Abstract
Background
As HIV steps into the third decade, there are more number of patients living on lifelong (antiretroviral therapy) ART and facing the threat of drug resistance with subsequent treatment failure. The aim of this study was to determine predictors of first-line ART failure with the objectives to estimate the burden of 2nd line ART.
Methods
A retrospective 5-year cohort of HIV patients who were initiated on first line ART in 2008–09 was studied. Patients were followed from the time of ART initiation. Kaplan–Meier methods and Cox proportional hazards regression models were used to estimate probabilities and predictors of first line ART failure.
Results
Of the total of 195 patients initiated on first line ART, 15 patients were switched to second line ART yielding 7.69% failure rate. During the 7178 person-years of follow-up, the incidence of first line ART failure was 2.09 per 1000 person-years. The Kaplan–Meier survival analysis gave a mean survival time of 55.6 months. BMI, CD4 count at ART initiation and presence of opportunistic infections were significant predictors of first line ART failure. The burden of second line ART patients by the end of 5 years of first line ART is expected to be 151 patients.
Conclusion
Though the first line ART failure is quite low in this study, we still need to be vigilant for lower BMI, low baseline CD4 count and occurrence of opportunistic infections to efficiently manage failures on first line ART.
Keywords: Antiretroviral therapy, Human immunodeficiency virus, Survival, First line ART failure
Introduction
The HIV epidemic is widely acknowledged to be a most severe health crisis of modern times. There is no cure and no vaccine. In absence of any cure, antiretroviral therapy (ART) is the only treatment that inhibits HIV. ART has changed the HIV disease to a manageable chronic condition by suppressing the viral load, increase in CD4 count and partial restoration of the immune function.1 Though the introduction of HAART has led to an increase in survival among HIV-infected patients, decreased HIV-associated morbidity and mortality, and improved quality of life among HIV patients, it is seen that a considerable proportion of patients fail to achieve a sustained virological response to therapy.2 As ART uptake increases resistant viruses develop leading to treatment failure. As a result of failure patients need to be shifted to second-line regimen to suppress viral load.3, 4 Of the total HIV patients on ART, around 2% are on a second-line regimen.5 Literature from South Africa estimated a high failure rate of 14% by 5 years on ART.6 Experience from the TREAT Asia HIV Observational database (TAHOD) showed that the rate of clinical failure on this regimen was 7.3 per 100 people – years.7 HIV surveillance in the armed forces promulgated by the HIV/AIDS policy of O/o DGAFMS and which is in consonance with the national policy promulgated by National AIDS Control Organisation, MoHFW is more systematic and efficient because of Advanced Immunodeficiency centres (AIDC), Immunodeficiency centres (IDC) and First Line Immunodeficiency centres (FIDC). However we still do not have the estimates of the patients requiring second line drugs.
In light of the above facts the primary objective of the paper was to estimate the incidence of first line ART failure and study its associated predictors. The secondary objective was to estimate the burden of second line ART.
Materials and methods
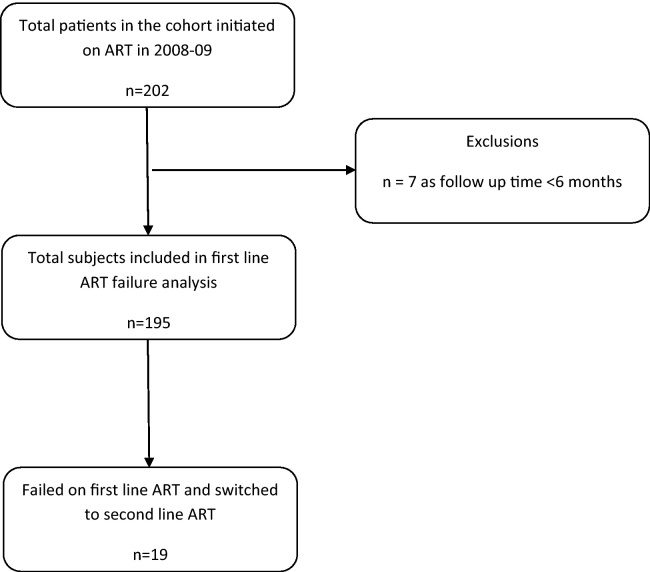
A cohort study of HIV-infected persons more than 18 years of age who were initiated standard first line ART in ART Centre of Pune in 2008–09 was undertaken. The study flow chart is given in Fig. 1. Administered ART drug regimen was as per government guidelines. The patients eligible were those with minimum of 6 months of follow-up and the study follow-up time was maximum of 5 years. Data on patients demographic variables and treatment information were gathered from individual case sheets and ART registers. Patient follow-up began on the date of ART initiation. Dependent variables considered were antiretroviral treatment failure and time to the occurrence of treatment failure. Predictors considered as independent variables included age, years since HIV diagnosis, weight at baseline, hemoglobin, CD4 at baseline, TB treatment and adherence of the patients. Ethical clearance was obtained from the institutional ethics committee. All the information obtained was kept in a confidential manner. Patient names were delinked to the results of the study.
