Abstract
Objective:
To compare the effects of an isokinetic fatigue protocol and a functional fatigue protocol on time to stabilization (TTS), ground reaction force (GRF), and joint kinematics during a jump landing.
Design and Setting:
Subjects were assessed on 2 occasions for TTS, GRF, and joint kinematics immediately before and after completing a fatigue protocol. One week separated the 2 sessions, and the order of fatigue protocols was randomly assigned and counterbalanced.
Subjects:
Twenty healthy male (n = 8, age = 21.8 ± 1.4 years, height = 180.6 ± 7.6 cm, and mass = 74.1 ± 13.0 kg) and female (n = 12, age = 22.2 ± 2.1 years, height = 169.3 ± 9.8 cm, and mass = 62.5 ± 10.1 kg) subjects volunteered to participate.
Measurements:
Subjects performed 2-legged jumps equivalent to 50% of maximum jump height, followed by a single-leg landing onto the center of a forceplate 70 cm from the starting position. Peak vertical GRF and vertical, medial-lateral, and anterior-posterior TTS were obtained from forceplate recordings. Maximum ankle dorsiflexion, knee-flexion, and knee-valgum angles were determined using 3-dimensional motion analysis.
Results:
A 2-way analysis of variance with repeated measures revealed no significant differences when comparing TTS, GRF, and joint kinematics after isokinetic and functional fatigue protocols.
Conclusions:
No difference was noted between isokinetic and functional fatigue protocols relative to dynamic stability when landing from a jump.
Keywords: time to stabilization, ground reaction force, postural stability, kinematics
Injuries to the knee and ankle are common in today's athletes and are most prevalent in cutting and jumping sports such as volleyball, football, soccer, and basketball.1–4 Although these injuries are often the result of direct contact, noncontact mechanisms such as landing from a jump also occur frequently.1–4 For example, Gray et al4 reported that 58% of all injuries in female basketball players occurred while landing from a jump. Similarly, Goodwin-Gerberich et al3 reported that jump landings during volleyball competition were associated with 63% of all reported injuries, including 61% of knee injuries. Successful landing from a jump requires strength, stability, and balance, which are also critical for providing inherent protection against joint injury. Thus, it is possible that the high rates of injury mentioned above were the result of strength deficits or impaired stability and balance. Jump landings involve the dissipation of kinetic energy and are often characterized as soft or stiff.5,6 Because the ground reaction force (GRF) is greater during a stiffer landing,5,6 GRF can be used to identify changes in landing stiffness. It has been suggested that increased muscular stiffness during landing would provide more joint stability and protection against joint injury.7 Both preparatory and reactive activities of the lower extremity musculature help to provide this stiffness and the dynamic stability required to protect the joints from injury during these landings.7 Thus, any delay or impairment in muscle activity and stiffness could allow excessive motion in the knee or ankle, possibly leading to injury.
Neuromuscular control plays a major role in dynamic joint stability and the body's inherent protection from injury,7–9 and neuromuscular fatigue can impair this control and stabil-ity.10–16 Time to stabilization (TTS) is a more recent measure of neuromuscular control that incorporates both sensory and mechanical systems to master the complex task of a jump landing. It is a quantifiable forceplate measure used to evaluate postural stability that, in short, describes the body's ability to minimize postural sway when transitioning from a dynamic to a static state.17 In addition, TTS can be considered a more functional test than traditional measures such as joint position sense and kinesthesia. Therefore, this measure provides a functional method for assessing the effects of fatigue on neuromuscular control and dynamic stability. Traditionally, isokinetic protocols have been used to cause fatigue in muscles and assess the effects of fatigue on neuromuscular control.10,12,13,15,16 These protocols generally consist of open kinetic chain movements and involve isolated joint motions and muscle groups. Thus, the ability to generalize the results of these studies to athletic training and competition can be questioned. More functional protocols would likely provide more information related to the changes that occur during true athletic training and competition. However, the research involving functional fatigue protocols is very limited, and comparisons with isokinetic protocols have not been conducted. Therefore, our purpose was to compare an isokinetic fatigue protocol (IFP) with a more functional fatigue protocol (FFP) using measures of dynamic stability during a jump landing. We hypothesized that dynamic stability would be impaired in the fatigued state as compared with the prefatigue state. Similarly, we hypothesized that this impairment would be more pronounced after the FFP.
