Abstract
Objective. To determine the impact of an interprofessional simulation using the SBAR (situation-background-assessment-recommendation/request) communication tool on pharmacy students’ self-perception of interprofessional competence and reactions towards interprofessional collaboration.
Design. Ninety-six pharmacy students participated in an interprofessional simulation within a required applications-based capstone course. Pharmacy students collaborated with nursing students on multiple patient cases in various settings using the SBAR communication tool over the telephone.
Assessment. Pharmacy students’ responses to all 20 items on the Interprofessional Collaborative Competency Attainment Survey (ICCAS) completed after participating in the simulation indicated significant positive changes. The themes identified in students’ reflection papers indicated the simulation was beneficial and student responses on satisfaction surveys were positive with a mean score of 4.2 on a 5-point Likert scale.
Conclusion. Implementation of an interprofessional simulation using the SBAR communication tool improved pharmacy students’ self-perception of interprofessional competence and attitudes toward interprofessional collaboration.
Keywords: interprofessional, communication, SBAR, simulation, pharmacy students
INTRODUCTION
Interprofessional practice and education (IPE) occurs when two or more students from different professions learn about, from, and with each other to enable collaboration and improve health outcomes.1 The Center for the Advancement of Pharmacy Education (CAPE) outcomes and the Accreditation Council for Pharmacy Education (ACPE) standards, which are both concerned with doctor of pharmacy (PharmD) degree programs, have incorporated IPE into their guiding documents.2,3 ACPE standard 11 encourages participation in interprofessional teams and IPE can help fulfill multiple CAPE domains, specifically subdomain 3.4 relating to interprofessional collaboration. In addition, the Interprofessional Education Collaborative (IPEC) developed core competencies for students in all health professions’ education to aid in breaking down the silos that exist in our current training models.4 There is increasing focus on realigning IPE with clinical practice redesign.5 This will help bridge the gap that can exist between education and practice in order to achieve the “Triple Aim” (improved patient experience of care, improved population outcomes, and reduced cost) in healthcare.6
Poor communication in the healthcare system has been linked to patient safety events.7 Poor communication is responsible for up to two-thirds of sentinel events, and of those events, over half were related specifically to poor transition of patient care between providers.8,9 The realities of our current complex healthcare system that may contribute to poor communication include the involvement of many team members using a variety of communication methods, professional hierarchies that inhibit communication, and members of the healthcare team constantly changing because of shift and schedule changes. One interprofessional communication strategy that has been recommended to improve quality and safety by overcoming some of these barriers is the Situation-Background-Assessment-Recommendation/Request (SBAR) communication tool.10
The SBAR communication tool is a simple, structured, and standardized technique that the United States military developed and used to improve communication between team members during urgent situations. Members of the healthcare industry later adopted it and the Joint Commission and the Institute for Healthcare Improvement now recommend this communication tool to be used in a wide variety of settings.10,11 It is also one of many tools provided in the TeamSTEPPS training program, which is often used in healthcare settings to improve teamwork, and ultimately patient care and safety.12 Many healthcare organizations have adopted the SBAR communication tool into their system and expect their clinicians to use it to enhance team-based communication. The actions required when using the SBAR tool are as follows: situation, succinctly state the problem; background, concisely present relevant information associated with the situation; assessment, provide an analysis and consider the various options; and recommendation, recommend a specific action. This format allows for standard expectations with regard to the content and structure of information that is communicated.
