Abstract
The relationship between cigarette smoking and depressive symptoms is well-established. Dispositional mindfulness has been associated with lower depressive symptoms, lower smoking dependence, and higher odds of smoking cessation. Given that mindfulness is multi-faceted, the current study examined which facets of mindfulness might mediate the relationship between depressive symptoms and smoking behavior. Participants (n = 72) completed the Smoking Consequences Questionnaire (SCQ), Center for Epidemiologic Studies Depression Scale (CESD), and Kentucky Inventory of Mindfulness Skills (KIMS; subscales-Observe, Describe, Acting with Awareness, Accepting without Judgment), and indicated number of cigarettes smoked per day (CPD). Simple mediation models (followed by multiple mediation when more than one facet was significant) tested whether mindfulness facets mediated the relationship between CESD and smoking behavior (CPD and SCQ subscales). Results indicated that 1) lower depressive symptoms were associated with higher Accepting without Judgment, which was related to lower Negative Reinforcement expectancies, 2) lower depressive symptoms were associated with increased Describe, which was associated with greater perceived Negative Consequences, 3) lower depressive symptoms were associated with higher Accepting without Judgment, which was associated with lower Negative Consequences expectancies, and 4) higher depressive symptoms were associated with higher scores on Observe, which related to both greater Positive Reinforcement and Negative Consequences expectancies. Greater Accepting without Judgment and Describe aspects of mindfulness may serve as protective factors in the relationship of depressive symptoms and smoking.
Keywords: mindfulness, depressive symptoms, smoking, mediation
Introduction
Cigarette smoking and depression are highly comorbid in adults. Forty-three percent of adults experiencing depression (defined as a score of 10 or higher on the Patient Health Questionnaire [PHQ-9]) currently smoke cigarettes (Pratt & Brody, 2010), compared to 16.8% of the general population of adults in the United States (Centers for Disease Control and Prevention [CDC], 2015). Individuals with elevated depressive symptoms have higher levels of tobacco dependence (i.e., report smoking more cigarettes per day, smoke more quickly upon awakening, endorse higher positive and negative reinforcement smoking expectancies) and have greater difficulty quitting smoking than those without depression (Pratt & Brody, 2010; Vinci, McVay, Copeland, & Carrigan, 2012). Identifying factors to aid smokers in managing depressive symptoms is one potential avenue for reducing smoking frequency and promoting cessation.
Mindfulness, the ability to purposefully direct one’s attention to the present moment without judging the experience as good or bad (Kabat-Zinn, 1994), may serve as a protective factor in the relationship between depression and smoking behavior. Mindfulness can be viewed as a dispositional or trait factor (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006), as well as a state or modifiable ability that can be enhanced through practice (Lau et al., 2006; Thompson & Waltz, 2007). Prior research has indicated that dispositional mindfulness is associated with lower depressive symptoms (Barnhofer, Duggan, & Griffith, 2011; Deng, Li, & Tang, 2014; Smith et al., 2011), lower nicotine dependence (Vidrine et al., 2009), and higher odds of smoking cessation (Heppner et al., 2016; Spears et al., 2016). Treatment studies support the utility of mindfulness-based interventions for reducing symptoms of depression (Hoffman, Sawyer, Witt, & Oh, 2010; Teasdale, Segal, Williams, Ridgeway, Soulsby, & Lau, 2000) and promoting smoking cessation (Brewer et al., 2011; Davis, Fleming, Bonus, & Baker, 2007; Davis, Goldberg, Anderson, Manley, Smith, & Baker. 2014; Davis, Manley, Goldberg, Smith, & Jorenby, 2014; Davis et al., 2013; Vidrine et al., 2016).
Mindfulness has been conceptualized as a multidimensional construct (Baer, Smith, & Allen, 2004), and research has begun to examine the roles of specific facets of mindfulness in predicting psychological functioning. For example, the Kentucky Inventory of Mindfulness Skills (KIMS), which has four subscales: 1) Observing (attending to various internal and external experiences, 2) Describing (labeling experiences without judging them), 3) Acting with Awareness (being fully present in the current experience), and 4) Accepting without Judgment (allowing the present experience to be what it is, without judging it or trying to change it in any way; also known as Nonjudging; Baer et al., 2004).
