Abstract
SDF-1 (stromal cell derived factor-1) has been found to be widely expressed during dental pulp inflammation, while hDPSCs (human dental pulp stem cells) contribute to the repair of dental pulp. We showed that the migration of hDPSCs was induced by SDF-1 in a concentration-dependent manner and could be inhibited with siCXCR4 (C-X-C chemokine receptor type 4) and siCDC42 (cell division control protein 42), as well as drug inhibitors such as AMD3100 (antagonist of CXCR4), LY294002 (inhibitor of PI3K) and PF573228 (inhibitor of FAK). It was also confirmed that SDF-1 regulated the phosphorylation of FAK (focal adhesion kinases) on cell membranes and the translocation of β-catenin into the cell nucleus. Subsequent experiments confirmed that the expression of CXCR4 and β-catenin and the phosphorylation of FAK, PI3K (phosphoinositide 3-kinase), Akt and GSK3β (glycogen synthase kinase-3β) were altered significantly with SDF-1 stimulation. FAK and PI3K worked in coordination during this process. Our findings provide direct evidence that SDF-1/CXCR4 axis induces hDPSCs migration through FAK/PI3K/Akt and GSK3β/β-catenin pathways, implicating a novel mechanism of dental pulp repair and a possible application of SDF-1 for the treatment of pulpitis.
Dental caries, the major cause of dentin damage, are widely seen worldwide. At the late stage of caries, inflammation will emerge at the dental pulp under the caries and induce apoptosis of odontoblasts. This process can be partially repaired under the effect of human dental pulp stem cells (hDPSCs). HDPSCs belong to mesenchymal stromal cells (MSCs) and express a number of chemokine and adhesion receptors1. Maintained in the stem cell niche around the blood vessels2, hDPSCs can be stimulated by chemokines expressed in extracellular matrixes. Thereafter, hDPSCs migrate to the damaged area and play a vital role during the regeneration of odontoblasts and the formation of reparative dentin3.
Chemotaxis is a complex cell behavior initiated by the binding of chemokines to their receptors, and accompanied by rearrangement of the cytoskeleton4. Chemokines are a group of secreted proteins able to induce the migration of cells that highly express their receptors5. Stromal cell derived factor-1 (also known as SDF-1 or CXCL12) interacts with its G-protein coupled receptor CXCR4 to induce SDF-1/CXCR4 signaling6. SDF-1 has also been shown to bind CXCR77, but this binding does not contribute significantly to cell chemotaxis8. Ischemic kidneys could recruit MSCs by secreting SDF-1, which could be blocked by an antibody against CXCR4 but not against CXCR79. Under physiological conditions, SDF-1/CXCR4 interaction participates in hematopoiesis and vascular development10. SDF-1 is essential for the migration of hematopoietic stem cells between bone marrow and blood11. The concentration of SDF-1 significantly correlates its effects, and excessive concentrations may act as an inhibitor12. Under pathological conditions, SDF-1 also contributes to the invasion and metastases of several tumor cells13. CXCR4 is expressed in a number of cancer cells, including prostate cancer, breast cancer and lung cancer. Additionally, inhibiting the activity of SDF-1 or blocking its binding to CXCR4 could reduce the migration or metastasis of cancer cells14. The SDF-1/CXCR4 axis is also upregulated during experimental models of burn wounds or myocardial infarction (MI)15.
Previous studies have shown that inflammation could improve the expression level of stromal cell derived factor-1α in dental pulp16. However, the signal networks that connect SDF-1 with the cell migration are still not well understood. The phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt) activation has been shown to participate in the chemotaxis of MSCs17. AMD3100 could reverse the levels of phospho-Akt during MSCs migration induced by SDF-1/CXCR4 axis. Inhibiting the activation of glycogen synthase kinase-3β (GSK3β) could increase the expression of CXCR418. β-catenin, which mediates the generation of mesoderm during embryogenesis19, participates in the migration and invasiveness of human mesenchymal cells20. It locates at the cell surface and links to actin cytoskeleton by binding to α-catenin. Upon activation, β-catenin dissociates from the cell membrane and translocates into nucleus to regulate the expressions of cytoskeleton proteins21. Previous reports demonstrated that GSK3β inhibition could augment the expression of β-catenin22.
During the process of chemotaxis, CDC42 which locates at the leading edge could be activated23. CDC42 belongs to the Rho GTPases family which regulates the arrangement of actin cytoskeleton and affects cell motility24. The dynamic remodeling of the cytoskeleton is necessary for cell migration. CDC42 modulates cell migration by coordinating the actin-based structures located at the leading edge of cells25. It is generally thought that CDC42 induce the formation of cellular protrusions such as filopodia by activating actin-associated proteins and inducing F-actin bundles26. Those actin-associated proteins include Wasp (Wiskott-Aldrich syndrome protein) and PAKs (p21-activated kinases), while Wasp regulates the formation of filopodia and actin polymerization and PAKs affects the activation of actin-binding protein cofilin27.
In the present study, we investigated the ability of SDF-1 to increase the migration of hDPSCs. Considering that both PI3K/Akt and GSK3β/β-catenin play roles during cell migration, we hypothesized that SDF-1 may regulate the migration of hDPSCs through these pathways. Additionally, given that CDC42 plays a critical role in cytoskeleton rearrangements, we hypothesized that the migration of hDPSCs stimulated by SDF-1 requires the participation of CDC42.
Results
The expression of CXCR4 and SDF-1 and their role in promoting migration in human dental pulp stem cells
Because SDF-1, as one type of chemokine, induces cell migration through its seven-transmembrane receptor CXCR4, we first analyzed the expression of CXCR4 in hDPSCs by RT-PCR, Western blot and immunofluorescence. Considering that CXCR4 had been well studied in HeLa cells, we chose them as the positive control. Because hDPSCs form clones during proliferation, six clones were divided into two groups to detect the expression of mRNA and protein. The results of electrophoresis showed CXCR4 mRNA expressions in all clones of hDPSCs as abundantly as that in HeLa (Fig. 1A). The expression levels of endogenous CXCR4 protein varied in these three clones, but all of them showed positive expression when compared with HeLa (Fig. 1B). The expression of CXCR4 in hDPSCs at the cell level was also observed by immunofluorescence. Cells incubated without a primary antibody were taken as the negative control (Fig. 1C). The Western blot results showed that SDF-1 affected the expression of CXCR4 in a dose-dependent manner (Fig. 1D).
Figure 1. Expression of CXCR4 and SDF-1 and their role in promoting migration of hDPSCs.
(A) RT-PCR analysis of CXCR4 mRNA in hDPSCs. (B) CXCR4 was identified by Western blot in hDPSCs. HeLa cells (A and B) were taken as positive control. (C) Immunofluorescence analysis of CXCR4 expression in hDPSCs. Cells not incubated with primary antibodies were taken as negative control. (D) The hDPSCs were cultured in medium with the indicated dose of SDF-1 for 48 hours and subjected to Western blot using CXCR4 antibody. (E) The hDPSCs were used in Transwell assays with the indicated dose of SDF-1 in the lower well. Cells that migrated to the lower side of the well were fixed and stained for 12 hours. Representative images are shown. The quantitative results (D and E) are the means ± SD of three independent experiments. Comparison with the control group (0 ng/ml): *p < 0.05; #p < 0.01. In (C), scale bar = 100 μm; in (E), scale bar = 200 μm.
We next detected the effect of SDF-1 on the migration of hDPSCs. Transwell assays were performed, and a concentration-dependent manner was obtained in this section (Fig. 1E). The increasing dose of SDF-1 in the lower compartment of Transwell significantly promoted the number of cells migrating to the lower side of the inserts. Even if the dose was as low as 30 ng/ml, SDF-1 treated cells still showed a difference compared with the control group. A statistically significant difference was observed when the dose was increased to 50 ng/ml.
