Abstract
Multiple primary malignancy is defined as two or more malignancies detected in an individual person. In particular, synchronous quintuple primary malignancy is extremely rare. A 52-year-old male with anal pain and intermittent blood-tinged stool was diagnosed with malignancies in the stomach, jejunum, ascending colon, transverse colon and rectum. He underwent a subtotal gastrectomy, segmental resection of the jejunum and total protocolectomy with end ileostomy. The postoperative pathologic findings were moderate differentiated gastric adenocarcinoma (pT1bN0M0, pStageIA), combined adenocarcinoma and neuroendocrine carcinoma of the jejunum (pT3N0M0, pStageIIA), three mucinous adenocarcinoma of the ascending colon (pT3N0M0, pStageIIA), transverse colon (pT1N0M0, pStageI) and rectum (pT3N1aM0, pStageIIIB). The tumors did not lack MLH-1 and MSH-2 expression, as the markers (bat26, D5S346, bat25, D2S123) suggest MSI-H presence. Adjuvant chemoradiotherapy was started according to regimen, FOLFOX 4 for advanced rectal cancer. Six years post-operation, the patient is currently attending regular follow-ups without recurrence or metastasis.
Keywords: Small bowel neoplasm, Stomach neoplasm, Synchronous quintuple primary cancer, Colon neoplasm
Core tip: We have experienced a case of synchronous quintuple primary gastrointestinal tract malignancies. Reports on synchronous quintuple primary malignancies are extremely rare. Hence, we report on the case, which developed in the stomach, jejunum, ascending colon, transverse colon and rectum with literature review.
INTRODUCTION
The occurrence of multiple primary malignancy, which is defined as two or more malignancies detected in an individual person, is becoming more frequent[1,2]. When multiple primary malignancies are diagnosed in multiple organs, they are classified into synchronous or metachronous subcategories according to the time of detection[3]. While there are a number of reports on cases of triple or quadruple primary malignancies, and metachronous quintuple primary malignancies, reports on synchronous quintuple primary malignancies are extremely rare. Here, we report on a case of synchronous quintuple primary gastrointestinal tract malignancy, which developed in the stomach, jejunum, ascending colon, transverse colon and rectum with literature review.
CASE REPORT
A 52-year-old male legal office worker was referred to our center as a result of anal pain and intermittent blood-tinged stool. Prior to his referral, the patient had quit smoking and consumption alcohol for an approximate 2 year period. However, the patient had a history of 30 years of smoking one pack a day and social drinking. His sister had been diagnosed with colon cancer at the age of 50 and underwent an operation. The other family members have no distinct medical history associated with malignancies. On a digital rectal examination, a rectal mass near the anus was found. Colonoscopy revealed three masses in the ascending colon, transverse colon and the rectum. Each mass was identified with mucinous adenocarcinoma, respectively. Esophagogastroduodenoscopy revealed an early gastric cancer (EGC) type IIc lesion at the antrum, posterior wall of the stomach with atrophic gastritis (Figure 1). A computed tomography (CT) scan for staging found another mass with lymphadenopathy at the jejunum and showed no significant lymph node enlargement around the stomach, colon and rectum (Figure 2). A positron emission tomography (PET)/CT showed abnormal increases in fluorodeoxy glucose (FDG) uptake in the ascending colon, rectum and jejunum but no definite abnormal FDG uptake along the gastric wall and transverse colon was noted. Diffuse increased FDG uptake was found at both thyroid glands, which allowed for the diagnosis of thyroiditis (Figure 3). The patient underwent a subtotal gastrectomy, segmental resection of the jejunum and a total proctocolectomy with the end ileostomy simultaneously during one operation.
Figure 1.