Because the SBAR communication tool is becoming increasingly popular in the healthcare arena, embedding it into health professions’ education is important. This integration will help close the gap between education and clinical practice. The Agency for Healthcare Research and Quality (AHRQ) has recommended that all professions be trained on the communication tool to achieve maximum effectiveness in interprofessional healthcare settings.12 Despite these recommendations, there are limited reports in the literature regarding training of students to use the communication tool.13-17 Within these limited publications, a wide variety of pedagogies are reported and the best training method has not been determined. Most of the literature related to the SBAR communication tool is situated in nursing education, and all of the training models took place within their own profession and did not involve other interprofessional learners.14-16 One study found that nursing students who received both classroom instruction and role-play instruction on the SBAR communication tool performed better in a simulated experience compared to those who received only classroom instruction.14 Similarly, another study found that significant improvements in the communication skills of nurses using the SBAR tool in role play compared to improvements seen after receiving lecture.15 An additional study found that students participating in an SBAR communication tool workshop that used role-play and video-simulated recall had significant increases in both their knowledge of the SBAR tool and their self-perceived attitudes towards using the SBAR tool.16
Specifically in the pharmacy education literature, there is a scarcity of information regarding use of the SBAR tool. Some pharmacy educators have recommended that the SBAR tool and other forms of interprofessional communication be incorporated into pharmacy curricula.18 However, only one study has examined the use of SBAR as an interprofessional communication tool in a required pharmacy course.17 This study required students to use the SBAR communication tool with a standardized colleague, who portrayed an attending physician. An improvement in pharmacy students’ self-confidence and interprofessional communication skills was seen following the simulation. The authors used this paucity in the literature along with the ACPE standards, CAPE outcomes, and IPEC competencies as the rationale for developing this IPE activity.
With the framework established, an interprofessional simulation with pharmacy and nursing students was developed within a Clinical Assessment course as a part of the pharmacy school curriculum. Specific learning objectives were: (1) apply pharmacotherapy knowledge to patient care within the scope of practice depending on pharmacy setting; (2) demonstrate a pharmacist role in patients’ care depending on pharmacy setting; and (3) communicate using the SBAR tool with nursing students to develop an appropriate plan of care for a patient. The objective of this study was to determine the impact an interprofessional simulation using the SBAR communication tool had on pharmacy students’ self-perception of interprofessional competence and their reactions toward interprofessional collaboration. Secondary objectives were to assess pharmacy students’ satisfaction with the simulation and their future intentions to use the SBAR communication tool.
DESIGN
The University of Kansas (KU) offers a four-year doctor of pharmacy (PharmD) degree to 170 students per class divided between two campuses. The main campus is in Lawrence, Kansas (150 students per class) and the regional campus is in Wichita, Kansas (20 students per class). The School of Pharmacy is the only health professions school residing on the Lawrence campus, with the others being located on the University of Kansas Medical Center (KUMC) campus in Kansas City, Kansas. In Wichita, several health professions’ programs (eg, nursing, physical therapy) are located at Wichita State University (WSU), which is not officially affiliated with KU. The distance between programs creates a barrier for live face-to-face IPE simulations.
Clinical Assessment is a required, two-credit hour applications-based course offered to third-year pharmacy students in the spring semester. The course a capstone experience to students prior to their participation in advanced pharmacy practice experiences. Students participated in a variety of weekly activities including active-learning strategies that often used standardized patients. Prior to this course, students had not participated in required activities related to IPE within the pharmacy curriculum.
For this experience, nursing students were selected as an interprofessional partner because of their familiarity with SBAR within their curriculum. The number of nursing students available to participate in this simulation from the collective nursing programs was smaller than the size of the pharmacy class. Therefore, to practically execute and not dilute the experience, our 170 pharmacy students were randomized to experience IPE through one of two different interprofessional simulations for the semester. The focus of this study is on one of these two simulations.
The simulation discussed in this study included senior level BSN nursing (n=94) and third-year pharmacy students (n=96) collaborating in small groups on two separate days over a two-week period. Two pharmacy and two nursing faculty members collaborated to create the content for the simulation, with each individual dedicating approximately 6 hours to development and logistic planning. During the actual interprofessional simulation, nine faculty members were required each day for approximately four hours to supervise the simulation, provide feedback and coaching, and lead a debriefing session. For this specific simulation, four pharmacy and four nursing groups were run simultaneously with one faculty member required for each professional student group. An additional faculty member led the group debriefing sessions.