While scarce, some research has begun to examine relationships between facets of mindfulness and depression. Among a combined sample of experienced meditators and college students, Cash and Whittingham (2010) found that higher levels of Acting with Awareness and Nonjudging were associated with lower depressive symptoms. Christopher, Neuser, Michael, and Baitmangalkar (2012) found that Acting with Awareness, Nonjudging, and Nonreactivity (noticing current experiences without immediately reacting to them) were associated with fewer depressive symptoms among a sample of community participants, whereas Observe was positively associated with depressive symptoms. Finally, Desrosiers and et al. (2013) found that within a sample of treatment-seeking adults, Nonjudging was associated with lowered depressive symptoms. Based on these findings, it appears that Acting with Awareness and Nonjudging are two facets of mindfulness that are most consistently linked to lower depressive symptoms in various samples.
A recent meta-analysis examining the relationship between facets of mindfulness and substance use behaviors found that Acting with Awareness, Nonjudging, and Nonreactivity are negatively associated with substance use (Karyadi, VanderVeen, & Cyders, 2014). The literature examining smoking behaviors specifically is very limited, but has found that among college students, Acting with Awareness was associated with smoking fewer cigarettes per day (Roberts & Danoff-Burg, 2010). Furthermore, among a sample of Latino smokers attempting to quit, Nonjudging was the only facet to predict long-term smoking abstinence (Spears et al., 2016).
The current study attempted to advance the scientific literature on the role that specific facets of mindfulness might play in the relationship between depressive symptoms and smoking behavior (cigarettes smoked per day and smoking expectancies). Based on previous research, we hypothesized that the facets of Acting with Awareness and Accepting without Judgment would be significant mediators of the relationship between depressive symptoms and smoking behavior. That is, individuals experiencing depressive symptoms may be more likely to act on “autopilot” (rather than being mindfully aware of their moment-to-moment actions) and more judgmental of their thoughts and emotions, both of which could increase risk for smoking.
Method
Participants
Participants were undergraduate students who enrolled in the study for course credit (the campus was not smoke-free at the time of this study). There were no specific inclusion or exclusion criteria to complete the study (other than being currently enrolled as a student at this university), and participants could complete the survey at any time during the semester. However, for the current analysis, only individuals who indicated that they smoked at least one cigarette per day were included (hence all participants were daily smokers).
Procedures
Participants completed all study procedures through a secure, online data collection website. After completing the online informed consent, all participants completed a series of questionnaires. Those relevant to the current study are presented here. All procedures were approved by the university’s Institutional Review Board.
Measures
Demographic Information and Tobacco Use
Participants completed a series of questions to indicate their gender, age, and race/ethnicity. They were also asked to report how many cigarettes they smoked per day (CPD) and for how long they had smoked.
Smoking Consequences Questionnaire (SCQ; Brandon & Baker, 1991)
The SCQ is a 50-item self-report measure that asks participants to answer questions related to their expectancies when smoking cigarettes on a 9-point Likert scale. The SCQ has four subscales – Negative Consequences (indicates negative consequences expected from smoking, such as health problems), Negative Reinforcement (represents expectations of negative reinforcement from smoking [primarily negative affect reduction]), Positive Reinforcement (represents smoking expectancies related to the positive effects of smoking, such as taste and mood enhancement), and Weight Control (indicates expectations of appetite and weight control from smoking). Internal consistency for the SCQ in the current sample was high (Chronbach’s alpha = .97).
Kentucky Inventory of Mindfulness Skills (KIMS; Baer, Smith, & Allen, 2004)
The KIMS is a 39-item self-report measure that assesses level of trait mindfulness according to a 5-point Likert scale. The KIMS has four subscales: Observing, Describing, Acting with Awareness, and Accepting without Judgment. Internal consistency for the KIMS was high in the current sample (Chronbach’s alpha = .93).
Center for Epidemiological Studies Depression Scale (CESD; Radloff, 1977)
The CESD is a 20-item self-report questionnaire that assesses depressive symptoms that were experienced within the past week. Participants rated their responses on a 4-point Likert scale. Internal consistency for the CESD in the current sample was high (Chronbach’s alpha = .93).
Data Analyses
First, linear regression analyses were conducted to examine unique associations between depressive symptoms and smoking outcomes. Separate regression analyses were conducted for each dependent variable (CPD and each subscale of the SCQ – Negative Consequences, Negative Reinforcement, Positive Reinforcement, Weight Control), controlling for gender, and age. CPD was also controlled in analyses predicting SCQ subscales.
Second, linear regression was utilized to examine the unique associations between facets of mindfulness and smoking outcomes, controlling for the same covariates as noted above, in addition to depressive symptoms. Dependent variables were CPD and the four subscales of the SCQ.
