9 knees whose alignment deviated from neutral in the valgus group, the mean postoperative FTA was 171.2 ± 6.2°, which showed a trend toward residual valgus deformity. Nakano et al. reported the results of TKA for valgus knees performed similarly to the method used in this study based on the NexGen LPS-Flex (they used the medial parapatellar approach in 24 knees and lateral parapatellar approach in 3 knees). They reported mean FTAs of 166.4 ± 4.2° preoperatively and 172.4 ± 2.7° postoperatively, and the alignment of 11 of the 27 knees was outside the range of neutral (172–177°) (178° in 1 knee, 171° in 4 knees, 170° in 3 knees, 169° in 1 knee, and 168° in 2 knees) [21]. This was a trend toward residual valgus deformity that was similar to that found in this study.
The implant positioning angles in the coronal plane (α and β angles) of 9 knees deviated from neutral alignment in the valgus group were 99.4 ± 3.4° and 91.8 ± 2.2°, respectively. It was suspected that over-valgus resection of the femur is one contributory factor to residual valgus alignment. Several authors have recommended using a 3–5° valgus femoral resection for valgus knees to avoid undercorrection of the valgus deformity [9, 22, 23]. Therefore, the implant positioning and alignment can be improved by adjusting the femoral resection angle.
Another possible reason for over-valgus resection is inappropriate insertion of an intramedullary rod. That is, it can be unintentionally inserted in the valgus position compared with the femoral anatomical axis as a consequence of adduction contracture of the hip joint. Numerous randomized studies have reported the use of computer-assisted surgical (CAS) techniques to increase the accuracy of component positioning in TKA. However, there are concerns about the increased operation times, capital costs, extra pin sites, and learning curve for surgeons. Nam et al. demonstrated that accelerometer-based portable navigation is very accurate for overall mechanical, femoral, and tibial component alignment in TKA and compares favorably with large-console CAS systems [24, 25]. We would like to use this system in the future.
In addition to the accuracy of bone resection, adequate lateral soft tissue release is important for preventing residual valgus deformity and patellofemoral alignment problems. The pie crust technique is one helpful method. First, a transverse incision is made through the arcuate ligament (posterolateral capsule), lateral to the popliteus tendon at the level of the tibial bone cut. Following this, multiple horizontal stab incisions are made through the iliotibial band and posterolateral capsule until medial–lateral soft tissue balance is achieved. Clarke et al. reported their clinical outcomes, which showed that the postoperative mean KSS was 97 (range, 87–100) and the mean range of motion was 121° (range, 100–145°) in their TKAs using the medial approach and pie crust technique. They emphasized that there were no clinical failures or cases of postoperative instability or radiographic loosening [15]. Koninckx et al. reported that the KSS improved significantly from 45 to 90 and the knee flexion improved from 110° to 137° in their use of TKA using the far medial approach and this technique. They also noted that no clinical instability or osteolytic lines were observed [26].
Peroneal nerve damage can occur during TKA. The potential risk of direct peroneal nerve injury is associated with the pie crust lateral soft tissue release because of the narrow operative field on the lateral side, especially in the MIS TKA through the medial approach. The mean nerve-to-bone distances have been reported as 1.49 cm (range, 0.91–2.18 cm) and 13.5 mm (11.2–18.6 mm) when detected with magnetic resonance imaging and in a cadaver study, respectively [27, 28]. These results suggest that the peroneal nerve is adequately protected at the posterolateral corner but the pie crust release should be performed carefully. There were no significant differences in the clinical outcomes between the valgus and varus groups and no cases of peroneal nerve injury in this study. These results lead us to believe that the pie crust technique is a useful and safe method.
The lateral approach has been proposed for treating valgus knees with TKA. The advantages of this approach are the direct release of contracted structures on the lateral side as a part of the surgical approach without compromising patella vascularization. On the other hand, the potential disadvantages include difficulty in patellar eversion, which sometimes requires tibial tubercle osteotomy, and the lower familiarity of many surgeons with this approach [26, 29, 30]. Niki et al. reported that 2 of 26 valgus knee patients who underwent TKA with a lateral subvastus approach did not obtain optimum alignment and only 1 patient had subsidence of the tibial component because of malpositioning [31]. It was suggested that, because of the high degree of technical difficulty, surgeons should not use this approach casually.
