Abstract
Background:
Nursing home (NH) residents are frequently transferred to the emergency department (ED) but there is little data on inter-facility variation, which has implications for intervention planning and implementation.
Objectives:
To describe variation in ED transfer rates (TRs) across NHs and the association with NH characteristics.
Design/setting:
Retrospective cohort study using linked administrative data from Ontario.
Participants:
71,780 residents of 604 NHs in 2010 and followed for one year.
Measurements:
Funnel plots were used to identify high transfer NHs and logistic regression to test the association with NH location, size, ownership and historical ED transfer rate.
Results:
One-year ED transfer rates ranged from 4.3% to 58.6% (mean 28.4%); 115 (19%) NHs were considered high. Being within five minutes of an ED, larger size and high historical ED transfer rate were associated with being a high ED transfer home.
Conclusion:
There was substantial variation across NHs. Consideration of characteristics such as proximity to an ED may be important in the development and targeting of different interventions for NHs.
Abstract
Contexte:
Les patients des foyers de soins infirmiers (FSI) sont souvent transférés aux services des urgences (SU), mais il existe peu de données sur les variations entre les établissements, ce qui entraîne des conséquences en matière de planification et de mise en place d'interventions.
Objectifs:
Décrire les variations dans le taux de transfert des FSI vers les SU, relativement aux caractéristiques des FSI.
Méthode:
Étude de cohorte rétrospective utilisant des données administratives de l'Ontario.
Participants:
71 780 patients suivis pendant une année, en 2010, provenant de 604 FSI.
Mesures:
Des diagrammes en entonnoir ont été utilisés pour déterminer les transferts élevés des FSI et des analyses de régression logistique ont été utilisées pour établir des liens avec l'emplacement et l'importance du FSI, les propriétaires de l'établissement et l'historique des taux de transfert vers les SU.
Résultats:
Le taux de transfert vers les SU, par an, se situe entre 4,3 % et 58,6 % (une moyenne de 28,4 %); le taux de transfert de 115 (19 %) des FSI était considéré comme élevé. Pour les FSI à moins de cinq minutes d'un SU, de grande importance et avec un taux de transfert historique élevé, ces FSI sont associés à un taux de transfert élevé.
Conclusion:
Il y a des variations majeures parmi les FSI. Considérer des caractéristiques telles que la proximité d'un SU peut être important afin de cibler et de développer les diverses interventions nécessaires pour les FSI.
Introduction
Emergency departments (EDs) are an important site of care for nursing home (NH) residents but the high rate of transfer has raised concerns about the provision of care in NHs. Few studies to date have examined variation across NHs in their ED transfer rates (TRs) or the extent to which this is associated with NH-level characteristics. Since the decision to transfer residents is made within the NH, through a combination of internal policies, resident and family preferences and documented care orders, variation in ED TRs may be a more direct measure of the influence of the NH than inpatient hospitalizations, which have been well-studied but are also a function of decision-making within the ED. Our previous research found that approximately 50% of residents who visited the ED were discharged back to the NH without hospitalization (Gruneir et al. 2010). Those findings illustrate that studying inpatient hospitalizations alone provide only partial information about acute care use by this population, while a broader focus on ED transfers more fully captures the transitions between the two sectors.
Without data on the extent to which ED transfers vary across NHs, it is difficult to know if current high rates result from sector-wide problems or from issues within specific NHs or specific types of NHs. This has implications for quality improvement implementation. Interventions to improve care for specific medical problems have been shown to reduce transfers without increasing the frequency of other adverse events (Loeb et al. 2006; McAiney et al. 2008) but they face barriers, including resource-intensity, to wider implementation. Facility-specific rates would allow for improved targeting of limited resources.
Given the paucity of data on variation in ED transfers across NHs, our intention is to provide population-based estimates to lay the groundwork for further study and intervention development. The objectives of this study are to quantify the extent of variation in ED TRs across NHs in Ontario, Canada, and to test the association of selected NH characteristics with observed variation in ED TRs.
Methods
This study was conducted in Ontario, Canada. In Ontario, NHs specifically refer to residential care settings intended for adults (aged ≥18 years) requiring round-the-clock nursing and/or support services and/or cannot live safely in a community setting; they typically do not provide post-acute services. There are three types of homes based on ownership: for-profit, non-profit and municipal. Both for-profit and non-profit homes are privately owned. Each municipality is required to maintain a certain number of NH beds, which operate in a non-profit manner. Regardless of ownership, all homes receive comparable per resident-day reimbursement from the provincial health insurance plan and are subject to the same restrictions on private fees for basic room-and-board reimbursement (McGrail et al. 2007; McGregor et al. 2005).
