Abstract
Objective
Most small for gestational age pregnancies are unrecognised before birth, resulting in substantial avoidable perinatal mortality and morbidity. Our objective was to develop multivariable prediction models for small for gestational age combining clinical risk factors and biomarkers at 15±1 weeks’ with ultrasound parameters at 20±1 weeks’ gestation.
Methods
Data from 5606 participants in the Screening for Pregnancy Endpoints (SCOPE) cohort study were divided into Training (n = 3735) and Validation datasets (n = 1871). The primary outcomes were All-SGA (small for gestational age with birthweight <10th customised centile), Normotensive-SGA (small for gestational age with a normotensive mother) and Hypertensive-SGA (small for gestational age with an hypertensive mother). The comparison group comprised women without the respective small for gestational age phenotype. Multivariable analysis was performed using stepwise logistic regression beginning with clinical variables, and subsequent additions of biomarker and then ultrasound (biometry and Doppler) variables. Model performance was assessed in Training and Validation datasets by calculating area under the curve.
Results
633 (11.2%) infants were All-SGA, 465(8.2%) Normotensive-SGA and 168 (3%) Hypertensive-SGA. Area under the curve (95% Confidence Intervals) for All-SGA using 15±1 weeks’ clinical variables, 15±1 weeks’ clinical+ biomarker variables and clinical + biomarkers + biometry /Doppler at 20±1 weeks’ were: 0.63 (0.59–0.67), 0.64 (0.60–0.68) and 0.69 (0.66–0.73) respectively in the Validation dataset; Normotensive-SGA results were similar: 0.61 (0.57–0.66), 0.61 (0.56–0.66) and 0.68 (0.64–0.73) with small increases in performance in the Training datasets. Area under the curve (95% Confidence Intervals) for Hypertensive-SGA were: 0.76 (0.70–0.82), 0.80 (0.75–0.86) and 0.84 (0.78–0.89) with minimal change in the Training datasets.
Conclusion
Models for prediction of small for gestational age, which combine biomarkers, clinical and ultrasound data from a cohort of low-risk nulliparous women achieved modest performance. Incorporation of biomarkers into the models resulted in no improvement in performance of prediction of All-SGA and Normotensive-SGA but a small improvement in prediction of Hypertensive-SGA. Our models currently have insufficient reliability for application in clinical practice however, they have potential utility in two-staged screening tests which include third trimester biomarkers and or fetal biometry.
Introduction
Approximately 40% of non-anomalous singleton stillbirths are small for gestational age (SGA) [1, 2] and live born SGA infants have increased risk of long-term adverse outcomes.[3–5] Placental insufficiency is a major contributor to the pathophysiology in SGA pregnancies.[6]
A limitation of antenatal care is that the majority of SGA pregnancies are not identified before birth.[7–9] SGA infants recognized before birth and delivered in a timely fashion have a four-fold reduction in composite severe morbidity/ mortality.[10] Reliable early pregnancy risk prediction, therefore has potential to reduce morbidity and mortality. As we have previously reported,[11] SGA infants can be broadly classified into two categories with distinct maternal phenotypes: SGA with a normotensive mother (Normotensive-SGA) and SGA where the mother has gestational hypertension, preeclampsia or chronic hypertension (Hypertensive-SGA).[7] We have previously reported that Normotensive- SGA comprise approximately three quarters of SGA infants and that risk factors for Normotensive-SGA and Hypertensive-SGA differ, suggesting they are distinct conditions from the prediction perspective.[12] We have recently published risk prediction models for these SGA sub-groups, derived from participants in the Screening for Pregnancy Endpoints (SCOPE) study, combining early pregnancy clinical variables with ultrasound parameters from the 20±1 weeks’ anatomy scan. Only modest predictive performance was achieved.[11] Abnormal placentation may be detected by altered biomarker concentrations in early pregnancy.[13–16] A recent systematic review of first trimester biomarkers to predict SGA reported that biomarkers alone had low predictive accuracy but speculated that performance would improve with addition of clinical characteristics and uterine artery Doppler.[17] An increase in predictive performance for SGA has been reported, after addition of first trimester biomarkers and uterine artery Doppler to clinical risk factors.[18]
Our primary objective was to develop multivariable prediction models for the respective SGA phenotypes, by combining biomarkers with clinical risk factors measured at 15±1 weeks’ and with uterine artery Doppler indices and fetal biometry at 20±1 weeks’ gestation. Since customized birthweight centiles may better identify small vulnerable babies with placental dysfunction, we used customized centiles to define SGA.[19–21]
We hypothesised that addition of 15±1 weeks’ biomarker data to models comprising clinical and ultrasound variables would result in significant improvements in prediction of SGA pregnancies.
Methods
The participants were healthy nulliparous women with singleton pregnancies recruited to the SCOPE study between November 2004 and February 2011 in Auckland, New Zealand, Adelaide, Australia, Manchester, Leeds and London, United Kingdom and Cork, Ireland. SCOPE (www.scopestudy.net) is a prospective, multi-centre cohort study with the main aim of developing screening tests to predict preeclampsia, SGA infants and spontaneous preterm birth. Ethical approval was obtained from institutional ethics committees of each participating center and all women provided written informed consent [New Zealand AKX/02/00/364–23 April 2003; Australia REC 1712/5/2008–2 November 2005; London and Manchester 06/MRE01/98–19 January 2007; Leeds 06/MRE01/98–5 November 2007 and Cork ECM5 (10) 05/02/08–6 February 2008]. Detailed methods have previously been described.[7, 22]
Exclusion criteria included 1) an elevated risk of preeclampsia, small for gestational age (SGA) or spontaneous preterm birth due to underlying medical conditions (known chronic hypertension, and/or pre-existing diabetes, renal disease, systemic lupus erythematosus, or anti-phospholipid syndrome), previous cervical knife cone biopsy, ≥3 terminations or ≥3 miscarriages or current ruptured membranes; 2) known major fetal anomaly or abnormal karyotype or 3) interventions (such as low dose aspirin) that might modify pregnancy outcome.[23] Women were recruited at 15±1 weeks’ gestation. Of the 8531 women invited to participate 5989 (70%) agreed and were interviewed and examined by a research midwife at 15±1 and 20±1 weeks’ and underwent ultrasound examination at 20±1 weeks’. Detailed clinical data were collected at each time point. The estimated date of delivery was calculated as follows: if the woman had a certain last menstrual period (LMP) date, the estimated date of delivery was only adjusted if either 1) a scan performed at <16 weeks’ gestation found a difference of ≥7 days between the scan gestation and that calculated by the LMP or 2) on 20±1 week scan a difference of ≥10 days was found between the scan gestation and that calculated from the LMP. If her LMP date was uncertain, then scan dates were used to calculate the estimated date of delivery. At the interview, data were entered into a secure internet-accessed, auditable database (MedSciNet AB, Sweden).
