Abstract
We conducted this study to clarify the current trends and healthcare resource usage in the treatment of inpatients with primary malignant brain tumors. The Diagnostic Procedure Combination (DPC) data of all inpatients treated between 2013 and 2014 in the 370 core and branch hospitals enrolled in the Japanese Neurosurgical Society training program were collected. DPC is a discharge abstract and administrative claims database of inpatients. We assessed 6,142 primary, malignant brain tumor patients. Patient information, diagnostic information, treatment procedure, and healthcare resource usage were analyzed. Chemotherapy was the most frequent treatment (27% of cases), followed by surgery (13%) and surgery + chemo-radiotherapy (11%). Temozolomide (TMZ), the most frequently used chemotherapeutic drug, was administered to 1,236 patients. Concomitant TMZ and radiotherapy was administered to 816 patients, and was performed according to the Stupp regimen in many cases. The mean length of hospital stay (LOS) was 16 days, and the mean medical cost was 1,077,690 yen. The average medical cost of TMZ-only treatment was 1,138,620 yen whilst it was 4,424,300 yen in concomitant TMZ patients. The LOS was significantly shorter in high-volume than in low-volume hospitals, and the medical cost was higher in hospitals treating 21–50 patients compared to those treating 1–10 patients. However, the direct medical cost of TMZ treatment was the same across different volume hospitals. This is the first report of current trends and healthcare resource usage in the treatment of primary malignant brain tumor inpatients in the TMZ era in Japan.
Keywords: malignant brain tumor, DPC, temozolomide, medical cost
Introduction
Malignant brain tumors are amongst the most lethal types of cancer. Its incidence is increasing, and hence, a growing number of patients are being treated in the clinic.1–4) The current incidence of primary brain tumors is 10–20 cases per 100,000 of the general population. Primary malignant brain tumors can be classified into a number of histological subtypes, but are mostly gliomas with a World Health Organization (WHO) grade between I and IV. Treatment consists of surgery, radiotherapy (RT), and chemotherapy (CTX), either alone or in combination, depending on the tumor histology and the patient’s condition. Temozolomide (TMZ) is an oral alkylating agent, and has been widely used to treat primary malignant glioma patients in Japan since 2006 when it was first covered by health insurance. After the publication of Stupp et al’s influential study, the standard initial treatment strategy for malignant glioma became concomitant RT and TMZ-based CTX.5) However, as TMZ is an expensive drug compared to carmustine and procarbazine, the economic burden of TMZ usage for the treatment of malignant glioma has been a matter of debate. For example, Wasserfallen et al reported that TMZ usage in concomitant and adjuvant treatment increased medical costs eight fold in a single institution cohort in Switzerland.6) Nevertheless, several studies demonstrated the cost-effectiveness of TMZ treatment in malignant brain tumor treatment.7–9) In this context, there is no data as to how many primary brain tumor patients are treated in Japanese hospitals, and how often TMZ is administered overall and in single hospitals. Given that concomitant TMZ treatment after surgery is considered the standard treatment internationally for malignant glioma, the medical economics of TMZ usage should be evaluated in individual countries because the health insurance system is different in each country.
In 2002, the Japanese government introduced a per diem prospective payment system with a Diagnosis-Related Groups (DRG)-like grouping, which is called Diagnostic Procedure Combination (DPC).10) Data for practices can be obtained from DPC, and an attending physician is responsible for clinical data entry for each patient. Using this database, we have previously reported the discharge outcomes of cerebrovascular disease patients in a nationwide retrospective analysis (the J-ASPECT study).11–13) In this study, we collected and analyzed all the DPC data for patients treated in 370 core and branch hospitals from a total of 847 hospitals participating in the Japan Neurosurgical Society training program. Brain tumor patients are treated in neurosurgical hospitals in Japan, and this treatment includes CTX and RT. Therefore, this dataset may include the majority of data for patients treated in Japan during the designated period.
The first aim of this study was to reveal what kind of therapeutic modality is administered, and the difference of modality based on patient age, focusing particularly on TMZ usage in the Japanese clinical setting. The second aim was to evaluate healthcare resource usage based on measures such as length of hospital stay (LOS) and direct medical cost using an exhaustive patient administrative claim database. Our findings clarify the current trends in the treatment of primary malignant brain tumor patients, and its associated medical economics in Japan.
