Abstract
Low- and middle-income countries (LMICs) face a critical shortage of basic surgical services. Adequate neurosurgical services can have a far-reaching positive impact on society’s health care and, consequently, the economic development in LMICs. Yet surgery, and specifically neurosurgery has been a long neglected sector of global health. This article reviews the current efforts to enhance neurosurgery education in LMICs and outlines ongoing approaches for improvement. In addition, we introduce the concept of a sustainable and cost-effective model to enhance neurosurgical resources in LMICs and describe the process and methods of online curriculum development.
Keywords: neurosurgery, surgery, education, training, health care
Introduction
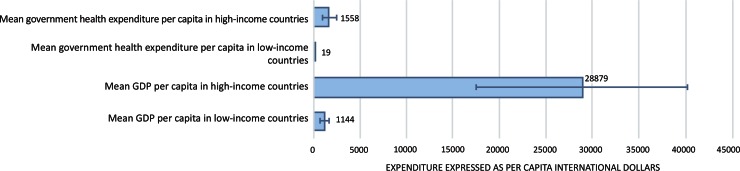
Over the past decades, significant progress has been made to improve global health. Average life expectancy has increased and child mortality rates have been reduced substantially.1) There has been significant progress in limiting infectious diseases because of improved sanitation, nutrition, drugs, and vaccines. Nevertheless, important inequalities between nations remain. Approximately 50 million people live in countries with an average life expectancy of less than 45 years.1) Such disparity is in large part rooted in economic priorities, with nations like Eritrea spending 3% of their US$4 billion gross domestic product on health in 2012, compared to nations like Japan (gross domestic product of US$4.2 trillion) that spent 10.3%.2) Per capita numbers also illustrate a wide disparity, which in turn affects health expenditures3) (Fig. 1).
Fig. 1.
Health care expenditures per capita in high- and low- income countries expressed as international dollars. Data collected from the World Health Organization (2011).3)
Because of its perceived high costs, surgical care has not been considered a health priority in many low-income nations. Around 2 billion people worldwide lack access to even basic surgical services.4) Without accessible surgical care, pervasive, yet easily treatable, diseases become debilitating illnesses with a high mortality and morbidity rate. Low- and middle- income countries (LMICs) face an extreme scarcity of facilities and basic equipment required for procedures.5) Indeed, deficient infrastructure and a lack of appropriate training for medical professionals are major obstacles to providing the necessary surgical services globally.
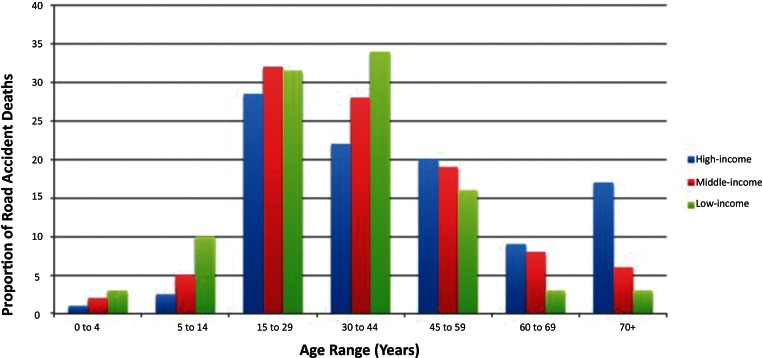
In the spectrum of global health, neurosurgery has been especially overlooked and falsely considered as an expensive luxury for the elite.6) However, neurological disorders affect people worldwide, regardless of age, sex, income, or level of education. Neurological illnesses, including traumatic brain injuries, degenerative diseases, and congenital disorders, affect up to one billion individuals.7) Together, they cause more than 6.8 million fatalities per year, which is about the same as the number of deaths from AIDS, tuberculosis, and malaria combined.8) Further, approximately 80% of the total fatalities due to road traffic accidents occur in LMICs.9) In many African nations, road traffic accidents cause as many deaths as malaria. Road traffic accidents alone are the most common cause of death for individuals between 15–29 years-old, a demographic group who is vital to the economic development of these nations.9) Indeed, the percentage of road accident deaths involving younger age groups is significantly higher in LMICs than in high-income countries9) (Fig. 2).
