Abstract
Acute appendicitis (AA) is the commonest cause of pain abdomen requiring surgical intervention. Diagnosis as well as management of acute appendicitis is mired in controversies and contradictions even today. Clinicians often face the dilemma of balancing negative appendectomy rate and perforation rate if the diagnosis is based on clinical scoring alone. Laboratory results are often non-specific. Imaging has an important role not only in diagnosing appendicitis and its complication but also suggesting alternate diagnosis in appropriate cases. However, there is no universally accepted diagnostic imaging algorithm for appendicitis. Imaging of acute appendicitis needs to be streamlined keeping pros and cons of the available investigative modalities. Radiography has practically no role today in the diagnosis and management of acute appendicitis. Ultrasonography (USG) should be the first line imaging modality for all ages, particularly for children and non-obese young adults including women of reproductive age group. If USG findings are unequivocal and correlate with clinical assessment, no further imaging is needed. In case of equivocal USG findings or clinico-radiological dissociation, follow-up/further imaging (computed tomography (CT) scan/magnetic resonance imaging (MRI)) is recommended. In pediatric and pregnant patients with inconclusive initial USG, MRI is the next option. Routine use of CT scan for diagnosis of AA needs to be discouraged. Our proposed version of a practical imaging algorithm, with USG first and always has been incorporated in the article.
Keywords: Acute appendicitis, Ultrasonography, CT scan, MRI
Introduction
Acute appendicitis (AA) is the commonest cause of pain abdomen in children and young adults requiring surgical intervention and has an estimated lifetime risk of 7–9%. AA, as we know today, was formally described by Reginald Fitz in the year 1886, although there are historical descriptions about appendix dating back as early as fifteenth century.1 As we clock 125 years since Fitz's initial description of ‘Perforating Inflammation of the Vermiform Appendix’, it is a painful reality that even today, the diagnosis as well as management of AA is mired in controversies and contradictions.2 Despite progressive advancement of our clinical understanding by the concerted efforts of physicians and surgeons over these years, complimented by technological evolution in laboratory and imaging sciences, the enigma of appendicitis still presents a diagnostic challenge quite frequently. A multitude of widely divergent and at times conflicting publications discussing about the ideal diagnostic modality and treatment algorithm for AA are being added regularly in the scientific knowledge bank, which by itself is a testimony for the uncertainty that exists in this field today.3, 4, 5, 6, 7, 8 Without a clearly defined, universally accepted diagnostic algorithm for AA, a condition which is so common in our day to day practice, diagnosticians are at crossroads in selecting the right path. In this review, we intend to make an attempt to organize the approach to AA, especially with reference to the imaging diagnosis.
Clinical perspectives
Historically, clinical assessment has always played a vital role in the diagnosis and management of AA, and remains the cornerstone of diagnosis even today.9 There are well-known confounders which often come in the way of accurate clinical diagnosis of AA, especially in the young women and extremes of age. Since the recognition of AA as a clinical entity, clinicians have been facing the dilemma of balancing two important but reciprocal measures, namely perforation rate and negative appendectomy rate (NAR). Alfredo Alvarado was one of the first to develop a practical score for early diagnosis of AA taking clinical and certain laboratory parameters with the sole aim to reduce NAR without proportionately increasing the perforation rate.10 Since then, a number of scoring systems have been and are still being developed to increase the diagnostic accuracy for AA.11, 12, 13, 14 Most of these scoring systems use clinical and various laboratory parameters for the diagnosis of AA. Alvarado scoring has been extensively used and tested in last three decades. Alvarado scoring is a useful clinico-pathological tool to diagnose AA, though many components of the scoring system are non-specific.
Prompt and accurate diagnosis with timely initiation of appropriate treatment remains the cornerstone for successful management of AA. The relative importance assigned to clinical diagnosis of AA based on history and physical examination findings, with or without laboratory markers, varies widely not only amongst different countries but even amongst institutions within the same country. It may not be incorrect to state that with the availability of various biomarkers and cross-sectional imaging like ultrasound, computed tomography (CT) scan and magnetic resonance imaging (MRI), clinical assessment is possibly being often relegated to a back seat. The situation becomes further complicated in the setting of pregnancy. However, it is heartening that though dwindling in numbers, there exist a sub-set of clinicians in many countries including India, who still trust their clinical acumen more than any investigative modalities when it comes to final diagnosis and management of AA.
