Abstract
Infection of adherent cell monolayers using a liquid inoculum represents an established method to reliably and quantitatively study virus infection, but poorly recapitulates the exposure and infection of cells in the respiratory tract that occurs during infection with aerosolized pathogens. To better simulate natural infection in vitro, we adapted a system that generates viral aerosols similar to those exhaled by infected humans to the inoculation of epithelial cell monolayers. Procedures for cellular infection and calculation of exposure dose were developed and tested using viruses characterized by distinct transmission and pathogenicity phenotypes: an HPAI H5N1, an LPAI H7N9, and a seasonal H3N2 virus. While all three aerosolized viruses were highly infectious in a human bronchial epithelial cell line (Calu-3) cultured submerged in media, differences between the viruses were observed in primary human alveolar epithelial cells and in Calu-3 cells cultured at air-liquid interface. This system provides a novel enhancement to traditional in vitro experiments, particularly those focused on the early stages of infection.
Keywords: Influenza, Aerosols, Cell culture, Viral replication, Avian viruses
Highlights
-
•
Human respiratory epithelial cells were exposed to aerosolized influenza virus.
-
•
Fewer than ten PFU were required to infect the Calu-3 human cell line.
-
•
Infection route influenced susceptibility of primary alveolar cells to infection.
-
•
Aerosolized virus was able to penetrate an apical mucin layer.
1. Introduction
Infection of adherent cell monolayers using a liquid inoculum represents an established method to reliably and quantitatively study virus infection. Relatively straightforward and inexpensive, this method allows for the frequent collection of viral samples and the testing of a variety of experimental conditions and discrete cell types including those of human origin. Unfortunately, traditional in vitro replication studies poorly recapitulate the exposure and infection of cells in the respiratory tract that occurs during natural exposure to aerosolized pathogens. Not only does infection occur while cells’ apical surface is immersed in liquid, but at typical cell densities, the often-used “low” multiplicity of infection (MOI) of 0.01 corresponds to a dose of over a thousand PFU per square centimeter.
Available evidence suggests that in the case of aerosol transmission, natural human influenza infection is likely initiated by substantially fewer particles. Studies of infected patients found low viral concentrations in aerosols generated by breathing, coughing, and/or sneezing (Fabian et al., 2008, Milton et al., 2013, Yang et al., 2011), and fewer than five TCID50 are capable of initiating symptomatic infection in experimentally exposed volunteers (Alford et al., 1966). Similar results have been observed in the ferret model; these animals can be infected with fewer than ten PFU and subsequently exhale under five PFU per minute (Gustin et al., 2015, Gustin et al., 2011, Gustin et al., 2013, Roberts et al., 2011). Using a library of barcoded viruses, Varble et al. found that respiratory droplet transmission between ferrets involved only single-digit numbers of virions (Varble et al., 2014). Reports of A(H7N9) cases developing subsequent to patient visits to live bird markets despite lack of poultry contact, and the detection of virus in air sampled from such markets, indicate that zoonotic infection may also occur after human exposure to low quantities of aerosolized virus (Li et al., 2015, Liu et al., 2014, Zhou et al., 2016).
In order to better study the effects of potentially damaging aerosols on human cells, the toxicology field has begun to expose cultured respiratory epithelial cells to aerosolized, rather than liquid-suspended, chemical and particulate matter. Cells have been shown to be more sensitive to the effects of the former (Bitterle et al., 2006, Raemy et al., 2012). In these studies, aerosol concentration can be measured by the use of optical or gravimetric methods. These types of methods are not effective for the measure of virus-containing aerosols, however, because they detect liquid droplet nuclei rather than the virus within them, and cannot differentiate between infectious and non-infectious virions. Microbiologists have developed aerosolization systems to overcome these challenges, and have used them for experimental infections of animals and to study the effect of environmental conditions on viability of numerous pathogens including Mycobacterium tuberculosis, Bacillus anthracis, measles virus, and influenza virus (Clark et al., 2011, Gustin et al., 2011, Lemon et al., 2011, Savransky et al., 2013). This work has provided important insights into the intra- and inter-host spread of these pathogens by facilitating the observation and manipulation of near-natural infection within a controlled laboratory environment. However, despite the frequent employment of in vitro studies to complement animal experimentation, use of an aerosol system for in vitro infection with any pathogen has not, to our knowledge, been previously described.
We combined aspects of the toxicological and microbiological approaches to establish a novel method to expose adherent mammalian cell monolayers in air-liquid interface to defined quantities of aerosolized influenza virus and compared this with traditional liquid inoculation. In order to most effectively mimic the conditions of natural infection, we explored the use of very low MOI infection and culture techniques designed to promote cell differentiation in conjunction with virus aerosolization. Using highly pathogenic avian influenza (HPAI), low pathogenic avian influenza (LPAI), and seasonal influenza viruses, we demonstrate that infection of respiratory epithelial cells with physiologically low concentrations of aerosolized virus can be successfully recreated inside the laboratory. In conjunction with research using animal models, these techniques facilitate a closer study of the infectivity of aerosolized influenza virus in the context of human infection. The approach described here is not restricted to influenza virus and would also be applicable to the study of other respiratory viruses of public health concern.
2. Materials and methods
2.1. Viruses
Influenza A viruses were propagated in the allantoic cavity of 10-day-old embryonated hens’ eggs and titered via standard plaque assay using Madin-Darby canine kidney (MDCK) cells as previously described (Maines et al., 2005, Zeng et al., 2007). All experiments were conducted under biosafety level 3 containment, including enhancements as required by the U.S. Department of Agriculture and the Federal Select Agent Program (Chosewood et al., 2009).
2.2. Cell culture and liquid inoculations
The bronchial epithelial cell line Calu-3 (ATCC) was cultured as previously described (Zeng et al., 2007). Primary human alveolar epithelial cells (Cell Biologics) were cryopreserved at passage 3, then grown and expanded per manufacturer's instructions. All cells were seeded on 24 mm diameter (6-well format) or 12 mm diameter (12-well format) semipermeable membrane inserts with a 0.4 µm pore size (Corning) and grown to confluence under submerged conditions. After reaching a transepithelial resistance of >1000 Ω2 (Zeng et al., 2007), apical media was removed from selected Calu-3 cells to create an air-liquid interface (ALI), which was maintained for three weeks to facilitate cell differentiation and the establishment of a mucin layer.
Prior to inoculation, apical media (if present) was removed from the cell monolayer and cells cultured under submerged conditions were washed to remove serum present in culture medium. Liquid inoculation was performed using 300 μL of virus, diluted as specified in the results, and incubated on the cell surface for one hour before washing. After infection, cells were cultured in cell type-specific serum-free medium to which 1 μg/mL N-p-tosyl-ʟ-phenylalanine chloromethyl ketone (TPCK)-treated trypsin (Sigma-Aldrich) was added for alveolar cell cultures. Aliquots of apical culture supernatant or wash media (incubated atop cells cultured at ALI for 20 min) were collected at the indicated times post-infection (p.i.) and immediately frozen at −80 °C until titration. Growth curves were generated and analyzed using Prism 6.0.7 (GraphPad Software Inc).
