Abstract
Aims: In a new-generation computed tomography (CT) scanner, coronary artery calcium (CAC) scores were measured using 3.0-mm slice reconstruction images originally acquired with 0.5 mm thickness scans in a single beat. This study investigated the usefulness of thin-slice (0.5 mm) reconstruction for identifying small calcifications in coronary arteries and evaluated the association with coronary plaques and stenosis compared to conventional 3.0-mm reconstruction images.
Methods: We evaluated 132 patients with zero CAC scores in conventional 3.0-mm Agatston method using a 320-slice CT. Then, 0.5-mm slice reconstruction was performed to identify small calcifications. The presence of stenosis and coronary plaques was assessed using coronary CT angiography.
Results: In total, 22 small calcifications were identified in 18 patients. There were 28 (21%) patients with any (≥ 25%) stenosis (34 lesions). Forty-seven coronary plaques were found in 33 patients (25%), including 7 calcified plaques in 7 patients (5%), 34 noncalcified plaques in 27 patients (20%), and 6 partially calcified plaques in 5 patients (4%). Patients with small calcifications had a significantly higher prevalence of noncalcified or partially calcified plaques (83% vs 14%; p < 0.001) and obstructive stenosis (33% vs 5.2%; p < 0.001) compared to those without small calcifications. The addition of small calcifications to the coronary risk factors when diagnosing stenosis significantly improved the diagnostic value.
Conclusion: Small calcifications detected by thin-slice 0.5-mm reconstruction are useful for distinguishing coronary atherosclerotic lesions in patients with zero CAC scores from conventional CT reconstruction.
Keywords: Coronary CT angiography, Small calcification, Coronary artery calcium, Coronary plaque
See editorial vol. 23: 1309–1310
Introduction
The coronary artery calcium (CAC) score as detected using computed tomography (CT) correlates with the presence of coronary artery disease (CAD)1–3), mortality, and coronary morbidity3–6) and has recently been reported to be related to left ventricular diastolic function7). The absence of CAC is associated with a very low risk of coronary mortality and morbidity, particularly in asymptomatic individuals. The CAC score has prognostic value in symptomatic patients, with significantly more events occurring in patients with higher CAC scores8, 9). However, several multicenter studies have demonstrated that zero CAC scores did not completely eliminate the possibility of CAD in some patients10–12).
Conventional scans for CAC measurement are usually performed with 2.5 to 3.0-mm slices1, 2). However, in the new-generation, 320-slice CT, 3.0-mm slice images are reconstructed from 0.5-mm slice, whole-heart data, and then 0.5-mm slice reconstruction images are available without additional radiation exposure13). The study found that small amounts of coronary calcium could be distinguished more sensitively with thin 0.5-mm slice reconstruction than with standard 3.0-mm reconstruction, resulting in a positive calcium score in 21% of patients who had zero calcium scores in standard reconstruction14). However, it is unclear whether these small calcifications have a clinical significance in identifying obstructive or nonobstructive lesions with the potential to rupture or erose.
Aim
We sought to investigate the usefulness of thin-slice, 0.5-mm reconstructions to identify small calcifications in the coronary artery wall, and to evaluate their importance in addition to conventional risk factors in CAD diagnosis among patients with zero CAC scores from conventional 3.0-mm slice reconstructions.
Methods
Study Population
From April 2012 to June 2013, we identified 153 consecutive participants with a CAC score of zero who underwent coronary CT angiography (CCTA). Exclusion criteria included poor CCTA images because of motion artifacts, poor coronary contrast concentration, and missing information, such as traditional coronary risk factors or laboratory data (n = 10). In total, 132 patients were included in the study. Indications for CCTA based on chest symptoms (chest pain, palpitation, or dyspnea) were as follows: typical type chest pain (n = 9), atypical or non-anginal type (n = 102), no symptom with ischemic findings (n = 11), and no symptom with high-risks (n = 10; 2 vascular diseases, 1 prior cerebral infarction, 2 familial hypercholesterolemia, 2 treated diabetes mellitus, and 3 multiple coronary risk factors). Furthermore, 43 patients underwent CCTA before catheter ablation for atrial fibrillation.
Risk Factor Assessment and Laboratory Examinations
Hypertensive patients were defined as those with a systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or who were receiving antihypertensive therapy. Dyslipidemia was defined as having a serum low-density lipoprotein cholesterol level ≥140 mg/dl on direct measurement, a serum triglyceride level ≥150 mg/dl, or currently receiving lipid-lowering medication. Diabetes mellitus was defined as a hemoglobin A1c level ≥6.5% and/or current use of hypoglycemic agents. Current smokers were defined as subjects who smoked regularly or had quit in the 30 days prior to CCTA15). For each participant, the Framingham risk score was calculated and a 10 year risk was estimated16). Estimated glomerular filtration rate (eGFR) was calculated based on the four-variable Modification of Diet in Renal Disease study equation17). The serum C-reacting protein level was measured.