Ironically, majority of research publications have focused on the ability of a particular diagnostic tool to detect presence or absence of AA as its prime objective rather than considering AA as a disease process having its own spectrum of evolution. Alternative diagnoses/differential diagnosis of clinical mimics of AA is discussed much less frequently. Similarly, the importance of close observation and monitoring in equivocal cases is often understated. Today, the fear of missing the diagnosis of AA is possibly unfounded. What adds to the woes are the reports of significant discordance between operative and histopathological diagnosis.15, 16
There has been a paradigm shift in the clinician's outlook as far as the optimal management of AA is concerned. Firstly, the clinicians are now striving to achieve the lowest possible NAR using whatever diagnostic means available today. This includes disproportionately increased usage of CT scan in many parts of the world over the last three decades. Gone are the days, when a NAR of 20–30% was acceptable to the clinicians. Secondly, it is amply clarified in the literature that there is no need to rush for early appendectomy in doubtful cases.17, 18 Thirdly, the age old concept of ‘early appendectomy’ as the sole remedy for all cases of AA is being increasingly questioned with an alternative, although debatable, therapeutic option of conservative treatment with antibiotics for the select group of uncomplicated AA.2, 7, 9, 19, 20, 21
Inflammatory biomarkers
A raised total leukocyte count with a shift to left is well known to be associated with AA depending on the severity of the disease. Similarly, C-reactive protein (CRP) has also been found to be helpful in supporting clinical diagnosis of AA. A combination of leukocyte count and CRP assay helps to predict appendicitis inflammatory response score.5, 12, 22 Various other biomarkers that are being studied include serum bilirubin level, D-dimer, pro-calcitonin, neutrophil to lymphocyte ratio, mean platelet volume, red blood cell distribution width, etc. It is important to understand here that most of these inflammatory markers are likely to be elevated/positive in many other inflammatory/infective conditions and are not specific to AA alone.
Role of radiology
Radiologists have always played significant role in the evaluation of a suspected case of AA. Since the advent of cross-sectional imaging, radiologist's role has vastly expanded in the diagnosis of AA and its complications. Today's clinicians have become increasingly dependent on imaging correlation besides laboratory markers to confirm their clinical judgment, before planning management of acute abdomen including AA. It would be very uncommon today to treat a patient of suspected AA without the help of cross-sectional imaging. The role of imaging lies not only in the prompt and accurate diagnosis of AA and its complications, but also in the reliable exclusion of AA and providing alternative diagnosis in the appropriate situation. It is widely believed, barring a few exceptions, that cross-sectional imaging has been instrumental in reducing NAR to a reasonably acceptable limit of 3–10%.8, 23, 24, 3 However, there is no universal consensus on the imaging modality of choice and diagnostic protocol for suspected AA. The current role of the imaging studies is discussed below.
Plain radiograph abdomen
A number of plain abdominal radiographic signs have been historically described for AA. However, in the present day context, plain abdominal radiograph is rarely recommended for the diagnostic workup for AA.25
Barium enema
Although barium enema findings of AA are described in the literature, the modality is no longer recommended because of low accuracy.
Ultrasonography (USG)
Way back in 1986, Puylaert published a landmark study on the utility of graded compression USG in the evaluation of AA.26 Since then, plenty of research papers have been published highlighting utility of USG in the diagnosis of AA. Meanwhile, there has been tremendous advancement in the ultrasound equipment technology and sonologists’ knowledge about diagnosing AA. Sonographic criteria for diagnosing AA in children and adults were developed.27 Chesbrough et al.28 found self-localization to be useful in aiding sonographic diagnosis of AA. Sonographic studies in late eighties and early nineties revealed sensitivity, specificity, and accuracy of USG for diagnosing AA ranging from 75 to 95%, 85 to 100%, 90 to 96%, respectively.29, 30, 31, 32, 33 Rioux32 and Ozel et al.34 reported visualization of normal appendix in 70–80% of patients without appendicitis. Till mid-nineties, USG enjoyed the indisputable reputation of an important additional diagnostic tool besides clinical and laboratory assessment in the management of AA.35
CT scan
At a time when USG was getting firmly established as the imaging of choice for diagnosing AA, a few sporadic studies on the role of CT scanning in suspected patients of AA started appearing in medical literature.38, 39, 40 CT scan signs of AA were described and overall, CT scan was found to be highly accurate for diagnosis of AA.41 The high sensitivity and specificity of CT scanning in AA made a case for regular use of CT scan in suspected AA including children, to improve patient care by reducing overall treatment cost, besides lowering the probability of negative appendectomy and perforation rates.42, 43 Many subsequent studies have reported superiority of CT scan over USG in the diagnosis and management of AA,44, 45, 46, 47 including modified techniques like ‘Focused CT scan for appendix’ to avoid needless radiation to the entire abdomen. While even non-contrast CT (NCCT) was found to be more accurate as compared to USG, contrast-enhanced CT scan with intravenous iodinated contrast and prior administration of oral contrast was found to improve diagnostic accuracy further when compared with NCCT.48 CT scan usage has seen consistent and sharp rise in last two decades because of its reported higher accuracy over USG and clinical assessment for AA, with many institutions preferring CT scanning as the primary imaging modality in suspected case of AA. Many researchers have affirmed that routine use of CT scan have led to proportionate decrease in the NAR.9, 49 However, it was also noted by many that liberal use of CT scan for AA may not help as much as claimed by previous studies50 and also there are known pitfalls of CT scan.51 The biggest problem faced today is the lack of clear guidelines or consensus as to the indications of using CT scanning in AA, leaving the discretion with institutions/regions to follow what possibly suit them the most.