Third, simple mediation models tested whether any of the facets of mindfulness mediated the relationship between depressive symptoms and smoking outcome (CPD and the four subscales of the SCQ). Facets were entered individually as mediators for each model. Gender, age, and CPD (CPD for the SCQ models only) were entered as covariates. For those models indicating that multiple facets of mindfulness significantly mediated the relationship between depressive symptoms and a given smoking outcome, those significant facets were entered together into a multiple mediation model to determine whether any facets remained significant mediators over and above the others. All mediation models were conducted using Hayes’ (2013) PROCESS macro (model number = 4). Five thousand bootstrapped samples estimated the indirect effect; bias-corrected confidence intervals were established around the estimated indirect effect. This approach to mediation allows the indirect effect to be independent from the total effect. Therefore, in order for mediation to occur, the total effect does not have to be significant (Hayes, 2013). Additionally, this approach does not require normality of the distribution of the sample, and thus has greater statistical power (Hayes, 2013).
Results
Participants (n = 72) were 75% female and 94.4% Caucasian, with an average age of 21.44 (SD = 4.87). Participants indicated smoking an average of 6.99 (SD = 5.78) cigarettes per day for an average of 51 months (SD = 55) and a median of 36 months. The average CESD score was 22.83 (SD = 9.86), suggesting risk for clinical depression based on a commonly used cut-off score of 16 (Radloff, 1977). The average score on each KIMS subscale is as follows: Observing (M = 2.94, SD = .78), Describing (M = 3.13, SD = .98), Acting with Awareness (M = 2.74, SD = .60), and Accepting without Judgment (M = 3.42, SD = 1.16). Although the sample ranged from rating KIMS items as 1 (never or rarely true) to 5 (very often or always true), on average participants rated the mindfulness items as “sometimes true” for them.
Three sets of results are presented below. First, associations between depressive symptoms and smoking variables are described. Second, associations between facets of mindfulness and smoking variables are presented. Finally, results of simple and multiple mediation models are presented in order to shed light on which aspects of mindfulness might mediate relationships between depressive symptoms and smoking outcome.
Associations between Depressive Symptoms and Smoking Variables
Greater depressive symptoms were associated with smoking more cigarettes per day, and higher scores on Negative Consequences, Negative Reinforcement, and Positive Reinforcement, after controlling for gender, age, and CPD. Depressive symptoms were not associated with the Weight Control subscale. See Table 1.
Table 1.
Associations between Depressive Symptoms and Smoking Variables
| CPD | SCQ Negative Consequences | SCQ Negative Reinforcement | SCQ Positive Reinforcement | SCQ Weight Control | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| t | β | t | β | t | β | t | β | t | β | |
| Gender | .85 | .10 | 3.64** | .39 | 2.95** | .31 | 2.38* | .24 | .15 | .02 |
| Age | 1.63 | .19 | 1.15 | .12 | −2.36* | −.25 | −1.12 | −.11 | −.70 | −.09 |
| CPD | - | - | .41 | .05 | 1.02 | .11 | 1.64 | .17 | 1.44 | .19 |
| CESD | 2.56* | .30 | 3.62** | .41 | 3.08** | .34 | 4.90** | .51 | 1.18 | .16 |
| Adj R2 | .10 | .37 | .31 | .43 | .03 | |||||
| F | 3.59* | 9.25** | 8.33** | 12.44** | 1.43 | |||||
Note. CPD = Cigarettes Smoked per Day; CESD = Center for Epidemiologic Studies Depression; SCQ = Smoking Consequences Questionnaire; β = standardized coefficient
p < .05;
p < .01
Associations between Facets of Mindfulness and Smoking Variables
Accepting without Judgment was associated with smoking significantly fewer cigarettes per day, after controlling for gender, age, CPD, and depressive symptoms. Accepting without Judgment was also associated with lower Negative Reinforcement expectancies (after controlling for CPD, demographics, and depressive symptoms). None of the KIMS subscales predicted Negative Consequences, Positive Reinforcement, or Weight Control subscales. See Table 2 for a complete summary of these findings.
Table 2.