Fig. 2.
Proportion of road traffic deaths by age range and country income status. Figure modified from the World Health Organization: Global Status Report on Road Safety (2013).9)
An additional factor that affects neurosurgical care is the number of trained neurosurgeons available to care for these disorders. According to the World Health Organization (2004) the median number of neurosurgeons per 100,000 individuals is 0.03 for low-income countries and 0.97 for high-income countries.7) This shortage is the most significant in Africa – this continent of approximately one billion people has around only 1200 practicing neurosurgeons.10) In countries where care is available, many of the neurosurgeons reside in urban areas, voiding the rural population access to neurosurgery.10) Collectively, neurological disorders are a “neglected epidemic” in LMICs.11,12)
Without investments to increase global surgical care, LMICs will continue to experience significant losses in economic productivity. In a recent article published in the Lancet, it is estimated that the economic burden of neurological disorders would cost a total of US$12.3 trillion between 2015 and 2030.4) In the developing world, approximately half the population are younger than 18 years of age.6) These individuals, soon to become the most productive members of society, form a particularly vulnerable population with respect to the risk of traumatic injuries, the most common and prevalent cause for neurological injury in LMICs.9) Clearly, an investment in affordable neurosurgical services for LMICs is not only an important life-saving action, it also fosters a much needed economic growth in the developing world.6)
Methods to Address the Lack of Global Neurosurgery, the need for Investment in Equipment, Training, and International Collaborations
The delayed and suboptimal delivery of neurosurgical care in LMICs is the combined result of many factors. First, many LMICs frequently have limited equipment and supplies to support diagnostic imaging capabilities as well as surgical infrastructure, restricting neurosurgeons in the care they can provide.5) Second, LMICs often see neurosurgical pathology presenting late in the course of the disease, making care far more complicated, and consequently increasing morbidity and mortality.6) Other remaining factors affecting care include resource limitations and the limited ability of patients’ financial access, affecting the availability of some neurosurgical services such as MR imaging.13)
Various strategies are available to address these issues and to increase the neurosurgical workforce in LMICs. Efforts have been made to prevent the rise of neurological disorders; these societal changes include laws for the increased use of helmets by motorcyclists to prevent traumatic brain injuries,14) and for the increase availability of immunizations against meningitis and malaria.7) While improved infrastructure and modern equipment will advance care in the short term, the most beneficial measure with significant long-term effectiveness is improvement of education and training of neurosurgery residents. If implemented efficiently, an improvement in education should not require a large financial investment and, yet, it can contribute greatly to strengthening capacity.
At the present time, not only is there a notable deficiency of neurosurgeons, but too few doctors are being trained to meet the increase surgical demands of the growing population.7) We consider that the most important aspect to ensure sustainable surgical health care improvement in LMICs is to develop long-term, capacity-building educational initiatives. A 2013 study conducted in Ethiopia discovered that the lack of educational resources is the main barrier preventing faculty members from providing optimal surgical training to the local residents.15) Taken together, fostering independent neurosurgeons by supporting the development of evidence-based programs in LMICs will strengthen surgical education and promote safe and high quality care.
Current Status of International Training and Methods of Education
As previously reasoned, providing neurosurgical training to surgeons in LMICs is the most sustainable and effective approach to increase access to neurosurgery globally. Central to an effective medical curriculum is to address the unique educational challenges of individual LMICs. There are currently several different methods for disseminating didactic neurosurgical knowledge to LMICs, and many of these efforts have been well established.5) Two important methods will be discussed, along with their benefits and shortcomings. Subsequently, we present an innovative and sustainable model of education, an approach that is most suitable for the delivery of neurosurgical knowledge in LMICs.