Fig. 1.
Study flow chart of first line ART failure and switch to second line ART.
Statistical analysis
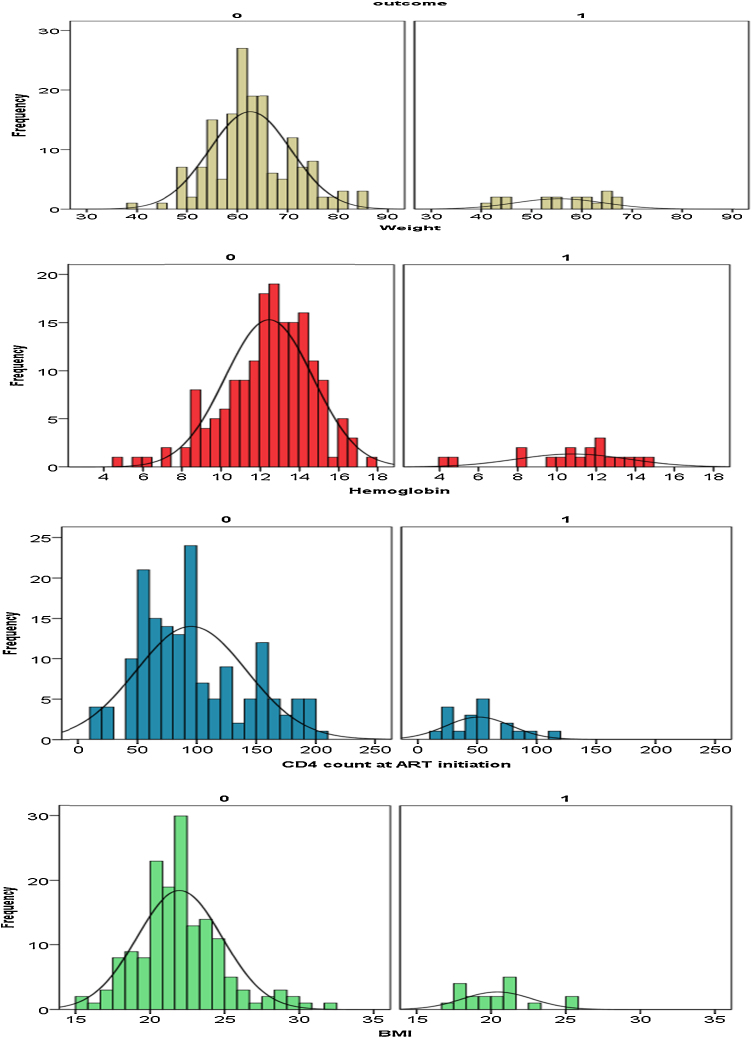
Failure analysis with failure rate and incidence per 100 person-years of follow-up were calculated. Incidence (hazard) rate was defined as number of new cases of disease per population at-risk per unit time (or mortality rate, if outcome is death). Time-to-event analysis was performed using the outcome of switch to second-line ART. Censoring is done if patient died, got posted out from the unit or after 60 months from ART initiation. The significance of the quantitative variables in the two groups namely first line ART failure and no failure was tested using unpaired t test and qualitative variables using chi square test. All variables, which were attested significant by t test or chi square, were only further subjected to the multivariate analysis using Cox proportional hazard model. The survival rates and year-wise survival probabilities were determined. Kaplan–Meier survival estimates and hazard ratios (HR) defined as ratio of incidence rates, using Cox proportional hazards regression model were used to analyze predictors of the first line ART failure and second line ART switch. All analyses were done using SPSS software, version 22.0 (SPSS) (Fig. 2).