SDF-1 mediated concentration-dependent and time-dependent activation of FAK, PI3K, Akt, and GSK3β and expression of β-catenin
SDF-1 mediated expression and activation of CXCR4 has been shown to regulate several signaling pathways related to cell development and migration28. To investigate the signal transition induced by SDF-1 in hDPSCs, we examined the phosphorylated protein level changes of FAK, PI3K, Akt and GSK3β, as well as the protein level alterations of β-catenin after cells were stimulated by the indicated concentration of SDF-1 (30, 50, or 100 ng/ml) for 2 hours (Fig. 2A). Compared with the control group, cells treated with SDF-1 showed greater expression of phosphorylated proteins. More phosphorylated GSK3β and β-catenin were detected with increasing concentration of SDF-1. However, no obvious differences of the expression of the phosphorylated proteins FAK, PI3K and Akt were observed among the treatment groups. Next, time course experiments were performed to examine the phosphorylated protein level alteration over time (Fig. 2B). The results obtained at 15 min showed that all the level of phosphorylated proteins in the treatment group were higher level than in the control group. Especially, the phosphorylated Akt increased more than 8 folds. However, the phosphorylated Akt level was downregulated as time increased to 90 min. Meanwhile, the expressions of β-catenin did not show any increase until 60 min.
Figure 2. SDF-1 mediated concentration-dependent and time-dependent effects on FAK, PI3K, Akt, GSK3β and β-catenin protein expression.
(A) The hDPSCs cultured in medium with the indicated dose of SDF-1 for 2 hours were subjected to Western blots. (B) The hDPSCs cultured in medium with SDF-1 (50 ng/ml) for the indicated times were detected by Western blot. Representative images and quantitative results (A and B) are shown. The membrane expression of p-FAK (C) and the nucleus translocation of β-catenin (D) were obtained after 50 ng/ml SDF-1 stimulation for 6 hours. Cells without SDF-1 stimulation were taken as control. The quantitative results (A and B) are the means ± SD of three independent experiments. The white arrows (C) indicate p-FAK at the leading edge. Comparison with the control group: *p < 0.05; #p < 0.01. In (C) and (D), scale bars = 50 μm.
Considering that cell migration depends on the regulation of focal adhesions by FAK and cell skeleton rearrangement by β-catenin, we determined their distributions after SDF-1 stimulation for 6 hours in hDPSCs. The results obtained with p-FAK immunofluorescence showed that enhanced expression of phosphorylated FAK was found at the leading edge of migrating cells compared to the control group (Fig. 2C). However, under the same condition, higher levels of β-catenin were located in the nucleus where they regulated cell migration by acting as a transcription factor (Fig. 2D).
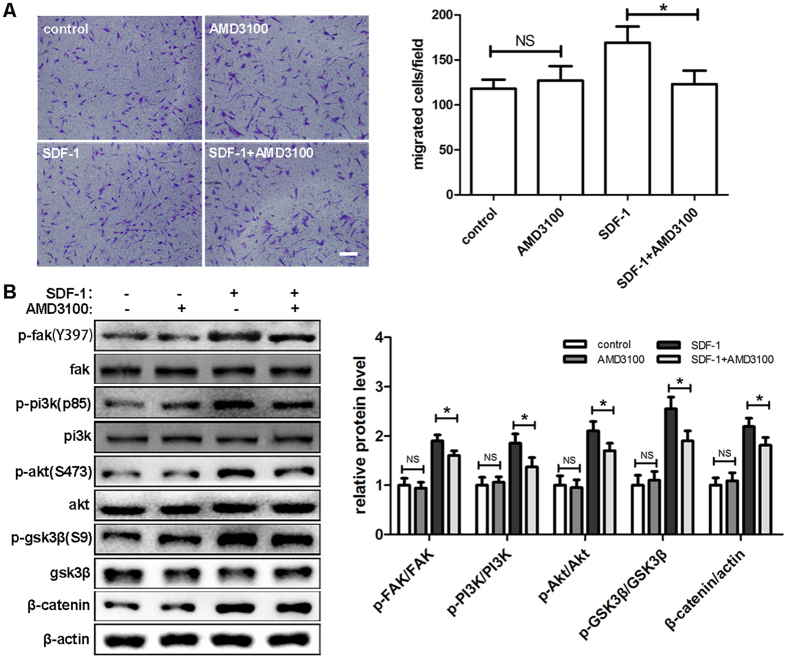
AMD3100 suppresses SDF-1/CXCR4 signaling and hDPSCs migration
As a selective CXCR4 antagonist, AMD3100 could disrupt the interaction of SDF-1 and CXCR429. Transwell assays were performed to observe its effects on hDPSCs migration. The results showed that AMD3100 significantly reduced cell migration caused by SDF-1, while no reduction was detected in the group treated with AMD3100 alone (Fig. 3A). Consistent with the migration study, no alteration was found in the level of phosphorylated protein of FAK, PI3K, Akt and GSK3β with AMD3100 treatment alone. However, AMD3100 successfully inhibited the increases of p-FAK, p-PI3K, p-Akt and p-GSK3β induced by SDF-1 treatment. The same results were also obtained in the expression of β-catenin (Fig. 3B).
Figure 3. AMD3100 suppressed SDF-1/CXCR4 signaling and hDPSCs migration.
(A) After preincubation with AMD3100 (100 ng/ml) for 1 hour, hDPSCs were used in Transwell assays with AMD3100 in the upper chamber and SDF-1 in the lower chamber and allowed to migrate for 12 hours. (B) After preincubation with AMD3100 for 1 hour and culture in medium with the indicated drug concentrations (100 ng/ml AMD3100, 50 ng/ml SDF-1) for 2 hours, cells were subjected to Western blots. The quantitative results (A and B) are the means ± SD of three independent experiments. NS, not significant; *p < 0.05. In (A), scale bar = 200 μm.
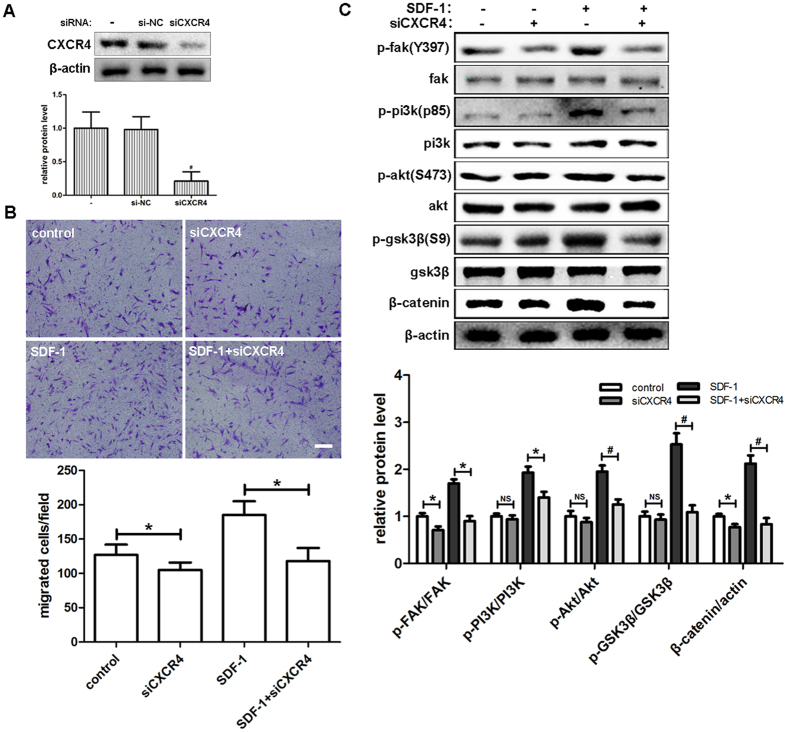
Downregulation of CXCR4 by siRNA transfection decreases hDPSCs migration and SDF-1/CXCR4 signaling
Since the function of SDF-1 depends on the activation of CXCR4, we investigated whether downregulation of CXCR4 by siRNA transfection could affect the migration of hDPSCs as we had observed with AMD3100 inhibition. First, we confirmed the knockdown effect of siRNA on the expression of CXCR4 in hDPSCs (Fig. 4A). Unlike AMD3100, treatment with siCXCR4 alone also inhibited the migration of hDPSCs in the Transwell assays. The increases of migrated cells by SDF-1 were completely diminished by siCXCR4 treatment (Fig. 4B). The results obtained with Western blot were similar to those of the Transwell assays. The expression of p-FAK and β-catenin was decreased by siCXCR4 when compared with the control group. The level of p-PI3K, p-Akt, and p-GSK3β also showed a slight downregulation with siCXCR4 alone, although no statistically significant differences were detected. In groups treated with SDF-1, all the levels of phosphorylated proteins and β-catenin experienced a significant reduction when pretreated with CXCR4 siRNA (Fig. 4C).