Associations between Mindfulness Facets and Smoking Variables
| CPD | SCQ Negative Consequences | SCQ Negative Reinforcement | SCQ Positive Reinforcement | SCQ Weight Control | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| t | β | t | β | t | β | t | β | t | β | |
| Gender | 1.52 | .18 | 3.18** | .34 | 3.37** | .32 | 1.75 | .18 | .23 | .03 |
| Age | 1.86 | .21 | .93 | .10 | −2.68* | −.25 | −1.36 | −.14 | −.78 | −.10 |
| CPD | - | - | .81 | .09 | .59 | .06 | 1.98 | .23 | .76 | .11 |
| CESD | .80 | .13 | 1.91 | .28 | .37 | .05 | 3.18** | .44 | .91 | .16 |
| KIMS Observe | −.95 | −.15 | 1.04 | .15 | .99 | .12 | 1.07 | .15 | −.48 | −.08 |
| KIMS Describe | −1.23 | −.16 | 1.83 | .21 | 1.06 | .11 | 1.33 | .15 | .90 | .13 |
| KIMS Acting with Awareness | 1.93 | .22 | −1.39 | −.15 | −1.23 | −.11 | −1.27 | −.13 | 1.55 | .20 |
| KIMS Accepting without Judgment | −2.18* | −.35 | −.88 | −.14 | −3.38** | −.45 | −.09 | −.01 | −1.14 | −.21 |
| Adj R2 | .18 | .44 | .52 | .46 | .04 | |||||
| F | 3.13** | 6.63** | 9.52** | 7.15** | ||||||
Note. CPD = Cigarettes Smoked per Day; CESD = Center for Epidemiologic Studies Depression; SCQ = Smoking Consequences Questionnaire; β = standardized coefficient
p < .05;
p < .01
Mediators of Associations between Depressive Symptoms and Smoking
Significant results from the simple mediation models are presented here, followed by the multiple mediation outcomes when relevant. Table 3 presents the results of each significant simple mediation model.
Table 3.
Significant Simple Mediation Results Listed by Smoking Outcome
| B | SE B | LLCI | ULCI | |
|---|---|---|---|---|
| Negative Consequences: Observing mediated CESD and Negative Consequences expectancies | ||||
| ab (indirect effect) | .498 | .232 | .132 | 1.027 |
| Negative Consequences: Describing mediated CESD and Negative Consequences expectancies | ||||
| ab (indirect effect) | −.231 | .164 | −.659 | −.008 |
| Negative Consequences: Accepting without Judgment mediated CESD and Negative Consequences expectancies | ||||
| ab (indirect effect) | .555 | .347 | .003 | 1.323 |
| Negative Reinforcement: Observing mediated CESD and Negative Reinforcement expectancies | ||||
| ab (indirect effect) | .527 | .216 | .195 | 1.059 |
| Negative Reinforcement: Accepting without Judgment mediated CESD and Negative Reinforcement expectancies | ||||
| ab (indirect effect) | .900 | .229 | .529 | 1.464 |
| Positive Reinforcement: Observing mediated CESD and Positive Reinforcement expectancies | ||||
| ab (indirect effect) | .332 | .207 | .017 | .834 |
Note. CPD = Cigarettes Smoked per Day; CESD = Center for Epidemiologic Studies Depression; SE = Standard Error
In the simple mediation models, Observe, Describe, and Accepting without Judgment each mediated the relationship between depressive symptoms and Negative Consequences. Specifically, higher depressive symptoms were associated with higher scores on Observe, which was associated with greater Negative Consequences expectancies; lower depressive symptoms were associated with higher Describe, which was associated with endorsement of greater Negative Consequences; lower depressive symptoms were associated with higher Accepting without Judgment, which was associated with lower Negative Consequences expectancies. When all three of these facets were entered into the multiple mediation model, none of the mindfulness facets uniquely mediated the relationship between depressive symptoms and Negative Consequences.
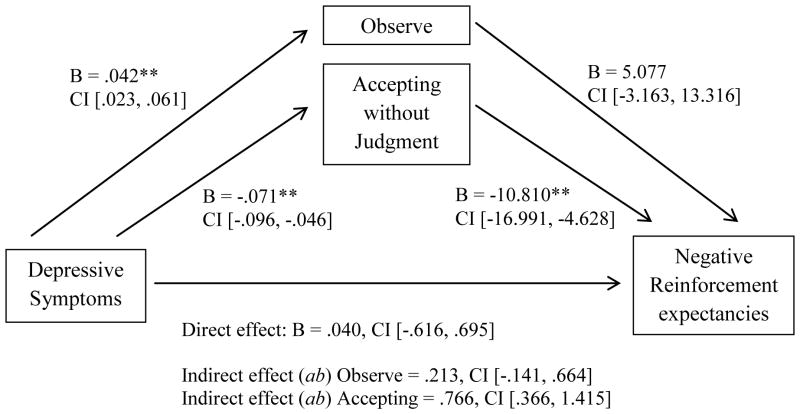
In the simple mediation models, Observe and Accepting without Judgment mediated the relationship between depressive symptoms and Negative Reinforcement. When these two mindfulness facets were entered into the multiple mediation model, Accepting without Judgment was the only significant mediator. Specifically, lower depressive symptoms were associated with higher Accepting without Judgment, which was related to lower Negative Reinforcement expectancies. See Figure 1 for the results of the multiple mediation model.