Materials and Methods
Data acquisition
Of the 847 hospitals participating in the Japan Neurosurgical Society training program, 392 agreed to participate in this study. We obtained data between April 2013 and Mach 2014 from 392 hospitals, but 22 hospitals were excluded from the analysis because insufficient data are available. In total, the data from 370 hospitals were analyzed, including the DPC data of 501,609 patients admitted to neurosurgical hospitals. This dataset included background patient information such as age, sex, Charlson score, and Japan Coma Scale (JCS) score: 1, 2, 3-digit, and we could acquire information about the treatment procedure and modality, and the administered drug. In addition, we could obtain healthcare resource usage information such as the LOS and direct medical cost. Direct medical costs include hospitalization, medications, imaging examinations, surgery, CTX, and RT. Analysis of indirect medical costs is not included in this study. As mentioned above, the DPC reimbursement system pays for the surgery, RT, and CTX as fee-for-service (FFS), while other costs for hospitalization, medications, blood examination, imaging examination, and physician time are inclusive. As the cost of chemotherapeutic drugs is inclusive, the dose and duration of CTX are not reflected in DPC reimbursement. The medical cost was converted into US dollars based on an exchange rate at 103 Japanese Yen per US dollar.
Patient extraction
In this study, we focused on patients with primary malignant brain tumors of neuroepithelial origin. The DPC database does not include diagnostic histological information. The ICD-10 codes denote different intracranial primary malignant tumors as follows: C71, malignant brain tumor; C70, malignant intracranial tumor originating in the meninges; and C72, malignant intracranial tumor originating in the cranial nerves. In order to extract information on primary malignant brain tumors of neuroepithelial origin, we used C71 as the DPC ICD-10 code. Using this code, we assumed that we could extract data on astrocytic, oligodendroglial, ependymal, pineal, embryonal, germ cell, and other neuroepithelial tumors. Primary central nervous system lymphomas were not included as they are specified by a different code. We also assumed that no malignant meningeal, mesenchymal, or peripheral nerve sheath tumors were included in the analysis. Patients with malignant tumors in the sellar region and pituitary tumors were also excluded. In total, data for 6,142 patients with a primary malignant brain tumor were retrieved using code C71. Data analysis was performed for these patients.
Evaluation of treatment modalities
The DPC database includes sub-codes that specify the surgical procedures and adjuvant therapy used, allowing demographic data to be stratified according to the treatment modalities described below.
Surgery
The type of surgical treatment is specified by a K-code. In this study, we aimed to extract data on surgical procedures related directly to tumor treatment. We used codes K169 (tumor removal by craniotomy), K171 (transsphenoidal tumor removal), and K151-2 (tumor removal by extended skull base craniotomy) to extract data for patients who had a tumor removed by craniotomy. In addition, to extract data on biopsies, we used codes K148 (only craniotomy), K1541 (functional stereotactic surgery [hemilateral]), and K164-4 (stereotactic hematoma evacuation) because stereotactic tumor biopsy was not K-coded as of the end of this study period. We also included codes K1492 (decompressive craniectomy), K145 (extra-ventricle drainage), and K174 (operation for hydrocephalus). Collectively, to extract data for malignant brain tumor patients who underwent surgery, we used codes K-169, K148, K1541, K164-4, K171, K151-2, K1492, K145, and K174 (Table 1).
Table 1.
Number of extracted patients according to K-code
| K-code | Description | Number of patients (%) |
|---|---|---|
| K1691 | Tumor removal by craniotomy (pineal region) | 18 (0.9) |
| K1692 | Tumor removal by craniotomy | 1688 (79.8) |
| K148 | Craniotomy only | 34 (1.6) |
| K1541 | Functional stereotactic surgery (hemilateral) | 83 (3.9) |
| K164-4 | Stereotactic hematoma evacuation | 45 (2.1) |
| K145 | Extraventricular drainage | 66 (3.1) |
| K174 | Operation for hydrocephalus | 129 (6.1) |
| K1492 | Decompressive craniectomy | 22 (1.0) |
| K151-2 | Tumor removal by extended skull base craniotomy | 13 (0.6) |
| K171 | Transsphenoidal tumor removal | 6 (0.3) |
| K171-2 | Endoscopic transsphenoidal tumor removal | 11 (0.5) |
CTX
In order to evaluate the use of chemotherapeutic drugs, we selected the following agents that are used in the neurosurgical clinic: TMZ, nimustine (ACNU), interferon, bevacizumab, methotrexate, carmustine, ifosfamide, cisplatin, carboplatin, vincristine, cyclophosphamide, and procarbazine. We considered that CTX had been administered when there was a code for CTX and one of these drugs were listed.
RT
In Japan, payments for RT are classified and coded according to the treatment modality. External beam therapy (EBT) is coded as M001, and stereotactic radiosurgery (SRS) and stereotactic RT (SRT) are coded as M001-2 and M001-3, respectively. In this study, we identified patients treated with RT and sub-categorized them by modality using these codes.