Figure 4. Downregulation of CXCR4 by siRNA transfection decreased the migration of hDPSCs and SDF-1/CXCR4 signaling.
(A) After transfection with siCXCR4 for 48 hours, hDPSCs were subjected to Western blot and CXCR4 was detected with the indicated antibody. (B) Cells transfected with siCXCR4 were used in Transwell assays with the indicated medium (50 ng/ml SDF-1) in the lower chamber. Cells that migrated to the lower side of the well were fixed and stained for 12 hours. Representative images are shown. (C) After transfection with siCXCR4 for 48 hours, cells were cultured in the indicated medium (50 ng/ml SDF-1) for 2 hours and subjected to Western blots. The quantitative results (A,B and C) are the means ± SD of three independent experiments. NS, not significant; *p < 0.05; #p < 0.01. In (B), scale bar = 200 μm.
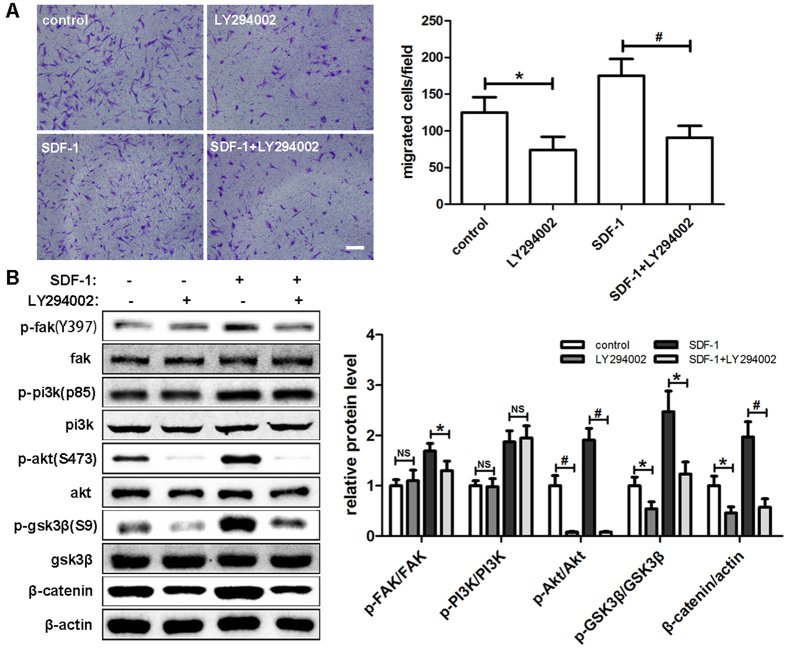
PI3K inhibition by LY294002 plays a negative role during the migration of hDPSCs
To assess the effect of PI3K/Akt signaling pathway on the migration of hDPSCs, cells were pretreated with 20 μM LY294002, a specific PI3K inhibitor, for 1 hour before SDF-1 treatment. A clear reduction by approximately 30% in migrating cells was detected when cells were treated with LY294002 alone. This finding suggests that the PI3K/Akt signaling pathway is necessary for hDPSCs migration. When combined with SDF-1, LY294002 still showed a large inhibitory effect compared with groups treated with SDF-1 alone (Fig. 5A). In subsequent experiments, we examined the expression levels of phosphorylated proteins in hDPSCs (Fig. 5B). Compared with the control group, p-Akt showed an extraordinary downregulation of more than 90% after LY294002 treatment alone. Similar results were also obtained for p-GSK3β and β-catenin with reductions of approximately 50%, but no significant differences were detected with p-FAK and p-PI3K. When combined with SDF-1, LY294002 significantly downregulated the expression levels of p-FAK, which was different from that with LY294002 alone. The comparisons of the other protein expressions were similar to what we observed in groups without SDF-1 treatment.
Figure 5. PI3K inhibition by LY294002 played a negative role during the migration of hDPSCs.
(A) After preincubation with LY294002 (20 μM) for 1 hour, hDPSCs were used in Transwell assays with LY294002 in the upper chamber and SDF-1 in the lower chamber and allowed to migrate for 12 hours. (B) After preincubation with LY294002 for 1 hour and culture in medium with the indicated drug concentrations (20 μM LY294002, 50 ng/ml SDF-1) for 2 hours, cells were subjected to Western blots. The quantitative results (A and B) are the means ± SD of three independent experiments. NS, not significant; *p < 0.05; #p < 0.01. In (A), scale bar = 200 μm.
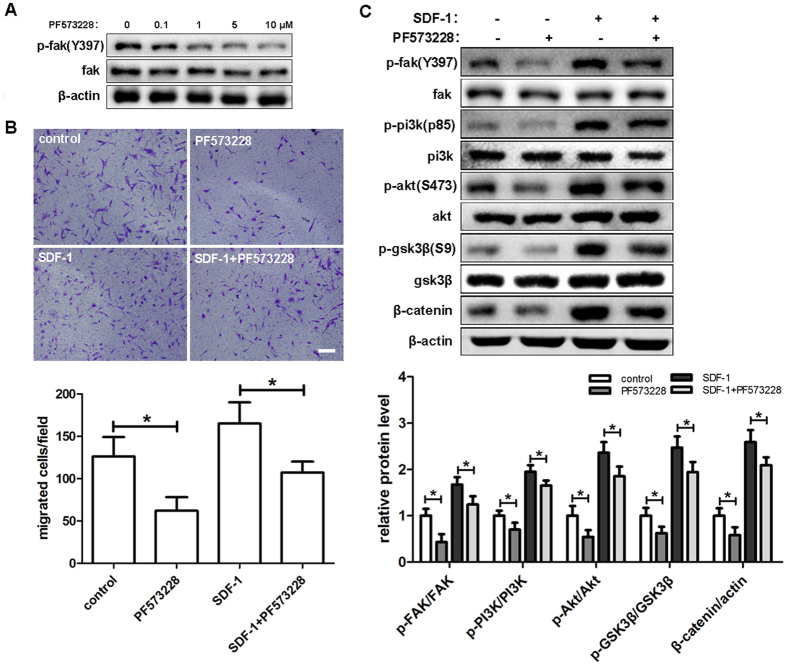
Effect of FAK inhibitor PF573228 on hDPSCs migration and SDF-1/CXCR4 signaling
Considering that focal adhesion kinase (FAK) is located on the cell membrane and interacts with the extra cellular matrix through integrins30, we determined whether FAK played a biological role during the migration of hDPSCs induced by SDF-1. Concentration-response experiments were performed, and 10 μM PF573228 was chosen to inhibit the activation of FAK based upon Western blot results (Fig. 6A). After treatment with PF573228 alone, the migration of hDPSCs was inhibited more than 50% compared with the untreated group. Similarly, the inhibitor also decreased hDPSCs migration after treatment with SDF-1 (Fig. 6B). In subsequent experiments, we analyzed the effect of PF573228 at the protein level and observed similar results as with cell migration. Whether the cells were treated with SDF-1 or not, the expression levels of p-FAK, p-PI3K, p-Akt, p-GSK3β and β-catenin were significantly downregulated by the inhibitor treatment. However, the differences between the groups treated with SDF-1 were no different than those without SDF-1 treatment (Fig. 6C).
