Abstract
Objective:
Primary care services form the foundation of modern healthcare systems, yet the breadth and complexity of services and diversity of patient populations may present challenges for creating comprehensive primary care information systems. Our objective is to develop regional-level information on the performance of primary care in Canada.
Methods:
A scoping review was conducted to identify existing initiatives in primary care performance measurement and reporting across 11 countries. The results of this review were used by our international team of primary care researchers and clinicians to propose an approach for regional-level primary care reporting.
Results:
We found a gap between conceptual primary care performance measurement frameworks in the peer-reviewed literature and real-world primary care performance measurement and reporting activities. We did not find a conceptual framework or analytic approach that could readily form the foundation of a regional-level primary care information system. Therefore, we propose an approach to reporting comprehensive and actionable performance information according to widely accepted core domains of primary care as well as different patient population groups.
Conclusions:
An approach that bridges the gap between conceptual frameworks and real-world performance measurement and reporting initiatives could address some of the potential pitfalls of existing ways of presenting performance information (i.e., by single diseases or by age). This approach could produce meaningful and actionable information on the quality of primary care services.
Abstract
Objectif:
Les services de soins primaires sont la base des systèmes de soins de santé modernes, mais l'étendue et la complexité des services ainsi que la diversité des patients peuvent présenter des défis quant à l'implantation de systèmes d'information efficaces sur les soins primaires. L'objectif est d'offrir de l'information au niveau régional sur le rendement des soins primaires au Canada.
Méthodes:
Une étude approfondie a été menée afin de recenser les initiatives existantes en ce qui concerne la mesure du rendement et la production de rapports sur le rendement des soins de santé de 11 pays. Les résultats de cette étude ont été utilisés par notre équipe internationale de chercheurs et de cliniciens en soins de santé primaires afin de proposer une approche pour la production de rapports sur le rendement des soins primaires au niveau régional.
Résultats:
Nous avons observé un écart entre, d'une part, les cadres théoriques pour la mesure du rendement présentés dans la littérature scientifique et, d'autre part, la mesure du rendement et la production de rapports que l'on trouve dans la réalité concrète des soins primaires. Les auteurs n'ont pas trouvé un cadre conceptuel ou une approche analytique qui pourrait servir de base pour un système d'information régional sur les soins de santé primaires. Par conséquent, nous proposons une approche en ce qui concerne la production de rapports sur le rendement: l'information doit être complète et exploitable, et elle doit être le fruit de ce qui est généralement accepté comme domaines centraux de soins de santé primaires, et elle doit aussi tenir compte des différents groupes de populations de patients.
Conclusions:
Une approche qui comble les différences entre le cadre théorique et la réalité en ce qui concerne la mesure du rendement et la production de rapports pourrait aborder quelques-unes des difficultés potentielles qui existent actuellement sur les manières de présenter l'information sur le rendement (par exemple, pour une seule maladie ou par âge). Cette approche pourrait produire de l'information utile et exploitable sur la qualité des services de soins de santé primaires.
Introduction
Providing information about the functioning of healthcare systems to relevant stakeholders, including providers, policy makers, patients and the general public is considered essential to a learning health system (Etheredge 2014; Smith et al. 2009). Performance information can be used to achieve a variety of ends including operating pay for performance programs, research, accreditation/benchmarking, practice management, quality improvement and public reporting (Adair et al. 2006a, 2006b; Kontopantelis et al. 2015; Panzer et al. 2013).
Health systems with strong primary care sectors are achieving better population health, equity, efficiency and quality of care (Kringos et al. 2013; Martin-Misener et al. 2012; Stange et al. 2014; Starfield et al. 2005). These are key dimensions of quality as outlined by the Institute of Medicine in their landmark report, Crossing the Quality Chasm (IOM 2001), as well as many other evidence-based conceptual frameworks for understanding important features of primary care (Hogg et al. 2008; Starfield 1998; Watson et al. 2004).
Performance measurement can be used to evaluate whether health systems are delivering quality care. Despite the importance of primary care as part of a high-functioning health system, comprehensive performance measurement in primary care is challenging because of the range and complexity of services provided, the dispersion of primary care practices (vs. acute care facilities), heterogeneity of the patient population and the early development stage of data collection systems (Kontopantelis et al. 2015; Russell 2015; Stange et al. 2014). Unlike specialist practitioners, primary care practitioners are involved in the full spectrum of care from health promotion and prevention, diagnosis and treatment of acute health issues, through to management of complex chronic conditions and end-of-life care planning (Starfield 1998). The patients seen by primary care practitioners are considerably more diverse than the patient groups seen by other healthcare professionals (Porter et al. 2013; Stange et al. 2014). One example demonstrating the broad scope of primary care practitioners is the finding that Canadian fee-for-service family physicians use up to 10 times the number of ICD diagnosis codes compared with other fee-for-service specialities (Cunningham et al. 2014).
Primary care in Canada, as elsewhere, is in the process of experimentation and change in organization, funding and care delivery (Hutchison and Glazier 2013; Hutchison et al. 2011). A large proportion of primary medical care is provided through family doctors who are mostly independent business operators (unlike a single health authority), which makes system management challenging. As such, there is need for a primary care performance measurement system that supports pan-Canadian learning as well as regional planning and policy development, because health system changes often occur at the regional level. This includes a need for information on how the primary care system meets the needs of patients seen in primary care, including the most medically complex groups of patients who have been identified as the target of reform efforts (Hutchison and Glazier 2013; Lane et al. 2015). Indeed, a central feature of successful performance measurement is alignment with the strategic direction and scope of healthcare systems. Furthermore, it is important for performance measurement to be underpinned with a robust conceptual framework to guide the selection of meaningful measures and indicators (Adair et al. 2006a, 2006b; IOM 2006; Smith et al. 2009). In other words, there should be a match between a primary care performance measurement system and accepted conceptual frameworks that articulate important features of high-quality primary care systems.
The objective of this project was to review existing trends and literature related to primary care performance measurement with the goal of identifying an approach that can form the basis of a regional-level pan-Canadian reporting system. The assumption is that improvement is always possible but is difficult to achieve in the absence of actionable information. We use the results of a scoping review of current initiatives in high-income countries and input from an international team of primary care researchers and clinicians to present an approach for measurement and reporting that can be used for system improvement.
Methods
Multidisciplinary research team
Our research team consists of a range of researchers (with expertise in both qualitative and quantitative methods) and health professionals (family doctors, nurses, psychologists and other allied health professionals) from Canada, the UK and Australia. This team was specifically established to reflect expertise in primary care research and performance measurement and reporting.