Ultrasound examination at 20±1 weeks’ was performed by trained sonographers and included fetal biometry and Doppler studies of the umbilical and uterine arteries. Fetal measurements were adjusted for gestational age by calculating the multiple of the median for each gestational week. Mean uterine resistance index (RI) was calculated from the left and right uterine RI. If only a left or right uterine RI was available, this was used as ‘mean RI’ (n = 98). Women without fetal biometry or Doppler studies were excluded from the analysis of ultrasound factors. Participants were followed prospectively, with pregnancy outcome data and infant measurements recorded by research midwives, usually within 72 hours of birth.
Outcome measures
All-SGA was defined as birthweight <10th customised centile, adjusted for maternal height, booking weight, ethnicity, delivery gestation and infant sex.[24] Normotensive-SGA was defined as birth of an SGA infant where the mother did not develop hypertension, and Hypertensive-SGA defined as birth of an SGA infant where the mother had developed gestational hypertension or preeclampsia and/or had exhibited mild chronic hypertension.7
Definitions
Gestational hypertension: systolic BP≥140 mmHg and/or diastolic BP ≥90mmHg on at least 2 occasions 4 hours apart after 20 weeks’, before the onset of labour. Preeclampsia: gestational hypertension or postpartum hypertension (as defined above, but developing for the first time after delivery) in association with proteinuria (24 hour urinary protein ≥ 300 mg, or spot urine protein: creatinine ratio ≥ 30 mg/mmol, or urine dipstick protein ≥ 2+) or any multi-system complication of preeclampsia.[23, 25] Mild chronic hypertension: systolic BP of 140–159 mmHg and/or diastolic BP 90–99 mmHg, on more than one reading, first identified at the 15±1 or 20±1 weeks’ SCOPE visit. No participants had recognised or treated hypertension before pregnancy. Non-SGA referred to all women who did not have SGA babies. This group included pregnancies with other complications such as spontaneous preterm birth or preeclampsia without SGA.
Datasets
To allow for model generalization, data was partitioned into a Training set for model fitting and a Validation set for empirical validation. A 2:1 ratio was achieved by randomly splitting the total dataset stratified by geographical areas of Australasia and Europe. The datasets were checked for major discrepancies in SCOPE centre and rates of SGA.
Clinical and ultrasound variables
Details of clinical and ultrasound variable selection and the variable reduction process have previously been reported.[11] Details of clinical variables used in the SGA models are available as supplementary material (Table A in S1 Appendix).
Biomarkers
Fifty three biomarkers were selected based on either à priori knowledge of a biological role in: i) placentation, ii) angiogenesis or inflammation, iii) an association with preeclampsia, or iv) involvement in glucose or lipid metabolism. A full list of all but seven of the biomarkers, details of ELISA methodologies and biomarker data transformation methodology has previously been published.[26] The additional seven biomarkers included adiponectin, total cholesterol, HDL-cholesterol, insulin, LDL-cholesterol, human placental growth hormone, and triglycerides. Details of these biomarkers and ELISA methodologies are included as supplementary material (S1 Appendix and Table B in S1 Appendix).
Statistical analysis
SAS (version 9.3) Cary, N.C. was used for statistical analyses. The comparison group for All-SGA was Not-SGA, for ‘Normotensive-SGA’ was ‘Not Normotensive-SGA’ (all women who did not have ‘Normotensive-SGA’ including those with ‘Hypertensive-SGA’), and for ‘Hypertensive-SGA’ the comparison group was ‘Not Hypertensive-SGA’ (all women who did not have ‘Hypertensive—SGA’ including those with ‘Normotensive-SGA’). Comparison of population characteristics and pregnancy outcomes was performed using Student’s t-test, analysis of variance (ANOVA), the Wilcoxon Rank Sum test or the χ2 test, as appropriate for data type. Comparisons of biomarker distributions were performed using t-tests on the log-transformed data, with p-values adjusted to control the False Discovery Rate.[27] Single variable logistic regression was then applied to each log-transformed biomarker, along with calculation of the Area under the Receiver Operating Characteristic curve (AUC).
Multivariable modelling
Single variable logistic regression for each SGA endpoint was used in the Training cohort to select biomarkers for potential inclusion in multivariable predictive models. A significance threshold for the adjusted p-values of 0.05 was used for variable selection. Distinct models were constructed per endpoint (All-SGA, Normotensive-SGA and Hypertensive-SGA) as follows: (1) biomarkers only measured at 15±1 weeks’ (2) clinical risk factors at 15±1 weeks’ (3) combination of biomarkers and clinical risk factors at 15±1 weeks’ (4) combinations of clinical risk factors (15±1 weeks’), biomarkers (15±1 weeks’) and ultrasound variables (20±1 weeks’).
The solely biomarker and clinical risk factor logistic regression models were constructed using backwards stepwise variable selection, starting from a model containing all available biomarker or clinical variables, respectively. Only biomarkers included in the ‘biomarker only’ model for the SGA endpoint were available for the combined logistic regression models. Similarly, only variables that remained in the multivariable logistic regression model using ‘clinical risk factors only’ for the SGA endpoint were available to the ‘combined biomarker and clinical risk factor’ models. Again, logistic regression models were constructed using backwards stepwise variable selection. Model performance was assessed in the Training and Validation datasets via calculation of AUC for each model, along with sensitivity, positive and negative predictive value, and positive and negative likelihood ratios at a 5% false positive rate (95% specificity).
Results
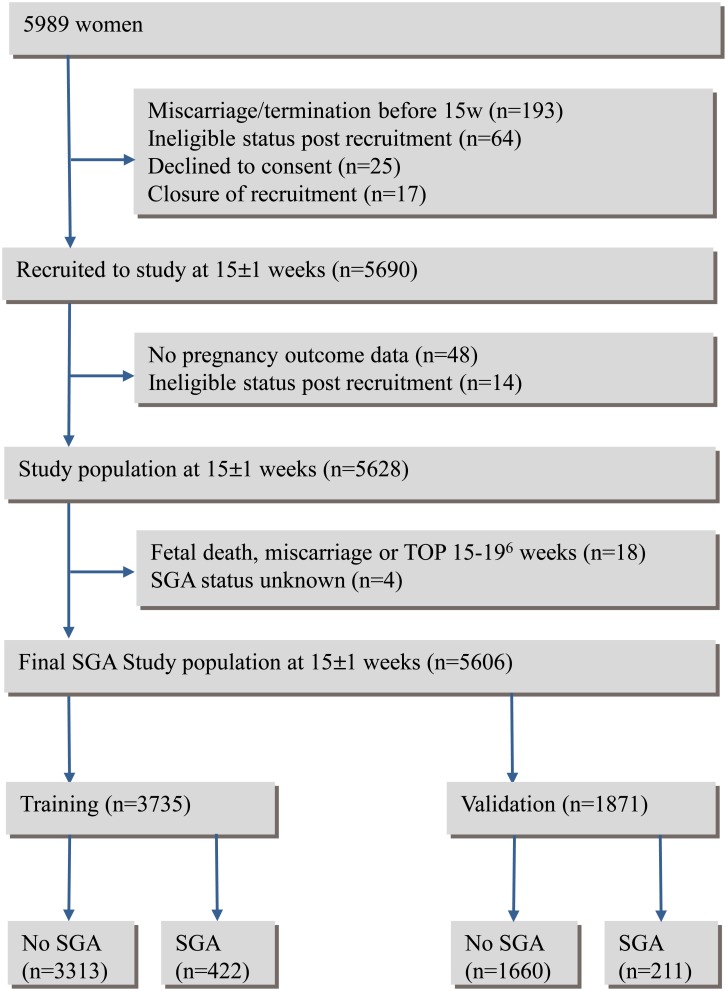
Consistent with our previous report, [11] 5690 healthy nulliparous women were recruited between November 2004 and February 2011 in Auckland, New Zealand, Adelaide, Australia, London, Leeds and Manchester, United Kingdom and Cork, Ireland and follow up was complete in 98.9% of participants. Our final study population with SGA data available was 5606. (Fig 1).
