Abstract
Antiviral therapy is a first line of defence against new influenza strains. Current pandemic preparations involve stock- piling oseltamivir, an oral neuraminidase inhibitor (NAI), so rapidly determining the effectiveness of NAIs against new viral strains is vital for deciding how to use the stockpile. Previous studies have shown that it is possible to extract the drug efficacy of antivirals from the viral decay rate of chronic infections. In the present work, we use a nonlinear mathematical model representing the course of an influenza infection to explore the possibility of extracting NAI drug efficacy using only the observed viral titer decay rates seen in patients. We first show that the effect of a time-varying antiviral concentration can be accurately approximated by a constant efficacy. We derive a relationship relating the true treatment dose and time elapsed between doses to the constant drug dose required to approximate the time- varying dose. Unfortunately, even with the simplification of a constant drug efficacy, we show that the viral decay rate depends not just on drug efficacy, but also on several viral infection parameters, such as infection and production rate, so that it is not possible to extract drug efficacy from viral decay rate alone.
Influenza is a viral infection of the upper respiratory tract that, even in it’s mild seasonal form, causes serious illness and death worldwide1. The rapid mutation rate of influenza virus2 along with occasional re-assortment events3 results in the emergence of new antigenic variants of influenza. The most popular antivirals currently used against influenza are neuraminidase inhibitors (NAIs). NAIs block the action of neuraminidase, an enzyme found on the surface of the influenza virus which is responsible for viral release from an infected cell4,5 causing virus to remain bound to the cell surface6. NAIs, particularly oseltamivir, are the antiviral of choice for pandemic stockpiles7 because resistance to NAIs remains low in circulating strains8,9 and they are effective against pH1N110, as well as avian influenza (H5N1)11,12. Given our reliance on NAIs and the rapid mutation of influenza into new strains, there is a need to develop methods to rapidly quantify the efficacy of NAIs against new strains of influenza.
There are a variety of techniques used to measure the susceptibilty of a viral strain to NAIs in vitro. Perhaps the most direct measure of susceptibility is through a neuraminidase inhibition assay which measures the drug’s effectiveness at inhibiting the neuraminidase activity of a particular viral strain13,14,15,16. The inhibition assay, unfortunately, is not equivalent to measuring the drug’s effectiveness at inhibiting viral release during an infection. During an infection virus can be released from the cell without the presence of neuraminidase17,18,19, so we might expect the efficacy of NAIs at blocking an infection to be lower than the efficacy measured in an inhibition assay. To account for this, the efficacy of NAIs is sometimes measured through a reduction in viral yield20, cytopathic effect21,22, or plaque formation20,23. Knowledge of the within host antiviral efficacy will help in estimating the effect of NAI treatment at the population level, through the use of multiscale models24,25,26, allowing public health officials to manage their stockpiles more effectively.
Influenza infections in humans add further complications. Variability in the metabolism and pharmacokinetics (PK) of drugs between individuals27 means that a given dose will have different efficacies in different patients. Thus there is a need to develop methods for determining the effectiveness of NAIs within a human host. Unfortunately, influenza infections are acute and peak quickly around 2 days post-infection. Therefore, characterizing the kinetics of viral titer growth prior to peak is difficult and sometimes impossible as it requires frequent samples within the first 48 of infection, often before patients actually experience symptoms. It is somewhat easier to collect information about the viral titer decay phase which occurs either after the viral titer has peaked or after highly effective treatment sufficient to abrogate the infection is applied. Indeed, several studies have relied on viral measurements starting near or after the viral titer peak to assess the efficacy of NAIs in patients28,29,30,31,32.
Chronic infections such as those caused by HIV or hepatitis B and C are amenable to extraction of antiviral efficacy from the chronic and relatively constant viral concentration and its ensuing decay following treatment33,34,35. This is because the chronic phase corresponds to a steady state in the viral kinetics (VK) model and the viral titer decay caused by the disruption of that steady state due to antiviral therapy reduces to a function which depends only on the antiviral efficacy and viral clearance rate. Unfortunately, this does not hold in the acute phase of infection because in that phase, infection decay due to antiviral efficacy is dampened by the continued infection growth which characterizes this phase. Yet, perhaps some assumptions could be made here too which would allow us to extract this information from the viral titer decays or perhaps allow us to eliminate some VK parameters from consideration.
Further compounding the problem is the periodic nature of drug treatment. Oseltamivir, the most commonly used NAI, is taken as a pill twice a day which causes fluctuations in the concentration of oseltamivir in the body27,36. Many VK models simply ignore these fluctuations and assume a constant drug concentration when drug is applied26,37. The short duration of a seasonal influenza infection means that the fluctuations in drug concentration are on a similar time scale as the infection itself, so it is not clear if the assumption of a constant drug concentration is valid.
In this paper, we use a mathematical model of the within host dynamics of influenza to examine the possibility of extracting drug efficacy from the viral titer decay rate. We first show that viral titers produced with a time-dependent drug concentration can be reproduced with the assumption of a constant drug concentration and that the constant drug assumption results in viral titers with the same viral decay rate as the viral titers produced with a time-dependent drug concentration. We then assess whether constant drug efficacy can be extracted from viral titer decay rate by performing a sensitivity analysis. We find, unfortunately, that the viral decay rate depends on many of the model parameters and we cannot extract drug efficacy without additional data to determine other infection parameters.
Results
Fitting treated viral titers
Determining a time-dependent treatment efficacy is difficult particularly given the sparsity of experimental viral titer data. To simplify the problem, we would like to be able to assume that drug efficacy is constant over the course of the infection, but because influenza infections are of short duration (typically 2–4 symptomatic days), oscillations in drug concentration are approximately on the same time scale as the infection. This is not the case for HIV and HCV where this type of analysis has proved useful33,34,35 — these infections last months or even years, so the small oscillations in drug concentration over a few hours are not significant and assuming a constant drug treatment efficacy is reasonable. This might not be the case for a rapidly changing infection such as influenza, so we must first determine whether we can reproduce the viral titer produced by a time-dependent drug treatment with the assumption of a constant drug treatment.