Data
This study was conducted using administrative data that were linked by unique, encoded identifiers and analyzed at the Institute for Clinical Evaluative Sciences (ICES) in Toronto, Ontario. Baseline resident data were obtained from the Resident Assessment Instrument Minimum Data Set version 2.0 (RAI-MDS 2.0), a comprehensive clinical assessment tool (Hirdes et al. 2003; Morris et al. 1994, 1999) mandated for use in Ontario. Assessments are completed at admission, three-month intervals and following major health changes. The RAI-MDS 2.0 is regularly used for research (Hawes et al. 1995). Information on ED transfers was obtained from the National Ambulatory Care Reporting System, a mandatory reporting requirement for all ED encounters in Ontario (CIHI 2007). Other administrative sources include the Registered Persons Database (RPDB) for demographics and the Occupancy Monitoring Database (OCCM) for NH descriptors. These data are regularly used for research and have been studied for their validity (Bronskill et al. 2004; Chan et al. 2001; Hux et al. 2002; Schull et al. 2007). The Research Ethics Board at Sunnybrook Health Sciences Centre reviewed this study.
Cohort
The cohort consists of all individuals 65 years and older who resided in an Ontario NH between January 1 and March 31, 2010. We excluded 23 NHs with fewer than 25 beds to reduce the likelihood of statistically unstable estimates (Intrator et al. 1999). Each resident was followed from baseline (the first assessment in the quarter) for one year until the first discharge from the NH, death or end of the 365-day follow-up period.
We described the cohort by demographics, diagnoses and functional ability. We used the MDS-embedded Cognitive Performance Scale (CPS) (Morris et al. 1994), Activities of Daily Living (ADL) Short Form Scale (Morris et al. 1994) and Changes in Health, End-Stage Disease, Signs and Symptoms (CHESS) Scale (Hirdes et al. 2003) to measure cognitive impairment, physical impairment and medical instability, respectively. All measures were obtained from the baseline RAI-MDS 2.0 assessment since some of our other work found limited changes in these measures over such a short follow-up period. We used only the first ED transfer after baseline since the incorporation of recurrent events was beyond the scope of this study.
We focused on four NH characteristics as available in our data: location, size, ownership and historical ED TR. Location was operationalized using two metrics. The first was urban versus rural setting based on community size. NHs in urban areas have better outcomes than those in rural areas, and it is thought that this may result from greater access to services (Temkin-Greener et al. 2012). The second metric was estimated travel time in minutes between the NH and the closest ED using ArcGIS 10 (ESRI) to map distances by postal code and posted speed limits on existing roadways. Based on preliminary analyses, travel time was dichotomized as <5 minutes or ≥5 minutes.
Facility size was based on the number of beds, dichotomized as <100 or ≥100 beds to be consistent with other studies (Zinn et al. 2007). Larger homes are thought to provide medical services more efficiently than smaller homes, resulting in lower hospitalization rates and better performance on other measures (Intrator et al. 1999, 2004). NH ownership was identified as one of for-profit, non-profit or municipal. Ownership type, most often measured as profit-status, has been well-studied with most research demonstrating better outcomes in non-profit homes (Hillmer et al. 2005; McGregor et al. 2006).
Lastly, we considered each NH's historical ED TR to assess the extent to which homes consistently have higher versus lower TRs over time. We estimated the three-month ED TR for each NH using residents identified between October 1 and December 31, 2009. We dichotomized this variable at the distribution mean (13%) based on preliminary analyses and because it was not normally distributed. We included historical ED TR as a means to test whether observed variation was random or persisted over time.
Analysis
The proportion of residents who experienced at least one ED transfer was estimated for each NH. We constructed a funnel plot to display variation in rates of ED transfer across NHs. The funnel plot was created by estimating a standardized transfer ratio for each NH (STRNH) that was plotted against the total number of residents in the NH. The STRNH is a ratio of the observed to the expected proportion of residents in the NH with an ED transfer. The provincial ED transfer rate was set as the expected value because no benchmark exists. The threshold of comparison was an STRNH of 1, meaning the observed and expected proportions are equal. We estimated 95% control bounds using binomial limits to characterize the degree of variation across NHs (Spiegelhalter 2005). The funnel plot allows for visual display of variation relative to pre-defined control bounds, so that deviation from the expected distribution can be easily observed (Rochon et al. 2007).
We divided NHs into three groups according to their position on the funnel plot. NHs were designated as having a high TR if they fell above the upper 95% control bound, an intermediate TR if they fell between the upper and lower 95% control bounds, and a low TR if they fell below the lower 95% control bound. Our intention was solely to describe NHs as high, intermediate or low relative to the provincial average – not that we anticipated that every NH in our study should have an expected ED TR equivalent to the provincial average.
