Abstract
Background:
Patients with functional dyspepsia (FD) may use specific coping strategies. Hence, the aim of the present study was to compare cognitive emotion regulation strategies in FD patients and healthy controls.
Materials and Methods:
This was a descriptive observational study. The sample consisted of 86 individuals, 43 of whom were patients diagnosed with FD. The patients referred to the psychosomatic disorders clinic, Isfahan, Iran. The comparative sample included 43 healthy controls (without digestive diagnoses) matched with the patients by age and gender. Subjects completed data on demographic factors and cognitive emotion regulation questionnaire.
Results:
The results indicated that there are significant differences between patients with FD and healthy controls according to using cognitive strategies. Scores of healthy controls in positive reappraisal and acceptance were significantly more than FD patients, and inversely, scores of FD patients in rumination and other-blame were meaningfully more than healthy controls.
Conclusion:
FD patients apply less adaptive strategies and more maladaptive strategies. It is seemed psychological interventions that focus on reducing maladaptive strategies and increasing adaptive strategies could be effective for FD patients.
Keywords: Cognitive emotion regulation strategies, functional dyspepsia, healthy controls
INTRODUCTION
Functional dyspepsia (FD), also called non ulcer dyspepsia is a gastric disorder relating to the large spectrum of functional gastrointestinal disorders (FGIDs).[1] Its symptoms based on ROME III criteria are bothersome postprandial fullness, epigastric pain, epigastric burning, early satiation, as well as no evidence of structural diseases that is, likely to explain the symptoms.[2] Several factors influence the nature and intensity of FD symptoms, such as the social environment (psychosocial stressors), behavioral features, cognitive competences, coping styles, comorbid psychological disorders.[3] In spite of the fact that no unique psychological or personality profile has been found in FD patients,[4] never less, studies have revealed that FD patients in comparison with healthy controls have shown high scores in the subscales of stress, behavior Type A, coping styles, depression, anxiety, neuroticism, somatization.[4,5] Furthermore, psychosocial stress, mood symptoms, and coping styles are predictors of FD.[5] Indeed, these show that FD may associates to various emotional problems or disorders. Emotional disorders involve failures in emotion regulation.
Emotion regulation refers to how we try to influence which emotions we have when we have them, and how we experience and express these emotions.[6] Many processes are involved in decreasing, maintaining, or increasing one or more aspects of emotion,[7] including, situation selection, situation modification, attentional deployment, cognitive changes and response modulation.[8] Emotion regulation has been divided into two aspects, antecedent-focused emotion regulation occurs before the emotion is generated, and response-focused emotion regulation occurs after the emotion is generated.[6,9] Moreover, emotion regulation strategies have been classified as adaptive and maladaptive. Adaptive strategies (i.e., perspective, reappraisal, behavioral activation, positive refocusing, social support, planning, benefit finding) are associated with higher mood ratings than the use of maladaptive strategies (i.e., rumination, self-blame, other-blame, substance use, expressive suppression, emotional suppression, denial, nonsuicidal self-injury).[10] The regulation of emotions through cognitions is inextricably associated with human life and helps to manage emotions after the experience of stressful events.[11] Nine cognitive strategies are recognized via the cognitive emotion regulation questionnaire (CERQ); each referring to what someone thinks after the encounter with negative events.[12] The cognitive emotion regulation is an important part of the coping strategies.[13]
As above said, coping responses is another psychological factor that influence FD symptoms. It has been showed that lack of the effective coping is characteristic of patients with FD.[14] They may apply a different coping pattern that is related to their elevated level of anxiety[15] or other emotional problems. Since FD is considered as a chronic disease and psychosocial difficulties arise secondarily from chronic digestive symptoms, it is assumed that FD patients may use specific cognitive strategies. Hence, it is important to study these strategies in the patients. Hence, the aim of the present study was to compare cognitive emotion regulation strategies in FD patients and healthy controls.