Figure 6. Effect of FAK inhibitor PF573228 on hDPSCs migration and SDF-1/CXCR4 signaling.
(A) hDPSCs were cultured in medium with the indicated concentration of PF573228 for 2 hours and then subjected to Western blot using the indicated antibodies. (B) After preincubation with PF573228 (10 μM) for 1 hour, the hDPSCs were used in Transwell assays with LY294002 in the upper chamber and SDF-1 in the lower chamber and allowed to migrate for 12 hours. (C) After preincubation with PF573228 (10 μM) for 1 hour, hDPSCs were subjected to Western blots and detected with the indicated antibodies. The quantitative results (B and C) are the means ± SD of three independent experiments. NS, not significant; *p < 0.05. In (B), scale bar = 200 μm.
siRNA mediated CDC42 inhibition decreases hDPSCs migration
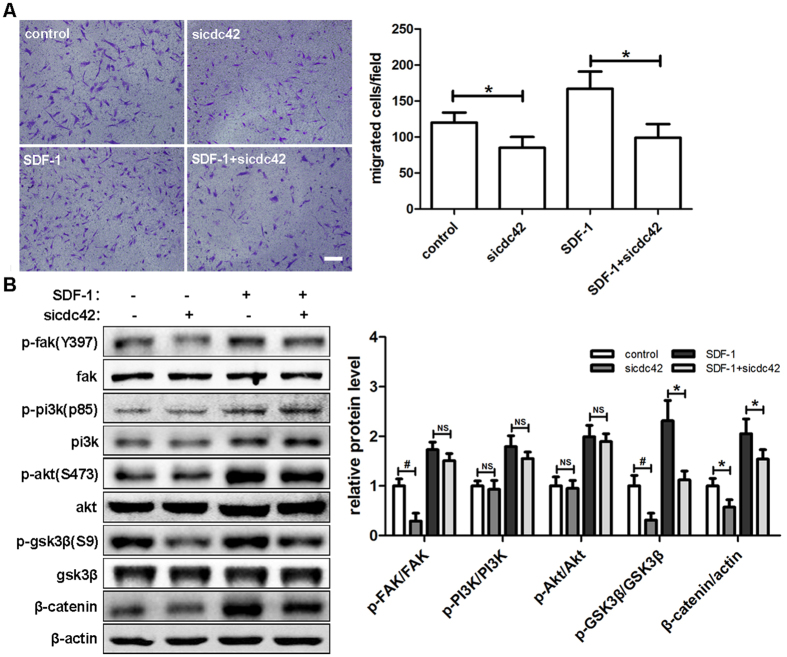
Cell skeleton rearrangements are required during cell migration, and CDC42 plays a central role in this process. Thus, we hypothesized that the migration of hDPSCs induced by SDF-1 could be regulated by CDC42. After transfection with siCDC42 (unpublished results) for 48 hours, migration assays were performed and the migrating ability of hDPSCs was clearly inhibited. Combined with SDF-1, siCDC42 almost reversed the increase of hDPSCs migration triggered by SDF-1 alone (Fig. 7A). Next, the effects of siCDC42 on the protein expression of the SDF-1 signaling pathway were examined (Fig. 7B). When the cells were treated with siCDC42 alone, the expression levels of p-FAK, p-GSK3β and β-catenin were downregulated significantly. Similar results were obtained in the groups treated with SDF-1 and siCDC42, except that no significant difference was detected for p-FAK. As for the phosphorylation levels of PI3K and Akt, no differences were observed with siCDC42, whether the cells were treated with SDF-1 or not.
Figure 7. SiRNA mediated CDC42 inhibition decreased hDPSCs migration.
(A) After transfection with siCDC42 for 48 hours, cells were used in Transwell assays with the indicated medium (50 ng/ml SDF-1) in the lower chamber and allowed to migrate for 12 hours. (B) After transfection with siCDC42 for 48 hours, cells were cultured in the indicated medium (50 ng/ml SDF-1) for 2 hours and then subjected to Western blots. The quantitative results (A and B) are the means ± SD of three independent experiments. NS, not significant; *p < 0.05; #p < 0.01. In (A), scale bar = 200 μm.
Discussion
The development of dental caries typically comes along with the invasion of bacteria into dentin, and the induction of pulpitis occurs when the odontoblasts under the caries are infected by the bacteria. Pulpitis is characterized by the loss of dentin and destruction of odontoblast cell layers. After treatment, the repair of the damaged tissues under both situations requires the participation of hDPSCs. However, because the hDPSCs reside in the stem cell niches near the blood vessels in the dental pulp, it is required for them to expand and migrate to the damaged area to generate new odontoblasts for repair. The migration and homing of hDPSCs to damaged tissue are probably a multistep process and share some common characteristics with the migration of leukocyte to inflammatory sites31. Because hDPSCs are used for therapeutic purposes, it would be important to understand the process regulating their migration.
The migration of stem cells is regulated by a number of secreted molecules, including chemokines. SDF-1 has been well known as an essential mediator during the physiological development of tissues and pathogenesis of many diseases32. SDF-1 has six different splicing variants (α, β, γ, δ, ε, ψ), of which SDF-1α is expressed widely across different tissues and mediates several different activities, including adhesion, chemotaxis and survival33. All the isoforms share a same N-terminal domain to bind and activate receptors and a different C-terminal domain to stabilize the interactions with receptors34. Increasing the expression level of SDF-1 could increase the capillary density of the myocardium after MI35. As a stem cell homing factor, SDF-1 contributes to tissue regeneration and healing by recruiting CXCR4 positive progenitors to the damaged area. The investigation of cell therapy for self-repair found that CXCR4, the receptor of SDF-1, was an important regulator of the migration towards the regions of brain injury36. Cytokines secreted during inflammation, including TNF (tumor necrosis factor) and VEGF (vascular endothelial growth factor), could also induce the expression of CXCR437.
Although previous studies have confirmed that SDF-1 is highly expressed during the inflammation of the dental pulp38, the specific roles of SDF-1 in the repair of the dental pulp still remains unclear. In the present study, we first demonstrated the expression of CXCR4 in hDPSCs compared with HeLa cells. SDF-1 has been shown to be a principal regulator of migration and mobilization of endothelial progenitor cells and hematopoietic stem cells39. Experiments in vivo found that MI in rats increased the level of SDF-1 that induced the migration of BMSCs40. Many experiments performed with tissue injury have confirmed the upregulation of the SDF-1/CXCR4 axis, such as burn wounds41, acute kidney injury42 and MI43. If SDF-1 signaling was disturbed, the recruitment of MSCs to the bone fractures and the repair would be inhibited44. All the studies above support the importance of the role of SDF-1/CXCR4 during stem cell migration. Our data also demonstrate that both the expression of CXCR4 and the migration of hDPSCs are highly upregulated by the indicated concentrations of SDF-1. Studies on the trans-endothelial migration of hematopoietic stem cells have revealed that SDF-1 is an important chemoattractant45, which could be the presumed role of SDF-1 in this study.