MRI
MRI has been in use for evaluation of AA for more than two decades.52 The main hurdles were limited availability of the facility, cost of investigation, time for imaging, and patient suitability for MRI. Advances in MRI technology (both software and hardware) have led to the development of faster yet high resolution sequences suitable for imaging of acute abdomen in a limited time.53 MRI is particularly suitable in pregnant patients where USG has shown varied results depending on period of gestation, and may soon become the first line imaging modality in such patients.54
Scintigraphy
(99 m) c labeled white blood cell scintigraphy has been described as an additional tool in diagnosing acute infection including AA.55 However, leukocyte scintigraphy is not routinely used to diagnose AA in the current scenario.
Imaging modality of choice – the big debate
Let us examine the pros and cons of the ups and downs in the utilization pattern of USG and CT scan for the diagnosis of AA in last three decades. At the outset, the fact that between USG and CT scan, neither modality is inferior to the other in terms of diagnosing AA needs to be re-iterated. As pointed out earlier, USG is a time-tested versatile modality not only for diagnosing AA, but also to exclude AA and suggest alternative diagnoses in relevant cases. The present day USG equipments enable acquiring high-resolution images of most parts of the abdomen including appendix. USG is invaluable in children and non-obese young adults including females. Trans-vaginal sonography is an added technological boon for diagnosing gynecological conditions mimicking AA. We firmly believe that even today, USG is a versatile imaging modality which has crucial role in the diagnosis and management of a suspected case of AA. In experienced hands, accuracy of USG approaches to that of CT/MRI scan. A normal USG study in a clinically low probability case virtually obviates need for any further study. Demonstration of a normal appendix on USG rules out AA. In experienced hands, non-visualization of appendix in a suspected case of AA is considered a valid reason for clinical observation rather than opt for supplementary imaging. A repeat USG study after 6–12 h of in-hospital observation is a valuable option before considering higher modalities like CT scan or MRI depending on the clinical situation. The capability of USG to provide alternative diagnosis in a suspected case of AA is often understated. USG is particularly suited for assessing children, non-obese adults, and women of reproductive age group, besides the inherent advantage of USG that it can be performed at the bedside if needed.36, 37 Addition of color Doppler, though at times complimentary to the gray-scale, did not have much impact in the diagnosis of AA. Presently, role of newer USG techniques like elastography is under clinical evaluation.
The main limitation (if any) of USG is the availability of trained sonologist who is willing to perform the USG at odd hours whenever needed. In many institutions/countries, availability of radiologists/trained sonologist off working hours is an administrative problem; consequently doing a CT scan and sending images to the radiologist becomes a viable alternative option which is one of the reasons for increase in CT usage during off-working hours in many institutions.56 The issue of technically suboptimal/equivocal USG imaging study can be resolved by clinical correlation and further/follow-up imaging like CT scan/MRI as per the institutional protocol. In this manner, the need for CT scanning as the primary modality for diagnosing AA can be significantly reduced without compromising the quality of health care. CT scan, particularly multi-detector CT, has a lead over USG in terms of being comparatively more accurate in diagnosing AA in most situations. But this relative superiority cannot be a reason for justifying indiscriminate use of CT scan for all cases of suspected AA.