MATERIALS AND METHODS
Study design and participants
This was a descriptive observational study. The sample consisted of 86 individuals, 43 of whom were patients diagnosed with FD (without comorbidity with other FGIDs) based on Rome III criteria by gastroenterologists. Rome III criteria for FD are bothersome postprandial fullness, epigastric pain, epigastric burning, early satiation, as well as no evidence of structural diseases that is likely to explain the symptoms. The patients referred to the psychosomatic disorders clinic, Isfahan, Iran. The comparative sample included 43 healthy controls (without digestive diagnoses) matched with the patients by age and gender. For ethics, the researcher assures o patients that their information will remain confidential.
Variable assessment
In the current study, demographic factors included age, gender, marital status and educational level.
The multidimensional CERQ was constructed to define what someone thinks after the experience of threatening or stressful events. The CERQ comprises nine conceptually distinct subscales: Acceptance, putting into perspective, positive refocusing, planning refocusing, positive reappraisal, catastrophizing, rumination, self-blame and other-blame. The CERQ has 18 items that must be measured on a 5-point Likert scale ranging from 1 (almost never) to 5 (almost always). A score of each subscale can be obtained by summing the scores of items belonging to the particular subscale. The higher the subscale score, the more the specific cognitive strategy is used.[16] A short 18-item version of the CERQ has 2-item subscales.[17] In assessing validity and reliability, the Persian version of CERQ-18 has had good psychometric features. Cronbach's alpha coefficients have been estimated for the subscales ranging from 0.68 (acceptance) to 0.82 (planning refocusing).[18]
Statistical analysis
Descriptive analysis was indicated as a mean and standard deviation. Wilcoxon analysis was performed to compare cognitive emotion regulation strategies in FD patients and healthy controls. The Statistical Package for the Social Sciences version 15.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analyzes.
RESULTS
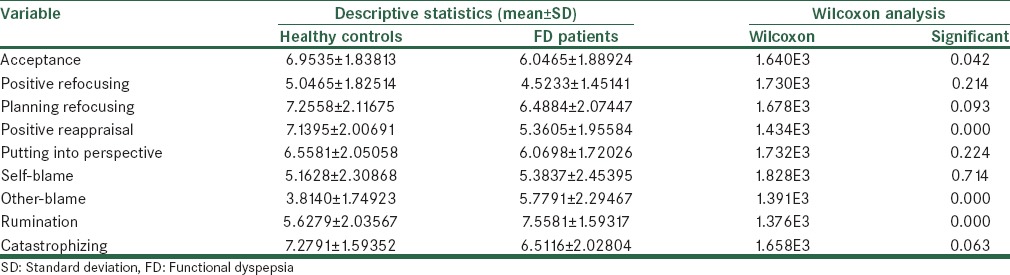
In the study, 43 patients (mean age = 33.72 ± 10.73; 79.1% female, 72.1% married, 35.7% graduated), and 43 healthy controls (mean age = 30.83 ± 7.68; 79.1% female, 55.8% married, 74.4% graduated) were examined. The results obtained for both FD and healthy groups are illustrated as descriptive data in Table 1. The mean of the two groups showed that the scores of all adaptive cognitive strategies in healthy controls were greater than patients with FD.
Table 1.
Descriptive statistics and Wilcoxon analysis of cognitive strategies in FD and healthy groups
In Figure 1, the cognitive strategies in both functional dyspepsia patients and healthy controls in terms of the mean are shown.
Figure 1.

Cognitive strategies in both FD patients and healthy controls in terms of the mean
Due to nonestablishing of the assumptions of normality of data distribution and homogeneity of variances, for comparison of FD patients and healthy controls in term of cognitive emotion regulation strategies, Wilcoxon analysis method was used.
The results of Wilcoxon analysis, which are also illustrated in Table 1, indicated that there are significant differences between patients with FD and healthy controls. In relation to adaptive strategies of positive reappraisal (P < 0.01) and acceptance (P < 0.05), scores of healthy controls were more than FD patients, and inversely, in relation to maladaptive strategies of rumination (P < 0.01) and other-blame (P < 0.01), scores of FD patients were more than healthy controls. Unexpectedly, catastrophizing as a maladaptive strategy was more in healthy controls, but it was not significant.
