Abstract
Context:
Scientific findings of adverse childhood experiences (ACEs) and their lifelong graded relationship with leading causes of death are well established. Many health care practitioners, however, have yet to implement ACEs screening in clinical practice. Furthermore, ACEs screening and trauma-informed care (TIC) are not part of standard graduate-level training.
Objective:
To 1) implement trauma-informed curriculum for multiple graduate health programs, 2) determine student understanding of and willingness to address ACEs, and 3) assess the relationship between students voluntarily evaluating their individual ACE Score and their attitude toward ACEs and TIC.
Design:
Prospective study with pre- and postcurricular surveys (12-question digital survey administered before and after the curriculum) for 967 graduate students from 9 health professions programs at 2 campuses who received curriculum focused on ACEs and TIC.
Main Outcome Measures:
Students’ understanding of ACEs and TIC, their awareness of personal ACEs, and their willingness to incorporate TIC in practice.
Results:
Among students who voluntarily completed an ACE questionnaire, there was statistical significance in familiarity with clinical and scientific findings of the ACE Study (p < 0.001) and familiarity with TIC (p < 0.02). A significant intercampus difference in the students’ familiarity with the scientific and clinical findings of the ACE Study (p < 0.05) was found.
Conclusion:
Students and future health care practitioners who voluntarily assess their ACE Score are significantly more likely to understand scientific and clinical findings of the ACE Study as well as TIC.
INTRODUCTION
The lifelong graded relationship between adverse childhood experiences (ACEs) and leading causes of death is well established. ACEs have been shown to be “the main determinant of the health and social well-being of the nation.”1 Starting in the mid-1990s researchers evaluated more than 17,000 upper-middle-class, college-educated adults in the Kaiser Foundation Health Plan to better understand the relationship between childhood trauma and disease in adulthood. They found that the wider the extent of exposure to 10 types of childhood abuse, neglect, and household dysfunction, the higher the individual’s risk of maladaptive behaviors, chronic health conditions, and early death.2 Many health care practitioners, however, have yet to consider ACEs in clinical practice. Furthermore, ACEs screening and trauma-informed care (TIC) are not part of standard health practitioner graduate-level discussions.
Child maltreatment is common and pervasive in our country.2,3 Most victims of maltreatment carry scars, sometimes unrecognized, throughout their lives. Scientific evidence shows that the consequences of childhood trauma and the excessive amount of toxic stress consequent to it are directly linked to addiction, mental health disorders, lack of impulse control, and other conditions such as chronic obstructive pulmonary disease, certain types of cancer, diabetes, coronary artery disease, liver disease, and even early death.2
Despite evidence clearly demonstrating significant consequences of ACEs, many health care practitioners have yet to learn about and be trained in TIC. Nadine Burke Harris, MD,3 from the Center for Youth Wellness in San Francisco, CA, explained in a TED (Technology, Entertainment and Design) conference in 2014 that even though practitioners equipped with the knowledge of ACEs can better address childhood trauma and more effectively provide health care to their patients, there seems to be a lack of enthusiasm among physicians and other health care practitioners to consider the lifelong impact of child maltreatment. Burke Harris3 suggested it is more than simply bringing up the difficult issue of unresolved childhood trauma, asking the ACE Score questions, and knowing what to do with the results. She proposed that it is the practitioners’ lack of willingness to consider their own childhood trauma and how it has affected their lives and even their performance in their profession.
Adverse Childhood Experiences and Trauma-Informed Care
Organizations throughout the US are implementing TIC, in which all efforts are coordinated to prevent, to treat, and to heal the lifelong consequences of child abuse.3–7 The trauma-informed practitioner recognizes the vast consequences of trauma in the developing years and throughout a person’s lifespan. A trauma-informed practitioner is better equipped to understand why their patients’ current state of health is not based on their addiction, maladaptive behavior, or mental illness as much as it is a consequence of the body’s physiologic and psychologic response to toxic stress in the developing years. After gathering results of a patient’s ACE Score questionnaire8 by mail, in person, or electronically, health care practitioners can formulate an appropriate therapeutic approach.