Fig 1. Flow chart of study population.
The data were divided into a Training set for model fitting (n = 3735) and a Validation set (n = 1871) (Fig 1). Of the 422 (11%) infants in the Training database who were SGA by customized centiles (All-SGA), 313 (8%) were born to normotensive mothers (Normotensive-SGA) and 109 (3%) to hypertensive mothers (Hypertensive-SGA). In the Validation database, 211 (11%) infants were SGA of whom 152 (8%) were Normotensive-SGA and 59 (3%) Hypertensive-SGA. Comparing Training and Validation sets, amongst the Hypertensive-SGA pregnancies, 44 (40%) and 26 (44%) women respectively had preeclampsia; 63 (58%), and 33 (56%) had gestational hypertension; 2 (2%) and none had mild chronic hypertension alone.
The baseline characteristics and pregnancy outcomes of the women who had SGA infants are compared with those with non-SGA infants in Table 1. Women with SGA infants were less likely to be primigravid, more likely to be single, less likely to be employed, more likely to have lower socioeconomic status, twice as likely to smoke and less likely to have a normal BMI than women with non-SGA pregnancies. They also reported lower mean birthweight and had higher systolic and diastolic blood pressures at 15±1 weeks’. They had a threefold increase in preterm delivery and higher rates of perinatal death than mothers of non-SGA infants.
Table 1. Study Population Characteristics at 15 ±1 Weeks’ and Pregnancy Outcome in the Total SGA Cohort (N = 5606).
| Non-SGA | All-SGA | p-value | |
|---|---|---|---|
| N = 4973 | N = 633 | ||
| Maternal Characteristics | |||
| Ethnicity | 0.54 | ||
| • Caucasian | 4481 (90) | 564 (89) | |
| • Maori or Pacific Islander* | 100 (2) | 13 (2) | |
| • Indian | 115 (2) | 19 (3) | |
| • Asian | 152 (3) | 16 (3) | |
| • Other† | 125 (3) | 21 (3) | |
| Primigravid | 3853 (78) | 466 (74) | 0.03 |
| Single | 458 (9) | 79 (13) | 0.009 |
| No paid employment | 708 (14) | 118 (19) | 0.003 |
| <12 years education | 1858 (37) | 258 (41) | 0.10 |
| Smoking status at 15 wks | <0.0001 | ||
| • Non smoker | 3821 (77) | 428 (68) | |
| • Ceased smoking before15wks | 669 (13) | 84 (13) | |
| • Current smoker | 483 (10) | 121 (19) | |
| BMI category | 0.002 | ||
| • <20.0 | 352 (7) | 50 (8) | |
| • 20.0–24.9 | 2518 (51) | 276 (44) | |
| • 25.0–29.9 | 1386 (28) | 186 (29) | |
| • ≥30 | 717 (14) | 121 (19) | |
| Maternal Characteristics | |||
| BMI (kg/m2) | 25.2 (4.8) | 25.9 (5.5) | 0.004 |
| Maternal age (y) | 28.7 (5.5) | 28.6 (5.8) | .67 |
| Socio-economic index | 42 (17) | 40 (16) | .006 |
| Maternal birthweight (g) | 3157 (908) | 2960 (946) | <.0001 |
| Systolic BP (mmHg) | 107 (10) | 108 (11) | <.0001 |
| Diastolic BP (mmHg) | 65 (8) | 66 (9) | .0002 |
| Pregnancy Outcome | |||
| Birthweight (g) | 3504 (505) | 2609 (578) | <.0001 |
| Gestational age at delivery (wks) | 39.8 (1.9) | 38.8 (3.5) | <.0001 |
| Total preterm births (<37wks) | 257 (5) | 94 (15) ‡ | <.0001 |
| Admitted to neonatal unit | 504 (10) | 143 (23) | <.0001 |
| Perinatal deaths§ | 16 (0.3) | 12 (2) | <.0001 |
| Hypertensive Pregnancy¶ | 592 (12) | 168 (27) | <.0001 |
Results expressed as N (%) or mean (SD) as appropriate;
* includes 71 Maori and 42 Pacific Islanders;
† includes 23 Australian Aborigines.
‡ 41 (8.8%) of Normotensive-SGA and 53 (31.5%) of Hypertensive-SGA
§ Rate/1000 births
¶ Hypertensive pregnancy defined as preeclampsia, gestational hypertension or mild chronic hypertension
Mean plasma biomarker concentrations (measured at 15±1 weeks’), results of univariable and multivariable analyses and AUCs for those biomarkers significantly associated with SGA, and the sub-phenotypes of SGA, are shown in Table 2. For All-SGA, eight biomarkers were associated with SGA after standard univariable analysis, with five remaining associated after controlling for the False Discovery Rate. The AUCs for these individual biomarkers was poor. After multivariable analysis, using Wilcoxon Rank Sum test, with p-values adjusted to control the False Discovery Rate, only two remained significantly associated with All-SGA in the reduced model: pregnancy-associated plasma protein A (PAPP-A) and vascular endothelial growth factor receptor-1 (VEGFR1) with AUC 0.60 (0.57–0.63).