2.3. Aerosol inoculations
The automated bioaerosol system used for all experiments has been previously described in detail (Gustin et al., 2011, Hartings and Roy, 2004) and all conditions were maintained here unless specified otherwise. Briefly, virus suspended in a solution of PBS-0.03% (w/v) BSA was aerosolized using a three-jet Collision nebulizer (BGI, Inc.) and passed through an exposure chamber at a rate of 20 L/min. Cells placed inside the exposure chamber on a wire mesh shelf were inoculated under air-liquid interface conditions ( Fig. 1). Using the AeroMP (Biaera Technologies) aerosol management platform, aerosol exposures were conducted at 21 °C and 50% relative humidity for 15 min followed by a 5 min purge to allow evacuation of the aerosolized virus from the chamber (Gustin et al., 2011). Prior to in vitro exposure, spray factor (SF) values were determined for stocks of all viruses to estimate the starting virus concentration in the nebulizer needed to obtain a desired concentration of virus in the aerosol. A Biosampler (SKC Inc) was used to quantify the virus actually aerosolized within the chamber during each exposure. Following aerosol exposure, membrane inserts were transferred to clean 6-well or 12-well plates and serum-free medium was added to apical and basolateral compartments as described above; cells maintained under ALI conditions had medium added to the basolateral compartment only. Confirmation of cell viability during aerosol exposure was performed using the WST-1 cell proliferation reagent (Roche Applied Science), according to manufacturer's instructions, with four independent samples tested for each condition.
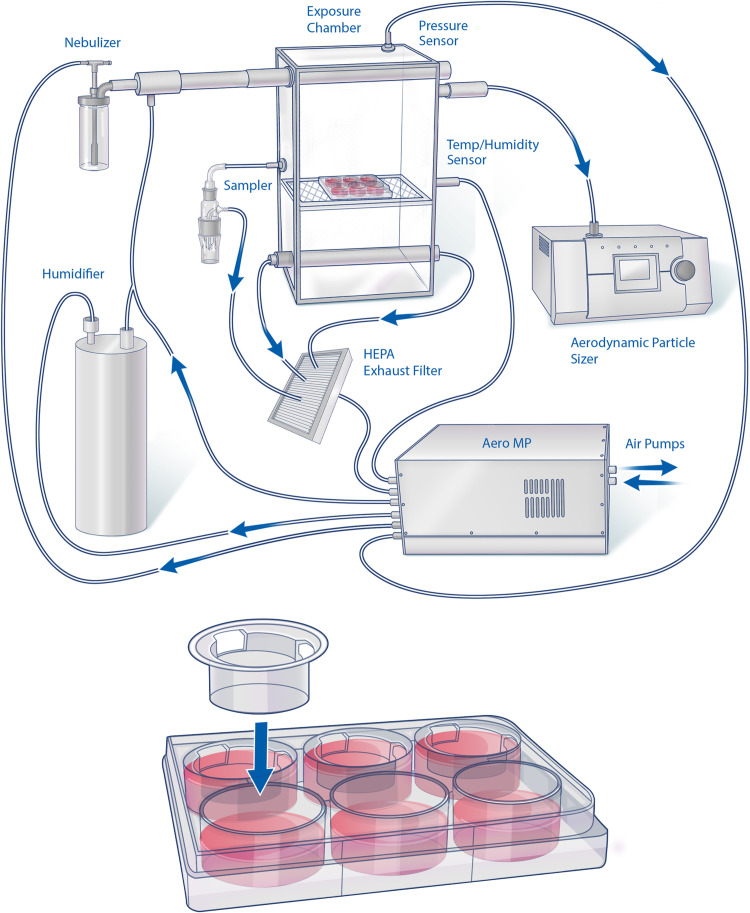
Fig. 1.
Graphic representation of aerosol system for in vitro use. Depiction of human cells cultured on transwell inserts and exposed to aerosolized influenza virus using a previously characterized system (Gustin et al., 2011). Cell culture dishes rest in the exposure chamber on a wire shelf under air-liquid interface conditions for the duration of the exposure. Inset, individual transwell inserts are transferred to sterile plates once removed from the exposure chamber.
2.4. Quantitation of Exposure and Infectious Doses
The total number of infectious virions passed through the chamber during the exposure session (N cham ) was calculated as
where C samp is the concentration of virus in the sampler, V samp is the volume of media in the sampler, and Q cham and Q samp represent the flow rates of chamber and sampler, respectively (see Supplemental methods for derivation). N cham was multiplied by the ratio of the surface area of each transwell (SA) to the cross-sectional area of the chamber (XA) to yield exposure dose (ED). ID50s were calculated according to the method of Reed and Muench, with the proportional distance multiplied by log 10 (dose above 50%)/log 10 (dose below 50%) to account for the deviation of exposure doses from exact 10-fold dilutions (Reed and Muench, 1938). Variability around the mean exposure dose was quantified using a binomial model with n viable virions passing through the chamber and a probability of success (virion lands on well) equal to SA/XA. Upper and lower critical values at the 95% confidence level were calculated using R 3.2.3 (R Foundation for Statistical Computing); the true exposure dose for any particular well has a 95% chance of falling between these two values. The cumulative probability distribution indicated that the minimum dose had to be three or greater for 95% of all wells to be inoculated with at least one virion. In order minimize the chance of including a well not exposed to any virus, we therefore aimed not to use mean exposure doses under 5 PFU. When this did occur due to variations in aerosolization efficiency, the minimum 50% infectious dose is reported as ≤3 PFU.
2.5. Real-time RT-PCR
Total RNA was extracted from mock-infected or virus-infected cell monolayers after removal of supernatant using the RNeasy mini kit (Qiagen). RT-PCR was performed with a QuantiTect SYBR green RT-PCR kit (Qiagen) in duplicate reactions from duplicate samples using an influenza A virus M1 gene primer set (Zeng et al., 2007). Influenza virus M gene RNA copy numbers were extrapolated using a standard curve based on samples of known M gene copy number.
3. Results
3.1. System establishment and exposure dose determination
Rather than use the type of exposure system described in studies of cellular responses to aerosolized particulate matter (eg. CULTEX Radial Flow System), we employed one intended for use in animal infection. Previously optimized for use with influenza virus (Gustin et al., 2011), this system and its components are designed to maintain the viability of biological aerosols. This system features a large exposure chamber, which allows for simultaneous exposure of several plates of cells, facilitating comparisons of different cell types or growth conditions between uniformly exposed wells (Fig. 1).
In vitro inoculations of cells grown on semi-permeable membrane inserts (transwells) were conducted as follows: apical media (if present) was removed immediately prior to exposure, then plates holding the inserts and basolateral media were placed in the chamber and exposed to ten-fold serial dilutions of aerosolized virus for a duration of 15 min. Following exposure, inserts were transferred to a sterile tissue culture plate containing fresh basolateral media and apical media was replaced. Mock infection led to no significant decrease in cell viability (data not shown), indicating that the presence of basolateral media was sufficient to keep the cells from drying out during exposure.
The ability to quantitate the dose to which an animal or cell monolayer is exposed is a critical component of experiments utilizing aerosol-based exposure systems (Hartings and Roy, 2004), and is necessary for comparison of aerosol infections with those conducted by the more traditional liquid route. We found that titration of virus collected in wells of media placed in the chamber alongside the cells was insufficiently sensitive to reliably quantify the low doses to which each monolayer was exposed (data not shown), possibly because deposition efficiency differed between the cell surface and the liquid media. We therefore modeled our approach on that used in aerosol inoculation of animals. Presented dose for an animal can be expressed as the total number of infectious virions passing through the chamber during an exposure session multiplied by the ratio of the volume of aerosol inhaled by the animal to the total volume of aerosol passed through the chamber (see Supplemental methods for derivation). For in vitro quantification, we substituted the ratio of the surface area of each transwell insert to the cross-sectional area of the chamber for the ratio of inhaled to total aerosol volume. Because the efficiency of particle deposition on the cell surface was estimated to be approximately 100%, presented dose and exposure dose were considered equivalent. No correlation between plate position within the chamber or well position within the plate and virological outcome was observed.