Coronary CT Scan Protocol
Coronary CT examinations were performed using a 320-slice CT scanner (Aquilion ONE; Toshiba Medical Systems, Tokyo, Japan). If the patient's resting heart rate was >65 beats per minute, a β-blocker (metoprolol 20–40 mg) was administered orally 60 minutes before the CT scan to avoid motion artifacts. All patients received 0.3 mg nitroglycerin immediately before the CT scan.
Prior to the contrast-enhanced scan, a non-contrast CT scan was performed to detect coronary artery calcifications. The scanning parameters were as follows: tube potential 120 kV; gantry rotation time 0.35 s; z-coverage 120–160 mm; and tube current between 200 mA and 540 mA according to body weight. Full cardiac non-contrast coronary artery imaging was performed in a single gantry rotation during breath-hold and inspiration in a single cardiac phase (75% of the R-R interval).
The contrast-enhanced coronary CT scan was performed by prospective ECG-triggered CCTA, with the center of the imaging window corresponding to 75% of the R-R interval (n = 80), or retrospective ECG-gated CTA (n = 52) with dose modulation (the window of full tube current limited to 65%–85% of the R-R interval) in 1–3 beats (depending on heart rate) during an inspiratory breath-hold. A patient's body weight-adjusted volume of nonionic contrast material (iodine 245 mg/kg) was injected into the antecubital vein over a fixed duration of 10 seconds, followed by 20 mL of 0.9% saline solution chaser at the same flow rate15, 18).
CAC Score and Identification of Small Coronary Calcifications
Non-contrast CT images were reconstructed with either standard 3.0 or 0.5-mm axial slices from the same data. CAC scores were calculated by the conventional Agatston method with 3.0-mm slice reconstruction using Smartscore version 4.0 software (GE Healthcare, Little Chalfont, Buckinghamshire, UK). A small calcification was defined as a calcium deposit visually identified in a 0.5-mm slice in non-enhanced axial data by two independent, blinded observers. Both readers (Y.U. and H.T.) were cardiologists who had more than 5 years' experience of assessing coronary CT images, and both agreed on the identification for all small calcifications.
Evaluation of CCTA
CCTA images were assessed by the same two observers according to the Society of Cardiovascular Computed Tomography-recommended 18-segment mode19). All coronary segments >2 mm in diameter were evaluated with curved multiplanar reformation and cross-sectional images in a direction perpendicular to the vessel center line. Obstructive stenosis was defined as luminal stenosis ≥50% and any stenosis as vessels with ≥25% stenosis.
Based on our previous report15), the observers determined the presence of calcified plaque (CP), non-calcified plaque (NCP), and partially calcified plaque (PCP). CP was defined as any structure with a CT density ≥130 HU which could be visualized separately from the contrast-enhanced coronary lumen. NCP was defined as any distinguishable region with a low-density (< 130 HU) area >1 mm2 in size. PCP was defined as having both calcified and non-calcified components.
Statistical Analysis
Continuous variables are presented as mean ± standard deviation, and categorical variables are presented as numbers (proportion). Student's t-test or the Wilcoxon test were used to compare continuous variables. The chi-square test was used to compare categorical variables. The presence of small calcifications was assessed as a binary outcome. Receiver-operating characteristic (ROC) curves were constructed to compare the accuracy of predictions of the presence of NCP and/or PCP (NCP/PCP), any stenosis, and obstructive stenosis. Any incremental improvement in the accuracy of prediction was determined after adding the presence of small calcifications to coronary risk factors, including age, sex, hypertension, dyslipidemia, diabetes mellitus, and current smoking, and calculating the c-statistics with 95% confidence interval (CI). p values of < 0.05 were considered statistically significant. All statistical analyses were performed with JMP 10 statistical software (SAS Institute Inc., Cary, NC, USA).
Results
Patient Characteristics
The mean age of the 132 patients was 57.3 ± 11.7 years, and 61% were men. Table 1 compares the clinical characteristics of patients with and without small calcifications. The proportions of men (89% vs 57%; p = 0.0099), hypertension (83% vs 46%; p = 0.0029), and current smoking (33% vs 13%; p = 0.030) in patients with small calcifications were significantly higher than in patients without small calcifications. The mean Framingham risk score was significantly higher in the small calcifications group than in the group without small calcifications (9.1 ± 5.3 vs 6.0 ± 5.7; p = 0.0072).
