Abstract
Background: While black mothers initiate human milk (HM) provision at lower rates than non-black mothers in the United States, some neonatal intensive care units (NICUs) report similar initiation rates regardless of race/ethnicity for mothers of very-low-birth-weight (VLBW) infants. However, racial disparity frequently becomes evident in the proportion of black infants who continue to receive HM feedings at NICU discharge. Since social factors have been associated with differences in HM provision for term infants, we sought to identify differences in social factors associated with HM feeding at discharge based on race/ethnicity.
Materials and Methods: A prospective cohort study of racially diverse mothers of VLBW infants measured social factors including maternal education, breastfeeding support, return to work/school, HM feeding goal, previous breastfeeding, or formula experience. Multivariate logistic regression modeling was applied to social factors to predict HM feeding at discharge. Additional regression models were created for racial/ethnic subgroups to identify differences.
Results: For all 362 mothers, WIC (Special Supplemental Nutrition Program for Women, Infants, and Children) eligibility and maternal goal near time of discharge of providing any HM negatively and positively predicted HM feeding at discharge, respectively. Perceived breastfeeding support from the infant's maternal grandmother negatively predicted HM feeding at discharge for black mothers.
Conclusions: Future interventions to increase duration of HM provision in VLBW infants should focus on the establishment and maintenance of maternal HM feeding goals. Further studies of the familial support system of black mothers are warranted to determine multigenerational impact and potential interventions.
Keywords: : premature infant, social factors, barriers, NICU, human milk
Introduction
In the United States, black (non-Hispanic) women give birth to very-low-birth-weight (VLBW, birth weight [BW] <1,500 g) infants 2.6 times more often than non-Hispanic white women,1 yet significantly fewer black premature infants receive human milk (HM; breast milk from own mother) compared to non-black premature infants.2,3 Since HM reduces the risk of prematurity-associated complications, including infections, necrotizing enterocolitis, rehospitalizations, and neurodevelopmental delay in a dose–response manner,2,4–7 this racial disparity increases the risk of potentially preventable complications for black VLBW infants. This racial disparity also reduces black mothers' dose-related benefits of lactation, such as reduced risks of breast and ovarian cancer, diabetes, hypertension, and myocardial infarction.8,9
Some neonatal intensive care units (NICUs) have successfully reduced racial disparities in HM initiation by mothers of VLBW infants.10,11 However, higher initiation rates do not translate to a sustained reduction in disparities because fewer black mothers continue to provide HM to their VLBW infants at the time of NICU discharge.3 In our recently completed prospective cohort study, 98% of 430 VLBW infants born to racially diverse mothers (52% black, 19% white, 27% Hispanic, 2% other) received some HM. As NICU discharge approached, 78% of black mothers indicated that their feeding goal was to provide HM,12 but only 28% of their infants were discharged receiving any HM versus 50% for non-black mothers. These data compel an examination of modifiable and nonmodifiable barriers, including NICU and non-NICU factors, which impact the duration of HM provision for this vulnerable population.
Non-NICU factors, for example, those that are independent of NICU lactation resources, may include neighborhood structural factors13 or social factors. Studies of social factors and lactation in mothers of term and preterm infants suggest differences in prevalence of these factors among different racial/ethnic groups, including the following: (1) previous experience with HM feeding in mothers of preterm infants,14,15 (2) previous experience with formula feeding in mothers of term infants,16 (3) return to work/school in mothers of preterm infants,15,17 (4) the role of social support of breastfeeding and pumping in mothers of preterm infants,17,18 (5) HM provision goal in mothers of term and preterm infants,14,19 (6) maternal education in mothers of preterm infants,15,18 and (7) public perception and attitudes on breastfeeding.20 Our objective was to determine whether specific social factors contributed to the disparity in rates of VLBW infants receiving HM at the time of NICU discharge.
Materials and Methods
This is a secondary analysis of a prospective cohort study of mothers of 430 VLBW infants who were admitted between February 2008 and December 2012 to Rush University Medical Center's (RUMC) level III NICU. The exclusion criteria have been described previously6,7,21; HM feeding was not a prerequisite for study participation. As per standard practice, all mothers received the same lactation care by employed NICU-specific breastfeeding peer counselors, all of whom are former NICU parents and represent the racial/ethnic composition of the patients cared for at RUMC.22 All mothers initiated pumping with a hospital-grade pump, were able to rent a hospital-grade pump with subsidized payment when discharged from the hospital, and had access to a complimentary weekly taxi service to bring them to the NICU. Informed consent was obtained from mothers for themselves and their infants.