Scoping review of primary care measurement initiatives: A comparison across 11 countries We conducted a scoping review of current practices in performance measurement and reporting to map what is currently known (or in our case, done) in this area (Arksey and O'Malley 2005; Levac et al. 2010). As our focus is pan-Canadian reporting, we sought to analyze the features of national primary care performance measurement initiatives across high-income countries, noting that many national initiatives include reporting at different levels of aggregation (e.g., practice-level, regional, state, national). The value in national approaches is standardization to support nationally consistent and locally relevant reporting such that regions can learn from high-performing regions across the nation. We selected the 11 countries included in the Commonwealth Fund's international primary care and health policy surveys: Australia, Canada, England, France, Germany, Netherlands, New Zealand, Norway, Sweden, Switzerland and the US (Davis et al. 2014; Schoen et al. 2009). This choice allowed us to cover several healthcare systems that are most similar to Canada and that have been previously compared to Canada in relation to primary care performance (Schoen et al. 2009).
We used information in the Commonwealth Fund international profiles of healthcare systems to start our search to identify national primary care performance initiatives across the 11 countries (The Commonwealth Fund 2014). We also asked those affiliated with our project (including representatives from Australia, France and the UK) to provide details of any organizations meeting our inclusion criteria.
Results are based on web pages retrieved during the date range 30 November 2014 to 20 May 2015. Our inclusion criteria were: national primary care performance measurement initiatives; the organization presented primary care indicator sets or performance results in the public domain in English. We extracted information on frameworks, terminology used to describe primary care and reporting activities.
Input from multidisciplinary research team
As we did not identify an approach we could directly adapt to the Canadian setting, a new approach was developed based on existing models to offer regional reporting and population segmentation (to monitor performance for different patient groups with expected different levels of need for services). The model was reviewed and adapted iteratively over several sessions by the research team.
Results
Primary care performance measurement initiatives
Seven of the 11 countries had national initiatives in the form of primary care indicator sets/specifications or reporting; three countries had limited information available in English (Norway, Switzerland and France) and we did not identify any initiatives in Germany (see Table 1). There were differences in the information available, ranging from static reports (Netherlands, Sweden and the US), to online atlases mapping geographic variations in care (New Zealand, Australia and Canada), as well as routinely updated reports and interactive web displays (Australia, Canada and England). In some jurisdictions, there were multiple initiatives: for example, there are several websites in England providing practice-, regional- and national-level information and a recognition that information needs to be streamlined to avoid duplication (The Health Foundation 2015). In contrast, there was limited information on pan-Canadian primary care performance. This is not surprising given that Canadian healthcare is provincially organized and we only considered national-level initiatives as part of our review. Primary care performance measurement and reporting activities (including provincial initiatives) were subject to several federal–provincial agreements (from 2004 to 2014) to report on certain elements of primary care performance, yet no province met their reporting obligations under that mandate and there was almost no pan-Canadian comparative data at the end of that decade (Johnston and Hogel 2016). More recently, there have been a growing number of provincial-level performance measurement initiatives such as the Primary Care Performance Measurement Framework developed by Health Quality Ontario and this organization's quality indicators are being reported to physicians and the public (Health Quality Ontario 2014).
Table 1.
Characteristics of national reporting systems that produce primary care performance information, by country
| Organizations reporting on primary care | Description | Reporting format | Framework: performance domains | Website |
|---|---|---|---|---|
| Australia | ||||
| MyHealthy Communities, National Health Performance Authority | National independent agency, reports local-level health information. Many of the MyHealthyCommunities measures focus on primary care. | Public reports and interactive website. | Whole of health system: Equity, effectiveness, efficiency and population health outcome measures. | <www.myhealthycommunities.gov.au/> |
| Canada | ||||
| Your Health System, Canadian Institute for Health Information (CIHI) Performance Measurement Framework | Independent agency, reports local-level and national health information. A small number of primary care indicators reported with other healthcare indicators; detailed in a report and interactive website. | Public reports and interactive website. | Whole of health system: Health system and context as inputs (e.g., social determinants of health). Health system outputs include access, person-centred, safe, appropriate, effective and efficiency. | <www.cihi.ca/cihi-ext-portal/internet/en/tabbedcontent/health+system+performance/our+health+system/cihi013620> |
| CIHI Pan-Canadian Primary Care Indicators | A suite of indicators developed specifically for pan-Canadian reporting. | Public report detailing indicators. No current pan-Canadian reporting. | Primary care specific (indicator groupings): acceptability, accessibility, appropriateness, comprehensiveness, coordination, effectiveness, efficiency, expenditure, governance, health status, information technology infrastructure and workforce. | <www.cihi.ca/CIHI-ext-portal/internet/EN/TabbedContent/types+of+care/primary+health/cihi006583> |
| England | ||||
| National Health Service (NHS) Outcomes Framework | A small number of primary care indicators reported with other healthcare indicators; detailed in a report. | Public reports and interactive website. | Premature mortality, quality of life (long-term conditions), recovery from illness, patient experience, patient safety. | <www.gov.uk/government/publications/nhs-outcomes-framework-2014-to-2015> |
| Quality and Outcomes Framework (QOF), NHS | Primary care indicators developed for pay-for-performance (physician incentives to improve care quality). | Public reports and interactive website. | Primary care specific: clinical, public health, quality and productivity (previously organizational), patient experience. | <http://qof.hscic.gov.uk/> |
| Care Quality Commission (CQC) | Monitoring system for general practices to help monitor the quality of care (e.g., used to plan inspection activities and also publicly available). | Public reports and interactive website. | Primary care specific: effectiveness, responsiveness and care. | <www.cqc.org.uk/> |
| NHS Choices | Launched to support the public become active consumers of healthcare and to make healthcare decisions. | Interactive website. | Whole of health system: user ratings, online facilities, patient experiences of care and quality of services, patients with long-term conditions, age of patients and use of hospitals. | <www.nhs.uk/pages/home.aspx> |
| GP Patient Survey (on behalf of NHS) | GP patient survey sent to over 1 million people across the UK.. | Public reports and interactive website. | No specific framework. Questions are in relation to access and experiences with primary care and dental care. | <https://gp-patient.co.uk/about> |
| New Zealand | ||||
| Atlas of Variation in Health Care, Health Quality and Safety Commission | National and local-level reporting. Several measures related to primary care contained in the online interactive Atlas. | Public reports and interactive website. | Indicator groupings by clinical areas. | <www.hqsc.govt.nz/our-programmes/health-quality-evaluation/projects/quality-accounts/> |