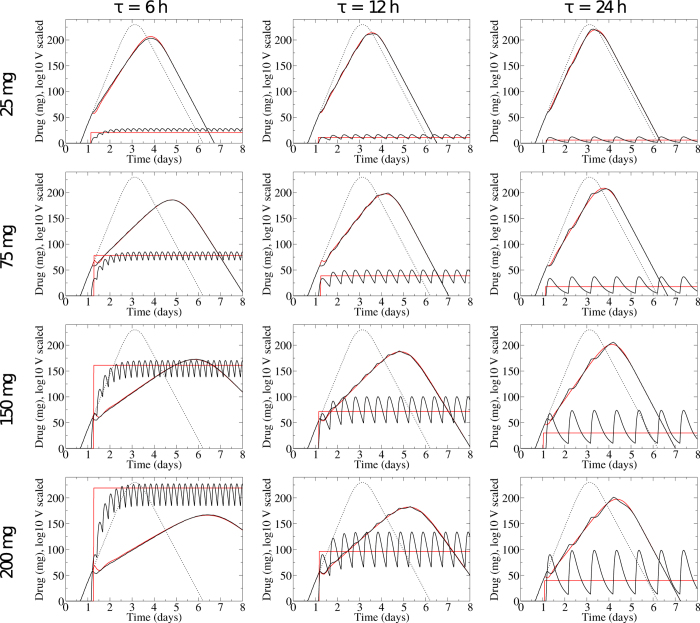
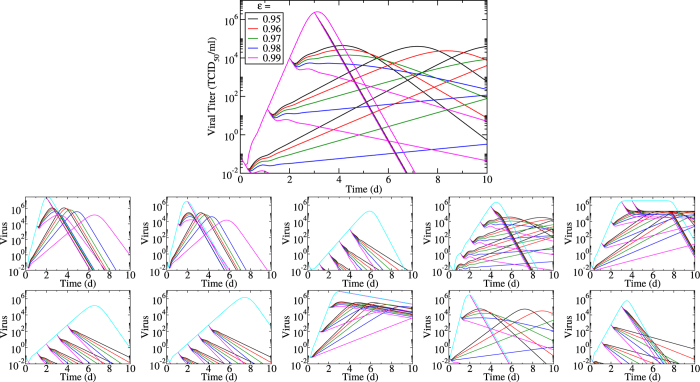
We generate viral titers using time-varying PK/PD models, Eq. (4), with treatment initiated at 28 h. We chose 28 h post-infection, the typical treatment administration time used in human drug trials38,39, as it is thought to be a few hours after the onset of symptoms and represents a typical time when patients might seek treatment. We then fit the viral titers assuming a constant value for the drug. We leave the constant drug value, Dcst, and the time of administration of the constant drug, ton, as free parameters. We explore a range of treatment regimens by varying the period of dosage, τ, from 0 (theoretical continuous infusion) to 48 h (every two days), and varying the true intake dose, Dadmin, from 0 to 200 mg. The typical treatment regimen for oseltamivir is 75 mg twice a day (τ = 12 h). Figure 1 shows the viral titers generated with a time-dependent drug concentration and our fits using the assumption of a constant drug concentration.
Figure 1. Comparing the effect of a constant vs time-varying antiviral concentration.
Viral titers and drug concentrations for infections treated with a time-varying drug concentration, D(t) from Eq. 4 (black lines), and the best fit assuming a constant drug concentration (red lines). The dashed line shows the untreated infection.
The viral titer curves obtained by assuming a constant antiviral concentration provide a good approximation of those obtained with the full PK/PD model. There is some discrepancy at high drug doses and large dosage periods (large Dadmin and τ) where the oscillations in drug concentration create oscillations in the viral titer. The assumption of a constant drug cannot reproduce these oscillations, so the fits in this range are not as good. Even during these oscillations, however, our fits are within the typical error of viral titer measurements40. It is also important to note that viral titers in human trials are typically sampled daily or bi-daily and so these oscillations likely would not be noticed in clinical trial data. There is also some discrepancy near the application time of the drug. In order to match the effect of the drug over the remainder of the viral titer curve, the constant drug needs to be applied at a slightly different time than the time-dependent drug. This leads to a small, experimentally indiscernible difference in the viral titer near the administration time.
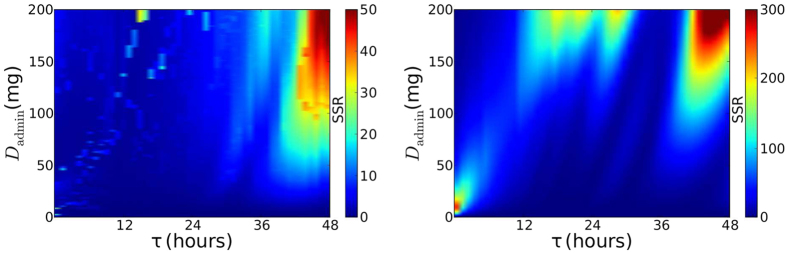
Figure 2 illustrates the goodness of our fits by examining the sum of square residuals (SSR) over the full range of dose concentrations and periods (Dadmin and τ). The absolute value for SSR is dependent on the number of data points used in the fit (which was kept constant for all fits) and so the value itself is meaningless, but we can use it as relative measure to determine where we have achieved better fits. Again, the region of high doses and large periods (large Dadmin and τ) has larger SSR as oscillations in drug concentration manifest themselves in the viral titer and our constant drug assumption begins to break down. This region does not include the two most common treatment regimens for oseltamivir: 75 mg dose once daily (τ = 24 h) for prophylactic therapy or 75 mg twice daily (τ = 12 h) for treatment41.
Figure 2. Evaluating the accuracy of assuming a constant drug concentration.
The goodness-of-fit (SSR) between viral titers resulting from PK modelling of the time-varying drug concentration and a fit of these titers using a constant drug concentration, Dcst, administered at fixed time, ton, when (Left) Dcst and ton are fitted; or (Right) ton = tadmin and Dcst is computed using Eq. (1).
Mapping pharmacokinetic parameters to constant parameters
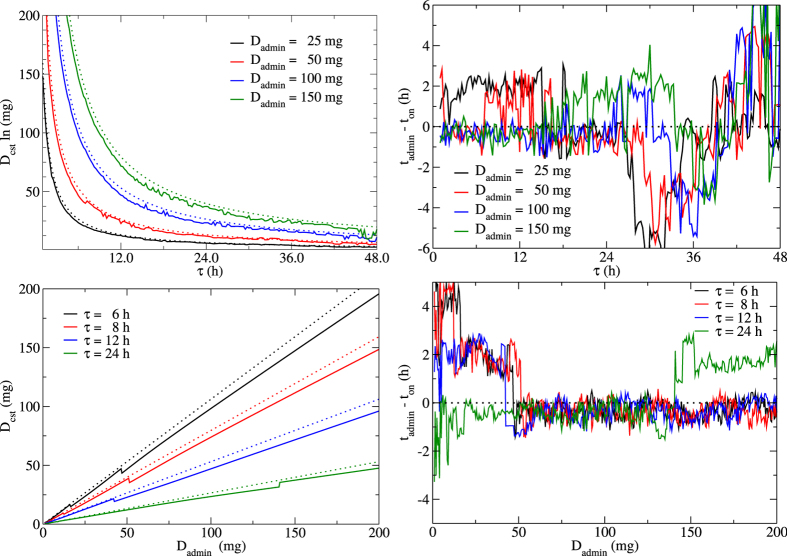
We determined that assuming a constant drug concentration can provide a good approximation to the full PK model. We must now identify relationships to map the PK parameters (Dadmin and τ) to the constant drug parameters (Dcst and ton). Figure 3 shows the relationships between the fitted constant parameters (Dcst and ton) and the PK parameters (τ and Dadmin). While there are slight deviations, the constant drug concentration, Dcst, appears to be approximately inversely proportional to the dosage period, τ, and linearly proportional to the real dose, Dadmin. An expression relating Dcst to the PK parameters can be derived by using an approximation of the full PK equation. A constant drug can be considered equivalent to a dosage period of τ = 0, i.e. no time elapsed between doses as though the drug was continuously applied. Using a Taylor expansion of Eq. (4) about τ = 0, we find an approximate expression for Dcst,
Figure 3. Relationship between parameters of the PK model and those of the constant drug concentration approximation.
