Abstract
Introduction: Zika virus could be transmitted in the state of Queensland, Australia, in parts of the state where the mosquito vectors are established.
Methods: We assessed the epidemic potential of Zika in Queensland from January 2015 to August 2016, and estimate the epidemic potential from September to December 2016, by calculating the temperature-dependent relative vectorial capacity (rVc), based on empirical and estimated parameters.
Results: Through 2015, we estimated a rVc of 0.119, 0.152, 0.170, and 0.175, respectively in the major cities of Brisbane, Rockhampton, Cairns, and Townsville. From January to August 2016, the epidemic potential trend was similar to 2015, however the highest epidemic potential was in Cairns. During September to November 2016, the epidemic potential is consistently the highest in Cairns, followed by Townsville, Rockhampton and Brisbane. Then, from November to December 2016, Townsville has the highest estimated epidemic potential.
Discussion: We demonstrate using a vectorial capacity model that ZIKV could have been locally transmitted in Queensland, Australia during 2015 and 2016. ZIKV remains a threat to Australia for the upcoming summer, during the Brazilian Carnival season, when the abundance of vectors is relatively high. Understanding the epidemic potential of local ZIKV transmission will allow better management of threats to blood safety and assessment of public health risk.
Introduction
In 2015, Zika virus (ZIKV) emerged throughout the Americas and in February 2016, the World Health Organization declared ZIKV a public health emergency of international concern.
ZIKV is principally transmitted from infected Aedes aegypti and Aedes albopictus mosquitoes, vectors of dengue and chikungunya viruses. ZIKV can also be transmitted from mother to fetus, through sexual contact and via blood transfusion1 , 2. Up to eighty percent of infected people are asymptomatic3. In adults, the illness is usually mild, and common symptoms include fever, rash, joint pain and conjunctivitis, lasting for up to one week. However, ZIKV can cause serious birth defects when acquired during pregnancy4.
In north and central Queensland, Australia, where Ae. aegypti is present, ZIKV could be locally transmitted if imported. Between 2012 and 7 October 2016, 36 of the 76 confirmed ZIKV infections in travelers notified nationally were reported from Queensland5. In response to the emerging public health risk, diagnostic services for ZIKV and preventative vector control have been strengthened in the north of the state. Local transmission has not yet been recorded; however due to the high asymptomatic rate, cryptic transmission is possible. We retrospectively visualize the epidemic potential of Zika in four cities in Queensland (Brisbane, Cairns, Rockhampton and Townsville) from January 2015 to August 2016, and estimate the epidemic potential from September to December 2016. This was temporally relevant due to the risk of ZIKV importation from the Rio 2016 Olympic and Paralympic Games6.
Materials and Methods
Study Area
Four cities in Queensland were selected: Cairns, Townsville and, Rockhampton, which share current potential risk of Zika transmission as Ae. aegypti is well established; and, Brisbane, the state capital, where there is no evidence of Ae. aegypti since the 1950s7. However, Ae. aegypti is present in regions of Queensland that are only a few hundred km north of Brisbane (e.g. township of Gin-Gin).
Data Set
Monthly minimum and maximum temperatures (°C) from January 2015 to August 2016 inclusive, were retrieved from the Australian Bureau of Meteorology8. Monthly average mean temperature was calculated (Fig. 1).
Monthly average temperature in Queensland cities, Australia, January 2015 - December 2016.
Monthly predictions of the maximum and minimum temperature medians for September to December 2016 based on historical values were used to estimate the corresponding mean temperature medians9 (Fig. 1).
Estimation of Zika Epidemic Potential
The relative vectorial capacity (rVc) represents the vector’s ability to spread disease among humans relative to the vector-to-human population ratio10 and is defined as:
with a) the average daily vector biting rate; T) temperature; bh) the probability of vector-to-human transmission per bite; bm) the probability of human-to-vector infection per bite; µm) the vector mortality rate; n) the duration of extrinsic incubation period (Table 1).
