Abstract
Introduction
Despite advances in treatment, head and neck cancer (HNC) patients often experience considerable functional impairment during and following treatment. As a result, family caregivers are essential in a patient’s recovery; however, few caregivers are well-prepared to handle the extensive caregiving needs of this patient population. To date, little is known about HNC caregivers’ informational needs in this role. Thus, we surveyed a sample of HNC caregivers about their informational needs including those related to interacting in the medical context as a caregiver and meeting patient needs. We also asked these caregivers their preferences for obtaining caregiving information.
Methods
We conducted a cross-sectional study of 59 family caregivers for HNC patients who had completed radiation therapy at a comprehensive cancer center.
Results
The majority of caregivers (74.6%) reported having high information need at diagnosis related to interacting as a caregiver. Although the need for such information decreased over time, over half still had a high need for information at treatment end. Importantly, caregivers who desired information about reducing patient pain and distress also reported having greater informational needs on issues related to interacting in the medical context. Further, the caregivers most often preferred to receive information from health care professionals as a first source. However, preferring an informal (e.g., Internet) resource at first was significantly associated with needing information on how to talk to a doctor or nurse.
Discussion
The development of evidence-based resources and tools for HNC caregivers as well as clinicians may help caregivers more effectively manage patient symptoms and warrants further attention. Further, Internet resources may represent an effective resource for providing caregivers with strategies toward enhancing communication with healthcare professionals.
Keywords: Head and neck cancer, caregiving, information seeking
Introduction
Head and neck cancer (HNC) and corresponding treatments result in substantial functional challenges for patients. Deficits in speech and swallowing are both highly prevalent and highly limiting for this population because of cancer symptoms and treatment-related side effects [1, 2]. Treatment can also result in impaired nutritional intake, pain, and psychological distress. Indeed, some HNC patients continue to experience pain despite ongoing pain management therapy [3]. And HNC patients tend to report poor psychological functioning, including high levels of anxiety and distress [4–7]. As a result, family caregivers fill essential roles in managing patient care and symptoms [8].
Despite the active role that HNC caregivers commonly assume, there is limited research on caregiver informational needs in the medical context. Available evidence suggests that communication is a particular area of concern for HNC caregivers. Specifically, knowing how to communicate with healthcare professionals was reported as a top concern in previous research of caregivers for HNC surgery patients [9], while a study involving caregivers of hospitalized HNC patients also noted concern with communicating in the medical context [8].
Properly integrating family caregivers during a patient’s health care visits can have positive implications for patients [10, 11]. For example, involvement of a family member at medical appointments has been shown to aid in medical decision-making [12]. And involving a relative during a patient’s medical care was associated with less aggressive medical care at the end of life, with aggressive care being associated with both poorer patient quality of life and higher caregiver bereavement [13]. Yet, to date, the practice of integrating caregivers in clinical settings varies due to concerns over patient privacy, time and reimbursement constraints with health professionals, and concern about patient autonomy or patient-caregiver disagreement on who ought to assume the role of treatment decision-maker [14].
In order to optimize caregiver engagement, it is essential to understand caregiver communication concerns in the medical context and their preferences for receiving information. Evidence shows that cancer caregivers have varied preferences for receiving information on caregiving [15–17], but this has not been fully explored among HNC caregivers.
In the present study, we explored HNC caregivers’ informational needs related to interacting in the medical setting as a caregiver, and whether greater needs were associated with concerns about managing patient pain or distress. We also explored how caregivers prefer to receive information relevant to providing care, and if informational needs were associated with such preferences. These descriptive findings will begin to shed light on how to best deliver information to HNC caregivers through preferred and targeted strategies.
Material and Methods
Participants
This cross-sectional study involved family caregivers for HNC patients who had completed radiation therapy at a comprehensive cancer center. A family caregiver was defined as the relative or friend who provided the patient with the most assistance. The Center’s Institutional Review Board (IRB) approved the study. Sixty-four caregivers consented to participate, with 59 (92.2%) completing the study survey.