Relationships between Dcst and τ (upper left), ton and τ (upper right), Dcst and Dadmin (bottom left), and ton and Dadmin (bottom right). Solid lines indicate actual values determined from fitting; dotted lines indicate our approximations using the constant drug concentration predicted by Eq. 1 and a constant value for ton.
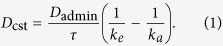 |
This equation confirms the relationships seen in Fig. 3 (left column) for Dcst, where the dotted lines give the values of Dcst predicted by Eq. 1. The approximation works best when τ and Dadmin are small but still provides a good estimate (within ~10 mg) of Dcst at high values of both τ and Dadmin.
In contrast, Fig. 3 (right column) reveals no clear relationship emerging between ton and either Dadmin or τ, showing small (typically less than 2 h), stochastic variations of ton about the true drug administration time, tadmin. The level of stochasticity in the fitted values of ton are likely an indication that the infection kinetics are not particularly sensitive to ton, with several nearby values providing equally good fits, leaving the fitting algorithm to settle on somewhat random neighbouring values. We opted for the simplest assumption, ton = tadmin, since ton appears to fluctuate about this value as Dadmin and τ are varied.
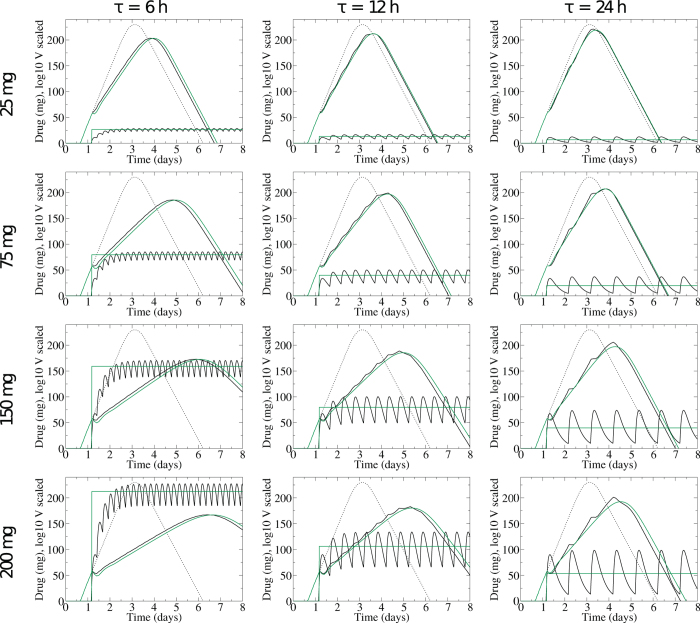
We now have approximations that allow us to map Dadmin and τ to Dcst and ton. Figure 4 shows the viral titers and drug concentrations generated by assuming a constant drug concentration determined by Eq. 1 administered at ton = tadmin (green line). The constant drug approximation produces viral titers very close to the viral titers generated with the full PK drug model (black lines). The approximations work well when τ and Dadmin are small although there is a slight shift in the time at which the viral titer peaks due to the assumption of a constant ton for all Dadmin and τ.
Figure 4. Viral titers and drug concentrations for infections treated with time-varying drug D(t) from Eq. 4 (black lines), and the viral titers and drug concentrations for infections treated with a constant drug concentration approximation from Eq. 1 and ton = tadmin.
The dashed line shows the untreated infection.
We calculated the SSR for the viral titers generated with our approximations (Fig. 2, right). For large τ, we still have the problem of oscillations in the PK viral titer that cannot be replicated by a constant drug concentration. The approximation has an additional problem when Dadmin is large and the drug concentration takes a long time to reach steady state. In this case, the assumption that ton = tadmin fails as Dcst should be applied after Dadmin to account for this prolonged ramp up time. These discrepancies, however, would not be experimentally distinguishable from the PK viral titers due to the inherent error of viral measurement40.
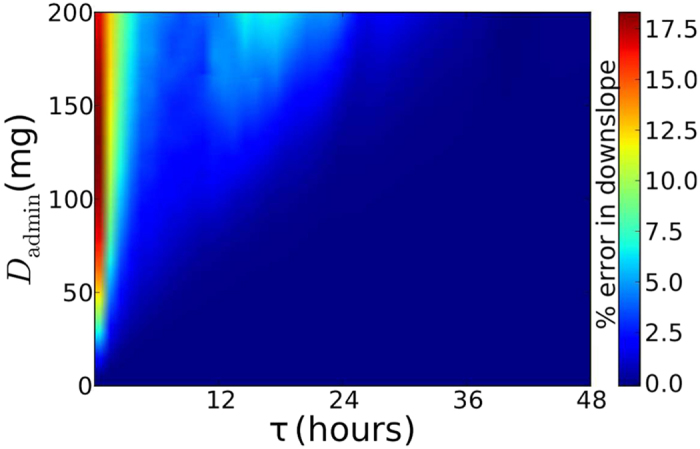
While the approximations do not always correctly reproduce every point on the time course, they do appear to accurately reproduce the general shape of the infection. In particular, we are interested in accurately reproducing the slope of the decay phase. Figure 5 shows the percent error in the decay rate. We see that the error is very small over a wide range of doses and dose timings, although there is a small region of more significant error for τ < 6 h. In this region, the constant drug assumption leads to a downslope estimate that is smaller than the actual slope so that analysis performed with the constant drug assumption would underestimate the actual efficacy of the drug. It is also unlikely that patients would take pills more often than four times per day, so available clinical trial data will likely be in the region of dose and dose timing where a constant drug assumption leads to a very good estimate of the actual viral decay rate.
Figure 5. Percent error in decay rate when using a constant drug concentration determined by Eq. (1) and applied at a fixed ton = tadmin to approximate viral titers produced with a time-dependent drug concentration.