| Norway - Limited information available in English | ||||
| Sweden | ||||
| Quality and Efficiency in Swedish Health Care, Swedish Association of Local Authorities and Regions | National and local-level reporting. Several measures related to primary care in the report. | Public report. | Whole of health system: overall indicators (e.g., mortality) and indicators by 12 clinical areas. | <www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/19072/2013-5-7.pdf> |
| Switzerland - Limited information available in English | ||||
| US | ||||
| Healthcare Effectiveness and Data Information Set (HEDIS) | A collection of indicators focused on primary care performance. Indicator specifications developed for health plans; designed to assist consumers in health plan selection. | Public report. | Indicators groupings: effectiveness, access, patient experience, utilization/resource use, health plan descriptive. | <www.ncqa.org/HEDISQualityMeasurement/WhatisHEDIS.aspx> |
| Physician Quality Reporting System (PQRS) | Government-run (Centres for Medicare and Medicaid) voluntary program collecting data on healthcare performance including primary care. | Indicators available online. Results not publicly reported; direct to physicians. | Indicator groupings: effectiveness, safety, communication/coordination, person-centred, efficiency, community/population health. | <www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/> |
| Physician Consortium Performance Improvement (PCPI) | Physician-led (American Medical Association) effort to drive improvement and support healthcare professionals. | Indicators available online. Results not publicly reported; direct to physicians. | Primary care: Indicators in 47 clinical areas. | <https://www.ama-assn.org/about/improving-health-outcomes> |
| Quality Indicators, Agency for Healthcare Research and Quality (AHRQ) | Indicator specifications for providers and clinicians: the prevention quality indicators relate to primary care. | Indicators available online, results not publicly reported. | Whole of health system: prevention quality and safety indicators related to primary care. | <www.qualityindicators.ahrq.gov/Modules/pqiresources.aspx> |
We found that most indicator sets reported by national organizations focused on clinical areas of performance (e.g., technical quality of care measures) with no specific over-arching conceptual framework. An exception to this was the Quality and Outcome Framework (UK), which was developed around a conceptual primary care framework that included organizational, clinical and patient experience dimensions, though most measures are focused on technical aspects of the quality of care. In fact, clinical, or technical, quality of care measures for single diseases such as diabetes and cardiovascular disease and prevention measures such as immunization rates currently dominate measurement, terminology and reporting efforts in many jurisdictions (Higgins et al. 2013). Where broader dimensions of primary care are considered, access to care is most commonly reported. This may evolve in the near future with agencies such as the National Quality Forum in the US (responsible for endorsing thousands of measures/indicators, including HEDIS measures) developing new approaches to measuring quality in specific patient populations particularly relevant to primary care such as patients with multi-morbidity.
There was a range in the level of focus on primary care, for example, the US HEDIS indicator set was developed specifically for primary care. And while there is currently no national primary care reporting system in Canada outside of the work produced by the Commonwealth Fund, the Canadian Institute for Health Information (CIHI) has developed some indicator specifications designed for pan-Canadian reporting (CIHI 2012). Some initiatives produced information on primary care as part of a broader conception of the healthcare system that included hospital care plus primary care and in some cases, population health (e.g., Dutch Health Performance Report, National Health Performance Authority, Quality and Efficiency in Swedish Health Care, Swedish Association of Local Authorities and Regions, CIHI Your Health initiative and reporting framework). The frameworks driving these initiatives were broad (i.e., not specifically focused on primary care), but measures remain in healthcare silos rather than, for example, tracking patient pathways from primary care to acute care.
Bringing it all together: input from a multidisciplinary research team to propose a matrix for performance measurement in primary care
In primary care, there is a history of research that has produced frameworks to capture the nature of primary care patients and organizational structure for the purposes of quality evaluation and system improvement (Hogg et al. 2008; Kringos et al. 2010; Starfield 1998; Watson et al. 2004). In terms of performance measurement and reporting, there appears to be a proliferation of measures and public reporting but little evidence of conceptual frameworks (e.g., Hogg et al. 2008; Kringos et al. 2010; Senn et al. 2014; Starfield 1998; Watson et al. 2004) being used to organize performance measurement activities. There is thus a mismatch between researcher-developed frameworks, which will not necessarily focus on implementation, and system-developed indicators not rooted in robust conceptual frameworks. To address this, our international team of primary care researchers and clinicians proposes an approach to bridge research and real-world primary care measurement and reporting building on the strengths of each initiative.
Rigorous conceptual frameworks help anchor measurement in some kind of logical system and convey why and what we are measuring. Indicator systems, in contrast, are practically focused, with indicators specific to patients who are the target of specific concern (e.g., diagnoses of interest). We propose that a fruitful path forward is a matrix approach to performance measurement, incorporating the focused approach of measurement in identified patient or population segments that represent different primary care needs (the rows), with measures chosen to reflect performance domains representing accepted features of high-quality primary care (the columns) (see Figure 1).
Figure 1.
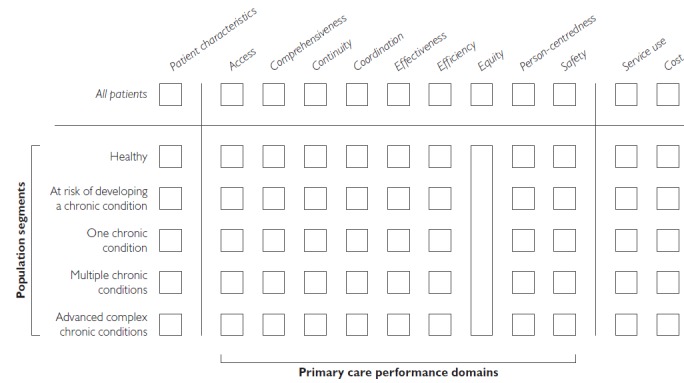
Proposed performance measurement framework*
*This framework is a matrix structure of domains of primary care performance by patient population segments. The selection of performance domains and population segments can be modified depending on the intended use of the framework or the specific jurisdiction.
We suggest that population segmentation can address the heterogeneity of primary care patients and produce actionable information on primary care functioning. The most common ways of stratifying or segmenting the population include presentation of information by age or specific diagnoses; however, these approaches may not accurately determine health system burden (Evans et al. 2010; Morgan and Cunningham 2011) or may produce many small categories, each of which account for only a small percentage of primary care patients. For example, not all elderly patients have high healthcare needs and patients with very different chronic conditions may share the same needs for resources or benefit from common care organization (Caminiti et al. 2013; Mukhi et al. 2014; Ricci-Cabello et al. 2015). As a result, existing approaches can require the use of hundreds of individual disease-specific measures but struggle to capture and measure patients with multi-morbidities (Caminiti et al. 2013; Mukhi et al. 2014) or to represent a practice or system overall. In the context of increasing complexity of patient diagnoses (e.g., multi-morbidity), patient populations could be grouped, not by specific diseases but by health status, functional ability and/or healthcare needs (Lynn et al. 2007). This has been proposed as an approach to support planning and organizing health service delivery (Lynn et al. 2007) and specifically, primary care service delivery (BC Ministry of Health 2014; Dow et al. 2013; Hewner et al. 2014; Porter et al. 2013; Zhou et al. 2014) but with little discussion about the potential implications for performance measurement.