Table 2. Univariable Analysis and AUC of Individual Biomarkers Measured at 15 ± 1 Weeks’ Gestation Comparing SGA Groups with Respective Controls.
| Biomarker | Controls | SGA Group | p-value* | q-value† | Univariable AUC (95% CI) | Reduced |
|---|---|---|---|---|---|---|
| Multivariable Model | ||||||
| p-value | ||||||
| ALL-SGA | ||||||
| Cystatin C, mg/mL | 1873 (1501–2343) | 1888 (1500–2461) | .01 | .08 | 0.52 (0.49–0.55) | |
| MIF, ng/mL | 9.2 (8.0–11.6) | 9.0 (7.7–10.9) | .002 | .02 | 0.54 (0.51–0.57) | |
| PAI-2‡, ng/mL | 1.0 (0.8–1.3) | 0.95 (0.7–1.2) | .003 | .02 | 0.55 (0.52–0.58) | |
| PAPP-A‡, ng/mL | 1.0 (0.6–1.8) | 0.8 (0.5–1.5) | <.001 | .002 | 0.58 (0.55–0.61) | 0.004 |
| PlGF‡, ng/mL | 1.0 (0.6–1.7) | 0.95 (0.5–1.7) | .009 | .06 | 0.54 (0.51–0.57) | |
| VEGFR1, ng/mL | 0.34 (0.21–0.54) | 0.28 (0.18–0.45) | <.001 | .002 | 0.58 (0.55–0.61) | 0.021 |
| Insulin, ng/mL | 16.5 (9.7–27.7) | 15.1 (8.7–25.5) | .009 | .06 | 0.53 (0.50–0.56) | |
| Triglycerides‡, mg/dL | 0.99 (0.8–1.2) | 1.02 (0.8–1.3) | <.001 | .002 | 0.52 (0.49–0.55) | |
| AUC = 0.59 (0.56–0.62) | ||||||
| NORMOTENSIVE-SGA | ||||||
| Caspase 3, ng/mL | 2.4 (1.4–4.2) | 2.0 (1.2–3.4) | .001 | .023 | 0.56 (0.53–0.59) | 0.045 |
| MIF, ng/mL | 9.2 (7.9–11.6) | 9.0 (7-7-10.9) | .004 | .06 | 0.54 (50.0–0.57) | |
| PAPP-A‡, ng/mL | 1.0 (0.6–1.8) | 0.8 (0.5–1.6) | .0001 | .003 | 0.57 (0.53–0.60) | 0.032 |
| VEGFR1, ng/mL | 0.27 (0.18–0.54) | 0.34 (0.21–0.42) | <.0001 | .003 | 0.59 (0.55–0.62) | 0.008 |
| AUC = 0.60 (0.57–0.63) | ||||||
| HYPERTENSIVE-SGA | ||||||
| PAPP-A‡, ng/mL | 1.0 (0.6–1.8) | 0.7 (0.4–1.5) | .001 | .006 | 0.59 (0.53–0.65) | 0.025 |
| PlGF‡, ng/mL | 1.0 (0.6–1.7) | 0.7 (0.3–1.3) | <.0001 | .002 | 0.60 (0.54–0.66) | 0.001 |
| Triglycerides‡, mg/dL | 1.0 (0.8–1.3) | 1.1 (0.9–1.5) | <.0001 | .002 | 0.61 (0.55–0.67) | 0.0001 |
| AUC = 0.66 (0.60–0.71) | ||||||
AUC, area under the receiver operating curve; CI, confidence interval; MIF, macrophage migration inhibitory factor; PAI-2, plasminogen activator inhibitor 2; PAPP-A, pregnancy-associated plasma protein A; PlGF, placental growth factor; VEGFR, vascular endothelial growth factor receptor;
Biomarker concentrations are shown as median (interquartile range);
* Based on Analysis of Log Transformed Data
† Based on False Discovery Rate
‡ Based on MoM Data
For Normotensive-SGA, Caspase-3 remained significant in the multivariable model together with PAPP-A and VEGFR1 with an AUC of 0.60 (0.57–0.63). For Hypertensive-SGA, PAPP-A, PlGF and Triglycerides were significantly discriminatory in univariable analysis after adjustment for False Discovery Rate. All remained significant after multivariable analysis, with an AUC of 0.66 (0.60–0.71).
The addition of biomarker data to clinical risk factors led to a small increment in AUC for All-SGA (2% in Training and 1% in Validation datasets) with a further modest increase with addition of ultrasound characteristics (6% and 5% increment for Training and Validation datasets respectively) with a final AUC for the Training dataset of 0.74 (0.71–0.76) and Validation dataset of 0.69 (0.66–0.73). Small incremental increases in AUC occurred in the Normotensive-SGA and Hypertensive-SGA prediction models with the addition of biomarker and ultrasound variables to clinical data. Final AUCs (which included ultrasound variables) were similar for All-SGA and Normotensive-SGA with final AUCs for Hypertensive-SGA approximately 10% higher (Table 3).
Table 3. AUCs from Multivariable Models to Predict SGA, Normotensive-SGA and Hypertensive-SGA.
| All-SGA | Normotensive-SGA | Hypertensive-SGA | ||||
|---|---|---|---|---|---|---|
| AUC (95% CI) | AUC (95% CI) | AUC (95% CI) | ||||
| Variables in Model | Training | Validation | Training | Validation | Training | Validation |
| 15 week Clinical* | 0.66 (0.64–0.69) | 0.63 (0.59–0.67) | 0.66 (0.63–0.70) | 0.61 (0.57–0.66) | 0.76 0.72–0.81) | 0.76 (0.70–0.82) |
| 15 week Clinical* +Biomarkers† | 0.68 (0.65–0.71) | 0.64 (0.60–0.68) | 0.69 (0.66–0.72) | 0.61 (0.56–0.66) | 0.78 (0.73–0.82) | 0.80 (0.75–0.86) |
| 15 week Clinical* +Biomarkers† | ||||||
| +20 week Ultrasound‡ | 0.74 (0.71–0.76) | 0.69 (0.66–0.73) | 0.73 (0.70–0.76) | 0.68 (0.64–0.73) | 0.82 (0.78–0.86) | 0.84 (0.78–0.89) |
AUC, area under the receiver operating curve; CI, confidence interval;
* Clinical: All-SGA (family history of coronary heart disease, maternal birthweight, >12 months to conceive, attending university, smoking, proteinuria, vigorous exercise, diastolic BP ≥80mmHg, recreational walking, Rhesus negative blood group, random glucose); Normotensive-SGA: (maternal birthweight, attending university, smoking, vigorous exercise, recreational walking, Rhesus negative blood group, random glucose): Hypertensive-SGA: (>12 months to conceive, family history of metabolic syndrome, family history of coronary heart disease, low fruit consumption, binge drinking, maternal birthweight, body mass index, systolic blood pressure ≥120mmHg, diastolic BP ≥80mmHg) (12)
† Biomarkers: All-SGA (PAPP-A, pregnancy-associated plasma protein A; PlGF, placental growth factor); Normotensive-SGA: (Caspase 3; PAPP-A; VEGFR1, vascular endothelial growth factor receptor); Hypertensive-SGA: (PAPP-A; PlGF; Triglycerides)
‡ Ultrasound: All-SGA and Normotensive-SGA: (head and abdominal circumference, uterine resistance index); Hypertensive-SGA: (uterine resistance index)
Table 4 summarizes the screening test characteristics of the final models combining clinical, biomarker and ultrasound variables in the Validation and Training datasets for the SGA groups at a 5% false positive rate.