The choice of implant for valgus deformity between the posterior-stabilized (PS) or cruciate-retaining (CR) implant is controversial. It is difficult to release the PCL appropriately because it is often contracted and degenerated in the valgus deformity. Furthermore, if the PCL seemssuperficially intact, it may gradually degenerate with time. Resection of the PCL increases the flexion gap and may often match the extension gap, which is frequently larger in the valgus deformity. The PS implant is more stable than the CR implant because of the post-cam mechanism, and allows for greater lateralization of the femoral and tibial components, which improves patellar tracking and minimizes the need to perform a lateral retinacular release. For these reasons, some authors have suggested that it is simpler to substitute a contracted PCL with a PS implant and that the PS implant should be used in valgus deformity [26, 30, 32-34]. The use of the PS implant can make the surgery easier and more reproductive for a surgeon wishing to obtain steady clinical outcomes. This is the main reason why we have introduced the PS implant for MIS TKA regardless of whether there is a valgus or varus deformity. This study achieved good clinical outcomes without any major complications.
This study had several limitations. First, the number of patients was small. Secondly, this study was not randomized and there was potential for confounding by indication since patients’ demographics and disease factors were different. Thirdly, we evaluated every alignment only in the coronal plane on a roentgenogram and not in the sagittal and axial planes. Roentgenography has several merits in that it is inexpensive and less invasive than other methods and can be performed in any institution. Fang et al. examined the importance of overall coronal alignment as a predictor of revision and concluded that outliers in overall coronal alignment have a higher rate of revision than well-aligned knees [35]. We consider that it is most important to first evaluate the coronal alignment. In future, we aim to improve the outcomes by adding evaluations of the sagittal and axial alignments using both roentgenography and computed tomography.
CONCLUSION
The study compared the background variables and clinical outcomes between the patients with valgus or varus knees who underwent MIS TKA through the medial approach. Compared with the varus group, the valgus group was significantly younger at the time of the operation and had a higher percentage of men and RA patients. The clinical outcomes in the valgus group included a smaller postoperative FTA compared with the varus group. It was believed that over-valgus resection of the femur was the one contributory factor to the residual valgus alignment. There were no significant differences in the ROM or KSS between the groups. These findings suggest that MIS TKA through the medial approach is one of the treatment options for patients with valgus deformity.
ACKNOWLEDGEMENTS
This work was performed at Department of Orthopaedic Surgery, Surgical Science, Tokai University School of Medicine, Isehara, Kanagawa, Japan.
LIST OF ABBREVIATIONS
- BMI
= Body mass index
- CR
= Cruciate-retaining
- FMA
= Femoral mechanical–anatomical
- FTA
= Femorotibial angle
- KSS
= Knee Society score
- MIS TKA
= Minimally invasive total knee arthroplasty
- OA
= Osteoarthritis
- PCL
= Posterior cruciate ligament
- PS
= Posterior-stabilized
- RA
= Rheumatoid arthritis
- ROM
= Range of motion.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Smith T.O., King J.J., Hing C.B. A meta-analysis of randomised controlled trials comparing the clinical and radiological outcomes following minimally invasive to conventional exposure for total knee arthroplasty. Knee. 2012;19(1):1–7. doi: 10.1016/j.knee.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Thienpont E. Faster recovery after minimally invasive surgery in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2013;21(10):2412–2417. doi: 10.1007/s00167-012-1978-6. [DOI] [PubMed] [Google Scholar]
- 3.Varela-Egocheaga J.R., Suárez-Suárez M.A., Fernández-Villán M., González-Sastre V., Varela-Gómez J.R., Rodríguez-Merchán C. Minimally invasive subvastus approach: improving the results of total knee arthroplasty: a prospective, randomized trial. Clin. Orthop. Relat. Res. 2010;468(5):1200–1208. doi: 10.1007/s11999-009-1160-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schroer W.C., Diesfeld P.J., Reedy M.E., LeMarr A.R. Mini-subvastus approach for total knee arthroplasty. J. Arthroplasty. 2008;23(1):19–25. doi: 10.1016/j.arth.2006.12.100. [DOI] [PubMed] [Google Scholar]