Visit-based model
Ongoing strategies to improve international neurosurgical care have largely relied on visits made by individual surgeons to regions of LMICs in need.16) In partnership with local surgeons, teams often travel to areas with where the need for a specific technique has been identified locally, and operate and teach for a short period of time.17) Organizations including the World Federation of Neurological Surgeons (WFNS)18) and Foundation for International Education in Neurological Surgery (FIENS)17) have employed site visits as part of their mandate to create educational initiatives in LMICs. Their efforts consist of regular courses and conferences that take place in LMICs, attracting local and regional neurosurgeons and bringing an international expertise to them. Japan has had an illustrious role in this regard, most recently under the guidance and leadership of Dr. Kato (WFNS Education Committee) and Dr. Kawase (WFNS Executive). The popularity of this model is owed to the several benefits directly observed from a hands-on approach to teaching neurosurgical skills. During each trip, opportunities for perioperative knowledge transfer and skill expansion are abundant as the visiting neurosurgeons are able to work alongside local trainees. An on-site training approach also benefits patients who are scheduled for surgery during the site visits; these individuals are treated locally by local neurosurgeons, side by side with experienced international neurosurgeons.
A visit-based approach, however, presents several challenges that limit its suitability as a long-term model of neurosurgical education. This model places its impetus on well-trained neurosurgeons to allocate the necessary time and financial resources in order to reach local doctors in LMICs.10) The number of sites relative to the number of visiting doctors, and the financial resources required constrain the amount and the duration of each visit. Surgical visits can also vary widely in the number of visiting staff, ranging from a large team of nurses, anesthesiologists, and surgeons to a single physician. As a result, site visits can become episodic in nature, restricting the visiting neurosurgeon’s ability to invest in local neurosurgical education and making it difficult for LMICs to gain a consistent and ongoing educational experience. A visit-based model can also potentially result in disruptions for the local clinical environment, as staff and trainees may reduce scheduled responsibilities in order to join in educational and developmental activities. Consistent visits by a neurosurgical team to the same site can result in building of a significant team relationship with a highly effective training, however, as a whole, a visit based approach could be criticized for its transient nature and for having limited long-term impact on global neurosurgery.19)
Online electronic learning model
Given the potential of the internet as a widespread global communication tool, distance electronic learning (eLearning) is growing as an accepted teaching tool, and is becoming widely used in the field of medicine.20) eLearning, in itself, is a multi-disciplinary platform spanning such tools as listservs, electronic libraries, webinars, and comprehensive online courses18) (Table 1). Not all of these models are applicable to neurosurgical training however. Blankstein et al.18) describe a number of eLearning tools that can be effective for neurosurgical trainees in LMICs. Organizations, such as the Ptolemy Project (Canada) and the School for Surgeons (Ireland), have employed eLearning tools to supplement the surgical training and advance the career of LMICs’ physicians.23) Online course administered through a stable virtual classroom platform such as Moodle (www.moodle.org) or WebCT (www.webct.com) allows for in-depth control over content delivery, including material, pace, and time of the lectures. Lectures can be delivered synchronously (faculty and residents are present online at the same time) or, in consideration of the geographical distance and the nature of neurosurgical hours, courses can be delivered asynchronously. The latter permits the faculty and residents to enter the course site and view the material at their convenience, within a defined period of time.
Table 1.
Summary of the methods of online education (listserv, online libraries, webinars, and online courses) and features of each, adapted from Blankstein et al.18)
| Listserv | Online libraries | Webinars | Online courses | |
|---|---|---|---|---|
| Level of structure | Lowest | Low | High | Highest |
| Resource-based | No | Yes | Yes | Yes |
| Instructional course | No | No | Yes | Yes |
| Self-paced | Yes | Yes | Yes | No |
| Faculty-based | No | No | No | Yes |
| Assessment methods | No | No | Possible, but not integrated | Yes |
| Metrics of student activity | No | No | No | Yes |
A fully online structured teaching tool can be used as a cost-effective substitute to the face-to-face learning environment offered by a visit-based model. An estimate of over $250 million is spent each year for surgical trips alone.21,22) In contrast, instruction using learning management systems would constitute a fraction of the cost. As the structure of the learning can be relatively self-paced, students and individuals have the option to enhance their learning in whichever particular topic they select.18) Trainees have the opportunity to access and review the necessary course material, instead of relying on the presence of visiting neurosurgeons.