Table 1. Clinical characteristics compared between presence and absence of small calcifications.
| Small calcification | Small calcification | ||
|---|---|---|---|
| present | absent | ||
| Characteristics | (n = 18) | (n = 114) | p value |
| Age (year) | 59.7 ± 13.5 | 56.9 ± 11.5 | 0.29 |
| Male n (%) | 16 (89%) | 65 (57%) | 0.0099 |
| Body mass index (kg/m2) | 23.2 ± 3.6 | 23.7 ± 4.7 | 0.62 |
| Hypertension n (%) | 15 (8%3) | 52 (46%) | 0.0029 |
| Dyslipidemia n (%) | 12 (67%) | 65 (57%) | 0.44 |
| Diabetes mellitus n (%) | 4 (22%) | 12 (11%) | 0.16 |
| Current smoker n (%) | 6 (33%) | 15 (13%) | 0.030 |
| Framingham-risk score (10 years risk %) | 9.1 ± 5.3 | 6.0 ± 5.7 | 0.0072 |
| Indication for CCTA | 0.12 | ||
| Evaluation for typical chest symptom n (%) | 2 (11%) | 7 (6%) | |
| Atypical or non-cardiac chest symptom n (%) | 10 (56%) | 92 (81%) | |
| No symptom with ischemic findings, | 3 (17%) | 8 (7%) | |
| No symptom, high-risk n (%) | 3 (17%) | 7 (6%) | |
| Catheter ablation for transient AF n (%) | 5 (28%) | 38 (33%) | 0.79 |
| Blood examination | |||
| HDL cholesterol (mg/dl) | 57.1 ± 16.1 | 66.4 ± 21.4 | 0.052 |
| LDL cholesterol (mg/dl) | 110.3 ± 30.7 | 123.6 ± 35.7 | 0.15 |
| Triglycerides (mg/dl) | 158.7 ± 120.5 | 132.5 ± 97.1 | 0.37 |
| Hemoglobin A1c (%) | 5.7 ± 1.0 | 5.4 ± 1.0 | 0.35 |
| eGFR (ml/min/1.73 km2) | 74.2 ± 17.3 | 74.2 ± 20.0 | 0.97 |
| C-reacting protein (mg/dl) | 0.11 ± 0.15 | 0.15 ± 0.21 | 0.55 |
| Medication | |||
| Aspirin use n (%) | 2 (11) | 5 (4) | 0.24 |
| Statin use n (%) | 4 (22) | 14 (12) | 0.25 |
| RAS inhibitor use n (%) | 8 (44) | 24 (21) | 0.031 |
| Hypoglycemic drugs n (%) | 3 (17) | 7 (6) | 0.12 |
Data expressed as number (percent) or mean ± standard deviation.
AF, atrial fibrillation; eGFR, estimated glomerular filtration rate; HDL, high-density lipoprotein; LDL, low-density lipoprotein; RAS, renin angiotensin system inhibitor.
Small Calcifications and CCTA Findings
Of a total of 2,052 segments from 132 patients, small calcifications were detected in 22 lesions from 18 patients (14%). Among all subjects, obstructive stenosis was found in 15 lesions from 12 patients (9%), and any stenosis in 34 lesions from 28 patients (21%). Any type of coronary plaque was visualized in 47 lesions of 33 patients (25%). CPs were observed in 7 lesions from 7 patients (5%); NCPs in 34 lesions from 27 patients (20%); and PCPs in 6 lesions from 5 patients (4%). A total of 40 NCP/PCPs were found in 30 patients (23%) (Table 2). Fig. 1 presents a representative case of a patient with small calcifications who had significant stenosis in the proximal left anterior descending artery.
Table 2. Small calcification and coronary computed tomography angiography finding.
| Number of patients | Number of segments | |
|---|---|---|
| Variables | (132 patients) | (2052 segments) |
| Small calcification | 18 (14%) | 22 (1.1%) |
| Any plaque | 33 (25%) | 47 (2.3%) |
| Calcified plaque | 7 (5%) | 7 (0.3%) |
| NCP | 27 (20%) | 34 (1.7%) |
| PCP | 5 (4%) | 6 (0.3%) |
| NCP and/or PCP | 30 (23%) | 40 (1.9%) |
| Any stenosis (≥25%) | 28 (21%) | 34 (1.7%) |
| Obstructive stenosis (≥50%) | 12 (9%) | 15 (0.7%) |
Data were expressed as number (percent). NCP, noncalcified plaque; PCP, partially calcified plaque
Fig. 1.