Table 1: Parameters used to estimate the relative vectorial capacity of Zika in Queensland, Australia.
| Parameters | Description | Estimate/equations | Relationship | Source |
|---|---|---|---|---|
| a(T) | average daily vector biting rate (number of bites per day) | = 0.0043T + 0.0943 with 21◦C ≤ T ≤ 32◦C | Virus-independent; Temperature-dependent | 10 |
| bm(T) | probability of human-to-vector infection per bite | = 0.0729T – 0.9037 if 12.4°C ≤ T ≤ 26.1°C | Virus-and temperature-dependent | 10 |
| = 1 if 26.1°C < T < 32.5°C | ||||
| = 0.57 | 13 | |||
| bh(T) | probability of vector to human transmission per bite | = 0.001044T(T – 12.286)x(32.461-T)1/2 for 12.286°C ≤ T < 32.461°C | Virus-and temperature-dependent | 10 |
| = 0.27 | 13 | |||
| n | duration of extrinsic incubation period (day) | = 7 | Virus-and temperature-dependent | 11 , 12 |
| = 10 | 14 | |||
| = 4 + e 5.15-0.123T | 10 | |||
| µm(T) | Daily vector mortality rate (number of deaths in mosquito population per day) | = 0.8692 – 0.1590T + 0.01116T2 – 3.408 x 10-4T3 + 3.80 X 10-6T4 | Virus-independent; Temperature-dependent | 10 |
The last has been estimated to be seven (ranging from five to ten)11 , 12 , 13 and to ten days14. bh, and bm have recently been estimated for ZIKV and Australian Ae. aegypti mosquitoes13. Dengue virus (DENV) is also transmitted by Ae. aegypti mosquitoes, for which the other parameters and their relationship to temperature have been well described10 , 15 , 16. Therefore, we adapted a temperature-driven model for DENV transmission by Ae. aegypti 10 , 15 , 16, with estimated values of n, bh, and bm for ZIKV to assess and compare the Zika epidemic potential over space and time10.
We performed three relative vectorial capacity calculations, equation 1 and 2 with a varying n, and equation 3, as a comparison, with all parameters specific to DENV.
Equation 1: Formula 1) with the average n equal to 7, based on Chouin-Carneiro et al. (2016), Li et al. (2012), and Hall-Mendelin et al. (2016). Hereafter referred to as rVc7.
Equation 2: Formula 1) with the average n equal to 10, based on Boorman and Porterfield (1956). Hereafter referred to as rVc10.
Equation 3: Formula 1) based on the DENV-specific parameters from Liu-Helmersson et al. (2014). Hereafter named rVc(T)dengue.
Monthly epidemic potentials and range from equations 1, 2, and 3 were calculated for each city. For January 2015-August 2016, mean maximum and minimum temperatures each month were used for calculations of rVc. Forecasts for future monthly epidemic potential in September-December 2016 were estimated as described above. We then compared the results from equations 1 and 2 using an analysis of variance (ANOVA), with the null hypothesis being that the mean of the relative vectorial capacity remains the same for both scenarios.
Threshold Value for the Epidemic Potential
The threshold value rVc^ for an epidemic to take place is defined by:
Although analyses of the infectious period (Th) for ZIKV are still ongoing, a recent study of 297 PCR-confirmed clinical cases in French Polynesia estimated Th to last for four to seven days17 , 18. Using an average value of Th of 5.5 days, and assuming that the human-to-mosquito ratio, m, equals 1, the rVc^ must be larger than 0.18 [0.14; 0.25] per day for a Zika outbreak to occur. As an uncertainty analysis, we used the variability range of the infectious period [4, 7] to estimate the range of the threshold value for the epidemic potential.