We used logistic regression to estimate the association between each NH characteristic and the likelihood of being a high ED transfer facility relative to being an intermediate/low transfer facility. We collapsed the intermediate and low ED transfer facilities into a single category in order to be consistent with our original research objectives; this a priori decision was supported by interim analyses that included comparisons across the ED transfer groups on the NH characteristics and resident case-mix variables. We used a three-step process to develop our final model. First, we separately modelled each NH characteristic against the dichotomous outcome to determine “crude” estimates of association. Second, we simultaneously modelled all NH characteristics in a single model to assess for any changes in the odds ratio (OR) and collinearity. Third, we sequentially added select case-mix variables to the model described in Step 2 as a means to test for the presence of confounding. Based on observed changes to the ORs on the NH characteristics of interest, our final adjusted model controlled for the following: the proportion of residents in the NH with severe cognitive impairment, the proportion of residents in the NH with behavioural problems and the proportion in the NH with unstable medical conditions (CHESS >4). None of the other case-mix variables influenced the measures of association. We selected this approach, as opposed to a multilevel model, because our main interest was in characterizing NHs with high ED TRs as opposed to identifying resident risk factors for transfer. All analyses were conducted using SAS versions 9.2 and 9.3.
Results
We identified 71,780 residents in 604 NHs. Table 1 shows facility-level baseline characteristics for the full cohort as well as stratified by ED TR grouping. Across NHs, the mean age was 84.4 (SD = 1.7) years and the mean proportion of females was 71.9% (SD = 7.9) with little variation across facility groupings. The majority of residents in all NH groups had a length of stay of one year or more. There was a high burden of cognitive impairment, physical impairment and difficult behaviours with limited observable differences across NH types.
Table 1.
Facility-level distribution of resident baseline characteristics for full cohort of NHs and stratified by relative ED transfer rate (71,780 residents at baseline)
| All NHs in cohort N = 604 | “High” transfer NHs n = 115 | “Intermediate” transfer NHs n = 359 | “Low” transfer NHs n = 130 | |
|---|---|---|---|---|
| Facility average age, mean (SD)* | 84.8 (1.7) | 84.2 (1.9) | 84.8 (1.6) | 85.1 (1.5) |
| Age groups, mean proportion (SD)§ | ||||
| 65-74 years | 10.6% (5.5%) | 12.1% (6.3%) | 10.3% (5.4%) | 9.8% (4.7%) |
| 75-84 years | 34.1% (6.5%) | 35.7% (6.4%) | 34.1% (6.5%) | 32.7% (6.1%) |
| 85-94 years | 46.2% (8.0%) | 43.7% (8.4%) | 46.4% (8.0%) | 48.0% (7.2%) |
| 95+ years | 9.1% (4.0%) | 8.4% (3.9%) | 9.2% (3.8%) | 9.5% (4.3%) |
| Women, mean proportion (SD) | 71.9% (7.9%) | 70.3% (7.6%) | 71.9% (8.1%) | 73.3% (7.4%) |
| Length of stay, mean proportion (SD) | ||||
| <30 days | 9.7% (6.2%) | 10.5% (9.4%) | 9.4% (5.2%) | 9.9% (5.3%) |
| 30-89 days | 1.6% (2.0%) | 1.6% (1.9%) | 1.6% (2.2%) | 1.4% (1.9%) |
| 90-364 days | 23.4% (6.7%) | 22.8% (7.0%) | 24.0% (7.0%) | 22.3% (5.5%) |
| 365 days or more | 65.3% (9.4%) | 65.1% (9.8%) | 65.0% (9.6%) | 66.4% (8.1%) |
| Cognitive performance scale score groups, mean proportion (SD) | ||||
| 0-2 (none to minimal) | 42.0% (10.9%) | 44.8% (11.0%) | 41.4% (10.6%) | 41.1% (11.3%) |