Although both infant and maternal data were prospectively collected, the original cohort study examined infant outcomes and costs of NICU care.6,7,21 The prospectively collected data included maternal age, highest education level (completed less than high school, high school, less than 4-year college, 4-year college or graduate degree), self-stated race/ethnicity (non-Hispanic black [black], non-Hispanic white [white], Hispanic, other [six Asian, one Native American]), marital status (dichotomous), and Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) eligibility (dichotomous).23 Since Asian mothers comprised a very small proportion of the cohort and had similar socioeconomic characteristics and breastfeeding rates24 to the white mothers in the cohort, Asian and white mothers were combined in analyses. The one Native American mother was excluded.
Questionnaires were prospectively administered by research assistants to collect longitudinal feeding goals,12 previous breastfeeding and formula feeding experience, plan to return to work or school after infant's birth, number of children in the household, and social support and nonsupport for breastfeeding and pumping (both as a dichotomous variable and identification of supportive/nonsupportive person). The number of collected feeding goals varied based on visitation patterns and discontinuation of feeding goal query once goal changed to “no HM,” and reasons for changing goals were not collected. The latest available feeding goal was used as the maternal goal near the time of discharge. Prospectively collected infant data included BW, gestational age (GA), gender, multiple gestation, and daily intake (mL) of HM and formula from birth to NICU discharge. HM feeding at discharge was determined by the infant's feedings on the last full day of hospitalization, classified as exclusive HM (only fortified or unfortified HM, no formula), partial HM (some HM and some formula), or no HM (only formula).11
The following social factors were examined in relation to HM feeding at discharge: for multiparous subjects (1) previous experience with HM feeding, (2) previous experience with formula feeding; for all subjects (3) return to work/school, (4) friend/family/peer support or nonsupport of breastfeeding and pumping, (5) HM provision goal near time of discharge from the NICU (any HM or none), and (6) maternal education.
Data analyses
Descriptive statistics include mean ± standard deviation and n (%). Data were analyzed using chi-square or the Mann–Whitney U test. Correlation coefficients (point-biserial, Spearman's rho, or phi as appropriate) were computed to assess the relationship between each social factor and HM at NICU discharge. Initially, social factors were regressed on HM feeding at NICU discharge for the entire cohort using multivariate logistic regression, controlling for maternal age, race/ethnicity, WIC eligibility, baseline employment/student status, marital status, number of children in household, infant BW, GA, gender, and length of NICU hospitalization. A separate analysis considered only multiparous mothers. To identify social factors that may be unique by racial/ethnic groups, bivariate and multivariate analyses were repeated separately for the three racial/ethnic subgroups. Analyses were conducted using SPSS version 22 (IBM Corp, Armonk, NY). Significance was set at p < 0.05 for all analyses.
Results
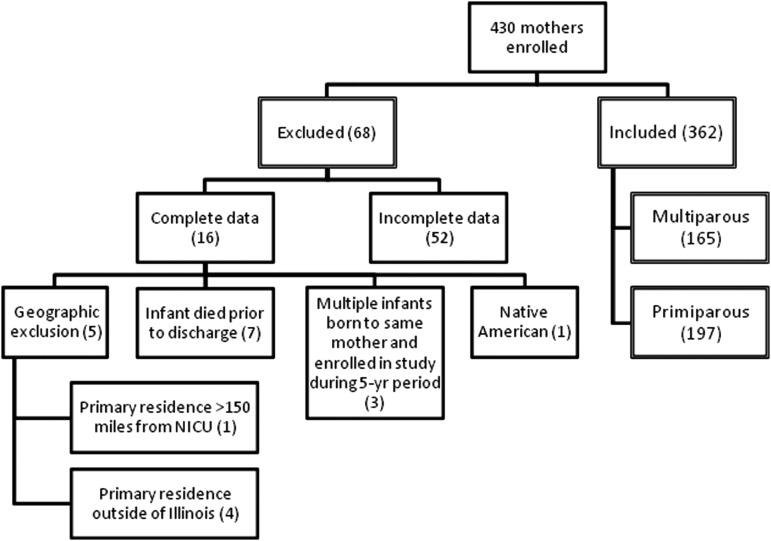
Of 430 enrolled mothers, 362 with complete data were included in this analysis (Fig. 1). Exclusion criteria included infants who died before NICU discharge (n = 7), family residence >150 miles from the NICU or outside Illinois (n = 5), multiple VLBW infants born to the same mother in separate pregnancies and enrolled in the study during the 5-year study period (n = 3), Native American (n = 1), and incomplete data (n = 52). The excluded mothers were similar to included mothers for race/ethnicity (p = 0.43) and all other characteristics, except excluded mothers were more likely to have a male infant (p < 0.05) with higher BW (1,126 ± 261 g excluded versus 1,035 ± 252 g included, p < 0.05), and were less likely to provide any HM during NICU stay (90.2% excluded versus 98.6% included, p < 0.001) or have a goal, near discharge, of providing exclusive HM (28.6% excluded versus 47% included, p < 0.05).