An important aspect in the consideration of eLearning for neurosurgical education involves factors that challenge its value as an effective teaching tool if used in isolation. For instance, there is the potential for limited guidance from faculty as well as limited interactivity, which can make students less engaged and can result in attrition from the courses, a well-known phenomenon in eLearning.24,25) Also, limited interactivity with faculty conflicts with current models of neurosurgery resident education. A sustainable eLearning tool in neurosurgical education needs to include the optimal methods of surgical training and technological advances available in eLearning platforms. Therefore, while easy to implement and cost-effective, an online electronic learning approach to neurosurgery can present critical challenges in allowing for interactivity and maintaining student engagement.
A collaborative approach
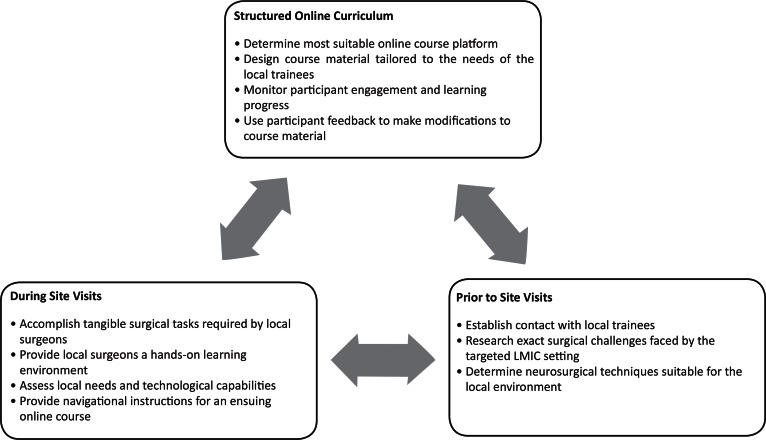
International collaborative efforts in neurosurgery require interaction among teams. Without the presence of visiting doctors, the full impact of hands-on learning experience is not adequately delivered. Long-term sustainable improvement depends on a collaborative approach where international faculty assists locally accessible education and training initiatives, support these initiatives and work in a forum that permits ongoing contact with the site. In this light, online courses, personalized to the site and complemented by annual visits appear to be the most effective option to achieve sustained improvements in neurosurgical education. This approach involves the deployment of initial site visits to allow for international faculty to understand the strengths as well as challenges faced by local neurosurgical trainees. Simultaneously, the opportunity provides local trainees to gain a face-to-face learning experience and interaction with the international faculty. The use of an online curriculum, in addition, would supplement the gaps in knowledge not addressed by site visits, such that local trainees are able to continually improve their neurosurgical knowledge and perform the needed surgeries (Fig. 3).
Fig. 3.
Schematic model of a collaborative approach to neurosurgical education, representing the relationship between international faculty, local trainees, and a structured online curriculum.
Four central features imperative to a localized neurosurgical educational program can be met by this approach, these are:
Identifying and understanding local needs and local participants;
Integrating modern surgical education with basic fundamental principles of neurosurgical care;
Focus on didactic component of neurosurgical education and parallel case discussions to enhance surgical decision-making;
Fostering independent growth within local neurosurgical programs.
A collaborative approach establishes a dialogue between international faculty and trainees located in the resource-poor setting. Prior to initial site visits, international neurosurgeons are able to familiarize themselves with the clinical, and socio-cultural challenges of the targeted settings in LMICs, and research the available resources. In collaboration with the local team, key decisions can be made to maximize the time and resources spent during the visit. Visiting surgeons also gain the opportunity to accomplish tangible tasks requested by the local surgeons, which are frequently different than preconceived notions about the needs of a specific site.