The SDF-1/CXCR4 axis has been shown to regulate cell migration through several signaling pathways46. PI3K is widely involved in the regulation of multiple stem cell migration by coordinating the function and localization of lipids through pleckstrin homology (PH) domains47, through which PI3K also recruits the protein kinase Akt. However, there are no related studies of the role of SDF-1α in hDPSCs migration. Microarray studies have demonstrated that SDF-1/CXCR4 axis inhibition may affect the GSK3β/β-catenin pathway48. To understand the molecular mechanisms underlying hDPSCs migration, both concentration-response and time course experiments were performed to evaluate the SDF-1 signaling pathway and showed that SDF-1 induces the phosphorylation of FAK, PI3K, Akt, and GSK3β, as well as the expression of β-catenin. This finding suggests that all of them participate in the function of SDF-1 during hDPSCs migration, though the exact connections among these proteins remain to be examined.
Consequently, because CXCR4 plays a key role in SDF-1/CXCR4 axis, we sought to determine the effect of CXCR4 knockdown on the migration of hDPSCs induced by SDF-1. Research on vascular progenitor migration has identified that CXCR4 directly participated in this process49, and preclinical studies have revealed that metastasis of cancer is directly mediated by CXCR450. Several pathways have been associated with CXCR4 in cancer cells, such as Erk/p38 and PI3K/Akt/NFκB, whereas CXCR4 inhibition deactivated Akt without Erk revealing cell context-specific pathway regulation51. In our present study, when no SDF-1 was added, the knockdown of CXCR4 still reduced the phosphorylation of FAK and the expression of β-catenin. This result suggests that CXCR4, more than a SDF-1 receptor, may also act as a regulator of another pathway and regulate cell migration through β-catenin. Under the stimulation of SDF-1, inhibiting the expression of p-FAK, p-PI3K, p-Akt, p-GSK3β and β-catenin by siCXCR4 identified their downstream roles in CXCR4 signaling in hDPSCs migration induced by SDF-1.
Additionally, our results also show that as the antagonist of CXCR4, AMD3100 significantly inhibited hDPSCs migration, which indicates a crucial role of SDF-1/CXCR4 axis in hDPSCs migration, though controversial evidence shows that blocking CXCR4 with AMD3100 could decrease tissue inflammation and increase progenitor cell migration to injury sites52. A previous study has demonstrated that the MSCs contribute to burn wound closure, which could be attenuated by the application of AMD310041. The above observation was consistent with studies in cancer cells, of which migration would be inhibited with AMD3100 treatment or CXCR4 knockdown53. Treatment with AMD3100 could also diminish the recruitment of bone marrow derived stem cells (BMDCs) after MI54.
The use of specific inhibitor of CXCR4 and CXCR4 expression silencing in hDPSCs with siRNA in this study confirmed that the effect of SDF-1 on hDPSCs migration was dependent on PI3K/Akt signaling. Previous studies have identified that PI3K is involved in multiple stem cell migration40. The same phenomenon has also been demonstrated in leukemic cell lines55 and neural precursor cells56. The increased MSC migration by SDF-1 and hypoxia were both mediated by PI3K/Akt pathway57, which could be significantly attenuated by PI3K inhibitor. Using specific chemical inhibitors to detected the role of PI3K/Akt, our data demonstrated that blockade of PI3K could remarkably suppress the migration hDPSCs, as well as the induction of SDF-1, which was consistent with the role of PI3K/Akt in T lymphocytes58 and neural stem cells59. Under both conditions with and without SDF-1, the inhibitor of PI3K significantly abrogated the expression of β-catenin and the phosphorylation of Akt and GSK3β, indicating that all of them were downstream effectors of SDF-1/CXCR4/PI3K. A previous study on cardiac stem/progenitor cells (CSPC) showed that SDF-1 affected GSK3β activity via the phosphorylation of Akt60 and the β-catenin levels in pancreatic islet cells could be stabilized by SDF-1 through inhibition of GSK3β activity61, which is consistent with our results. Although the phosphorylation of FAK was not affected by the inhibitor of PI3K without SDF-1, it was downregulated by the inhibitor under SDF-1 stimulation. Moreover, phosphorylation of FAK at Y397 could induce the activation and recruitment of PI3K62. However, the phosphorylation of PI3K was inhibited by the inhibitor of FAK under both circumstances. These controversial results suggest that FAK and PI3K may work in coordination with each other during the hDPSCs migration induced by SDF-1.
In response to extracellular signaling mediated by G protein coupled receptors or Intergrins, FAK participates in the cytoskeleton rearrangements and the cycle of focal adhesion. It has also been shown to contribute epithelial cell migration63 and play roles in adhesion by activating multiple signaling pathways. We then determined that CXCR4 interacted with FAK in response to SDF-1. Previous experiments showed that FAK could be activated by SDF-1 in hematopoietic cell lineages, as well as in breast cancer cells64. Studies in progenitor B cells demonstrated that the prolonged activation of FAK correlated with the increased responsiveness of pro-B cells to SDF-165. Our data indicates that the phosphorylation of FAK is necessary for the migration of hDPSCs and that specific inhibition of FAK by inhibitor leads to the decreased activation of the PI3K/Akt pathway. These data remind us again that FAK works at the upstream of the PI3K/Akt pathway.
Previous evidence has identified that Rho family GTPases regulate cell migration by affecting cell-cell adhesion and cytoskeleton rearrangements66. During cell migration, CDC42 controls the formation of filopodia67, which may participate in the recognition of extracellular signals68, such as chemotactic gradients. SDF-1 could also induce actin polymerization and initiate signaling pathways involved in cytoskeleton rearrangement69. SDF-1α expression in liver cancer can activate small GTPases, including CDC42, through interacting with CXCR470. Our results make it clear that CDC42 makes a difference during migration of hDPSCs induced by SDF-1. Although the PI3K/Akt pathway was not influenced by the knockdown of CDC42, both the upstream and downstream of PI3K/Akt was inhibited by siCDC42 during the migration of hDPSCs. We also noticed that the knockdown of CDC42 had little effect on the phosphorylation of FAK with SDF-1 stimulation, which may be the result of SDF-1 effect.
Conclusion
Our studies delineate the mechanisms during the migration of hDPSCs towards SDF-1. SDF-1 is an important regulator of hDPSCs migration, though it remains to be elucidated whether it is secreted by stem cells or inflammatory cells. All the results above demonstrate that SDF-1/CXCR4 axis interacts with FAK/PI3K/Akt and GSK3β/β-catenin pathways in regulating hDPSCs migration (see Fig. 8 for overview). These studies provide a framework to study the mechanism of SDF-1 on hDPSCs migration and some directions on the application of SDF-1 in dental pulp repair. Further questions about the reactions of hDPSCs after SDF-1 application in vivo and how to use SDF-1 during treatment are the subjects of future investigation.
Figure 8. Schematic illustration showing the putative signaling pathways involved in SDF-1 mediated migration of hDPSCs.
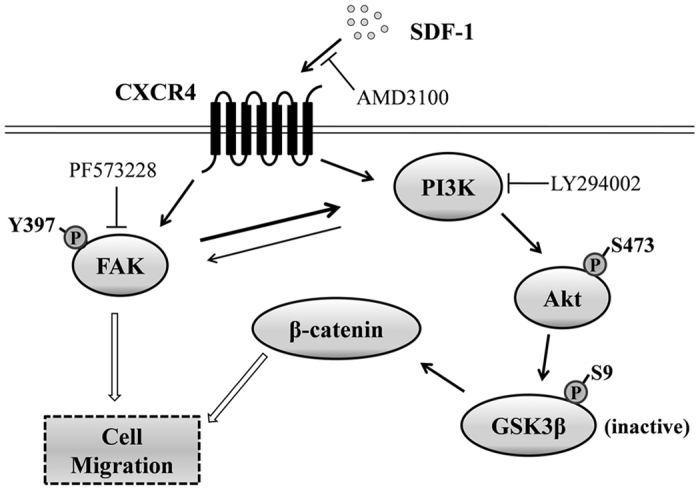
Extracellular SDF-1 induces the engagement of CXCR4, leading to the activation and coordination of FAK and PI3K. Consequently, the phosphorylation of Akt at ser473 inhibits the activation of GSK3β resulting in an increase of β-catenin expression. As a result, the SDF-1/CXCR4 axis activates FAK/PI3K/Akt and GSK3β/β-catenin pathways leading to the migration of hDPSCs.