Statistical analysis
LOS and medical cost were treated by log transformed value. Geometric means and their 95% confidence intervals were calculated. A general linear mixed model analysis was performed to determine statistically significant differences in mode of therapy on LOS or medical cost adjusted for age, sex, and the Charlson and JCS scores as a fixed effect and the hospital as a random effect. The differences in the number of patients per hospital were also determined. Reference population was set on male, average age (46.28), JCS = 0, and average Charlson score = 4.28, and then estimates and their 95% confidence interval for LOS and medical cost were presented. A value of p < 0.05 was considered statistically significant. The reference category for the number of patients per hospital was 1–10, and the JCS score had a value of 0, 1, 2, or 3. The analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethical statement
The research plan was designed by the authors and approved by the Institutional Review Board of Kyushu University. The requirement for individual informed consent was waived.
Results
Patient demographics
Of 6,142 primary malignant brain tumor patients, 57% were male and 43% were female. With regard to age, 18% of the patients were children aged 15 years or younger, 65% were adult patients aged between 16 and 70 years, and 17% were elderly patients aged over 71 years. The tumor type was unknown in 3% of the patients; 58% of patients had a primary tumor and 39% of patients had recurrent disease (Table 2). The number of patients treated in a single institution varied between 1 and 277, with a median of 7 (Fig. 1), indicating that many hospitals treated less than 20 primary malignant brain tumor patients (small-volume hospitals), and a few hospitals treated more than 100 patients (high-volume hospital).
Table 2.
Demographics and clinical characteristics of patients included in this study
| Total, n | 6,142 |
| Male, n (%) | 3,489 (56.8) |
| Age | |
| ≤15, n (%) | 1,091 (17.8) |
| 16–70, n (%) | 3,984 (64.9) |
| ≥71, n (%) | 1,067 (17.4) |
| Primary, n (%) | 3,549 (57.8) |
| Japan Coma scale | |
| 0, n (%) | 4,211 (68.6) |
| 1-digit code, n (%) | 1,592 (25.9) |
| 2-digit code, n (%) | 240 (3.9) |
| 3-digit code, n (%) | 99 (1.6) |
| Charlson score | |
| 2, n (%) | 1,948 (31.7) |
| 3, n (%) | 733 (11.9) |
| 4, n (%) | 757 (12.3) |
| 5, n (%) | 962 (15.7) |
| 6–10, n (%) | 1643 (26.8) |
| 11–15, n (%) | 99 (1.6) |
Fig. 1.
The distribution of the number of primary malignant brain tumor patients treated at each hospital
Surgery
Of 6,142 primary malignant brain tumor patients, 2,236 were assigned a surgical K-code, and of these, 1,963 patients had a K-code related to surgery to treat the tumor (Fig. 2A, Table 1). The remaining 273 patients underwent procedures not directly related to the tumor, such as brain abscess evacuation, tracheostomy, or central venous catheter insertion. According to data from the Japan Neurosurgical Society, there were 25,160 brain tumor surgeries in neurosurgical hospitals in 2013. Therefore, the number of surgical cases analyzed in this study is equivalent to 7.8% of all brain tumor surgeries in Japan for a period of one year.
Fig. 2.
(A) Frequency of each treatment modality (B) The ratio of different radiotherapy modalities in age groups (C) The distribution of types of therapy for all patients, and (D) by age group
Radiation
A total of 1,510 primary brain tumor patients underwent RT (Fig. 2A), of whom, 1,203 were treated using EBT, 90 using SRS, and 217 using SRT. EBT was the most popular radiation modality followed by SRT and SRS in all age groups (Fig. 2B), and the frequency of these modalities were very similar.