Further, collaboration paves way for the establishment for an ensuing online curriculum that extends the newly acquired perioperative techniques. As the implementation of a successful online curriculum requires careful design of course material tailored to the audience’s needs, means of determining the appropriate course structure and material can be made during initial site visits. Through the use of an online platform, participant engagement and interest in course can also be measured through their course-site hits (measurements of course activities online), time spent online, and discussion forum activity. Additionally, pre- and post-course assessments can be used to monitor the learning progress. To make important modifications to course material, further consultation visits can be made when deemed necessary.
A structured online curriculum allows residents to interact with international faculty online through lectures, discussion forums, and surgical case reviews. This collaborative approach to neurosurgical education transforms eLearning into a personalized course specifically tailored to address locally identified needs and to support local surgical capacity. Although limited in deployment, several examples exist in the application of eLearning protocols, in geographic areas such as India, Ghana, and Cambodia.26,27)
Conclusion
A variety of education and care delivery models have the potential to serve and to facilitate residency education and training in LMICs and improve the quality of global neurosurgery. Having complementary components allows a program to maximize and grow its strengths. The use of structured and methodical online education complemented by site visits can effectively and sustainably improve neurosurgical care in LMICs by strengthening the didactic elements in neurosurgical training. It is clear that neurosurgical training is not about technical skills alone. Along with didactic elements, familiarization with comprehensive patient management and surgical decision-making are critical components in training. This preparation is a fundamental requirement for every resident, and can be easily implemented online. This, in turn, will bridge the gap in neurosurgical access between developed and low-income countries. The use of site visits provides opportunities to address needs with respect to the delivery of care and training level, while an online curriculum offers more opportunities to establish a long-term learning environment for the local trainees. We believe this model of education appears to be the most powerful method of strengthening neurosurgical proficiency in low-resource settings.
Footnotes
Conflicts of Interest Disclosure
The authors declare that there is no conflict of interest (COI) regarding this article according to the criteria of The Japan Neurosurgical Society. Dr. Mojgan Hodaie is the founder of NEURONproject, a non-for-profit educational venture dedicated to training neurosurgical residents in low and middle income countries (LMICs). Dr. Hodaie has no financial research associated with this manuscript, but has previously received scientific research support from the Canadian Institute of Health Research, Multiple Sclerosis Society of Canada, Brain Canada, Elekta and Mitacs Canada
References
- 1). 50 Facts : Global health situation and trends 1955–2025. World Health Organ Tech Rep Ser 1: 3– 10, 1998. [Google Scholar]
- 2). World health statistics 2015 World Health Organ Tech Rep Ser 1: 3– 25, 2015. [Google Scholar]
- 3). Kea X, Saksenaa P, Hollyb A: The determinants of health expenditure: a country-level panel data analysis. World Health Organization 1: 1– 28, 2011. [Google Scholar]
- 4). Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, Bickler SW, Conteh L, Dare AJ, Davies J: Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. The Lancet 386: 569– 624, 2015. [DOI] [PubMed] [Google Scholar]
- 5). Butler MW: Developing pediatric surgery in low-and middle-income countries: An evaluation of contemporary education and care delivery models. Sem in Pediatr Surg 25: 43– 50, 2015. [DOI] [PubMed] [Google Scholar]