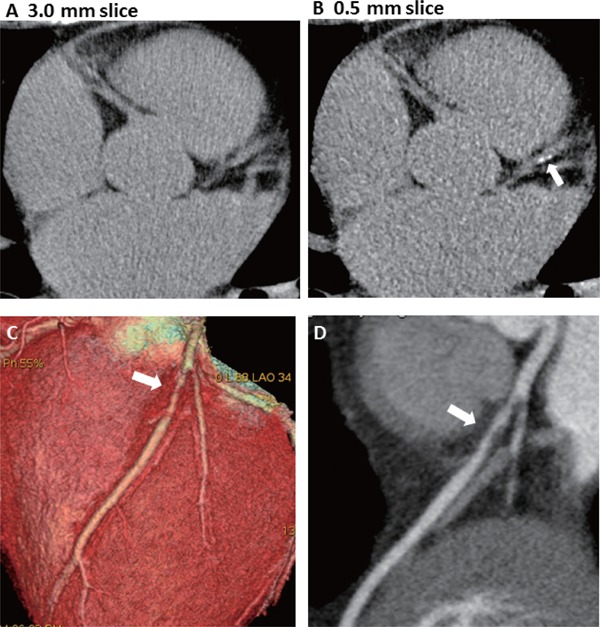
Representative case of a 58-year-old man who had a zero coronary artery calcium score but also had a small calcification; non-contrast scan of the proximal left anterior descending artery (LAD) with a conventional 3.0-mm slice (A) and a 0.5-mm slice (B). Volume rendering (C) and curved multiplanar construction (D) images in coronary computed tomography angiography showed obstructive stenosis in the proximal LAD (arrow).
CCTA findings were compared between groups with (n = 18) and without (n = 114) small calcifications (Fig. 2). All patients in the small calcification group had at least one plaque of any type, compared to 13% in the no small calcification group (p < 0.001). The prevalence of NCP/PCPs was significantly higher in the small calcification group than in the no small calcification group (83% vs 14%; p < 0.001). In addition, there was a significantly higher proportion of patients in the small calcification group than in the no small calcification group with any stenosis (83% vs 11%; p < 0.001) or obstructive stenosis (33% vs 5.2%; p < 0.001)
Fig. 2.
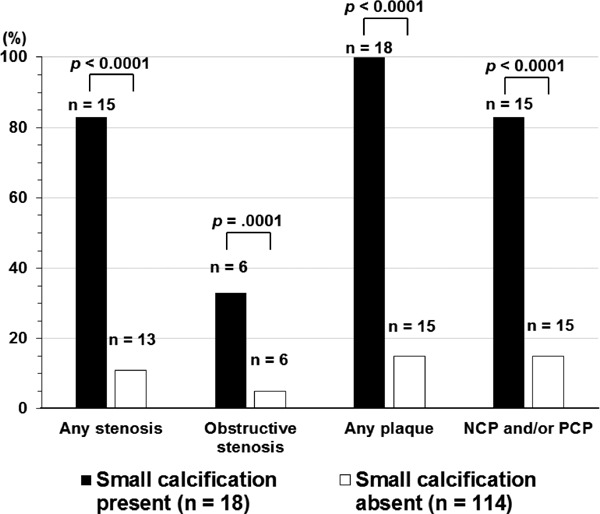
Prevalence of stenosis or plaques in coronary computed tomography angiography according to the presence (solid bar) or absence (open bar) of small calcifications.
Incremental Diagnostic Values of Small Calcifications with Coronary Risk Factors to Detect Plaques and Stenosis
ROC analyses demonstrated that the c-statistics for coronary risk factors, including age, sex, hypertension, dyslipidemia, diabetes mellitus, and current smoking, for the presence of NCP/PCPs, any stenosis, and obstructive stenosis were 0.81 (95% CI, 0.72–0.87), 0.82 (95% CI, 0.73–0.88) and 0.89 (95% CI, 0.81–0.94), respectively. The c-statistics for the presence of NCP/PCPs and any stenosis were significantly increased after the addition of the presence of small calcifications to 0.89 (95% CI, 0.82–0.94; p = 0.0037) and 0.89 (95% CI, 0.81–0.94; p = 0.013), respectively. However, the presence of small calcifications did not significantly increase the diagnostic value for the presence of obstructive stenosis (p = 0.50) (Fig. 3).
Fig. 3.