METHODS
Subjects
Twenty healthy subjects, 8 men (age = 21.8 ± 1.4 years, height = 180.6 ± 7.6 cm, and mass = 74.1 ± 13.0 kg) and 12 women (age = 22.2 ± 2.1 years, height = 169.3 ± 9.8 cm, and mass = 62.5 ± 10.1 kg), participated in this study. All subjects were free from lower extremity injury, central nervous system injury, and any disorder that might affect neuromuscular control. Before participating, subjects read and signed an informed consent agreement that was approved by the university's institutional review board, which also approved the study.
Instrumentation
We measured jump landing vertical, anterior-posterior, and medial-lateral GRF and moments of force at a frequency of 600 Hz using a Bertec triaxial forceplate (Bertec Corp, Columbus, OH). The forceplate uses a series of force transducers to record the GRF and its point of application over time. After sampling, the forceplate data underwent an analog-to-digital conversion and were stored on a personal computer using data-acquisition and data-analysis software (Peak Performance Technologies, Englewood, CO). The jump-landing motions were captured at a frequency of 60 Hz using 2 motion recorder cameras (US JVC Corp, Fairfield, NJ). The cameras were positioned anterolateral and posterolateral to the forceplate, so that both cameras could record the position of each retroreflective marker placed on the lateral aspect of the greater femoral trochanter, mid thigh, knee joint line, mid shank, lateral malleolus, calcaneus, and head of the fifth metatarsal, thus enabling 3-dimensional analysis (Figure 1).18 The forceplate served as the trigger for video acquisition. The video cameras and forceplate were time synchronized using the Peak Motus video-analysis system (Peak Performance Technologies). A calibration frame (16 control points: 1.3 m × 1.1 m × 0.9 m) was used for 3-dimensional space reconstruction. The sampling of video recording was initiated 50 ms before initial contact (determined from GRF recordings) and continued for 20 seconds after contact.
Figure 1.
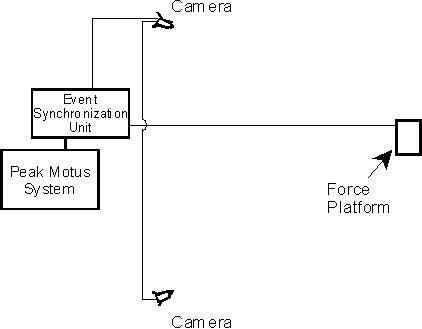
Camera setup.
An isokinetic dynamometer (KinCom 125AP, Chattanooga Group, Hixson, TN) was integrated with a computer, and appropriate software was used to assess plantar-flexion and dorsiflexion peak torque (PT) and to induce plantar-flexor and dorsiflexor fatigue during the IFP. The manufacturer's specifications for ankle plantar-flexion and dorsiflexion testing were followed during all procedures. To determine functional fatigue, we used an infrared timing device (Brower Timing Systems, Salt Lake City, UT) to time subjects during the FFP. The device transmitters project an infrared beam at both the start and finish lines of the functional fatigue course. Time began as the subjects crossed the starting beam and ended as they crossed the finish line.
Procedures
Each subject reported to the research laboratory on 2 occasions. At the first session, a medical history questionnaire was completed. After being cleared to participate, the subjects were assessed for their maximum vertical jump height (Vertmax). To begin the measure, we instructed each subject to stand next to a Vertec vertical jump tester (Sports Imports, Columbus, OH) and reach up and touch the highest vane possible (in 1.27-cm increments) while maintaining a double-leg stance on the toes. We recorded the height as the subject's standing reach height. We then instructed the subjects to perform a maximum jump using a countermovement jump technique and touch the highest vane possible. Each subject performed 3 trials, and the maximum height was recorded. Maximum vertical jump height was determined as the difference between the maximum height reached during the countermovement jump and the standing-reach height.