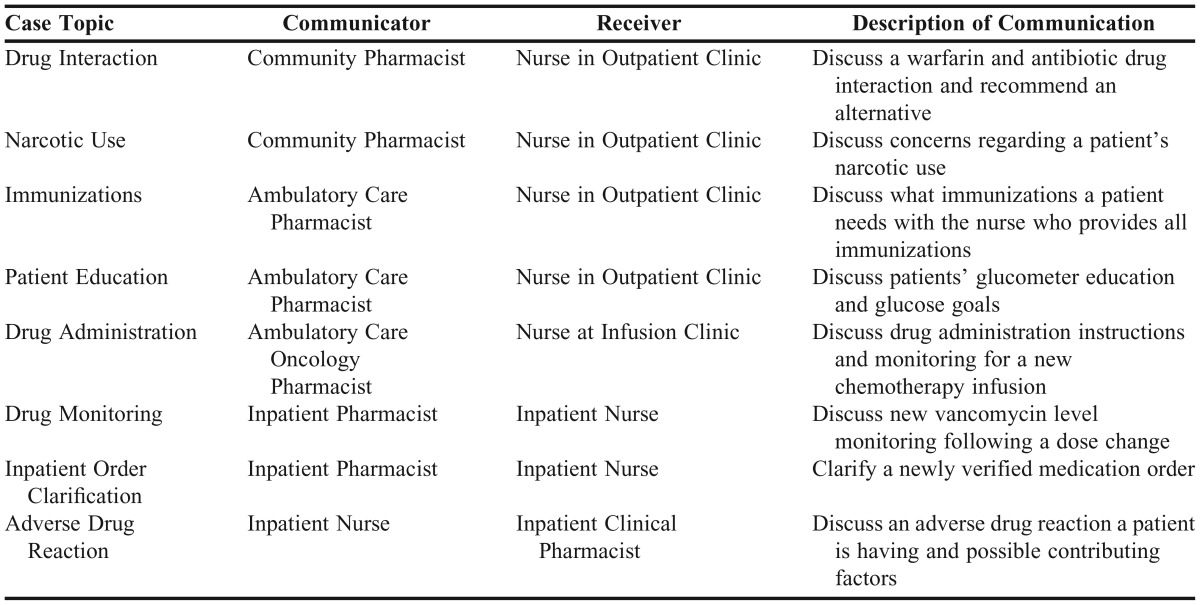
Students used telephones and the SBAR communication tool to convey information and collaborate on the development of a shared-care plan. The simulation created communication from three pharmacy settings (community, ambulatory care, and inpatient) to the corresponding nurse settings (primary care and inpatient) in regards to a variety of clinical content (drug administration, adverse drug reaction, etc). The clinical content of these cases is highlighted in Table 1. Each student was assigned to a group of three pharmacy students and three nursing students. To give pharmacy students exposure to additional scenarios and a chance to improve their interprofessional communication skills, the simulation was repeated the following week using four new patient cases. The same pharmacy students participated in both weeks; however, some nursing students were not able to return so other nursing students took their places during the second week.
Table 1.
Communication Case Descriptions
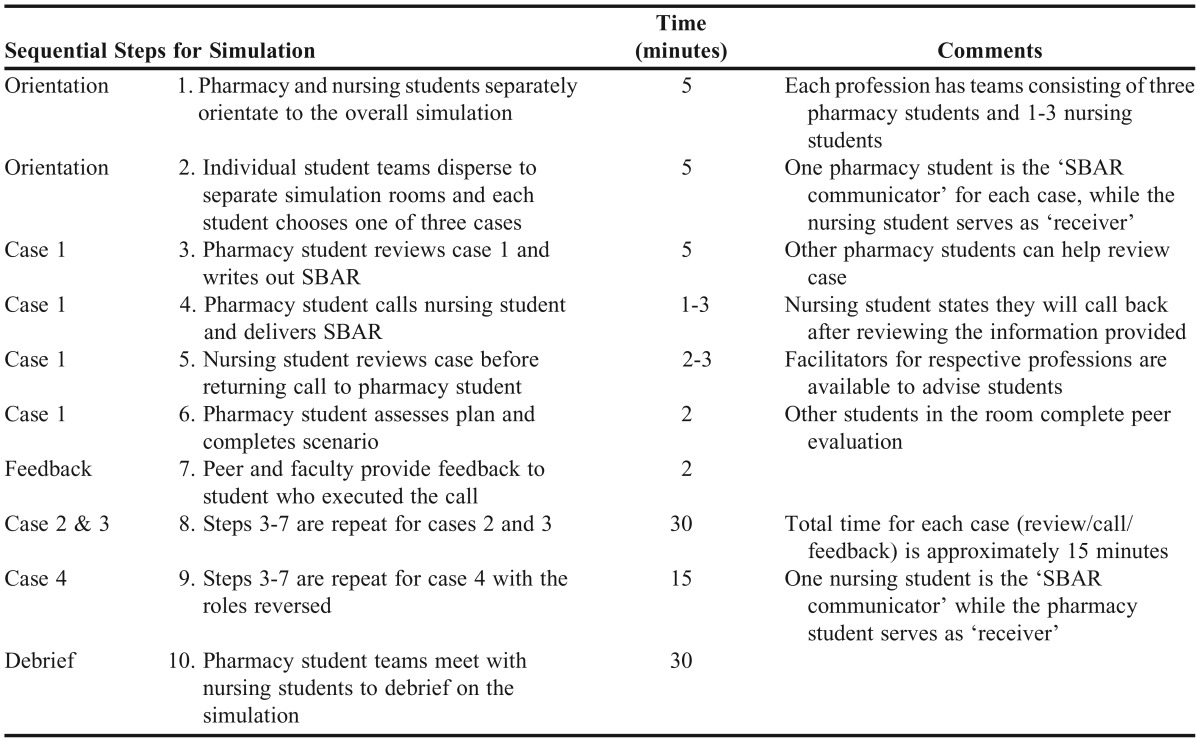
The simulation took place in eight rooms (four rooms for each profession) and lasted a half-day for three days during week 1. This schedule was repeated again during week 2. The pharmacy and nursing students were located in separate buildings, and in many cases, in different cities. For each student, the simulation lasted 60 minutes and the group debriefing lasted 30 minutes, for a total of 90 minutes spent during week 1 and 90 minutes during week 2. During each 60-minute active simulation time, the pharmacy and nursing groups had to communicate and collaborate