Figure 1.
Multiple Mediator Model: Accepting without Judgment significantly Mediated the Relationship between Depressive Symptoms and Negative Reinforcement Expectancies (* = p < .05; ** = p < .01)
In the simple mediation models, only Observe mediated the relationship between depressive symptoms and Positive Reinforcement, such that greater depressive symptoms were associated with higher scores on Observe, which were related to greater Positive Reinforcement expectancies.
Discussion
The primary aim of this cross-sectional study was to examine unique relationships among facets of mindfulness, depressive symptoms, and smoking behaviors. Consistent with previous literature, we found that greater depressive symptoms were associated with smoking more cigarettes per day and with higher endorsement of Negative Consequences, Negative Reinforcement, and Positive Reinforcement smoking expectancies. Results also indicated that Accepting without Judgment was uniquely associated with smoking fewer cigarettes per day and lower Negative Reinforcement Expectancies. Mediational models determined that 1) the mindfulness facets of Observe, Describe, and Accepting without Judgment each uniquely mediated the relationship between depressive symptoms and Negative Consequences expectancies about smoking (although the direction of relationships varied for different facets of mindfulness as described below), 2) greater Accepting without Judgment mediated the relationship between lower depressive symptoms and lower Negative Reinforcement expectancies, and 3) greater Observe mediated the relationship between higher depressive symptoms and higher Positive Reinforcement expectancies. To our knowledge, these analyses are the first to examine the relationship between facets of mindfulness, depressive symptoms and smoking behavior, and shed light on the complicated nature of these relationships.
We found that the Accepting without Judgment facet appears to be a particularly important component of mindfulness when examining how it relates to depressive symptoms and smoking. Not only was Accepting without Judgment associated with lower nicotine dependence, but it also mediated the relationship between depressive symptoms and Negative Reinforcement expectancies, such that lower depressive symptoms were associated with higher Accepting without Judgment, which was associated with lower Negative Reinforcement expectancies (e.g., “When I’m angry a cigarette can calm me down; Smoking helps me deal with depression.”). That is, an individual who is not experiencing depressive symptoms may be more able to mindfully sit with uncomfortable thoughts/emotions/sensations without judging them (or themselves) as “bad,” which is less likely to trigger smoking in attempt to eliminate such experiences. On the other hand, a depressed individual who does judge his/her thoughts/emotions/sensations as “bad” may be more likely to smoke in an attempt to get rid of these unpleasant experiences. These findings suggest that the acceptance facet may serve as a protective factor in the relationship between depressive symptoms and smoking behavior. Recently, Spears et al. (2016) found that among a Hispanic sample of adults making a quit attempt, Nonjudging was the only mindfulness facet that predicted long-term smoking abstinence. Thus, when considering both smoking behavior and smoking cessation, acceptance appears to be a very important component of mindfulness that likely serves as a protective factor.
Regarding Positive Reinforcement, greater depressive symptoms were associated with higher scores on Observe, which were then associated with higher endorsement of Positive Reinforcement expectancies for smoking (e.g., “I like to watch the smoke from my cigarette; I really enjoy a cigarette when I’m relaxed and feeling good; I enjoy the taste sensations while smoking”). In other words, an individual with depressive symptoms might be especially attuned to internal and external sensations (particularly those that are uncomfortable or distressing), which could increase the perceived need to smoke to enhance mood. It makes sense that the tendency to notice depressive thoughts/emotions/sensations (perhaps with a judgmental, rather than accepting attitude) would increase the likelihood of smoking in attempt to increase mood. These results suggest that Observe (at least when not combined with other mindfulness facets) may not be a particularly beneficial mindfulness facet regarding depressive symptoms and smoking expectancies. This finding is consistent with prior research suggesting that whereas most facets of mindfulness are associated with better psychosocial functioning, Observe is not uniquely helpful in samples of non-meditators (Baer et al., 2008; Cebolla et al., 2012). It may be that Observe confers benefits when combined with other facets (e.g., Observe may be more beneficial among long-term meditators who have learned to observe sensations non-judgmentally over time; Baer et al., 2008). Future research should determine whether Observe, when combined with other components of mindfulness (e.g., Accepting without Judgment), may serve in a different capacity in the relationship between depressive symptoms and Positive Reinforcement.