Table 4. Screening Test Characteristics, at 95% Specificity, for All-SGA, Normotensive-SGA and Hypertensive-SGA of the Multivariable Models Based on Combining Clinical Risk Factors, Biomarkers and Ultrasound Data.
| Clinical Group | Pretest Prevalence | Sensitivity | Positive Predictive Value | Negative Predictive Value | PositiveLikelihood Ratio | Negative Likelihood Ratio |
|---|---|---|---|---|---|---|
| All-SGA | ||||||
| Training | 11.3% | 21 (17, 25) | 35 (29, 41) | 91 (90, 92) | 4.20 (3.29, 5.36) | 0.83 (0.79, 0.87) |
| Validation | 19 (14, 25) | 32 (23, 40) | 91 (89, 92) | 3.86 (2.69, 5.53) | 0.85 (0.79, 0.91) | |
| Normotensive-SGA | ||||||
| Training | 8.4% | 21 (17, 26) | 28 (22, 34) | 93 (92, 94) | 4.22 (3.24, 5.52) | 0.83 (0.78, 0.88) |
| Validation | 16 (9, 22) | 20 (13, 28) | 93 (92, 94) | 3.09 (1.98, 4.83) | 0.89 (0.83, 0.96) | |
| Hypertensive-SGA | ||||||
| Training | 2.9% | 28 (19, 38) | 13 (8, 18) | 98 (98, 99) | 7.02 (5.20, 9.49) | 0.68 (0.59, 0.79) |
| Validation | 42 (29, 55) | 20 (13, 27) | 98 (97, 99) | 8.38 (5.81, 12.11) | 0.61 (0.49, 0.76) | |
Discussion
We present a series of models, developed in a large, well-phenotyped international pregnancy cohort of low-risk nulliparous women, which combine biomarkers, clinical and ultrasound data to predict the risk of SGA and its different phenotypes. We have previously performed a detailed analysis of early pregnancy clinical risk factors combined with ultrasound parameters at 20±1 weeks’ gestation in this cohort that resulted in modest performance for the prediction of SGA (AUC of 0.69 for All-SGA).[11] We hypothesized that early pregnancy prediction of SGA would be improved by addition of biomarkers, in line with previous studies.[18] However, despite the selection of the biomarkers for known associations, no single biomarker, or combination of biomarkers, substantially improved the performance of the clinical/ultrasound-based risk model. As the phenotypes of SGA have low prevalence (from 2%-14% of the antenatal population), a clinically useful test generally needs to have a high positive LR (> 10) and low negative LR (< 0.10).[28] The performance of our models for the prediction of All-SGA and its phenotypes in healthy nulliparous women, by these stringent criteria, is insufficient for application in clinical practice.
Interesting insights were provided into possible biological determinants of the different SGA phenotypes. PAPP-A, a reduction in which was common to all models, is a syncytiotrophoblast-derived metalloprotease, which binds to and cleaves insulin-like growth factor binding proteins IGFBP- 3 and IGFBP-4.[29] These binding proteins, and cleavage products, have reduced affinity for the IGFs, thereby increasing biologically available IGFs. This increases placental growth and function, which enhances nutrient transport to the fetus.[30, 31] Low PAPP-A, results in less bioavailable IGFs and decreased growth.[32] Our findings are consistent with several large population-based screening studies [33–35] and a recent meta-analysis.[17]
The majority of SGA infants (73.8%) were born to mothers who remained normotensive in pregnancy and hence there is substantial overlap between All-SGA and Normotensive-SGA clinical risk predictors [11] which is mirrored by the biomarker data. In addition to PAPP-A, raised VEGFR1 was common to All-SGA and Normotensive-SGA. VEGF is involved in vasculogenesis and angiogenesis in early placental development,[36] and has both membrane bound and circulating soluble forms (soluble fms-like tyrosine kinase-1 or sFlt-1). sFlt-1 binds and reduces free levels of VEGF, thereby blunting the pro-angiogenic effect reducing fetal growth.
The performance of each of our models, though comparable with reports by others,[37] was insufficient to warrant introduction into clinical practice. Additional information in later gestation may be necessary to improve prediction of risk for SGA. Arguably, the clinical need for an accurate screening test is greatest in Normotensive-SGA; unlike Hypertensive-SGA, these pregnancies often lack overt clinical signs to alert the clinician to the at-risk fetus.
Hypertensive-SGA comprised of 96/168 (57%) mothers with gestational hypertension and 70/168 (42%) with preeclampsia.[25] The group with gestational hypertension and SGA would now meet the updated criteria for definition of preeclampsia.[38] Overall, 31.5% of women with Hypertensive-SGA were delivered at < 37 weeks highlighting the combination of fetal and maternal manifestations of defective early placentation. In line with this, a reduction in placental growth factor (PlGF) was common to models for preeclampsia and Hypertensive-SGA.[26] PlGF, a member of the VEGF family, is an angiogenic, pro-inflammatory factor produced by trophoblast cells, with a central role in the regulation of VEGF–dependent angiogenesis.[39] Consistent with our results, recent evidence suggests that low PlGF has potential to be incorporated in screening for early-onset disease, which is often accompanied by uteroplacental dysfunction and SGA.[14, 26] Another interesting finding was the role of Caspase-3, important in apoptosis, in normotensive-SGA and not found in Hypertensive-SGA. Apoptosis is important in remodeling of developing tissue, including the placenta as well as pathological conditions.[40, 41] Its role in the etiology of placental development and disease needs to be explored.
Strengths of the study include the unique composition of the SCOPE cohort, which aimed to predict late pregnancy complications in low-risk nulliparous women who comprise approximately 40% of births in many Western countries.[42–45] The biobank was prospectively collected and curated using a rigorous protocol and pre-specified clinical phenotyping. Stronger prediction of SGA has been reported in some previous studies,[18,46] but these were typically conducted in heterogeneous populations including women with underlying medical conditions [18] or where the control population comprised women with uncomplicated pregnancies.[46] In both scenarios, screening performance can be overestimated.
Limitations include the ethnic homogeneity, more than 90% of participants being Caucasian. The low incidence of SGA subtypes (e.g. Hypertensive-SGA) may have led to models being over-fitted. Moreover, SCOPE’s primary aim [26] was to screen and select biomarkers for prediction of preeclampsia, and prediction of SGA was a planned secondary analysis. Other biomarkers for future consideration might include glycogen phosphorylase isoenzyme BB [47] or beta-hCG.[34,48] Metabolomic analyses warrant further investigation as we recently demonstrated in a case-control study that 19 metabolites combined to give an AUC for SGA of 0.9.[49] Finally, the SCOPE study was designed to generate early pregnancy screening tests and did not include a third-trimester blood sample or ultrasound scan. For early pregnancy prediction of SGA, our models are inadequate for clinical use. However, PlGF (and possibly other biomarkers) may have greater utility closer to disease onset [50–52] and there is potential for evaluation of a two-stage test with those who screen positive in early pregnancy receiving low dose aspirin [53] and late pregnancy screening with PlGF and/or a growth scan at 36 weeks.[54] Sovio et al [54] reported that 57% of SGA infants were identified by ultrasound performed in a research setting at 36 weeks of gestation whereas scanning earlier in the third trimester is less reliable for detection of SGA.[55] An algorithm whereby women who have moderate or high risk screening for SGA at 19–24 weeks are selectively offered further third trimester scanning at 32 and or 36 weeks has been proposed and now requires validation.[56]
Conclusions
Modest prediction of SGA was obtained by combining early pregnancy clinical risk factors, biomarkers and biometry and Doppler data from the 20-weeks’ anatomy scan in healthy nulliparous women. Addition of biomarker data to our previous clinical and ultrasound models did not improve performance. There is an urgent need to develop reliable tools for prediction of SGA, especially the majority group of Normotensive-SGA, who are usually not detected until after birth. Such tools could reduce perinatal morbidity and mortality. This paper gives new insights into the potential molecular mechanisms of placental and hypertensive disease in pregnancy.