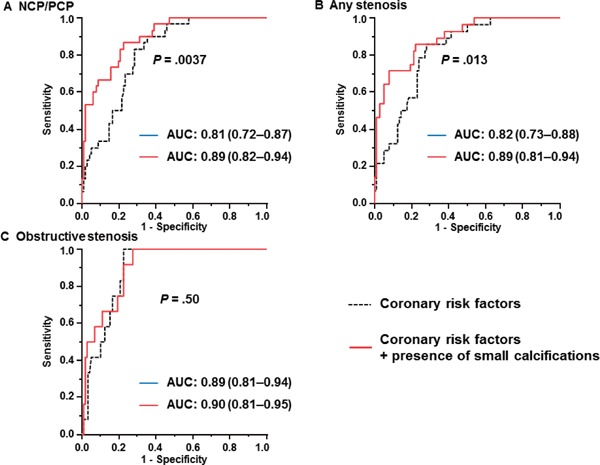
Incremental diagnostic values of small calcifications in addition to coronary risk factors for identifying patients with (A) noncalcified plaques (NCPs) and/or partially calcified plaques (PCPs), (B) any stenosis (≥25%), or (C) obstructive stenosis (≥50%). Coronary risk factors included age, sex, hypertension, dyslipidemia, diabetes mellitus, and current smoking.
Discussion
Small calcifications detected in 0.5-mm slice reconstructions increased the possibility of obstructive and non-obstructive CAD in patients with a conventional zero CAC score. Patients with small calcifications had a higher prevalence of multiple coronary risk factors compared to patients without small calcifications. Furthermore, small calcifications in addition to traditional coronary risk factors had incremental diagnostic values when predicting any coronary stenosis. Consequently, we believe that the identification of small calcifications is a convenient and efficient method for stratifying the risk of CAD.
Prevalence of Coronary Plaques and Stenosis in Patients with Zero CAC Scores
The identification of small calcifications using thin-slice reconstruction can help identify subjects with zero CAC scores from conventional reconstructions who are at higher risk for CAD. Although the prevalence of CAD is very low in subjects with a zero CAC score, the presence of CAD cannot be completely dismissed. The present study showed that 23% of patients had NCP/PCPs, 21% had any stenosis, and 9% had obstructive stenosis on CCTA. Previous studies identified a 13%–39% prevalence for coronary plaques in patients with a zero CAC score20, 21). The CoRE-64 study found that 19% of patients with zero CAC scores had obstructive CAD9). Our previous study with a 64-slice CT found NCP/PCPs in 29% and obstructive stenosis in 4% of suspected CAD patients with zero CAC scores22). In the present study, the prevalence of obstructive CAD in the conventional zero CAC group decreased from 9% to 5.2% with the use of 0.5-mm thin-slice reconstructions.
The predictive values of zero CAC scores in excluding CAD were different for asymptomatic and symptomatic patients. However, 10 patients with CAC scores of zero in the present study, even with no chest symptoms, were considered to be equivalent to symptomatic patients, because most of them had complications such as extra-coronary vascular disease, diabetes, or familial hypercholesterolemia. On the other hand, 32% of cases in our data had transient atrial fibrillation scheduled for catheter ablation. The usefulness of CAC scores and CCTA for these cases are still controversial.
Clinical Significance of Small Calcifications in Patients with Conventional Zero CAC Scores
The present study indicated that the detection of small calcifications in earlier stages of coronary atherosclerosis was important in identifying coronary plaques or stenosis in patients with conventional zero CAC scores. A recent multicenter study demonstrated that patients with coronary stenosis detected by CCTA, regardless of obstruction, had a poorer prognoses than those without23). We found small calcifications in 14% of patients with zero CAC scores from conventional 3.0-mm reconstructions. The proportion was similar or lower than that in previous reports, and several articles demonstrated that the conventional CAC method misclassified 21%–23% of patients13, 14, 24). In addition, Van der Biji et al. reported that in thin-slice reconstruction, the Agatston score was overestimated because the peak CT attenuation number in each voxel was counted14). However, in fact, our study demonstrated that small calcifications in thin-slice images were associated with coronary atherosclerotic lesions. Taken together, we propose that assessment of visually detecting small calcifications may allow identification of patients with CAD and rupture-prone coronary atherosclerotic lesions in subjects with conventional zero CAC scores.
Generally, vascular calcifications have been associated with advanced stages of atherosclerosis25). However, some studies have reported that micro-calcification was occasionally observed in the early stage of atherosclerosis26, 27). In addition, spotty calcifications detected by intravascular ultrasound were reported to be associated with coronary plaque vulnerability28). Therefore, this new method is expected to be a useful indicator for examination by CCTA, and for therapeutic interventions.