| 3-4 (moderate) | 34.3% (9.3%) | 32.0% (8.5%) | 34.6% (9.3%) | 35.6% (9.5%) |
| 5-6 (severe) | 23.7% (9.3%) | 23.2% (8.9%) | 24.0% (9.5%) | 23.3% (9.0%) |
| Facility average cognitive performance scale score, mean (SD) | 2.8 (0.4) | 2.7 (0.5) | 2.8 (0.4) | 2.8 (0.4) |
| Activities of daily living short-form scale groups, mean proportion (SD) | ||||
| 0-1 (minimal) | 14.7% (7.7%) | 16.0% (8.0%) | 14.7% (7.8%) | 13.4% (7.0%) |
| 2-3 (moderate) | 37.6% (8.8%) | 37.1% (8.1%) | 37.5% (8.7%) | 38.2% (9.5%) |
| 4-5 (dependent) | 47.8% (10.3%) | 46.9% (10.5%) | 47.8% (10.3%) | 48.5% (10.4%) |
| Facility average ADL short-form scale mean (SD) | 3.5 (0.4) | 3.4 (0.4) | 3.5 (0.4) | 3.5 (0.4) |
| Problem behaviours, mean proportion (SD) | ||||
| Inappropriate | 18.4% (10.1%) | 15.8% (8.6%) | 18.1% (9.4%) | 21.5% (12.2%) |
| Verbally abusive | 19.3% (7.9%) | 18.8% (7.9%) | 19.2% (7.9%) | 19.8% (7.8%) |
| Physically abusive | 12.1% (5.7%) | 10.9% (4.7%) | 12.2% (6.1%) | 13.0% (5.6%) |
| Wandering | 17.2% (7.2%) | 15.9% (6.8%) | 17.3% (7.2%) | 18.2% (7.4%) |
| Resists care | 36.2% (14.0%) | 33.4% (12.3%) | 36.1% (14.1%) | 38.8% (14.6%) |
| CHESS scale score, mean proportion (SD) | ||||
| 0 | 46.9% (14.7%) | 50.9% (14.0%) | 46.9% (14.4%) | 43.3% (15.2%) |
| 1 | 31.7% (7.8%) | 31.0% (7.6%) | 31.6% (7.8%) | 32.5% (7.9%) |
| 2 | 14.8% (7.4%) | 12.9% (6.1%) | 14.9% (7.4%) | 16.1% (8.2%) |
| 3 | 4.5% (3.7%) | 3.6% (2.8%) | 4.5% (3.5%) | 5.5% (4.5%) |
| 4 | 1.7% (1.8%) | 1.4% (1.5%) | 1.6% (1.6%) | 2.1% (2.3%) |
| 5 | 0.4% (0.9%) | 0.2% (0.5%) | 0.4% (0.9%) | 0.5% (1.1%) |
| Facility average CHESS score, mean (SD) | 0.8 (0.3) | 0.7 (0.3) | 0.8 (0.3) | 0.9 (0.4) |
| Major diagnoses - mean proportion (SD) | ||||
| Diabetes mellitus | 24.7% (6.2%) | 26.4% (6.8%) | 24.9% (6.1%) | 22.7% (5.5%) |
| Arteriosclerotic heart disease | 12.9% (10.5%) | 11.9% (10.4%) | 12.9% (10.8%) | 13.6% (10.0%) |
| Cardiac dysrhythmia | 7.0% (5.7%) | 6.0% (4.8%) | 7.2% (6.0%) | 7.4% (5.6%) |
| Congestive heart failure | 12.5% (5.2%) | 11.8% (4.7%) | 12.5% (5.1%) | 13.2% (5.8%) |
| Peripheral vascular disease | 5.3% (3.9%) | 5.5% (3.8%) | 5.2% (3.7%) | 5.4% (4.7%) |
| Arthritis | 39.3% (12.8%) | 35.7% (12.3%) | 39.2% (12.1%) | 42.9% (14.1%) |
| Osteoporosis | 25.7% (10.3%) | 24.4% (8.1%) | 25.3% (9.8%) | 28.1% (12.6%) |
| Alzheimer's disease | 18.6% (9.1%) | 17.0% (8.6%) | 18.8% (9.2%) | 19.7% (8.9%) |
| Dementia (other than Alzheimer's) | 44.1% (11.2%) | 44.3% (11.8%) | 44.2% (11.2%) | 43.6% (11.0%) |
| Stroke (cerebrovascular accident) | 21.5% (6.5%) | 21.8% (6.7%) | 21.5% (6.5%) | 21.2% (6.7%) |
| Parkinson disease | 6.9% (3.0%) | 6.5% (3.0%) | 7.0% (3.1%) | 7.1% (3.0%) |
| Anxiety disorder | 7.8% (5.3%) | 7.1% (5.3%) | 7.7% (5.5%) | 8.6% (4.7%) |
| Depression | 28.5% (11.1%) | 25.7% (9.6%) | 28.2% (10.9%) | 31.6% (12.3%) |
| Emphysema/Chronic obstructive pulmonary disease | 14.8% (6.5%) | 14.4% (6.3%) | 14.8% (6.6%) | 15.1% (6.4%) |
| Cancer | 8.5% (4.9%) | 8.3% (4.7%) | 8.6% (5.0%) | 8.5% (5.1%) |
| Renal failure | 8.1% (6.2%) | 8.1% (6.4%) | 8.1% (6.2%) | 7.9% (5.9%) |
| Accidents, mean proportion (SD) | ||||
| Fell in past 30 days | 13.2% (4.9%) | 12.6% (5.1%) | 13.4% (4.8%) | 13.3% (4.9%) |
| Fell in past 180 days | 25.3% (8.9%) | 24.0% (9.0%) | 25.3% (8.8%) | 26.3% (9.0%) |
| Fracture in past 180 days (hip or other) | 2.8% (2.0%) | 2.5% (1.9%) | 2.9% (2.1%) | 2.6% (2.0%) |
CHESS = Changes in Health, End-Stage Disease, Signs and Symptoms Scale; ED = emergency department; NH = nursing home; SD = standard deviation.