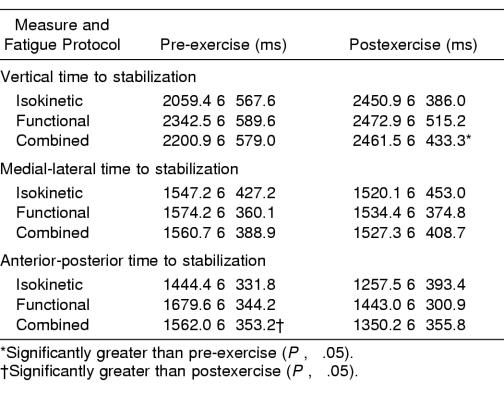
Immediately after Vertmax testing, we demonstrated the jump-landing task and TTS protocol to each subject. The jump-landing task consisted of a single-leg landing from a jump height equivalent to 50% of the Vertmax.19,20 To begin this task, each subject stood 70 cm from the center of the forceplate and jumped with both legs toward the center of the plate (Figure 2A). We instructed subjects to reach up and touch a vane on the Vertec stand indicating 50% of the Vertmax before landing on the forceplate. We further instructed subjects to land on the stance leg, stabilize as quickly as possible, and balance with their hands on their hips while facing straight ahead (Figure 2B). The stance leg was defined as the leg with which the participant did not prefer to kick a ball. We allowed subjects to practice this task, giving them as many practice trials as required to ensure consistent performance before beginning the actual experimental trials. Once subjects felt comfortable with the protocol, we pretested them for TTS, GRF, and joint kinematics during the jump-landing task. Each subject performed 3 trials of the jump-landing task and TTS protocol. If a subject lost balance and touched the floor with the contralateral limb, the trial was discarded and repeated. Similarly, if a short additional hop occurred on landing, the trial was discarded and repeated.
Figure 2.
Jump protocol. A, Starting position. B, Ending position.
After completing the pretest trials, subjects performed 1 of 2 fatigue protocols. Isokinetic fatigue was induced using the KinCom isokinetic dynamometer. As part of a warm-up, 3 submaximal repetitions were first performed to familiarize the subjects with the dynamometer. Three maximal repetitions were then performed using the overlay mode to complete the warm-up. After a 1-minute rest period, each subject was assessed for plantar-flexor and dorsiflexor concentric PT at 30°·s−1 and 120°·s−1, respectively.21,22 Fatigue was then induced using continuous concentric contractions of the plantar flexors and dorsiflexors at the same velocities. Fatigue was determined as the point at which the plantar-flexion and dorsiflexion torques decreased below 50% of their respective PT values for 3 consecutive repetitions.10,15,16,21 The FFP began with an instructional and practice walk through the protocol course. To allow familiarization and warm-up, practice occurred at all 6 stations:
The Southeast Missouri (SEMO) Agility Drill. The SEMO agility drill consists of a series of forward sprints, diagonal back pedaling, and side shuffling, which was completed 3 times within a regulation-size key of a basketball court.
Plyometric box jumps. Plyometric box jumps involve a series of quick, powerful contractions of the lower extremity musculature to jump, land, stabilize, and jump again onto 3 boxes at heights of 31, 46, and 61 cm placed 61 cm apart from each other.
Side-to-side bounds. Side-to-side bounds are a series of 30 lateral jumps in alternating opposite directions covering a distance of 0.6 m with each jump.
Minitramp jumps. Minitramp jumps consist of a series of 30 small jumps incorporating vertical and horizontal movement on and off a trampoline.
Cocontraction arc. The cocontraction arc is a series of ten 180° arcs completed by side shuffling while resisting tension induced by an elastic cord. All subjects were required to keep the elastic cord taut to maintain the radius of the arc.
Two-legged hop sequence. The 2-legged hop sequence uses a series of markers randomly spaced over a distance of 304.8 cm. Subjects jumped onto and immediately off each marker toward the next marker. The markers were placed so that the 2-legged jumps were multidirectional for the 3 repetitions.
After familiarization, each subject completed a timed run at maximal effort to serve as baseline, which was then followed by 1 minute of rest. The time to complete each run through the course was measured using the infrared timing device. Subjects then completed successive runs through the course as quickly as possible until fatigue was induced. Fatigue was determined as the point at which the time to complete the course increased by 50% compared with the initial maximal effort run for each subject.23,24
Posttesting procedures, identical to those used to collect pretest data, were initiated within 1 minute after completion of the fatigue protocol. Subjects were not allowed any practice trials at this time, however. After posttesting, we instructed subjects to report for a second session at least 1 week later to allow sufficient recovery time from the initial fatigue protocol. Subjects reported back to the laboratory where they performed the same jump landing protocol before and after completing the second fatigue protocol. The order of the fatigue protocols was randomized and counterbalanced to eliminate any learning effect.
Data Reduction
We calculated TTS using 2 methods. Vertical TTS was established as the time when the vertical force component reached and stayed within 5.0% of the subject's body weight after landing.25,26 Medial-lateral and anterior-posterior TTS were determined using sequential estimation.25 This technique incorporates an algorithm to calculate a cumulative average of the data points in a series by successively adding 1 point at a time. This cumulative average was then compared against the overall series mean. A subject was considered stable when the sequential average remained within ±0.25 SDs of the overall series mean. The series consisted of all raw data points within the first 3 seconds after touchdown. Peak vertical GRF after foot strike was determined by the Peak Performance software. The raw peak vertical GRF data were then expressed relative to the subject's body weight. For each measure, the mean of the 3 jump landing trials was used in the analysis.