Limitations
First, our study was retrospective and had a small number of patients with CAC scores of zero, and did not evaluate patients with positive (>0) CAC scores. It is unclear whether the identification of small calcifications in 0.5-mm slice images is more useful for detecting coronary plaques and stenosis as detected by CCTA than stratification by conventional CAC score in patients with positive CAC scores. This study did not examine the prevalence of stenosis with invasive coronary angiography. Second, because of the low incidence of small calcification, we could not compare predictive powers in sub-group analyses such as scheduled catheter ablations for transient atrial fibrillation. Third, our data indicated that small calcifications had incremental diagnostic values when used with with coronary risk factors to predict coronary plaques and any stenosis, but not to predict obstructive stenosis. We believe that the identification of small calcifications was useful for detecting early stages of coronary atherosclerosis which have the potential to progress to obstructive lesions or culprit lesions in acute coronary syndrome. Furthermore, CT-derived vulnerable characteristic analyses were not performed because of the small numbers of NCP and/or PCP (40 segments in 30 patients). Finally, small calcifications detected by thin-slice scans may be misidentified because the signal-to-noise ratio in the thin-slice images is higher than that in conventional-slice images. However, recent developments in CT, such as using iterative reconstruction to decrease the signal-to-noise ratio, should overcome this problem29, 30).
Conclusions
The identification of small calcifications using 0.5-mm thin-slice reconstruction is useful for detecting coronary plaques and coronary stenosis in patients with zero CAC scores from conventional 3.0-mm slice reconstructions. In contrast, because the incidence of coronary lesions in patients without CAC in a thin-slice reconstruction was lower compared to conventional zero CAC, the need for contrast-enhanced CCTA may be eliminated in such patients.
Acknowledgments and Notice of Grant Support
This study was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (Tokyo, Japan, No. 23591044), and an MSD Research Grant.
Disclosures
None of the authors have any conflicts of interest to disclose.
Supplemental data
Comparison between AF ablation patients and no AF ablation patients.
| parameter | AF (n = 43) | no AF (n = 89) | P value |
|---|---|---|---|
| Age (yrs) | 56.6 ± 11.4 | 57.7 ± 12.0 | 0.63 |
| Male, % | 79 | 53 | 0.004 |
| Hypertension, % | 44 | 54 | 0.35 |
| Dyslipidemia, % | 40 | 67 | 0.003 |
| Diabetes mellitus, % | 5 | 15 | 0.089 |
| Smoking, % | 14 | 17 | 0.8 |
| FRS | 5.9 ± 3.8 | 6.7 ± 6.4 | 0.62 |
| CCTA results | |||
| Small calcification, % | 11 | 15 | 0.79 |
| obstructive stenosis, % | 2 | 8 | 0.27 |
| any stenosis, % | 12 | 26 | 0.07 |
| Plaque, % | 16 | 29 | 0.13 |
Predictive values of small calcification.
| parameter | AF (n = 43) SC+, SC− | no AF (n = 89) SC+, SC− |
|---|---|---|
| any stenosis, | 3/5 (60%), 2/38 (5%) | 12/13 (15%), 11/76 (92%) |
| Odds ratio (p value) | 24 (p = 0.0075) | 70 (p < 0.0001) |
References
- 1). Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R: Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol, 1990; 15: 827-832 [DOI] [PubMed] [Google Scholar]
- 2). Budoff MJ, Georgiou D, Brody A, Agatston AS, Kennedy J, Wolfkiel C, Stanford W, Shields P, Lewis RJ, Janowitz WR, Rich S, Brundage BH: Ultrafast computed tomography as a diagnostic modality in the detection of coronary artery disease: a multicenter study. Circulation, 1996; 93: 898-904 [DOI] [PubMed] [Google Scholar]
- 3). Yamamoto H, Kitagawa T, Kihara Y: Clinical implications of the coronary artery calcium score in Japanese patients. J Atheroscler Thromb, 2014; 21: 1101-1108 [DOI] [PubMed] [Google Scholar]
- 4). Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O'Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA: Coronary calcium as a predictor of coronary events in four racial or ethnic groups. New Engl J Med, 2008; 358: 1336-1345 [DOI] [PubMed] [Google Scholar]