Regarding the Negative Consequences subscale, first, the relationship between higher depressive symptoms and higher endorsement of Negative Consequences from smoking was explained by higher Observe. That is, depressed individuals may be more likely to observe and notice present-moment thoughts/emotions/sensations, leading to higher expectancies that smoking is related to negative consequences. Thus, depressed individuals might be more aware of the negative consequences of smoking, and this could be explained through their ability to observe present-moment experiences. These findings make sense in light of the theory of depressive realism, which suggests that depressed individuals are able to make observations that are more accurate than non-depressed individuals (Alloy & Abramson, 1988; Moore & Fresco, 2012). In our sample, more depressed individuals endorsed that smoking has greater negative consequences, and this relationship could be explained by having an increased awareness of sensations (e.g., greater awareness of difficulties breathing associated with smoking). Second, lower depressive symptoms were related to higher Describe, which was associated with higher endorsement of Negative Consequences for smoking. That is, individuals with fewer depressive symptoms may be more able to describe their experiences in words. Having the ability to articulate these experiences (e.g., frustration about not being able to breathe as easily) might increase the likelihood of acknowledging the negative consequences of smoking. These results suggest that the ability to describe thoughts/emotions/sensations may serve as a protective factor in the relationship between depressive symptoms and Negative Consequence expectancies.
Third, lower depressive symptoms were associated with higher Accepting without Judgment skills, which was associated with lower endorsement of Negative Consequences from smoking (i.e., these individuals perceived fewer negative consequences of smoking). This finding is somewhat surprising and counterintuitive, as we would expect accepting skills to be related to a higher endorsement of Negative Consequences for smoking. Upon further examination of the actual statements that comprise the Negative Consequences subscale, some phrases have a strong judgmental component (e.g., “I look ridiculous while smoking; Smoking makes me seem less attractive; People think less of me if they see me smoking.”). While these statements certainly do not make up the majority of the subscale, it is likely that individuals with high acceptance might rate these phrases as less true for them. Additional research on the relationship between Accepting without Judgment and Negative Consequences expectancies would aid in further understanding this relationship.
Our findings support the need to examine the multidimensional construct of mindfulness by closely exploring how individual facets relate to outcomes of interest. While overall we found support that mindfulness is likely a protective factor in the relationship between depressive symptoms and smoking behavior, this finding was not uniform across facets (e.g., Observe). To our knowledge, only one prior study has examined how facets of mindfulness uniquely relate to smoking cessation (Spears et al., 2016). That said, research on other substance use behaviors, such as alcohol, has shown that certain facets of mindfulness (e.g., Acting with Awareness, Nonjudging) are uniquely associated with decreased problematic alcohol use (Fernandez, Wood, Stein, & Rossi, 2010; Murphy & MacKillop, 2011; Reynolds, Keough, & O’Connor, 2015; Vinci, Spears, Peltier, & Copeland, 2016). Similar findings have been found when examining the relationship between depressive symptoms and facets of mindfulness (Cash & Whittingham, 2010; Christopher et al., 2012; Desrosiers et al., 2013).
Given that smoking is the leading preventable cause of morbidity and mortality (US Department of Health and Human Services, 2014), our findings have important clinical implications. Accepting without Judgment and Describe both served as protective facets in the relationship between depressive symptoms and Negative Reinforcement and Negative Consequences expectancies, respectively, and efforts to target these mindfulness facets through treatment should be explored, particularly among depressed individuals. For example, treatment could encourage bringing a non-judgmental perspective to thoughts/emotions/sensations that are related to depression (i.e., practicing acceptance) without trying to get rid of them by smoking. Smokers could also be encouraged to describe in words the physical sensations that they experience (e.g., how it feels to experience some of the physical consequences of smoking; how it feels to breathe more freely when they have not smoked for a while) in order to increase perceived consequences of smoking (and perhaps increase motivation to quit). Future research is needed to examine how mindfulness-based treatments for smokers can best target certain facets of mindfulness (e.g., Accepting without Judgment) that might be most beneficial with regard to enhancing cessation in depressed smokers.
Limitations and avenues for future research should be noted. First, these results are cross sectional and casual interpretations cannot be made; future research should examine these constructs in a longitudinal manner. Second, the study consisted of a somewhat small sample of college student smokers who were predominately female and Caucasian; these results may or may not generalize to other smoking populations. Future research should explore the role that mindfulness facets might play in the relationship between depressive symptoms and smoking behavior in other types of samples (e.g., clinically depressed individuals; racially/ethnically diverse smokers; treatment-seeking samples). A particularly interesting future avenue of research would be to explore the role of trait mindfulness among depressed smokers making a quit attempt. Additionally, we did not examine whether our mediational results differed for men vs women due to the low percentage of men in our sample; future research should explore any gender differences among the variables examined here. Third, we used the KIMS rather than the FFMQ, which is now a more commonly used multidimensional measure of mindfulness. It is possible that aspects of mindfulness that are not captured by the KIMS (e.g., Nonreactivity, which is a subscale of the FFMQ but not the KIMS; Baer et al., 2006) may also be important in the relationship between depressive symptoms and smoking-related outcomes. Fourth, the ability of individuals to assess their own level of trait mindfulness is an inherent limitation when using self-report measures of mindfulness and should be considered when interpreting the findings. Fifth, we did not ask participants about any previous experiences they may have had with mindfulness practices, which should be considered in future research when assessing mindfulness.