The euphoria of using indiscriminate CT scan for AA started fading in the face of long-term radiation concerns, although CT scan usage is still unacceptably high in the name of accuracy in many parts of the world, particularly the United States. Researchers at many parts of the world including the authors feel that USG first followed by limited CT/MRI exclusively as a problem-solving modality in equivocal cases is a much better option than ‘CT-first’ policy.8, 9, 57, 58 The role of USG as a screening modality is being re-introduced and reinforced by improving the quality of USG and its reporting.57, 59, 60 Current trends show reduction in CT usage and resurgence in use of USG for diagnosis of AA, with encouraging results. Also, the possibility of low-dose CT scan protocols without compromising the diagnostic quality of imaging is being explored, with promising results in last 5 years.61, 62
If we look at the existing literature, we find that there are mainly two schools of researchers, one group dealing with USG and another group dealing with CT with resultant modality bias. As a reader, one gets more than enough literature favoring or opposing usage of any one of these two modalities and accordingly one would be able to justify using either USG or CT scan for diagnosing AA. Another setback is that most of the published literature on AA focuses on AA alone rather than the actual clinical presentation as acute pain abdomen or pain right iliac fossa. A sizeable number of such studies describe AA as an all or none phenomenon rather than as a continuum of disease spectrum which may change in its severity depending on various factors. This problem is compounded by a few percentages of AA which resolve of its own or after presumptive antibiotic therapy.
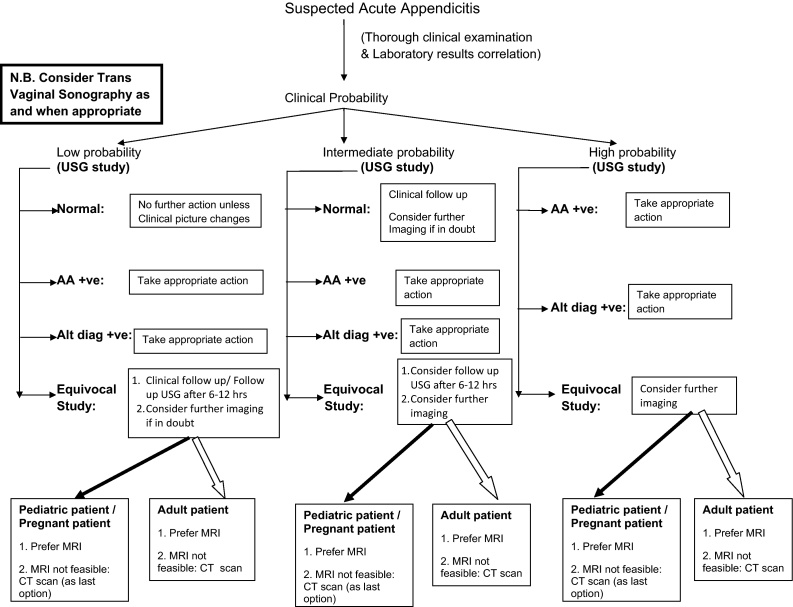
The need today is to follow a universal diagnostic algorithm and the imaging modality that is best suited for a particular clinical scenario, with least adverse impact to the patient. The authors firmly believe that there is a need to look at this issue in a more holistic manner and establish a clear-cut universally acceptable diagnostic algorithm for AA. Our proposed version of a practical imaging algorithm, with USG first and always, is depicted in Fig. 1.
Fig. 1.
Flowchart showing proposed version of a practical imaging algorithm, with USG first and always.
In this context, we also strongly recommend that the ACR appropriateness criteria4 for diagnosing AA (2011) need to be revisited in view of the radiation concern associated with CT scan and restated efficacy of USG. It is also time to integrate imaging (USG and or CT/MRI) findings into the already existing scoring systems and develop new clinico-pathological–radiological scoring systems for maximizing diagnostic accuracy.63
Conclusion
Imaging of AA needs to be streamlined keeping pros and cons of the available investigative modalities. Radiography has practically no role today in the diagnosis and management of AA. USG should be the first line imaging modality for all ages, particularly for children and non-obese young adults including women of reproductive age group. If USG findings are unequivocal and correlate with clinical assessment, no further imaging is needed. In case of equivocal USG findings or clinico-radiological dissociation, follow-up/further imaging (CT scan/MRI) is recommended. In pediatric and pregnant patients with inconclusive initial USG, MRI is the next option. Routine use of CT scan for diagnosis of AA needs to be discouraged.
Conflicts of interest
The authors have none to declare.