FIG. 1.
Cohort diagram of included and excluded subjects.
Table 1 summarizes maternal and infant characteristics and social factors for the 362 mother-infant dyads and by race/ethnicity subgroups. Feeding goals were assessed 3 [2–5] (median [interquartile range]) times per mother with the maternal goal near discharge assessed at infant's day of life 37 [11–61]. Among all mothers, black mothers were significantly younger and less likely to be married, provide HM at NICU discharge, and have support from family/friend/partner. Hispanic mothers were significantly less likely to have been employed or been a student before delivery or to have a plan to return to work or school, and more likely to have less than a high school education. Among multiparous mothers, black mothers were significantly less likely to have experience with breastfeeding.
Table 1.
Cohort Characteristics
| Characteristics of cohorta | Total (n = 362) | Black (n = 183) | White/Asian (n = 82) | Hispanic (n = 97) |
|---|---|---|---|---|
| Maternal characteristics | ||||
| Maternal age (years)*** | 27.3 ± 6.4 | 26.2 ± 6.3 | 28.8 ± 5.6 | 28.2 ± 6.8 |
| WIC eligible*** | 264 (72.5) | 154 (83.2) | 31 (37.8) | 79 (81.4) |
| Multiparous | 165 (45.3) | 91 (49.2) | 31 (37.8) | 43 (44.3) |
| Married*** | 142 (39.1) | 28 (15.1) | 57 (70.4) | 57 (58.8) |
| Provided any HM while infant in NICU | 359 (98.6) | 180 (97.3) | 82 (100) | 97 (100) |
| HM at NICU discharge*** | 125 (34.3) | 45 (24.3) | 36 (43.9) | 44 (45.4) |
| Number of children in household | 2.0 ± 1.4 | 2.2 ± 1.6 | 1.8 ± 1.2 | 2.0 ± 1.3 |
| Infant characteristics | ||||
| Multiple gestation*** | 58 (15.9) | 22 (11.9) | 28 (34.1) | 8 (8.2) |
| Male | 187 (51.4) | 97 (52.4) | 44 (53.7) | 46 (47.4) |
| Birth GA (completed weeks) | 27.9 ± 2.4 | 27.9 ± 2.4 | 27.7 ± 2.5 | 28.1 ± 2.4 |
| Birth weight (g)* | 1,035 ± 252 | 1,020 ± 254 | 1,002 ± 244 | 1,092 ± 250 |
| Length of NICU hospitalization (days) | 73.2 ± 35.0 | 73.1 ± 37.5 | 77.9 ± 33.4 | 69.3 ± 30.9 |
| Social factors | ||||
| Experience with breastfeedingb*** | 100 (60.6) | 42 (47.2) | 27 (81.8) | 31 (72.1) |
| Experience with formula feedingb | 150 (90.9) | 84 (94.4) | 29 (87.9) | 37 (86.0) |
| Employed or Student before delivery*** | 232 (64.1) | 121 (66.1) | 63 (76.8) | 48 (49.5) |
| Plan to return to work or school** | 177 (48.6) | 94 (50.8) | 49 (59.8) | 34 (35.1) |
| Support from family/friend/partner* | 346 (95.1) | 171 (92.4) | 81 (98.8) | 94 (96.9) |
| Nonsupport from family/friend/partner | 6 (1.6) | 4 (2.2) | 2 (2.4) | 0 (0) |
| HM provision goal near time of discharge | ||||
| Exclusive HM | 171 (47.0) | 74 (40.0) | 45 (54.9) | 52 (53.6) |
| HM and formula | 106 (29.1) | 61 (33.3) | 18 (22.0) | 27 (27.8) |
| Exclusive Formula/Uncertain | 87 (23.9) | 50 (27.0) | 20 (23.2) | 18 (18.6) |
| Maternal education*** | ||||
| Less than high school | 60 (16.5) | 17 (9.2) | 8 (9.8) | 35 (36.1) |
| High school complete | 93 (25.5) | 52 (28.1) | 15 (18.3) | 26 (26.8) |
| Some college or trade school | 136 (37.4) | 88 (47.6) | 26 (31.7) | 22 (22.7) |
| Completed 4-year college | 75 (20.6) | 28 (15.1) | 33 (40.2) | 14 (14.4) |
Data expressed as mean ± standard deviation or n (%). Data were analyzed using chi-square or the Mann–Whitney U test.
Asterisks indicate significant differences by race/ethnicity.
Experience with breastfeeding and formula presented only for multiparous cases (n = 165).
p < 0.05; **p < 0.01; ***p < 0.001.