Results
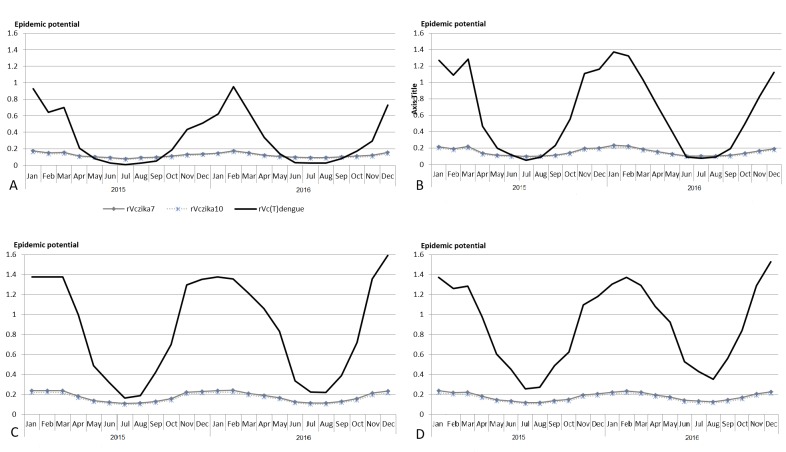
The resulting rVc from equations 1 (rVc7), 2 (rVc10) and 3 (rVc(T)dengue) are presented in Fig. 2. The rVc(T)dengue is consistently higher than rVc7 and rVc10 throughout the study period in Townsville and Cairns (Fig. 2).
Comparison of epidemic potentials calculated using three relative vectorial capacity estimates of mosquitoes to transmit Zika virus in Queensland cities, Australia, January 2015 - December 2016.
A) Brisbane, B) Rockhampton, C) Townsville, D) Cairns; rVc: relative vectorial capacity; rVc7: when the extrinsic incubation equal 7; rVc10: when the extrinsic incubation equal 10; rVc(T) corresponds to Liu-Helmersson et al. (2014) calculation with temperature as a variable for each parameters
At α = 0.05, p_value = 0.139 and F critical is larger than F, therefore we did not reject the null hypothesis. The difference between the mean rVc7 and rVc10 was, therefore, not significantly different from zero. The equations are thus interchangeable, so we used rVc7 in the following analyses.
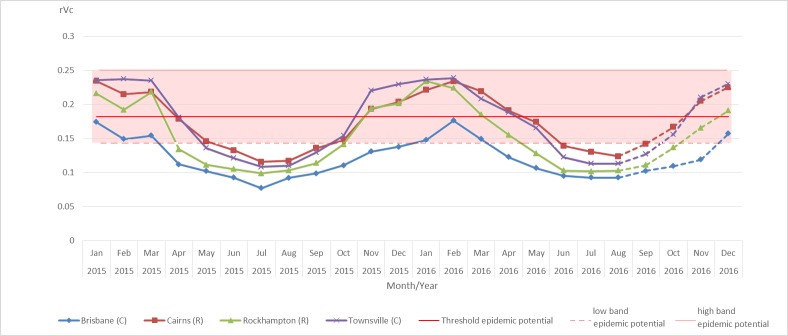
Through 2015, we estimated an overall relative vectorial capacity (rVc7) of 0.119 in Brisbane, 0.152 in Rockhampton, 0.170 in Cairns, and 0.175 in Townsville. Throughout 2015, the lowest rVc7 was estimated for Brisbane. When compared with Townsville, the estimated rVc7 in Cairns was lower from January to April and October to December 2015, but higher during the rest of the year (Fig. 3).
Estimation of the relative vectorial capacity of mosquitoes to transmit Zika virus in Queensland cities, Australia, from January 2015 - August 2016 and forecast from September to December 2016.
Lines: Estimation from observed temperatures; dash: Estimation from predicted temperatures The relative vectorial capacity was estimated by using rVc7. Red line shows mean of the threshold value of the epidemic potential; shaded region shows its variability range
From January to August 2016, the epidemic potential trend was similar to 2015 with the highest epidemic potential in Cairns (Fig. 3), and an estimated rVc7 of 0.123 in Brisbane, 0.154 in Rockhampton, 1.173 in Townsville, and 1.179 in Cairns. From September to November 2016, the monthly estimated epidemic potential based on the mean temperature median predictions was consistently the highest in Cairns, followed by Townsville, Rockhampton and Brisbane (Fig. 3), with estimates of 0.171, 0.164, 0.138, and 0.110, respectively. Then, from November to December 2016, Townsville has the highest estimated epidemic potential.