- 5). Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, Flores FR, Callister TQ, Raggi P, Berman DS: Long-term prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol, 2007; 49: 1860-1870 [DOI] [PubMed] [Google Scholar]
- 6). Erbel R, Möhlenkamp S, Moebus S, Schmermund A, Lehmann N, Stang A, Dragano N, Grönemeyer D, Seibel R, Kälsch H, Bröcker-Preuss M, Mann K, Siegrist J, Jöckel KH, Heinz Nixdorf Recall Study Investigative Group : Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol, 2010; 56: 1397-1406 [DOI] [PubMed] [Google Scholar]
- 7). Maragiannis D, Schutt RC, Gramze NL, Chaikriangkrai K, McGregor K, Chin K, Nabi F, Little SH, Nagueh SF, Chang SM: Association of Left Ventricular Diastolic Dysfunction with Subclinical Coronary Atherosclerotic Disease Burden Using Coronary Artery Calcium Scoring. J Atheroscler Thromb, 2015; 22: 1278-1286 [DOI] [PubMed] [Google Scholar]
- 8). Blaha M, Budoff MJ, Shaw LJ, Khosa F, Rumberger JA, Berman D, Callister T, Raggi P, Blumenthal RS, Nasir K: Absence of coronary artery calcification and all-cause mortality. JACC Cardiovasc Imaging, 2009; 2: 692-700 [DOI] [PubMed] [Google Scholar]
- 9). Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffmann U, Cury RC, Abbara S, Brady TJ, Budoff MJ, Blumenthal RS, Nasir K: Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovascular imaging, 2009; 2: 675-688 [DOI] [PubMed] [Google Scholar]
- 10). Yamamoto H, Ohashi N, Ishibashi K, Utsunomiya H, Kunita E, Oka T, Horiguchi J, Kihara Y: Coronary calcium score as a predictor for coronary artery disease and cardiac events in Japanese high-risk patients. Circ J, 2011; 75: 2424-2431 [DOI] [PubMed] [Google Scholar]
- 11). Gottlieb I, Miller JM, Arbab-Zadeh A, Dewey M, Clouse ME, Sara L, Niinuma H, Bush DE, Paul N, Vavere AL, Texter J, Brinker J, Lima JA, Rochitte CE: The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol, 2010; 55: 627-634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Villines TC, Hulten EA, Shaw LJ, Goyal M, Dunning A, Achenbach S, Al-Mallah M, Berman DS, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng VY, Chinnaiyan K, Chow BJ, Delago A, Hadamitzky M, Hausleiter J, Kaufmann P, Lin FY, Maffei E, Raff GL, Min JK, CONFIRM Registry Investigators : Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: results from the CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter) registry. J Am Coll Cardiol, 2011; 58: 2533-2540 [DOI] [PubMed] [Google Scholar]
- 13). Aslam A, Khokhar US, Chaudhry A, Abramowicz A, Rajper N, Cortegiano M, Poon M, Voros S: Assessment of isotropic calcium using 0.5-mm reconstructions from 320-row CT data sets identifies more patients with nonzero Agatston score and more subclinical atherosclerosis than standard 3.0-mm coronary artery calcium scan CT angiography. J Cardiovasc Comput Tomgr, 2014; 8: 58-66 [DOI] [PubMed] [Google Scholar]
- 14). van der Bijl N, de Bruin PW, Geleijns J, Bax JJ, Schuijf JD, de Roos A, Kroft LJ: Assessment of coronary artery calcium by using volumetric 320-row multi-detector computed tomography: comparison of 0.5 mm with 3.0 mm slice reconstructions. Int J Cardiovasc Imaging, 2010; 26: 473-482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Urabe Y, Yamamoto H, Kitagawa T, Utsunomiya H, Tsushima H, Tatsugami F, Awai K, Kihara Y: Association between serum levels of n-3 polyunsaturated fatty acids and coronary plaque detected by coronary computed tomography angiography in patients receiving statin therapy. Circ J, 2013; 77: 2578-2585 [DOI] [PubMed] [Google Scholar]
- 16). Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA, 2001; 285: 2486-2497 [DOI] [PubMed] [Google Scholar]
- 17). Stevens LA, Coresh J, Greene T, Levey AS: Assessing kidney function--measured and estimated glomerular filtration rate. N Engl J Med, 2006; 354: 2473-2483 [DOI] [PubMed] [Google Scholar]