Determining drug efficacy from viral decay
We have now shown that we can reproduce viral titers produced with time-dependent drug treatment under the assumption of a constant drug concentration. More importantly, we have shown that the assumption of a constant drug concentration accurately estimates the slope of the decay phase of viral titer over a range of doses and dose timings. Thus, we can assume a constant drug concentration when attempting to determine the drug efficacy of NAIs. We can now investigate the effect of treatment with oseltamivir on viral titer decay. In our viral kinetics model, we incorporate the effect of treatment with oseltamivir as reducing the production rate of virus by infectious cells such that p → (1 − ε)p with ε ∈ [0,1] representing the antiviral efficacy. In the model, ε is initially set to zero and is instantaneously set to the desired efficacy at the time of treatment initiation and maintained constant from that time on.
When assessing data from clinical trials, many factors and parameters are unknown. For example, an infection with a given influenza strain within a given patient will be characterized by a set of viral kinetic parameters (e.g., virus production and clearance rate, virus infectivity) which will differ across influenza strains and from patient-to-patient42,43. Additionally, in the case of recruitment studies, the time at which patients became infected is not known and cannot be determined accurately. It is important, therefore, to evaluate to what extent these unknowns can affect the observed viral titer decay rates from which we hope to determine the efficacy of the antiviral treatment received.
If we can assume that viral load is proportional to infectious cells (V = kI), then the equation for virus can be solved directly to yield
 |
While k remains unknown and likely depends on other viral kinetic parameters, c could potentially be estimated from mock infection experiments43,44, so at least a relative efficacy could be determined from the slope of viral decay. This means we need to determine when the assumption of viral load and infectious cell proportionality holds. While virus is proportional to the number of infectious cells for some parts of the infection, this is not a good approximation for other parts of the cycle, as shown in Fig. 6. In the early stages of infection, there are not yet any infectious cells, so the ratio V/I is infinite. V/I decreases rapidly as the number of infectious cells increases, but it doesn’t reach a constant until about 12 hours into the infection. This constant phase lasts until about 3 days post-infection at which point the number of infectious cells starts to decrease again (infectious cells die off faster than virus is cleared), causing V/I to rise again. In the case of influenza A virus infections in vitro, it is known that the decay rate of virus is not proportional to that of infectious or infected cells. That is because the infectious cell lifespan is normally rather than exponentially distributed whereas the lifespan of infectious virus is exponentially distributed45. Note that the duration of the roughly 2.5 day period when V/I is constant will depend on the values of β, p, c, τE, and τI, so that in practice, we cannot be entirely sure of the time period when this analysis is applicable. In the case of challenge studies, when time of infection is well-known, it might then be possible to extract efficacy from viral decay, if we are certain that drug treatment is initiated during the phase when V/I is constant. Note that we cannot use this simplifying assumption for treatment initiated early in the infection when V/I varies rapidly.
Figure 6. Ratio of viral titer to infectious cells.
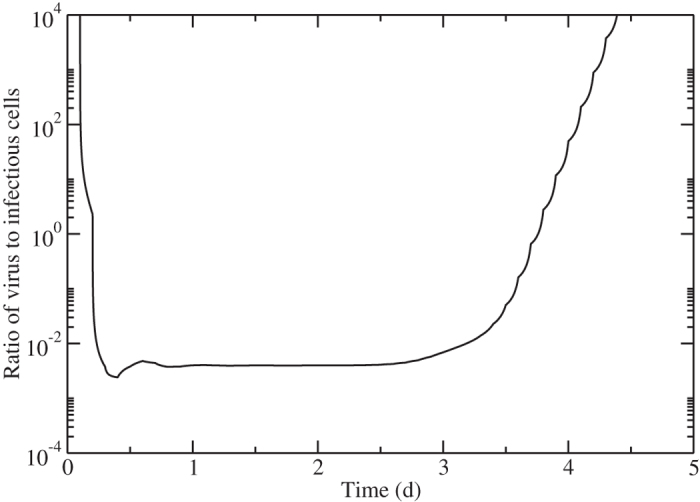
The ratio of viral titer to infectious cells over the course of an influenza infection.
For patients whose time of infection is not known, however, the situation is not so clear-cut. Even supposing that we are certain of when the period of constant V/I starts and ends, we cannot tell whether we are applying the drug during this time period. Patients typically start to experience symptoms about 1–2 days post-infection46,47. By the time they get to a doctor and fill a prescription, we can expect them to actually start treatment about 2–3 days post-infection, possibly during the time when V/I is rising again.
To investigate how limiting this assumption might be, we examined the viral titer time courses obtained under a variety of antiviral efficacies applied at various times post infection (Fig. 7). We also explore the effect of varying viral infection parameters by varying each parameter by a factor of 10 above and below (with the exception of τE which is varied by a factor of two above its base value to prevent unrealistic viral titers) its base value. Note that we have performed the same analysis using a simpler model of influenza infection and found similar results (supplementary material).
Figure 7. Effect of infection parameters on viral titer decay.
Oseltamivir treatment is applied at various times post infection and at different efficacies. Top graph shows the effect of different treatments on the base viral infection parameters. The effect of varying the base infection parameters is also explored by either decreasing (bottom row) or increasing (upper row) viral production rate (p) (first column), infection rate (β) (second column), viral clearance rate (c) (third column), eclipse duration (τE) (fourth column), infectious lifespan (τI) (last column) by 10-fold (except τE, see text) compared to the base parameters.
We see that viral titer decay is steepest when treatment is applied near viral titer peak. This is because prior to viral peak, viral titer decay due to the suppression of the infection by the antiviral is partly countered by a weakened but persistent infection progression. In contrast, after viral titer peak, viral titer decay occurs irrespective of antiviral treatment. In that phase, decay due to treatment is more pronounced than in the period prior to viral titer peak because at that point all susceptible cells have been consumed and treatment only suppresses viral production in already infected cells which are continuously being lost. In some cases, viral infection parameters are such that even in the presence of treatment, viral titer growth is only subdued and does not immediately result in viral titer decay, but instead results in viral titer growth for a time. Figures showing the effect of antiviral treatment on infectious and eclipse cells are included as supplementary material.