DISCUSSION
Based on the purpose of the research, we compared cognitive emotion regulation strategies in FD patients and healthy controls. The results showed that FD patients utilize significantly two maladaptive strategies of rumination and other-blame more than healthy controls, and reversely, healthy individuals apply adaptive strategies especially positive reappraisal and acceptation more than the patients. The possible explanation is that these differences could emerge from some personality characteristics of the patients, co morbidity of emotional problems (e.g., stress), and the chronic nature of the disease. In general, the findings are in line with the findings showing us that there are a relationship between emotion regulation strategies and psychopathological symptoms.[12,13,16,19,20,21,22]
Maladaptive strategies may lead to emotional turbulence in individuals under stress that make recovery more difficult.[23] Patients with psychological problems tend to focus more on their emotional experience and ruminate more on sadness than healthy individuals.[15] Some studies have shown that rumination increases negative mood-congruent thinking, interferes with problem-solving and useful behavior and repels social support.[24] According to the metacognitive model, rumination causes emotional dysfunction and pathology and have more extensive deleterious effects associated with elaboration of self-knowledge and blocking adaptive restructuring.[25] So, to escape their aversive self-awareness, some people who ruminate may turn to other symptoms[26] such as somatic symptoms that may conduce to FD.
In addition, other-blame has found to be correlated with psychological[13,19,21] and somatic symptoms.[1] It has been indicated that other-blame and projection are mostly coping strategies applied amongst Iranian. In fact, Iranians do not seem to relate the adverse events to their own responsibility. This probably stems from the idea that the distress is not necessarily under their control and receives influence from other sources.[13] Hence, the existence of psychological problems in FD patients may causes they use more other-blame strategy.
Vice versa, adaptive strategies lead to better emotional and health outcomes.[20] Positive reappraisal that refers to thoughts of creating a positive meaning to the event in terms of personal growth,[15] substitute the actual emotionally painful event with positive and pleasant thoughts or in a sense, linking a positive meaning to what occurred.[27,28] Thus, positive reappraisal to be negatively related to psychopathology.[13,16,21,23] Martin and Dahlen found that positive reappraisal is the most valuable predictors of negative emotions.[22]
Furthermore, it has been shown that acceptance is negatively related to negative emotions.[23] Acceptance strategies, referring to thoughts of accepting and resigning with regard to what have experienced or happened,[21] are especially effective in increasing pain tolerance. It can change the way of responding to pain related thoughts and feelings and offer a broader area of behavior, that is, to say tolerating painful stimulation longer.[29] FD patients perceive their experienced stressors as more uncontrollable and as having a greater impact. Hence, they use less acceptance strategy when handling stressful life event.[15]
The symptom that FD patients often complain to is a pain; therefore the way they manage it is important and highly influences the outcome of the disease.[1] Adaptive strategies (i.e., acceptance and positive reappraisal) are effective in decreasing pain intensity and negative affect.[29] The efficacy in emotion regulation relates to the quality of life and reduced negative affect even after controlling for effects of pain coping efficacy and pain coping. So, emotion regulation capacities may have a unique role in the prediction of specific aspects of adjustment among people with chronic pain.[30]
In general, our study showed that FD patients apply less adaptive strategies. According to Heiy, using at least one adaptive strategy, whether that is, with or without the additional use of a maladaptive strategy, is associated with considerably higher mood ratings than events in which no adaptive strategy was used. This suggests that it may be more advantageous to focus on increasing adaptive strategy use rather than decreasing or eliminating maladaptive strategies.[10] On the other hand, the patients had relatively higher scores in most of the maladaptive strategies than healthy individuals. Strategies of rumination and other-blame may overcome patients’ attempts to apply adaptive strategies such as reappraisal or acceptance, because it has been suggested that the use of maladaptive strategies might play a more central role in psychopathology than the nonuse of adaptive strategies. In fact, the adaptive strategies have showed weaker relationships with psychopathology symptoms than the maladaptive strategies.[24] Hence, it is seemed psychological interventions that focus on reducing maladaptive strategies and increasing adaptive strategies could be effective for FD patients.