Measurement
Caregiver Demographics
Key caregiver characteristics were collected including caregiver age, race/ethnicity, education level, gender, income, employment status, and the care recipient’s relationship to the caregiver (e.g., spouse/partner or other).
Patient Clinical Characteristics
Patient clinical data collected included HNC cancer site, American Joint Committee on Cancer stage, treatment regimens (e.g., receipt of chemotherapy, surgery), and time since diagnosis.
Informational Needs
Informational needs were measured using an abbreviated form of the Cancer Caregiver Needs Checklist [18]. Specifically, we asked each caregiver to respond if he or she desired information on five topics related to interacting in the medical context as a caregiver at diagnosis, start of treatment, and end of treatment (See Table 2 for the specific items). Similar to other research [9, 19], we categorized the number of needs among caregivers into low (0–2 needs) or high (3–5 needs). We also asked caregivers whether they needed information on “how to lessen a patient’s pain and distress” at diagnosis, treatment start and treatment end [18].
Resource Preferences
To establish resource preferences, caregivers were asked the following question: “If you were looking for information to help you take care of your friend or relative, where would you turn first?” Response options included: doctor; nurse or other health care professional; telephone service, Internet (including web-content); books, magazines, or other printed materials (excluding web-content); DVDs; church or religious organization; relative or friend; government agency; support group; hospital/clinic; non-profit or community organization; other (write in response); don’t know. Caregivers were asked to select one response. This question was adapted from a national survey of informal caregivers in the U.S. conducted in 2003 by the National Alliance for Caregiving and AARP [20]. We further categorized the responses into “formal” (doctor; nurse or other health care professional) and “informal” (all other responses above) resource preference. The caregivers were also asked: “Where else would you prefer to receive information about taking care of your friend or relative?” Response options were the same as above, but caregivers were instructed to check more than one response if needed.
Statistical Analyses
Descriptive statistics were used to characterize caregivers’ information needs and resource preferences for caregiving information. Chi-square analyses were used to evaluate potential associations between background variables and information needs and resources preferences as well the relationship between information needs and resources preferences.
Results
The caregivers (n=59) were primarily white (94.7%) and female (81.4%) with a mean age of 54.6 years (SD=12.7). See Table 1 for additional caregiver demographics. Primary cancer site for patients included oral cavity (49.2%), tonsilar (30.5%), nasopharynx (8.5%), larynx (6.8%), hypopharynx (1.7%), oropharynx (1.7%) and scalp (1.7%) cancer. In addition to radiation therapy, a majority of patients also received chemotherapy (71.2%), and 39% had undergone surgery. On average, caregivers completed the questionnaires approximately 16 months (mean 16.49, SD = 12.31) after a patient’s diagnosis.
Table 1.
Caregiver demographics and characteristics (N=59 unless noted)
| Variable | n (%) or Mean (± SD) |
|---|---|
| Mean Age | 54.6 (SD=12.7) |
| Education | |
| Trade school | 2 (3.4%) |
| High school graduate/GED | 26 (41.1%) |
| Some college | 11 (18.6%) |
| College graduate | 14 (23.7%) |
| Graduate degree | 6 (10.2) |
| Income (N=54) | |
| Less than $10,000 | 3 (5.5%) |
| 10,000–29,999 | 5 (9.2%) |
| 30,000–49,999 | 11 (20.3%) |
| 50,000–64,999 | 8 (14.8%) |
| Above 65,000 | 27 (50%) |
| Employment Status | |
| Employed | 36 (61%) |
| Unemployed | 5 (8.5%) |
| Retired | 14 (23.7%) |
| Student | 1 (1.7%) |
| Full-time homemaker | 3 (5.1%) |
| Race (N=57) | |
| African American | 1 (1.8%) |
| Asian | 2 (3.5%) |
| Caucasian/white | 54 (94.7%) |
| Gender | |
| Female | 48 (81.4%) |
| Male | 11(18.6) |
| Caregiver’s relationship to patient | |
| Spouse | 45 (76.3%) |
| Adult Child | 13 (22.1%) |
| Adult Grandchild | 1 (1.7%) |
Caregiver Informational Needs
At least 50% of the caregivers reported 3 or more information needs related to interacting in the medical setting as a caregiver at each time point, including diagnosis (74.6%), treatment start (66.1%), and treatment end (50.8%). The average need for information decreased across the time points, including diagnosis (3.39, SD=.195), treatment start (3.07, SD=.204), and treatment end (2.49, SD=.229) at (F (2, 116); 10.61, p=.000). Post hoc analyses indicate that communication needs differed significantly from diagnosis to treatment end (p < .001) and from treatment start to treatment end (p = .003) but not from diagnosis to treatment start. No background variables were significantly associated with having more information needs at any time point.