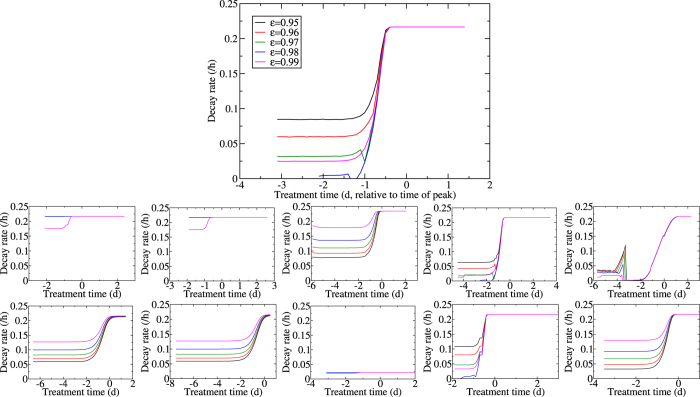
Since time of viral titer peak seems to play an important role in viral titer decay rates, we also explored how the latter varies as a function of the treatment time relative to the time of viral titer peak. In Fig. 8, we show the viral titer decay rate, determined by performing a linear regression of ln(V) versus time, for each treatment intervention applied at various time relative to viral titer peak. Viral titer decay is steeper when treatment is applied after viral titer peak than prior to it. There is a stronger dependence of viral titer decay on drug efficacy when treatment is started well before the peak. When treatment is applied near the peak this difference becomes smaller and the rate of viral titer decay becomes mostly independent of drug efficacy. In fact, closer examination of the asymptotic value of the viral decay rate after viral titer peak reveals it is equal to the viral clearance rate used in our model, namely 0.22 h−1. The viral decay rate after viral titer peak is due solely to the clearance of the virions and not to neuraminidase inhibitor treatment whose inhibition of viral production has become ineffective since most cells have already died. This means that antiviral efficacy cannot be determined from viral decay rates for treatment initiated near or after the peak of the infection. Unfortunately, even if we are confident that treatment was initiated before the viral titer peak, our investigation reveals that the rate of viral titer decay is dependent on all infection parameters. Thus, a higher viral decay rate in one patient could be attributed to either a higher antiviral efficacy in that patient or a lower value in one or more of the viral growth parameters in that patient possibly due to a more effective immune response, or both; these three possibilities are indistinguishable from inspection of viral titer decay alone.
Figure 8. Effect of treatment delay on viral titer decay.
Oseltamivir treatment is applied at various times post infection and at different efficacies. The effect of varying the base infection parameters is also explored by either decreasing (bottom row) or increasing (top row) viral production rate (p) (first column), infection rate (β) (second column), viral clearance rate (c) (third column), eclipse duration (τE) (fourth column), infectious lifespan (τI) (last column) by 10-fold (except τE, see text) compared to the base parameters.
Discussion
Motivated by studies of HIV and HCV that used mathematical modelling to extract drug treatment efficacy from viral decay rates33,34,35, we investigated the possibility of extracting drug treatment efficacy for influenza infections. Determining drug efficacy for influenza is a slightly more challenging problem because of the short duration and rapidly changing viral titer of influenza. HIV and HCV are chronic infections and drug treatment is typically applied when the infection is in a stable steady state, making it possible to use simplifying assumptions and perform a mathematical analysis of the system. Influenza, on the other hand, does not reach a steady state making mathematical analysis of drug treatment more complex.
One key assumption used in the HIV and HCV analysis is that drug treatment is constant over time. While this is also a common assumption in modelling of influenza infections26,37,48, it has not been determined whether this is actually a reasonable assumption. The typical treatment for influenza involves taking a pill twice a day. This leads to oscillations in the drug concentration. In long-lasting infections such as HIV and HCV, such oscillations are short compared to the duration of the infection. Influenza, however, typically lasts 7 d, so 12 h oscillations in drug concentration might be significant. Herein, we derive an expression (Eq. 1) for converting the time-varying infection dose into a constant drug concentration. We find that with this expression, the approximation of a constant antiviral concentration is appropriate as long as the oscillations in drug concentration are insufficient to create oscillations in the treated viral titers. In particular, we are able to accurately estimate viral decay rate over a broad range of doses and timings under the constant drug assumption. We do not, however, correctly reproduce the time of viral peak; the viral titer curves produced with our constant drug assumptions are shifted in time relative to the original PK viral titers. Our assumptions work best when the true dose (Dadmin) and the time elapsed between successive oral doses (τ) are not too large so that the time to antiviral concentration steady state is short. When the true drug concentration consists of a series of sparsely spaced spikes, then, not surprisingly, the assumption of a constant drug concentration does not accurately reproduce viral titer kinetics.
Since we found that assuming a constant drug concentration for modelling of influenza infections is a reasonable assumption, we used the simplification of a constant drug assumption to assess whether it is possible to extract drug efficacy from the viral decay rate alone. A previous study derived an analytical expression for the viral decay rate of untreated influenza infections modelled using exponential transitions between cell states49. This study determined that the viral decay rate is determined by the smallest of c, 1/τI, or 1/τE. Our model is based on more realistic probability distributions for cell transitions50 which does not have this same dependency. Our application of drug also complicates the analysis since we are sometimes imposing viral decay when an untreated infection would still be growing. A simplifying assumption of viral load and infectious cell proportionality is possible for influenza, but our analysis showed that this assumption only holds for about 60 h during the course of the infection. Since we often do not know when the infection started, it is difficult to judge whether this assumption is valid for the patient we are assessing. However, the key point of our manuscript is not whether in theory the efficacy could be extractable provided that certain conditions are met. Rather, the key point is whether the efficacy of an antiviral drug can reliably be determined from viral titer decay alone. For example, viral titer decay alone cannot confirm (or deny) that V is proportional to I during said decay and assuming that it is would not be appropriate unless other knowledge/information is available (i.e. not just viral titer decay data alone). While others might have made this assumption in the past and might have claimed to have estimated antiviral efficacy via this assumption, then it is their claim that is too strong. That is, unless they provided additional evidence (i.e. beyond viral decay data alone) that I is indeed proportional to V during decay for their particular virus/host system.
Moreover, it is clear that the rate of decay of viral titer in this model is determined not only by drug efficacy, but also by the viral infection parameters and the time at which treatment is initiated. Similar parameter dependencies have been observed in chronic infections51 although for chronic infections it is often possible to estimate these parameters with data collected from the chronic phase of the infection. In the case of influenza, we often only have clinical data from the decay phase, so it is difficult to estimate infection parameters. This means that a larger viral decay rate in a patient could be attributed to either or both increased antiviral efficacy and decreased viral titer growth parameters. Thus, not surprisingly, antiviral efficacy cannot be determined from viral titer decay alone and requires knowledge of the parameters driving infection growth in each patient. To establish these parameters, viral titers at the early time of the infection (i.e., during viral titer growth) are required in sufficient number to determine the infection growth rate (i.e., at least 3 viral titer samples prior to viral titer peak to reasonably characterize the viral titer up-slope).