There are several limitations in this study. This is a cross-sectional analysis; therefore, we cannot determine causality. Other limitations are that variables scores were based on self-report measures and sampling was not based on simple random because limited statistical population. Hence, we should be cautious in generalizing the findings. In addition, other social factors that may affect digestive diseases have been overlooked.
CONCLUSION
FD patients apply less adaptive strategies and more maladaptive strategies. It is seemed to be psychological interventions that focus on reducing maladaptive strategies (e.g., mindfulness based stress reduction, mindfulness integrated cognitive behavior therapy) and increasing adaptive strategies (e.g., emotion-focused cognitive behavioral therapy, acceptance and commitment therapy) could be effective for FD patients. Thus, it is probably that we can decrease or improve symptoms of FD patients.
Financial support and sponsorship
This work was supported by Psychosomatic Research Center of Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We wish to thank Psychosomatic Research Center of Isfahan University of Medical Sciences who supported this work and also all patients who participated in our study.
REFERENCES
- 1.Micut R, Tanasescu MD, Dragos D. A review of the psychoemotional factors in functional dyspepsia. Rev Med Rom. 2012;60:278–86. [PMC free article] [PubMed] [Google Scholar]
- 2.Drossman DA, Corazziari E, Delvaux M, Spiller RC, Talley NJ, Thompson WG, et al. Rome III: The Functional Gastrointestinal Disorders. 3rd ed. Virginia: Degnon Associates; 2006. [Google Scholar]
- 3.Budavari AI, Olden KW. Micut R, Tanasescu MD, Dragos D, editors. Psychosocial aspects of functional gastrointestinal disorders. A review of the psychoemotional factors in functional dyspepsia. Rev Med Rom. 2012;60:278–86. [Google Scholar]
- 4.Ringel Y, Drossman DA. Functional Dyspepsia. UNC Center for Functional GI and Motility Disorders. 2015. [Last accessed on 2015 Sep 16]. Available from: https://www.med.unc.edu/ibs/files/educational-gi handouts .
- 5.De la Roca-Chiapas JM, Solís-Ortiz S, Fajardo-Araujo M, Sosa M, Córdova-Fraga T, Rosa-Zarate A. Stress profile, coping style, anxiety, depression, and gastric emptying as predictors of functional dyspepsia: A case-control study. J Psychosom Res. 2010;68:73–81. doi: 10.1016/j.jpsychores.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Gross JJ. The emerging field of emotion regulation: An integrative review. Rev Gen Psychol. 1998;2:271–99. [Google Scholar]
- 7.Gross JJ. Emotion regulation in adulthood: Timing is everything. Curr Dir Psychol Sci. 2001;10:214–9. [Google Scholar]
- 8.Gross JJ. In: Emotion regulation. Handbook of Emotion. 3rd ed. 31. Lewis M, Haviland-Jones JM, Feldman Barrett L, editors. New York: The Guilford Press; 2008. pp. 497–512. [Google Scholar]
- 9.Gross JJ, Munoz RF. Emotion regulation and mental health. Clin Psychol (N Y) 1995;2:151–64. [Google Scholar]
- 10.Heiy JE. Emotion Regulation Flexibility: An Exploration of the Effect of Flexibility in Emotion Regulation on Mood. Thesis of MA: The Ohio State University; 2010. [Google Scholar]
- 11.Garnefski N, Kraaij V, Spinhoven PH. Garnefski N, Kraaij V, editors. Negative life events, cognitive emotion regulation and depression. Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Pers Individ Dif. 2006;40:1659–69. [Google Scholar]
- 12.Garnefski N, Koopman H, Kraaij V, ten Cate R. Brief report: Cognitive emotion regulation strategies and psychological adjustment in adolescents with a chronic disease. J Adolesc. 2009;32:449–54. doi: 10.1016/j.adolescence.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Oftadehal M, Mahmoodi-Kahriz B, Torrabinami M. Cognitive emotion regulation, depression and stress in Iranian students. Neurosci Res Lett. 2012;3:44–7. [Google Scholar]