on four separate cases, with each case lasting 15 minutes. For three of the cases, a pharmacy student was the “SBAR communicator” and the nursing student was the “receiver.” For the fourth case, the roles were reversed. This design (3 vs 1) was intentional to provide more opportunities for the pharmacy students to practice interprofessional communication using the SBAR tool because nursing students had an opportunity to practice the tool previously in their curriculum.
Immediately after each 60-minute simulation, participating pharmacy and nursing students came together in person or via video conference if in separate locations for a required debriefing session to reflect on roles and responsibilities, interprofessional communication, and specifically the use of the SBAR communication tool. This process was repeated two more times with new students resulting in three repetitions of the simulation and debriefing session occurring each afternoon for three days each week to get all students through the activity (Table 2).
Table 2.
Logistics of SBAR Communication Simulation
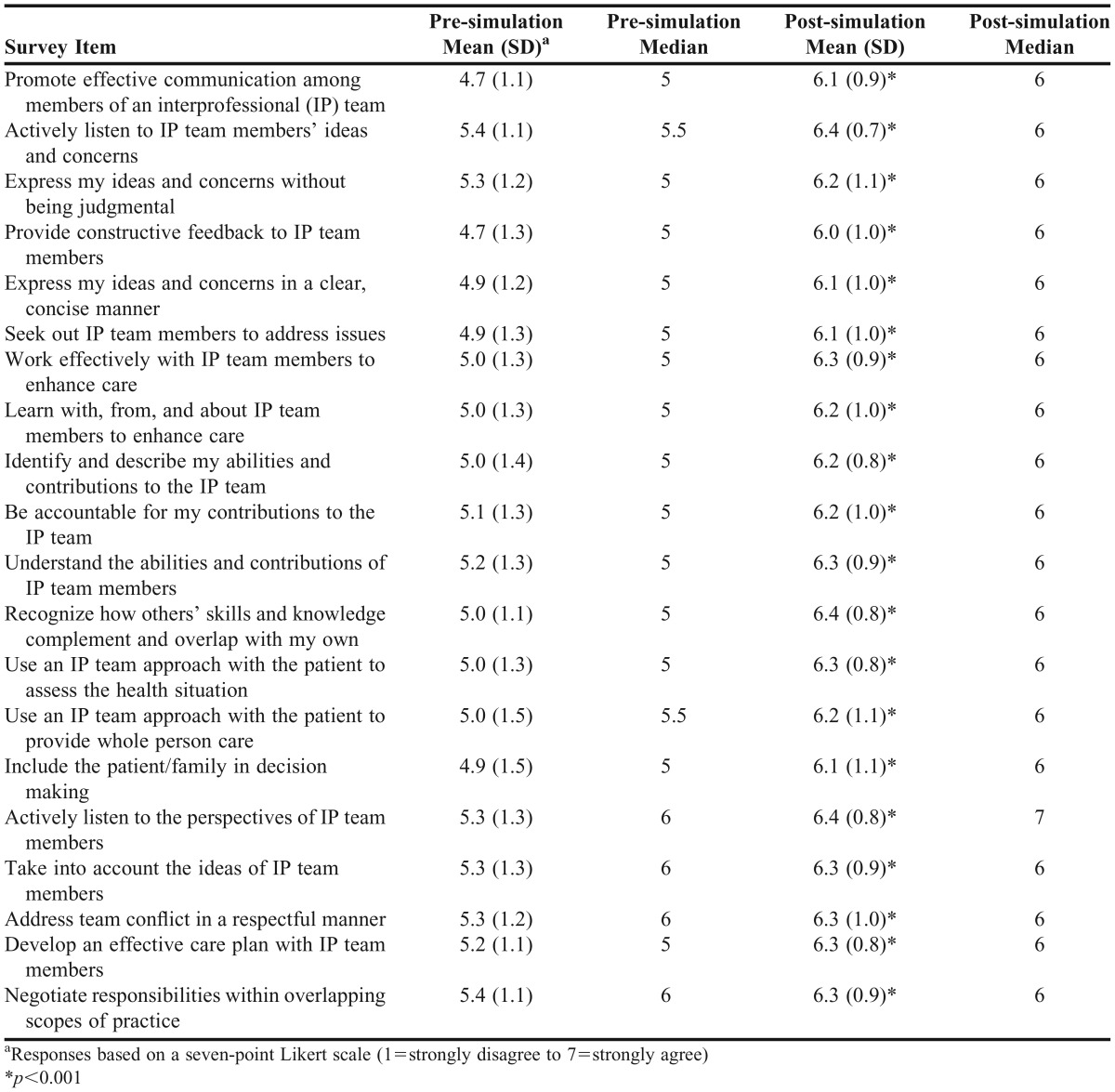
At the end of the semester, the Interprofessional Collaborative Competency Attainment Survey (ICCAS)19 was administered to the entire class, including those who were assigned to the alternative simulation. The ICCAS was used to assess self-perception of interprofessional competence. Completion of the ICCAS was anonymous and voluntary. The ICCAS, a self-assessment instrument for interprofessional collaborative practice, contains 20 items which participants rate on a seven-point Likert scale (1=strongly disagree to 7=strongly agree, plus an option to rate items as ‘‘not applicable.”) The survey is a retrospective pretest posttest design, thus, both parts are administered simultaneously after the IPE intervention. The ICCAS instructions ask learners to reflect back on their competence and rate each item based on their competency level before the IPE activity and after the activity. The pretest portion of the survey has two factors: the participant’s own role/skills when collaborating and the participant’s involvement with the rest of the team. The posttest includes only one factor regarding interprofessional collaboration. After finishing both weeks of the simulation, pharmacy students were asked to complete an anonymous satisfaction survey using a 5-point Likert scale (1= strongly disagree to 5=strongly agree).
After the simulation, students were given five prompts and asked to write a reflection paper regarding their reactions to interprofessional collaboration and future use of the SBAR communication tool. The five prompts were: (1) pharmacist’s role regarding interprofessional collaboration; (2) student confidence in interprofessional collaboration skills; (3) student confidence using the SBAR tool; (4) behavior change as a result of interprofessional collaboration during the simulation; and (5) students’ most important “take-home point” after participation. Completing the simulation and reflection paper were requirements for the Clinical Assessment course. Students who completed the reflection paper received a grade of pass for this activity while students who did not received a grade of fail.