Another key concern in determining antiviral efficacy is distinguishing viral decay due to antiviral treatment from that due to the natural resolution of the infection. We found applying antiviral treatment later results in larger viral titer decay rates. Since influenza is an acute infection, it typically resolves on its own and the viral decay after viral peak occurs even in the absence of antiviral treatment. That natural viral decay rate is likely modulated by the strength of the immune response in clearing both infected cells and free virus. Therefore, viral titer decay in treated patients can be due to either or both natural resolution of the infection and the action of the antiviral. As such, even with a comprehensive, well-sampled, viral titer time course, it might not be possible to resolve antiviral efficacy in a given patient as it would be indistinguishable from natural infection resolution. Studies where decay phase of the viral load are used to examine the efficacy of NAIs28,29,30,31,32 are tacitly assuming that all their patients can be described with the same infection parameters, particularly that they would have the same natural decay rate in the absence of antivirals. This is not a reasonable assumption, and our study shows that even small variations in underlying dynamical parameters will alter the measured viral decay rate. We believe antiviral efficacy in treating influenza is best determined from massive sets of viral titers and would manifest therein as a statistically significant departure of the viral kinetic parameters of a treated group versus that of an untreated group. Perhaps sub-optimal treatment in some of the antiviral-treated group would help show a progression or shift in the viral kinetics parameter(s) from the placebo-treated to the effectively treated patient groups which could make a more convincing case for the efficacy of the antiviral in affecting that viral kinetic parameter.
Methods
Viral kinetic model
We use a modified version50 of the basic influenza infection model first presented in ref. 48.
 |
Target cells (T) are infected at a rate β/N, where N is the total number of cells, and enter the eclipse phase. Eclipse cells (E) are cells that have been infected by virus (V) but are not yet releasing any new virions. Infectious cells (I) are producing and releasing virus at a rate p. Infectious cells eventually stop producing virus (and/or die) and are removed from the system. Virus is removed at clearance rate c. Transition from eclipse to infectious is a probabilistic process where PE(t) (or PI(t)) is the probability that the cell remains in the eclipse (or infectious) phase for a time t, and fE(t) is the associated probability density function. We model both transitions with normal distributions having standard deviations σE or σI and average lifespans τE and τI. The use of the normal distribution is more biologically realistic than the exponential distribution tacitly assumed by ordinary differential equations, as the normal distribution imposes a minimum length of time in which the cell must remain in that state and does not allow cells to remain in a particular state for excessively long times50.
We model the action of NAIs, which block viral release4,5, as reducing the production rate p. The drug is applied via the parameter ε(t), which is a number between 0 and 1 and represents the potentially time-varying efficacy of the drug. Viral kinetic parameters were taken from ref. 48 and are presented in Table 1.
Table 1. Parameters and initial conditions taken from ref. 48 unless otherwise indicated.
| Parameter | Meaning | Value |
|---|---|---|
| Viral kinetic parameters | ||
| β | Infection rate | 3.2 × 10−5 d−1 ⋅ [TCID50/mL]−1 |
| p | Production rate | 4.6 × 10−2TCID50⋅d−1⋅mL−1 |
| c | Clearance rate | 5.2 d−1 |
| τE | Eclipse phase, mean duration | 6 h |
| σE | Eclipse phase, standard deviation | 1 h45 |
| τI | Infectious lifespan, mean duration | 12 h45 |
| σI | Infectious lifespan, standard deviation | 1 h45 |
| Initial conditions | ||
| T0 | Initial number of target cells | 4 × 108cells |
| E0 | Initial number of eclipse cells | 0 cells |
| I0 | Initial number of infectious cells | 0 cells |
| V0 | Initial amount of virus | 7.5 × 10−2TCID50 |
| Pharmacokinetic/pharmacodynamic parameters | ||
| ka | Drug absorption rate | 0.46 h−1 54 |
| ke | Drug elimination rate | 0.11 h−1 54 |
| EC50 | 50% effective concentration | 7.3 mg [see text] |
| εmax | Maximum inhibitory effect | 0.98 [see text] |
Pharmacokinetic and pharmacodynamic models
Our aim is to determine whether the viral titer resulting from a time-varying drug treatment can be approximated by viral titers produced with the assumption of constant drug treatment. For this, we need a time-varying PK model to simulate time-varying drug treatment regimens. We use the following PK model to simulate the course of a time-varying drug regimen52,
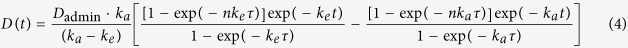 |
where Dadmin is the dose of the pill administered in units of mg, τ is the time between doses, ka and ke are the drug absorption and elimination rates, respectively, and n is the number of doses administered. Time, t, is measured from the nth dose. We use the pharmacokinetic (PK) parameters for oseltamivir because it is the most commonly prescribed NAI53. The parameters were obtained from studies of oseltamivir PK54 and are presented in Table 1. Note that we are not trying to reproduce the full pharmacokinetics of oseltamivir, which as a prodrug would require a two compartment PK model55, but are trying to ascertain whether a time-varying drug regimen can reasonably be approximated by an assumption of a constant level of drug.
The drug efficacy used in the viral kinetics model is related to drug dose through the Emax pharmacodynamic (PD) model56,
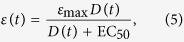 |
where EC50 is the dose at which half the maximal effect is achieved and εmax is the maximum effect of the drug. Efficacy is between 0 and 1 and represents the fractional reduction in production from an untreated infection. For example, an efficacy of 0.4 reduces the viral production rate by 40%. In the case of a time-varying drug dose, and thus a time-varying drug efficacy, the effective production rate will also vary in time. Oseltamivir binds to and inhibits the activity of neuraminidase4,5, as the amount of drug available in the system varies with time, the number of bound, deactivated neuraminidase proteins will also vary, altering the viruses ability to release itself from the cell surface.
The EC50 for oseltamivir is dependent on the viral strain and so it can vary widely, from 0.0008–35 μM57. We decided to use 0.5 μM as it is approximately in the middle of this wide range. Note that we are using EC50 rather than IC50 because the viral kinetics model models the effect of the drug on the course of the infections and not inhibition of NA activity by the drug58. Drug efficacy is a unitless quantity so drug dose can be represented either as the oral dose or as the blood plasma concentration with no loss in generality as long as EC50 is represented in the same units. Since we are modelling in vivo human infections which are treated by giving pills with doses in milligrams, we convert the EC50 to milligrams based on parameters from ref. 54 for ease of interpretation. There have not, to date, been any studies that have determined εmax for oseltamivir. Instead, we use the results of previous modelling studies of zanamivir (a drug in the same class as oseltamivir) treatment of influenza infections26,48 and set εmax = 0.98.
Additional Information
How to cite this article: Palmer, J. et al. The in vivo efficacy of neuraminidase inhibitors cannot be determined from the decay rates of influenza viral titers observed in treated patients. Sci. Rep. 7, 40210; doi: 10.1038/srep40210 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
The authors would like to thank the reviewers for their helpful comments. This research was supported in part by Discovery Grant 355837-2013 from the Natural Sciences and Engineering Research Council of Canada (to C.A.A.B.), Early Researcher Award ER13-09-040 (to C.A.A.B.) from the Ministry of Research and Innovation of the Government of Ontario, with additional support through the iTHES research programme at RIKEN (to C.A.A.B.). This work was made possible by the facilities of the Shared Hierarchical Academic Research Computing Network (SHARCNET: www.sharcnet.ca) and Compute/Calcul Canada.