Supporting Information
(DOCX)
Acknowledgments
We would like to thank the pregnant women who participated in the SCOPE Study, the SCOPE Country Project Managers Mrs D Healy, University of Adelaide, Mrs A Briley, Kings College London, and Mrs N Murphy and Mrs E Snapes, University College Cork, Miss Eliza Chan, University of Auckland, for development of the databases and Dr Mik Black, University of Otago, for creating the training and validation databases. Membership of the SCOPE consortium is available from SCOPE@ucc.ie.
Data Availability
The SCOPE study which commenced recruitment in 2004 did not seek specific consent from participants for sharing their data publicly. However, the SCOPE Consortium Scientific Advisory Board is happy to receive and consider applications from interested parties who can email the chairperson, Professor Louise Kenny at <L.Kenny@ucc.ie>. Applicants will be asked to complete a Research Application Form specifying details for their planned study which will then be reviewed by the SCOPE Scientific Advisory Board. The SCOPE Consortium is keen to promote collaboration among researchers and to see our unique SCOPE database and pregnancy biobank used in studies which meet our ethics and consenting process. Therefore, we are a member of the MotherChild Link Registry. http://www.linkregistry.org/search.aspx.
Funding Statement
The New Zealand SCOPE study was funded by the New Enterprise Research Fund, Foundation for Research Science and Technology; Health Research Council (04/198) http://www.hrc.govt.nz/; Evelyn Bond Fund, Auckland District Health Board Charitable Trust (http://www.adhb.govt.nz/researchoffice/A+Grant-Cmtee/ADHB_Grants_Committee.htm#ABOUT_THE_ADHB_CHARITABLE_TRUST), The Australian SCOPE study was funded by the Premier’s Science and Research Fund, South Australian Government (http://www.statedevelopment.sa.gov.au/science/premiers-research-and-industry-fund), The Irish SCOPE study was funded by the Health Research Board of Ireland (CSA/2007/2; http://www.hrb.ie), The UK SCOPE study was funded by National Health Service NEAT Grant (Neat Grant FSD025), Biotechnology and Biological Sciences Research council (www.bbsrc.ac.uk/funding; GT084) and University of Manchester Proof of Concept Funding (University of Manchester); Guy’s and St. Thomas’ Charity (King’s College London) and Tommy’s charity (http://www.tommys.org/; King’s College London and University of Manchester); and Cerebra UK (www.cerebra.org.uk; University of Leeds). The biomarker study was funded by an unrestricted research grant from Alere Inc, San Diego, CA (www.alere.com), to the universities in the SCOPE consortium. L.C. Kenny is supported by a Science Foundation Ireland Program Grant for INFANT (12/RC/2272). C.T. Roberts is supported by a National Health and Medical Research Council (NHMRC) Senior Research Fellowship GNT1020749. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Gardosi J, Kady SM, McGeown P, Francis A, Tonks A. Classification of stillbirth by relevant condition at death (ReCoDe): population based cohort study. BMJ. 2005;331(7525):1113–7. 10.1136/bmj.38629.587639.7C [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.PMMRC. Sixth Annual Report of the Perinatal and Maternal Mortality Review Committee: Reporting mortality 2010. Wellington: Health Quality & Safety Commission; 2012.
- 3.Barker DJP, Osmond C, Forsen TJ, Kajantie E, Eriksson JG. Maternal and social origins of hypertension. Hypertension. 2007;50(3):565–71. 10.1161/HYPERTENSIONAHA.107.091512 [DOI] [PubMed] [Google Scholar]
- 4.Baschat AA., Neurodevelopment following fetal growth restriction and its relationship with antepartum parameters of placental dysfunction. Ultrasound Obstet Gynecol. 2011;37(5):501–14. 10.1002/uog.9008 [DOI] [PubMed] [Google Scholar]
- 5.MacLennan AH, Thompson SC, Gecz J. Cerebral palsy: causes, pathways, and the role of genetic variants. Am J Obstet Gynecol. 2015;213(6):779–88. 10.1016/j.ajog.2015.05.034 [DOI] [PubMed] [Google Scholar]
- 6.Parra-Saavedra M, Crovetto F, Triunfo S, Savchev S, Peguero A, Nadal A, et al. Placental findings in late-onset SGA births without Doppler signs of placental insufficiency. Placenta. 2013;34(12):1136–41. 10.1016/j.placenta.2013.09.018 [DOI] [PubMed] [Google Scholar]
- 7.McCowan LME, Roberts CT, Dekker GA, Taylor RS, Chan EHY, Kenny LC, Baker PN, et al. Risk factors for small-for-gestational-age infants by customised birthweight centiles: data from an international prospective cohort study. BJOG. 2010;117(13):1599–607. 10.1111/j.1471-0528.2010.02737.x [DOI] [PubMed] [Google Scholar]
- 8.Roex A, Nikpoor P, van Eerd E, Hodyl N, Dekker G. Serial plotting on customised fundal height charts results in doubling of the antenatal detection of small for gestational age fetuses in nulliparous women. Aust N Z J Obstet Gynaecol. 2012;52(1):78–82. 10.1111/j.1479-828X.2011.01408.x [DOI] [PubMed] [Google Scholar]
- 9.Wright J, Morse K, Kody S, Francis A. Audit of fundal height measurement plotted on customised growth charts. MIDIRS Midwifery Digest. 2006;16(3):341–5. [Google Scholar]
- 10.Lindqvist PG, Molin J. Does antenatal identification of small-for-gestational age fetuses significantly improve their outcome? Ultrasound Obstet Gynecol. 2005;25(3):258–64. 10.1002/uog.1806 [DOI] [PubMed] [Google Scholar]
- 11.McCowan LM, Thompson JM, Taylor RS, North RA, Poston L, Baker PN, et al. Clinical prediction in early pregnancy of infants small for gestational age by customised birthweight centiles: findings from a healthy nulliparous cohort. PLoS ONE. 2013;8(8):e70917 10.1371/journal.pone.0070917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Groom KM, North RA, Poppe KK, Sadler L, McCowan LM. The association between customised small for gestational age infants and pre-eclampsia or gestational hypertension varies with gestation at delivery. BJOG. 2007;114(4):478–84. 10.1111/j.1471-0528.2007.01277.x [DOI] [PubMed] [Google Scholar]