CTX
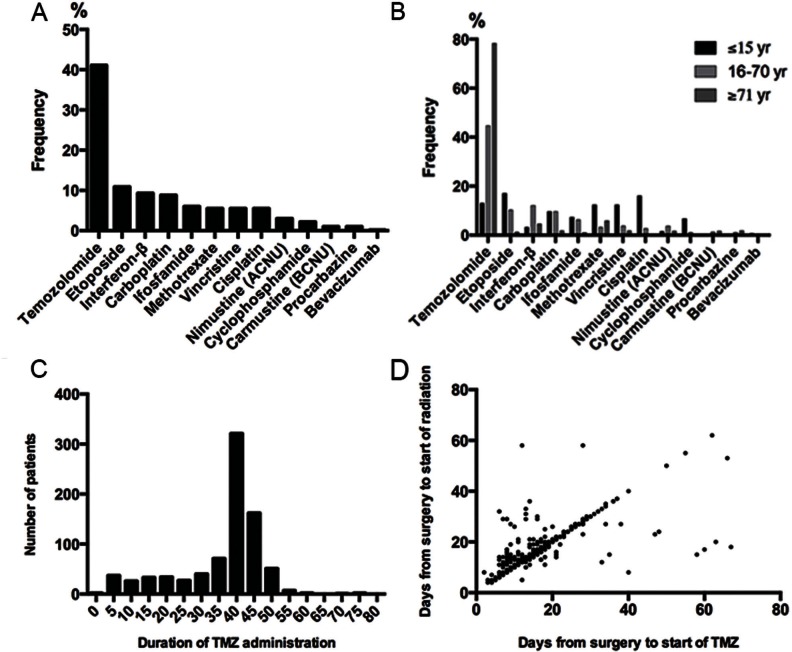
CTX was administered to 3,079 of the 6,142 patients with a primary brain tumor (Fig. 2A), using a total of 4,728 different regimens. As shown in Fig. 3A, the most frequently used drugs were TMZ (41%), followed by etoposide (11%), interferon-β (9%), and carboplatin (9%). Bevacizumab and carmustine were rarely used because they were not covered by health insurance at the start of this study period. With respect to age group, pediatric patients were less frequently administered TMZ compared to adults, but were more frequently treated using etoposide, carboplatin, methotrexate, vincristine, cisplatin, or cyclophosphamide (Fig. 3B). We also investigated the frequency with which combinations of drugs were administered to different age groups (Table 3). In total, combination therapy was used in 871 cases, and combined carboplatin and etoposide (CARE), or combined TMZ and interferon-β, were both commonly used in the adult group. In contrast, combined cisplatin and vincristine was most frequently used for pediatric patients, followed by combinations of carboplatin and etoposide, or ifosfamide, cisplatin, and etoposide (ICE) at a similar frequency. Combined cyclophosphamide, cisplatin, and vincristine therapy (Packer regimen) was also commonly used in the pediatric group.
Fig. 3.
Frequency with which each type of chemotherapeutic drug was administered for primary malignant brain tumor patients (for a total of 4,728 regimens) in (A) all patients and (B) patients in different age groups (C) The distribution of the duration of temozolomide (TMZ) administration for primary malignant brain tumor patients undergoing initial treatment (D) Relationship between the time between surgery and the start of TMZ or radiotherapy for primary malignant brain tumor patients undergoing initial treatment
Table 3.
Combination of chemotherapeutic drug according to the patient age group
| Chemotherapeutic drug (n = 871) | ≤15 yr (%) | 16–70 yr (%) | ≥71 yr (%) |
|---|---|---|---|
| Carboplatin + Etoposide | 69 (25.7) | 253 (43.7) | 5 (20.8) |
| Temozolomide + Interferon-β | 22 (8.2) | 229 (39.6) | 16 (66.7) |
| Cisplatin + Vincristine | 90 (33.6) | 19 (3.3) | 0 |
| Ifosfamide + Cisplatin + Etoposide | 60 (22.4) | 46 (7.9) | 0 |
| Cyclophosphamide + Cisplatin + Vincristine | 27 (10.1) | 7 (1.2) | 0 |
| Procarbazine + Nimustine + Vincristine | 0 | 25 (4.3) | 3 (12.5) |
We focused our analysis on TMZ, as it is the most commonly used chemotherapeutic drug for the treatment of malignant glioma. The most common duration of TMZ administration for initial cases (816 cases) was between 40 and 45 days, which is consistent with the standard concomitant TMZ treatment protocol of 42 days for initial malignant gliomas (Fig. 3C). In addition, in the concomitant TMZ treatment protocol, TMZ therapy and RT were initiated on the same day for most patients (Fig. 3D).
Mode of therapy
The 6,142 primary malignant brain tumor patients were classified into eight groups depending on whether they underwent surgery alone, surgery + RT, surgery + CTX, surgery + chemo-radiotherapy (CRT), RT, CTX, CRT, or none of these (Fig. 2A, C). Patients with primary tumors were most frequently treated using CTX, followed by surgery, and surgery + CRT. Pediatric patients less frequently underwent surgical treatment and were more often treated using CTX compared to adults. Hence, the type of therapy varied between adult and pediatric patients (Fig. 2D).
LOS
We analyzed the LOS with respect to the mode of therapy. The mean LOS of all the patients was 16 days. When we stratified the data according to the mode of therapy, primary tumor patients who underwent surgery had longer hospital stays compared to non-surgically treated patients (Table 4). In the subgroup of primary tumor patients who underwent surgery, the mean LOS was long amongst those who underwent surgery + CRT (73.8 days), followed by surgery + RT (65.5 days), surgery + CTX (38 days), and surgery alone (23.2 days). CRT was the most common treatment administered to patients who did not undergo surgery. When we stratified the patients according to the number of primary malignant brain tumor patients treated by their hospital, the LOS was significantly shorter in high-volume hospitals than in low-volume hospitals (Table 5).
Table 4.