Fig. 2.
Distribution of various predictors for patients who have not failed (0) and failed (1) on first line ART.
Results
Baseline patient characteristics for complete cohort
A total of 202 patients, of whom 195 HIV patients >18 years of age and all male patients who were initiated on first line ART in 2008, were eligible in the study with more than 6 months of follow-up. These 195 patients contributed 7178 person-years follow-up. The mean age of the patients was 36.54(SD = 7.69). Majority of the patients (65%) were from the age group of 25–45 years of age. Most of the subjects were secondary educated (76.3%) and 93.16% were married. Probable mode of transmission was heterosexual mode for 57% and for remaining 43% gave history of unknown transmission mode. 15.9% of the patients had the CD4 count at ART initiation below 50, 32.8% had between 50–99 and 51.3% had their CD4 count more than equal to 100. The mean weight of the patients was 62 kgs (SD = 8.52) and mean BMI of 21.81 (SD = 2.88). Mean Hemoglobin levels were 12.24 with SD of 2.39 and the average CD4 count at ART initiation was 91 (SD = 47.01) with median of 83. Of the total patients, 18% (n = 35) had opportunistic infections in the form of tuberculosis and herpes zoster. There were two patients (1.0%) who had AIDS. Fig. 3 shows the distribution of various parameters for the groups who failed on first line ART and who did not fail. Fig. 4 gives the distribution of patients by their infection status. Counseling as per the national guidelines were been provided to all the patients. Adherence of the patients was measured as >95 drug adherence. There were 7 patients (3.6%) who were nonadherent to the drugs. The initial cohort of 223 was analyzed for the time taken from HIV diagnosis to first line ART initiation. The average time from HIV diagnosis to first line ART initiation was 51 months (SD = 39) with median time of 42 months. The cohort of 195 patients on first line ART was followed with a minimum follow-up of 6 months and maximum of 60 months with mean of 47.15 months (SD = 15.13) and median follow-up of 49 months. There were 8 (4%) patients who died, and 9 (4.6%) patients who retired from the services after initiation of ART. The baseline characteristics of the cohort with respect to various predictors are depicted in Table 1.
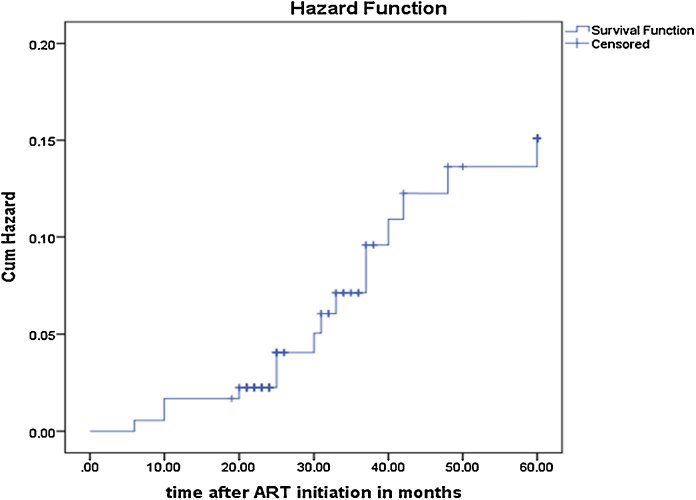
Fig. 3.
Kaplan–Meier Hazard function.
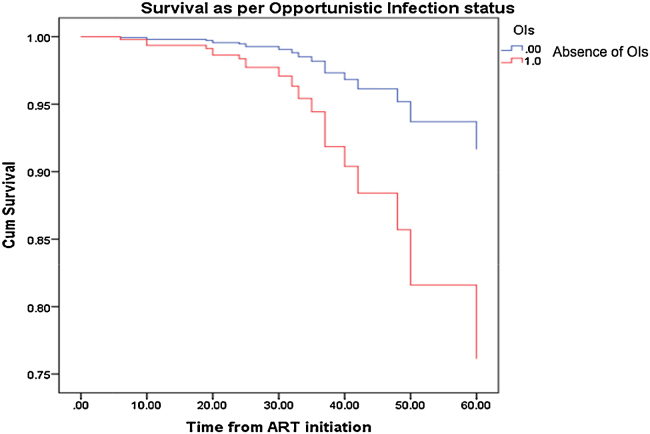
Fig. 4.