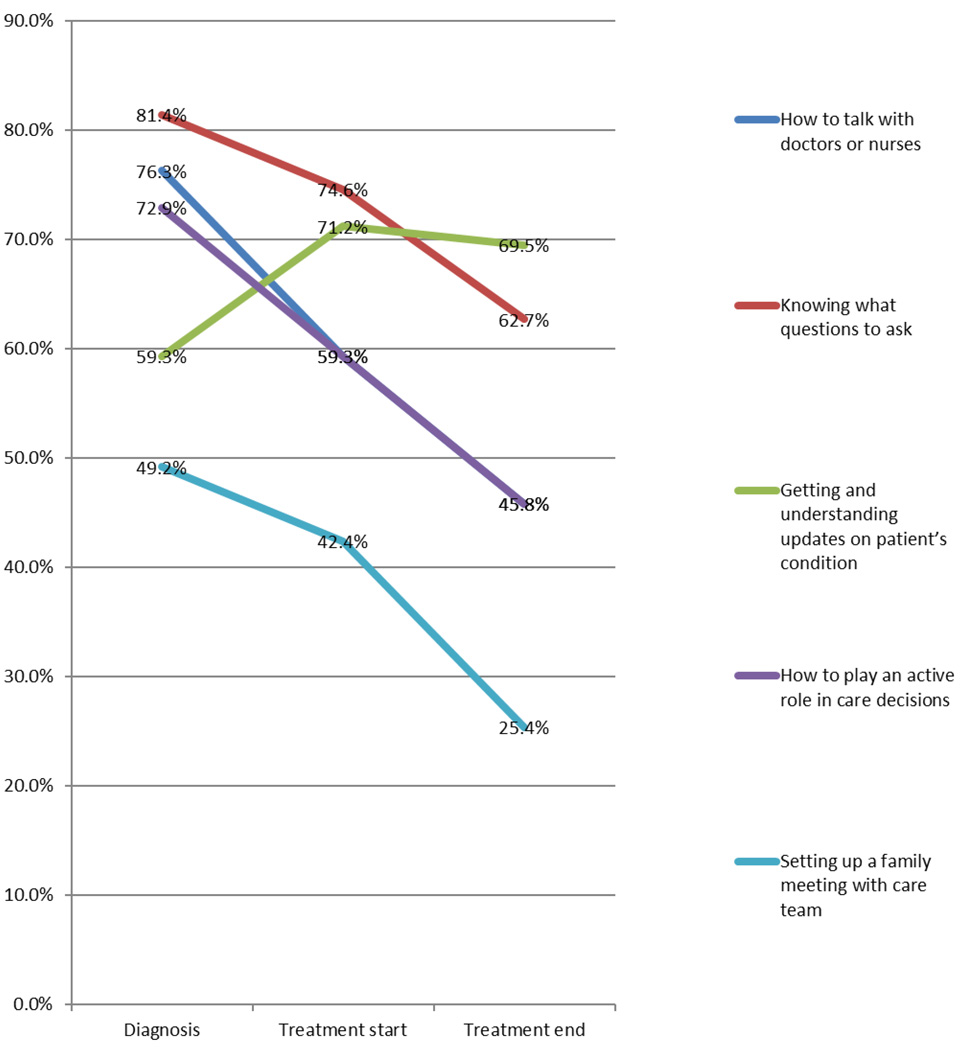
Figure 1 describes the HNC caregivers’ responses to individual items at diagnosis, treatment start and treatment end. Of the background variables, employment and relationship status were significantly associated with certain items. Specifically, a higher percentage of employed caregivers reported needing information on how to get updates on a patient’s condition at diagnosis (72.2%, n=36) and treatment start (86.1%, n=36) time points compared to those who were not employed (39.1%, n=23, χ2(1) =6.37, p=.016; 47.8% (n=23), χ2(1)=10.02, p=.003; respectively). Further, a higher percentage of non-spouse caregivers (93.3%, n=15) needed information at diagnosis on how to play an active role in care decisions compared to spouse/partner caregivers (65.9%, n=44; χ2(1)=4.26, p=.048).