The current findings suggest that facets of mindfulness uniquely mediate the relationship between depressive symptoms and smoking behavior, which to our knowledge has not been previously examined. Accepting without Judgment and Describe appear to serve as protective factors, whereas the facet of Observe predicted increased positive reinforcement expectancies from smoking. It is possible that Observe may best function in combination with other facets (although additional research is needed to confirm this hypothesis). Future research should continue to examine specific components of mindfulness in order to better inform mindfulness-based treatments for smoking cessation that target depressed individuals.
Footnotes
Ethical Standards
All data collection procedures presented here were approved by the University’s Institutional Review Board (IRB) and thus have been performed in accordance with the ethical standards in the 1964 Declaration of Helsinki and its later amendments.
The authors declare no conflict of interest.
References
- Alloy LB, Abramson LY. Depressive realism: Four theoretical perspectives. In: Alloy LB, editor. Cognitive processes in depression. New York, NY: Guildford; 1988. pp. 223–265. [Google Scholar]
- Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: The Kentucky Inventory of Mindfulness Skills. Assessment. 2004;11(3):191–206. doi: 10.1177/1073191104268029. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, … Williams JMG. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15:329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Barnhofer T, Duggan DS, Griffith JW. Dispositional mindfulness moderates the relation between neuroticism and depressive symptoms. Personality and Individual Differences. 2011;51:958–962. doi: 10.1016/j.paid.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon T, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychological Assessment. 1991;3:484–491. [Google Scholar]
- Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, Rounsaville BJ. Mindfulness training for smoking cessation: Results from a randomized controlled trial. Drug and Alcohol Dependence. 2011;119:72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cash M, Whittingham K. What facets of mindfulness contribute to psychological well-being and depressive, anxious, and stress-related symptomatology? Mindfulness. 2010;1:177–182. [Google Scholar]
- Cebolla A, Garcia-Palacios A, Soler J, Guillen V, Banos R, Botella C. Psychometric properties of the Spanish validation of the five facets of mindfulness questionnaire. The European Journal of Psychiatry. 2012;26:118–126. [Google Scholar]
- Centers for Disease Control and Prevention. Current Cigarette Smoking Among Adults—United States, 2005–2014. Morbidity and Mortality Weekly Report. 2015;64(44):1233–1240. doi: 10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- Christopher MS, Neuser NJ, Michael PG, Baitmangalkar A. Exploring the psychometric properties of the five facet mindfulness questionnaire. Mindfulness. 2012;3:124–131. [Google Scholar]
- Davis JM, Fleming MF, Bonus KA, Baker TB. A pilot study on mindfulness based stress reduction for smokers. BMC Complementary and Alternative Medicine. 2007;7:2. doi: 10.1186/1472-6882-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Goldberg SB, Anderson MC, Manley AR, Smith SS, Baker TB. Randomized trial on mindfulness training for smokers targeted to a disadvantaged population. Substance Use and Misuse. 2014;49(5):571–585. doi: 10.3109/10826084.2013.770025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Manley AR, Goldberg SB, Smith SS, Jorenby DE. Randomized trial comparing mindfulness training for smokers to a matched control. Journal of Substance Abuse Treatment. 2014;47(3):213–221. doi: 10.1016/j.jsat.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Mills DM, Stankevitz KA, Manley AR, Majeskie MR, Smith SS. Pilot randomized trial on mindfulness training for smokers in young adult binge drinkers. BMC Complementary and Alternative Med. 2013;13:215. doi: 10.1186/1472-6882-13-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng Y, Li S, Tang Y. The relationship between wandering mind, depression and mindfulness. Mindfulness. 2014;5:124–128. [Google Scholar]