Length of hospital stay and medical cost depending on therapeutic modalities
| Modalities | n | Length of stay (days) | n | Medical cost (10 thousand yen) | ||
|---|---|---|---|---|---|---|
| Geometric mean | 95% CI | Geometric mean | 95% CI | |||
| None | 1893 | 8.0 | 0.6–101.3 | 1774 | 39.1 | 4.1–369.1 |
| CTX | 1672 | 11.0 | 1.3–93.7 | 1640 | 64.5 | 11.3–370.1 |
| RT | 321 | 11.9 | 1.4–98.4 | 302 | 97.1 | 32.8–287.8 |
| CRT | 414 | 37.9 | 7.8–183.6 | 408 | 230.5 | 69.8–761.4 |
| Surgery | 779 | 23.2 | 7.4–73.2 | 763 | 275.2 | 132.5–571.5 |
| Surgery + CTX | 313 | 38.0 | 9.7–148.2 | 309 | 393.8 | 181.3–855.3 |
| Surgery + RT | 70 | 65.5 | 26.5–162.4 | 68 | 475.7 | 264.3–856.1 |
| Surgery + CRT | 680 | 73.8 | 35.0–155.7 | 672 | 592.6 | 341.3–1029.0 |
Table 5.
Length of hospital stay according to the patient volume of the hospital
| Patient volume | n | Length of stay (days) | Analysis of mixed model | |||
|---|---|---|---|---|---|---|
| Geometric mean | 95% CI | p value | Estimates for reference population | |||
| Estimates | 95% CI | |||||
| 1–10 | 998 | 24.6 | 2.7–227.5 | – | 18.1 | 16.4–20.0 |
| 11–20 | 863 | 20.8 | 2.2–194.4 | 0.256 | 16.6 | 14.5–18.9 |
| 21–50 | 1109 | 18.4 | 1.5–221.1 | 0.854 | 18.4 | 15.8–21.5 |
| 51–100 | 1480 | 16.0 | 1.4–182.9 | 0.181 | 15.8 | 13.2–18.9 |
| ≧101 | 1692 | 10.0 | 0.8–124.5 | 0.001 | 11.5 | 8.9–14.9 |
Direct medical cost
The DPC dataset also lists inpatient direct medical costs including surgery, CTX, RT, hospital stay, and other diagnostic and treatment modalities. The average direct medical cost for treating the patients was 1,077,690 yen. Consistent with the LOS, surgical treatment was much more expensive than non-surgical therapy (Table 4). Surgery + CRT was the most expensive treatment, at 5,926,220 yen, followed by surgery + RT (4,757,000 yen) and surgery + CTX (3,937,540 yen). The mean cost of surgery was 2,752,300 yen. We found that medical cost was higher in hospitals treating 21–50 patients compared to those treating 1–10 patients (Table 6). However, although the medical cost was lower in high-volume hospitals than in small-volume hospitals, this difference was not statistically significant. In the DPC system, days and dose of TMZ administration for the primary patients are not translated in the medical expenditure, which means that medical cost depends on whether TMZ is administered. We analyzed medical expenditure for TMZ only patients (420 cases) and concomitant TMZ patients (816 cases) according to the number of the patients per hospital. In TMZ only patients, the average medical cost was 1,138,620 yen, whilst for concomitant TMZ patients it was 4,424,300 yen, indicating that the direct medical cost increases more than two fold when it includes RT in Japan. In both groups, the medical cost was not statistically different among hospitals with different patient volumes (Table 6).
Table 6.
Direct medical cost according to the patient volume of the hospital
| Patient volume | Medical cost (10 thousand yen) | Analysis of mixed model | ||||
|---|---|---|---|---|---|---|
| n | Geometric mean | 95% CI of geometric mean | p value | Estimates for reference population | ||
| Estimates | 95% CI | |||||
| 1–10 | 977 | 133.5 | 13.5–1318.3 | – | 110.1 | 99.2–122.1 |
| 11–20 | 795 | 135.6 | 13.4–1373.9 | 0.334 | 119.3 | 103.7–137.3 |
| 21–50 | 1063 | 134.0 | 11.6–1549.2 | 0.011 | 139.7 | 119.0–163.9 |
| 51–100 | 1472 | 110.2 | 8.2–1475.4 | 0.655 | 115.2 | 96.1–138.1 |
| ≧101 | 1629 | 72.0 | 5.5–941.0 | 0.224 | 92.9 | 71.7–120.3 |
Discussion
In this study, we analyzed the current status of malignant brain tumor treatment using the DPC database in Japan. The advantage of using DPC data is that patient and hospital information, diagnosis, procedures, and administrative claim data are completely enumerated for all of the patients in the participating hospitals. Another benefit is that all of these data can be collected from the administrative claims database of inpatients without additional effort by medical staff. This study covered 370 hospitals (44%) out of all 847 Japanese Neurosurgical Society training program core and branch hospitals. Thus, we think that our study is a good representation of the current trends in malignant brain tumor treatment in Japan. Approximately 24,000 patients are newly diagnosed with primary malignant brain cancer annually in the United States.3,4) In this study, 3,562 (58%) of the 6,142 malignant tumor patients had primary disease, which is equivalent to 15% of all the patients in the United States.