3.2. Validation of experimental approach
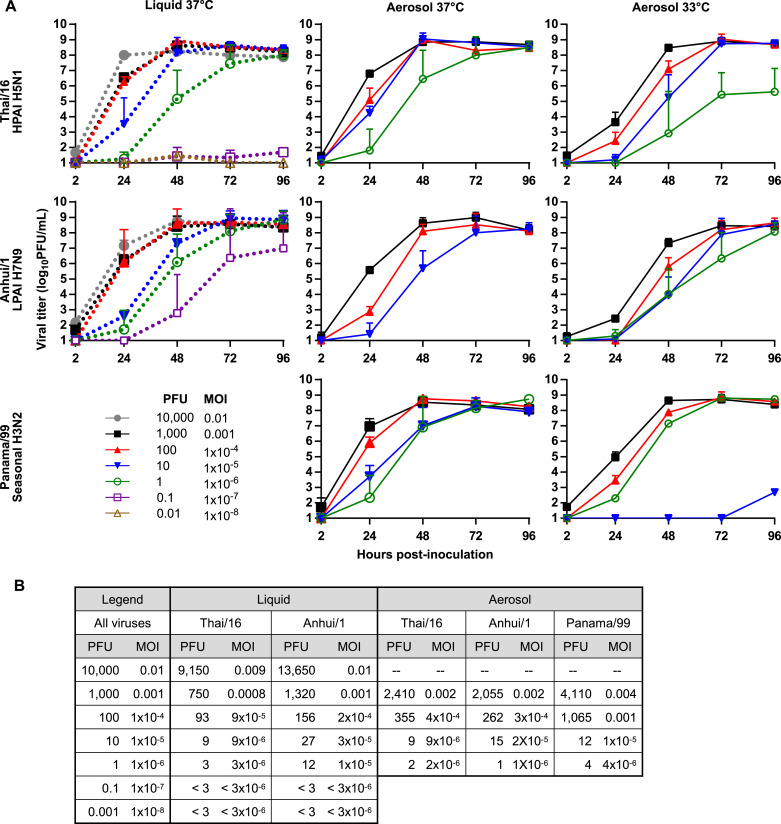
Initial characterization studies were conducted using the Calu-3 human bronchial epithelial cell line. This cell type is relevant to respiratory infection and has previously been shown to support replication of a variety of influenza A viruses, though published studies have typically used MOIs of 0.01 (equivalent to 10,000 TCID50 or PFU per 24 mm well) or higher (Zeng et al., 2007, Zhou et al., 2011). In order to generate comparison data for aerosol infections, we first conducted an analogous experiment using traditional liquid inoculation at a wide range of doses. Two influenza viruses known to replicate with high efficiency (A/Thailand/16/2004 [Thai/16, HPAI A(H5N1)] and A/Anhui/1/2013 [Anhui/1, LPAI A(H7N9)], both isolated from fatal human cases) were serially diluted and used to inoculate quintuplicate wells. Because of the potential for both random and systemic error in making repeated serial dilutions, we titrated all inocula, enabling us to more precisely estimate the number of infectious virions to which each well was exposed. RNA was collected from the cell monolayers of two wells 24 h post-inoculation and assayed for the presence of viral nucleic acid via RT-PCR with primers specific to the M1 gene. Growth kinetics in the remaining three wells were monitored by titration of cell supernatants collected between 2 and 96 h post-infection ( Fig. 2). At inoculum doses above our limit of detection (10 PFU/mL or 3 PFU/well), both viruses consistently infected all replicate wells and replicated to high titer, though growth was somewhat delayed at lower inoculation doses relative to higher ones ( Figs. 2, 3B). We also observed robust replication in cultures inoculated with approximately 1 PFU (dose estimated from serial dilution) of Anhui/1 virus. At doses of less than one PFU, infection was infrequent, characterized by low titers and undetectable levels of viral nucleic acid in the cell monolayer 24 h after inoculation.
Fig. 2.
Replication of influenza A viruses in Calu-3 cells. A) Calu-3 cells were infected by the traditional liquid route (dashed line) or the aerosol route (solid line) at the target MOI with the viruses shown, and cultured at 37 °C or 33 °C. Culture supernatants were collected at the indicated times p.i., and titers were determined by standard plaque assay to quantify infectious virus. The limit of detection was 10 PFU. Error bars indicate standard deviation. Lines represent positive wells (infectious virus detected at two sequential timepoints or at 96 h alone, 3/3 unless otherwise noted) only. Cultures with 2/3 positive wells: Thai/16 33 °C aerosol 1×10−6, liquid 1×10−7; Anhui/1 33 °C aerosol 1×10−6, liquid 1×10−7; Panama/99 37 °C aerosol 1×10−6. Cultures with 1/3 positive wells: Thai/16 37 °C liquid 1×10−8; Panama/99 33 °C aerosol 1×10−5 and 1×10−6. B) Exact inoculum dose (PFU) and MOI for each infection shown in panel..
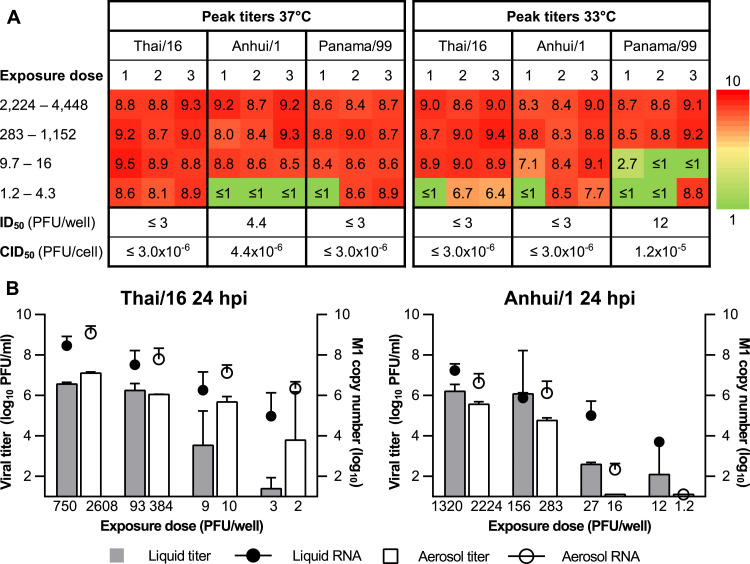
Fig. 3.
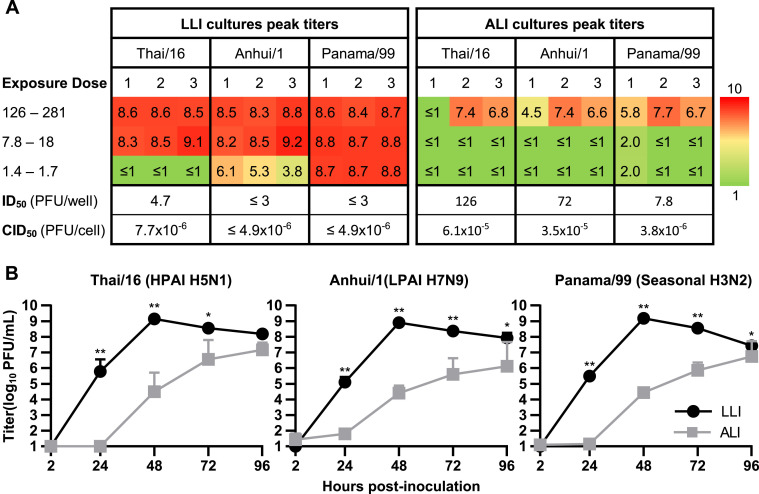
Infection and replication in Calu-3 cells after aerosol exposure. A) Peak viral titers detected in each well inoculated via the aerosol route. Titers (log10PFU/mL) are provided for each well that showed evidence of productive replication, defined as infectious virus detected at two sequential timepoints or at 96 h alone (full replication curves are shown in Fig. 2). Exposure dose (PFU) varied slightly between viruses and is therefore listed as a range. Exact exposure doses for each virus are listed in Table S1. Cells cultured at 33 and 37 °C were exposed concurrently. CID50 indicates the 50% cellular infectious dose, or MOI required to achieve 50% infectivity, calculated by dividing ID50 by the cell number. Limit of detection was 10 PFU. B) Comparison of viral supernatant titer (left Y axis) and M copy number (right Y axis) present in the cell monolayer between aerosol and liquid inoculation at 24 h p.i. Cells were cultured at 37 °C. Supernatants were collected immediately prior to lysis of the cell monolayer for RNA collection. Each parameter is expressed as mean ± standard deviation of two independent wells. Limit of detection for M segment RNA was 10 copies..