Figure 1.
Percent of caregivers (n=59) indicating a specific need for information per time point.
Informational needs and reducing patient concerns
A high percentage of caregivers reported needing information on how to reduce a patient’s pain or distress at diagnosis (66.1%), treatment start (74.6%), and at treatment end (44.1%). Having greater needs related to interacting in the medical context as a caregiver was associated with the need for information related to reducing pain or distress of a patient. A significantly higher proportion of caregivers with greater medical communication-related information needs (3–5 needs) reported needing information about how to lessen patient pain or distress at diagnosis (75%; n=44, χ2(1)=6.12, p = 0.025), treatment start (84.6%, n=39; χ2(1)=6.12, p = 0.025), and treatment end (60%, n=30, χ2(1)=6.29, p = 0.018) compared to caregivers with low medical interaction-related information needs (0–2) [40%, n=15; 55%, n=20; 27.6%, n=29, respectively].
Caregiver Resource Preferences
A majority of the caregivers reported that they would first seek caregiving information from a formal health care professional (doctor, nurse, or social worker) (76.6%, n=47), while 23.4% reported that they would first go to an informal resource (e.g., Internet, family or friend, non-profit). Among these caregivers who reported that a formal source would be their initial resource for caregiving information (n=36), the Internet (36.1%) was most frequently reported as the secondary or additional informal resource. Preference for the Internet was followed by caregiving information from a support group (22.2%), a relative or friend (25%), print materials (13.9%), a non-profit organization (8.3%), a church or religious group (11.1%), a telephone service (8.3%), DVDs (5.6%), and a government agency (5.6%). Among caregivers who noted a preference to go first to an informal information source (i.e., Internet, family or friend, or non-profit) (n=11), 54.5% indicated they would seek additional information from a doctor and 63.6% from another health professional. Having more information needs related to interacting in the medical context was not associated with a specific resource preference for caregiving information. However, a significantly higher percentage of caregivers reporting a preference for an informal resource preference as their first resource (100%, n=11) indicated a need for information on how to talk to a doctor or nurse than those who indicated a preference for a formal resource (66.7%, n=36; χ2(1)= 4.92, p=.044). No other specific item or background variable was associated with resource preference.
Discussion
A high and consistent need for information on interacting in the medical context was evident across the caregiving trajectory in this sample of HNC caregivers. At least one out of every two caregivers reported needing information on 3 or more topics related to interacting in the medical context at diagnosis, treatment start, and treatment end. Though such needs did decrease from diagnosis to treatment end, no significant difference was noted from diagnosis to treatment start. This presents at least two clinical interactions, potentially covering topics such as treatment decision-making and symptom management, in which some caregivers might have been unsure of how to effectively communicate or interact in the medical context.