Footnotes
H.M.D. is currently receiving a grant from Janssen R&D, and C.A.A.B. has previously received a grant from AstraZeneca R&D.
Author Contributions C.A.A.B. conceived the experiment(s), J.P. and H.M.D. conducted the experiment(s), J.P., H.M.D. and C.A.A.B. analysed the results, J.P. and H.M.D. wrote the manuscript. All authors reviewed the manuscript.
References
- Centres for Disease Control and Prevention (CDC). Influenza activity – United States and worldwide, 2007–08 season. Morb Mortal Wkly Rep 57, 692–697 (2008). [PubMed] [Google Scholar]
- Drake J. W. Rates of spontaneous mutation among RNA viruses. Proc. Natl. Acad. Sci. USA 90, 4171–4175 (1993). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghedin E. et al. Mixed infection and the genesis of influenza virus diversity. J. Virol. 83, 8832–8841 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abed Y. et al. Characterization of 2 influenza A(H3N2) clinical isolates with reduced susceptibility to neuraminidase inhibitors due to mutations in the hemagglutinin gene. J. Infect. Dis. 186, 1074–1080 (2002). [DOI] [PubMed] [Google Scholar]
- Gubareva L. V., Kaiser L. & Hayden F. G. Influenza virus neuraminidase inhibitors. Lancet 355, 827–835 (2000). [DOI] [PubMed] [Google Scholar]
- Gubareva L. V. et al. Characterization of mutants of influenza A virus selected with the neuraminidase inhibitor 4-guanidino-Neu5Ac2en. J. Virol. 70, 1818–1827 (1996). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schünemann H. J. et al. WHO rapid advice guidelines for pharmacological management of sporadic human infection with avian influenza A (H5N1) virus. Lancet Infect. Dis. 7, 21–31 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baz M., Abed Y., McDonald J. & Boivin G. Characterization of multidrug-resistant influenza A/H3N2 viruses shed during 1 year by an immunocompromised child. Clin. Infect. Dis. 43, 1555–1561 (2006). [DOI] [PubMed] [Google Scholar]
- Weinstock D. M. & Zucotti G. The evolution of influenza resistance and treatment. JAMA 301, 1066–1069 (2009). [DOI] [PubMed] [Google Scholar]
- Kawai N. et al. Comparison of the clinical symptoms and the effectiveness of neuraminidase inhibitors for patients with pandemic influenza H1N1 2009 or seasonal H1N1 influenza in the 2007–2008 and 2008–2009 seasons. J. Infect. Chemother. 17, 375–381 (2011). [DOI] [PubMed] [Google Scholar]
- Rameix-Welti M.-A., van der Werf S. & Naffakh N. Sensitivity of H5N1 influenza viruses to oseltamivir: An update. Future Virol. 3, 157–165 (2008). [Google Scholar]
- de Jong M. D. et al. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N. Engl. J. Med. 353, 2667–2672 (2005). [DOI] [PubMed] [Google Scholar]
- Wetherall N. T. et al. Evaluation of neuraminidase enzyme assays using different substrates to measure susceptibility of influenza virus clinical isolates to neuraminidase inhibitors: Report of the neuraminidase inhibitor susceptibility network. Journal of Clinical Microbiology 41, 742–750 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubareva L. V., Webster R. G. & Hayden F. G. Detection of influenza virus resistance to neuraminidase inhibitors by an enzyme inhibition assay. Antiviral Res. 53, 47–61 (2002). [DOI] [PubMed] [Google Scholar]
- Nguyen J. T., Sheu T. G., Mishin V. P., Klimov A. I. & Gubareva L. V. Assessment of pandemic and seasonal influenza A (H1N1) virus susceptibility to neuraminidase inhibitors in three enzyme activity inhibition assays. Antimicrob. Agents Chemother. 54, 3671–3677 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okomo-Adhiambo M., Sheu T. G. & Gubareva L. V. Assays for monitoring susceptibility of influenza viruses to neuraminidase inhibitors. Influenza and Other Resp. Viruses 7, 44–49 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubareva L. V. et al. A release-competent influenza a virus mutant lacking the coding capacity for the neuraminidase active site. J. Gen. Virol. 83, 2683–2692 (2002). [DOI] [PubMed] [Google Scholar]
- Hughes M. T., Matrosovich M., Rodgers M. E., McGregor M. & Kawaoka Y. Influenza A viruses lacking sialidase activity can undergo multiple cycles of replication in cell culture, eggs, or mice. J. Virol. 74, 5206–5212 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C., Eichelberger M. C., Compans R. W. & Air G. M. Influenza type A virus neuraminidase does not play a role in viral entry, replication, assembly, or budding. J. Virol. 69, 1099–1106 (1995). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer K. et al. Neuraminidase inhibitor susceptibility of swine influenza A viruses isolated in germany between 1981 and 2008. Med. Microbiol. and Immunol. 201, 61–72 (2012). [DOI] [PubMed] [Google Scholar]
- Hoopes J. D. et al. Triple combination antiviral drug (TCAD) composed of amantadine, oseltamivir, and ribavirin impedes the selection of drug-resistant influenza A virus. PLoS ONE 6, e29778 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen J. T. et al. Triple combination of oseltamivir, amantadine, and ribavirin displays synergistic activity against multiple influenza virus strains in vitro. Antimicrob. Agents Chemother. 53, 4115–4126 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samson M. et al. Characterization of drug-resistant influenza virus A(H1N1) and A(H3N2) variants selected in vitro with laninamivir. Antimicrob. Agents Chemother. 58, 5220–5228 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dang Y.-X., Li X.-Z. & Martcheva M. Competitive exclusion in a multi-strain immuno-epidemiological influenza model with environmental transmission. J. Biol. Dyn. 10, 416–456 (2016). [DOI] [PubMed] [Google Scholar]
- Pawelek K. A., Salmeron C. & Valle S. D. Connecting within and between-hosts dynamics in the influenza infection-staged epidemiological models with behavior change. J. Coupled Systems Multiscale Dyn. 3, 233–243 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handel A., Longini Jr, I. M. & Antia R. Neuraminidase inhibitor resistance in influenza: Assessing the danger of its generation and spread. PLoS Comput. Biol. 3, e240 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- He G., Massarella J. & Ward P. Clinical pharmacokinetics of the prodrug oseltamivir and its active metabolite Ro 64-0802. Clin. Pharmacokinet. 37, 471–484 (1999). [DOI] [PubMed] [Google Scholar]
- Zhang Y. et al. Efficacy of oseltamivir-peramivir combination therapy compared to oseltamivir monotherapy for influenza A (H7N9) infection: a retrospective study. BMC Infect. Dis. 16, 76 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitley R. et al. Single dose peramivir for the treatment of acute seasonal influenza: integrated analysis of efficacy and safety from two placebo-controlled trials. Antiviral Therapy 20, 709–719 (2015). [DOI] [PubMed] [Google Scholar]