With a threshold value for a Zika outbreak fixed at rVc = 0.18 day-1, and assuming suitable transmission conditions without vector control programs, Cairns, Townsville and, to a lesser extent, Rockhampton, would have been suitable for ZIKV transmission during the warmer seasons in 2015 and 2016. When the threshold value is equal to 0.14, (Th equal to seven days), Brisbane would also become suitable for ZIKV transmission during the warmer months and Rockhampton, Townsville and Cairns, would have a longer potential transmission season for ZIKV. If, however, Th is equal to four days (rVc = 0.25 day-1), none of these cities would be suitable for ZIKV transmission. When the threshold value rVc varies within [0.14; 0.25], the suitability for each city to transmit ZIKV might change (see Fig. 3).
Discussion and Conclusions
Zika is a significant global public health issue. We demonstrate that, based on an average infectious period of 5.5 days17 , 18, Zika virus transmission by vector mosquitoes could have occurred in Cairns, Townsville and Rockhampton during the warmer months in 2015 and 2016, with Brisbane unsuitable for transmission. However, this changes when we take a lower epidemic potential threshold, based on a longer infectious period. Except for Brisbane where the vector is not yet established, these results are consistent with the epidemic potential of dengue virus in Cairns and Townsville.
While estimates are preliminary, these analyses point to the importance of further investigations of the infectious period as well as the infection and transmission rates of ZIKV and Australian mosquitoes (Ae. aegypti and Ae. albopictus) to allow more accurate estimates of the epidemic potential for ZIKV in Australia.
The Rio de Janeiro 2016 Olympics (5–21 August 2016) and the Paralympic Games (7–18 September 2016) were the two most prominent mass gathering events to take place in the Americas since the emergence of ZIKV in this region. A large number of visitors attended these events6. An upcoming event in Brazil that also attracts tourists from Australia is the Rio de Janeiro Carnival (24-28 February 2017), a period where mosquito abundance is highest (in Brazil as well as Queensland).
Our study considered only the risk posed by vector-mediated transmission and did not include consideration of the potential for sexual transmission19 , 20 , 21 which may occur across Australia, irrespective of the presence or absence of suitable vectors. Importantly, a recent study has shown that while sexual transmission increases the risk of infection and epidemic size (number of cases), by itself it may not initiate or sustain an outbreak22. Thus it is likely that vector-borne transmission is, by far, the greatest concern to vulnerable locations in Queensland.
More importantly, ZIKV poses a particular challenge in that 80% of cases have no symptoms, and thus would not be detected by a syndromic surveillance system23. We were particularly concerned with the prospect that infected travelers from the 2016 Rio Olympics or Paralympics games arriving in Cairns or Townsville might carry Zika, and our projections show that, in this event, epidemic transmission would have been low in winter, but possible during the warmer months in North Queensland.
Vector-borne transmission of ZIKV is expected to have a similar seasonal pattern to that of dengue and chikungunya, with lower transmission in winter. Nonetheless, the potential for vector-mediated transmission in the absence of overt cases due to asymptomatic infections will likely require a shift of focus for health authorities from emergency response currently effective for dengue case notifications toward broad-scale preventative programs, and emerging control methodologies (for example, Wolbachia, which is currently being released in Cairns and Townsville regions as a research field trial)24. The frequency of ZIKV importations into South East Queensland suggests that an investment in more comprehensive vector surveillance would be warranted to confirm the apparent absence of Ae. aegypti from Brisbane since the 1950s, and detect any incursions from the nearby endemic regions of Queensland. ZIKV transmission through blood transfusion is possible. Therefore, this virus poses a threat directly to blood safety, and indirectly on donor attendance.
This study has significant implications, highlighting the importance of adapting timely preventive measures and case management to an emerging arbovirus and underscores the public health challenges associated with mass gathering events involving the international movement of attendees returning to vulnerable cities. Although at this stage, the epidemic potential for early 2017 could not be forecast, it is likely that it will follow a similar trend to 2015-2016. Attendees of the Carnival in Brazil (along with other travelers visiting other zika-affected areas), who are traveling to Queensland where the vector is established, should follow the precautions and recommendations issued by their national health authorities. In north and parts of central Queensland where the vectors are present, immediate reporting of clinically suspected cases of ZIKV infection to local public health units is critical.