Effectively involving a caregiver in the care of an older adult has been shown to improve outcomes, such as patient quality of life and caregiver adjustment. Findings from this sample of HNC caregivers show a significant association between needing information on interacting in the medical context as a caregiver and needing information on how to reduce a patient’s pain or distress. A greater proportion of those with a high number of medical interaction-related information needs (i.e., 3–5) reported needing information on how to reduce a patient’s pain and distress compared to those reporting fewer medical communication-related information needs. As such, having more questions related to how to communicate in the medical context as a caregiver could adversely impact a caregiver’s ability to assist a patient at home. It is important further explore this potential association longitudinally and among a larger sample of HNC caregivers, including incorporating specific patient outcomes. Providing caregivers with education on how to communicate or interact in the medical context as a caregiver might lead to improved caregiver and patient outcomes. In recent decades, attention has focused on efforts to improve doctor-patient communication, believing that such improvements would improve quality of care and patient outcomes [21]. Likewise, efforts geared also to caregivers may aid in improving clinical interactions and contribute to improved patient outcomes, and should be further explored.
In addition to educating caregivers, training clinicians on how to incorporate a caregiver might also be beneficial. Though more research is needed, findings from this research suggest that simply asking caregivers questions during a medical interaction might be helpful. Specifically, given the finding that employment status was associated with needing information on how to get updates on a patient’s condition, clinicians may need to query employed caregivers regarding: “What is the best way to update you on the patient’s condition based on your work schedule?” Or, for non-spouse caregivers, asking at patient diagnosis “how can we [doctors or nurses] best help you carry out this role?” Tailoring communication to the caregiver may improve his or her comfort level and ultimately make for better information processing toward the benefit of the patient.
The findings also highlight a potentially important disconnect in that a majority of caregivers preferred to receive information from formal health care professionals, but also report needing information on how to interact in the medical context. Further, a higher percentage of those who reported that they would first go to an informal resource reported needing information on how to talk to a doctor at diagnosis compared to those who would first go to a health care professional. Using informal resources, such as the Internet, might be an effective strategy to teach caregivers how to communicate in the medical context (e.g., education or modeling on how to talk to a doctor; what questions to ask; how to take an active role as a caregiver). Future research with larger samples should explore strategies for enhancing the communication between caregivers and healthcare professionals as well as providing complementary resources.
Limitations
This cross-sectional research provides an important first step in understanding the medical communication-related information needs and resource preferences of HNC caregivers. However, there are several limitations of this research. The information needs checklist is a retrospective assessment requiring the caregiver to reflect back on earlier stages in the care process and the reliance on memory could be problematic given the potential stress of caregiving. Further, the sample size is modest and may not be representative of the caregivers of HNC patients in general. Similarly, the sample lacked diversity in gender and race/ethnicity, and thus, future research on caregiver communication needs across a diverse sample is warranted.
Conclusion
This research highlights areas of need for information related to interacting in the medical context for a sample of HNC caregivers, and the potential adverse consequence lacking information might have on being equipped to reduce patient concerns. Future research should explore how best to educate and engage caregivers and clinicians on effective patient-caregiver-healthcare provider interactions. This might include the development of a tool kit for enhancing caregiver-clinician communication, particularly among the subgroup of caregivers identified as experiencing the highest needs.
Acknowledgments
This work was funded through National Institute of Health grants R41CA144100 and P30CA006927.
Footnotes
Conflict of Interest
The author(s) declared no conflicts of interest with respect to the authorship and/or publication of this article.