- 6). Ellegala DB, Simpson L, Mayegga E, Nuwas E, Samo H, Naman N, Word DB, Nicholas JS: Neurosurgical capacity building in the developing world through focused training: Clinical article. J Neurosurg 121: 1526– 1532, 2014. [DOI] [PubMed] [Google Scholar]
- 7). Neurological disorders: public health challenges World Health Organ Tech Rep Ser 1: 75– 76, 2006. [Google Scholar]
- 8). Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG: Injuries: the neglected burden in developing countries. Bull World Health Organ 87: 246– 246, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). WHO global status report on road safety 2013: supporting a decade of action. World Health Organ Tech Rep Ser 1: 2– 10, 2013. [Google Scholar]
- 10). Albright AL, Ferson SS: Developing pediatric neurosurgery in a developing country. J Child Neuro 12: 1559– 1564, 2012. [DOI] [PubMed] [Google Scholar]
- 11). Mueller BK, Mueller R, Schoemaker H: Stimulating neuroregeneration as a therapeutic drug approach for traumatic brain injury. Br J Pharmacol 157: 675– 685, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Nantulya VM, Reich MR: The neglected epidemic: road traffic injuries in developing countries. BMJ 324: 1139, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13). Hambrecht A, Duenas MJ, Hahn EJ, Aryan HE, Hughes SA, Waters D, Levy ML, Jandial R: Strategic design for pediatric neurosurgery missions across the Western Hemisphere. Surg Neuro Int 4: 62, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14). Cassidy JD, Carroll L, Peloso P, Borg J, Von Holst H, Holm L, Kraus J, Coronado V: Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on mild traumatic brain injury. J Rehab Med 36: 28– 60, 2004. [DOI] [PubMed] [Google Scholar]
- 15). Cadotte DW, Blankstein M, Bekele A, Dessalegn S, Pain C, Derbew M, Bernstein M, Howard A: Establishing a surgical partnership between Addis Ababa, Ethiopia, and Toronto, Canada. Can J Surg 55: 19, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16). Shrime MG, Sleemi A, Ravilla TD: Charitable platforms in global surgery: a systematic review of their effectiveness, cost-effectiveness, sustainability, and role training. W J Surg 39: 10– 20, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). Mosberg WH, Jr, Svien HJ, Tyrer AR, Jr, Mount L, Mosberg WH, Jr, Voris HC, Evans JP, Hayes GJ, Livingston KE, Thompson RK: Foundation for International Education in Neurological Surgery, Incorporated. J Neurosurg 33: 481– 484, 1970. [DOI] [PubMed] [Google Scholar]
- 18). Blankstein U, Dakurah T, Bagan M, Hodaie M: Structured online neurosurgical education as a novel method of education delivery in the developing world. W Neurosurg 76: 224– 230, 2011. [DOI] [PubMed] [Google Scholar]
- 19). Riviello R, Lipnick MS, Ozgediz D: Medical missions, surgical education, and capacity building. J Am Coll Surg 213: 572, 2011. [DOI] [PubMed] [Google Scholar]
- 20). Masic I: E-Learning as new method of medical education. Acta Informatica Medica 16: 102, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21). Parikh PY, Nwariaku FE: Ethics in Global Surgery. Academic Global Surgery 15: 29– 37, 2016. [Google Scholar]
- 22). Maki J, Qualls M, White B, Kleefield S, Crone R: Health impact assessment and short-term medical missions: a methods study to evaluate quality of care. BMC Health Services Research 8: 1, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23). Casey KM: Opening the doors to surgical education in low-and middle-income countries. JAMA Surg 149: 347, 2014. [DOI] [PubMed] [Google Scholar]
- 24). Angelino LM, Williams FK, Natvig D: Strategies to Engage Online Students and Reduce Attrition Rates. J Educat Online 4: 22, 2007. [Google Scholar]
- 25). Moody J: Distance education: Why are the attrition rates so high? Quarterly Review of Distance Education 5: 205, 2004. [Google Scholar]
- 26). Vyas R, Albright S, Walker D, Zachariah A, Lee MY: Clinical training at remote sites using mobile technology: An India-USA partnership. Distance Education 31: 2, 2010. [Google Scholar]
- 27). Hodaie M, Bernstein I, Liang K: NEURONProject- Neurosurgical Education with Universal Reach Online. Retrieved from http://www.neuronproject.org/ 1: 1, 2016. [Google Scholar]