Methods
Isolation and culture of human dental pulp stem cells
Normal human third molars without caries were obtained from patients 18 to 22 years of age for orthodontic reasons or because of impaction. The whole procedure was carried on using a protocol approved by the Institutional Review Board of the Fourth Military Medical University. We confirmed that all methods were performed in accordance with the relevant guidelines and informed consent was obtained from all subjects. Briefly, the extracted teeth were transported to the laboratory on ice within 2 hours of collection. The dental pulp were dissected out of the teeth, minced and digested with 3 mg/ml collagenase type I at 37 °C for 45 min. After washing three times with PBS, cells were suspended in the α-modification of Eagle’s Medium (α-MEM) with 15% fetal bovine serum, 100 units/ml penicillin and streptomycin, seeded at the density of 2 × 103/well in 6-well plates and cultured at 37 °C in a 5% CO2 incubator. The medium was refreshed every 2 days, and cells were passaged when reaching 80% confluence. Passages 3 to 5 were used in this study, and all experiments were performed at least three times.
Immunofluorescence staining
Human dental pulp stem cells were seeded on coverslips overnight and fixed in 4% paraformaldehyde solution in PBS for 15 min at 4 °C. After washing with PBS three times, cells were permeated with 0.1% Triton-100 for 10 min and blocked by 5% bovine serum albumin (BSA) for 30 min at room temperature. Cells were then incubated at 4 °C with diluted anti-CXCR4 antibody (Abcam, 1:100) overnight. Fluorescein isothiocyanate (FITC) labeled donkey anti-rabbit secondary antibodies were added onto cells for 1 h at 4 °C after washing. Pictures were taken with Olympus FV1000 confocal microscope and acquired using the FV10-ASW3.1 Viewer software. After seeding for 12 hours and culture in α-MEM with 10% FBS and 50 ng/ml SDF-1α (Gibco, USA) for 2 hours, primary antibodies against phospho-FAK (Y397, Abcam) and β-catenin (Cell Signaling Technology) were used as described above. Dilutions without primary antibodies served as negative control.
Western blot analysis
Human dental pulp stem cells were seeded in plates and reached 80% confluence at 37 °C in a 5% CO2 incubator. Cells were then washed with PBS and lysed in ice-cold radio-immunoprecipitation assay (RIPA) buffer with a complete protease inhibitor cocktail (Sigma). Primary antibodies against CXCR4, PI3K (p85α), phosphor-Akt (S473) and total Akt (Abcam), phospho-FAK (Y397), FAK, phospho-PI3K (p85), phospho-GSK3β (S9), GSK3β, β-catenin and β-ACTIN (Cell Signaling Technology) were purchased and used as recommended by the manufacturers. Proteins were extracted, resolved by SDS-PAGE and then transferred to PVDF (polyvinylidene difluoride) membranes. After blocking in 5% non-fat dry milk in TBST (Tris-Buffered Saline with Tween) for 2 hours and probing with the indicated primary antibodies at 4 °C overnight, the membranes were rinsed and incubated with dilutions of the appropriate secondary antibodies conjugated with horseradish peroxidase (Cell Signaling Technology) for 1 hour at room temperature and with the enhanced chemiluminescence kit (Millipore) for a few seconds. Signals were captured using ChemiDoc MP system (Bio-Rad) and Image Lab software (Bio-Rad). After treatment with SDF-1, siRNA or inhibitors for the indicated time at 37 °C in a 5% CO2 incubator, proteins were extracted and treated as described above. β-actin was used as an internal control. Quantization of the level of phosphorylated proteins was calculated by normalizing the p-form with the total amount.
RT-PCR
Total cellular RNA was isolated from cells using Trizol reagent (Takara) according to the manufacturer’s instruction. The cDNA was synthesized using PrimeScript RT reagent Kit with gDNA Eraser (Takara) according to the manufacturer’s protocols. Standard PCR reactions were performed and the products were examined by electrophoresis on 1% agarose (Biowest, French) gel. After staining with EB (ethidium bromide) dilution, pictures were taken with the ChemiDoc MP system (Bio-Rad).
siRNA Transfection
siCXCR4, siCDC42 and scrambled siRNA were designed and produced by RiboBio (Guangzhou, China). All siRNA were diluted to working concentration in RNase-free water. Human dental pulp stem cells were transfected with 50 nM siRNA using DharmaFECT Transfection Reagents (Dharmacon) according to manufacturer’s protocols. Briefly, cells were transfected with siRNA or vehicle when reaching 50–60% confluence. Total RNA was isolated after 24 hours. Total proteins were extracted and Transwell assays were performed after 48 hours.
Cell Migration Assay using Transwell System
Human dental pulp stem cells were cultured in α-MEM with 10% FBS and penicillin/streptomycin to reach 50–60% confluence. For siRNA treatment, cells were transfected with siCXCR4 or siCDC42 as described above for 48 hours. For the inhibitor treatment, cells were preincubated with AMD3100 (100 ng/ml), LY294002 (20 μM) and/or PF573228 (10 μM) (all purchased from Sigma) for 1 hour at 37 °C in a 5% CO2 incubator. After treatment with the indicated siRNA or inhibitor in each group and dissociation with 0.25% trypsin into single cell suspension, cells were seeded in the upper chamber of a 24-well Transwell of 8 μm pore size (Corning, USA) with a density of 2.5 × 104 cells/well and cultured in the same medium as that used before dissociation. Medium with SDF-1 (50 ng/ml) was added to the lower chamber. After migration at 37 °C for 12 hours, cells were washed with PBS, fixed with 4% paraformaldehyde solution in PBS for 15 min at 4 °C and stained with 0.1% crystal violet. On the upper side of the Transwell chamber, the cells were removed with a cotton applicator. On the lower side of the chamber, cells were counted in five random fields.
Statistical Analysis
Data shown in this study are expressed as the mean ± standard deviation (SD) from at least three independent experiments. Statistical analysis was performed using SPSS Statistics 20.0 software. The statistical significance of the differences between two groups was analyzed by Student’s t test at a significance level of P < 0.05.
Additional Information
How to cite this article: Li, M. et al. SDF-1/CXCR4 axis induces human dental pulp stem cell migration through FAK/PI3K/Akt and GSK3β/β-catenin pathways. Sci. Rep. 7, 40161; doi: 10.1038/srep40161 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (No. 31271048, 81670975 and 81271126).
Footnotes
Author Contributions M.L. and X.S. designed and conducted the experiments. M.L. organized and wrote the manuscript. X.S. collected and analyzed the data. L.M. and L.J. assisted in conducting the experiments and analyzed the data. W.Z. and M.X. contributed to conducting the experiments and discussing the results. Q.Y. conceived the project and approved the manuscript.