References
- 1.Murphy BA, et al. Quality of life research in head and neck cancer: a review of the current state of the science. Crit Rev Oncol Hematol. 2007;62(3):251–267. doi: 10.1016/j.critrevonc.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Ronis DL, et al. Changes in quality of life over 1 year in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg. 2008;134(3):241–248. doi: 10.1001/archoto.2007.43. [DOI] [PubMed] [Google Scholar]
- 3.Epstein JB WD, Fischer DJ, Kim YO, Villines D. Neuropathic and nociceptive pain in head and neck cancer patients receiving radiation therapy. Head Neck Oncol. 2009;1:26. doi: 10.1186/1758-3284-1-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hammerlid E, A-E M, Bjordal K, Biörklund A, Evensen J, Boysen M, Jannert M KS, Sullivan M, Westin T. A prospective multicentre study in Sweden and Norway of mental distress and psychiatric morbidity in head and neck cancer patients. Br J Cancer. 1999;80(5–6):766–774. doi: 10.1038/sj.bjc.6690420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen SC, et al. Distress and care needs in newly diagnosed oral cavity cancer patients receiving surgery. Oral Oncol. 2009;45(9):815–820. doi: 10.1016/j.oraloncology.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Gil F CG, Hilker I, Benito L. First anxiety, afterwards depression: psychological distress in cancer patients at diagnosis and after medical treatment. Stress Health. 2012;28(5):362–367. doi: 10.1002/smi.2445. [DOI] [PubMed] [Google Scholar]
- 7.Henry M HL, Morrison M, Yang JW, Li XJ, Lin S, Zeitouni A, Payne R, MA Macdonald C, Kost K, Black M, Hier M. Head and neck cancer patients want us to support them psychologically in the posttreatment period: Survey results. Palliat Support Care. 2013:1–13. doi: 10.1017/S1478951513000771. [DOI] [PubMed] [Google Scholar]
- 8.Rodriguez CS, Blischak DM. Communication needs of nonspeaking hospitalized postoperative patients with head and neck cancer. Appl Nurs Res. 2010;23(2):110–115. doi: 10.1016/j.apnr.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Chen SC, et al. Unmet supportive care needs and characteristics of family caregivers of patients with oral cancer after surgery. Psycho-Oncology. 2014 doi: 10.1002/pon.3458. [DOI] [PubMed] [Google Scholar]
- 10.IOM. Retooling for an aging America: Building the health care workforce. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 11.Glajchen M. The emerging role and needs of family caregivers in cancer care. J Support Oncol. 2004;2(2):145–155. [PubMed] [Google Scholar]
- 12.Clayman ML, et al. Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Soc Sci Med. 2005;60(7):1583–1591. doi: 10.1016/j.socscimed.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Wright AA, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shin DW, et al. Preferences for and experiences of family involvement in cancer treatment decision-making: patient-caregiver dyads study. Psychooncology. 2013;22(11):2624–2631. doi: 10.1002/pon.3339. [DOI] [PubMed] [Google Scholar]
- 15.Longacre ML. Cancer caregivers information needs and resource preferences. J Cancer Educ. 2013;28(2):297–305. doi: 10.1007/s13187-013-0472-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basch EM, et al. Use of information resources by patients with cancer and their companions. Cancer. 2004;100(11):2476–2483. doi: 10.1002/cncr.20261. [DOI] [PubMed] [Google Scholar]
- 17.James N, et al. A study of information seeking by cancer patients and their carers. Clin Oncol (R Coll Radiol) 2007;19(5):356–362. doi: 10.1016/j.clon.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 18.DuBenske LL, et al. Caregivers' differing needs across key experiences of the advanced cancer disease trajectory. Palliat Support Care. 2008;6(3):265–272. doi: 10.1017/S1478951508000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fang CY, et al. Informational needs of head and neck cancer patients. Health Technol (Berl) 2012;2(1):57–62. doi: 10.1007/s12553-012-0020-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Alliance for Caregiving & AARP. Caregiving in the U.S. 2004 [Google Scholar]
- 21.Bredart A, Bouleuc C, Dolbeault S. Doctor-patient communication and satisfaction with care in oncology. Curr Opin Oncol. 2005;17(4):351–354. doi: 10.1097/01.cco.0000167734.26454.30. [DOI] [PubMed] [Google Scholar]