An intervention can begin simply by asking, “Tell me how that has affected you later in your life,” or “How would you feel if you learned that a child you care about was growing up exactly as you did?”4 Once practitioners understand that a behavior or health condition is related to a patient’s ACEs, they are better equipped to see the problem as the patient’s adaptation. For example, smoking can be an anxiolytic and/or antidepressant, or obesity can be a mechanism to avert unwanted sexual advances. Working with such perspective conveys acceptance and compassion.4
Patients can be reassured that ‘the ACEs were not your fault,’ ‘It is not all in your head,’ and ‘You are experiencing a normal response to abnormal life experiences in childhood. Help exists for that.’ … Attending to the root problem and not to the patient’s adaptation to the problem allows providers to address the ‘fire’ rather than merely the ‘smoke.’ In addition, the higher-quality clinician-patient relationship arising from this approach is itself therapeutic.4
Sometimes starting the conversation is all that must happen for patients to start processing the connections of their childhood trauma to current ailments. This knowledge alone may empower patients and start them on the path to emotional and physical healing. Someday, perhaps all practitioners can echo these profound words: “Gradually, we came to see that asking, listening, and enabling a patient to go home feeling still accepted, is in itself a major intervention. The clinical practice of asking, listening, and accepting is doing.”9
Implementation of Trauma-Informed Care in Practice
Fortunately, many communities and hospital administrations are making training in ACEs and TIC available and even implementing efforts to transform various health care systems.5–7 Without specifically implementing screening methods, some organizations choose to teach and to openly discuss the psychobiology of toxic stress and long-term health consequences of ACEs. However, as noted by the authors of the original ACE Study,2 some practitioners make excuses for why they do not make changes in their practice, excuses that do not scratch the surface as to why there is refusal to change.
Internist and family practice colleagues, while commonly finding the ACE study quite interesting, generally did not want to use its findings in practice, citing time factors and lack of training as explanations. Those in fee-for-service practice additionally cited lack of insurance coverage. While superficially plausible, we saw these often were cover excuses for deeper resistance, sometimes related to the awakening of personal ghosts, as well as discomfort in discussing topics we have all been taught are protected by social taboos related to sex and the privacy of family lives.9
[Emphasis added.]
Because the awakening of these “personal ghosts” is a very important factor in the ability to connect with one’s patient, this adds yet another reason to transform medical training to address ACEs and TIC. Moreover, it is important for practitioners to address the impact of their own ACEs on work performance. Researchers found a strong and graded relationship between one’s ACE Score and job problems, financial problems, and absenteeism in addition to “four areas of health and well-being that employers and medical practitioners have difficulty managing (relationship problems, emotional distress, somatic symptoms, substance abuse)… .”10
Trauma-informed practitioners who have implemented changes in their practice have witnessed improvements in staff and organizational health, in addition to improvements in their patients’ medical care.4,7 For example, in the late 1980s and early 1990s a team of health care practitioners based in Philadelphia, PA, clearly saw the consequences of violence and trauma in their patients.7 They worked to form a healing system for traumatized patients and began implementing patient care through a trauma-informed approach. Later called The Sanctuary Model, this method seeks to provide healing from violence and has grown to help train workers and organizations on how to create and maintain “physical, psychological, social and moral safety within a social environment.”7 Participants “become thoroughly familiar with the psychobiology of trauma and disrupted attachment and the multiple ways that [posttraumatic stress disorder] … and other trauma-related disorders present in the children, adults and families they work with.”7
Sandra Bloom, MD,7 founder of The Sanctuary Model, recounts positive effects of one such implementation of The Sanctuary Model in pediatric residential facilities in Pennsylvania for both patients and staff. There were five important differences in the staff:
Support: how much children help and support each other; how supportive staff is toward the children; Spontaneity: how much the program encourages the open expression of feelings by children and staff; Autonomy: how self-sufficient and independent staff perceive that the children are in making their own decisions; Personal Problem Orientation: the extent to which children seek to understand their feelings and personal problems; Safety: the extent to which staff feel they: can challenge their peers and supervisors, can express opinions in staff meetings, will not be blamed for problems, and have clear guidelines … .7
Specifically analyzing data of service utilization from 2007 to 2009 of children discharged from residential treatment facilities (RTFs) that implemented The Sanctuary Model vs other RTFs, Dr Bloom noted: “RTF providers implementing Sanctuary had: a substantially shorter length of stay … a substantial increase in the percentage of youth discharged who received outpatient services in the three months following discharge; a lower increase in the percentage of children readmitted to RTFs in the 90 days following discharge.”7
Citing how TIC is shown to be therapeutic for both the patient and the organization or practitioner who implements it, Dr Bloom7 also explains that simply “[l]earning about the psychobiology of stress, toxic stress, and trauma is liberating for people.” Yet many practitioners are reticent to discuss the impact of childhood trauma with their patients, remaining personally unaware of its importance. One objective of this study is to advance the understanding of graduate health students regarding ACEs and TIC, in light of their own attitudes toward discussing trauma with their patients, as well as their attitudes toward their own ACEs.