- Sugaya N. et al. Comparison between virus shedding and fever duration after treating children with pandemic A H1N1/09 and children with A H3N2 with a neuraminidase inhibitor. Antivir. Ther. 20, 49–55 (2015). [DOI] [PubMed] [Google Scholar]
- Sato M. et al. Sequential influenza B viral load and susceptibility in children treated with oseltamivir and zanamivir. Ped. Inf. Dis. J 33, E168–E172 (2014). [DOI] [PubMed] [Google Scholar]
- Takemoto Y. et al. Clinical effects of oseltamivir, zanamivir, laninamivir and peramivir on seasonal influenza infection in outpatients in japan during the winter of 2012–2013. Chemother. 59, 373–378 (2013). [DOI] [PubMed] [Google Scholar]
- Neumann A. U. et al. Hepatitis C viral dynamics in vivo and the antiviral efficacy of interferon-α therapy. Science 282, 103–107 (1998). [DOI] [PubMed] [Google Scholar]
- Nowak M. A. et al. Viral dynamics in hepatitis B virus infection. Proc. Natl. Acad. Sci. USA 93, 4398–4402 (1996). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perelson A. S., Neumann A. U., Markowitz M., Leonard J. M. & Ho D. D. HIV-1 dynamics in vivo: Virion clearance rate, infected cell life-span, and viral generation time. Science 271, 1582–1586 (1996). [DOI] [PubMed] [Google Scholar]
- Massarella J. W. et al. The pharmacokinetics and tolerability of the oral neuraminidase inhibitor oseltamivir (Ro 64-0796/GS4104) in healthy adult and elderly volunteers. J. Clin. Pharmacol. 40, 836–843 (2000). [DOI] [PubMed] [Google Scholar]
- Dobrovolny H. M., Gieschke R., Davies B. E., Jumbe N. L. & Beauchemin C. A. A. Neuraminidase inhibitors for treatment of human and avian strain influenza: A comparative study. J. Theor. Biol. 269, 234–244 (2011). [DOI] [PubMed] [Google Scholar]
- Hayden F. G. et al. Use of the oral neuraminidase inhibitor oseltamivir in experimental human influenza: randomized controlled trials for prevention and treatment. JAMA 282, 1240–1246 (1999). [DOI] [PubMed] [Google Scholar]
- Gubareva L. V., Kaiser L., Matrosovich M. N., Soo-Hoo Y. & Hayden F. G. Selection of influenza virus mutants in experimentally infected volunteers treated with oseltamivir. J. Infect. Dis. 183, 523–531 (2001). [DOI] [PubMed] [Google Scholar]
- LaBarre D. D. & Lowy R. J. Improvements in methods for calculating virus titer estimates from TCID50 and plaque assays. J. Virol. Methods 96, 107–126 (2001). [DOI] [PubMed] [Google Scholar]
- Widmer N. et al. Oseltamivir in seasonal, avian H5N1 and pandemic 2009 A/H1N1 influenza: Pharmacokinetic and pharmacodynamic characteristics. Clin. Pharmacokinet. 49, 741–765 (2010). [DOI] [PubMed] [Google Scholar]
- Holder B. P. et al. Assessing the in vitro fitness of an oseltamivir-resistant seasonal A/H1N1 influenza strain using a mathematical model. PLoS ONE 6, e14767 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinilla L. T., Holder B. P., Abed Y., Boivin G. & Beauchemin C. A. A. The H275Y neuraminidase mutation of the pandemic A/H1N1 influenza virus lengthens the eclipse phase and reduces viral output of infected cells, potentially compromising fitness in ferrets. J. Virol. 86, 10651–10660 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchemin C. A. A. et al. Modeling amantadine treatment of influenza A virus in vitro. J. Theor. Biol. 254, 439–451 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holder B. P., Liao L. E., Simon P., Boivin G. & Beauchemin C. A. A. Design considerations in building in silico equivalents of common experimental influenza virus assays and the benefits of such an approach. Autoimmunity 44 (2011). [DOI] [PubMed] [Google Scholar]
- Hayden F. G. et al. Local and systemic cytokine responses during experimental human influenza A virus infection. Relation to symptom formation and host defense. J. Clin. Invest. 101, 643–649 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz R. S. et al. Nasal cytokine and chemokine response in experimental influenza A virus infection: Results of a placebo-controlled trial of intravenous zanamivir treatment. J. Infect. Dis. 180, 586–593 (1999). [DOI] [PubMed] [Google Scholar]
- Baccam P., Beauchemin C., Macken C. A., Hayden F. G. & Perelson A. S. Kinetics of influenza A virus infection in humans. J. Virol. 80, 7590–7599 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A. M., Adler F. R. & Perelson A. S. An accurate two-phase approximate solution to an acute viral infection model. J. Math. Biol. 60, 711–726 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holder B. P. & Beauchemin C. A. A. Exploring the effect of implementing different biological delays in constructing kinetic models of influenza infection within a host or cell culture. BMC Public Health 11, S10 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd A. L. The dependence of viral parameter estimates on the assumed viral life cycle: Limitations of studies of viral load data. Proc. Biol. Sci. 268, 847–854 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhillon S. & Kostrzewski A. (eds) Clinical Pharmacokinetics 1st edn. (Pharmaceutical Press, London, 2006). [Google Scholar]
- Hsieh Y.-H., Chen K.-F., Gaydos C. A., Rothman R. E. & Kelen G. D. Antiviral prescriptions to US ambulatory care visits with a diagnosis of influenza before and after high level of adamantane resistance 2005–06 season. PLoS One 5, e8945 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rayner C. R., Chanu P., Gieschke R., Boak L. M. & Jonsson E. N. Population pharmacokinetics of oseltamivir when coadministered with probenecid. J. Clin. Pharmacol. 48, 935–947 (2008). [DOI] [PubMed] [Google Scholar]
- Davies B. E. Pharmacokinetics of oseltamivir: an oral antiviral for the treatment and prophylaxis of influenza in diverse populations. J. Antimicrob. Chemother. 65, 5–10 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holford N. H. G. & Sheiner L. B. Understanding the dose-effect relationship: Clinical application of pharmacokinetic-pharmacodynamic models. Clin. Pharmacokinet. 6, 429–453 (1981). [DOI] [PubMed] [Google Scholar]
- Roche Pharmaceuticals. Tamiflu (oseltamivir phosphate) capsules and for oral suspension. Roche Laboratories Inc. (2005). [Google Scholar]
- Beggs N. F. & Dobrovolny H. M. Determining drug efficacy parameters for mathematical models of influenza. J. Biol. Dynamics 9, 332–346 (2015). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.