Survival as per Opportunistic Infection Status.
Table 1.
Base line characteristics of the cohort of patients on first line ART.
| Variable | Overall | First line ART |
p value | |
|---|---|---|---|---|
| Failed | Not failed | |||
| Age | 39.56 (9.04) | 40.94 (11.24) | 39.41 (8.80) | 0.49 |
| Weight* | 61.84 (8.45) | 55.53 (8.78) | 62.56 (8.13) | 0.001 |
| BMI* | 21.81 (2.84) | 20.41 (2.33) | 21.97 (2.86) | 0.003 |
| Hemoglobin* | 12.27 (2.35) | 10.78 (2.84) | 12.44 (2.24) | 0.023 |
| CD4 count at ART initiation* | 90.80 (47.01) | 51.21 (27.52) | 95.39 (46.69) | 0.000 |
| Presence of opportunistic infections* (%) | 35 (17.95) | 13 (37.14) | 22 (62.85) | 0.000 |
| Drug non adherence* (%) | 7 (3.59) | 5 (71.43) | 2 (28.57) | 0.000 |
Significant at 0.05 level in the group with outcome as first line failure and no first line failure.
Baseline characteristics as per failure status
There were 15 patients who failed on first line ART in the five years of follow-up. The mean weight in the group of patients who failed was slightly lower with 58 years (SD = 7.77) as compared to average age of 62.38 (SD = 8.51) years for the group who did not fail first line ART. There was no significant difference in the age of the two groups (p = 0.49). All the other parameters were also on the lower side in ART failure group compared to others. The hemoglobin levels were less with mean of 10.85 (SD = 3.10) for first line ART failure group as compared to those patients who did not fail with a higher hemoglobin level of 12.38 (SD = 2.28). We found significant difference in the hemoglobin levels in the failed and not failed group with p = 0.023. Similarly the mean BMI in failed group was 20.78 (SD = 2.92) as compared to 19.46 (SD = 2.37) with significant p value of 0.003. The mean CD4 count at ART initiation for the cohort was 53 (SD = 30.69) and median count of 50 for patients who failed first line ART which was at much lower level than those who did not fail with mean of 94 (SD = 45) and median CD4 count of 89. There was statistically significant difference in the CD4 count at ART initiation with p = 0.000. The presence of opportunistic infections as well as drug nonadherence was significantly different (p = 0.000) in two groups with 13 (86%) and 5 (71%) having OIs and who were nonadherent, respectively, in the failed group.
Treatment failure and burden of second line ART people
A total of 195 patients initiated on first line ART were analyzed. There were 15 failures on first line ART who were switched to second line ART yielding 7.69% failure rate. During the 7178 person-years of follow-up the incidence of first line ART failure was 2.09 per 1000 person-years or 0.21 per 100 person-years. The Kaplan–Meier survival analysis gave a mean survival time of 55.6 months (95% confidence interval CI: 53.67–57.62) (Fig. 3). The instantaneous rate of occurrence of first line ART at given time (hazard rate) at end of 1st year is 1.68 (95% CI: 0–3.64), at end of 2nd year 2.25 (95% CI: 0.94–4.4), by end of 3rd year 7.12 (95% CI: 4.5–11.6), by end of 4th year 13.63 (95% CI: 8.7–22.3) and by end of 5th year is 15.09 (95% CI: 7.6–22.6) after first line ART initiation. This implies that if we have 100 patients initiated on first line ART then there would be around 2 patients who would fail on first line ART by the end of first year. Similarly by the end of 5 years of ART, there would be 15 patients who would fail on first line ART.
Predictors of first line ART failure using Cox proportional hazard model
Except for age all variables showed statistically significant difference in two groups. Variables, which were significant in bivariate analysis, were considered for Cox proportional hazard model. As weight and BMI showed multicollinearity as were highly correlated, we included BMI in the multivariate model. Thus BMI, hemoglobin, CD4 at ART initiation, presence or absence of opportunistic infection and drug adherence (Yes/No) were included for Cox proportional hazard analysis. The analysis of the Cox proportional hazard model is shown in Table 2. The analysis brings out that BMI, CD4 count at ART initiation and presence of opportunistic infections are significant predictors of first line ART failure. The hazard ratio, which is ratio of incidence rates, is given in Table 3 with negative β coefficients implying that with unit decrease in the predictor variable there is increased hazard for first line ART failure. For BMI, β = −0.33 and HR = e−0.332 = 0.72 (95% CI = 0.55–0.93). Thus for every unit increase in BMI there is (1-HR) = (1–0.72) = 0.28 i.e. 28% reduction in failing on first line ART. Similarly for every unit increase in baseline CD4 count at ART initiation, there was 5% reduction in failing on first line ART. Patients with opportunistic infections have more than 3.5-fold higher incidence (95% CI: 1.10–12.12) of first line ART failure compared to patients with no opportunistic infections. Other variables namely nonadherence, weight and hemoglobin were not statistically significant. Fig. 4 shows the survival curve as per the presence and absence of opportunistic infections.