- 14.Wrzesinska MA, Kocur J. The assessment of personality traits and coping style level among the patients with functional dyspepsia and irritable bowel syndrome. Psychiatr Pol. 2008;42:709–17. [PubMed] [Google Scholar]
- 15.Cheng C, Hui WM, Lrtdam SK. Coping style of individuals with functional dyspepsia. Psychosom Med. 1999;61:789–95. doi: 10.1097/00006842-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Garnefski N, Teerds J, Kraaij V, Legerstee J, van den Kommer T. Cognitive emotion regulation strategies and depressive symptoms: Differences between males and females. Pers Individ Dif. 2004;36:267–76. [Google Scholar]
- 17.Garnefski N, Kraaij V. Cognitive emotion regulation questionnaire – Development of a short 18-item version (CERQ-short) Pers Individ Dif. 2006;41:1045–53. [Google Scholar]
- 18.Hassani J. The evaluation of validity and reliability cognitive emotion regulation questionnaire short form. J Behav Sci. 2011;9:229–40. [Google Scholar]
- 19.Abdi S, Babapoor J, Fathi H. Relationship between cognitive emotion regulation styles and general health among university students. JAUMS. 2011;8:258–65. [Google Scholar]
- 20.Garnefski N, Kraaij V. The cognitive emotion regulation questionnaire. Eur J Psychol Assess. 2007;23:141–9. [Google Scholar]
- 21.Garnefski N, Kraaij V. Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Pers Individ Dif. 2006;40:1659–69. [Google Scholar]
- 22.Martin RC, Dahlen ER. Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Pers Individ Dif. 2005;39:1249–60. [Google Scholar]
- 23.Wang Y, Yi J, He J, Chen G, Li L, Yang Y, et al. Cognitive emotion regulation strategies as predictors of depressive symptoms in women newly diagnosed with breast cancer. Psychooncology. 2014;23:93–9. doi: 10.1002/pon.3376. [DOI] [PubMed] [Google Scholar]
- 24.Aldao A, Nolen-Hoeksema S. Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behav Res Ther. 2010;48:974–83. doi: 10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 25.Bahrami F, Kasaei R, Zamani A. Preventing worry and rumination by induced positive emotion. Int J Prev Med. 2012;3:102–9. [PMC free article] [PubMed] [Google Scholar]
- 26.Heatherton TF, Baumeister RF. Aldao A, Nolen-Hoeksema S, editors. Binge eating as escape from self-awareness. Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behav Res Ther. 2010;48:974–83. doi: 10.1016/j.brat.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 27.Carver CS, Scheier MF, Weintraub JK. Oftadehal M, Mahmoodi-Kahriz B, Torrabinami M, editors. Assessing coping strategies: A theoretically based approach. Cognitive emotion regulation, depression and stress in Iranian students. Neurosci Res Lett. 2012;3:4–7. [Google Scholar]
- 28.Spirito A, Stark LJ, Williams C. Oftadehal M, Mahmoodi-Kahriz B, Torrabinami M, editors. Development of a brief coping checklist for use with pediatric populations. Cognitive emotion regulation, depression and stress in Iranian students. Neurosci Res Lett. 2012;3:4–7. [Google Scholar]
- 29.Kohl A, Rief W, Glombiewski JA. How effective are acceptance strategies. A meta-analytic review of experimental results? J Behav Ther Exp Psychiatry. 2012;43:988–1001. doi: 10.1016/j.jbtep.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 30.Agar-Wilson M, Jackson T. Are emotion regulation skills related to adjustment among people with chronic pain, independent of pain coping? Eur J Pain. 2012;16:105–14. doi: 10.1016/j.ejpain.2011.05.011. [DOI] [PubMed] [Google Scholar]