Average means across all facilities in the category.
Average proportion across all facilities in the category.
Over one year, 20,829 (29%) residents were transferred to the ED at least once. The timing of the first ED transfers relative to the baseline assessment was 13.9% within 28 days, 49.7% between 28 and less than 180 days and 36.4% between 180 and 365 days. 12.5% of residents died within 30 days of their first ED transfer (data not shown). The facility-level mean proportion of residents with an ED transfer was 28.4% (SD 10.1) and ranged from 4.3% to 58.6% (interquartile range: 21.6–34.5%). Based on the STRNH, approximately 30 NHs (5%) were expected to each fall above and below the 95% control bounds. As Figure 1 illustrates, 115 (19%) NHs fell above the upper 95% control bound and 130 (21.5%) fell below the lower 95% control bound, suggesting greater variation than expected.
Figure 1.
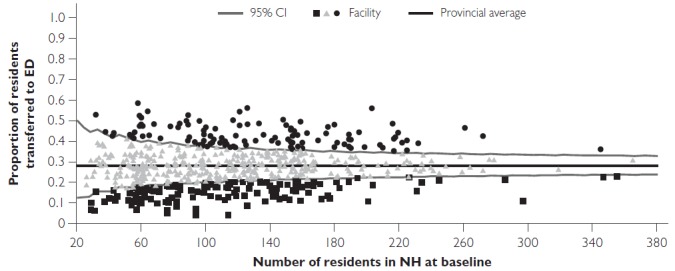
Proportion of nursing home residents in facility with at least 1 ED visit over one year, plotted with funnels approximated using exact binomial limit
CI = confidence interval; ED = emergency department; NH = nursing home.
Differences in the distribution of NH characteristics according to ED TR groupings are shown in Table 2. NHs with high ED TRs were most often urban, within a 5-minute drive of an ED, and larger. There was little difference in ownership, although high TR homes were somewhat less likely to be municipally owned. The mean historical ED TR declined from 18.6 (SD 5.4) in the high TR group to 8.5 (SD 3.5) in the low group (not shown).
Table 2.
Distribution of NH characteristics by ED transfer rate
| NH-specific rates of ED transfer | Association between NH characteristics and high transfer rate NH | ||||
|---|---|---|---|---|---|
| High rate | Intermediate rate | Low rate | Total | ||
| n = 115 | n = 359 | n = 130 | N = 604 | Adjusted OR§ (95% CI) | |
| ED transfer rate range* | 35.5-58.6% | 17.7-41.2% | 4.3-23.1% | 4.3-58.6% | - |
| Location, n (%) | |||||
| Rura | 20 (17.4%) | 111 (30.9%) | 35 (26.9%) | 166 (27.5%) | Reference |
| Urbar | 95 (82.6%) | 248 (69.1%) | 95 (73.1%) | 438 (72.5%) | 1.41 (0.76, 2.61) |
| ≥5 minutes to closest ED | 37 (31.6%) | 171 (47.3%) | 60 (46.2%) | 268 (44.1%) | Reference |
| <5 minutes to closest ED | 78 (68.4%) | 188 (52.7%) | 70 (53.8%) | 336 (55.9%) | 1.77 (1.09, 2.86) |
| Size, n (%) | |||||
| <100 beds | 28 (24.4%) | 161 (44.8%) | 56 (43.1%) | 245 (40.6%) | Reference |
| ≥100 beds | 87 (75.6%) | 198 (55.2%) | 74 (56.9%) | 359 (59.4%) | 1.91 (1.13, 3.23) |
| Ownership,¶ n (%) | |||||
| Municipal | 14 (12.3%) | 61 (17.2%) | 27 (20.9%) | 102 (17.1%) | Reference |
| Non-profit | 27 (23.7%) | 80 (22.5%) | 36 (27.9%) | 143 (23.9%) | 1.64 (0.76, 3.56) |
| For-profit | 73 (64.0%) | 214 (60.3%) | 66 (51.2%) | 353 (59.0%) | 1.57 (0.79, 3.12) |
| Historical transfer rate, n (%) | |||||
| <13% | 96 (84.2%) | 183 (51.0%) | 12 (9.2%) | 291 (48.3%) | Reference |
| ≥ 13% | 19 (15.8%) | 176 (49%) | 118 (90.8%) | 313 (51.7%) | 7.03 (4.04, 12.24) |
CI = confidence intervals; ED = emergency department; NH = nursing homes; OR = odds ratio.
Transfer rates overlap owing to funnel shape of control bounds.
All NH factors modelled simultaneously and adjusted for NH case-mix variables (proportion of residents with each behavioural problems, cognitive impairment and high levels of instability).