References
- 1.Hamill J.K., Liley A., Hill A.G. Historical aspects of appendicitis in children. Aust N Z J Surg. 2014;84:307–310. doi: 10.1111/ans.12425. [DOI] [PubMed] [Google Scholar]
- 2.Wray C.J., Kao L.S., Millas S.G., Tsao K., Ko T.C. Acute appendicitis: controversies in diagnosis and management. Curr Probl Surg. 2013;50(2):54–86. doi: 10.1067/j.cpsurg.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Boonstra P.A., van Veen R.N., Stockmann H.B. Less negative appendectomies due to imaging in patients with suspected appendicitis. Surg Endosc. 2015;29(8):2365–2370. doi: 10.1007/s00464-014-3963-2. [DOI] [PubMed] [Google Scholar]
- 4.Smith M.P., Katz D.S., Lalani T. ACR Appropriateness Criteria® right lower quadrant pain – suspected appendicitis. Ultrasound Q. 2015;31(2):85–91. doi: 10.1097/RUQ.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 5.Andersson M., Rubér M., Ekerfelt C., Hallgren H.B., Olaison G., Andersson R.E. Can new inflammatory markers improve the diagnosis of acute appendicitis? World J Surg. 2014;38(11):2777–2783. doi: 10.1007/s00268-014-2708-7. [DOI] [PubMed] [Google Scholar]
- 6.Bliss L.A., Yang C.J., Kent T.S., Ng S.C., Critchlow J.F., Tseng J.F. Appendicitis in the modern era: universal problem and variable treatment. Surg Endosc. 2015;29(7):1897–1902. doi: 10.1007/s00464-014-3882-2. [DOI] [PubMed] [Google Scholar]
- 7.Svensson J.F., Patkova B., Almström M. Nonoperative treatment with antibiotics versus surgery for acute non perforated appendicitis in children: a pilot randomized controlled trial. Ann Surg. 2015;261(1):67–71. doi: 10.1097/SLA.0000000000000835. [DOI] [PubMed] [Google Scholar]
- 8.Aspelund G., Fingeret A., Gross E. Ultrasonography/MRI versus CT for diagnosing appendicitis. Pediatrics. 2014;133(4):586–593. doi: 10.1542/peds.2013-2128. [DOI] [PubMed] [Google Scholar]
- 9.Bhangu A., Søreide K., Di Saverio S., Assarsson J.H., Drake F.T. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386(10000):1278–1287. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 10.Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557–564. doi: 10.1016/s0196-0644(86)80993-3. [DOI] [PubMed] [Google Scholar]
- 11.Pogorelić Z., Rak S., Mrklić I., Jurić I. Prospective validation of Alvarado score and pediatric appendicitis score for the diagnosis of acute appendicitis in children. Pediatr Emerg Care. 2015;31(3):164–168. doi: 10.1097/PEC.0000000000000375. [DOI] [PubMed] [Google Scholar]
- 12.Yap T.L., Chen Y., Low W.W. A new 2-step risk-stratification clinical score for suspected appendicitis in children. J Pediatr Surg. 2015 doi: 10.1016/j.jpedsurg.2015.08.028. pii: S0022-3468(15)00542-4. [DOI] [PubMed] [Google Scholar]
- 13.Kollár D., McCartan D.P., Bourke M., Cross K.S., Dowdall J. Predicting acute appendicitis? A comparison of the Alvarado score, the appendicitis inflammatory response score and clinical assessment. World J Surg. 2015;39(1):104–109. doi: 10.1007/s00268-014-2794-6. [DOI] [PubMed] [Google Scholar]
- 14.Sammalkorpi H.E., Mentula P., Leppäniemi A. A new adult appendicitis score improves diagnostic accuracy of acute appendicitis – a prospective study. BMC Gastroenterol. 2014;26(14):114. doi: 10.1186/1471-230X-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fallon S.C., Kim M.E., Hallmark C.A. Correlating surgical and pathological diagnoses in pediatric appendicitis. J Pediatr Surg. 2015;50(4):638–641. doi: 10.1016/j.jpedsurg.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Correa J., Jimeno J., Vallverdu H. Correlation between intraoperative surgical diagnosis of complicated acute appendicitis and the pathology report: clinical implications. Surg Infect (Larchmt) 2015;16(1):41–44. doi: 10.1089/sur.2013.155. [DOI] [PubMed] [Google Scholar]