Our analysis revealed that many of the hospitals treated less than 20 patients with primary malignant brain tumors in a single year. There are very few high-volume centers treating more than 100 malignant brain tumor patients per year in Japan, in contrast with the USA, Europe, Korea, and China, where malignant brain tumor patients are treated in high-volume core center hospitals. Regarding the use of cytotoxic chemotherapeutic drugs, we found that TMZ was administered to approximately 40% of patients, and that the next most frequently used drug was administered to less than 10% of patients, indicating that TMZ is the most widely prescribed drug for treating primary malignant brain tumors. However, amongst pediatric patients, TMZ was less frequently administered than platinum-based drugs, etoposide, vincristine, and ifosfamide. This may be because TMZ offers no significant benefit in pediatric patients,14) or, in part, because germ cell and embryonal tumors occur frequently in pediatric patients. Indeed, combination CTX, which is usually administered for germ cell and embryonal tumors, was most frequently used to treat pediatric tumors.
According to the standard protocol, RT consists of fractionated focal irradiation at a dose of 2 Gy per fraction for a total dose of 60 Gy, which is administered once daily 5 days per week over a period of 6 weeks. Concomitant CTX consisted of TMZ at a dose of 75 mg per square meter per day, administered 7 days per week from the first day of RT until the last day of RT. We found that TMZ administration most frequently lasted 40–45 days for many of the initial primary malignant brain tumor patients. In addition, RT and TMZ administration often started at the same time postoperatively, suggesting that concomitant CTX and RT is the current trend for initial primary malignant brain tumors in Japan. Taken together, our findings demonstrate that TMZ treatment for initial primary malignant brain tumor patients was undertaken according to the international standard protocol in Japanese neurosurgical hospitals.
We also evaluated the frequency with which different therapies were used to treat the patients. The most frequent treatment was CTX (27%), followed by surgery (13%), and surgery + CRT (11%). No single treatment type was used for more than 30% of patients. This differs from findings using the Brain Tumor Registry dataset,15) where surgery + CRT was most frequently used (51%), followed by surgery (18%) and surgery + RT (18%). Observation alone and other treatments accounted for only 2% of patients. There are a number of possible reasons for this discrepancy between the datasets. First, because tumor histology is not included in the DPC dataset, it is possible that this varies significantly between the datasets, which would be reflected in the different therapies used. Second, the TMZ administration for malignant glioma was covered by Japanese health insurance in 2006, which means that Brain Tumor Registry data were collected before the TMZ era between 2001 and 2004. This might explain why CTX (possibly involving TMZ) was used more frequently for patients included in our dataset. Third, actively treated patients in the university and national center (core) hospitals might have been selectively included in the Brain Tumor Registry. Given that our data are collected from all of the patients in registered hospitals including branch hospitals, our results reflect the current situation regarding malignant brain tumor treatment after admission to Japanese neurosurgical hospitals.
Sub-analysis of therapy type for primary tumor patients demonstrated that pediatric patients less frequently underwent surgical treatment, including surgery alone or combined with CRT, compared with adult and elderly patients. However, pediatric patients more frequently underwent CTX. This suggests that pediatric patients are more often treated using CTX than RT, and indeed the prevalence of RT regardless of surgery and CTX was 7.5%, 18%, and 25% in pediatric, adult, and elderly patients, respectively. Regarding the type of RT used, SRS/SRT accounted for a quarter of all RT used to treat primary brain tumors.
Our analysis also revealed novel findings regarding health care data in Japan. Japan sustains full and equal health insurance coverage with a single reimbursement fee system for all physicians and patients.16) Under this system, the mean LOS for primary malignant brain tumor patients was 16 days. Hospital stays generally get longer with increasingly complex modes of therapy. According to the 2011 data of the Ministry of Health, Labour and Welfare in Japan, the mean LOS or all cancer patients was 19.5 days.17) The mean LOS in our dataset was closer to this value (16 days). Accordingly, the mean LOS in the surgically treated groups was 46 days. The Ministry of Health, Labour and Welfare data also reveal that patients who undergo craniotomy have the longest stay in hospital (mean 48.5 days) among all patients undergoing surgery. As data for patients with benign tumors are also included in the Ministry of Health, Labour and Welfare dataset, this study is the first to demonstrate that the LOS of malignant brain tumor patients depends on the mode of therapy. Given that CTX or RT is more likely to be administered as an inpatient treatment in Japan, we need to be careful in comparing healthcare resource usage between countries.