Objectives
We designed a curriculum to help students become comfortable addressing typically uncomfortable topics, practice listening and collaborating skills, and ultimately form confidence to implement their knowledge of ACEs and TIC in clinical practice. Using a model of teamwork and collaboration, we sought to better understand future health care practitioners’ consideration of the lifelong effects of trauma and violence, and ways to combat resistance to such understanding. We hypothesized that health professions students would be more confident in understanding the clinical importance of ACEs and TIC as they assessed their own history of ACEs. The objectives of this study were to 1) implement trauma-informed curriculum for multiple graduate health programs, 2) determine student understanding of and willingness to address ACEs, and 3) assess the relationship between students voluntarily evaluating their individual ACE Score and their attitude toward ACEs and TIC. Our goal was to formulate a method of instructing the next generation of health care practitioners on ways to prevent, to recognize, and to address unresolved childhood trauma and to inspire other training programs to do the same.
METHODS
A total of 967 students from 9 health profession programs (doctor of osteopathy [DO], doctor of podiatric medicine, doctor of optometry, doctor of dental medicine, doctor of physical therapy, doctor of veterinary medicine, doctor of pharmacy, master of science in nursing-entry, and master of science in physician assistant studies) primarily in Pomona, CA, were enrolled in the study. Participating students received curriculum focused on ACEs and TIC in an interprofessional education course. The DO program was the largest, with 340 students. It consisted of 230 students on the Pomona campus and 110 students at an expansion site in Lebanon, OR. A multiquestion digital survey administered before and after the curriculum assessed students’ understanding of ACEs and TIC, their awareness of personal ACEs, and their willingness to incorporate TIC in practice (see Sidebar: The Pre- and Postcurriculum Survey). Because students were not required to complete the pre- and postcurricular surveys as part of the curriculum, we sent reminder e-mails encouraging participation in the opportunity to help advance important research. The questions with the most revealing results, graded on an interval scale, are as follows:
How familiar are you with the clinical and scientific findings of the ACE Study?
How familiar are you with trauma-informed care?
How likely will you be to administer and assess an ACE questionnaire on your patients?
How confident are you in knowing what to do to help your patient after discussing his/her history of trauma?
Have you completed a personal ACE questionnaire in the past?
The Pre- and Postcurriculum Survey.
-
How familiar are you with the clinical and scientific findings of the Adverse Childhood Experiences (ACEs) Study?
Unfamiliar / Somewhat Familiar / Extremely Familiar
-
How familiar are you with Trauma-Informed Care?
Unfamiliar / Somewhat Familiar / Extremely Familiar
-
How comfortable are you discussing with your patient their personal history of physical, emotional, and sexual abuse?
Uncomfortable / Somewhat Comfortable / Extremely Comfortable
-
How important do you think it is for a patient’s medical record to include any history of physical, emotional, and sexual abuse?
Not important / Somewhat Important / Extremely Important
-
How likely will you be to administer and assess an ACEs questionnaire on your patients?
Unlikely / Somewhat Likely / Extremely Likely / Uncertain what this is
-
How confident are you in knowing what to do to help your patient after discussing his/her history of trauma?
Not Confident / Somewhat Confident / Extremely Confident
-
Have you completed an ACEs questionnaire in the past?
No / Yes
-
If no, how likely are you to complete an ACEs questionnaire on yourself?
Unlikely / Somewhat Likely / Extremely Likely / Uncertain what this is
-
If no, how comfortable are you completing an ACEs questionnaire on yourself?
Unlikely / Somewhat Likely / Extremely Likely / Uncertain what this is
-
If yes, how likely are you to discuss your personal results of the questionnaire with your own physician?
Unlikely / Somewhat Likely / Extremely Likely
-
If yes, how comfortable are you discussing the results of the questionnaire with your own physician?
Uncomfortable / Somewhat Comfortable / Extremely Comfortable
-
What is your sex?