As the need for primary care services may be vastly different for patients in different groups, reporting by population segment may directly inform resource allocation efforts or the organization of services (i.e., to match services to patient need). For example, in Figure 2, continuity for all patients is average, whereas performance by patient group ranges from low (healthy patients) to high (multiple chronic conditions, advanced chronic conditions). In this example, the lower continuity scores for healthy patients might not be of concern to a regional healthcare planner as these patients are relatively stable with relatively few primary care needs; yet the high scores for more complex patients suggest success in the delivery of primary care for this particular dimension. If in this example continuity of care was low for the most complex patients, this may be a cause of concern for clinicians and decision-makers in a given region. Specifically, it is important that continuity of care is adequate for patients with multiple complex chronic disease, both from a quality and cost perspective; these patients use significantly more healthcare services, including multiple providers, prescriptions and routine tests, compared to a healthy patient with no chronic conditions who uses very few health services, and high continuity of care has been associated with reduced use of hospital services, which are the most expensive part of the healthcare system (Burge et al. 2003; Haggerty 2012; Haggerty et al. 2003). This example demonstrates that population segmentation would allow fine-tuning of performance on important dimensions according to patterns of care associated with improved patient outcomes and reduced healthcare costs.
Figure 2.
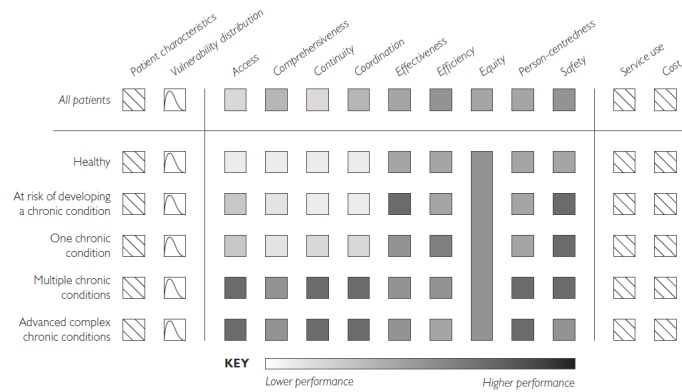
Demonstration of the performance measurement framework in practice*
*This figure shows that results for healthcare regions may be average across “all patients” but vary within different population segments. For the purposes of simplicity, results are mapped for each domain; in reality, there will be multiple measures for each performance domain. The vulnerability distribution for each patient group will be factored into some measures to assess equity.
Determining Population Segments
We propose categorizing patients according to the nature and extent of expected primary care involvement, ranging from minimal (e.g., routine screening, treatment for minor time-limited conditions) through to high intensity involvement (e.g., care coordination, symptom management, ongoing tests, prescription management, and coordinating care across multiple settings and providers) (Ashman and Beresovsky 2013; Venkatesh et al. 2014).
While the specifics will vary by jurisdiction, using a set of principles (Box 1), we provide an example of five population segments that we plan to test for acceptability as part of our pan-Canadian stakeholder engagement plan for the Transformation project (Table 2). The five groups are: healthy, at risk of developing a chronic condition, one chronic condition, multiple chronic conditions and advanced complex chronic conditions (including patients approaching the end of life). We note that groups will not be of equal size; healthy patients will comprise the largest proportion of the total population in any primary care system and they will have the lowest per capita service use and relatively light requirements for primary care. In contrast, patients with multiple chronic conditions will be one of the smallest groups (by total population) but will in all likelihood account for the greatest per capita use of primary care services.
Box 1. Principles for developing population segments to form the basis of a regional-level primary care information system.
We considered principles used in examples of population segmentation with a focus on the work of Lynn et al. (2007), Porter et al. (2013) and others (BC Ministry of Health 2014; Dow et al. 2013; Hewner et al. 2014; Zhou et al. 2014) to provide some guidance on optimal features of population segments. We have established the following criteria:
Captures the vast majority of people who interact with primary care services.
Based on anticipated (vs. actual) primary care involvement with an aim to identify groups based on “need for primary care” as opposed to utilization of primary care services. This is a more nuanced approach to developing groups using health service use, but it is likely to correlate with health service use given that sicker patients usually use more healthcare services (Bayliss et al. 2015; Ionescu-Ittu et al. 2007; Lynn et al. 2007).
Relatively homogenous in terms of the primary healthcare needs and health priorities of patients in each group (e.g., staying healthy, getting better, living with illness or dealing with a life-limiting illness).
Mutually exclusive such that the tallying of groups is equal to the whole population.
The number of groups would be large enough to enable regional comparisons yet small enough to enable reporting at smaller levels (e.g., practice-level reporting, if this became an area of interest at some stage in the future).
Enable tracking the quality of care longitudinally (i.e., patients may be classified into different segments over time as their health status improves or deteriorates).
Table 2.
Population segments for inclusion in primary care performance measurement framework
| Population group | Description | Rationale for inclusion in a primary performance measurement framework |
|---|---|---|
| Healthy | No ongoing medical conditions or behavioural risk factors. Possible acute conditions that require time-limited treatment (e.g., pregnancy, accidental injury). | Comprises the majority of the population; expected use of primary care is low (Porter et al. 2013). The role of primary care is maintenance of health and possible management of time-limited acute conditions. |
| At risk of developing a chronic conditior | Presence of medical risk factors for developing a chronic disease (e.g., overweight or obese, smoking excessive alcohol consumption, recreational drug use, sedentary lifestyle) | A growing proportion of the population; expected use of primary care is low but this is a priority group as primary care has a role in treatment plans for modifiable risk factors (Thorpe 2005). Primary care has an important role in preventive medicine such as behavioural programs for weight management and smoking cessation. Successful strategies could result in patients moving into the healthy population group as opposed to developing chronic disease(s) (Porter et al. 2013). |
| One chronic condition | One ongoing chronic condition with impact on functional status (e.g., diabetes mellitus, hypertension). | A growing proportion of the population; expected use of primary care is moderate with the majority of primary care patients having at least one chronic disease (Bayliss et al. 2014; Milani and Lavie 2014). Evidence-based guidelines are available to guide the care of these patients; technical quality of care metrics may be useful for this patient group. Successful management may prevent the development of additional chronic diseases. Primary care has a role in ongoing disease management and prevention of secondary complications (Porter et al. 2013). |
| Multiple chronic conditions | Two or more ongoing chronic conditions with impact on functional status | A growing proportion of the population; expected use of primary care is high (Banerjee 2014; Bayliss et al. 2014; Fortin et al. 2012; Koller et al. 2014). There are few evidence-based guidelines or quality metrics currently available to guide care for this patient group. As such, data on the performance of primary care for this group has particular utility. Primary care has a role in ongoing disease management and prevention of secondary complications (Porter et al. 2013). |
| Advanced complex chronic conditions | Multiple advanced chronic conditions with complications or patient approaching the end of life | The smallest population segment, but these patients use more healthcare services than any other group (Lunney et al. 2002; Lynn et al. 2007); expected use of primary care will vary and there are concerns about the quality of care (e.g., over-reliance on hospital services, underutilization of primary care or palliative services). Primary care has a role in ongoing disease management, prevention of secondary complications with the aim of avoiding the need for unplanned hospital care (Porter et al. 2013). |
Given that factors such as social determinants of health and other relevant risk factors may be dependent on local-level context (e.g., population characteristics, resource allocation priorities), we suggest incorporating these into the measurement system for specific measures/indicators rather than further segmenting population groups into more and less vulnerable patients.