Not available for all NHs.
For all NH characteristics, except ownership, there was some attenuation of the OR in the simultaneous model relative to the independent models but little additional change following case-mix adjustment (results of the fully adjusted model only are shown in Table 2). Being within a 5-minute drive of an ED (OR 1.8, 95% CI: [1.1, 2.9]) and large size (OR 1.9, 95% CI: [1.1, 3.2]) were both associated with a high ED TR. Historical ED TR demonstrated the strongest association (OR 7.0, 95% CI: [4.0, 12.2]). Urban location showed an association with high ED TR in the independent model but this did not persist after adding distance. Ownership type was not associated with ED TR.
Discussion
We found that almost one-third of NH residents were transferred to the ED at least once over one year but that this varied 13-fold across homes. Nearly 20% of all NHs were identified as having high rates of ED transfer – substantially more than the expected 5%. We further found that high ED TR was associated with home characteristics even after controlling for case-mix.
Research on antipsychotics, physical restraints, feeding tubes and hospitalizations has shown that facility-level variation across NH is a complex issue with multiple and multi-layered inputs. Our results suggest that the same is true for ED transfers. Building on our previous work, we found that proximity to an ED was associated with a high ED TR, independent of urban–rural setting, which itself was not predictive. Our preliminary analyses did show that NHs within close proximity of an ED were more likely to be in urban settings, but not exclusively so, suggesting that physical proximity and urban-rural setting are related, yet different, issues. Although research on other quality metrics has generally found better outcomes among urban NHs, the relationship with hospitalization has been less clear and there is little research looking specifically at ED transfers (Gessert et al. 2006; Kang et al. 2011; Phillips et al. 2004). Research from non-NH populations shows that proximity is associated with ED use and hospitalizations (Goodman et al. 1997; Ludwick et al. 2009). Our findings suggest that ease of access may be an important driver of ED transfer but whether it contributes to higher levels of “inappropriate” use remains unclear.
We also found that larger homes were more likely to have high ED TRs. This is contradictory to other evidence, which has shown better performance among larger homes (Intrator et al. 1999, 2004; Mor et al. 2011). Our preliminary analyses found that larger homes were more likely to be in urban areas and have a higher historical ED TR. It may be that larger NHs are more likely to share other characteristics, such as more stringent policies around ED transfers, that we were unable to measure here.
Although the point estimates on for-profit and non-profit nursing homes indicated higher odds of being a high ED TR home relative to municipal facilities, the confidence intervals were wide and crossed 1.0, indicating no significant association. Research from British Columbia, another Canadian province, found the impact of profit-status was modified by other aspects of ownership; specifically, only certain types of non-profit NHs, including those amalgamated to a health authority, had lower hospitalization rates than for-profit homes, and that there was no difference between single-site non-profit and for-profit homes (McGregor et al. 2006). In Ontario, all NHs are subject to the same provincial legislation on reimbursement, private fees and spending allocations, which may explain why we did not observe differences by profit status.
Even after controlling for case-mix, NHs with a higher historical TR had sevenfold greater odds of being in the high ED transfer group than those homes with lower historical rates. This likely represents the influence of time-invariant factors that we were unable to examine. For example, we lacked data on staffing, which is likely both invariant over the period studied and associated with ED TRs. It also likely reflects an NH's underlying culture, which is typically difficult to operationalize in studies such as ours. Others have shown that homes do exhibit an internal set of shared values that can have important implications for care practices. For example, a recent study of hospital transfers found that staff perceptions of what constituted “avoidable” varied greatly across homes even when similar reasons for transfer were identified (Lamb et al. 2011).
Safe reductions in ED TRs will likely require a multi-pronged approach that addresses issues with the resident and family, care providers, NH practice and the local environment. Finding such stark variation in facility TRs suggests that different NHs will likely require different strategies to improve outcomes. While this study does not elucidate how such interventions should be targeted, it does identify issues for future research. For example, our findings on location suggest that a more nuanced approach than urban–rural dichotomy may be more appropriate for studying regional effects. As well, there is a need for data on staff perceptions of the role of the ED in resident care and the extent to which it varies across NHs. This type of data opens up opportunities for discussion with high and low TR NHs on their perceptions of contributing factors and practices.
Limitations
There are limitations to this study. There are a number of NH characteristics that we could not measure such as staffing. Evidence from Ontario suggests that there is limited variation in nurse staffing; however, this and other staff types cannot be ruled out as important factors. Other NH characteristics that we could not consider include engagement in quality improvement, cultural affiliation and access to medical consultants. Resident and family insistence for ED transfer are frequently cited as a significant factor but there is little data on how these preferences vary across NHs. The historical ED TR was based on the quarter prior to study baseline because the RAI-MDS was not fully implemented in Ontario until 2009. Future work would benefit from a longer time span on ED transfer trends. Finally, we excluded very small NHs which were likely concentrated in rural areas; however, given the small number (n = 23; 3.7% of all NHs) we do not anticipate that this had any influence on our findings.