In this study, we first evaluated the direct medical cost for the treatment of inpatient primary malignant brain tumor patients in Japan. The mean medical cost of all 6,142 patients was 1,077,690 yen, which is equivalent to 10,463 US dollars at the exchange rate of 103 Japanese yen per US dollar. A recent publication showed that the total direct cost for surgery and RT ranged from 50,600 to 92,700 US dollars in the United States.9) We found that the medical cost of patients undergoing both surgery and RT was 4,757,000 yen (46,184 dollars) in this study. Although the direct medical cost cannot be compared between countries with different health insurance systems, it seems clear that the direct medical expenditure for combined surgery and RT is within the same range in both countries. As expected, the medical costs are greater for patients undergoing surgery, RT, and CTX, at 5,926,220 yen (57,536 dollars). Concerning TMZ treatment, the cost of treating patients undergoing concomitant TMZ therapy after surgery was 4,424,300 yen (42,541 dollars). A previous study found that the medical cost of inpatients with concomitant TMZ therapy was 59,121 US dollars in the United States,18) which indicates that medical costs including TMZ treatment is lower than that in the United States. Furthermore, our results showed that the direct medical cost of patients undergoing surgery with only TMZ and concomitant TMZ is similar among the hospitals regardless of patient volume. This indicates that the same level of treatment is administered for primary malignant brain tumor patients across all hospitals in Japan, which may partly be because TMZ use is included in the DPC system, and thus, the dose and duration of TMZ administration is not reflected in the direct medical cost.
A limitation of this study is that detailed information concerning the tumor site, histology, and extent of resection was not available in the DPC data set. Furthermore, because the DPC dataset only includes mortality data for the corresponding admission period, information on patient outcomes after discharge is not included. Thus, the survival rate cannot be calculated. Moreover, outpatient data are not included. Nevertheless, this study provides a clear picture of the current trend of treatment for malignant brain tumors in Japan. If we can link this population-based dataset to the standard registration database, we could obtain very useful information regarding the treatment of malignant brain tumor patients.
In summary, we have assessed the current treatment and healthcare resource usage of malignant brain tumor patients in Japan using exhaustive claim data from 6,142 patients. This study could act as a road map towards the establishment of a better health care policy.
TMZ only
| Patient volume | Medical cost (10 thousand yen) | ||
|---|---|---|---|
| n | Geometric mean | 95% CI | |
| 1–10 | 82 | 162.2 | 27.4–958.9 |
| 11–20 | 55 | 107.6 | 11.8–984.2 |
| 21–50 | 82 | 137.1 | 17.4–1080.5 |
| 51–100 | 105 | 101.7 | 11.3–918.6 |
| ≧101 | 93 | 83.1 | 12.5–554.3 |
TMZ + RT (concomitant)
| Patient volume | n | Medical cost (10 thousand yen) | |
|---|---|---|---|
| Geometric mean | 95% CI | ||
| 1–10 | 149 | 463.7 | 160.3–1341.1 |
| 11–20 | 125 | 460.3 | 159.3–1329.6 |
| 21–50 | 169 | 460.2 | 161.5–1311.3 |
| 51–100 | 226 | 410.6 | 116.4–1449.0 |
| ≧101 | 140 | 437.0 | 146.9–1300.2 |
Reference population means male, average age(46.28), JCS = 0, and average Charlson score = 4.28
Acknowledgement
This study was conducted as the Joint Project of the 34th annual meeting of the Japanese Congress of Neurosurgeons (President K.I.) and the Japan Neurosurgical Society. We also thank Profs. Takamasa Kayama and Nobuo Hashimoto for their supervision of this collaborative project with the Japan Neurosurgical Society.
Footnotes
Conflict of Interest
The authors declare that there are no potential conflicts of interest in relation to this study.