Aerosol experiments were conducted with three viruses chosen to represent a diversity of mammalian in vivo pathogenicity and transmissibility phenotypes: Thai/16, Anhui/1, and A/Panama/2007/99 (Panama/1999, seasonal A(H3N2)). All three viruses infected Calu-3 cells with high efficiency following aerosol exposure (Fig. 3). We observed rates of productive infection comparable to those seen after inoculation using a liquid suspension, with 50% infectious doses (ID50s) for all three viruses of under five PFU. High peak viral titers (108 PFU/mL) were detected in the supernatant regardless of exposure dose, though, as with liquid inoculum, replication was delayed at lower inoculation doses (Fig. 3). Parallel cultures were incubated post-exposure at 33 °C, a temperature thought to represent that of the mammalian upper respiratory tract, after infection to see whether infectivity was temperature-dependent. We found that while 24-h titers of the two avian viruses were slightly lower at this temperature than at 37 °C, infectivity of these cultures was reduced only for Panama/99 virus, and only slightly (ID50 of 12 vs ≤3 PFU).
The concordance in infectious dose between aerosol and liquid inoculations suggested that our calculated exposure dose for each well accurately represented the average number of virions to which a well was truly exposed. To confirm this, we conducted a series of exposures at doses near 1 PFU (range 0.02-7 PFU) per well. In light of our liquid exposure data with Thai/16 and Anhui/1, we reasoned that if the calculated exposure doses were accurate, the majority of Calu-3 wells should be infected with either of these viruses at doses ≥1 PFU, whereas few wells would be infected at doses <1 PFU. Consistent infection at calculated doses under 1 PFU would indicate that the true exposure dose was higher than the calculated one. Conversely, infrequent infection at doses ≥1 PFU would suggest that the actual exposure dose was less than the calculated one. In order to conduct a quantitative analysis, we determined the number of wells we would expect to become infected after each set of exposures using a Poisson binomial model (Hong, 2013). We statistically compared the expected number of infected wells (based on our calculated exposure dose) to the number of wells observed to be infected in our experiment (reflective of actual exposure dose) ( Table 1). Even though our tests were highly powered (≥99% chance of detecting a half-log difference between true and calculated exposure doses if a difference was present), we did not detect such a difference for either of the viruses tested (p>0.05). This suggested that our estimation of 100% deposition efficiency did not compromise our exposure dose estimates.
Table 1.
Concordance between observed and expected infection rates of wells exposed by the aerosol route to doses near 1 PFU.
| Exposure dosea | Virus | Observed # infectedb | Expected # infectedc | p-valued | Powere |
|---|---|---|---|---|---|
| >1 PFU | Thai/16 | 9/12 | ≥10.5/12 | 0.17 | 0.99 |
| Anhui/1 | 15/18 | ≥16.5/18 | 0.18 | 1 | |
| <1 PFU | Thai/16 | 8/24 | ≤8.0/24 | 0.58 | 1 |
| Anhui/1 | 0/18 | ≤6.1/18 | 1 | 1 |
Calculated exposure dose, as described in the text.
Number of experimentally infected wells, as determined by ≥10 PFU/mL of virus in the supernatant at both 72 and 96 h post-inoculation.
Number of wells expected to be infected based on calculated exposure dose. Determined using a Poisson binomial distribution where n = the number of exposed wells and p= the probability of an exposure dose of ≥1 PFU, where exposure dose follows a binomial distribution where n = total virions and p= well surface area/chamber cross-sectional area.
One-sided p-value reflecting the statistical significance of the difference between the number of wells expected and observed to be infected. Calculated using the Poisson binomial distribution described above.
Power to detect a half-log or greater difference between calculated and actual exposure dose.
3.3. Infection of primary human alveolar cells
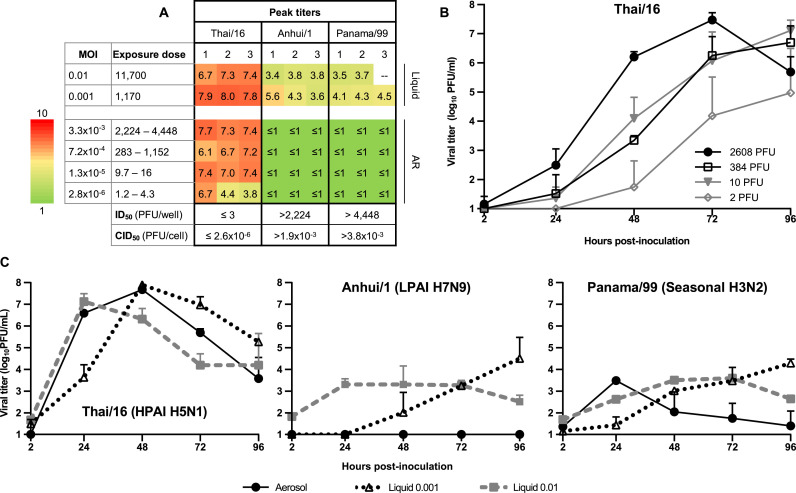
Having validated our methodology using a transformed cell line, we next investigated the ability of low-dose aerosols to infect primary human alveolar epithelial cells. Seasonal influenza A viruses are typically restricted to the upper respiratory tract during infection of humans and mammalian models, while avian viruses are often detected in the lungs. However, multiple in vitro studies have found primary human alveolar cells to be permissive for the replication of human influenza viruses (Weinheimer et al., 2012, Yu et al., 2011). We hypothesized that this discrepancy might be an artifact caused by the artificial nature of the liquid inoculum used in the in vitro studies. After confirming that liquid-based inoculation with Thai/16, Anhui/1, and Panama/99 viruses at an MOI of 0.01 led to productive replication in primary human alveolar cells ( Figs. 4A and C), we exposed the alveolar cells to multiple concentrations of the same three viruses, this time by the aerosol route. Thai/16 virus was highly infectious, replicating productively in wells exposed to an average of ≤3 PFU (MOI=2.6×10−6). In contrast, replication of Panama/99 or Anhui/1 viruses could not be detected at any of the doses tested following aerosol inoculation (Fig. 4A). Repetition of the highest-dose aerosol inoculation confirmed the absence of detectable replication of Anhui/1 virus (Fig. 4C). Low levels of Panama/99 virus were present in the cell supernatant of all three triplicate wells, but in all cases, titers peaked 24 h post-infection and declined thereafter, indicating unsustained or unproductive replication. To determine whether the lack of replication was a product of inoculation route or dose, we exposed cells to a liquid inoculum at an MOI (~0.001) equivalent to that of our most concentrated aerosol inoculation. Growth kinetics were similar to those observed after the 0.01 MOI infections, suggesting that the lack of replication in a permissive cell type could be attributed to the aerosol delivery of the virus and not to its low concentration.