Changes between pre- and post-ICCAS results were analyzed for significance using the Wilcoxon signed rank test because of the ordinal data and response option of “not applicable.” Because analysis using nonparametric and parametric tests showed identical statistical significance, the results using a paired t test are reported. Quantitative and qualitative methods were employed to assess student satisfaction of the simulation, perceived competency, reactions toward interprofessional collaboration, and future use of interprofessional communication tools such as the SBAR following the simulation. All data were analyzed using SPSS, v. 22.0, software system (IBM, Armonk, New York). Satisfaction data were analyzed using descriptive statistics. Two of the faculty investigators (MK & SS) independently analyzed reflection data for major themes using Dedoose, v. 6.1.11, a web-based application for qualitative and mixed methods research (SocioCultural Research Consultants, Los Angeles, CA). Twelve codes, such as “patient safety” or “gained confidence,” were determined before qualitative analysis was conducted to identify common themes. Then the investigators used the codes during their analysis to determine the most prevalent themes from the student reflections. A pooled Cohen’s kappa value was found to be 0.65 between the two faculty investigators, which indicated good interrater agreement. This project was determined to be exempt by the university’s institutional review board.
EVALUATION AND ASSESSMENT
Of the 96 pharmacy students randomly assigned to this simulation, 58 voluntarily and anonymously responded to the ICCAS (60% response rate) at the end of the semester. Pharmacy students’ self-perception of interprofessional competence improved after participation in this simulation as evidenced by a significant positive change occurring for all 20 items in all factors (p<0.001). Complete results can be found in Table 3.
Table 3.
Pharmacy Students’ Performance on the Interprofessional Collaborative Competency Attainment Survey (ICCAS) After Completing an Interprofessional Simulation (n=58)
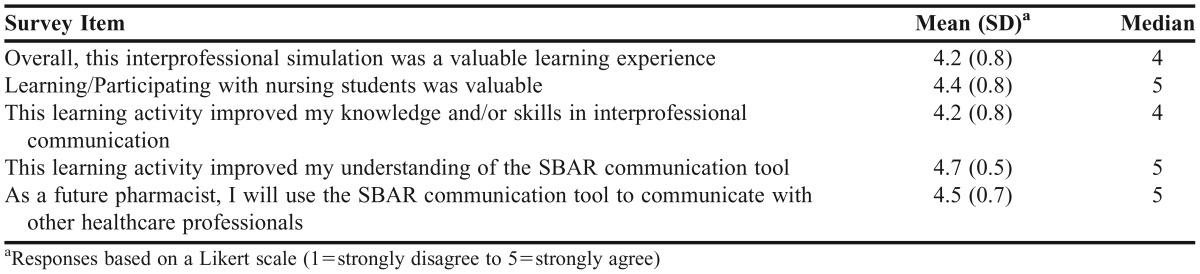
The satisfaction survey, completed by all 96 pharmacy students (100% response rate), showed that students felt the simulation was a valuable experience (mean Likert score=4.2). Additionally, results showed that students plan on using the SBAR communication tool as a future pharmacist (mean Likert score=4.5). Complete satisfaction results can be found in Table 4.
Table 4.
Student Satisfaction Results After Completing an Interprofessional Simulation (n=96)
Ninety students completed written reflection papers (94% response rate), which were analyzed to determine common themes. Beneficial comments towards communication were seen in >90% of the reflection papers. Approximately 70% of students recognized that the SBAR tool allowed them to deliver an organized message, which was one of two themes most frequently occurring with regards to behavioral change after communication. Almost half (46%) of the students mentioned that this simulation allowed them to gain confidence using the SBAR communication tool, while more than 80% wrote that they planned to use the tool in the future, either on advanced pharmacy practice experiences or as a pharmacist. Overall, the importance of communication, the positive impact of interprofessional collaboration on patient care, the ability to deliver an organized message, and the importance of having respect for other health professions were the most common take-home points for students following this simulation.
DISCUSSION
Integrating an interprofessional simulation using the SBAR communication tool proved to be a beneficial component to the clinical assessment course. The simulation positively impacted pharmacy students’ self-perception of interprofessional competence and reactions towards interprofessional collaboration. Additionally, the simulation helped fulfill pharmacy accreditation standards and the IPEC competency domain of interprofessional communication. Overall, students were satisfied with the experience and intend to use the SBAR communication tool in the future.