Conclusion
We observed 13-fold variation in ED TRs across Ontario NHs, and that far more NHs than expected were identified as having high TRs. There is no standard “appropriate” rate of ED transfer, but the rates reported here appear high and the wide variation suggests that there are opportunities to reduce them. While our findings suggest that certain types of NHs could benefit from intervention, they also demonstrate the need for a comprehensive approach to understanding the impact of location, facility structure and other characteristics, such as staffing and culture, on transfer decisions and related outcomes.
Acknowledgements
The authors would like to thank Dilzayn Panjwani, MSc at the Women's College Research Institute for her assistance in preparing the manuscript. This work was supported by the Canadian Institutes of Health Research (CIHR); Institute of Health Services and Policy Research [grant number MOP 89943]; CIHR Institute of Nutrition, Metabolism, and Diabetes [grant number OTG-88591] to [AG]; and the CIHR New Investigator Award to [AG]. There are no conflicts of interest to declare.
Contributor Information
Andrea Gruneir, Assistant Professor, Department of Family Medicine, University of Alberta, Edmonton, AB.
Susan E. Bronskill, Scientist, Institute for Clinical Evaluative Sciences, Toronto, ON.
Alice Newman, Analyst, Institute for Clinical Evaluative Sciences, Toronto, ON.
Chaim M. Bell, Professor, Department of Medicine, Mount Sinai Hospital/University of Toronto, Toronto, ON.
Peter Gozdyra, Medical Geographer, Institute for Clinical Evaluative Sciences, Toronto, ON.
Geoffrey M. Anderson, Professor, Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON.
Paula A. Rochon, Senior Scientist, Women's College Research Institute, Women's College Hospital, Toronto, ON.
References
- Bronskill S.E., Anderson G.M., Sykora K., Wodchis W.P., Gill S., Shulman K.I., Rochon P.A. 2004. “Neuroleptic Drug Therapy in Older Adults Newly Admitted to Nursing Homes: Incidence, Dose, and Specialist Contact.” Journal of the American Geriatrics Society 52: 749–55. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI). 2007. NACRS Background and General Data Limitations Documentation 2006–2007. Ottawa, ON: CIHI. [Google Scholar]
- Chan B.T.B., Schull M.J., Schultz S.E. 2001. Emergency Department Services in Ontario 1993–2000. Toronto, ON: Institute of Clinical Evaluative Sciences. [Google Scholar]
- Gessert C.E., Elliott B.A., Peden-McAlpine C. 2006. “Family Decision-Making for Nursing Home Residents with Dementia: Rural–Urban Differences.” Journal of Rural Health 22(1): 1–8. [DOI] [PubMed] [Google Scholar]
- Goodman D.C., Fisher E., Stukel T.A., Chang C. 1997. “The Distance to Community Medical Care and the Likelihood of Hospitalization: Is Closer Always Better?” American Journal of Public Health 87(7): 1144–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruneir A., Bell C.M., Bronskill S.E., Schull M., Anderson G.M., Rochon P.A. 2010. “Frequency and Pattern of Emergency Department Visits by Long-Term Care Residents – A Population-Based Study.” Journal of the American Geriatrics Society 58(3): 510–17. [DOI] [PubMed] [Google Scholar]
- Hawes C., Morris J.N., Phillips C.D., Mor V., Fries B.E., Nonemaker S. 1995. “Reliability Estimates for the Minimum Data Set for Nursing Home Resident Assessment and Care Screening (MDS).” Gerontologist 35(2): 172–78. [DOI] [PubMed] [Google Scholar]
- Hillmer M.P., Wodchis W.P., Gill S.S, Anderson G.M., Rochon P.A. 2005. “Nursing Home Profit Status and Quality of Care: Is There Any Evidence of an Association?” Medical Care Research and Review 62(2): 139–66. [DOI] [PubMed] [Google Scholar]
- Hirdes J.P., Frijters D.H., Teare G.F. 2003. “The MDS-CHESS Scale: A New Measure to Predict Mortality in Institutionalized Older People.” Journal of the American Geriatrics Society 51(1): 96–100. [DOI] [PubMed] [Google Scholar]
- Hux J.E., Ivis F., Flintoft V., Bica A. 2002. “Diabetes in Ontario: Determination of Prevalence and Incidence Using a Validated Administrative Data Algorithm.” Diabetes Care 25 (3): 512–16. [DOI] [PubMed] [Google Scholar]
- Intrator O., Castle N.G., Mor V. 1999. “Facility Characteristics Associated with Hospitalization of Nursing Home Residents: Results of a National Study.” Medical Care 37(3): 228–37. [DOI] [PubMed] [Google Scholar]