- 17.Yardeni D., Hirschl R.B., Drongowski R.A., Teitelbaum D.H., Geiger J.D., Coran A.G. Delayed versus immediate surgery in acute appendicitis: do we need to operate during the night? J Pediatr Surg. 2004;39(3):464–469. doi: 10.1016/j.jpedsurg.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 18.Kim S.H., Park S.J., Park Y.Y., Choi S.I. Delayed appendectomy is safe in patients with acute non perforated appendicitis. Int Surg. 2015;100(6):1004–1010. doi: 10.9738/INTSURG-D-14-00240.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salminen P., Paajanen H., Rautio T. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313(23):2340–2348. doi: 10.1001/jama.2015.6154. [DOI] [PubMed] [Google Scholar]
- 20.Flum D.R. Clinical practice. Acute appendicitis – appendectomy or the antibiotics first strategy. N Engl J Med. 2015;372(20):1937–1943. doi: 10.1056/NEJMcp1215006. [DOI] [PubMed] [Google Scholar]
- 21.Kirby A., Hobson R.P., Burke D., Cleveland V., Ford G., West R.M. Appendicectomy for suspected uncomplicated appendicitis is associated with fewer complications than conservative antibiotic management: a meta-analysis of post-intervention complications. J Infect. 2015;70(2):105–110. doi: 10.1016/j.jinf.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 22.Al-Abed Y.A., Alobaid N., Myint F. Diagnostic markers in acute appendicitis. Am J Surg. 2015;209(6):1043–1047. doi: 10.1016/j.amjsurg.2014.05.024. [DOI] [PubMed] [Google Scholar]
- 23.Binkovitz L.A., Unsdorfer K.M., Thapa P. Pediatric appendiceal ultrasound: accuracy, determinacy and clinical outcomes. Pediatr Radiol. 2015;45(13):1934–1944. doi: 10.1007/s00247-015-3432-7. [DOI] [PubMed] [Google Scholar]
- 24.Lahaye M.J., Lambregts D.M., Mutsaers E. Mandatory imaging cuts costs and reduces the rate of unnecessary surgeries in the diagnostic work-up of patients suspected of having appendicitis. Eur Radiol. 2015;25(5):1464–1470. doi: 10.1007/s00330-014-3531-0. [DOI] [PubMed] [Google Scholar]
- 25.Oncel M., Degirmenci B., Demirhan N., Hakyemez B., Altuntas Y.E., Aydinli M. Is the use of plain abdominal radiographs (PAR) a necessity for all patients with suspected acute appendicitis in emergency services? Curr Surg. 2003;60(3):296–300. doi: 10.1016/S0149-7944(02)00732-8. [DOI] [PubMed] [Google Scholar]
- 26.Puylaert J.B. Acute appendicitis: US evaluation using graded compression. Radiology. 1986;158(2):355–360. doi: 10.1148/radiology.158.2.2934762. [DOI] [PubMed] [Google Scholar]
- 27.Jeffrey R.B., Jr., Laing F.C., Townsend R.R. Acute appendicitis: sonographic criteria based on 250 cases. Radiology. 1988;167(2):327–329. doi: 10.1148/radiology.167.2.3282253. [DOI] [PubMed] [Google Scholar]
- 28.Chesbrough R.M., Burkhard T.K., Balsara Z.N., Goff W.B., 2nd, Davis D.J. Self-localization in US of appendicitis: an addition to graded compression. Radiology. 1993;187(2):349–351. doi: 10.1148/radiology.187.2.8475271. [DOI] [PubMed] [Google Scholar]
- 29.Puylaert J.B., Rutgers P.H., Lalisang R.I. A prospective study of ultrasonography in the diagnosis of appendicitis. N Engl J Med. 1987;317(11):666–669. doi: 10.1056/NEJM198709103171103. [DOI] [PubMed] [Google Scholar]
- 30.Vignault F., Filiatrault D., Brandt M.L., Garel L., Grignon A., Ouimet A. Acute appendicitis in children: evaluation with US. Radiology. 1990;176(2):501–504. doi: 10.1148/radiology.176.2.2195594. [DOI] [PubMed] [Google Scholar]
- 31.Schwerk W.B., Wichtrup B., Rüschoff J., Rothmund M. Acute and perforated appendicitis: current experience with ultrasound-aided diagnosis. World J Surg. 1990;14(2):271–276. doi: 10.1007/BF01664891. [DOI] [PubMed] [Google Scholar]
- 32.Rioux M. Sonographic detection of the normal and abnormal appendix. Am J Roentgenol. 1992;158(4):773–778. doi: 10.2214/ajr.158.4.1546592. [DOI] [PubMed] [Google Scholar]