Identifying Performance Domains
There are a variety of domains that have been used to describe primary care performance internationally (Hogg et al. 2008; Kringos et al. 2010). A recent synthesis of over 80 studies identified 10 core dimensions of primary care across three measurement domains of structure (governance, economic conditions and workforce development), process (access, comprehensiveness, continuity and coordination) and outcome (quality, efficiency and equity) (Kringos et al. 2010). For the purposes of regional primary healthcare performance measurement, we suggest using commonly accepted domains that cover the broadest scope of primary care practice. Perhaps the most cited domains of primary care are those defined by Starfield (1998), who described primary care as having the following attributes: first point of contact (accessibility); person-focused and longitudinal care (continuity); provision of care for all but uncommon conditions (comprehensive); and coordination/integration of care provided by other healthcare providers (Starfield 1998). We also suggest inclusion of the Institute of Medicine's six domains of quality proposed in the seminal report, Crossing the Quality Chasm, which continues to be the enduring definition of healthcare quality: access (or timeliness), safety, patient experience (patient-centredness), efficiency, effectiveness and equity (IOM 2001, 2006).
To complement the primary care performance domains, we suggest tracking information on health services use and cost (including physician visits, hospital services, emergency room visits, diagnostic and therapeutic procedures and medicines), overall and by healthcare sector. For example, we will examine the nature and costs of primary care service use and hospital use by population subgroups. Such information is important as effective use of primary care (e.g., health promotion, prevention) could impact total cost and health outcomes, and this lens allows for examination of the extent of integration across health sectors (Berwick et al. 2008). Presenting information on primary care in isolation perpetuates the fragmented nature of health service delivery and does not promote an environment of shared accountability across hospital and community settings (IOM 2006; Venkatesh et al. 2014). As Venkatesh et al. stated; “Unlike quality measures … the health of patients cannot be sliced into specific care settings or cut into pieces among provider types” (Venkatesh et al. 2014: 76).
Discussion
We compared national primary care performance measurement initiatives across 11 countries with the goal of identifying an approach we could use to drive the development of a regional-level pan-Canadian primary information system. Despite a growing range of reporting activity, few systems used conceptual frameworks of primary care. To address this, we propose a matrix approach to primary care performance measurement and reporting that is grounded in the organization of primary care services (Hogg et al. 2008; Kringos et al. 2010; Watson et al. 2004) and primary care needs of different population groups. Our approach looks beyond single-disease or age-based segmentation approaches because not all patients with a given condition or of a given age have the same healthcare needs and reporting by condition has decreasing value when a growing number of patients are diagnosed with multiple conditions (Banerjee 2014; Barnett et al. 2012; Bayliss et al. 2014).
We suggest that population segmentation may mitigate or reduce the need for complex case-mix adjustment methods (Smith et al. 2009) – something that is usually recommended when producing comparative performance information. Risk adjustment attempts to account for differences in patient populations to allow for fair comparisons of health system performance, but even with cutting-edge risk adjustment and state-of-the-art data sets, we are currently unable to adequately measure all of the patient and health system factors that may influence health system performance (Doggen et al. 2014; Smith et al. 2009). In contrast, the population segmentation approach effectively serves as a stratification approach instead of trying to risk-adjust within a broader population grouping. Perhaps more importantly in this context, stratification is potentially more useful in providing actionable information because it identifies differences rather than trying to reduce differences or understand performance on average. At a local level, this allows for transparency about regional differences in patient characteristics and healthcare needs as well as being able to compare the performance of primary care with other regions.
Our matrix aligns with primary care service delivery and patient populations, thus optimizing the potential impact of performance measurement and reporting activities. This approach recognizes the variation in the type of care required by patients who use primary care, ranging from patients who are stable and require only acute and time-limited treatment to long-term chronic disease management, with the latter accounting for the majority of modern day primary care visits (Milani and Lavie 2014). We have deliberately chosen to identify patient groups based on expected primary care need/use (prospectively) rather than “high utilizer” approaches that select the most costly patients and track them over time (Emeche 2015; Newton and Lefebvre 2015). Our approach could provide more nuanced information that will allow clinicians and decision-makers to identify gaps in the delivery of primary care (e.g., sick patients without access to care) and information for policy makers to channel resource allocation and efforts for improved efficiency and value for money in healthcare over time (e.g., duplication of tests for patients with low continuity of care) (Panzer et al. 2013; Porter 2010).
While beyond the scope of this paper, there will be many challenges to consider in implementing our approach into an actionable pan-Canadian primary care reporting system (Adair et al. 2006a, 2006b; Panzer et al. 2013). Our approach is designed to be flexible and adaptable to different settings and jurisdictions but implementation should include stake-holder engagement (Ivers et al. 2014; Oliver et al. 2014) to ensure that the framework and resulting performance information aligns with existing initiatives and meets the needs of the target users that may include patients, clinicians, decision-makers and health system managers. Our project team has embarked upon an extensive stakeholder consultation process using case studies, deliberative dialogues and workshops to gain input on implementing our performance matrix (developing patient subgroups and indicator selection).
Another important challenge is avoiding selecting and reporting measures based on what is easiest to measure given data availability and historically popular metrics. The approach we have taken is to develop a data infrastructure that combines patient, provider, primary care organization and health system perspectives. We are using our data infrastructure (surveys and health administrative data) to develop our population segments and choose measures to report on; however, there are other data sources (e.g., electronic health records, clinical data) that could be harnessed to develop population segments and report on primary care performance (Vuik et al. 2016). Regardless of what data are available, there is the challenge of choosing how to segment the population. We present one possible five-category segmentation approach, but again, the framework is meant to be flexible and calibrated to local needs. Determining the segments could be done very simply, for example, based on patient age, or in a more complex way, including morbidity and/or socio-economic status. These decisions will best be made with stakeholder engagement, as any segmentation must be meaningful to the potential users of the resulting performance information (The Health Foundation 2015).