Fig. 4.
Replication of influenza A viruses in primary human alveolar epithelial cells. A) Peak viral titers detected in each well inoculated via the aerosol route, as described in the legend for Fig. 3A. B) Replication curves for Thai/16 aerosol inoculations shown in panel A. Titers shown represent mean ± standard deviation of three wells. C) Comparison of replication kinetics subsequent to aerosol or liquid inoculation of human primary alveolar epithelial cells. Cells were infected by the aerosol route (solid black line), or by the traditional liquid route (dotted line) at an MOI of 0.01 (gray) or 0.001 (black). Aerosol MOIs were 0.002, 0.0006, and 0.002 for Thai/16, Anhui/1, and Panama/99 viruses, respectively. Culture supernatants were collected at the indicated times p.i., and titers were determined by standard plaque assay to quantify infectious virus. The limit of detection was 10 PFU. Mean ± SD from triplicate cultures (duplicate for Panama/99 liquid inoculum, 0.01 MOI) is shown..
3.4. Infection of cells cultured under air-liquid interface
In order to reach susceptible cells, inhaled pathogens must penetrate the mucus layer coating the airway epithelium. The mucus layer and epithelium can be simulated in vitro by culturing respiratory cell lines or primary cells at air-liquid interface (ALI: media is present only on the basolateral side of the monolayer, with the apical side left exposed to air). Culture at ALI causes cells to differentiate and form a pseudostratified, columnar epithelium, comprising multiple cell types, including mucus-secreting goblet cells (Kreft et al., 2015). However, it has not previously been possible to recreate the interaction of aerosolized pathogens with respiratory mucus in an in vitro setting. We therefore compared the susceptibility of Calu-3 cells grown at ALI and liquid-liquid interface (LLI: media present on apical and basolateral sides) to infection with aerosolized virus. Infectivity of Calu-3 cells cultured at ALI for three weeks (sufficient to induce substantial mucus production (Haghi et al., 2010; Kreft et al., 2015)) varied by virus ( Fig. 5): Panama/99 infectivity was only slightly abrogated (ID50 increased from ≤3 to 7) whereas Thai/16 and Anhui/1 were over 25 times less infectious in the ALI-cultured cells than those cultured at LLI. When cells were successfully infected with any of the viruses, replication was delayed and reached lower titers in ALI cultures as compared to LLI (Fig. 5). Together, these data demonstrate that the capacity for aerosolized inocula to infect cultures of differentiated human airway cells is abrogated but not eliminated by the presence of a mucin layer.
Fig. 5.
Comparison of viral infectivity and replication between cells cultured at liquid-liquid (LLI) or air-liquid (ALI) interface. A) Peak viral titers detected in each well inoculated via the aerosol route, as described in the legend for Fig 3A. Exact exposure doses are listed in Table S2. Cells cultured at LLI and ALI were exposed concurrently and therefore have identical exposure doses. B) Replication curves from wells exposed to 116–260 PFU shown in panel A. Culture supernatants were collected at the indicated times p.i., and titers were determined by standard plaque assay to quantify infectious virus. The limit of detection was 10 PFU. Titers shown represent mean ± standard deviation of three wells (two in the case of Thai/16). Two-way ANOVA showed that overall titer differences between cells cultured at LLI and ALI were statistically significant (p<0.05). For each virus, titers from LLI and ALI wells were compared at each individual timepoint (p-values were adjusted for multiple comparisons using the Bonferroni correction): * indicates p<0.05, ** indicates p<0.001.
4. Discussion
While a growing body of work describes the characteristics of aerosolized microbes, the interaction of pathogen-laden aerosols with the airway epithelium has not been specifically examined. We demonstrate here that infection of adherent cell monolayers by aerosol is feasible, and we describe and validate a straightforward method for the calculation of exposure dose, which facilitates comparison between infections using liquid and aerosol inocula. While in vitro replication studies typically measure viral titers over time after infection with a single MOI, we found that measuring viral infectivity at a variety of MOIs was more informative.
Measurements of infectivity may also be more relevant to virus transmission. Interestingly, we found that culture of Calu-3 cells at 33 °C post-aerosol-inoculation did not significantly reduce the ability of any of the viruses tested to establish infection. While we did not perform a liquid comparison, we would expect comparable results given the consistency of replication of the tested viruses in this cell type. It is important to note, however, that all three viruses have a lysine at position 627 of the PB2 gene rather than a glutamate, which is known to restrict replication at this temperature (Neumann and Kawaoka, 2015). More significant effects on infectivity might be observed with viruses that have a glutamate at this position or in other cell types.
Studies utilizing very low MOI may play an important role in advancing our understanding of influenza virus transmission by simulating in vitro the conditions under which infection is first established in a new human host. At decreased MOI, for example, the rate at which semi-infectious particles are able to replicate synergistically through cellular co-infection is reduced (Fonville et al., 2015), but the diminished proliferation of defective interfering particles may lessen innate immune activation, thereby allowing for increased viral replication. Indeed, previously published work with influenza and other viruses describes differences in viral replication at high and low MOI (Aggarwal et al., 2011, Huh et al., 2008, Miller et al., 1994). We have demonstrated here the feasibility of studies using very low MOI; though we observed only subtle changes in replication kinetics as MOI decreased, similar across all viruses tested, more pronounced effects may be observed with other viruses, cell types, and/or culture conditions (e.g. temperature).
Droplet nuclei (<5 µm) containing virus, unlike larger (>5 µm) droplets or virus present on surfaces, reaches the lower respiratory tract when inhaled (BeruBe et al., 2009). We were therefore particularly interested in the ability of aerosolized virus to infect primary human alveolar cells. We found that both the seasonal virus Panama/99 and an outbreak-associated H7N9 virus, Anhui/1, replicated productively in primary human pneumocytes after inoculation via the liquid, but not aerosol, route whereas the H5N1 virus Thai/16 was highly infectious and replicated to high titer regardless of inoculation method. For Panama/99 virus, these in vitro results are consistent with both ferret studies, which do not detect virus replication in the lungs, and with human seasonal virus infections, which are typically limited to the upper respiratory tract. In contrast, severe human A(H7N9) cases have been characterized by symptoms of lung infection (Chen et al., 2013, Gao et al., 2013, Hu et al., 2013, Yang et al., 2014, Yu et al., 2013b), and virus has been detected in the lungs of experimentally infected animals (Belser et al., 2013, de Wit et al., 2014, Gabbard et al., 2014, Watanabe et al., 2013, Xu et al., 2014, Zhang et al., 2013, Zhu et al., 2013). Our findings raise the possibility that the development of viral pneumonia associated with H7N9 virus develops not upon initial exposure, but subsequent to viral spread from adjacent tissues, and warrant further investigation regarding the dynamics of H7N9 virus infection throughout the respiratory tract. The need for such spread may provide a window of opportunity for the immune system to restrict the virus before it causes severe disease, which would explain the apparent prevalence of clinically inapparent and mild infection with this virus (Chen et al., 2014, Ip et al., 2013, Yu et al., 2013a).