We assessed lower extremity kinematics during the jump-landing trials using the video cameras and the Peak Motus motion analysis system. After each testing session, the trials were automatically digitized, and the 3-dimensional positional data were scaled and smoothed, using a fourth-order Butterworth filter with an optimal cutoff frequency determined by the Jackson knee-point method27 and Peak Performance software. Coordinates were expressed relative to a global reference frame with axes pointing in the forward (x), lateral (y), and vertical (z) directions. For each subject, all trials were digitized, and the mean maximum knee- and ankle-flexion and maximum knee-valgus angles were used in all subsequent analyses. Three-dimensional ankle flexion was determined using the locations of the fifth metatarsal and calcaneus and the lateral malleolus and lateral knee joint-line markers. Similarly, the 3-dimensional knee-flexion angle was determined using the locations of the greater trochanter, lateral knee joint-line, and lateral malleolus markers. Knee valgus was measured as the greatest linear difference between the y coordinates of the greater trochanter and lateral knee joint-line markers from 1 frame before touchdown and the point of the greatest valgus angle after touchdown.
Statistical Analysis
Separate 2 × 2 analyses of variance with repeated measures on each factor were calculated for each of the dependent variables. The 2 within-subject factors included fatigue protocol, with 2 levels (IFP and FFP), and time, with 2 levels (pre- and postfatigue testing). The level of statistical significance for all tests was set at .05.
RESULTS
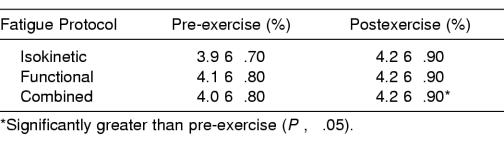
Time to Stabilization
Significant time main effects were observed for the vertical (F1,19 = 9.17; P = .007) and anterior-posterior (F1,19 = 9.20; P = .008) TTS (Table 1). Vertical TTS increased from before to after exercise, whereas the anterior-posterior TTS decreased. A significant protocol main effect for the anterior-posterior TTS was noted (F1,19 = 4.61; P = .047) because it took longer to stabilize during the FFP session (1561.3 ± 340.3 ms) than during the IFP session (1350.9 ± 371.9 ms). However, main effects were not significant for protocol for the vertical TTS (F1,19 = 4.96; P = .490) or for time (F1,19 = .180; P = .676) or protocol (F1,19 = .148; P = .706) for the medial-lateral TTS. The type of fatigue protocol had no effect on TTS because no significant protocol × time interactions were observed for the vertical (F1,19 = 2.05; P = .169), anterior-posterior (F1,19 = .001; P = .984), or medial-lateral (F1,19 = .019; P = .893) directions.
Table 1.
Time to Stabilization
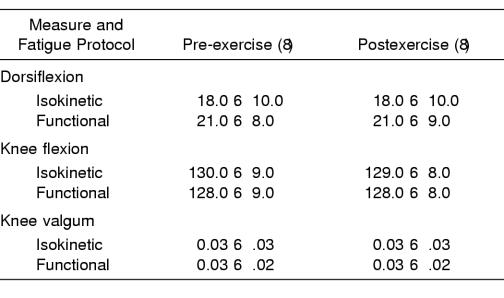
Ground Reaction Force
A significant time main effect was seen (F1,19 = 9.59; P = .006) because the peak postexercise GRF was significantly larger than that at pre-exercise (Table 2). However, no significant protocol main effect was demonstrated (F1,19 = 1.39; P = .257), and no protocol × time interaction was observed (F1,19 = 2.73; P = .115).
Table 2.
Peak Vertical Ground Reaction Force
Joint Kinematics
The maximum ankle-flexion scores, as measured from the neutral position, ranged from 38° of plantar flexion to 1° of dorsiflexion at pre-exercise and from 35° of plantar flexion to 4° of dorsiflexion at postexercise (Table 3). The maximum knee-flexion scores ranged from 111° to 146° at pre-exercise and from 114° to 143° at postexercise, whereas the maximum knee-valgum scores ranged from −.009 m to 0.09 m and from −.008 m to 0.084 m at pre-exercise and postexercise, respectively.
Table 3.
