Abstract
Positive psychological constructs are associated with superior outcomes in cardiac patients, but there has been minimal study of positive psychology (PP) interventions in this population. Our objective was to describe the intervention development and pilot testing of an 8-week phone-based PP intervention for patients following an acute coronary syndrome (ACS). Initial intervention development and single-arm proof-of-concept trial, plus comparison of the PP intervention to a subsequently-recruited treatment as usual (TAU) cohort. PP development utilized existing literature, expert input, and qualitative interview data in ACS patients. In the proof-of-concept trial, the primary outcomes were feasibility and acceptability, measured by rates of exercise completion and participant ratings of exercise ease/utility. Secondary outcomes were pre-post changes in psychological outcomes and TAU comparisons, measured using effect sizes (Cohen's d). The PP intervention and treatment manual were successfully created. In the proof-of-concept trial, 17/23 PP participants (74 %) completed at least 5 of 8 exercises. Participants rated the ease (M = 7.4/10; SD = 2.1) and utility (M = 8.1/10, SD = 1.6) of PP exercises highly. There were moderate pre-post improvements (ds = .46–.69) in positive affect, anxiety, and depression, but minimal effects on dispositional optimism (d = .08). Compared to TAU participants (n = 22), PP participants demonstrated greater improvements in positive affect, anxiety, and depression (ds = . 47–.71), but not optimism. A PP intervention was feasible, well-accepted, and associated with improvements in most psychological measures among cardiac patients. These results provide support for a larger trial focusing on behavioral outcomes.
Keywords: Myocardial infarction, Unstable angina, Positive affect, Optimism, Mental health, Intervention
1 Introduction
Each year, 1.1 million persons in the United States are hospitalized for an acute coronary syndrome (ACS; myocardial infarction or unstable angina) (Mozaffarian et al. 2015; Aspinwall and Tedeschi 2010). Among post-ACS patients, 20 % will die within a year of their initial cardiac event (Kolansky 2009; Fishbach and Labroo 2007). Adhering to cardiac health behaviors (e.g., physical activity, low-fat diet, and medications) is vital to prognosis following an ACS (Chow et al. 2010; Gehi et al. 2007), but the majority of ACS patients are non-adherent to one or more of these behaviors following their event (Chow et al. 2010; Mozaffarian et al. 2015; Sud et al. 2005).
Psychological factors may play an important role in clinical outcomes and health behavior adherence in this population. Depression has been associated with the development of cardiac disease and elevated rates of cardiac mortality in patients with and without known heart disease (Celano and Huffman 2011; Barth et al. 2004; Lett et al. 2004). Furthermore, these connections have typically been independent of sociodemographic factors or traditional cardiac risk factors. In the specific population of ACS patients, depression is considered by the American Heart Association to be a risk factor for poor prognosis following an ACS (Lichtman et al. 2014), possibly due to the known associations of depression with nonadherence to diet, physical activity, medications, and other key secondary prevention measures (Ziegelstein et al. 2000). However, depression interventions in cardiac patients have not consistently led to changes in adherence or outcomes (Glassman et al. 2002; Jiang et al. 2008; Lesperance et al. 2007; Berkman et al. 2003), and only 15 % of ACS patients have clinical depression (Celano and Huffman 2011). Thus, a depression intervention to improve ACS prognosis may have limited impact.
Conversely, positive affect, optimism, and other positive psychological constructs have been independently associated with fewer rehospitalizations and reduced mortality in patients with heart disease (Chocron et al. 2000; Konstam et al. 1996; Steptoe et al. 2009). Importantly, the benefits of positive psychological states also appear to be independent of the effects of depression and other negative affective states on cardiac outcomes (Chida and Steptoe 2008; Scheier et al. 1999; Tindle et al. 2012). These links between positive psychological constructs and cardiac outcomes may be mediated by health behaviors. Positive constructs, for example, have been associated with greater adherence to a heart-healthy diet (Kelloniemi et al. 2005; Giltay et al. 2007) and being physically active (Steptoe et al. 2006; Browning et al. 2009; Giltay et al. 2007).