- 33.Abu-Yousef M.M., Phillips M.E., Franken E.A., Jr., Al-Jurf A.S., Smith W.L. Sonography of acute appendicitis: a critical review. Crit Rev Diagn Imaging. 1989;29(4):381–408. [PubMed] [Google Scholar]
- 34.Ozel A., Orhan U.P., Akdana B. Sonographic appearance of the normal appendix in children. J Clin Ultrasound. 2011;39(4):183–186. doi: 10.1002/jcu.20807. [DOI] [PubMed] [Google Scholar]
- 35.Wade D.S., Marrow S.E., Balsara Z.N., Burkhard T.K., Goff W.B. Accuracy of ultrasound in the diagnosis of acute appendicitis compared with the surgeon's clinical impression. Arch Surg. 1993;128(9):1039–1046. doi: 10.1001/archsurg.1993.01420210103014. [DOI] [PubMed] [Google Scholar]
- 36.Stewart J.K., Olcott E.W., Jeffrey R.B. Sonography for appendicitis: non visualization of the appendix is an indication for active clinical observation rather than direct referral for computed tomography. J Clin Ultrasound. 2012;40(8):455–461. doi: 10.1002/jcu.21928. [DOI] [PubMed] [Google Scholar]
- 37.Pacharn P., Ying J., Linam L.E., Brody A.S., Babcock D.S. Sonography in the evaluation of acute appendicitis: are negative sonographic findings good enough? J Ultrasound Med. 2010;29(12):1749–1755. doi: 10.7863/jum.2010.29.12.1749. [DOI] [PubMed] [Google Scholar]
- 38.Gale M.E., Birnbaum S., Gerzof S.G., Sloan G., Johnson W.C., Robbins A.H. CT appearance of appendicitis and its local complications. J Comput Assist Tomogr. 1985;9(1):34–37. doi: 10.1097/00004728-198501000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Balthazar E.J., Megibow A.J., Hulnick D. CT of appendicitis. Am J Roentgenol. 1986;147(4):705–710. doi: 10.2214/ajr.147.4.705. [DOI] [PubMed] [Google Scholar]
- 40.Malone A.J., Jr., Wolf C.R., Malmed A.S., Melliere B.F. Diagnosis of acute appendicitis: value of unenhanced CT. Am J Roentgenol. 1993;160(4):763–766. doi: 10.2214/ajr.160.4.8456661. [DOI] [PubMed] [Google Scholar]
- 41.Rao P.M., Rhea J.T., Novelline R.A. Sensitivity and specificity of the individual CT signs of appendicitis: experience with 200 helical appendiceal CT examinations. J Comput Assist Tomogr. 1997;21(5):686–692. doi: 10.1097/00004728-199709000-00002. [DOI] [PubMed] [Google Scholar]
- 42.Rao P.M., Rhea J.T., Novelline R.A., Mostafavi A.A., McCabe C.J. Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med. 1998;338(3):141–146. doi: 10.1056/NEJM199801153380301. [DOI] [PubMed] [Google Scholar]
- 43.Peña B.M., Taylor G.A., Lund D.P., Mandl K.D. Effect of computed tomography on patient management and costs in children with suspected appendicitis. Pediatrics. 1999;104(3 Pt 1):440–446. doi: 10.1542/peds.104.3.440. [DOI] [PubMed] [Google Scholar]
- 44.Balthazar E.J., Birnbaum B.A., Yee J., Megibow A.J., Roshkow J., Gray C. Acute appendicitis: CT and US correlation in 100 patients. Radiology. 1994;190(1):31–35. doi: 10.1148/radiology.190.1.8259423. [DOI] [PubMed] [Google Scholar]
- 45.Rao P.M., Rhea J.T., Rattner D.W., Venus L.G., Novelline R.A. Introduction of appendiceal CT: impact on negative appendectomy and appendiceal perforation rates. Ann Surg. 1999;229(3):344–349. doi: 10.1097/00000658-199903000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pickuth D., Heywang-Köbrunner S.H., Spielmann R.P. Suspected acute appendicitis: is ultrasonography or computed tomography the preferred imaging technique? Eur J Surg. 2000;166(4):315–319. doi: 10.1080/110241500750009177. [DOI] [PubMed] [Google Scholar]
- 47.Sivit C.J., Applegate K.E., Stallion A. Imaging evaluation of suspected appendicitis in a pediatric population: effectiveness of sonography versus CT. Am J Roentgenol. 2000;175(4):977–980. doi: 10.2214/ajr.175.4.1750977. [DOI] [PubMed] [Google Scholar]
- 48.Jacobs J.E., Birnbaum B.A., Macari M. Acute appendicitis: comparison of helical CT diagnosis focused technique with oral contrast material versus non focused technique with oral and intravenous contrast material. Radiology. 2001;220(3):683–690. doi: 10.1148/radiol.2202001557. [DOI] [PubMed] [Google Scholar]