Maximum Joint Angles
No significant time main effects were observed for maximum ankle flexion (F1,19 = .02; P = .905), knee flexion (F1,19 = .58; P = .456), and knee valgum (F1,19 = .12; P = .737). Similarly, protocol main effects were not significant for the ankle (F1,19 = .94; P = .344), knee flexion (F1,19 = .67; P = .425), or knee valgum (F1,19 = .07; P = .796). The type of fatigue protocol had no effect on joint kinematics because protocol × time interactions for maximum ankle flexion (F1,19 = .06; P = .803), knee flexion (F1,19 = .21; P = .652), and knee valgum (F1,19 = .79; P = .386) were not significant.
DISCUSSION
Our purpose was to determine if fatigue induced in a manner that mimics athletic activity would have a greater effect on TTS, GRF, and joint kinematics compared with isokinetically induced fatigue. We hypothesized that fatigue would impair dynamic stability and increase TTS, GRF, and maximum joint angles after a jump landing. We further hypothesized that this impairment would be more pronounced after the FFP. Our hypotheses were partially supported because vertical TTS and GRF increased from pre-exercise to postexercise values. However, no differences were observed when comparing the 2 fatigue protocols. We also failed to observe increases in anterior-posterior and medial-lateral TTS and maximum joint angles.
We are the first to directly compare an IFP with an FFP using a measure of neuromuscular control. It is well accepted that neuromuscular control plays a major role in dynamic joint stability and the body's inherent protection from injury8,9 and that neuromuscular fatigue can impair this control and stability. For example, muscle fatigue has been shown to impair shoulder kinesthesia10,13 and shoulder position sense,15,28 whereas similar observations have been made at the knee14 and ankle.11 However, not all groups have shown deficits in neuromuscular control under fatigue conditions.28 Traditionally, IFPs have been used to fatigue muscles and assess the resulting effects.10,12,13,15,16 Fatigue is generally determined as a failure to maintain a required or expected force, which can be objectively determined when induced using an isokinetic dynamometer. We defined isokinetic fatigue as the inability to maintain at least 50% of plantar-flexion and dorsiflexion PT over 3 consecutive repetitions. We chose this threshold because it had been used as an indicator of fatigue that impaired neuromuscular function.10,11,15,16,21,27 For example, Yaggie and McGregor16 used this criteria for plantar-flexor and dorsiflexor fatigue when they observed impairments in postural control. Similarly, Carpenter et al10 used a similar protocol to induce fatigue in the internal rotators and observed deficits in shoulder kinesthesia. In contrast to these findings, we did not observe changes in TTS and joint kinematics after isokinetic fatigue. Yaggie and McGregor16 noted that the changes in postural control were transient and recovered within 20 minutes. Time should not have influenced our findings because the subjects began the jump-landing task within 1 minute after exercise.
Various measures of neuromuscular control have been used to examine the influence of fatigue. Many authors used measures of kinesthesia10 and position sense,28 which generally consisted of isolated joint movements performed in an open kinetic chain. Similarly, Skinner et al14 used open kinetic chain movements to examine both measures at the knee. However, during functional tasks, both open and closed kinetic chain movements occurred, involving more than one joint and muscle group. Taking this into consideration, Yaggie and McGregor16 used a measure of postural sway and observed impairments subsequent to an ankle-fatigue protocol. A measure of postural sway may be considered more functional because it involves more than one joint and is performed in a closed kinetic chain position. Our measure of TTS is much more dynamic than these measures and more difficult to perform because it requires strength, coordination, balance, and stability. Thus, it is possible that TTS is not sensitive enough to detect changes caused by fatigue. Although we did observe changes in vertical TTS as a result of fatigue, we failed to observe changes in anterior-posterior or medial-lateral TTS. Only one other group has reported changes in TTS after fatigue.24 As we did, they used an FFP protocol and observed an increase in vertical TTS. However, these authors did not report anterior-posterior or medial-lateral TTS, so whether changes occurred is unknown.
We also observed an increase in peak vertical GRF after fatigue. However, the type of fatigue had no effect on this measure. This finding might have been due to an inability of the quadriceps and triceps surae muscles to eccentrically decelerate the body from a jump landing. This inability to control deceleration creates a more unimodal, or flatfoot, landing style, associated with a more extended body position and increased GRF during landings. However, if this had occurred, we would have expected greater changes after the FFP. Although the IFP involved the triceps surae, only the FFP would have resulted in quadriceps fatigue. It is also possible that a more extended body position during landing would have caused a decreased knee-flexion angle at foot strike. A flexed knee at foot strike has been shown to decrease GRF, in part because it allows for a better angle of pull for the quadriceps muscle to decelerate the body during the jump landing.5,29 However, this is speculation because we did not assess knee angle at foot strike. We expected a decreased stability and a stiffer landing after fatigue; thus, these changes partially supported our initial hypotheses.