Corresponding Author
Elvina Viennet: eviennet@redcrossblood.org.au
Competing Interests
The authors have declared that there are no competing interests.
Data Availability
All relevant data have been made available in the figshare repository (DOI: 10.6084/m9.figshare.3993981).
Biographies
Gina Mincham has eight years’ experience in the field of research working for the Healthy Environments and Healthy People Research Group (prev. Mosquitoes and Public Health Research Group). She holds great experience in field and laboratory work as well as managing small research projects such as testing new mosquito repellents and assisting in testing new head lice treatment options available. Gina has extensive experience managing mosquito surveillance projects and has been issuing monthly SA Mosquito Intelligence Reports that are published by the Healthy Environments and Healthy People Research Group on-line. (http://www.unisa.edu.au/Research/Sansom-Institute-for-Health-Research/Research-at-the-Sansom/Research-Concentrations/Mosquitoes-and-Public-Health-Research-Group/Research-projects/) In 2011 she completed a Medical Entomology Master Class at James Cook University.In September 2013 Gina participated in the Australian Entomological Society’s 44th AGM and Scientific Conference – Invertebrates in Extreme Environments which included a presentation of a poster on urban wetlands pre and post-construction. In more recent times Gina has been involved with Australian research projects in medical entomology. These include studies of dengue in future climates. In her current role as a Research Assistant, she has been conducting the modelling of Aedes aegypti populations in North Queensland using the CIMSiM modelling package by putting together climate data and entomological data. This work also included the modelling of dengue transmission using the DENSiM modelling package. Currently Gina is assisting in a project modelling dengue transmission in China. Gina has experience in partnerships and continuous communications with local and state governments. All the field work she has been and is currently involved in includes the reporting and communication with local councils as well as responding to community complaints and concerns. Gina Mincham is qualified with a Bachelor of Science (Honours) in Health Science from the University of South Australia and is currently enrolled in the Masters of Population Health Practice looking at evaluating dengue management strategies using a simulation model for Guangzhou, Southern China.
Medical Entomologist, Metro North Public Health Unit, Queensland Health
I am a zoologist, general practitioner, epidemiologist and public health physician. I have general and specialist medical registration. I was appointed Associate Professor at the National Centre for Epidemiology and Population Health (NCEPH) & The Medical School at The Australian National University in 2008. Infectious disease epidemiology is a particular interest. Ross River virus, Australia’s most important climate sensitive arbovirus, is a long standing interest. I was lead author on the most comprehensive review of the virus, its ecology and clinical manifestations (cited over 250 times), a large mosquito trapping study for Ross River virus isolation and an important inception cohort study of disease natural history. I've also published on tuberculosis, Adenovirus, meningococcus, dengue and malaria. I worked as a doctor in Far North Queensland in the 1990s, gaining experience in high risk obstetrics, rural and remote medicine, Indigenous Health, and General Practice. During 2002-7 I managed adults with intellectual disabilities in a tertiary hospital setting. I'm particularly proud of my resarch on the use of antipsychotic medication for aggression in intellectually disabled adults - placebo is safer, cheaper and no less effective (Tyrer et al., Lancet, 2008). I continue to practice medicine. Interchange General Practice, where I work, is an accredited general practice training practice, and I'm accredited as a GP supervisor with the local training provider, GPSynergy. Annually from 2012 to 2015 I have been invited to teach for Institut Pasteur and Oxford University in Ho Chi Minh City, Vietnam. I've supervised students working in infectious disease epidemiology, Indigenous health, and the health of disabled people. I have significant international experience and exposure. As a consultant I have advised on outbreak investigation in Henan Province, China, vector-borne disease and climate change in Cambodia, and emerging disease surveillance in the Indian Ocean.
Leader of R&D Team within the Australian Red Cross Blood Service
Funding Statement
Funding for this study was made available through the Australian Red Cross Blood Service. Australian governments fund the Australian Red Cross Blood Service to provide blood, blood products and services to the Australian community.