Using the Calu-3 cell line, we demonstrated that growth under ALI conditions reduced the efficiency of both initial infection and subsequent viral replication. The high viscosity of mucus and abundance of virus-binding sialic acids may limit the diffusion of virus between cells, thereby reducing viral titers. Notably, abrogation in infectivity resulting from culture at ALI was more pronounced with the two avian viruses tested than the seasonal virus Panama/99. This finding is consistent with the hypothesis that respiratory mucus serves as an important barrier to the ability of avian influenza viruses to transmit between humans, possibly because their specificity for α2,3-linked sialic acids makes them more susceptible to binding and entrapment by mucus, which some studies have suggested contains glycans primarily in the α2,3 conformation (Baum and Paulson, 1990, Couceiro et al., 1993). Use of reverse genetics techniques to compare viruses differing only in the sialic acid binding preferences of the hemagglutinin and/or neuraminidase proteins will allow for further investigation of this phenomenon.
Aerosol inoculation, particularly when used in conjunction with increasingly sophisticated techniques for in vitro cell culture, offers a unique opportunity to study virus-cell interactions in an environment resembling that of the human respiratory tract. Our studies suggest that aerosol inoculation may enhance studies of viral tropism and improve our understanding of the effects of environmental conditions on the ability of influenza virus to initiate infection. Continued investigation regarding the role of inoculation route in viral binding and entry processes will further our understanding of the infectivity of influenza viruses with distinct phenotypes. In addition to influenza, the methods outlined here could be used for the study of other respiratory viruses such as severe acute respiratory syndrome (SARS) virus, varicella zoster virus (VZV), and measles virus, as well as the risk assessment of novel pathogens. The ability to combine aerosol inoculation with the benefits of in vitro study, notably the ability to study specific cell types in isolation, will facilitate a greater understanding of the infectivity and tropism of respiratory pathogens of public health concern.
Acknowledgements
We thank the China CDC for facilitating access to virus, Justin Hartings for technical assistance, and Alissa Eckert for graphical assistance. H.M.C. and J.A.P. were supported by the Oak Ridge Institute for Science and Education. The findings and conclusions in this report are those of the authors and do not necessarily reflect the views of the funding agency.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.virol.2016.10.007.
Appendix A. Supplementary material
Supplementary material
.
References
- Aggarwal K., Jing F., Maranga L., Liu J. Bioprocess optimization for cell culture based influenza vaccine production. Vaccine. 2011;29:3320–3328. doi: 10.1016/j.vaccine.2011.01.081. [DOI] [PubMed] [Google Scholar]
- Alford, R.H., Kasel, J.A., Gerone, P.J., Knight, V., 1966. Human influenza resulting from aerosol inhalation. Proceedings of the Society for Experimental Biology and Medicine. Society for Experimental Biology and Medicine, New York, N.Y. 122, pp. 800–804. [DOI] [PubMed]
- Baum L.G., Paulson J.C. Sialyloligosaccharides of the respiratory epithelium in the selection of human influenza virus receptor specificity. Acta Histochem. Suppl. 1990;40:35–38. [PubMed] [Google Scholar]
- Belser J.A., Gustin K.M., Pearce M.B., Maines T.R., Zeng H., Pappas C., Sun X., Carney P.J., Villanueva J.M., Stevens J., Katz J.M., Tumpey T.M. Pathogenesis and transmission of avian influenza A (H7N9) virus in ferrets and mice. Nature. 2013;501:556–559. doi: 10.1038/nature12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BeruBe, K., Aufderheide, M., Breheny, D., Clothier, R., Combes, R., Duffin, R., Forbes, B., Gaca, M., Gray, A., Hall, I., Kelly, M., Lethem, M., Liebsch, M., Merolla, L., Morin, J.P., Seagrave, J., Swartz, M.A., Tetley, T.D., Umachandran, M., 2009. In vitro models of inhalation toxicity and disease. The report of a FRAME workshop. Alternatives to laboratory animals : ATLA 37, 89–141. [PubMed]
- Bitterle E., Karg E., Schroeppel A., Kreyling W.G., Tippe A., Ferron G.A., Schmid O., Heyder J., Maier K.L., Hofer T. Dose-controlled exposure of A549 epithelial cells at the air-liquid interface to airborne ultrafine carbonaceous particles. Chemosphere. 2006;65:1784–1790. doi: 10.1016/j.chemosphere.2006.04.035. [DOI] [PubMed] [Google Scholar]
- Chen Y., Liang W., Yang S., Wu N., Gao H., Sheng J., Yao H., Wo J., Fang Q., Cui D., Li Y., Yao X., Zhang Y., Wu H., Zheng S., Diao H., Xia S., Zhang Y., Chan K.H., Tsoi H.W., Teng J.L., Song W., Wang P., Lau S.Y., Zheng M., Chan J.F., Chen K.K., Li H., Yuen, K.Y L. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet. 2013;381:1916–1925. doi: 10.1016/S0140-6736(13)60903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z., Liu H., Lu J., Luo L., Li K., Liu Y., Lau E.H., Di B., Wang H., Yang Z., Xiao X. Asymptomatic, mild, and severe influenza A(H7N9) virus infection in humans, Guangzhou, China. Emerg. Infect. Dis. 2014;20:1535–1540. doi: 10.3201/eid2009.140424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chosewood, L.C., Wilson, D.E., Centers for Disease, C., Prevention, National Institutes of, H., 2009. Biosafety in microbiological and biomedical laboratories. U.S. Dept. of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institutes of Health : [For sale by the Supt. of Docs., U.S. G.P.O.], Washington D.C.
- Clark S.O., Hall Y., Kelly D.L., Hatch G.J., Williams A. Survival of Mycobacterium tuberculosis during experimental aerosolization and implications for aerosol challenge models. J. Appl. Microbiol. 2011;111:350–359. doi: 10.1111/j.1365-2672.2011.05069.x. [DOI] [PubMed] [Google Scholar]
- Couceiro J.N., Paulson J.C., Baum L.G. Influenza virus strains selectively recognize sialyloligosaccharides on human respiratory epithelium; the role of the host cell in selection of hemagglutinin receptor specificity. Virus Res. 1993;29:155–165. doi: 10.1016/0168-1702(93)90056-s. [DOI] [PubMed] [Google Scholar]