During a forward jump landing, the musculature must decelerate and stabilize the body's center of mass as it travels in a downward and anterior direction. A successful landing depends on the body's ability to resist the collapse of the lower extremities by applying extensor moments of force to reduce the body's downward velocity to zero without injury.5 The extensor moments primarily work eccentrically at the hip and knee to absorb the kinetic energy of the landing task. In fact, Zhang et al6 suggested that eccentric strength and neuromuscular control of the lower extremity are vital to the consistency and safety of the lower extremity during landings. It has been shown that ankle musculature activity begins first at landing, followed by the knee and hip musculature.26 Kovács et al30 reported that the largest mean power was produced by the ankle plantar flexors during forefoot landings, followed by the knee and hip extensors. Forefoot landings accounted for 90% of the landings in our study. Thus, it is possible that plantar-flexor and dorsiflexor fatigue alone would not impair TTS and joint kinematics after a jump landing because the nonfatigued muscles of the knee and hip would continue to provide stability. Myers et al28 reported similar findings in shoulder position sense subsequent to internal and external rotator fatigue. However, this protocol failed to influence performance on a single-arm stability test (similar to a single-leg stability test), as determined by sway velocity. Similar to our tests, Myers et al28 induced fatigue using an isokinetic protocol. Thus, generalizing the results to athletic training and competition, which combines open and closed kinetic chain activities and involves numerous joints and muscle groups, can be questioned. In an attempt to induce fatigue in a more functional manner, Johnston et al12 used a closed kinetic chain isokinetic protocol. This type of fatigue resulted in both unilateral and bilateral static postural-control deficits. However, they observed no changes in dynamic postural control. Their results may not be generalized to the fatigue that occurs during athletic training and competition because their protocol was performed in a single, controlled plane and was limited to the hip, knee, and ankle joints. Taking this into consideration, our FFP was designed to mimic common movements that would occur on the field or court and were not limited to a single plane or to the lower extremity. We defined functional fatigue as the point at which the time to complete the course increased by 50% compared with the initial maximal effort run for each subject. We would expect the increased time to complete the course to involve a combination of ankle, knee, and hip muscle fatigue, as well as trunk and upper extremity fatigue. However, this type of fatigue did not have an effect on TTS or joint kinematics. As previously mentioned, it is possible that measures of TTS and joint kinematics during a jump-landing task are not sensitive enough to detect changes in healthy individuals, even when multiple muscle groups are fatigued. Several landing protocols have been used previously to measure TTS and dynamic stability, including forward and lateral step-down tests and single-leg hop tests.18–20,24,25
In many of these studies, previously injured subjects were compared with a healthy population.19,20,24,25 The results suggested that subjects suffering from functional ankle instability19,20,24 and subjects with anterior cruciate ligament deficiencies25 experience increased (longer) TTS scores than healthy subjects. We used only healthy subjects in the present investigation and failed to observe changes under fatigue conditions.
One potential limitation to our study and others investigating fatigue is subject effort. Although the subjects were instructed to give maximal effort during exercise, it is possible that reduced effort, as opposed to actual fatigue, affected performance. During the IFP, we required the plantar-flexion and dorsiflexion torques to decrease to less than 50% of their respective PT values for 3 consecutive repetitions. One reason for this criterion is to account for a lapse in effort, but the possibility of such a lapse is not completely eliminated. It is important to note that the effects of subject effort are not limited to isokinetic fatigue because reduced effort would also increase the time to complete the FFP. We would expect that changes resulting from reduced effort, as opposed to actual fatigue, would not affect our stability measures. Thus, various levels of subject effort could have affected our results. Similarly, we do not know the extent of the central contribution to fatigue. Because of the way we induced both isokinetic and functional fatigue, we assumed that the primary contribution occurred at the periphery. However, we must also assume that some contribution was made by central factors. This assumption is based on previous reports that both central and peripheral mechanisms contribute to the fatigue observed during sustained and repeated maximum voluntary isometric contractions of the plantar flexors and dorsiflexors.31,32 We did not control or monitor factors that can influence central fatigue, such as caffeine ingestion, hypoglycemia, and sleep loss. Individual differences in any of these factors might have influenced our results. One limitation more specific to our FFP was that we had no way to objectively determine the extent of fatigue for each muscle group. Thus, we had no way of determining the contribution of each group or joint to overall fatigue. It is also possible that cardiorespiratory limitations affected the time to complete the course. Although these limitations would influence the occurrence of fatigue (based on our functional definition), they would not likely alter the TTS and joint kinematics after the jump landing. This measure is anaerobic in nature and occurs over a short duration.