Male / Female
In the interprofessional education course designed to promote collaboration and patient-centered care, participants work through various relevant health care cases in teams consisting of students from each health profession. Teams of at least 9 gather in small rooms with a proctor who helps facilitate the discussion. Three sessions, each of which lasts approximately 2 hours, occur 1 weeknight a week for 3 weeks. Each session is developed to prompt conversation about what one’s practice will look like and how it will be better served through collaborating with other health care professionals working with the same patient. In the week between each session, students are asked to prepare and research a topic that contributes to team-specific learning goals (questions not addressed during the prior session). In October 2015, and within this framework, we implemented a case specifically devoted to ACEs and TIC wherein the 3 sessions included the following:
Session 1: Students received instruction by trauma-informed practitioners who understand the importance of ACEs in practice. The Medical Director of a local child abuse intervention center presented a live lecture to DO students at the Lebanon, OR, campus. This was recorded and made available to all other programs involved in the curriculum if they were unable to provide a live lecturer for their own students. The purpose of this lecture was to instruct on abuse and neglect in its various forms, specifically within the scope of ACEs. Students learned the lifelong consequences of childhood trauma, how it may present in clinical practice, and reasons for practitioners to implement TIC.
Session 2: Each team watched Dr Burke Harris’ TED talk “How Childhood Trauma Affects Health Across a Lifetime” and studied the Web site for Consequences of Lifetime Exposure to Violence and Abuse (http://coleva.net) with a discipline-specific approach. (Veterinary students were referred to an article linking animal abuse as a marker for child abuse.11) They then discussed the ACE Study and toxic stress, and practiced ways to empathetically treat patients. Students were to discuss with each other how they, in their respective professions, could better understand the health of their patients.
Session 3: Teams role-played a factual case of an adult with ACEs, alternating roles as practitioner or patient in working through a therapeutic process. Each team explored how health professions can collaborate to meet patients’ needs. Finally, each team created a fact sheet intended for the general public to understand ACEs and TIC.
RESULTS
Of the 967 students who took part in the ACEs and TIC curriculum, 267 submitted responses to the precurricular survey (response rate, 27.6%) and 422 submitted responses to the postcurricular survey (response rate, 43.6%). Of the 267 precurricular responses, 5 respondents had at one time assessed their own ACE Score, which increased to 68 respondents in the postcurricular survey. We then looked solely at the 169 anonymous students who responded to both pre- and postcurricular surveys, matching the data to more effectively assess our intervention.
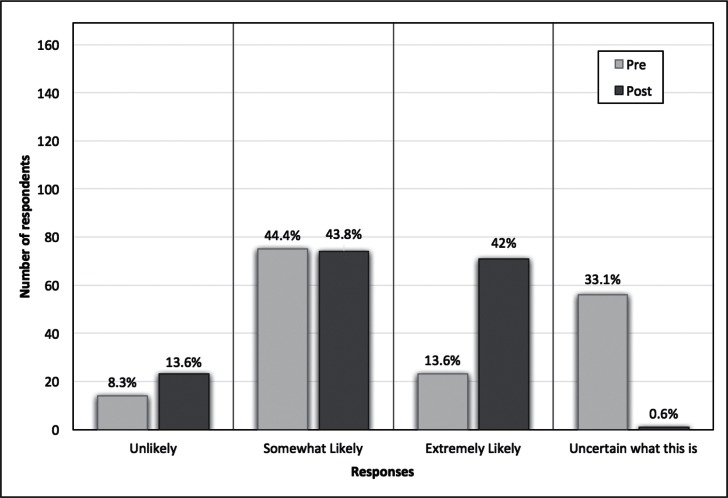
There was a substantial increase in the students who were “extremely likely” to administer and assess an ACE questionnaire for their patients (13.6% of respondents precurriculum [n = 23] vs 42.0% postcurriculum [n = 71]). Of these 169 students, 1 respondent did not answer this particular question and appeared as the 0.6% “Uncertain what this is” seen in Figure 1. Among the 13.6% of respondents who answered “unlikely” to administer an ACE questionnaire for their patients in the postcurricular survey, 44.0% (n = 10) were from the veterinary program; the next largest represented program was pharmacy, with 21.7% (n = 5).
Figure 1.
Precurricular (Pre) and postcurricular (Post) survey responses of health professions students to the survey question, “How likely will you be to administer and assess an ACE questionnaire for your patients?”
ACE = adverse childhood experiences.