References
- Marquez-Curtis L. A. & Janowska-Wieczorek A. Enhancing the migration ability of mesenchymal stromal cells by targeting the SDF-1/CXCR4 axis. Biomed Res Int 2013, 561098 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi S. & Gronthos S. Perivascular niche of postnatal mesenchymal stem cells in human bone marrow and dental pulp. J Bone Miner Res 18, 696–704 (2003). [DOI] [PubMed] [Google Scholar]
- Smith A. J. & Lesot H. Induction and regulation of crown dentinogenesis: embryonic events as a template for dental tissue repair? Crit Rev Oral Biol Med 12, 425–37 (2001). [DOI] [PubMed] [Google Scholar]
- Mills S. C. et al. Cell migration towards CXCL12 in leukemic cells compared to breast cancer cells. Cell Signal 28, 316–24 (2016). [DOI] [PubMed] [Google Scholar]
- Luster A. D. Chemokines–chemotactic cytokines that mediate inflammation. N Engl J Med 338, 436–45 (1998). [DOI] [PubMed] [Google Scholar]
- Yi T. et al. Quantitative phosphoproteomic analysis reveals system-wide signaling pathways downstream of SDF-1/CXCR4 in breast cancer stem cells. Proc Natl Acad Sci USA 111, E2182–90 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns J. M. et al. A novel chemokine receptor for SDF-1 and I-TAC involved in cell survival, cell adhesion, and tumor development. J Exp Med 203, 2201–13 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabel B. A. et al. Elucidation of CXCR7-mediated signaling events and inhibition of CXCR4-mediated tumor cell transendothelial migration by CXCR7 ligands. J Immunol 183, 3204–11 (2009). [DOI] [PubMed] [Google Scholar]
- Liu H. et al. The role of SDF-1-CXCR4/CXCR7 axis in the therapeutic effects of hypoxia-preconditioned mesenchymal stem cells for renal ischemia/reperfusion injury. PLoS One 7, e34608 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen T. et al. Stromal cell-derived factor-1/CXCR4 signaling modifies the capillary-like organization of human embryonic stem cell-derived endothelium in vitro. Stem Cells 25, 392–401 (2007). [DOI] [PubMed] [Google Scholar]
- Patrussi L. et al. Negative regulation of chemokine receptor signaling and B-cell chemotaxis by p66Shc. Cell Death Dis 5, e1068 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy I. et al. CXCL12 chemokine expression suppresses human pancreatic cancer growth and metastasis. PLoS One 9, e90400 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips R. J. et al. The stromal derived factor-1/CXCL12-CXC chemokine receptor 4 biological axis in non-small cell lung cancer metastases. Am J Respir Crit Care Med 167, 1676–86 (2003). [DOI] [PubMed] [Google Scholar]
- Su L. et al. Differential expression of CXCR4 is associated with the metastatic potential of human non-small cell lung cancer cells. Clin Cancer Res 11, 8273–80 (2005). [DOI] [PubMed] [Google Scholar]
- Ghadge S. K., Muhlstedt S., Ozcelik C. & Bader M. SDF-1alpha as a therapeutic stem cell homing factor in myocardial infarction. Pharmacol Ther 129, 97–108 (2011). [DOI] [PubMed] [Google Scholar]
- Jiang L. et al. The expression and role of stromal cell-derived factor-1alpha-CXCR4 axis in human dental pulp. J Endod 34, 939–44 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J., Crawford R., Chen C. & Xiao Y. The key regulatory roles of the PI3K/Akt signaling pathway in the functionalities of mesenchymal stem cells and applications in tissue regeneration. Tissue Eng Part B Rev 19, 516–28 (2013). [DOI] [PubMed] [Google Scholar]
- Kim Y. S. et al. Direct GSK-3beta inhibition enhances mesenchymal stromal cell migration by increasing expression of beta-PIX and CXCR4. Mol Neurobiol 47, 811–20 (2013). [DOI] [PubMed] [Google Scholar]
- Haegel H. et al. Lack of beta-catenin affects mouse development at gastrulation. Development 121, 3529–37 (1995). [DOI] [PubMed] [Google Scholar]
- Cheon S. S. et al. beta-Catenin stabilization dysregulates mesenchymal cell proliferation, motility, and invasiveness and causes aggressive fibromatosis and hyperplastic cutaneous wounds. Proc Natl Acad Sci USA 99, 6973–8 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilles C. et al. Transactivation of vimentin by beta-catenin in human breast cancer cells. Cancer Res 63, 2658–64 (2003). [PubMed] [Google Scholar]
- Kim M. H., Lee Y. J., Kim M. O., Kim J. S. & Han H. J. Effect of leukotriene D4 on mouse embryonic stem cell migration and proliferation: involvement of PI3K/Akt as well as GSK-3beta/beta-catenin signaling pathways. J Cell Biochem 111, 686–98 (2010). [DOI] [PubMed] [Google Scholar]
- Wang F. et al. Lipid products of PI(3)Ks maintain persistent cell polarity and directed motility in neutrophils. Nat Cell Biol 4, 513–8 (2002). [DOI] [PubMed] [Google Scholar]
- Hall A. Rho GTPases and the actin cytoskeleton. Science 279, 509–14 (1998). [DOI] [PubMed] [Google Scholar]
- Ridley A. J., Paterson H. F., Johnston C. L., Diekmann D. & Hall A. The small GTP-binding protein rac regulates growth factor-induced membrane ruffling. Cell 70, 401–10 (1992). [DOI] [PubMed] [Google Scholar]
- Mattila P. K. & Lappalainen P. Filopodia: molecular architecture and cellular functions. Nat Rev Mol Cell Biol 9, 446–54 (2008). [DOI] [PubMed] [Google Scholar]
- Melendez J., Grogg M. & Zheng Y. Signaling role of Cdc42 in regulating mammalian physiology. J Biol Chem 286, 2375–81 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porta C., Paglino C. & Mosca A. Targeting PI3K/Akt/mTOR Signaling in Cancer. Front Oncol 4, 64 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domanska U. M. et al. A review on CXCR4/CXCL12 axis in oncology: no place to hide. Eur J Cancer 49, 219–30 (2013). [DOI] [PubMed] [Google Scholar]
- Nader G. P., Ezratty E. J. & Gundersen G. G. FAK, talin and PIPKIgamma regulate endocytosed integrin activation to polarize focal adhesion assembly. Nat Cell Biol 18, 491–503 (2016). [DOI] [PubMed] [Google Scholar]
- Baer P. C. & Geiger H. Mesenchymal stem cell interactions with growth factors on kidney repair. Curr Opin Nephrol Hypertens 19, 1–6 (2010). [DOI] [PubMed] [Google Scholar]
- Bonecchi R. et al. Chemokines and chemokine receptors: an overview. Front Biosci (Landmark Ed) 14, 540–51 (2009). [DOI] [PubMed] [Google Scholar]
- Yamaguchi J. et al. Stromal cell-derived factor-1 effects on ex vivo expanded endothelial progenitor cell recruitment for ischemic neovascularization. Circulation 107, 1322–8 (2003). [DOI] [PubMed] [Google Scholar]
- Crump M. P. et al. Solution structure and basis for functional activity of stromal cell-derived factor-1; dissociation of CXCR4 activation from binding and inhibition of HIV-1. EMBO J 16, 6996–7007 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeger F. H., Zeiher A. M. & Dimmeler S. Cell-enhancement strategies for the treatment of ischemic heart disease. Nat Clin Pract Cardiovasc Med 4 Suppl 1, S110–3 (2007). [DOI] [PubMed] [Google Scholar]
- Tran P. B., Banisadr G., Ren D., Chenn A. & Miller R. J. Chemokine receptor expression by neural progenitor cells in neurogenic regions of mouse brain. J Comp Neurol 500, 1007–33 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulbe H., Hagemann T., Szlosarek P. W., Balkwill F. R. & Wilson J. L. The inflammatory cytokine tumor necrosis factor-alpha regulates chemokine receptor expression on ovarian cancer cells. Cancer Res 65, 10355–62 (2005). [DOI] [PubMed] [Google Scholar]