CONCLUSIONS
Our results suggest that isolated ankle musculature fatigue induced isokinetically can cause functional changes similar to those after fatigue induced in a more functional manner. Thus, findings from an IFP could potentially be generalized to changes occurring during athletic training and competition. Our observations also suggest that a more strenuous fatigue protocol might be required to detect changes when complex neuromuscular control measures are examined. It would be beneficial for future researchers to focus on comparing FFPs and IFPs on other measures of neuromuscular control, such as proprioception and postural stability. It would also be helpful to compare these protocols in an injured population.
REFERENCES
- 1.Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34:86–92. [PMC free article] [PubMed] [Google Scholar]
- 2.Ekstrand J, Gillquist J. Soccer injuries and their mechanisms: a prospective study. Med Sci Sports Exerc. 1983;15:267–270. doi: 10.1249/00005768-198315030-00014. [DOI] [PubMed] [Google Scholar]
- 3.Goodwin-Gerberich SG, Luhmann S, Finke C, Priest JD, Beard BJ. Analysis of severe injuries associated with volleyball activities. Physician Sportsmed. 1982;15(8):75–79. [Google Scholar]
- 4.Gray J, Taunton JE, McKenzie DC, Clement DB, McConkey JP, Davidson RG. A survey of injuries to the anterior cruciate ligament of the knee in female basketball players. Int J Sports Med. 1985;6:314–316. doi: 10.1055/s-2008-1025861. [DOI] [PubMed] [Google Scholar]
- 5.Devita P, Skelly WA. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med Sci Sports Exerc. 1992;24:108–115. [PubMed] [Google Scholar]
- 6.Zhang SN, Bates BT, Dufek JS. Contributions of lower extremity joints to energy dissipation during landings. Med Sci Sports Exerc. 2000;32:812–819. doi: 10.1097/00005768-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Riemann BL, Lephart SM. The sensorimotor system, II: the role of proprioception in motor control and functional joint stability. J Athl Train. 2002;37:80–84. [PMC free article] [PubMed] [Google Scholar]
- 8.Aune AK, Nordsletten K, Skjeldal S, Madsen JE, Ekeland A. Hamstrings and gastrocnemius co-contraction protects the anterior cruciate ligament against failure: an in vivo study in the rat. J Orthop Res. 1995;13:147–150. doi: 10.1002/jor.1100130122. [DOI] [PubMed] [Google Scholar]
- 9.Lephart SM, Henry TJ. Functional rehabilitation for the upper and lower extremity. Orthop Clin North Am. 1995;26:579–592. [PubMed] [Google Scholar]
- 10.Carpenter JE, Blasier RB, Pellizzon GG. The effects of muscle fatigue on shoulder joint position sense. Am J Sports Med. 1998;26:262–265. doi: 10.1177/03635465980260021701. [DOI] [PubMed] [Google Scholar]
- 11.Forestier N, Teasdale N, Nougier V. Alteration of the position sense at the ankle induced by muscular fatigue in humans. Med Sci Sports Exerc. 2002;34:117–122. doi: 10.1097/00005768-200201000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Johnston RB, 3rd, Howard ME, Cawley PW, Losse GM. Effect of lower extremity muscular fatigue on motor control performance. Med Sci Sports Exerc. 1998;30:1703–1707. doi: 10.1097/00005768-199812000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Pedersen J, Lönn J, Hellström F, Djupsjöbacka M, Johansson H. Localized muscle fatigue decreases the acuity of the movement sense in the human shoulder. Med Sci Sports Exerc. 1999;31:1047–1052. doi: 10.1097/00005768-199907000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Skinner HB, Wyatt MP, Hodgdon JA, Conard DW, Barrack RL. Effect of fatigue on joint position of the knee. J Orthop Res. 1986;4:112–118. doi: 10.1002/jor.1100040115. [DOI] [PubMed] [Google Scholar]