- Desrosiers A, Klemanski DH, Nolen-Hoeksema S. Mapping mindfulness facets onto dimensions of anxiety and depression. Behavior Therapy. 2013;44:373–384. doi: 10.1016/j.beth.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez AC, Wood MD, Stein AR, Rossi JS. Measuring mindfulness and examining its relationship with alcohol use and negative consequences. Psychology of Addictive Behaviors. 2010;24:608–616. doi: 10.1037/a0021742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis. New York, NY: Guilford Press; 2013. [Google Scholar]
- Heppner WL, Spears CA, Correa-Fernandez V, Castro Y, Li ZY, Guo B, … Wetter DW. Dispositional mindfulness predicts enhanced smoking cessation and smoking lapse recovery. Annals of Behavioral Medicine. 2016 doi: 10.1007/s12160-015-9759-3. online first. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman SG, Sawyer AT, Witt AA, Oh D. The effects of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are: Mindfulness in everyday life. New York, NY: Hyperion; 1994. [Google Scholar]
- Karyadi KA, VanderVeen JD, Cyders MA. A meta-analysis of the relationship between trait mindfulness and substance use behaviors. Drug and Alcohol Dependence. 2014;143:1–10. doi: 10.1016/j.drugalcdep.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau MA, Bishop SR, Segal ZV, Buis T, Anderson ND, Carlson L, Carmody J. The Toronto Mindfulness Scale: Development and validation. Journal of Clinical Psychology. 2006;62:1445–1467. doi: 10.1002/jclp.20326. [DOI] [PubMed] [Google Scholar]
- Moore MT, Fresco DM. Depressive realism: A meta-analytic review. Clinical Psychology Review. 2012;32:496–509. doi: 10.1016/j.cpr.2012.05.004. [DOI] [PubMed] [Google Scholar]
- Murphy C, MacKillop J. Living in the here and now: Interrelationships between impulsivity, mindfulness, and alcohol misuse. Psychopharmacology. 2011;219:527–536. doi: 10.1007/s00213-011-2573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt LA, Brody DJ. NCHS data brief, no 34. Hyattsville, MD: National Center for Health Statistics; 2010. Depression and smoking in the US household populations aged 20 and over, 2005–2008. [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general populations. Applied Psychological Measurement. 1977;1:384–401. [Google Scholar]
- Reynolds A, Keough MT, O’Connor RM. Is being mindfulness associated with reduced risk for internally-motivated drinking and alcohol use among undergraduates? Addictive Behaviors. 2015;42:222–226. doi: 10.1016/j.addbeh.2014.11.027. [DOI] [PubMed] [Google Scholar]
- Roberts KC, Danoff-Burg S. Mindfulness and health behaviors: Is paying attention good for you? Journal of American College Health. 2010;59:165–173. doi: 10.1080/07448481.2010.484452. [DOI] [PubMed] [Google Scholar]
- Smith BW, Ortiz A, Steffen LE, Tooley EM, Wiggins KT, Yeater EA, … Bernard ML. Mindfulness is associated with fewer PTSD symptoms, depressive symptoms, physical symptoms, and alcohol problems in urban firefighters. Journal of Consulting and Clinical Psychology. 2011;79:613–617. doi: 10.1037/a0025189. [DOI] [PubMed] [Google Scholar]
- Spears CA, Houchins SC, Stewart DQ, Chen M, Correa-Fernandez C, Cano MA, Wetter DW. Nonjudging facet of mindfulness predicts enhanced smoking cessation in Hispanics. Psychology of Addictive Behavior. 2016;29:918–923. doi: 10.1037/adb0000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68:615–623. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- Thompson BL, Waltz J. Everyday mindfulness and mindfulness meditation: overlapping constructs or not? Personality and Individual Differences. 2007;43:1875–1885. [Google Scholar]
- U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- Vinci C, McVay MM, Copeland AL, Carrigan MH. The relationship between depression level and smoking motives in college smokers. Psychology of Addictive Behaviors. 2012;26:162–165. doi: 10.1037/a0023772. [DOI] [PubMed] [Google Scholar]
- Vinci C, Spears CA, Peltier MR, Copeland AL. Drinking motives mediate the relationship between facets of mindfulness and problematic alcohol use. Mindfulness. 2016;7:754–763. doi: 10.1007/s12671-016-0515-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidrine JI, Businelle MS, Cinciripini P, Li Y, Marcus MT, Waters AJ, Reitzel LR, Wetter DW. Associations of mindfulness with nicotine dependence, withdrawal, and agency. Substance Abuse. 2009;30:318–327. doi: 10.1080/08897070903252973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidrine JI, Spears CA, Heppner WL, Reitzel LR, Marcus MT, Cinciripini P, … Wetter DW. Efficacy of mindfulness-based addiction treatment (MBAT) for smoking cessation: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2016 doi: 10.1037/ccp0000117. [DOI] [PMC free article] [PubMed] [Google Scholar]