This study adds to the limited literature on use of the SBAR tool outside of nursing education by evaluating SBAR use by additional interprofessional learners, including pharmacy students. While a prior study included the novel use of the SBAR tool during a standardized colleague experience, it combined students from two different health professions.17
In our study, pharmacy students reported that using the SBAR communication tool enhanced their ability to organize information and make recommendations when speaking to other healthcare professionals. This has implications for improved patient care and safety. Allowing students to gain comfort and confidence in interprofessional communication will hopefully benefit them upon graduation as effective communication is integral for patient safety, especially during care transitions.20
The use of the validated ICCAS to measure self-reported competencies is a strength of this study. Although responses are self-reported, the ICCAS goes beyond measuring the impact of IPE on student attitudes and assesses the impact on their interprofessional behavior, which is a challenging area to assess in IPE.21 The retrospective pretest/posttest design of the ICCAS allowed students to have a better perspective on their improvement in interprofessional competencies.19
The design of the ICCAS administration is also less likely than a pretest/posttest design to be influenced by outside work experience or professional maturation which may occur throughout the semester. Furthermore, the mixed-methods assessment allowed for measurement of the educational impact of this simulation beyond the ICCAS. Using the Dedoose application, authors of this study could systematically determine common themes in reflection papers to gain a better understanding on the students’ perspective. These assessment measures help to justify the value of this simulation.
Another strength of this study is the design, which was advantageous in overcoming common logistical barriers to IPE. Timing and physical space are some of the challenges that exist in organizing IPE activities and have been previously identified.22 This simulation did not require students to be in the same location, which avoided additional travel and the need to find extra classroom space. Including students on a separate campus as well as students at another university demonstrated that this simulation can be carried out regardless of physical location. This unique inclusion of students from a different university can serve as an example for those who do not have other health professions schools on their campus. Additionally, all of this was done without any costly technology resources. The approach used in this simulation could be implemented by other institutions that may face similar barriers to incorporating IPE activities.
While there are many strengths of this study, it is not without limitations. Students’ self-perception of interprofessional competence statistically improved for all survey items. However, the educational significance of those findings could be debated. Our study demonstrated that students already had higher levels of self-perceived interprofessional competence (based on presimulation median responses of 5 or 6); therefore, large increases in self-reported competence were unlikely. The ICCAS was administered to all of the pharmacy students at the end of the semester, but not to the nursing students. The response rate of the ICCAS could have been improved. Administering the ICCAS immediately following the simulation, as was done with the satisfaction survey, could have resulted in a higher response rate. Student performance was assessed by peers through the use of a rubric; however, this was for formative feedback as students did not receive any evaluations from faculty regarding their performance. This interprofessional simulation did require a large amount of faculty facilitation as is expected with most IPE or simulation pedagogies, so other institutions should carefully consider available resources prior to implementing the simulation. Lastly, the results are reported for a single institution in a single academic year, with no performance on prior required coursework to serve as a benchmark for comparison.
Moving forward, these limitations will be addressed and the interprofessional simulation will continue to be offered in the school of pharmacy. Because the simulation has such a strong focus on interprofessional communication using the SBAR communication tool, the faculty members involved in the study felt that future students would benefit from completing this simulation earlier in the curriculum. They believe the students would still be able to understand the important concepts presented. Additionally, the students in this study had limited IPE exposure and yet still benefitted from the simulation, which further supports the consideration of early exposure in the curriculum. Students could start to incorporate the SBAR communication tool in introductory pharmacy practice experiences and also in their workplace. Despite these limitations, other schools of pharmacy could consider implementing an interprofessional simulation highlighting the use of the SBAR communication tool to fulfill national IPE competencies and ACPE accreditation standards.
SUMMARY
Incorporating an interprofessional simulation using the SBAR communication tool within a required course positively impacted pharmacy students’ self-perception of interprofessional competence, reactions toward interprofessional collaboration, and future intentions to use the SBAR communication tool. The instructional design also proved to be effective in avoiding a common barrier of physical space and location associated with IPE. In order to fulfill curricular needs and meet national accreditation standards, other schools of pharmacy should consider implementing a similar simulation.
REFERENCES
- 1. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva: WHO; 2010. [PubMed]
- 2.Medina MS, Plaza CM, Stowe CD, et al. Center for the Advancement of Pharmacy Education 2013 Educational Outcomes. Am J Pharm Educ. 2013;77(8):Article 162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional programs in pharmacy leading to the doctor of pharmacy degree. 2011. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed July 20, 2015.