There is an emerging focus on positive psychology (PP), a discipline that aims to improve the frequency and intensity of positive emotional experiences through intentional actions (Seligman et al. 2005; Sin and Lyubomirsky 2009). PP interventions use targeted activities in several domains, including altruism (e.g., performing acts of kindness), gratitude (e.g., savoring positive life events), and optimism (e.g., imagining positive future outcomes). A meta-analysis of 39 trials in over 6000 participants found that PP programs consistently led to increased happiness, less depression, and improvements in overall well-being (Bolier et al. 2013), and such benefits can last months post-intervention (Sin and Lyubomirsky 2009; Seligman et al. 2005).
PP interventions in medically ill populations have been far less common, though interventions to improve positive affect have been recently completed in patients with HIV (Moskowitz et al. 2012), type 2 diabetes (Cohn et al. 2014), and coronary disease or hypertension (Charlson et al. 2007). Developing a feasible and effective PP intervention that promotes well-being in ACS patients could result in improved positive psychological constructs, with potential downstream effects on cardiac biomarkers and key health behaviors that have been associated with lower rates of recurrent cardiac events and death.
Patients hospitalized for an ACS may represent an ideal population in which to initiate a PP intervention. This is a large population at high risk of adverse outcomes, and therefore an intervention that improves psychological health and health behaviors post-ACS may have substantial effects on individual and population health. In addition, hospitalization for ACS may represent a key opportunity during which engagement in mental health or behavior change may be more likely (Auer et al. 2008). Finally, a wide range of positive psychological constructs (primarily dispositional optimism, subjective well-being, and positive affect) are associated with cardiovascular mortality and with health behaviors (e.g., physical activity) that are critical to prognosis in this population (DuBois et al. 2012, 2015). However, a PP intervention for post-ACS patients has not been developed and tested to assess its feasibility and efficacy.
Accordingly, we developed an 8-week phone-based PP intervention for ACS patients, utilizing information from PP literature, experts, and qualitative interviews. In this paper, we describe the creation of this PP intervention, including the rationale, intervention components, training procedures, and delivery. We also describe results of a small, non-randomized proof-of-concept trial of the intervention in ACS patients. The primary aim of this trial was to assess the feasibility and acceptability of the intervention, with secondary efficacy aims to assess: (a) pre-post differences on psychological outcomes in the PP intervention and (b) compare psychological improvement in the PP group to a subsequently recruited treatment as usual (TAU) cohort.
2 Methods
2.1 Treatment Development
2.1.1 Intervention Rationale
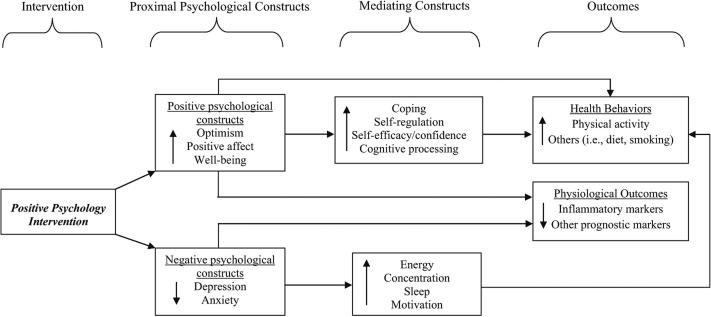
A PP intervention could have several concurrent and beneficial effects in post-ACS patients (see model, Fig. 1). First, PP interventions could lead to improved clinical outcomes through their direct effects on positive psychological targets. Higher levels of positive psychological constructs may lead to improvements in coping, motivation, self-regulation, cognitive processing, and self-efficacy/confidence (Aspinwall and Tedeschi 2010; Fishbach and Labroo 2007; Pressman and Cohen 2005; Huffman et al. 2014a). These effects could, in turn, improve initiation and maintenance of physical activity and healthier diet (Giltay et al. 2007; Shepperd et al. 1996). In addition, positive psychological constructs, most commonly dispositional optimism, positive affect, and well-being, have also been independently associated with lower levels of lipids, inflammation, and other biomarkers linked to cardiac prognosis (Ryff et al. 2004; Boehm et al. 2013; Ikeda et al. 2011; Brouwers et al. 2013).
Fig. 1.