- Intrator O., Zinn J., Mor V. 2004. “Nursing Home Characteristics and Potentially Preventable Hospitalizations of Long-Stay Residents.” Journal of the American Geriatrics Society 52(10): 1730–36. [DOI] [PubMed] [Google Scholar]
- Kang Y., Meng H., Miller N.A. 2011. “Rurality and Nursing Home Quality: Evidence from the 2004 National Nursing Home Survey.” Gerontologist 51(6): 761–73. [DOI] [PubMed] [Google Scholar]
- Lamb G., Tappen R., Diaz S., Herndon L., Ouslander J.G. 2011. “Avoidability of Hospital Transfers of Nursing Home Residents: Perspectives of Frontline Staff.” Journal of the American Geriatrics Society 59: 1665–72. [DOI] [PubMed] [Google Scholar]
- Loeb M., Carusone S.C., Goeree R., Walter S.D., Brazil K., Krueger P. et al. 2006. “Effect of a Clinical Pathway to Reduce Hospitalizations in Nursing Home Residents with Pneumonia: A Randomized Controlled Trial.” Journal of the American Medical Association 295(21): 2503–10. [DOI] [PubMed] [Google Scholar]
- Ludwick A., Fu R., Warden C., Lowe R.A. 2009. “Distances to Emergency Department and to Primary Care provider's Office Affect Emergency Department Use in Children.” Academic Emergency Medicine 16: 411–17. [DOI] [PubMed] [Google Scholar]
- McAiney C.A., Haughton D., Jennings J., Farr D., Hillier L., Morden P. 2008. “A Unique Practice Model for Nurse Practitioners in Long-Term Care Homes.” Journal of Advanced Nursing 62(5): 562–71. [DOI] [PubMed] [Google Scholar]
- McGrail K.M., McGregor M.J., Cohen M., Tate R.B., Ronald L.A. 2007. “For-Profit Versus Not-For- Profit Delivery of Long-Term Care.” Canadian Medical Association Journal 176(1): 57–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor M.J., Cohen M., McGrail K., Broemeling A.M., Adler R.N., Schulzer M. et al. 2005. “Staffing Levels in Not-For-Profit and For-Profit Long-Term Care Facilities: Does Type of Ownership Matter?” Canadian Medical Association Journal 172(5): 645–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor M.J., Tate R.B., McGrail K.M., Ronald L.A., Broemeling A.M., Cohen M. 2006. “Care Outcomes in Long-Term Care Facilities in British Columbia, Canada. Does Ownership Matter?” Medical Care 44(10): 929–35. [DOI] [PubMed] [Google Scholar]
- Mor V., Gruneir A., Feng Z., Grabowski D.C., Intrator O., Zinn J. 2011. “The Effect of State Policies on Nursing Home Resident outcomes.” Journal of the American Geriatrics Society 59(1): 3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J.N., Fries B.E., Mehr D.R., Hawes C., Phillips C.D., Mor V. et al. 1994. “MDS Cognitive Performance Scale.” The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 49(4): M174–M82. [DOI] [PubMed] [Google Scholar]
- Morris J.C., Fries B.E., Morris S.A. 1999. “Scaling ADLs Within the MDS.” The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 54A: M546–M53. [DOI] [PubMed] [Google Scholar]
- Phillips C.D., Holan S., Sherman M., Williams M.L., Hawes C. 2004. “Rurality and Nursing Home Quality: Results from a National Sample of Nursing Home Admissions.” American Journal of Public Health 94: 1717–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochon P.A., Stukel T.A., Bronskill S.E., Gomes T., Sykora K., Wodchis W.P. et al. 2007. “Variation in Nursing Home Antipsychotic Prescribing Rates.” Archives of Internal Medicine 167: 676–83. [DOI] [PubMed] [Google Scholar]
- Schull M.J., Kiss A., Szalai J.P. 2007. “The Effect of Low-Complexity Patients on Emergency Department Waiting Times.” Annals of Emergency Medicine 49: 257–64, 64 e1. [DOI] [PubMed] [Google Scholar]
- Spiegelhalter D.J. 2005. “Funnel Plots for Comparing Institutional Performance.” Statistics in Medicine 24: 1185–202. [DOI] [PubMed] [Google Scholar]
- Temkin-Greener H., Zheng N.T., Mukamel D.B. 2012. “Rural–Urban Differences in End-of-Life Nursing Home Care: Facility and Environmental Factors.” Gerontologist 52(3): 335–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinn J.S., Mor V., Feng Z., Intrator O. 2007. “Doing Better to do Good: The Impact of Strategic Adaptation on Nursing Home Performance.” Health Services Research Journal 42: 1200–18. [DOI] [PMC free article] [PubMed] [Google Scholar]