- 15.Voight ML, Hardin JA, Blackburn TA, Tippett S, Canner GC. The effects of muscle fatigue on and the relationship of arm dominance to shoulder proprioception. J Orthop Sports Phys Ther. 1996;23:348–352. doi: 10.2519/jospt.1996.23.6.348. [DOI] [PubMed] [Google Scholar]
- 16.Yaggie JA, McGregor SJ. Effects of isokinetic ankle fatigue on the maintenance of balance and postural limits. Arch Phys Med Rehabil. 2002;83:224–228. doi: 10.1053/apmr.2002.28032. [DOI] [PubMed] [Google Scholar]
- 17.Ross SE, Guskiewicz KM. Time to stabilization: a method for analyzing dynamic postural stability. Athl Ther Today. 2003;8(3):37–39. [Google Scholar]
- 18.Caulfield BM, Garrett M. Functional instability of the ankle: differences in patterns of ankle and knee movement prior to and post landing in a single leg jump. Int J Sports Med. 2002;23:64–68. doi: 10.1055/s-2002-19272. [DOI] [PubMed] [Google Scholar]
- 19.Ross SE, Guskiewicz KM, Yu B. Time to stabilization differences in functionally unstable and stable ankles [abstract] J Athl Train. 2002;37:S-22. [Google Scholar]
- 20.Ross SE, Guskiewicz KM, Yu B. Comparison of time to stabilization measures in functionally unstable versus stable ankles [abstract] J Athl Train. 2001;36:S-76. [Google Scholar]
- 21.Joyce CJ, Perrin DH, Arnold BL, Granata KP, Gansneder BM, Gieck JH. Dorsiflexor and plantar flexor muscle fatigue decreases postural control [abstract] J Athl Train. 2001;36:S-32. [Google Scholar]
- 22.Ochsendorf DT, Mattacola CG, Arnold BL. Effects of orthotics on postural sway following fatigue of the plantar flexors and dorsiflexors. J Athl Train. 2000;35:26–30. [PMC free article] [PubMed] [Google Scholar]
- 23.Douex AT, Horodyski MB, Kaminski TW, Dodd SL, Rozea G. The effects of muscle fatigue on lower body proprioception as measured by dynamic postural stability [abstract] J Athl Train. 2000;35:S-15. [Google Scholar]
- 24.Shills JJ, Kaminski TW, Tillman MD. Comparing time to stabilization values following an acute bout of intensive exercise in those with functional ankle instability [abstract] J Athl Train. 2003;38:S-50. [Google Scholar]
- 25.Colby SM, Hintermeister RA, Torry MR, Steadman JR. Lower limb stability with ACL impairment. J Orthop Sports Phys Ther. 1999;29:444–451. doi: 10.2519/jospt.1999.29.8.444. [DOI] [PubMed] [Google Scholar]
- 26.McKinley P, Pedotti A. Motor strategies in landing from a jump: the role of skill in task execution. Exp Brain Res. 1992;90:427–40. doi: 10.1007/BF00227257. [DOI] [PubMed] [Google Scholar]
- 27.Jackson KM. Fitting of mathematical functions to biomechanical data. IEEE Trans Biomed Eng. 1979;26:122–124. doi: 10.1109/tbme.1979.326551. [DOI] [PubMed] [Google Scholar]
- 28.Myers JB, Guskiewicz KM, Schneider RA, Prentice WE. Proprioception and neuromuscular control of the shoulder after muscle fatigue. J Athl Train. 1999;34:362–367. [PMC free article] [PubMed] [Google Scholar]
- 29.McNair PJ, Prapavessis H, Callender K. Decreasing landing forces: effect of instruction. Br J Sports Med. 2000;34:293–296. doi: 10.1136/bjsm.34.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kovács I, Tihanyi J, Devita P, Rácz L, Barrier J, Hortobágyi T. Foot placement modifies kinematics and kinetics during drop jumping. Med Sci Sports Exerc. 1999;31:708–716. doi: 10.1097/00005768-199905000-00014. [DOI] [PubMed] [Google Scholar]
- 31.Kent-Braun JA. Central and peripheral contributions to muscle fatigue in humans during sustained maximal effort. Eur J Appl Physiol Occup Physiol. 1999;80:57–63. doi: 10.1007/s004210050558. [DOI] [PubMed] [Google Scholar]
- 32.Nordlund MM, Thorstensson A, Cresswell AG. Central and peripheral contributions to fatigue in relation to level of activation during repeated maximal voluntary isometric plantar flexions. J Appl Physiol. 2004;96:218–225. doi: 10.1152/japplphysiol.00650.2003. [DOI] [PubMed] [Google Scholar]