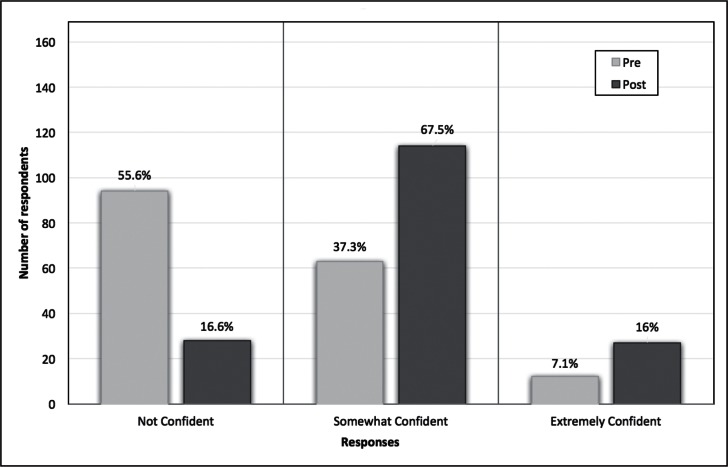
Respondents’ confidence levels in helping a patient with a history of trauma likewise increased (Figure 2). Those reporting feeling “somewhat confident” increased from 37.3% (n = 63) on the precurricular survey to 67.5% (n = 114) on the postcurricular survey, and there was more than twice the increase in responses to being “extremely confident”—from 7.1% (n = 12) on the precurricular survey to 16.0% (n = 27) on the postcurricular survey.
Figure 2.
Precurricular (Pre) and postcurricular (Post) survey responses of health professions students to the survey question, “How confident are you in knowing what to do to help your patient after discussing his/her history of trauma?”
Recognizing the predictable increase in postcurricular responses regarding understanding of ACEs and TIC after our intervention, we looked closer at respondents who had voluntarily assessed their own ACE Score. We did this using a χ2 test of independence to assess postcurricular survey responses from 422 students. These 422 students were represented by all 9 health professions programs and consisted of 144 men (34.1%) and 278 women (65.9%). One hundred forty-six students were from the DO program, with 83 from the Pomona, CA, campus and 63 from the Lebanon, OR, campus. There was no significant difference in responses based on sex. Looking at the response rate from the DO program at each campus, we noted that students at the Lebanon campus were overall much more likely to participate in the postcurricular survey (63/110, 57.3%) than were Pomona students (83/230, 36.1%).
In a comparison of all postcurricular survey responses between Pomona and Lebanon DO students, a statistically significant intercampus difference in the DO students’ familiarity with scientific and clinical findings of the ACE Study (degrees of freedom = 2, n = 146, χ2 = 6.422, p < 0.05) was found. Only 26.5% (61/230) of DO students at the Pomona campus were familiar with the clinical and scientific findings of the ACE Study, compared with a much higher 46.0% (51/110) of DO students at the Lebanon campus. Most significantly, respondents who voluntarily completed an ACE questionnaire (68/422 = 16.1%), compared with students who did not complete an ACE questionnaire, were more familiar with the clinical and scientific findings of the ACE Study (degrees of freedom = 2, n = 422, χ2 = 24.417, p < 0.001), and with TIC (degrees of freedom = 2, n = 422, χ2 = 8.264, p < 0.02). There was a higher proportion of Lebanon-based DO students who assessed their own ACE Score (25/110, 22.7%) vs Pomona-based DO students (15/230, 6.5%).
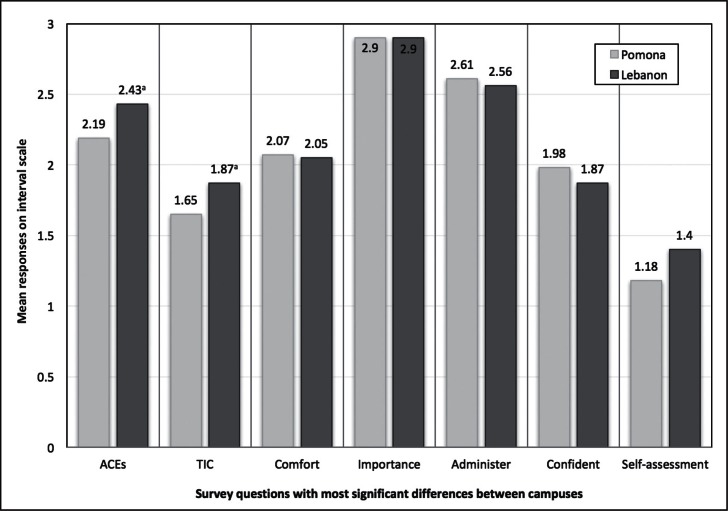
As Figure 3 depicts, the major differences between students at the two campuses were found to be 1) familiarity with the original ACE Study, 2) familiarity with TIC, and 3) self-assessment of one’s own ACE Score. Responses related to comfort level and the importance of discussing childhood trauma, as well as likelihood of administering the questionnaire and confidence in knowing how to help, were similar between campuses.