References
- 1). Wrensch M, Minn Y, Chew T, Bondy M, Berger MS: Epidemiology of primary brain tumors: current concepts and review of the literature. Neuro-oncology 4: 278– 299, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Nakamura H, Makino K, Yano S, Kuratsu J, Kumamoto Brain Tumor Research Group : Epidemiological study of primary intracranial tumors: a regional survey in Kumamoto prefecture in southern Japan—20-year study. Int J Clin Oncol 16: 314– 321, 2011. [DOI] [PubMed] [Google Scholar]
- 3). Ostrom QT, Gittleman H, Liao P, Rouse C, Chen Y, Dowling J, Wolinsky Y, Kruchko C, Barnholtz-Sloan J: CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro-oncology 16 Suppl 4: iv1– iv63, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4). SEER Cancer Statistics Factsheets : Brain and Other Nervous System Cancer. National Cancer Institute; Bethesda, MD, http://seer.cancer.gov/stattacts/html/brain.html [Google Scholar]
- 5). Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B, Belanger K, Hau P, Brandes AA, Gijtenbeek J, Marosi C, Vecht CJ, Mokhtari K, Wesseling P, Villa S, Eisenhauer E, Gorlia T, Weller M, Lacombe D, Cairncross JG, Mirimanoff RO: European Organisation for Research and Treatment of Cancer Brain Tumour and Radiation Oncology Groups; National Cancer Institute of Canada Clinical Trials Group. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10: 459– 466, 2009. [DOI] [PubMed] [Google Scholar]
- 6). Wasserfallen JB, Ostermann S, Pica A, Mirimanoff RO, Leyvraz S, Villemure JG, Stupp R: Can we afford to add chemotherapy to radiotherapy for glioblastoma multiforme? Cost-identification analysis of concomitant and adjuvant treatment with temozolomide until patient death. Cancer 101: 2098– 2105, 2004. [DOI] [PubMed] [Google Scholar]
- 7). Lamers LM, Stupp R, van den Bent MJ, Al MJ, Gorlia T, Wasserfallen JB, Mittmann N, Jin Seung S, Crott R, Uyl-de Groot CA: EORTC 26981/22981 NCI-C CE3 Intergroup Study. Cost-effectiveness of temozolomide for the treatment of newly diagnosed glioblastoma multiforme: a report from the EORTC 26981/22981 NCI-C CE3 Intergroup Study. Cancer 112: 1337– 1344, 2008. [DOI] [PubMed] [Google Scholar]
- 8). Messali A, Hay JW, Villacorta R: The cost-effectiveness of temozolomide in the adjuvant treatment of newly diagnosed glioblastoma in the United States. Neuro-oncology 15: 1532– 1542, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). Raizer JJ, Fitzner KA, Jacobs DI, Bennett CL, Liebling DB, Luu TH, Trifilio SM, Grimm SA, Fisher MJ, Haleem MS, Ray PS, McKoy JM, DeBoer R, Tulas KM, Deeb M, McKoy JM: Economics of Malignant Gliomas: A Critical Review. J Oncol Pract 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). Hamada H, Sekimoto M, Imanaka Y: Effects of the per diem prospective payment system with DRG-like grouping system (DPC/PDPS) on resource usage and healthcare quality in Japan. Health Policy 107: 194– 201, 2012. [DOI] [PubMed] [Google Scholar]
- 11). Iihara K, Nishimura K, Kada A, Nakagawara J, Ogasawara K, Ono J, Shiokawa Y, Aruga T, Miyachi S, Nagata I, Toyoda K, Matsuda S, Miyamoto Y, Suzuki A, Ishikawa KB, Kataoka H, Nakamura F, Kamitani S: Effects of comprehensive stroke care capabilities on in-hospital mortality of patients with ischemic and hemorrhagic stroke: J–ASPECT study. PloS one 9: e96819, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Iihara K, Nishimura K, Kada A, Nakagawara J, Toyoda K, Ogasawara K, Ono J, Shiokawa Y, Aruga T, Miyachi S, Nagata I, Matsuda S, Ishikawa KB, Suzuki A, Mori H, Nakamura F: J-ASPECT Study Collaborators. The impact of comprehensive stroke care capacity on the hospital volume of stroke interventions: a nationwide study in Japan: J-ASPECT study. J Stroke Cerebrovasc Dis 23: 1001– 1018, 2014. [DOI] [PubMed] [Google Scholar]
- 13). Kamitani S, Nishimura K, Nakamura F, Kada A, Nakagawara J, Toyoda K, Ogasawara K, Ono J, Shiokawa Y, Aruga T, Miyachi S, Nagata I, Matsuda S, Miyamoto Y, Iwata M, Suzuki A, Ishikawa KB, Kataoka H, Morita K, Kobayashi Y, Iihara K: Consciousness level and off-hour admission affect discharge outcome of acute stroke patients: a J-ASPECT study. J Am Heart Assoc 3: e001059, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14). MacDonald TJ, Aguilera D, Kramm CM: Treatment of high-grade glioma in children and adolescents. Neuro-oncology 13: 1049– 1058, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Japan TCoBTRo : Report of brain tumor registry of Japan (2001–2004). 13th edition. Neurol Med Chir (Tokyo) suppl 1( 54): 1– 102, 2014. [Google Scholar]
- 16). Reich MR, Shibuya K: The Future of Japan's Health System—Sustaining Good Health with Equity at Low Cost. N Eng J Med 373: 1793– 1797, 2015. [DOI] [PubMed] [Google Scholar]
- 17). Statistical survey conducted by Ministry of health, Labour and Welfare. http://www.mhlw.go.jp/toukei/saikin/hw/kanja/11/index.html, 2011.
- 18). Ray S, Bonafede MM, Mohile NA: Treatment patterns, survival, and healthcare costs of patients with malignant gliomas in a large US commercially insured population. Am Health Drug Benefits 7: 140– 149, 2014. [PMC free article] [PubMed] [Google Scholar]