The proposed matrix approach to primary care performance measurement reflects a need for regional planning based on healthcare needs of populations in an era of increasing patient complexity and multi-morbidity. To our knowledge, this is the first primary care performance measurement approach to make use of broad conceptual frameworks containing multiple dimensions of primary care and population segmentation – an approach that may move this field forward. Our work is timely in the context of the new Canadian health accord and suggestions that a per capita approach to funding be replaced with an approach that takes into account regional variations in population characteristics (Vogel 2015). While there have been suggestions that the age of populations might be a way to organize funding, we suggest that a more nuanced approach that groups patients according to complexity and healthcare needs may be a more useful way to understand the performance of primary care and other parts of the healthcare system (Lynn et al. 2007).
Acknowledgements
This research was funded by the Canadian Institutes of Health Research (CIHR) and Michael Smith Foundation for Health Research (Agreement number 01247-000) through a Community-Based Primary Health Care (CBPHC) Innovation Team grant.
Contributor Information
Julia M. Langton, Research Associate, Centre for Health Services and Policy Research, University of British, Columbia Vancouver, BC.
Sabrina T. Wong, Professor, Centre for Health Services and Policy Research & School of Nursing, University of British Columbia, Vancouver, BC.
Sharon Johnston, Associate Professor, Department of Family Medicine, University of Ottawa & Bruyere Research Institute, Ottawa, ON.
Julia Abelson, Professor, Department of Clinical Epidemiology & Biostatistics, Centre for Health Economics and Policy Analysis, McMaster University, Hamilton, ON.
Mehdi Ammi, Assistant Professor, School of Public Policy & Administration, Carleton University, Ottawa, ON.
Fred Burge, Professor, Faculty of Medicine, Dalhousie University, Halifax, NS.
John Campbell, Professor, Primary Care Research Group, University of Exeter Medical School, Exeter, UK.
Jeannie Haggerty, Professor, Faculty of Medicine, McGill University, Montréal, QC.
William Hogg, Professor, Department of Family Medicine, University of Ottawa & Bruyere Research Institute, Ottawa, ON.
Walter P. Wodchis, Associate Professor, Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON.
Kimberlyn McGrail, Associate Professor, Centre for Health Services and Policy Research, University of British Columbia, Vancouver, BC.
References
- Adair C.E., Simpson E., Casebeer A.L., Birdsell J.M., Hayden K.A., Lewis S. 2006a. “Performance Measurement in Healthcare: Part I – Concepts and Trends from a State of the Science Review.” Healthcare Policy 1(4): 85–104. 10.12927/hcpol.2006.18248. [PMC free article] [PubMed] [Google Scholar]
- Adair C.E., Simpson E., Casebeer A.L., Birdsell J.M., Hayden K.A., Lewis S. 2006b. “Performance Measurement in Healthcare: Part II – State of the Science Findings by Stage of the Performance Measurement Process.” Healthcare Policy 2(1): 56–78. 10.12927/hcpol.2006.18338. [PMC free article] [PubMed] [Google Scholar]
- Arksey H., O'Malley L. 2005. “Scoping Studies: Towards a Methodological Framework.” International Journal of Social Research Methodology 8(1): 19–32. 10.1080/1364557032000119616. [Google Scholar]
- Ashman J.J., Beresovsky V. 2013. “Multiple Chronic Conditions among US Adults Who Visited Physician Offices: Data from the National Ambulatory Medical Care Survey, 2009.” Preventing Chronic Disease 10: E64. 10.5888/pcd10.120308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee S. 2014. “Multimorbidity – Older Adults Need Health Care that Can Count Past One.” Lancet 385(9968): 587–89. 10.1016/S0140-6736(14)61596-8. [DOI] [PubMed] [Google Scholar]
- Barnett K., Mercer S.W., Norbury M., Watt G., Wyke S., Guthrie B. 2012. “Epidemiology of Multimorbidity and Implications for Health Care, Research, and Medical Education: A Cross-Sectional Study.” Lancet 380(9836): 37–43. 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- Bayliss E.A., Bonds D.E., Boyd C.M., Davis M.M., Finke B., Fox M.H. et al. 2014. “Understanding the Context of Health for Persons with Multiple Chronic Conditions: Moving from What Is the Matter to What Matters.” Annals of Family Medicine 12(3): 260–69. 10.1370/afm.1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayliss E.A., Ellis J.L., Shoup J.A., Zeng C., McQuillan D.B., Steiner J.F. 2015. “Effect of Continuity of Care on Hospital Utilization for Seniors with Multiple Medical Conditions in an Integrated Health Care System.” The Annals of Family Medicine 13(2): 123–29. 10.1370/afm.1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BC Ministry of Health. 2014. The Blue Matrix: How Big Data Provides Insight into the Health of the Population and their Use of Health Care in British Columbia | ihdlnconference2014.org. Retrieved October 14, 2014. <www.ihdlnconference2014.org/abstract/Burd>.
- Berwick D.M., Nolan T.W., Whittington J. 2008. “The Triple Aim: Care, Health, and Cost.” Health Affairs (Project Hope) 27(3): 759–69. 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- Burge F., Lawson B., Johnston G. 2003. “Family Physician Continuity of Care and Emergency Department Use in End-of-Life Cancer Care.” Medical Care 41(8): 992–1001. <http://ovidsp.ovid.com/ovidweb.cgi?T=JS&C SC=Y&NEWS=N&PAGE=fulltext&D=med4&AN=12886178>. [DOI] [PubMed] [Google Scholar]
- Caminiti C., Meschi T., Braglia L., Diodati F., Iezzi E., Marcomini B. et al. 2013. “Reducing Unnecessary Hospital Days to Improve Quality of Care Through Physician Accountability: A Cluster Randomised Trial.” BMC Health Services Research 13: 14. 10.1186/1472-6963-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI). 2012. Pan-Canadian Primary Health Care Indicator Update Report. Retrieved June 17, 2016. <https://secure.cihi.ca/estore/productFamily.htm?locale=en&pf=PFC2000&lang=en>.
- Cunningham C.T., Cai P., Topps D., Svenson L.W., Jetté N., Quan H. 2014. “Mining Rich Health Data from Canadian Physician Claims: Features and Face Validity.” BMC Research Notes 7(1): 682. 10.1186/1756-0500-7-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis K., Stremikis K., Squires D., Cathy S. 2014. “Mirror, Mirror on the Wall, 2014 Update: How the U.S. Health Care System Compares Internationally, The Commonwealth Fund.” <www.commonwealthfund.org/publications/fund-reports/2014/jun/mirror-mirror>.