- 5.Cheng T., Liu T., Zhang G., Peng X., Zhang X. Does minimally invasive surgery improve short-term recovery in total knee arthroplasty? Clin. Orthop. Relat. Res. 2010;468(6):1635–1648. doi: 10.1007/s11999-010-1285-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gandhi R., Smith H., Lefaivre K.A., Davey J.R., Mahomed N.N. Complications after minimally invasive total knee arthroplasty as compared with traditional incision techniques: a meta-analysis. J. Arthroplasty. 2011;26(1):29–35. doi: 10.1016/j.arth.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 7.Nestor B.J., Toulson C.E., Backus S.I., Lyman S.L., Foote K.L., Windsor R.E. Mini-midvastus vs standard medial parapatellar approach: a prospective, randomized, double-blinded study in patients undergoing bilateral total knee arthroplasty. J. Arthroplasty. 2010;25(6) Suppl.:5–11, 11.e1. doi: 10.1016/j.arth.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Wegrzyn J., Parratte S., Coleman-Wood K., Kaufman K.R., Pagnano M.W. The John Insall award: no benefit of minimally invasive TKA on gait and strength outcomes: a randomized controlled trial. Clin. Orthop. Relat. Res. 2013;471(1):46–55. doi: 10.1007/s11999-012-2486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elkus M., Ranawat C.S., Rasquinha V.J., Babhulkar S., Rossi R., Ranawat A.S. Total knee arthroplasty for severe valgus deformity. Five to fourteen-year follow-up. J. Bone Joint Surg. Am. 2004;86-A(12):2671–2676. doi: 10.2106/00004623-200412000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Karachalios T., Sarangi P.P., Newman J.H. Severe varus and valgus deformities treated by total knee arthroplasty. J. Bone Joint Surg. Br. 1994;76(6):938–942. [PubMed] [Google Scholar]
- 11.Rajgopal A., Dahiya V., Vasdev A., Kochhar H., Tyagi V. Long-term results of total knee arthroplasty for valgus knees: soft-tissue release technique and implant selection. J. Orthop. Surg. (Hong Kong) 2011;19(1):60–63. doi: 10.1177/230949901101900114. [DOI] [PubMed] [Google Scholar]
- 12.Dehring D.J., Arens J.F. Pulmonary thromboembolism: disease recognition and patient management. Anesthesiology. 1990;73(1):146–164. doi: 10.1097/00000542-199007000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Coon T.M. Quadriceps-sparing minimally invasive technique for total knee arthroplasty : a new classification. Orthopade. 2007;36(12):1113–1119. doi: 10.1007/s00132-007-1172-6. [DOI] [PubMed] [Google Scholar]
- 14.Martin A., Sheinkop M.B., Langhenry M.M., Oelsch C., Widemschek M., von Strempel A. Accuracy of side-cutting implantation instruments for total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2009;17(4):374–381. doi: 10.1007/s00167-008-0704-x. [DOI] [PubMed] [Google Scholar]
- 15.Clarke H.D., Fuchs R., Scuderi G.R., Scott W.N., Insall J.N. Clinical results in valgus total knee arthroplasty with the pie crust technique of lateral soft tissue releases. J. Arthroplasty. 2005;20(8):1010–1014. doi: 10.1016/j.arth.2005.03.036. [DOI] [PubMed] [Google Scholar]
- 16.Ewald F.C. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin. Orthop. Relat. Res. 1989;(248):9–12. [PubMed] [Google Scholar]
- 17.Chou P.H., Chen W.M., Chen C.F., Chiang C.C., Liu C.L., Chen T.H. Clinical comparison of valgus and varus deformities in primary total knee arthroplasty following midvastus approach. J. Arthroplasty. 2012;27(4):604–612. doi: 10.1016/j.arth.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 18.Jingjit W., Poomcharoen P., Limmahakhun S., Klunklin K., Leerapun T., Rojanasthien S. Femoral mechanical-anatomical angle of osteoarthritic knees. J. Med. Assoc. Thai. 2014;97(12):1314–1318. [PubMed] [Google Scholar]
- 19.Curtin B., Fehring T.K., Lauber J. Errors in knee alignment using fixed femoral resection angles. Orthopedics. 2014;37(7):e644–e648. doi: 10.3928/01477447-20140626-56. [DOI] [PubMed] [Google Scholar]