Figure 3.
Comparison of responses to survey questions between osteopathic medical students from both campuses (Pomona, CA, and Lebanon, OR) who assessed their own Adverse Childhood Experiences Score, with the major difference being that Lebanon-based students received a hard copy of the Adverse Childhood Experiences and Resilience/Stress questionnaires. The X-axis represents 7 of the survey questions. The Y-axis represents the mean of responses on an interval scale of 1 = unfamiliar, uncomfortable, unlikely, etc; 2 = somewhat familiar, somewhat comfortable, somewhat likely, etc; and 3 = extremely familiar, extremely comfortable, extremely likely, etc. For the self-assessment question, 1 = no; 2 = yes.
a p < 0.05.
ACEs = How familiar are you with the clinical and scientific findings of the Adverse Childhood Experiences Study?; Administer = How likely will you be to administer and assess an Adverse Childhood Experiences questionnaire on your patients?; Comfort = How comfortable are you discussing with your patient their personal history of physical, emotional, and sexual abuse?; Confident = How confident are you in knowing what to do to help your patient after discussing their history of trauma?; Importance = How important do you think it is for a patient’s medical record to include any history of physical, emotional, and sexual abuse?; Lebanon = Lebanon, OR, campus; Pomona = Pomona, CA, campus; Self-assessment = Have you completed an Adverse Childhood Experiences questionnaire in the past?; TIC = How familiar are you with Trauma-Informed Care?
DISCUSSION
The study data (cross tabulations available online at: www.thepermanentejournal.org/files/2017/16-061.pdf) support our hypothesis that students and future health care practitioners voluntarily assessing their ACE Score are significantly more likely to understand the scientific and clinical findings of the ACE Study and TIC. Because of the surveys not being required for the course, we were pleased with what we consider a high response rate (precurricular survey, 267/967, 27.6% vs postcurricular survey, 422/967, 43.6%). From the available data, we can’t explain why 354 of the postcurricular survey respondents chose not to calculate their own ACE Score or if there was any reason beyond it being voluntary (ie, lack of time, disinterest, thought to be trivial, fear of personal trauma).
A follow-up longitudinal study throughout the careers of these students might demonstrate how their approach to patients may differ from other practitioners who were not similarly trained. Measuring patient satisfaction, number of outpatient visits, and practitioner/staff health and professional attitude will help us determine the long-term effectiveness of integrating TIC into graduate programs for both practitioners and their patients. Further study is needed to assess practitioners’ awareness of their own ACEs and their approach to TIC of patients, which can also include the level of trust between practitioner and patient. Added considerations would include match or mismatch between the sex of the patient and the practitioner and willingness to discuss ACEs. It would also be important to evaluate for the most compassionate and effective method that practitioners may choose to administer the questionnaire, whether it be in the clinic, mailed to patients’ homes, or sent electronically.
Study limitations included a small sample size of personal ACE assessment because the institutional review board (IRB) of our institution denied assessment of students’ ACE Score as part of the study. Because we were not approved to gather respondents’ ACE Scores, we are unable to know if students with a higher ACE Score would be more familiar with ACEs and TIC than students with a lower ACE Score. Nor do we know the respondents’ comfort level and perceived importance in discussing a patient’s traumatic history, or their likelihood to administer an ACE questionnaire for their patients scaled in relation to their own ACE Score. If the IRB had approved respondents’ assessment of their own ACE Score as part of the intervention, we are confident the curriculum would have had a greater impact, because more students would have probably assessed their own ACE Score and thereby acquired better understanding of ACEs and TIC.
With a substantial increase in the amount of respondents who had assessed their own ACE Score, from 5 precurriculum to 68 postcurriculum, the data show that merely assessing one’s own ACE Score increases the understanding of and familiarity with ACEs and TIC. To be sure, a future study with an even larger population would include having all students self-administer an ACE questionnaire. To allay any fears or misunderstanding from the IRB, we will instruct students on the importance of building personal resiliency factors when working in health care, a field that in itself may be retraumatizing.