Table 2.
Cox proportional hazard model for prediction of first line ART failure.
| Variables in the equation | ||||||
|---|---|---|---|---|---|---|
| B | SE | Significance | HR | 95% CI for HR |
||
| Lower | Upper | |||||
| BMI* | −0.332 | 0.133 | 0.01 | 0.718 | 0.553 | 0.930 |
| Hemoglobin | −0.061 | 0.103 | 0.555 | 0.941 | 0.770 | 1.151 |
| Presence of OIs* | 1.295 | 0.612 | 0.034 | 3.652 | 1.100 | 12.124 |
| Non adherence | 0.941 | 0.643 | 0.143 | 2.562 | 0.727 | 9.028 |
| Baseline CD4 count at ART initiation* | −0.042 | 0.009 | 0.000 | 0.959 | 0.942 | 0.977 |
Significant at 0.05 level of significance.
Table 3.
Expected burden of second line by end of each year.
| Time (years) | First line ART failure | Hazard rate per 1000 patients | Burden of second line ART = expected first line ART failures per 1000 person going on first line ART | 95% confidence interval for expected first line ART failures |
|---|---|---|---|---|
| End of 1st year | 3 | 0.0168 | 17 | (0, 36) |
| End of 2nd year | 4 | 0.0225 | 23 | (1, 44) |
| End of 3rd year | 9 | 0.0712 | 71 | (46, 117) |
| End of 4th year | 14 | 0.1363 | 136 | (87, 224) |
| End of 5th year | 15 | 0.1506 | 151 | (76, 227) |
Burden of second line ART
The Kaplan–Meier analysis gives the hazard rates as given in Table 3. If 1000 HIV people initiating first line ART are followed then by the end of first year of treatment 17 patients (95% CI: 0–36) are expected to fail. Similarly by the end of corresponding second, third, fourth and fifth years, we find that 23 (95% CI: 1–44), 71 (95% CI: 46–117), 136 (95% CI: 87–224) and 151 (95% CI: 76–227) people fail first line ART. It can be seen from Table 3 that the hazards of failure keep increasing over the time periods.
Discussion
To our best knowledge this is the first long-term cohort study of five years to determine failure rate on first line ART among HIV patients. Our study is amongst very few in India and first cohort study in Armed Forces which estimated the rate of failure of first line ART and determined the burden of second line ART.
The beneficial evidence of ART in HIV treatment is documented globally.8, 9 Many countries including India have rolled out free ART programmes.10 The improvements in health in HIV patients are assessed by routine monitoring of viral loads and CD4 counts. Viral load testing is not regularly carried out in many developing countries due to the cost involved and CD4 decline are used as surrogate markers for treatment failure. According to the statistics from UNAIDS and World Health Organisation, India ranks third among the countries having most number of HIV-infected patients and HIV-related deaths in the world; however very limited data on the number of patients in need of second line ART are available. In India around 2.1 million people are living with HIV.11 As per the reports of National AIDS Control Programme, of the 0.6 million HIV people on ART in 2012, 5503 were switched to second line ART.12 Even in armed forces, where management of HIV is more systematic and efficient, the data on burden of second line ART are unavailable.