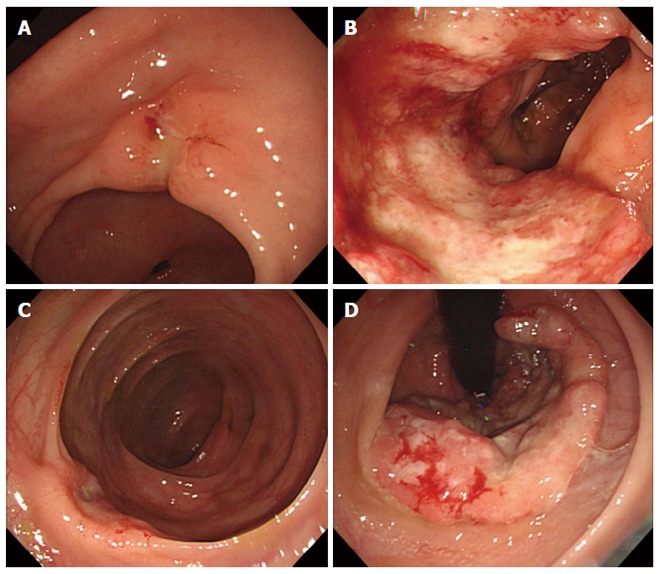
Endoscopic findings. A: Early gastric cancer type IIc lesion at antrum, posterior wall of stomach; B: Ulcerative mass at proximal ascending colon, diagnosed with adenocarcinoma; C: Concave mass at transverse colon, diagnosed with adenocarcinoma; D: Ulcerative rectal mass near anus, diagnosed with adenocarcinoma pathologically.
Figure 2.

Computed tomography finding. Focal irregular wall thickening at proximal jejunum with lymphadenopathy, suggesting adenocarcinoma.
Figure 3.

Positron emission tomography/computed tomography findings. Revealed abnormal increased fluorodeoxy glucose (FDG) uptakes in ascending colon, rectum and jejunum but no definite abnormal FDG uptake along the gastric wall and transverse colon was noted. Diffuse increased FDG uptake was found at both thyroid glands, which allowed for the diagnosis of thyroiditis.
The pathologic results following the gastrectomy determined the gastric tumor to be EGC type IIc, tubular adenocarcinoma, moderate differentiated, intestinal type by the Lauren classification system, with a depth of invasion into the submucosa (T1b) and no lymph node metastasis in 19 lymph nodes (pT1bN0M0, pStageIA). The pathologic results at the jejunum revealed a 7.0 cm × 4.5 cm sized, combined adenocarcinoma and neuroendocrine carcinoma, with a depth of invasion into the subserosa (T3) and no lymph node metastasis in 8 lymph nodes (pT3N0M0, pStageIIA). The specimen gained from the total proctocolectomy had three adenocarcinomas at the ascending colon, 5.5 cm × 4.5 cm sized, mucinous adenocarcinoma, with modified Astler-Coller’s stage C2, with a depth of invasion into the subserosa. At the transverse colon, mucinous adenocarcinoma arising from high grade tubulovillous adenoma was presented with a depth of involvement up until the muscularis mucosa without penetration. Results from analysis of the rectum showed 6.5 cm × 3.8 cm sized, mucinous adenocarcinoma with modified Astler-Coller’s stage C2, invasion to perirectal fat tissue was identified. A total of 67 lymph nodes were dissected by proctocolectomy, with 1 perirectal lymph node showing metastasis. The stages of the ascending colon, transverse colon and rectal cancer were pStageIIA (pT3N0M0), pStageI(pT1N0M0) and pStageIIIB (pT3N1aM0), respectively. The tumors of the colon and rectum were evaluated with MLH-1 and MSH-2 expression for Lynch syndrome, both gene expressions were present and functioning. The gastric and colorectal tumors were evaluated with microsatellite instability (MSI). The results showed MSI-high (MSI-H) for MSI markers (bat26, D5S346, bat25, D2S123) and microsatellite stable (MSS) for the other marker (D17S250). Consequently, postoperative adjuvant chemoradiotherapy was started according to the regimen, FOLFOX 4 (Oxaliplatin, 5-fluorouracil (5-FU) and leucovorin) for rectal cancer. Six years post operation, the patient is currently attending regular follow-ups and is without recurrence or metastasis, reporting a normal bill of health.