Furthermore, a standardization error occurred between both campuses in which students on the Pomona campus lacked a personal hard copy of the ACE and Resilience/Stress questionnaires.8,12 This error resulted in Lebanon-based students being proportionately more likely to assess their own ACE Score, with a statistically significant intercampus difference in students’ familiarity with the clinical and scientific findings of the ACE Study. In our χ2 test of independence, we should have assessed the level of significance of ACE Score self-assessment between campuses, but we chose not to in order to limit the number of comparisons being made. We are confident, however, had we included this assessment, the proportion of Lebanon students vs Pomona students would have been statistically significant because of the aforementioned standardization error. Acknowledging that people who voluntarily self-administer an ACE questionnaire are self-selecting, it is unclear whether this self-selecting population already had personal or clinical experience in assessing ACEs. However, we do know that only 5 of the 267 precurricular respondents had at one time assessed their own ACE Score.
Other major limitations of our study included controlling for variation between the programs and campuses regarding lecturers and facilitators. Compared with the other graduate programs, veterinary and pharmacy students were less likely to foresee themselves administering an ACE questionnaire, perhaps because of a perceived lack of feasible application in their fields. Future study will therefore necessitate for controlling variation in the different learners at various stages of training, by students’ ages, and by their respective program of study.
Several months after the IRB denied the original proposal to assess students’ ACE Scores, stating that they were “surprised [we] would even suggest” doing so, we ascertained more of the reasoning. With the remote possibility of even a minor number of the 950 students unable to process a traumatic childhood without help, the lack of mental health resources created the ultimate barrier to such a risk. What we are clearly seeing are systems-based barriers in assessing a history of ACEs for fear of retraumatization, liability, and even a personal discomfort/bias of discussing one’s own history of ACEs. Protecting subjects in research that could potentially prompt overwhelming emotions is a conscientious objection on the part of the IRB. What our data show, however, is that respondents who voluntarily assessed their own ACE Score are more familiar with the science of ACEs and TIC and are more willing to assess their patients’ ACE Score compared with respondents who did not voluntarily assess their ACE Score. We hope learning the psychobiology of ACEs was and has been liberating for the students in our study, as witnessed in others by Dr Bloom.7 Perhaps allowing the Lebanon-based students to understand the importance of their own resilience, from being shown the Resilience/Stress Questionnaire, served as an important protective factor.
In a major health professions training institution, the hesitancy to ask students about a possible traumatic childhood shows a misunderstanding of reasons and of the therapeutic consequences of doing so. Patients disclose highly personal information to their health care professional in a way few others are entrusted. The nature of the physician-patient relationship holds the possibility of enkindling past trauma for both practitioner and patient. If we are to comprehensively address the health of our patients, especially regarding circumstances surrounding their developing years, we ourselves must personally do the same.
It is time we make these fundamental changes of addressing our own ACEs, becoming trauma-informed, and inspiring resilience in our patients. As exclaimed by Ginsburg,13 health care practitioners can often work with difficult populations and revert to a model of addressing “what is wrong” with their patients, rather than attempting to understand “what happened to them.” Without a TIC paradigm, practitioners can themselves become burnt out, feeling less capable of offering care for their patients. Sharing his experience in adolescent medicine in his book Building Resilience in Children and Teens, Ginsburg stresses the importance of recognizing the vital role of resilience for all health care practitioners, and the patients we serve:
As a professional, being trauma-informed positions you to serve more effectively. … [and] prevents our own burnout. It allows us to learn to hold people’s pain without owning their pain … it allows us to understand others’ behavior in context, rather than taking their behaviors (eg, their weariness of trusting us) personally. We know what is and what is not about us. Knowing when not to personalize protects our boundaries and stems our frustration and, therefore, may increase our professional longevity.13
CONCLUSION
This research study is an answer to the call of the pioneers of TIC who have opened our eyes, such as Vincent Felitti, MD; Robert Anda, MD; Sandra Bloom, MD; Nadine Burke Harris, MD; Bessel van der Kolk, MD; and others. Consideration of one’s own ACEs, while learning of ACEs and TIC in the health professions setting, allows students and future health care practitioners to better understand the scientific and clinical significance of the lifelong effects of patients’ traumatic histories. With refined perspective after better understanding the importance of ACEs, we are empowered to connect with our patients in their circumstance. The challenge we face as health care practitioners is to see our patients for who they really are—just like us—a composite of several circumstances with more than just a “chief complaint.” Whether the patient is 5 or 50 years of age, the challenge is the same.