Model depicting potential pathways from positive psychological well-being to behavioral and physiological effects
Furthermore, post-ACS patients have elevated rates of depression and anxiety (Hare et al. 2014). Symptoms of depression and anxiety, such as reduced energy, concentration, motivation, and sleep (Hare et al. 2014), may lead to reduced health behavior adherence, as has been observed in depressed post-ACS patients (Ziegelstein et al. 2000). These negative psychological syndromes are also associated with adverse physiological effects (e.g., increased inflammation) that have been linked to post-ACS mortality (Huffman et al. 2014a). PP interventions have been consistently associated with reducing depression and distress (Bolier et al. 2013) and could potentially improve the adverse behavioral and physiological effects associated with depression, anxiety, and overall psychological distress in ACS patients.
2.1.2 Intervention Development
To test the model presented in Fig. 1, the first step was to carefully develop a PP intervention. Our plan for development of an intervention for post-ACS patients was to identify existing, well-validated positive psychology exercises, and customize an intervention centered around these exercises in three ways: (1) to utilize qualitative interviews with post-ACS patients to identify (among existing exercises) the exercises/constructs that felt most relevant and useful to the participants, (2) to also use these interviews to identify aspects of the intervention (e.g., duration, delivery method) that fit the needs and desires of ACS patients in the immediate post-hospital period, and (3) to develop a written treatment manual (and protocol for phone-based discussions between interventionists and participants) that described the potential utility of these exercises in the context of their recent cardiac event (e.g., how an exercise on personal strengths could relate to taking on new challenges related to heart disease). We chose not to create a series of all-new exercises, given that new exercises would not have been validated or well-tested in other cohorts, and that existing exercises already addressed the targeted conceptual domains.
Accordingly, a PP intervention was generated based on prior PP development experience, existing literature on successful PP programs, and specific information gathered during qualitative interviews with ACS patients (Huffman et al. 2014b, 2015). First, we completed a literature review to identify the content and structure of typical PP interventions (Seligman et al. 2005; Sin and Lyubomirsky 2009). This literature search revealed that PP interventions typically consist of PP “exercises” that use reflective, written, or behavioral tasks related to positive thoughts, feelings, and behaviors. In addition, completion of several PP-related activities clustered within a short timeframe (e.g., completing three kind acts in 1 day) has been shown to have a stronger effect on well-being than spreading out such activities (Lyubomirsky et al. 2005; Sin and Lyubomirsky 2009). This observation helped inform the structure of the exercises used in the present intervention.
The specific exercises were selected from three sources. First, we considered those positive psychological constructs that have been most consistently linked to health behaviors (e.g., positive affect, optimism) (DuBois et al. 2012), to identify the most relevant psychological targets. Next, the PP intervention literature was reviewed and discussed with our team's PP content expert to identify frequently used, validated, and effective PP intervention exercises in medically ill and non-medical cohorts (Seligman et al. 2005; Gander et al. 2013; Krumholz et al. 2005; Moskowitz et al. 2012). Finally, we reviewed two additional studies (Huffman et al. 2011, 2014a) that examined the feasibility, impact, and efficacy of PP exercises in cardiac and psychiatric patients, including a very small pilot study (n = 9 in PP group) in ACS or heart failure patients (Huffman et al. 2011). This literature review identified several simple, well-accepted exercises, especially those focusing on gratitude and leveraging personal strengths.
Of note, we maintained a specific focus on exercises and concepts within the domain of PP, and did not expand to additional concepts such as self-efficacy or locus of control. We did this to specifically test whether PP interventions would provide benefit in this population, given that PP interventions target distinct constructs—positive affect, optimism, and mood—that have been linked to physical activity and superior cardiac outcomes (DuBois et al. 2015; Boehm and Kubzansky 2012), use validated PP exercises found effective in dozens of studies (Bolier et al. 2013) and do not require extensive provider training or numerous in-person sessions for patients (Seligman et al. 2005). These factors suggested that PP interventions alone might be distinctive, effective, and feasible.
Once candidate exercises and potential intervention logistics were identified, in-depth qualitative interviews with 34 ACS patients were completed in-person during their hospital admission and 3 months later (n = 28) by phone (Huffman et al. 2014b). These qualitative interviews were conducted among ACS patients in the same hospital as the proof-of-concept trial described below. Participants in these interviews had characteristics that were similar to those of patients in the present study, but included a somewhat greater proportion of men (65 %) and non-White patients (35 %).