DISCUSSION
According to the Warren and Gates criteria, multiple primary malignancies are defined if the following 4 conditions are satisfied: (1) each tumor is malignant; (2) each tumor has its own pathological features; (3) tumors occur in different parts of the organs, and are not continuous with each other; and (4) each tumor has its own metastatic pathway and the diagnosis of metastatic or recurrent tumors can be excluded[4,5]. In the case of this study, though three malignancies gathered at the colon and rectum, each of these malignancies were determined to be primary cancers. They were distinguished as primary malignancies which originated from independent polyps and masses with distinct margins. Synchronous malignancies are defined as more than two primary cancers occurring within a 6 mo period after diagnosis of the first tumor, post the 6 mo period patients with further diagnosed malignancies can be referred to as having metachronous cancers[6]. According to these definitions, the patient in this particular case was thus diagnosed with synchronous quintuple primary cancer.
The occurrences of multiple primary malignancies have increased in recent years. Many factors can be attributed to this increase, including an increasing proportion of elderly patients in the general population, regular medical check-ups and increased number of cancer survivors[2,7]. Reported incidences of multiple primary malignancies are approximately 1%-10%. Metachronous multiple primary malignancies are more common than synchronous malignancies with a ratio 2.7:1. Double primary tumors are most common and triple, quadruple tumors are relatively rare. This is exemplified by the lack of publications on the tumors with no more than 20 published cases of quintuple (or more numbers) primary malignancies and less than 5 cases of synchronous quintuple (or more) cases being presented, this figure includes current cases in English literature[3,8] (Table 1).
Table 1.
Published cases of synchronous quintuple primary malignancies in English literature
| Year | Country | Age/sex | Location | Pathology |
| 1995 | Germany | 67/M | Descending colon | Adenocarcinoma |
| Kidney | Adenocarcinoma | |||
| Prostate | Adenocarcinoma | |||
| Bladder | Transitional cell carcinoma | |||
| Bladder | malignant fibrous histocytoma | |||
| 2012 | Japan | 46/F | Right ovary | Clear cell adenocarcinoma |
| Endometrium | Endometrioid adenocarcinoma | |||
| Ascending colon | Adenocarcinoma | |||
| Rectum | Adenocarcinoma | |||
| Left lung | Papillary adenocarcinoma | |||
| 2015 | United States | 57/F | Right popliteal fossa | Malignant melanoma |
| Left breast | Invasive lobular carcinoma | |||
| Left axillary lymph node | Diffuse large B cell lymphoma | |||
| Left axillary lymph node | Nodular lymphocyte predominant Hodgkin lymphoma | |||
| Left tibial soft tissue | Giant cell tumor |
F: Female; M: Male.
The patient was suspected for Lynch syndrome, however, the tumors all possessed MLH1, MSH2 gene expression. Therefore, the patient was unlikely to have Lynch syndrome. On the other hand, the tumors had MSI-H for MSI markers (bat26, D5S346, bat25, D2S123) and MSS for the other marker (D17S250). MSI is believed to be a factor in carcinogenesis[9]. Hence, diagnostics suggested MSI may be responsible for carcinogenesis in the patient.
To decide treatment option for multiple primary malignancy patient, the stages of each synchronous malignancy is the most important factor[2]. In the current case, with the exception of rectal cancer, there was no evidence of lymph node metastasis and had stages with relatively more favorable outcomes than stage IIIB rectal cancer. Therefore, the adjuvant therapy was focused on the rectal cancer and favorable results were achieved.
In conclusion, surgeons should consider the possibility of multiple primary malignancies before surgery for intestinal tract malignancies. It is essential to perform full preoperative evaluations including esophagogastroduodenoscopy, colonoscopy, CT scan, PET/CT, and other imaging modalities, if needed. In addition, the stage of each malignancy is the most important factor to determine treatment options for multiple primary synchronous malignancy patients.
COMMENTS
Case characteristics
A 52-year-old male was diagnosed with synchronous quintuple primary malignancies in the stomach, jejunum, ascending colon, transverse colon and rectum.
Clinical diagnosis
The patient was diagnosed with malignancies in the stomach, jejunum, ascending colon, transverse colon and rectum.