GA, gestational age; HM, human milk; NICU, neonatal intensive care unit; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
Correlations with HM feeding at discharge for entire cohort
For the entire cohort, significant correlations were found between social factors and HM feeding at discharge. Positively correlated social factors included older maternal age (r = 0.26, p < 0.001), Hispanic ethnicity (r = 0.14, p = 0.006), being married (r = 0.31, p < 0.001), higher level of maternal education (r = 0.19, p < 0.001), and having a goal of any HM near discharge (r = 0.31, p < 0.001). Negatively correlated social factors included black race (r = −0.22, p < 0.001), WIC eligibility (r = −0.34, p < 0.001), previous experience with formula feeding (r = −0.12, p = 0.023), and additional children in the household (r = −0.14, p = 0.010). Overall, neither friend/family/peer support nor nonsupport of breastfeeding was significantly correlated with HM feeding at NICU discharge. When examining the specific person who was supportive (e.g., infant's father, mother's sister, mother's mother), only support of the mother's mother (infant's maternal grandmother) was significantly correlated with HM feeding at NICU discharge, although in a negative manner (r = −0.13, p = 0.013).
Multivariate binary logistic regression analysis for entire cohort
We found that the strongest predictor of HM feeding at NICU discharge was the maternal goal of any HM near discharge (OR 8.38 [95% CI 3.42–20.53], p < 0.001). Significant negative predictors were support from the mother's mother (OR 0.45 [95% CI 0.26–0.79], p = 0.005) and WIC eligibility (OR 0.34 [95% CI 0.15–0.75], p = 0.008) (Table 2). To determine the extent that previous experience with either HM or formula influenced HM feeding at NICU discharge, we examined the multiparous subgroup. Maternal goal of any HM near discharge was again the strongest predictor of HM feeding at discharge (OR 10.47 [95% CI 1.83–59.95], p = 0.008), and female infant was also a significant predictor (OR 2.60 [95% CI 1.02–6.63], p = 0.044).
Table 2.
Logistic Regression of Social Factors and Human Milk Feeding at Discharge
| Total cohort (n = 362) | Multiparous subjects (n = 165) | |||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95%CI) | p | |
| Maternal age | 1.04 (0.99–1.10) | 0.103 | 1.05 (0.97–1.15) | 0.239 |
| Infant GA | 1.02 (0.85–1.23) | 0.794 | 0.97 (0.69–1.34) | 0.838 |
| Infant BW | 1.00 (1.00–1.00) | 0.877 | 1.00 (1.00–1.00) | 0.991 |
| Length of NICU hospitalization | 0.99 (0.98–1.00) | 0.202 | 0.98 (0.95–1.00) | 0.092 |
| Female infant | 0.96 (0.56–1.63) | 0.883 | 2.60 (1.02–6.63) | 0.044 |
| Race/ethnicitya | 0.250 | 0.415 | ||
| Black | 1.79 (0.78–4.09) | 0.168 | 1.82 (0.44–7.58) | 0.409 |
| Hispanic | 1.00 (0.46–2.19) | 0.996 | 0.75 (0.19–2.91) | 0.673 |
| Maternal educationb | 0.275 | 0.808 | ||
| Less than high school | 1.18 (0.40–3.45) | 0.767 | 1.36 (0.17–10.61) | 0.769 |
| High school complete | 0.52 (0.20–1.37) | 0.185 | 0.68 (0.11–4.10) | 0.678 |
| Some college or trade school | 0.81 (0.36–1.83) | 0.611 | 1.06 (0.22–4.97) | 0.945 |
| WIC eligible | 0.34 (0.15–0.75) | 0.008 | 0.40 (0.11–1.45) | 0.162 |
| Employed or student | 0.67 (0.27–1.66) | 0.393 | 0.22 (0.03–1.76) | 0.153 |
| Plan to return to work or school | 1.51 (0.66–3.48) | 0.332 | 5.64 (0.69–45.92) | 0.106 |
| Married | 1.61 (0.78–3.31) | 0.200 | 1.30 (0.43–3.95) | 0.646 |
| Number of children in household | 0.88 (0.68–1.12) | 0.287 | 0.77 (0.51–1.15) | 0.197 |
| Primiparous | 1.33 (0.66–2.68) | 0.422 | N/A | |
| Experience with breastfeeding | N/A | 2.46 (0.85–7.08) | 0.095 | |
| Experience with formula feeding | N/A | 0.29 (0.05–1.50) | 0.139 | |
| Breastfeeding support from infant's father | 0.94 (0.53–1.66) | 0.821 | 1.65 (0.64–4.26) | 0.299 |
| Breastfeeding support from mother's mother | 0.45 (0.26–0.79) | 0.005 | 0.49 (0.19–1.24) | 0.130 |
| Goal of any HM near discharge | 8.38 (3.42–20.53) | <0.001 | 10.47 (1.83–59.95) | 0.008 |
Significance was set at p < 0.05. Bold font denotes statistical significance.