- 20.Deakin A.H., Basanagoudar P.L., Nunag P., Johnston A.T., Sarungi M. Natural distribution of the femoral mechanical-anatomical angle in an osteoarthritic population and its relevance to total knee arthroplasty. Knee. 2012;19(2):120–123. doi: 10.1016/j.knee.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Nakano N., Matsumoto T., Muratsu H., Matsushita T., Takayama K., Matsuzaki T., Kuroda R., Kurosaka M. Results of total knee arthroplasty with NexGen LPS-Flex for osteoarthritis in the valgus knee: a study of 26 patients followed for a minimum of 2 years. Eur. J. Orthop. Surg. Traumatol. 2015;25(2):375–380. doi: 10.1007/s00590-014-1505-1. [DOI] [PubMed] [Google Scholar]
- 22.Apostolopoulos A.P., Nikolopoulos D.D., Polyzois I., Nakos A., Liarokapis S., Stefanakis G., Michos I.V. Total knee arthroplasty in severe valgus deformity: interest of combining a lateral approach with a tibial tubercle osteotomy. Orthop. Traumatol. Surg. Res. 2010;96(7):777–784. doi: 10.1016/j.otsr.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 23.Nikolopoulos D.D., Polyzois I., Apostolopoulos A.P., Rossas C., Moutsios-Rentzos A., Michos I.V. Total knee arthroplasty in severe valgus knee deformity: comparison of a standard medial parapatellar approach combined with tibial tubercle osteotomy. Knee Surg. Sports Traumatol. Arthrosc. 2011;19(11):1834–1842. doi: 10.1007/s00167-011-1474-4. [DOI] [PubMed] [Google Scholar]
- 24.Nam D., Nawabi D.H., Cross M.B., Heyse T.J., Mayman D.J. Accelerometer-based computer navigation for performing the distal femoral resection in total knee arthroplasty. J. Arthroplasty. 2012;27(9):1717–1722. doi: 10.1016/j.arth.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 25.Nam D., Weeks K.D., Reinhardt K.R., Nawabi D.H., Cross M.B., Mayman D.J. Accelerometer-based, portable navigation vs imageless, large-console computer-assisted navigation in total knee arthroplasty: a comparison of radiographic results. J. Arthroplasty. 2013;28(2):255–261. doi: 10.1016/j.arth.2012.04.023. [DOI] [PubMed] [Google Scholar]
- 26.Koninckx A., Schwab P.E., Deltour A., Thienpont E. The minimally invasive far medial subvastus approach for total knee arthroplasty in valgus knees. Knee Surg. Sports Traumatol. Arthrosc. 2014;22(8):1765–1770. doi: 10.1007/s00167-013-2701-y. [DOI] [PubMed] [Google Scholar]
- 27.Bruzzone M., Ranawat A., Castoldi F., Dettoni F., Rossi P., Rossi R. The risk of direct peroneal nerve injury using the Ranawat inside-out lateral release technique in valgus total knee arthroplasty. J. Arthroplasty. 2010;25(1):161–165. doi: 10.1016/j.arth.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 28.Clarke H.D., Schwartz J.B., Math K.R., Scuderi G.R. Anatomic risk of peroneal nerve injury with the pie crust technique for valgus release in total knee arthroplasty. J. Arthroplasty. 2004;19(1):40–44. doi: 10.1016/j.arth.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 29.Buechel F.F. A sequential three-step lateral release for correcting fixed valgus knee deformities during total knee arthroplasty. Clin. Orthop. Relat. Res. 1990;(260):170–175. [PubMed] [Google Scholar]
- 30.Rossi R., Rosso F., Cottino U., Dettoni F., Bonasia D.E., Bruzzone M. Total knee arthroplasty in the valgus knee. Int. Orthop. 2014;38(2):273–283. doi: 10.1007/s00264-013-2227-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Niki Y., Matsumoto H., Hakozaki A., Kanagawa H., Toyama Y., Suda Y. Clinical and radiographic outcomes of minimally invasive total knee arthroplasty through a lateral approach. Knee Surg. Sports Traumatol. Arthrosc. 2011;19(6):973–979. doi: 10.1007/s00167-010-1323-x. [DOI] [PubMed] [Google Scholar]
- 32.Anderson J.A., Baldini A., MacDonald J.H., Pellicci P.M., Sculco T.P. Primary constrained condylar knee arthroplasty without stem extensions for the valgus knee. Clin. Orthop. Relat. Res. 2006;442(442):199–203. doi: 10.1097/01.blo.0000185675.99696.29. [DOI] [PubMed] [Google Scholar]
- 33.Easley M.E., Insall J.N., Scuderi G.R., Bullek D.D. Primary constrained condylar knee arthroplasty for the arthritic valgus knee. Clin. Orthop. Relat. Res. 2000;(380):58–64. doi: 10.1097/00003086-200011000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Lombardi A.V., Jr, Dodds K.L., Berend K.R., Mallory T.H., Adams J.B. An algorithmic approach to total knee arthroplasty in the valgus knee. J. Bone Joint Surg. Am. 2004;86-A(Suppl. 2):62–71. doi: 10.2106/00004623-200412002-00010. [DOI] [PubMed] [Google Scholar]
- 35.Fang D.M., Ritter M.A., Davis K.E. Coronal alignment in total knee arthroplasty: just how important is it? J. Arthroplasty. 2009;24(6) Suppl.:39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]