- 49.Kim K., Lee C.C., Song K.J., Kim W., Suh G., Singer A.J. The impact of helical computed tomography on the negative appendectomy rate: a multi-center comparison. J Emerg Med. 2008;34(1):3–6. doi: 10.1016/j.jemermed.2007.05.042. [DOI] [PubMed] [Google Scholar]
- 50.Martin A.E., Vollman D., Adler B., Caniano D.A. CT scans may not reduce the negative appendectomy rate in children. J Pediatr Surg. 2004;39(6):886–890. doi: 10.1016/j.jpedsurg.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 51.Soyer P., Dohan A., Eveno C. Pitfalls and mimickers at 64-section helical CT that cause negative appendectomy: an analysis from 1057 appendectomies. Clin Imaging. 2013;37(5):895–901. doi: 10.1016/j.clinimag.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 52.Incesu L., Coskun A., Selcuk M.B., Akan H., Sozubir S., Bernay F. Acute appendicitis: MR imaging and sonographic correlation. Am J Roentgenol. 1997;168(3):669–674. doi: 10.2214/ajr.168.3.9057512. [DOI] [PubMed] [Google Scholar]
- 53.Byott S., Harris I. Rapid acquisition axial and coronal T2 HASTE MR in the evaluation of acute abdominal pain. Eur J Radiol. 2015 doi: 10.1016/j.ejrad.2015.10.002. pii: S0720-048X(15)30120-0. [DOI] [PubMed] [Google Scholar]
- 54.Konrad J., Grand D., Lourenco A. MRI: first-line imaging modality for pregnant patients with suspected appendicitis. Abdom Imaging. 2015;40(8):3359–3364. doi: 10.1007/s00261-015-0540-7. [DOI] [PubMed] [Google Scholar]
- 55.Aydın F., Kın Cengiz A., Güngör F. Tc-99 m labeled HMPAO white blood cell scintigraphy in pediatric patients. Mol Imaging Radionucl Ther. 2012;21(1):13–18. doi: 10.4274/Mirt.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Burr A., Renaud E.J., Manno M. Glowing in the dark: time of day as a determinant of radiographic imaging in the evaluation of abdominal pain in children. J Pediatr Surg. 2011;46(1):188–191. doi: 10.1016/j.jpedsurg.2010.09.088. [DOI] [PubMed] [Google Scholar]
- 57.Thirumoorthi A.S., Fefferman N.R., Ginsburg H.B., Kuenzler K.A., Tomita S.S. Managing radiation exposure in children – reexamining the role of ultrasound in the diagnosis of appendicitis. J Pediatr Surg. 2012;47(12):2268–2272. doi: 10.1016/j.jpedsurg.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 58.Blitman N.M., Anwar M., Brady K.B., Taragin B.H., Freeman K. Value of focused appendicitis ultrasound and Alvarado score in predicting appendicitis in children: can we reduce the use of CT? Am J Roentgenol. 2015;204(6):W707–W712. doi: 10.2214/AJR.14.13212. [DOI] [PubMed] [Google Scholar]
- 59.Kotagal M., Richards M.K., Chapman T. Improving ultrasound quality to reduce computed tomography use in pediatric appendicitis: the safe and sound campaign. Am J Surg. 2015;209(5):896–900. doi: 10.1016/j.amjsurg.2014.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pare J.R., Langlois B.K., Scalera S.A. Revival of the use of ultrasound in screening for appendicitis in young adult men. J Clin Ultrasound. 2015 doi: 10.1002/jcu.22282. [DOI] [PubMed] [Google Scholar]
- 61.Kim K., Kim Y.H., Kim S.Y. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med. 2012;366(17):1596–1605. doi: 10.1056/NEJMoa1110734. [DOI] [PubMed] [Google Scholar]
- 62.Kim S.H., Yoon J.H., Lee J.H. Low-dose CT for patients with clinically suspected acute appendicitis: optimal strength of sinogram affirmed iterative reconstruction for image quality and diagnostic performance. Acta Radiol. 2015;56(8):899–907. doi: 10.1177/0284185114542297. [DOI] [PubMed] [Google Scholar]
- 63.Atema J.J., van Rossem C.C., Leeuwenburgh M.M., Stoker J., Boermeester M.A. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br J Surg. 2015;102(8):979–990. doi: 10.1002/bjs.9835. [DOI] [PubMed] [Google Scholar]