- de Wit E., Rasmussen A.L., Feldmann F., Bushmaker T., Martellaro C., Haddock E., Okumura A., Proll S.C., Chang J., Gardner D., Katze M.G., Munster V.J., Feldmann H. Influenza virus A/Anhui/1/2013 (H7N9) replicates efficiently in the upper and lower respiratory tracts of cynomolgus macaques. mBio. 2014:5. doi: 10.1128/mBio.01331-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabian P., McDevitt J.J., DeHaan W.H., Fung R.O., Cowling B.J., Chan K.H., Leung G.M., Milton D.K. Influenza virus in human exhaled breath: an observational study. PloS One. 2008;3:e2691. doi: 10.1371/journal.pone.0002691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonville J.M., Marshall N., Tao H., Steel J., Lowen A.C. Influenza virus reassortment is enhanced by semi-infectious particles but can be suppressed by defective interfering particles. PLoS Pathog. 2015;11:e1005204. doi: 10.1371/journal.ppat.1005204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbard J.D., Dlugolenski D., Van Riel D., Marshall N., Galloway S.E., Howerth E.W., Campbell P.J., Jones C., Johnson S., Byrd-Leotis L., Steinhauer D.A., Kuiken T., Tompkins S.M., Tripp R., Lowen A.C., Steel J. Novel H7N9 influenza virus shows low infectious dose, high growth rate, and efficient contact transmission in the guinea pig model. J. Virol. 2014;88:1502–1512. doi: 10.1128/JVI.02959-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao H.N., Lu H.Z., Cao B., Du B., Shang H., Gan J.H., Lu S.H., Yang Y.D., Fang Q., Shen Y.Z., Xi X.M., Gu Q., Zhou X.M., Qu H.P., Yan Z., Li F.M., Zhao W., Gao Z.C., Wang G.F., Ruan L.X., Wang W.H., Ye J., Cao H.F., Li X.W., Zhang W.H., Fang X.C., He J., Liang W.F., Xie J., Zeng M., Wu X.Z., Li J., Xia Q., Jin Z.C., Chen Q., Tang C., Zhang Z.Y., Hou B.M., Feng Z.X., Sheng J.F., Zhong N.S., Li L.J. Clinical findings in 111 cases of influenza A (H7N9) virus infection. New Engl. J. Med. 2013;368:2277–2285. doi: 10.1056/NEJMoa1305584. [DOI] [PubMed] [Google Scholar]
- Gustin K.M., Belser J.A., Veguilla V., Zeng H., Katz J.M., Tumpey T.M., Maines T.R. Environmental conditions affect exhalation of H3N2 seasonal and variant influenza viruses and respiratory droplet transmission in ferrets. PloS One. 2015;10:e0125874. doi: 10.1371/journal.pone.0125874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustin K.M., Belser J.A., Wadford D.A., Pearce M.B., Katz J.M., Tumpey T.M., Maines T.R. Influenza virus aerosol exposure and analytical system for ferrets. Proc. Natl. Acad. Sci. USA. 2011;108:8432–8437. doi: 10.1073/pnas.1100768108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustin K.M., Katz J.M., Tumpey T.M., Maines T.R. Comparison of the levels of infectious virus in respirable aerosols exhaled by ferrets infected with influenza viruses exhibiting diverse transmissibility phenotypes. J. Virol. 2013;87:7864–7873. doi: 10.1128/JVI.00719-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haghi M., Young P.M., Traini D., Jaiswal R., Gong J., Bebawy M. Time- and passage-dependent characteristics of a Calu-3 respiratory epithelial cell model. Drug Dev. Ind. Pharm. 2010;36:1207–1214. doi: 10.3109/03639041003695113. [DOI] [PubMed] [Google Scholar]
- Hartings J.M., Roy C.J. The automated bioaerosol exposure system: preclinical platform development and a respiratory dosimetry application with nonhuman primates. J. Pharmacol. Toxicol. Methods. 2004;49:39–55. doi: 10.1016/j.vascn.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Hong Y. On computing the distribution function for the Poisson binomial distribution. Comput. Stat. Data Anal. 2013;59:41–51. [Google Scholar]
- Hu Y., Lu S., Song Z., Wang W., Hao P., Li J., Zhang X., Yen H.L., Shi B., Li T., Guan W., Xu L., Liu Y., Wang S., Zhang X., Tian D., Zhu Z., He J., Huang K., Chen H., Zheng L., Li X., Ping J., Kang B., Xi X., Zha L., Li Y., Zhang Z., Peiris M., Yuan Z. Association between adverse clinical outcome in human disease caused by novel influenza A H7N9 virus and sustained viral shedding and emergence of antiviral resistance. Lancet. 2013;381:2273–2279. doi: 10.1016/S0140-6736(13)61125-3. [DOI] [PubMed] [Google Scholar]
- Huh Y.H., Kim Y.E., Kim E.T., Park J.J., Song M.J., Zhu H., Hayward G.S., Ahn J.H. Binding STAT2 by the acidic domain of human cytomegalovirus IE1 promotes viral growth and is negatively regulated by SUMO. J. Virol. 2008;82:10444–10454. doi: 10.1128/JVI.00833-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ip D.K., Liao Q., Wu P., Gao Z., Cao B., Feng L., Xu X., Jiang H., Li M., Bao J., Zheng J., Zhang Q., Chang Z., Li Y., Yu J., Liu F., Ni M.Y., Wu J.T., Cowling B.J., Yang W., Leung G.M., Yu H. Detection of mild to moderate influenza A/H7N9 infection by China’s national sentinel surveillance system for influenza-like illness: case series. BMJ (Clinical research ed.) 2013;346:f3693. doi: 10.1136/bmj.f3693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreft M.E., Jerman U.D., Lasic E., Hevir-Kene N., Rizner T.L., Peternel L., Kristan K. The characterization of the human cell line Calu-3 under different culture conditions and its use as an optimized in vitro model to investigate bronchial epithelial function. Eur. J. Pharm. Sci.: Off. J. Eur. Fed. Pharm. Sci. 2015;69:1–9. doi: 10.1016/j.ejps.2014.12.017. [DOI] [PubMed] [Google Scholar]
- Lemon K., de Vries R.D., Mesman A.W., McQuaid S., van Amerongen G., Yuksel S., Ludlow M., Rennick L.J., Kuiken T., Rima B.K., Geijtenbeek T.B., Osterhaus A.D., Duprex W.P., de Swart R.L. Early target cells of measles virus after aerosol infection of non-human primates. PLoS Pathog. 2011;7:e1001263. doi: 10.1371/journal.ppat.1001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Chen J., Yang G., Zheng Y.X., Mao S.H., Zhu W.P., Yu X.L., Gao Y., Pan Q.C., Yuan Z.A. Case-control study of risk factors for human infection with avian influenza A(H7N9) virus in Shanghai, China, 2013. Epidemiol. Infect. 2015;143:1826–1832. doi: 10.1017/S0950268814003264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu B., Havers F., Chen E., Yuan Z., Yuan H., Ou J., Shang M., Kang K., Liao K., Liu F., Li D., Ding H., Zhou L., Zhu W., Ding F., Zhang P., Wang X., Yao J., Xiang N., Zhou S., Liu X., Song Y., Su H., Wang R., Cai J., Cao Y., Wang X., Bai T., Wang J., Feng Z., Zhang Y., Widdowson M.A., Li Q. Risk factors for influenza A(H7N9) disease--China, 2013. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 2014;59:787–794. doi: 10.1093/cid/ciu423. [DOI] [PubMed] [Google Scholar]
- Maines T.R., Lu X.H., Erb S.M., Edwards L., Guarner J., Greer P.W., Nguyen D.C., Szretter K.J., Chen L.M., Thawatsupha P., Chittaganpitch M., Waicharoen S., Nguyen D.T., Nguyen T., Nguyen H.H., Kim J.H., Hoang L.T., Kang C., Phuong L.S., Lim W., Zaki S., Donis R.O., Cox N.J., Katz J.M., Tumpey T.M. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J. Virol. 2005;79:11788–11800. doi: 10.1128/JVI.79.18.11788-11800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M.D., Warmerdam M.T., Gaston I., Greene W.C., Feinberg M.B. The human immunodeficiency virus-1 nef gene product: a positive factor for viral infection and replication in primary lymphocytes and macrophages. J. Exp. Med. 1994;179:101–113. doi: 10.1084/jem.179.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milton D.K., Fabian M.P., Cowling B.J., Grantham M.L., McDevitt J.J. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9:e1003205. doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann G., Kawaoka Y. Transmission of influenza A viruses. Virology. 2015;479–480:234–246. doi: 10.1016/j.virol.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raemy D.O., Grass R.N., Stark W.J., Schumacher C.M., Clift M.J., Gehr P., Rothen-Rutishauser B. Effects of flame made zinc oxide particles in human lung cells - a comparison of aerosol and suspension exposures. Part. Fibre Toxicol. 2012;9:33. doi: 10.1186/1743-8977-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed L.J., Muench H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938;27:493–497. [Google Scholar]