- 13.Foidart JM, Munaut C, Chantraine F, Akolekar R, Nicolaides KH. Maternal plasma soluble endoglin at 11–13 weeks' gestation in pre-eclampsia. Ultrasound Obstet Gynecol. 2010;35(6):680–7. 10.1002/uog.7621 [DOI] [PubMed] [Google Scholar]
- 14.Myers JE, Kenny LC, McCowan LM, Chan EH, Dekker GA, Poston L, et al. Angiogenic factors combined with clinical risk factors to predict preterm pre-eclampsia in nulliparous women: a predictive test accuracy study. BJOG. 2013;120(10):1215–23. 10.1111/1471-0528.12195 [DOI] [PubMed] [Google Scholar]
- 15.Myers JE, Tuytten R, Thomas G, Laroy W, Kas K, Vanpoucke G, et al. Integrated proteomics pipeline yields novel biomarkers for predicting preeclampsia. Hypertension. 2013;61(6):1281–8. 10.1161/HYPERTENSIONAHA.113.01168 [DOI] [PubMed] [Google Scholar]
- 16.Poon LCY, Syngelaki A, Akolekar R, Lai J, Nicolaides KH. Combined screening for preeclampsia and small for gestational age at 11–13 weeks. Fetal Diagn Ther. 2013;33(1):16–27. 10.1159/000341712 [DOI] [PubMed] [Google Scholar]
- 17.Zhong Y, Zhu F, Ding Y. Serum screening in first trimester to predict pre-eclampsia, small for gestational age and preterm delivery: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2015;15:191 10.1186/s12884-015-0608-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karagiannis G, Akolekar R, Sarquis R, Wright D, Nicolaides KH. Prediction of small-for-gestation neonates from biophysical and biochemical markers at 11–13 weeks. Fetal Diagn Ther. 2011;29(2):148–54. 10.1159/000321694 [DOI] [PubMed] [Google Scholar]
- 19.Anderson NH, Sadler LC, McKinlay CJ, McCowan LM. INTERGROWTH 21st versus Customized Birthweight Standards For Identification Of Perinatal Mortality And Morbidity. Am J Obstet Gynecol. 2015. [DOI] [PubMed] [Google Scholar]
- 20.Gardosi J, Clausson B, Francis A. The value of customised centiles in assessing perinatal mortality risk associated with parity and maternal size. BJOG. 2009;116(10):1356–63. 10.1111/j.1471-0528.2009.02245.x [DOI] [PubMed] [Google Scholar]
- 21.McCowan L, Harding J, Stewart A. Customised birthweight centiles predict SGA pregnancies with perinatal morbidity. Br J Obstet Gynaecol. 2005;112:1026–33. [DOI] [PubMed] [Google Scholar]
- 22.North RA, McCowan LME, Dekker GA, Poston L, Chan EHY, Stewart AW, et al. Clinical risk prediction for pre-eclampsia in nulliparous women: development of model in international prospective cohort. BMJ. 2011;342:d1875 10.1136/bmj.d1875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Australian NZCTR. ACTRN12607000551493: Screening nulliparous women to identify the combinations of clinical risk factors and/or biomarkers required to predict preeclampsia, small for gestational age babies and spontaneous preterm birth. Sydney (NSW): Australian New Zealand Clinical Trials Registry: The University of Sydney (Australia); 2007 [cited 2007 26/10/2007]. www.anzctr.org.au/trial_view.aspx?ID=82254. 2007.
- 24.McCowan L, Stewart AW, Francis A, Gardosi J. A customised birthweight centile calculator developed fo1r a New Zealand population. Aust N Z J Obstet Gynaecol. 2004;44(5):428–31. 10.1111/j.1479-828X.2004.00272.x [DOI] [PubMed] [Google Scholar]
- 25.Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy 2001;20(1):IX–XIV. [DOI] [PubMed] [Google Scholar]
- 26.Kenny LC, Black MA, Poston L, Taylor R, Myers JE, Baker PN, et al. Early pregnancy prediction of preeclampsia in nulliparous women, combining clinical risk and biomarkers: the Screening for Pregnancy Endpoints (SCOPE) international cohort study. Hypertension. 2014;64(3):644–52. 10.1161/HYPERTENSIONAHA.114.03578 [DOI] [PubMed] [Google Scholar]
- 27.Schwarz GE. Estimating the dimension of a model. Ann Stat. 1978;6:461–4. [Google Scholar]
- 28.Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ. 2004;329(7458):168–9. 10.1136/bmj.329.7458.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bonno M, Oxvig C, Kephart GM, Wagner JM, Kristensen T, Sottrup-Jensen L, et al. Localization of pregnancy-associated plasma protein-A and colocalization of pregnancy-associated plasma protein-A messenger ribonucleic acid and eosinophil granule major basic protein messenger ribonucleic acid in placenta. Lab Invest. 1994;71(4):560–6. [PubMed] [Google Scholar]
- 30.Roberts CT, Owens JA, Sferruzzi-Perri AN. Distinct actions of insulin-like growth factors (IGFs) on placental development and fetal growth: lessons from mice and guinea pigs. Placenta. 2008;29 Suppl A:S42–7. [DOI] [PubMed] [Google Scholar]
- 31.Sferruzzi-Perri AN, Owens JA, Pringle KG, Roberts CT. The neglected role of insulin-like growth factors in the maternal circulation regulating fetal growth. J Physiol (Lond). 2011;589(Pt 1):7–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Conover CA, Bale LK, Overgaard MT, Johnstone EW, Laursen UH, Fuchtbauer EM, et al. Metalloproteinase pregnancy-associated plasma protein A is a critical growth regulatory factor during fetal development. Development. 2004;131(5):1187–94. 10.1242/dev.00997 [DOI] [PubMed] [Google Scholar]
- 33.Dugoff L, Hobbins JC, Malone FD, Porter TF, Luthy D, Comstock CH, et al. First-trimester maternal serum PAPP-A and free-beta subunit human chorionic gonadotropin concentrations and nuchal translucency are associated with obstetric complications: a population-based screening study (the FASTER Trial). Am J Obstet Gynecol. 2004;191(4):1446–51. 10.1016/j.ajog.2004.06.052 [DOI] [PubMed] [Google Scholar]
- 34.Krantz D, Goetzl L, Simpson JL, Thom E, Zachary J, Hallahan TW, et al. Association of extreme first-trimester free human chorionic gonadotropin-beta, pregnancy-associated plasma protein A, and nuchal translucency with intrauterine growth restriction and other adverse pregnancy outcomes. Am J Obstet Gynecol. 2004;191(4):1452–8. 10.1016/j.ajog.2004.05.068 [DOI] [PubMed] [Google Scholar]
- 35.Smith GC, Stenhouse EJ, Crossley JA, Aitken DA, Cameron AD, Connor JM. Early pregnancy levels of pregnancy-associated plasma protein a and the risk of intrauterine growth restriction, premature birth, preeclampsia, and stillbirth. J Clin Endocrinol Metab. 2002;87(4):1762–7. 10.1210/jcem.87.4.8430 [DOI] [PubMed] [Google Scholar]