- Doggen K., Lavens A., Van Casteren V. 2014. “The Right Indicator for the Job: Different Levels of Rigor may be Appropriate for the Development of Quality Indicators. Comment on Stelfox and Straus.” Journal of Clinical Epidemiology 67(9): 963–64. 10.1016/j.jclinepi.2014.03.001. [DOI] [PubMed] [Google Scholar]
- Dow A.W., Bohannon A., Garland S., Mazmanian P.E., Retchin S.M. 2013. “The Effects of Expanding Primary Care Access for the Uninsured: Implications for the Health Care Workforce Under Health Reform.” Academic Medicine: Journal of the Association of American Medical Colleges 88(12): 1855–61. 10.1097/ACM.0000000000000032. [DOI] [PubMed] [Google Scholar]
- Emeche U. 2015. “Is a Strategy Focused on Super-Utilizers Equal to the Task of Health Care System Transformation? Yes.” Annals of Family Medicine 13(1): 6–7. 10.1370/afm.1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etheredge L.M. 2014. “Rapid Learning: A Breakthrough Agenda.” Health Affairs (Project Hope) 33(7): 1155–62. 10.1377/hlthaff.2014.0043. [DOI] [PubMed] [Google Scholar]
- Evans R.G., McGrail K.M., Morgan S.G., Barer M.L., Hertzman C. 2010. “APOCALYPSE NO: Population Aging and the Future of Health Care Systems.” Canadian Journal on Aging 20(S1): 160–91. 10.1017/S0714980800015282. [Google Scholar]
- Fortin M., Stewart M., Poitras M.-E., Almirall J., Maddocks H. 2012. “A Systematic Review of Prevalence Studies on Multimorbidity: Toward a More Uniform Methodology.” Annals of Family Medicine 10(2): 142–51. 10.1370/afm.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggerty J.L. 2012. “Ordering the Chaos for Patients with Multimorbidity.” BMJ (Clinical Research Ed.) 345(sep07_1): e5915. 10.1136/bmj.e5915. [DOI] [PubMed] [Google Scholar]
- Haggerty J.L., Reid R.J., Freeman G.K., Starfield B.H., Adair C.E., McKendry R. 2003. “Continuity of Care: A Multidisciplinary Review.” BMJ (Clinical Research Ed.) 327(7425): 1219–21. 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Quality Ontario. 2014. A Primary Care Performance Measurement Framework for Ontario. Toronto, ON: Author. [Google Scholar]
- Hewner S., Seo J.Y., Gothard S.E., Johnson B.J. 2014. “Aligning Population-Based Care Management with Chronic Disease Complexity.” Nursing Outlook 62(4): 250–8. 10.1016/j.outlook.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Higgins A., Veselovskiy G., McKown L. 2013. “Provider Performance Measures in Private and Public Programs: Achieving Meaningful Alignment with Flexibility to Innovate.” Health Affairs 32(8): 1453–61. /10.1377/hlthaff.2013.0007. [DOI] [PubMed] [Google Scholar]
- Hogg W., Rowan M., Russell G., Geneau R., Muldoon L. 2008. “Framework for Primary Care Organizations: The Importance of a Structural Domain.” International Journal for Quality in Health Care 20(5): 308–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchison B., Glazier R. 2013. “Ontario's Primary Care Reforms Have Transformed the Local Care Landscape, but a Plan is Needed for Ongoing Improvement.” Health Affairs (Project Hope) 32(4): 695–703. 10.1377/hlthaff.2012.1087. [DOI] [PubMed] [Google Scholar]
- Hutchison B., Levesque J.-F., Strumpf E., Coyle N. 2011. “Primary Health Care in Canada: Systems in Motion.” The Milbank Quarterly 89: 256–88. 10.1111/j.1468-0009.2011.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (IOM). 2001. Crossing the Quality Chasm: A New Health System for the 21st Century, Committee on Quality Health Care in America. Washington, DC: National Academy Press. [Google Scholar]
- Institute of Medicine (IOM). 2006. Performance Measurement: Accelerating Improvement. Performance Measurement: Accelerating Improvement. Washington, DC: National Academy Press; <www.iom.edu/Reports/2005/Performance-Measurement-Accelerating-Improvement.aspx>. [Google Scholar]
- Ionescu-Ittu R., McCusker J., McCusker A., Vadeboncoeur A.-M., Roberge D., Larouche D. et al. 2007. “Continuity of Primary Care and Emergency Department Utilization Among Elderly People.” Canadian Medical Association Journal 177(11): 1362–68. 10.1503/cmaj.061615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivers N.M., Sales A., Colquhoun H., Michie S., Foy R., Francis J.J., Grimshaw J.M. 2014. “No More ‘Business as Usual' with Audit and Feedback Interventions: Towards an Agenda for a Reinvigorated Intervention.” Implementation Science 9(1): 14. 10.1186/1748-5908-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston S., Hogel M. 2016. “A Decade Lost: Primary Healthcare Performance Reporting Across Canada under the Action Plan for Health System Renewal.” Healthcare Policy 11(4): 95–110. 10.12927/hcpol.2016.24593. [PMC free article] [PubMed] [Google Scholar]
- Koller D., Schön G., Schäfer I., Glaeske G., van den Bussche H., Hansen H. 2014. “Multimorbidity and Long-Term Care Dependency–A Five-Year Follow-Up.” BMC Geriatrics 14: 70. 10.1186/1471-2318-14-70>. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kontopantelis E., Springate D.A., Ashworth M., Webb R.T., Buchan I.E., Doran T. 2015. “Investigating the Relationship Between Quality of Primary Care and Premature Mortality in England: A Spatial Whole-Population Study.” BMJ 350(mar02 1): h904–h904. 10.1136/bmj.h904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kringos D.S., Boerma W.G.W., Hutchinson A., Hutchinson J., Groenewegen P.P. 2010. “The Breadth of Primary Care: A Systematic Literature Review of Its Core Dimensions.” BMC Health Services Research 10(1): 65. 10.1186/1472-6963-10-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kringos D.S., Boerma W., van der Zee J., Groenewegen P. 2013. “Europe's Strong Primary Care Systems Are Linked to Better Population Health but Also to Higher Health Spending.” Health Affairs (Project Hope) 32(4): 686–94. 10.1377/hlthaff.2012.1242. [DOI] [PubMed] [Google Scholar]
- Lane N.E., Maxwell C.J., Gruneir A., Bronskill S.E., Wodchis W.P. 2015. “Absence of a Socioeconomic Gradient in Older Adults' Survival with Multiple Chronic Conditions.” EBioMedicine 2(12): 2094–100. 10.1016/j.ebiom.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac D., Colquhoun H., O'Brien K.K. 2010. “Scoping Studies: Advancing the Methodology.” Implementation Science 5(1): 69. 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lunney J.R., Lynn J., Hogan C. 2002. “Profiles of Older Medicare Decedents.” Journal of the American Geriatrics Society 50: 1108–12. 10.1046/j.1532-5415.2002.50268.x. [DOI] [PubMed] [Google Scholar]