- Jiang H. W., Ling J. Q. & Gong Q. M. The expression of stromal cell-derived factor 1 (SDF-1) in inflamed human dental pulp. J Endod 34, 1351–4 (2008). [DOI] [PubMed] [Google Scholar]
- Gupta S. K., Lysko P. G., Pillarisetti K., Ohlstein E. & Stadel J. M. Chemokine receptors in human endothelial cells. Functional expression of CXCR4 and its transcriptional regulation by inflammatory cytokines. J Biol Chem 273, 4282–7 (1998). [DOI] [PubMed] [Google Scholar]
- Yu J. et al. SDF-1/CXCR4-mediated migration of transplanted bone marrow stromal cells toward areas of heart myocardial infarction through activation of PI3K/Akt. J Cardiovasc Pharmacol 55, 496–505 (2010). [DOI] [PubMed] [Google Scholar]
- Hu C. et al. CXCL12/CXCR4 axis promotes mesenchymal stem cell mobilization to burn wounds and contributes to wound repair. J Surg Res 183, 427–34 (2013). [DOI] [PubMed] [Google Scholar]
- Liu N., Tian J., Cheng J. & Zhang J. Migration of CXCR4 gene-modified bone marrow-derived mesenchymal stem cells to the acute injured kidney. J Cell Biochem 114, 2677–89 (2013). [DOI] [PubMed] [Google Scholar]
- Penn M. S., Pastore J., Miller T. & Aras R. SDF-1 in myocardial repair. Gene Ther 19, 583–7 (2012). [DOI] [PubMed] [Google Scholar]
- Kitaori T. et al. Stromal cell-derived factor 1/CXCR4 signaling is critical for the recruitment of mesenchymal stem cells to the fracture site during skeletal repair in a mouse model. Arthritis Rheum 60, 813–23 (2009). [DOI] [PubMed] [Google Scholar]
- Glass T. J. et al. Stromal cell-derived factor-1 and hematopoietic cell homing in an adult zebrafish model of hematopoietic cell transplantation. Blood 118, 766–74 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son B. R. et al. Migration of bone marrow and cord blood mesenchymal stem cells in vitro is regulated by stromal-derived factor-1-CXCR4 and hepatocyte growth factor-c-met axes and involves matrix metalloproteinases. Stem Cells 24, 1254–64 (2006). [DOI] [PubMed] [Google Scholar]
- Zheng H., Fu G., Dai T. & Huang H. Migration of endothelial progenitor cells mediated by stromal cell-derived factor-1alpha/CXCR4 via PI3K/Akt/eNOS signal transduction pathway. J Cardiovasc Pharmacol 50, 274–80 (2007). [DOI] [PubMed] [Google Scholar]
- Cho B. S. et al. Antileukemia activity of the novel peptidic CXCR4 antagonist LY2510924 as monotherapy and in combination with chemotherapy. Blood 126, 222–32 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong M. M. et al. Sirolimus stimulates vascular stem/progenitor cell migration and differentiation into smooth muscle cells via epidermal growth factor receptor/extracellular signal-regulated kinase/beta-catenin signaling pathway. Arterioscler Thromb Vasc Biol 33, 2397–406 (2013). [DOI] [PubMed] [Google Scholar]
- Taichman R. S. et al. Use of the stromal cell-derived factor-1/CXCR4 pathway in prostate cancer metastasis to bone. Cancer Res 62, 1832–7 (2002). [PubMed] [Google Scholar]
- Mo W. et al. CXCR4/CXCL12 mediate autocrine cell- cycle progression in NF1-associated malignant peripheral nerve sheath tumors. Cell 152, 1077–90 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jujo K. et al. CXCR4 blockade augments bone marrow progenitor cell recruitment to the neovasculature and reduces mortality after myocardial infarction. Proc Natl Acad Sci USA 107, 11008–13 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu Q. et al. Hypoxia-inducible factor 1alpha (HIF-1alpha) and reactive oxygen species (ROS) mediates radiation-induced invasiveness through the SDF-1alpha/CXCR4 pathway in non-small cell lung carcinoma cells. Oncotarget 6, 10893–907 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbott J. D. et al. Stromal cell-derived factor-1alpha plays a critical role in stem cell recruitment to the heart after myocardial infarction but is not sufficient to induce homing in the absence of injury. Circulation 110, 3300–5 (2004). [DOI] [PubMed] [Google Scholar]
- Ganju R. K. et al. The alpha-chemokine, stromal cell-derived factor-1alpha, binds to the transmembrane G-protein-coupled CXCR-4 receptor and activates multiple signal transduction pathways. J Biol Chem 273, 23169–75 (1998). [DOI] [PubMed] [Google Scholar]
- Chen Y., Wei Y., Liu J. & Zhang H. Chemotactic responses of neural stem cells to SDF-1alpha correlate closely with their differentiation status. J Mol Neurosci 54, 219–33 (2014). [DOI] [PubMed] [Google Scholar]
- Liu X. et al. SDF-1/CXCR4 axis modulates bone marrow mesenchymal stem cell apoptosis, migration and cytokine secretion. Protein Cell 2, 845–54 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjorthaug H. S. & Aasheim H. C. Ephrin-A1 stimulates migration of CD8+CCR7+ T lymphocytes. Eur J Immunol 37, 2326–36 (2007). [DOI] [PubMed] [Google Scholar]
- Cui C. et al. Stichopus japonicus Polysaccharide, Fucoidan, or Heparin Enhanced the SDF-1alpha/CXCR4 Axis and Promoted NSC Migration via Activation of the PI3K/Akt/FOXO3a Signaling Pathway. Cell Mol Neurobiol (2016). [DOI] [PubMed] [Google Scholar]
- Dimova N., Wysoczynski M. & Rokosh G. Stromal cell derived factor-1alpha promotes C-Kit+ cardiac stem/progenitor cell quiescence through casein kinase 1alpha and GSK3beta. Stem Cells 32, 487–99 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer L. et al. GSK-3-selective inhibitors derived from Tyrian purple indirubins. Chem Biol 10, 1255–66 (2003). [DOI] [PubMed] [Google Scholar]
- Hauck C. R. et al. Inhibition of focal adhesion kinase expression or activity disrupts epidermal growth factor-stimulated signaling promoting the migration of invasive human carcinoma cells. Cancer Res 61, 7079–90 (2001). [PubMed] [Google Scholar]
- Owen C. R., Yuan L. & Basson M. D. Smad3 knockout mice exhibit impaired intestinal mucosal healing. Lab Invest 88, 1101–9 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandis A. Z., Prasad A., Band H., Klosel R. & Ganju R. K. Regulation of CXCR4-mediated chemotaxis and chemoinvasion of breast cancer cells. Oncogene 23, 157–67 (2004). [DOI] [PubMed] [Google Scholar]
- Honczarenko M. et al. SDF-1 responsiveness does not correlate with CXCR4 expression levels of developing human bone marrow B cells. Blood 94, 2990–8 (1999). [PubMed] [Google Scholar]
- Clark E. A., Golub T. R., Lander E. S. & Hynes R. O. Genomic analysis of metastasis reveals an essential role for RhoC. Nature 406, 532–5 (2000). [DOI] [PubMed] [Google Scholar]
- Ridley A. J. Rho GTPases and cell migration. J Cell Sci 114, 2713–22 (2001). [DOI] [PubMed] [Google Scholar]
- O’Connor T. P., Duerr J. S. & Bentley D. Pioneer growth cone steering decisions mediated by single filopodial contacts in situ. J Neurosci 10, 3935–46 (1990). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voermans C., Anthony E. C., Mul E., van der Schoot E. & Hordijk P. SDF-1-induced actin polymerization and migration in human hematopoietic progenitor cells. Exp Hematol 29, 1456–64 (2001). [DOI] [PubMed] [Google Scholar]
- Yagi H. et al. A synthetic biology approach reveals a CXCR4-G13-Rho signaling axis driving transendothelial migration of metastatic breast cancer cells. Sci Signal 4, ra60 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]