- Roberts K.L., Shelton H., Scull M., Pickles R., Barclay W.S. Lack of transmission of a human influenza virus with avian receptor specificity between ferrets is not due to decreased virus shedding but rather a lower infectivity in vivo. J. Gen. Virol. 2011;92:1822–1831. doi: 10.1099/vir.0.031203-0. [DOI] [PubMed] [Google Scholar]
- Savransky V., Sanford D.C., Syar E., Austin J.L., Tordoff K.P., Anderson M.S., Stark G.V., Barnewall R.E., Briscoe C.M., Lemiale-Bierinx L., Park S., Ionin B., Skiadopoulos M.H. Pathology and pathophysiology of inhalational anthrax in a guinea pig model. Infect. Immun. 2013;81:1152–1163. doi: 10.1128/IAI.01289-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varble A., Albrecht R.A., Backes S., Crumiller M., Bouvier N.M., Sachs D., Garcia-Sastre A., tenOever B.R. Influenza A virus transmission bottlenecks are defined by infection route and recipient host. Cell Host Microbe. 2014;16:691–700. doi: 10.1016/j.chom.2014.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe T., Kiso M., Fukuyama S., Nakajima N., Imai M., Yamada S., Murakami S., Yamayoshi S., Iwatsuki-Horimoto K., Sakoda Y., Takashita E., McBride R., Noda T., Hatta M., Imai H., Zhao D., Kishida N., Shirakura M., de Vries R.P., Shichinohe S., Okamatsu M., Tamura T., Tomita Y., Fujimoto N., Goto K., Katsura H., Kawakami E., Ishikawa I., Watanabe S., Ito M., Sakai-Tagawa Y., Sugita Y., Uraki R., Yamaji R., Eisfeld A.J., Zhong G., Fan S., Ping J., Maher E.A., Hanson A., Uchida Y., Saito T., Ozawa M., Neumann G., Kida H., Odagiri T., Paulson J.C., Hasegawa H., Tashiro M., Kawaoka Y. Characterization of H7N9 influenza A viruses isolated from humans. Nature. 2013;501:551–555. doi: 10.1038/nature12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinheimer V.K., Becher A., Tonnies M., Holland G., Knepper J., Bauer T.T., Schneider P., Neudecker J., Ruckert J.C., Szymanski K., Temmesfeld-Wollbrueck B., Gruber A.D., Bannert N., Suttorp N., Hippenstiel S., Wolff T., Hocke A.C. Influenza A viruses target type II pneumocytes in the human lung. J. Infect. Dis. 2012;206:1685–1694. doi: 10.1093/infdis/jis455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L., Bao L., Deng W., Dong L., Zhu H., Chen T., Lv Q., Li F., Yuan J., Xiang Z., Gao K., Xu Y., Huang L., Li Y., Liu J., Yao Y., Yu P., Li X., Huang W., Zhao X., Lan Y., Guo J., Yong W., Wei Q., Chen H., Zhang L., Qin C. Novel avian-origin human influenza A(H7N9) can be transmitted between ferrets via respiratory droplets. J. Infect. Dis. 2014;209:551–556. doi: 10.1093/infdis/jit474. [DOI] [PubMed] [Google Scholar]
- Yang S., Chen Y., Cui D., Yao H., Lou J., Huo Z., Xie G., Yu F., Zheng S., Yang Y., Zhu Y., Lu X., Liu X., Lau S.Y., Chan J.F., Yuen K.K., Chen K.Y., Li, L H. Avian-origin influenza A(H7N9) infection in influenza A(H7N9)-affected areas of China: a serological study. J. Infect. Dis. 2014;209:265–269. doi: 10.1093/infdis/jit430. [DOI] [PubMed] [Google Scholar]
- Yang W., Elankumaran S., Marr L.C. Concentrations and size distributions of airborne influenza A viruses measured indoors at a health centre, a day-care centre and on aeroplanes. J. R. Soc., Interface / R. Soc. 2011;8:1176–1184. doi: 10.1098/rsif.2010.0686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H., Cowling B.J., Feng L., Lau E.H., Liao Q., Tsang T.K., Peng Z., Wu P., Liu F., Fang V.J., Zhang H., Li M., Zeng L., Xu Z., Li Z., Luo H., Li Q., Feng Z., Cao B., Yang W., Wu J.T., Wang Y., Leung G.M. Human infection with avian influenza A H7N9 virus: an assessment of clinical severity. Lancet. 2013;382:138–145. doi: 10.1016/S0140-6736(13)61207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L., Wang Z., Chen Y., Ding W., Jia H., Chan J.F., Chen K.K., Yang H., Liang Y., Zheng W., Yao S., Yang H., Cao S., Dai H., Zhao X., Li H., Bao J., Chen Q., Hou, X P., Li L., Yuen K.Y. Clinical, virological, and histopathological manifestations of fatal human infections by avian influenza A(H7N9) virus. Clin. Infect. Dis.: Off. Publ. Infect. Dis. Soc. Am. 2013;57:1449–1457. doi: 10.1093/cid/cit541. [DOI] [PubMed] [Google Scholar]
- Yu W.C., Chan R.W., Wang J., Travanty E.A., Nicholls J.M., Peiris J.S., Mason R.J., Chan M.C. Viral replication and innate host responses in primary human alveolar epithelial cells and alveolar macrophages infected with influenza H5N1 and H1N1 viruses. J. Virol. 2011;85:6844–6855. doi: 10.1128/JVI.02200-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng H., Goldsmith C., Thawatsupha P., Chittaganpitch M., Waicharoen S., Zaki S., Tumpey T.M., Katz J.M. Highly pathogenic avian influenza H5N1 viruses elicit an attenuated type i interferon response in polarized human bronchial epithelial cells. J. Virol. 2007;81:12439–12449. doi: 10.1128/JVI.01134-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Q., Shi J., Deng G., Guo J., Zeng X., He X., Kong H., Gu C., Li X., Liu J., Wang G., Chen Y., Liu L., Liang L., Li Y., Fan J., Wang J., Li W., Guan L., Li Q., Yang H., Chen P., Jiang L., Guan Y., Xin X., Jiang Y., Tian G., Wang X., Qiao C., Li C., Bu Z., Chen H. H7N9 influenza viruses are transmissible in ferrets by respiratory droplet. Science. 2013;341:410–414. doi: 10.1126/science.1240532. [DOI] [PubMed] [Google Scholar]
- Zhou B., Li Y., Halpin R., Hine E., Spiro D.J., Wentworth D.E. PB2 residue 158 is a pathogenic determinant of pandemic H1N1 and H5 influenza a viruses in mice. J. Virol. 2011;85:357–365. doi: 10.1128/JVI.01694-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J., Wu J., Zeng X., Huang G., Zou L., Song Y., Gopinath D., Zhang X., Kang M., Lin J., Cowling B.J., Lindsley W.G., Ke C., Peiris J.S., Yen H.L. Isolation of H5N6, H7N9 and H9N2 avian influenza A viruses from air sampled at live poultry markets in China, 2014 and 2015. Eur. Surveill. 2016;21 doi: 10.2807/1560-7917.ES.2016.21.35.30331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H., Wang D., Kelvin D.J., Li L., Zheng Z., Yoon S.W., Wong S.S., Farooqui A., Wang J., Banner D., Chen R., Zheng R., Zhou J., Zhang Y., Hong W., Dong W., Cai Q., Roehrl M.H., Huang S.S., Kelvin A.A., Yao T., Zhou B., Chen X., Leung G.M., Poon L.L., Webster R.G., Webby R.J., Peiris J.S., Guan Y., Shu Y. Infectivity, transmission, and pathology of human-isolated H7N9 influenza virus in ferrets and pigs. Science. 2013;341:183–186. doi: 10.1126/science.1239844. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material