Imaging diagnosis
Esophagogastroduodenoscopy revealed an early gastric cancer (EGC) at the antrum. Colonoscopy revealed three masses in the ascending colon, transverse colon and the rectum. A computed tomography (CT) scan found a mass at the jejunum and showed no significant lymph node enlargement around the stomach, colon and rectum. A positron emission tomography (PET)/CT showed abnormal increases in fluorodeoxy glucose (FDG) uptake in the ascending colon, rectum and jejunum but no definite abnormal FDG uptake along the gastric wall and transverse colon was noted.
Pathological diagnosis
The pathologic results determined the gastric tumor to be tubular adenocarcinoma. The mass at the jejunum revealed combined adenocarcinoma and neuroendocrine carcinoma. The specimen gained from the total proctocolectomy had three adenocarcinomas.
Treatment
The patient underwent a subtotal gastrectomy, segmental resection of the jejunum and a total proctocolectomy with the end ileostomy simultaneously during one operation.
Related reports
Three case reports of synchronous quintuple malignancy were published in English literature.
Experiences and lessons
Surgeons should consider the possibility of multiple primary malignancies before surgery for intestinal tract malignancies. The stage of each malignancy is the most important factor to determine treatment options for multiple primary synchronous malignancy patients.
Peer-review
It’s a well written, well-illustrated, prolonged follow-up of the patient case report.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Institutional review board statement: The case report was exempt from institutional review board of the Pusan National University Yangsan Hospital.
Informed consent statement: The patient provided informed written consent prior to the treatment.
Conflict-of-interest statement: All the authors have no conflicts of interests to declare.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: September 12, 2016
First decision: September 28, 2016
Article in press: October 31, 2016
P- Reviewer: Biondi A, Ennaifer R S- Editor: Gong ZM L- Editor: A E- Editor: Liu WX
References
- 1.Maruyama T, Nakasone T, Maruyama N, Matayoshi A, Arasaki A. Synchronous quadruple multiple primary cancers of the tongue, bilateral breasts, and kidney in a female patient with a disease-free survival time of more than 5 years: a case report. World J Surg Oncol. 2015;13:263. doi: 10.1186/s12957-015-0684-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oh SJ, Bae DS, Suh BJ. Synchronous triple primary cancers occurring in the stomach, kidney, and thyroid. Ann Surg Treat Res. 2015;88:345–348. doi: 10.4174/astr.2015.88.6.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Komiyama S, Nishio E, Ichikawa R, Miyamura H, Kawamura K, Komiyama M, Nishio Y, Udagawa Y. Asymptomatic synchronous quintuple primary cancers. Gynecol Obstet Invest. 2012;74:324–328. doi: 10.1159/000339135. [DOI] [PubMed] [Google Scholar]
- 4.Warren S, Gates O. Multiple primary malignant tumors: survey of the literature and a statistical study. Am J Cancer. 1932;16:1358–1414. [Google Scholar]
- 5.Xu LL, Gu KS. Clinical retrospective analysis of cases with multiple primary malignant neoplasms. Genet Mol Res. 2014;13:9271–9284. doi: 10.4238/2014.March.12.19. [DOI] [PubMed] [Google Scholar]
- 6.Moertel CG, Dockerty MB, Baggenstoss AH. Multiple primary malignant neoplasms. I. Introduction and presentation of data. Cancer. 1961;14:221–230. doi: 10.1002/1097-0142(196103/04)14:2<221::aid-cncr2820140202>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 7.Cercato MC, Colella E, Ferraresi V, Diodoro MG, Tonachella R. Report of two cases of quintuple primary malignancies and review of the literature. Anticancer Res. 2008;28:2953–2958. [PubMed] [Google Scholar]
- 8.Testori A, Cioffi U, De Simone M, Bini F, Vaghi A, Lemos AA, Ciulla MM, Alloisio M. Multiple primary synchronous malignant tumors. BMC Res Notes. 2015;8:730. doi: 10.1186/s13104-015-1724-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li B, Liu HY, Guo SH, Sun P, Gong FM, Jia BQ. Detection of microsatellite instability in gastric cancer and dysplasia tissues. Int J Clin Exp Med. 2015;8:21442–21447. [PMC free article] [PubMed] [Google Scholar]