- Lynn J., Straube B.M., Bell K.M., Jencks S.F., Kambic R.T. 2007. “Using Population Segmentation to Provide Better Health Care for All: The ‘Bridges to Health' model.” Milbank Quarterly 85(2): 185–208; discussion 209–212. 10.1111/j.1468-0009.2007.00483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin-Misener R., Valaitis R., Wong S.T., MacDonald M., Meagher-Stewart D., Kaczorowski J. et al. 2012. “A Scoping Literature of Collaboration between Primary Care and Public Health.” Primary Health Care Research and Development 13(4): 327–46. [DOI] [PubMed] [Google Scholar]
- Milani R.V., Lavie C.J. 2014. “Healthcare 2020: Reengineering Healthcare Delivery to Combat Chronic Disease.” The American Journal of Medicine 128(4): 337–43. 10.1016/j.amjmed.2014.10.047. [DOI] [PubMed] [Google Scholar]
- Morgan S., Cunningham C. 2011. “Population Aging and the Determinants of Healthcare Expenditures: The Case of Hospital, Medical and Pharmaceutical Care in British Columbia, 1996 to 2006.” Healthcare Policy 7(1): 68–79. 10.12927/hcpol.2011.22525. [PMC free article] [PubMed] [Google Scholar]
- Mukhi S., Barnsley J., Deber R.D. 2014. “Accountability and Primary Healthcare.” Healthcare Policy 10(SP): 90–98. 10.12927/hcpol.2014.23849. [PMC free article] [PubMed] [Google Scholar]
- Newton W.P., Lefebvre A. 2015. “Is a Strategy Focused on Super-Utilizers Equal to the Task of Health Care System Transformation?” Annals of Internal Medicine 13(1): 8–9. 10.1370/afm.1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver K., Innvar S., Lorenc T., Woodman J., Thomas J. 2014. “A Systematic Review of Barriers to and Facilitators of the Use of Evidence by Policymakers.” BMC Health Services Research 14(1): 2. 10.1186/1472-6963-14-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panzer R.J., Gitomer R.S., Greene W.H., Webster P.R., Landry K.R., Riccobono C.A. 2013. “Increasing Demands for Quality Measurement.” JAMA 310(18): 1971–80. 10.1001/jama.2013.282047. [DOI] [PubMed] [Google Scholar]
- Porter M. 2010. “What Is Value in Health Care?” New England Journal of Medicine 363: 2477–81. 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- Porter M.E., Pabo E.A., Lee T.H. 2013. “Redesigning Primary Care: A Strategic Vision to Improve Value by Organizing Around Patients' Needs.” Health Affairs (Project Hope) 32(3): 516–25. 10.1377/hlthaff.2012.0961. [DOI] [PubMed] [Google Scholar]
- Ricci-Cabello I., Stevens S., Kontopantelis E., Dalton A.R.H., Griffiths R.I., Campbell J.L. et al. 2015. “Impact of the Prevalence of Concordant and Discordant Conditions on the Quality of Diabetes Care in Family Practices in England.” The Annals of Family Medicine 13(6): 514–22. 10.1370/afm.1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell G. 2015. “Does Paying for Performance in Primary Care Save Lives?” BMJ (Clinical Research Ed.) 350: h1051. 10.1136/bmj.h1051. [DOI] [PubMed] [Google Scholar]
- Schoen C., Osborn R., Doty M.M., Squires D., Peugh J., Applebaum S. 2009. “A Survey of Primary Care Physicians in Eleven Countries, 2009: Perspectives on Care, Costs, and Experiences.” Health Affairs (Project Hope) 28(6): w1171–83. 10.1377/hlthaff.28.6.w1171. [DOI] [PubMed] [Google Scholar]
- Senn N., Breton M., Ebert S., Levesque J.-F. 2014. “Comparative Analysis of Primary Care Organizational Frameworks.” in North American Primary Care Research Group Conference New York, NY. [Google Scholar]
- Smith P.C., Mossialos E., Papanicolas I., Leatherman S. 2009. “Performance Measurement for Health System Improvement: Experiences, Challenges and Prospects.” in Peter S.L., Smith C., Mossialos E., Papanicolas I., (Ed.), The Cambridge Health Economics, Policy and Management Series. Cambridge: Cambridge University Press; <www.euro.who.int/en/about-us/partners/observatory/publications/studies/performance-measurement-for-health-system-improvement-experiences,-challenges-and-prospects>. [Google Scholar]
- Stange K.C., Etz R.S., Gullett H., Sweeney S.A., Miller W.L., Jaén C.R. et al. 2014. “Metrics for Assessing Improvements in Primary Health Care.” Annual Review of Public Health 35: 423–42. 10.1146/annurev-publhealth-032013-182438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield B. 1998. Primary Care: Balancing Health Needs, Services, and Technology. New York, NY: Oxford University Press. [Google Scholar]
- Starfield B., Shi L., Macinko J. 2005. “Contribution of Primary Care to Health Systems and Health.” Milbank Quarterly 83(3): 457–502. 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Commonwealth Fund. 2014. International Profiles of Health Care Systems: Australia, Canada, Denmark, England, France, Germany, Italy, Japan, The Netherlands, New Zealand, Norway, Singapore, Sweden, Switzerland, and the United States – The Commonwealth Fund. Retrieved February 17, 2016. <www.commonwealthfund.org/publications/fund-reports/2015/jan/international-profiles-2014>.
- The Health Foundation. 2015. Indicators of Quality of Care in General Practices in England. Retrieved October 19, 2016. <www.health.org.uk/publication/indicators-quality-care-general-practices-england>.
- Thorpe K.E. 2005. “The Rise in Health Care Spending and What to Do About It.” Health Affairs (Project Hope) 24(6): 1436–45. 10.1377/hlthaff.24.6.1436. [DOI] [PubMed] [Google Scholar]
- Venkatesh A., Goodrich K., Conway P.H. 2014. “Opportunities for Quality Measurement to Improve the Value of Care for Patients with Multiple Chronic Conditions.” Annals of Internal Medicine 161(10 Suppl.): S76–80. 10.7326/M13-3014. [DOI] [PubMed] [Google Scholar]
- Vogel L. 2015. “Provinces Optimistic for Health Accord Talks.” Canadian Medical Association Journal 188(2): E27–E28. 10.1503/cmaj.109-5206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuik S.I., Mayer E.K., Darzi A. 2016. “Patient Segmentation Analysis Offers Significant Benefits for Integrated Care and Support.” Health Affairs 35(5): 769–75. 10.1377/hlthaff.2015.1311. [DOI] [PubMed] [Google Scholar]
- Watson D.E., Broemeling A.M., Reid R.J., Black C. 2004. A Results-Based Logic Model for Primary Health Care: Laying an Evidence-Based Foundation to Guide Performance Measurement, Monitoring, and Evaluation. Vancouver, BC: Centre for Health Services and Policy Research. [Google Scholar]
- Zhou Y.Y., Wong W., Li H. 2014. “Improving Care for Older Adults: A Model to Segment the Senior.” The Permanente Journal 18(3): 18–21. [DOI] [PMC free article] [PubMed] [Google Scholar]