- 18). Tatsugami F, Matsuki M, Inada Y, Kanazawa S, Nakai G, Takeda Y, Morita H, Takada H, Ashida K, Yoshikawa S, Fukumura K, Narumi Y: Feasibility of low-volume injections of contrast material with a body weight-adapted iodine-dose protocol in 320-detector row coronary CT angiography. Acad Radiol, 2010; 17: 207-211 [DOI] [PubMed] [Google Scholar]
- 19). Raff GL, Abidov A, Achenbach S, Berman DS, Boxt LM, Budoff MJ, Cheng V, DeFrance T, Hellinger JC, Karlsberg RP, Society of Cardiovascular Computed Tomography : SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr, 2009; 3: 122-136 [DOI] [PubMed] [Google Scholar]
- 20). Henneman MM, Schuijf JD, Pundziute G, van Werkhoven JM, van der Wall EE, Jukema JW, Bax JJ: Noninvasive evaluation with multislice computed tomography in suspected acute coronary syndrome: Plaque morphology on multislice computed tomography versus coronary calcium score. J Am Coll Cardiol, 2008; 52: 216-222 [DOI] [PubMed] [Google Scholar]
- 21). Uretsky S, Rozanski A, Singh P, Supariwala A, Atluri P, Bangalore S, Pappas TW, Fisher EA, Peters MR: The presence, characterization and prognosis of coronary plaques among patients with zero coronary calcium scores. Int J Cardiovasc Imaging, 2011; 27: 805-812 [DOI] [PubMed] [Google Scholar]
- 22). Tsushima H, Yamamoto H, Kitagawa T, Utsunomiya H, Kunita E, Oka T, Urabe Y, Tsushima H, Awai K, Kihara Y: Association of epicardial and abdominal visceral adipose tissue with coronary atherosclerosis in patients with a coronary artery calcium score of zero. Circ J, 2015; 79: 1084-1091 [DOI] [PubMed] [Google Scholar]
- 23). Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah M, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng V, Chinnaiyan K, Chow BJ, Delago A, Hadamitzky M, Hausleiter J, Kaufmann P, Maffei E, Raff G, Shaw LJ, Villines T, Berman DS, CONFIRM Investigators : Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol, 2011; 58: 849-860 [DOI] [PubMed] [Google Scholar]
- 24). Arnold BA, Xiang P, Budoff MJ, Mao SS: Very small calcifications are detected and scored in the coronary arteries from small voxel MDCT images using a new automated/calibrated scoring method with statistical and patient specific plaque definitions. Int J Cardiovasc Imaging, 2012; 28: 1193-1204 [DOI] [PubMed] [Google Scholar]
- 25). Stary HC, Chandler AB, Dinsmore RE, Fuster V, Glagov S, Insull W, Jr, Rosenfeld ME, Schwartz CJ, Wagner WD, Wissler RW: A definition of advanced types of atheroscle rotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Arterioscler Thromb Vasc Biol, 1995; 15: 1512-1531 [DOI] [PubMed] [Google Scholar]
- 26). Aikawa E, Nahrendorf M, Figueiredo JL, Swirski FK, Shtatland T, Kohler RH, Jaffer FA, Aikawa M, Weissleder R: Osteogenesis associates with inflammation in early-stage atherosclerosis evaluated by molecular imaging in vivo. Circulation, 2007; 116: 2841-2850 [DOI] [PubMed] [Google Scholar]
- 27). Roijers RB, Debernardi N, Cleutjens JP, Schurgers LJ, Mutsaers PH, van der Vusse GJ: Microcalcifications in early intimal lesions of atherosclerotic human coronary arteries. Am J Pathol, 2011; 178: 2879-2887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28). Ehara S, Kobayashi Y, Yoshiyama M, Shimada K, Shimada Y, Fukuda D, Nakamura Y, Yamashita H, Yamagishi H, Takeuchi K, Naruko T, Haze K, Becker AE, Yoshikawa J, Ueda M: Spotty calcification typifies the culprit plaque in patients with acute myocardial infarction: an intravascular ultrasound study. Circulation, 2004; 110: 3424-3429 [DOI] [PubMed] [Google Scholar]
- 29). Leipsic J, Labountry TM, Heilbron B, Min JK, Mancini GB, Lin FY, Taylor C, Dunning A, Earls JP: Adaptive statistical iterative reconstruction: assessment of image noise and image quality in coronary CT angiography. AJR Am J Roentgenol, 2010; 195: 649-654 [DOI] [PubMed] [Google Scholar]
- 30). Tatsugami F, Matsuki M, Nakai G, Inada Y, Kanazawa S, Takeda Y, Morita H, Takada H, Yoshikawa S, Fukumura K, Narumi Y: The effect of adaptive iterative dose reduction on image quality in 320-detector row CT coronary angiography. Br J Radiol, 2012; 85: e378-e382 [DOI] [PMC free article] [PubMed] [Google Scholar]