Compared to white.
Compared to maternal education = Completed 4-year college.
BW, birth weight; CI, confidence interval; OR, odds ratio.
Correlations with HM feeding at discharge for racial/ethnic subgroups
Subgroup analyses demonstrated numerous social factors that significantly correlated with HM feeding at discharge (Table 3), but varied by racial/ethnic subgroup. However for all subgroups, being married and having a goal of any HM near discharge were positively correlated with HM feeding at NICU discharge, whereas WIC eligibility was negatively correlated. Again, neither friend/family/peer support nor nonsupport of breastfeeding was significantly correlated with HM feeding at discharge.
Table 3.
Significant Correlations of Social Factors with Human Milk Feeding at Discharge Stratified by Race/Ethnicity
| Correlation | p | |
|---|---|---|
| White (n = 82) | ||
| Maternal age | 0.27 | 0.016 |
| Married | 0.29 | 0.008 |
| Education level | 0.43 | <0.001 |
| WIC eligibility | −0.33 | 0.002 |
| Employed or student | 0.25 | 0.022 |
| Goal of any HM near discharge | 0.31 | 0.004 |
| Hispanic (n = 97) | ||
| Married | 0.30 | 0.003 |
| WIC eligibility | −0.26 | 0.011 |
| Goal of any HM near discharge | 0.33 | 0.001 |
| Black (n = 183) | ||
| Maternal age | 0.25 | 0.001 |
| Married | 0.15 | 0.050 |
| Education level | 0.31 | <0.001 |
| WIC eligibility | −0.35 | <0.001 |
| Employed or student | 0.17 | 0.023 |
| Plan to return to work or school | 0.20 | 0.007 |
| Goal of any HM near discharge | 0.29 | <0.001 |
Correlation coefficients: point-biserial, Spearman's rho, or phi as appropriate. Significance was set at p < 0.05.
Multivariate binary logistic regression analysis for racial/ethnic subgroups
Although neither support nor nonsupport of breastfeeding was correlated with HM feeding at discharge in subgroup analyses, the specific support person was included in subgroup multivariate logistic regressions because support by the mother's mother in the multivariate analysis was significant for the entire cohort. For black mothers, support from the mother's mother (OR 0.27 [95% CI 0.11–0.68], p = 0.006) and maternal goal of any HM near discharge (OR 25.80 [95% CI 4.27–155.71], p < 0.001) significantly predicted HM feeding at NICU discharge. For Hispanic mothers, maternal goal of any HM near discharge was a significant predictor of HM feeding at NICU discharge (OR 15.42 [95% CI 2.49–95.67], p = 0.003), while no significant factors were identified for white mothers.
Discussion
In our diverse urban cohort, the most significant predictor of HM feeding at NICU discharge was a maternal goal of any HM near discharge, a finding that was consistent for the entire cohort, racial/ethnic subgroups, and multiparous subjects. This finding agrees with previous research that has shown that predetermined goals or intent to provide HM is one of the strongest predictors of HM provision for mothers of both term and preterm infants.14,19,25,26 However, these studies vary in the timing for measurement of breastfeeding intent and range from once prenatally to serial measures over a longer interval.
In a review based on the Pregnancy Risk Assessment Monitoring System data from 2000 to 2003, predelivery breastfeeding intent was the strongest predictor of initiation, although the sample differed significantly from our study with the majority being white mothers of term infants.19 A separate study of primarily white mothers who received WIC benefits and completed a survey ≥6 months postdelivery found that prenatal intent was strongly associated with initiation, but not duration of breastfeeding. The study did not provide details about whether preterm births were excluded, the timing of maternal surveys, and may have been limited by recall bias.26 In a NICU study of mothers of term and preterm infants, mothers who provided HM for greater than 4 months postdischarge were twice as likely to have a preset plan to breastfeed compared to other mothers, although the timing for measurement of breastfeeding intent was not specified.14
A limitation in previous studies is the overall lack of consistency in the timing for measuring HM provision goals. Previous studies by our research team have found that mothers of VLBW infants change HM provision goals multiple times over the course of the NICU hospitalization.12 We recently reported that fewer black mothers of VLBW infants had a prenatal goal of HM provision, but changed this goal in the early postbirth period such that racial/ethnic differences disappeared by day of life 15. Furthermore, these HM provision goals continued to change over the NICU hospitalization with exclusive HM provision goals decreasing for all racial subgroups. However, in the last measured HM provision goal before NICU discharge, no racial/ethnic differences were noted and black mothers indicated that they wanted to continue to provide HM at rates comparable to non-black mothers. These findings highlight the dynamic nature of HM provision goals in mothers of VLBW infants and indicate that maternal goal-setting is not a static event. Thus, our study, which includes a median of three prospective HM provision goal measurements per mother, differs importantly from other research that has incorporated only a single measure, oftentimes assessed prenatally and retrospectively.