Our study provided evidence that the first line ART failure rate is much lower with 2.2 per 1000 person-years. The failure rate at the end of first, 2nd, 3rd, 4th and 5th years was 1.68, 3.4, 9.3, 15.8 and 18.7, respectively. The failure rate is much lower as compared to other studies carried out in India as well as other countries. This may be due to good adherence, counseling and regular follow-up of these patients. Also management of HIV patients in armed forces by a rigorous system of Advanced Immunodeficiency centres (AIDC), Immunodeficiency centres IDC and First Line Immunodeficiency centres (FIDC) adds to this lower rate. The structured service education programmes and regular counseling periodically conducted as compared to civil ART centres is also one of the reasons for this low failure rate. The TREAT ASIA Observational study13, 14 documented high rates of treatment failure or modification at 11.6 per 100 patient-years for the cohort initiating ART in 2011–2013. Other studies from India reported similar survival rates. A study from National AIDS Research Institute (NARI)15 reported 85% survival by end of 5 years while another study from north India reported decreasing survival rates of 90%, 87% and 84% by end of 6 months, 1 year and 3 years. Another Indian study by Bachani et al16 analyzing the treatment outcomes of patients enrolled in India's national first-line antiretroviral therapy programme showed 71% survival rate after 2 years of ART. The study also highlighted the predictors of survival and documented that patients with low baseline CD4 count of <50 were significantly more likely to die with an increased hazard of 2.5 compared to patients with baseline CD4 count of more than 50 cells/cmm. A meta analysis17 by WHO reported a failure rate of 1.9 per 100 person-years of follow-up. Further analysis by region revealed the failure rate ranging from 2.64 in Africa, 2.57 in Latin America to 1.11 in Asia.
Detailed analysis of the predictors in our study found that low CD4 count at ART initiation and presence of OIs as significant predictors for failure which corroborates with several other studies 18, 19, 20, 21 with a logical reasoning that low baseline CD4 count causes more opportunistic infections leading to disease progression and more chances of associated ill health and lower compliance due to intolerance. Few studies21 have also documented that patients with lower height for age recordings at ART initiation (HR = 3.25), pediatric patients (HR = 1.85), patients with chronic diarrhea after ART initiation (HR = 3.44) and patients with base line CD4 count below 50 cells/mm3 (HR = 2.30) had high chances of treatment failure.
Our cohort had ART initiation at CD4 count of 200; however the national HIV policy by NACO changed the criteria of ART initiation at CD4 count of <350 in 2010. Armed Forces HIV policy also changed the guidelines of ART initiation at <350 CD4 count in 2010 as recommended in national guidelines by NACO. However TREAT ASIA study has shown that treatment failures and period of ART initiation were not associated. Further, medicine is a continuously evolving science and it may not be sacrosanct that figures of CD4 counts of 350 or even 500 as per new WHO 2013 may remain the guiding principle of treatment for all times to come. In such a scenario we may have to resort to documented failure rate in a particular cohort. One of the limitations of our study was that viral load recordings as well the resistance pattern was not available for all the patients as it was carried out in very few patients. The failure rates are expected to be much more if virologic failure is considered for estimation. Secondly as a consequence of being retrospective cohort study in nature, using health records that had already been collected, not all pertinent risk factors affecting first line ART failure may have been identified and subsequently recorded.
Conclusion
Failure on first line antiretroviral therapy (ART) regimen requires patients to be shifted to more expensive and less tolerable second line drugs. Though the first line ART failure is quite low in the present study pointing out that ART is effective in our settings, we still need to be vigilant for lower BMI, low baseline CD4 count and occurrence of opportunistic infections.
Conflicts of interest
The authors have none to declare.
Acknowledgements
This paper is based on Armed Forces Medical Research Committee Project No 4216/2011 granted and funded by the office of the Directorate General Armed Forces Medical Services and Defence Research Development Organization, Government of India.
The authors are thankful to O/o DGAFMS for granting the project, Mr. S. Shinde, counselor at the ART centre, Dept of Medicine, Dept of Microbiology and Central Disease Registry for all the support provided for the project.