- 36.Ahmad S, Ahmed A. Elevated placental soluble vascular endothelial growth factor receptor-1 inhibits angiogenesis in preeclampsia. Circ Res. 2004;95(9):884–91. 10.1161/01.RES.0000147365.86159.f5 [DOI] [PubMed] [Google Scholar]
- 37.Crovetto F, Triunfo S, Crispi F, Rodriguez-Sureda V, Roma E, Dominguez C, et al. First trimester screening with specific algorithms for early and late onset fetal growth restriction. Ultrasound Obstet Gynecol. 2016. [DOI] [PubMed] [Google Scholar]
- 38.Tranquilli AL, Dekker G, Magee L, Roberts J, Sibai BM, Steyn W, et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens. 2014;4(2):97–104. [DOI] [PubMed] [Google Scholar]
- 39.Andraweera PH, Dekker GA, Roberts CT. The vascular endothelial growth factor family in adverse pregnancy outcomes. Hum Reprod Update. 2012;18(4):436–57. 10.1093/humupd/dms011 [DOI] [PubMed] [Google Scholar]
- 40.Cali U, Cavkaytar S, Sirvan L, Danisman N. Placental apoptosis in preeclampsia, intrauterine growth retardation, and HELLP syndrome: an immunohistochemical study with caspase-3 and bcl-2. Clin Exp Obstet Gynecol. 2013;40(1):45–8. [PubMed] [Google Scholar]
- 41.Endo H, Okamoto A, Yamada K, Nikaido T, Tanaka T. Frequent apoptosis in placental villi from pregnancies complicated with intrauterine growth restriction and without maternal symptoms. Int J Mol Med. 2005;16(1):79–84. [PubMed] [Google Scholar]
- 42.Infoshore. Total confinements by District Health Board by previous births Wellington, NZ: Statistics NZ; 2011. http://www.stats.govt.nz/infoshare/SelectVariables.aspx?pxID=3ca84481-6909-4556-97b5-c452f3187ad2
- 43.Li Z, Zeki R, Hilder L, Sullivan EA. Australian Mothers and Babies 2010; Perinatal statistics series no. 27. Cat. no. PER 57. Canberra, Australia: AIHW National Perinatal Epidemiology and Statistics Unit; 2012.
- 44.National Perinatal Reporting System. Perinatal Statistics Report 2010. Ireland, Division HRaI; 2012.
- 45.Office for National Statistics. Birth Statistics 2008, Series FM1 No.37. UK; 2009.
- 46.Triunfo S, Crovetto F, Scazzocchio E, Parra-Saavedra M, Gratacos E, Figueras F. Contingent versus routine third-trimester screening for late fetal growth restriction. Ultrasound Obstet Gynecol. 2016;47(1):81–8. 10.1002/uog.15740 [DOI] [PubMed] [Google Scholar]
- 47.McCarthy F, Doyle A, Khashan A, Kenny L. Altered Maternal Plasma Glycogen Phosphorylase Isoenzyme BB as a Biomarker for Preeclampsia and Small for Gestational Age. Reprod Sci. 2015:pii: 1933719115616495. [DOI] [PubMed] [Google Scholar]
- 48.Montanari L, Alfei A, Albonico G, Moratti R, Arossa A, Beneventi F, et al. The impact of first-trimester serum free beta-human chorionic gonadotropin and pregnancy-associated plasma protein A on the diagnosis of fetal growth restriction and small for gestational age infant. Fetal Diagn Ther. 2009;25(1):130–5. 10.1159/000207554 [DOI] [PubMed] [Google Scholar]
- 49.Horgan RP, Broadhurst DI, Walsh SK, Dunn WB, Brown M, Roberts CT, et al. Metabolic profiling uncovers a phenotypic signature of small for gestational age in early pregnancy. J Proteome Res. 2011;10(8):3660–73. 10.1021/pr2002897 [DOI] [PubMed] [Google Scholar]
- 50.Chaiworapongsa T, Romero R, Whitten AE, Korzeniewski SJ, Chaemsaithong P, Hernandez-Andrade E, et al. The use of angiogenic biomarkers in maternal blood to identify which SGA fetuses will require a preterm delivery and mothers who will develop pre-eclampsia. J Matern Fetal Neonatal Med 2016;29(8):1214–28. 10.3109/14767058.2015.1048431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chappell LC, Duckworth S, Seed PT, Griffin M, Myers J, Mackillop L, et al. Diagnostic accuracy of placental growth factor in women with suspected preeclampsia: a prospective multicenter study. Circulation. 2013;128(19):2121–31. 10.1161/CIRCULATIONAHA.113.003215 [DOI] [PubMed] [Google Scholar]
- 52.Griffin M, Seed PT, Webster L, Myers J, MacKillop L, Simpson N, et al. Diagnostic accuracy of placental growth factor and ultrasound parameters to predict the small-for-gestational-age infant in women presenting with reduced symphysis-fundus height. Ultrasound Obstet Gynecol. 2015;46(2):182–90. 10.1002/uog.14860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol. 2010;116(2 Pt 1):402–14. [DOI] [PubMed] [Google Scholar]
- 54.Sovio U, White IR, Dacey A, Pasupathy D, Smith GC. Screening for fetal growth restriction with universal third trimester ultrasonography in nulliparous women in the Pregnancy Outcome Prediction (POP) study: a prospective cohort study.[Erratum appears in Lancet. 2015 Nov 21;386(10008):2058]. Lancet. 2015;386(10008):2089–97. 10.1016/S0140-6736(15)00131-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reboul Q, Delabaere A, Cheng LZ, Nuyt AM, Wu Y, Chauleur C, et al. Prediction of small for gestational age neonates by third trimester fetal biometry and impact of ultrasound-delivery interval. Ultrasound Obstet Gynecol. 2016;6:6. [DOI] [PubMed] [Google Scholar]
- 56.Poon LC, Lesmes C, Gallo DM, Akolekar R, Nicolaides KH. Prediction of small-for-gestational-age neonates: screening by biophysical and biochemical markers at 19–24 weeks. Ultrasound Obstet Gynecol. 2015;46(4):437–45. 10.1002/uog.14904 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
The SCOPE study which commenced recruitment in 2004 did not seek specific consent from participants for sharing their data publicly. However, the SCOPE Consortium Scientific Advisory Board is happy to receive and consider applications from interested parties who can email the chairperson, Professor Louise Kenny at <L.Kenny@ucc.ie>. Applicants will be asked to complete a Research Application Form specifying details for their planned study which will then be reviewed by the SCOPE Scientific Advisory Board. The SCOPE Consortium is keen to promote collaboration among researchers and to see our unique SCOPE database and pregnancy biobank used in studies which meet our ethics and consenting process. Therefore, we are a member of the MotherChild Link Registry. http://www.linkregistry.org/search.aspx.