Acknowledgments
The authors would like to thank Sorrel Stielstra, PhD, for her help with statistical analysis.
Kathleen Loudon, ELS, of Loudon Health Communications, provided editorial assistance.
Footnotes
Disclosure Statement
The authors have no conflicts of interest to disclose.
Woe
The days of childhood are but days of woe.
— The Retrospect, Robert Southey, 1774–1843, English poet
References
- 1.Felitti VJ. [Origins of addictive behavior: evidence from a study of stressful childhood experiences]. [Article in German] Prax Kinderpsychol Kinderpsychiatr. 2003 Oct;52(8):547–59. [PubMed] [Google Scholar]
- 2.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998 May;14(4):245–58. doi: 10.1016/s0749-3797(98)00017-8. . [DOI] [PubMed] [Google Scholar]
- 3.Burke Harris N. How childhood trauma affects health across a lifetime [video] New York, NY: TED Conferences LLC; 2014. Sep, [cited 2016 Jul 27]. Available from: www.ted.com/talks/nadine_burke_harris_how_childhood_trauma_affects_health_across_a_lifetime. [Google Scholar]
- 4.Clarke D, Schulman E, McCollum D, Felitti V. Clinical approaches for adult ACE survivors experiencing unexplained physical symptoms and health problems [Internet] Jacksonville, FL: Academy on Violence and Abuse; 2015. [cited 2016 Jul 27]. Available from: www.avahealth.org/aces_best_practices/clinical-approaches-for-adults.html. [Google Scholar]
- 5.Forstadt LA, Rains M. Working with adverse childhood experiences: Maine’s history, present and future. A report for the Maine Children’s Growth Council [Internet] Augusta, ME: Maine Children’s Growth Council Health Accountability Team; 2011. Dec, [cited 2016 Jul 27]. Available from: http://tcmhs.org/pdfs/ACES_Report_Final.pdf. [Google Scholar]
- 6.Clifford Beers Clinic: help, healing, hope [Internet] New Haven, CT: Clifford Beers Clinic; p. c2015. [cited 2016 Aug 2]. Available from: http://aces.cliffordbeers.org/. [Google Scholar]
- 7.Testimony of Sandra L, Bloom MD . Prepared for Attorney General’s national task force on children exposed to violence Defending childhood: protect, heal, thrive Public hearing #4. Detroit, MI: Wayne State University; 2012. Apr 24, [Google Scholar]
- 8.Anda RF. The ACE score calculator [Internet] San Diego, CA: Sparrow Consulting LLC; 2007. [cited 2016 Jul 27]. Available from: http://acestudy.org/the-ace-score.html. [Google Scholar]
- 9.Felitti VJ, Anda RF. The lifelong effects of adverse childhood experiences. In: Chadwick DL, Giardino AP, Alexander R, Thackeray JD, Esernio-Jenssen D, editors. Chadwick’s child maltreatment: sexual abuse and psychological maltreatment. 4th ed. Vol. 2. Florissant, MO: STM Learning, Inc; 2014. pp. 203–15. [Google Scholar]
- 10.Anda RF, Fleisher VI, Felitti VJ, et al. Childhood abuse, household dysfunction, and indicators of impaired worker performance in adulthood. Perm J. 2004 Winter;8(1):30–8. doi: 10.7812/TPP/03-089. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arkow P. A link across the lifespan: animal abuse as a marker for traumatic experiences in child abuse, domestic violence and elder abuse [Internet] Shakopee, MN: Academy on Violence and Abuse; 2015. [cited 2016 Jul 27]. Available from: https://avahealthorg.presencehost.net/file_download/inline/b64aff80-5461-4d9b-9cdc-cf9b47f30174. [Google Scholar]
- 12.Rains M, McLinn K. Resilience/stress questionnaire [Internet] Augusta, ME: Southern Kennebec Healthy Start; updated 2003 [cited 2016 Jul 27]. Available from: www.wcasa.org/file_open.php?id=801. [Google Scholar]
- 13.Ginsberg KR. Building resilience in children and teens: giving kids roots and wings. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2015. p. 164. [Google Scholar]