An unexpected finding in this study was that support for breastfeeding from the mother's mother was negatively associated with HM feeding at discharge for the entire cohort as well as for the black subgroup. Fabiyi et al. found that, while support may not have a significant effect on HM initiation in NICU mothers, lower levels of support were associated with lower HM expression as measured as a proportionate volume compared to mothers who had greater support.18 The support of family and friends, in particular, was associated with an increased frequency of HM expression17 and duration14 in mothers with infants in the NICU. In light of this conflicting literature, we were perplexed as to why, despite our subjects listing their mothers as a supportive person in their decision to provide HM, this support correlated negatively with HM feeding at discharge, especially in younger and unmarried mothers (data not shown). Although previous studies have examined the relationship between young mothers and their own mothers as it relates to stress and development of parenting skills, to our knowledge, these studies have included only populations of mothers of healthy term infants. For example, Arnold et al. found that a majority of women reported caregiving structures other than the infant's mother and father, with the most common pair being the mother and maternal grandmother.27 Mothers coparenting with their own mothers were more likely to experience parenting stress and child dysfunction compared to mothers coparenting with the father of the baby.
In a study looking at first-time, unmarried black mothers, intergenerational coresidence correlated with increasing stress for black mothers, whereas nonintergenerational households (still with intergenerational contact) were associated with decreasing stress.28 In addition, Black and Nitz examined a population of urban, low-income, first-time adolescent mothers residing with the maternal grandmother of the infant and found that the coresiding grandmother appeared to facilitate more support for the adolescent role (e.g., mothers were more likely to remain in school), than for the maternal role; thus suggesting that the support of the maternal grandmother was primarily directed toward facilitating the mother's growth and development.29
Similarly, literature specifically focused on black mothers of primarily term infants demonstrates that the opinion of the mother's mother is very important.30 While some black mothers report that their mothers encourage breastfeeding,31 others report the opposite experience with mothers disapproving of breastfeeding.32 An intergenerational factor specific to black women is the long-lasting impact and legacy of slavery that may negatively impact HM provision for black women as generations of black women were raised with limited breastfeeding role models or exposure to breastfeeding.32–35 This historical context may impact current mothers of VLBW infants, but the maternal grandmothers are even more likely to be influenced by this history, which may directly or subconsciously impact their role in supporting their daughters in providing HM. In addition, black mothers and/or maternal grandmothers may still positively associate formula with a sign of wealth and status.35,36 Interventions that seek to support young mothers may wish to focus on this complex relationship, with its benefits and challenges, between the infant's mother and maternal grandmother,27,37 especially when breastfeeding is not an experience that has been shared by the grandmother in her own parenting history.
In our cohort, WIC eligibility was a significant negative predictor of HM feeding at discharge, similar to other investigators that have demonstrated a negative effect of low-income status on HM provision.10,38 This relationship likely reflects an effect of economic status rather than a reflection of WIC lactation support because mothers in this study received intensive lactation care in the NICU where the study was conducted. Surprisingly, many other commonly accepted factors thought to predict HM feeding at discharge were not significant predictors in our cohort, including previous experience with breastfeeding,15,30 formula,16 or return to work/school.17 However, we collected only mothers' plans to return to work/school since we did not have confirmatory data to discern if mothers actually did or did not return to work/school for all subjects. In addition, maternal education15,18 and number of children in the home10 were not significant predictors for HM feeding at discharge. The lack of effect of maternal education is surprising, but may also have been partially due to an interaction between race/ethnicity and education, since Hispanic mothers were more likely to have less than high school education, but provided HM feeding at discharge at rates similar to white mothers. However, no effect of maternal education was detected in the racial/ethnic subgroup analyses. We speculate that the lack of impact of maternal education was partially mitigated by the intensive lactation care received by our study cohort in the NICU.
Limitations
A limitation of our study was that mothers were less likely to give definitive answers for persons who did not support their breastfeeding choice than those who did support their choice. Nonsupport may be more subtle and difficult to identify, yet may still negatively impact HM provision. Further limitations include that the measure of support involved the mother's perception of support as well as the fact that support was measured early in the immediate postbirth and represented a snapshot, not the dynamic nature of interpersonal relationships. A potential limitation is the time interval between the latest feeding goal and infant discharge, which on average was 1 month, but varied based on visitation patterns and timing of decision to exclusively feed formula. However, we anticipate that collecting feeding goals immediately before discharge would only strengthen the relationship between goals and HM feeding at discharge. Another limitation is the potential impact of maternal milk production on goal setting, in that mothers with lower milk volume may have lower HM feeding goals. This analysis was focused on social factors, but future studies will incorporate multiple categories of factors, including pumping and milk volume characteristics, which may impact HM feeding at discharge. Also, our data do not include information about nativity, which may affect breastfeeding initiation in low-income mothers, with greater initiation rates in immigrant mothers than U.S.-born mothers.39
Conclusions
This study adds value to the existing literature by examining non-NICU factors that may influence HM feeding at NICU discharge in VLBW infants. In our urban NICU with extensive in-NICU lactation care,40 many black mothers of VLBW infants did not meet their HM provision goals at the time of NICU discharge, despite exceptionally high initiation rates. We identified significant factors that merit further study, specifically maternal goals for HM provision, intergenerational relationships, and the social support networks resulting from these relationships. Future research should target interventions that focus on early, prepregnancy establishment and subsequent maintenance of HM feeding goals through to NICU discharge, with particular attention to black and/or economically disadvantaged women.