- 4. Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: report of an expert panel. Washington, DC: Interprofessional Education Collaborative; 2011.
- 5. Cox M, Naylor M. Transforming patient care: aligning interprofessional education with clinical practice redesign. Conference recommendations. Atlanta, GA; 2013.
- 6.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff. 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm. A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. http://www.nap.edu/openbook.php?isbn=0309072808. Accessed July 20, 2015.
- 8.The Joint Commission. Sentinel Event Data Root Causes by Event Type, 2000-2014. http://www.tsigconsulting.com/tolcam/wp-content/uploads/2015/04/TJC-Sentinel-Event-Root_Causes_by_Event_Type_2004-2014.pdf/. Accessed November 23, 2016.
- 9. Pillow M, ed. Improving Hand-off Communication. Oakbrook Terrace, IL: The Joint Commission; 2007.
- 10.Institute for Healthcare Improvement. SBAR communication technique. http://www.ihi.org/explore/SBARCommunicationTechnique/Pages/default.aspx. Accessed July 20, 2015.
- 11. The Joint Commission, 2013. SBAR-a powerful tool to help improve communication. 2013. http://www.jointcommission.org/At_home_with_the_joint_commission/sbar_%E2%80%93_a_powerful_tool_to_help_improve_communication/. Accessed July 20, 2015.
- 12.Agency for Healthcare Research and Quality. TeamSTEPPS 2.0 Essentials. http://www.ahrq.gov/professionals/education/curriculum-tools/teamstepps/instructor/essentials/slessentials.html#s5. Accessed July 20, 2015. [DOI] [PubMed]
- 13.Marshall S, Harrison J, Flanagan B. The teaching of a structured tool improves the clarity and content of interprofessional clinical communication. Qual Saf Health Care. 2009;18(2):137–140. doi: 10.1136/qshc.2007.025247. [DOI] [PubMed] [Google Scholar]
- 14.Kesten KS. Role-play using SBAR technique to improve observed communication skills in senior nursing students. J Nurs Educ. 2011;50(2):79–87. doi: 10.3928/01484834-20101230-02. [DOI] [PubMed] [Google Scholar]
- 15.Toghian Chaharsoughi N, Ahrari S, Alikhah S. Comparison the effect of teaching of SBAR technique with role play and lecturing on communication skill of nurses. J Caring Sci. 2014;3(2):141–147. doi: 10.5681/jcs.2014.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang W, Liang Z, Blazeck A, Greene B. Improving Chinese nursing students’ communication skills by utilizing video-stimulated recall and role-play case scenarios to introduce them to the SBAR technique. Nurse Educ Today. 2015;35(7):881–887. doi: 10.1016/j.nedt.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 17.Shrader S, Dunn B, Blake E, Phillips C. Incorporating Standardized Colleague Simulations in a Clinical Assessment Course and Evaluating the Impact on Interprofessional Communication. Am J Pharm Educ. 2015;79(4):Article 57. doi: 10.5688/ajpe79457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vogt EM, Robinson DC, Chambers-Fox SL. Educating for safety in the pharmacy curriculum. Am J Pharm Educ. 2011;75(7):Article 140. doi: 10.5688/ajpe757140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Archibald D, Trumpower D, MacDonald CJ. Validation of the interprofessional collaborative competency attainment survey (ICCAS) J Interprof Care. 2014;28(6):553–558. doi: 10.3109/13561820.2014.917407. [DOI] [PubMed] [Google Scholar]
- 20.Hume AL, Kirwin J, Bieber HL, et al. Improving care transitions: current practice and future opportunities for pharmacists. Pharmacotherapy. 2012;32(11):e326–e337. doi: 10.1002/phar.1215. [DOI] [PubMed] [Google Scholar]
- 21.Reeves S, Boet S, Zierler B, Kitto S. Interprofessional education and practice guide No. 3: evaluating interprofessional education. J Interprof Care. 2015;29(4):305–312. doi: 10.3109/13561820.2014.1003637. [DOI] [PubMed] [Google Scholar]
- 22.Begley CM. Developing inter-professional learning: tactics, teamwork and talk. Nurse Educ Today. 2009;29(3):276–283. doi: 10.1016/j.nedt.2008.09.006. [DOI] [PubMed] [Google Scholar]