Contributor Information
Elvina Viennet, Research and Development, Australian Red Cross Blood Service, Kelvin Grove, Queensland, Australia.
Gina Mincham, Centre for Population Health Research, University of South Australia, Adelaide, South Australia, Australia.
Francesca D. Frentiu, Institute of Health and Biomedical Innovation & School of Biomedical Sciences, Queensland University of Technology, Kelvin Grove, Queensland, Australia
Cassie C. Jansen, Metro North Public Health Unit, Metro North Hospital and Health Service, Windsor, Queensland, Australia
Brian L. Montgomery, Metro South Public Health Unit, Metro South Hospital and Health Service, Brisbane, Queensland, Australia
David Harley, Research School of Population Health, The Australian National University, Australian Capital Territory, Australia.
Robert L.P. Flower, Research and Development, Australian Red Cross Blood Service, Kelvin Grove, Queensland, Australia
Craig R. Williams, Centre for Population Health Research, University of South Australia, Adelaide, South Australia, Australia
Helen M. Faddy, Research and Development, Australian Red Cross Blood Service, Kelvin Grove, Queensland, Australia
References
- 1.Petersen LR, Jamieson DJ, Powers AM, Honein MA. Zika Virus. N Engl J Med. 2016;374(16):1552-63. [DOI] [PubMed]
- 2.Motta IJF, Spencer BR, Cordeiro da Silva SG, Arruda MB, Dobbin JA, Gonzaga YBM, et al. Evidence for Transmission of Zika Virus by Platelet Transfusion. N Engl J Med. 2016;375(11):1101-3. doi: doi:10.1056/NEJMc1607262. PubMed PMID: 27532622. [DOI] [PubMed]
- 3.Duffy MR, Chen T-H, Hancock WT, Powers AM, Kool JL, Lanciotti RS, et al. Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med. 2009;360(24):2536-43. doi: doi:10.1056/NEJMoa0805715. PubMed PMID: 19516034. [DOI] [PubMed]
- 4.Mlakar J, Korva M, Tul N, Popović M, Poljšak-Prijatelj M, Mraz J, et al. Zika Virus Associated with Microcephaly. N Engl J Med. 2016;374(10):951-8. doi: doi:10.1056/NEJMoa1600651. PubMed PMID: 26862926. [DOI] [PubMed]
- 5.Australian Government. Zika virus - notifications of Zika virus infection (Zika). In: Health Do, editor. 30 September 2016.
- 6.European Centre for Disease Prevention and Control. Rapid Risk Assessment. Zika virus disease epidemic: potential association with microcephaly and Guillain–Barré syndrome. Stockholm: ECDC, 2016 11 April 2016. [Accessed: 14 July 2016]
- 7.Russell RC, Currie BJ, Lindsay MD, Mackenzie JS, Ritchie SA, Whelan PI. Dengue and climate change in Australia: predictions for the future should incorporate knowledge from the past. Med J Aust. 2009;190(5):265-8. PubMed PMID: ISI:000265400000015 [DOI] [PubMed]
- 8.Australian Government BoM. Climate data online [Internet]. 2016 [Accessed: 14 July 2016];Available from:
- 9.Australian Government, Bureau of Meteorology. Climate outlooks – monthly and seasonal [Internet]. 2016 [Accessed: 28 July 2016]
- 10.Liu-Helmersson J, Stenlund H, Wilder-Smith A, Rocklöv J. Vectorial capacity of Aedes aegypti: Effects of temperature and implications for global dengue epidemic potential. PLoS ONE. 2014;9(3):e89783. doi: 10.1371/journal.pone.0089783. [DOI] [PMC free article] [PubMed]
- 11.Li MI, Wong PSJ, Ng LC, Tan CH. Oral Susceptibility of Singapore Aedes (Stegomyia) aegypti (Linnaeus) to Zika Virus. PLoS Negl Trop Dis. 2012;6(8):e1792. doi: 10.1371/journal.pntd.0001792. 10.1371/journal.pntd.0001792 [DOI] [PMC free article] [PubMed]