Acknowledgments
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R03HD081412. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure Statement
No competing financial interests exist.
References
- 1.National Center for Health Statistics, Final Natality Data. Very low birthweight by race/ethnicity: United States, 2011–2013. Available at www.marchofdimes.org/Peristats (accessed July22, 2015)
- 2.Vohr BR, Poindexter BB, Dusick AM, et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics 2006;118:e115–e123 [DOI] [PubMed] [Google Scholar]
- 3.Lee HC, Gould JB. Factors influencing breast milk versus formula feeding at discharge for very low birth weight infants in California. J Pediatr 2009;155:657–662.e1–e2 [DOI] [PubMed] [Google Scholar]
- 4.Schanler RJ, Shulman RJ, Lau C. Feeding strategies for premature infants: Beneficial outcomes of feeding fortified human milk versus preterm formula. Pediatrics 1999;103:1150–1157 [DOI] [PubMed] [Google Scholar]
- 5.Sisk PM, Lovelady CA, Dillard RG, et al. Early human milk feeding is associated with a lower risk of necrotizing enterocolitis in very low birth weight infants. J Perinatol 2007;27:428–433 [DOI] [PubMed] [Google Scholar]
- 6.Patel AL, Johnson TJ, Engstrom JL, et al. Impact of early human milk on sepsis and health care costs in very low birth weight infants. J Perinatol 2013;33:514–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson TJ, Patel AL, Bigger HR, et al. Cost savings of human milk as a strategy to reduce the incidence of necrotizing enterocolitis in very low birth weight infants. Neonatology 2015;107:271–276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stuebe AM. The risks of not breastfeeding for mothers and infants. Rev Obstet Gynecol 2009;2:222–231 [PMC free article] [PubMed] [Google Scholar]
- 9.Victora CG, Bahl R, Barros AJ, et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016;387:475–490 [DOI] [PubMed] [Google Scholar]
- 10.Sisk PM, Lovelady CA, Dillard RG, et al. Lactation counseling for mothers of very low birth weight infants: Effect on maternal anxiety and infant intake of human milk. Pediatrics 2006;117:e67–e75 [DOI] [PubMed] [Google Scholar]
- 11.Bigger HR, Fogg LJ, Patel A, et al. Quality indicators for human milk use in very low birth weight infants: Are we measuring what we should be measuring? J Perinatol 2014;34:287–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoban R, Bigger H, Patel AL, et al. Goals for human milk feeding in mothers of very low birth weight infants: How do goals change and are they achieved during the NICU hospitalization? Breastfeed Med 2015;10:305–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riley BS, Schoeny M, Rogers L, et al. Barriers to human milk feeding at discharge of VLBW infants: Evaluation of neighborhood structural factors. Breastfeed Med 2016;11:335–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Purdy IB, Singh N, Le C, et al. Biophysiologic and social stress relationships with breast milk feeding pre- and post-discharge from the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs 2012;41:347–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Briere CE, McGrath J, Cong X, et al. An integrative review of factors that influence breastfeeding duration for premature infants after NICU hospitalization. J Obstet Gynecol Neonatal Nurs 2014;43:272–281 [DOI] [PubMed] [Google Scholar]
- 16.Nommsen-Rivers LA, Chantry CJ, Cohen RJ, et al. Comfort with the idea of formula feeding helps explain ethnic disparity in breastfeeding intentions among expectant first-time mothers. Breastfeed Med 2010;5:25–33 [DOI] [PubMed] [Google Scholar]
- 17.Sisk PM, Quandt S, Parson N, et al. Breast milk expression and maintenance in mothers of very low birth weight infants: Supports and barriers. J Hum Lact 2010;26:368–375 [DOI] [PubMed] [Google Scholar]
- 18.Fabiyi C, Rankin K, Norr K, et al. The association of low social support with breast milk expression in low-income mother-preterm infant dyads. J Hum Lact 2015;31:490–497 [DOI] [PubMed] [Google Scholar]
- 19.Colaizy TT, Saftlas AF, Morriss FH., Jr. Maternal intention to breast-feed and breast-feeding outcomes in term and preterm infants: Pregnancy risk assessment monitoring system (PRAMS), 2000–2003. Public Health Nutr 2012;15:702–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li R, Fridinger F, Grummer-Strawn L. Public perceptions on breastfeeding constraints. J Hum Lact 2002;18:227–235 [DOI] [PubMed] [Google Scholar]