References
- 1.Hima Bindu A., Naga Anusha P. Adverse effects of highly active anti-retroviral therapy (HAART) J Antivir Antiretrovir. 2011;3:060–064. [Google Scholar]
- 2.World Health Organization . 2013. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection, Recommendations for a Public Health Approach.http://www.who.int/hiv/pub/guidelines/arv2013/download/en/index.html [PubMed] [Google Scholar]
- 3.World Health Organization . 2014. HIV/AIDS. Available from: http://www.who.int/mediacentre/factsheets/fs360/en/ Accessed November 12. [Google Scholar]
- 4.Kanapathipillai R., McGuire M., Mogha R., Szumilin E., Heinzelmann A., Pujades-Rodríguez M. Benefit of viral load testing for confirmation of immunological failure in HIV patients treated in rural Malawi. Trop Med Int Health. 2011;16(12):1495–1500. doi: 10.1111/j.1365-3156.2011.02874.x. [DOI] [PubMed] [Google Scholar]
- 5.WHO U., UNICEF . 2009, September. Towards universal access: scaling up priority HIV/AIDS interventions in the health sector—progress report. [Google Scholar]
- 6.Boulle A., Van Cutsem G., Hilderbrand K. Seven-year experience of a primary care antiretroviral treatment programme in Khayelitsha, South Africa. AIDS. 2010;24(February (4)):563–572. doi: 10.1097/QAD.0b013e328333bfb7. [DOI] [PubMed] [Google Scholar]
- 7.Zhou J., Paton N.I., Ditangco R. Experience with the use of a first-line regimen of stavudine, lamivudine and nevirapine in patients in the TREAT Asia HIV Observational Database. HIV Med. 2007;8:8–16. doi: 10.1111/j.1468-1293.2007.00417.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammer S.M., Squires K.E., Hughes M.D. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic millimeter or less. AIDS Clinical Trials Group 320 Study Team. N Engl J Med. 1997;337:725–733. doi: 10.1056/NEJM199709113371101. [DOI] [PubMed] [Google Scholar]
- 9.Palella F.J., Delaney K.M., Moorman A.C. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853–860. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- 10.Ghate M., Tripathy S., Gangakhedkar R. Use of first line antiretroviral therapy from a free ART programme clinic in Pune, India – a preliminary report. Indian J Med Res. 2013;137(5):942–949. [PMC free article] [PubMed] [Google Scholar]
- 11.Department of AIDS Control, National AIDS Control Organization . Ministry of Health & Family Welfare, Government of India; 2013. Annual report 2012–2013. [Google Scholar]
- 12.Khan S., Das M., Andries A. Second-line failure and first experience with third-line antiretroviral therapy in Mumbai, India. Global Health Action. 2014:7. doi: 10.3402/gha.v7.24861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou J., Kumarasamy N., Ditangco R. The TREAT Asia HIV observational database: baseline and retrospective data. J Acquir Immune Defic Syndr (1999) 2005;38(2):174–179. doi: 10.1097/01.qai.0000145351.96815.d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boettiger D.C., Kerr S., Ditangco R. Trends in first-line antiretroviral therapy in Asia: results from the TREAT Asia HIV observational database. PLOS ONE. 2014;9(9):e106525. doi: 10.1371/journal.pone.0106525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma S.K., Dhooria S., Prasad K.T. Outcomes of antiretroviral therapy in a northern Indian urban clinic. Bull World Health Organ. 2010;88:222–226. doi: 10.2471/BLT.09.068759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bachani D., Garg R., Rewari B.B. Two-year treatment outcomes of patients enrolled in India's national first-line antiretroviral therapy programme. Natl Med J India. 2010;23:7–12. [PubMed] [Google Scholar]
- 17.Renaud-Théry F., Duncombe C., Kerr S., Thierry S., Perriens J. World Health Organization; Geneva: 2008. Adult antiretroviral therapy in resource limited settings: a systematic review of first-line failure and attrition rates. [Google Scholar]
- 18.Singh A., Agarwal A., Chakravarty J. Predictive markers of failure of first line anti retroviral treatment in HIV patients in India. J AIDS Clin Res. 2013;4:210. [Google Scholar]
- 19.Robbins G.K., Daniels B., Zheng H. Predictors of antiretroviral treatment failure in an urban HIV clinic. J Acquir Immune Defic Syndr. 2007;44:30–37. doi: 10.1097/01.qai.0000248351.10383.b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Srasuebkul P., Ungsedhapand C., Ruxrungtham K. Predictive factors for immunological and virological endpoints in Thai patients receiving combination antiretroviral treatment. HIV Med. 2007;8:46–54. doi: 10.1111/j.1468-1293.2007.00427.x. [DOI] [PubMed] [Google Scholar]
- 21.Bacha T., Tilahun B., Worku A. Predictors of treatment failure and time to detection and switching in HIV-infected Ethiopian children receiving first line anti-retroviral therapy. BMC Infect Dis. 2012;12:197. doi: 10.1186/1471-2334-12-197. [DOI] [PMC free article] [PubMed] [Google Scholar]