- 12.Chouin-Carneiro T, Vega-Rua A, Vazeille M, Yebakima A, Girod R, Goindin D, et al. Differential Susceptibilities of Aedes aegypti and Aedes albopictus from the Americas to Zika Virus. PLoS Negl Trop Dis. 2016;10(3):e0004543. doi: 10.1371/journal.pntd.0004543 [DOI] [PMC free article] [PubMed]
- 13.Hall-Mendelin S, Pyke AT, Moore PR, Mackay IM, McMahon JL, Ritchie SA, et al. Assessment of Local Mosquito Species Incriminates Aedes aegypti as the Potential Vector of Zika Virus in Australia. PLoS Negl Trop Dis. 2016;10(9):e0004959. doi: 10.1371/journal.pntd.0004959. [DOI] [PMC free article] [PubMed]
- 14.Boorman JP, Porterfield JS. A simple technique for infection of mosquitoes with viruses; transmission of Zika virus. Trans R Soc Trop Med Hyg. 1956;50(3):238-42. Epub 1956/05/01. PubMed PMID: 13337908; [DOI] [PubMed]
- 15.Lambrechts L, Paaijmans KP, Fansiri T, Carrington LB, Kramer LD, Thomas MB, et al. Impact of daily temperature fluctuations on dengue virus transmission by Aedes aegypti. Proc Natl Acad Sci USA. 2011;108(18):7460-5. PubMed PMID: ISI:000290203100040; [DOI] [PMC free article] [PubMed]
- 16.Liu-Helmersson J, Quam M, Wilder-Smith A, Stenlund H, Ebi K, Massad E, et al. Climate Change and Aedes Vectors: 21st Century Projections for Dengue Transmission in Europe. EBioMedicine. 2016;7:267-77. [DOI] [PMC free article] [PubMed]
- 17.Mallet HP, Vial AL, Musso D. Bilan de l’épidémie a virus ZIKA en Polynésie Francaise 2013–2014. 2015;Available from:
- 18.Kucharski AJ, Funk S, Eggo RM, Mallet H-P, Edmunds WJ, Nilles EJ. Transmission Dynamics of Zika Virus in Island Populations: A Modelling Analysis of the 2013–14 French Polynesia Outbreak. PLoS Negl Trop Dis. 2016;10(5):e0004726. doi: 10.1371/journal.pntd.0004726. [DOI] [PMC free article] [PubMed]
- 19.Mansuy JM, Dutertre M, Mengelle C, Fourcade C, Marchou B, Delobel P, et al. Zika virus: high infectious viral load in semen, a new sexually transmitted pathogen? Lancet Infect Dis. 16(4):405. doi: 10.1016/S1473-3099(16)00138-9. [DOI] [PubMed]
- 20.Venturi G, Zammarchi L, Fortuna C, Remoli ME, Benedetti E, Fiorentini C, et al. An autochthonous case of Zika due to possible sexual transmission, Florence, Italy, 2014. Euro Surveill. 2016;21(8). Epub 2016/03/05. doi: 10.2807/1560-7917.es.2016.21.8.30148. PubMed PMID: 26939607; [DOI] [PubMed]
- 21.Canada’s first case of sexually-transmitted Zika virus confirmed in Ontario [Internet]. April 25, 2016. Available from:
- 22.Gao D, Lou Y, He D, Porco TC, Kuang Y, Chowell G, et al. Prevention and Control of Zika as a Mosquito-Borne and Sexually Transmitted Disease: A Mathematical Modeling Analysis. Scientific Reports. 2016;6:28070. doi: 10.1038/srep28070. [DOI] [PMC free article] [PubMed]
- 23.What real threat does Zika pose to the Rio Olympics? History has an answer [Internet]. February 12, 2016 [Accessed: 15 May 2016]. Available from:
- 24.Ritchie S. Rear and release: a new paradigm for dengue control. Austral Entomology. 2014;53(4):363-7. doi: 10.1111/aen.12127.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data have been made available in the figshare repository (DOI: 10.6084/m9.figshare.3993981).