- 21.Patel AL, Johnson TJ, Robin B, et al. The direct and indirect influence of own mother's milk on bronchopulmonary dysplasia and costs. Arch Dis Child Fetal Neonatal Ed 2016. [Epub ahead of print]; DOI: 10.1136/archdischild-2016-310898 [DOI] [PMC free article] [PubMed]
- 22.Meier PP, Engstrom JL, Rossman B. Breastfeeding peer counselors as direct lactation care providers in the neonatal intensive care unit. J Hum Lact 2013;29:313–322 [DOI] [PubMed] [Google Scholar]
- 23.U.S. Department of Agriculture. WIC Income Eligibility Guidelines 2013–2014. Updated 2013. Available at http://origin.www.fns.usda.gov/wic/howtoapply/incomeguidelines.htm (accessed June30, 2014)
- 24.Jones KM, Power ML, Queenan JT, et al. Racial and ethnic disparities in breastfeeding. Breastfeed Med 2015;10:186–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sisk PM, Lovelady CA, Dillard RG, et al. Maternal and infant characteristics associated with human milk feeding in very low birth weight infants. J Hum Lact 2009;25:412–419 [DOI] [PubMed] [Google Scholar]
- 26.Dunn RL, Kalich KA, Fedrizzi R, et al. Barriers and contributors to breastfeeding in WIC mothers: A social ecological perspective. Breastfeed Med 2015;10:493–501 [DOI] [PubMed] [Google Scholar]
- 27.Arnold A, Lewis J, Maximovich A, et al. Antecedents and consequences of caregiving structure on young mothers and their infants. Matern Child Health J 2011;15:1037–1045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaskin-Butler VT, Engert T, Markievitz M, et al. Prenatal representations of coparenting among unmarried first-time African American mothers. Fam Process 2012;51:360–375 [DOI] [PubMed] [Google Scholar]
- 29.Black MM, Nitz K. Grandmother co-residence, parenting, and child development among low income, urban teen mothers. J Adolesc Health 1996;18:218–226 [DOI] [PubMed] [Google Scholar]
- 30.Reeves EA, Woods-Giscombe CL. Infant-feeding practices among African American women: Social-ecological analysis and implications for practice. J Transcult Nurs 2015;26:219–226 [DOI] [PubMed] [Google Scholar]
- 31.Furman LM, Banks EC, North AB. Breastfeeding among high-risk inner-city African-American mothers: A risky choice? Breastfeed Med 2013;8:58–67 [DOI] [PubMed] [Google Scholar]
- 32.Spencer B, Wambach K, Domain EW. African American women's breastfeeding experiences: Cultural, personal, and political voices. Qual Health Res 2015;25:974–987 [DOI] [PubMed] [Google Scholar]
- 33.Johnson A, Kirk R, Rosenblum KL, et al. Enhancing breastfeeding rates among African American women: A systematic review of current psychosocial interventions. Breastfeed Med 2015;10:45–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sublette C, Sublette N. The American Slave Coast: A History of the Slave-Breeding Industry. Chicago, IL: Chicago Review Press, 2015. [Google Scholar]
- 35.Asiodu I, Flaskerud J. Got milk? A look at breastfeeding from an African American perspective. Issues Ment Health Nurs 2011;32:544–546 [DOI] [PubMed] [Google Scholar]
- 36.Gross TT, Powell R, Anderson AK, et al. WIC peer counselors' perceptions of breastfeeding in African American women with lower incomes. J Hum Lact 2015;31:99–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sellers K, Black MM, Boris NW, et al. Adolescent mothers' relationships with their own mothers: Impact on parenting outcomes. J Fam Psychol 2011;25:117–126 [DOI] [PubMed] [Google Scholar]
- 38.Odom EC, Li R, Scanlon KS, et al. Reasons for earlier than desired cessation of breastfeeding. Pediatrics 2013;131:e726–e732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lee HJ, Ilo IT, McCollum KF, et al. Racial/ethnic differences in breastfeeding initiation and duration among low-income, inner-city mothers. Soc Sci Q 2009;90:1251–1271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meier PP, Patel AL, Bigger HR, et al. Supporting breastfeeding in the neonatal intensive care unit: Rush mother's milk club as a case study of evidence-based care. Pediatr Clin North Am 2013;60:209–226 [DOI] [PubMed] [Google Scholar]