These interviews included specific questions about patients’ interest in participating in a PP program, their preferred mode of delivery, the optimal intervention duration, and feedback on multiple candidate exercises (Huffman et al. 2014b). Patients most consistently recommended a relatively brief phone-based intervention, a focus on past success and personal strengths, and allowing choice in selecting the exercises. Participants were interviewed 3 months after hospital discharge to assess whether their positive psychological experiences or PP intervention delivery preferences might change over the course of their recovery. Overall, there was moderately greater frequency and breadth of positive psychological experiences in the hospital compared to 3 months later, and gratitude and optimism were the most common positive constructs noted at both timepoints (Huffman et al. 2014b).
2.1.3 PP Exercises
Based on the literature review and qualitative interviews, we generated a set of exercises for participants to complete once a week for 8 weeks. For example, we selected a gratitude letter because gratitude is common post-ACS (Laerum et al. 1988), because post-ACS patients in our qualitative interviews felt that exercises focused on gratitude may be useful, and because this exercise (in a cohort of medical psychiatry patients) received the highest ratings of utility out of 9 total exercises (Huffman et al. 2014a). We chose the personal strengths exercise for similar reasons: post-ACS patients had been particularly interested in exercises focused on cultivating strengths, and this exercise had performed well in our prior work. Based on feedback from the qualitative interviews, the intervention assigned different weekly PP exercises (Table 1) for the first 6 weeks. For the last 2 weeks, participants chose to repeat or modify an exercise from prior weeks, given evidence that being allowed a choice of PP exercises enhances the impact of the intervention (Gander et al. 2013). Prior to implementation, the full research team completed each exercise to test feasibility and discuss potential improvements.
Table 1.
PP exercises used in the proof-of-concept intervention trial
| Recalling positive events/counting blessings (Seligman et al. 2005) (Week 1, in hospital). Participants recalled three events, small or large, in the preceding week that were associated with satisfaction, happiness, pride, or other positive states |
| Using personal strengths (Seligman et al. 2005) (Week 2, this and subsequent exercises assigned at phone sessions). Participants assessed their personal strengths from a strength inventory and then selected one to use in a new way during the next week |
| Gratitude letter (Seligman et al. 2005) (Week 3). Participants wrote a letter of gratitude thanking a person for an act of kindness. The participant could, at their discretion, share the letter |
| Enjoyable and meaningful activities (Krumholz et al. 2005; Barth et al. 2004) (Week 4). Participants completed a series of three self-selected activities: an enjoyable activity completed alone, an enjoyable activity completed with others, and an activity that was deeply meaningful and built towards long-term goals |
| Recalling and leveraging past success (Seligman et al. 2005) (Week 5). Participants recalled a prior event in which they experienced success. Next, they wrote about the event, their contribution to the success, and the positive feelings evoked by recalling it |
| Acts of kindness (Lyubomirsky and Layous 2013) (Week 6). Participants completed three acts of kindness in 1 day. The acts could be small or large, planned or spontaneous, but they were to be completed solely to be kind to another person |
| Participant's choice (Weeks 7 and 8). Participants selected exercise(s) from prior weeks they wished to repeat. The interventionist and participant discussed the prior exercises, selected one, and discussed any necessary alterations to the focus or content of the exercise |
2.1.4 Intervention Materials and Delivery
A PP treatment manual was developed (see “Appendix” for excerpts). The manual contained a general introduction describing the goals and procedures of the intervention, a chapter for each weekly exercise with instructions, space to record details about each exercise and any related positive thoughts and feelings, and a section to provide ratings of the ease and utility of each exercise. For the final week, the manual contained a structured grid to schedule specific PP activities for the next several weeks, to promote maintenance of these activities, given the importance of practicing PP for improving longer-term outcomes (Lyubomirsky et al. 2005; Gander et al. 2013). Finally, the manual ended with a “toolbox” section. Participants were encouraged to use this section to record exercises or associated skills that were particularly effective in promoting positive affect, for future use. Along with this treatment manual, we created an annotated interventionist manual that guided interventionists in delivering the exercises and provided specific advice regarding potential barriers or problems.
Enrollment and completion of the first exercise occurred during hospitalization. After discharge, subsequent PP exercises were completed independently by participants and then reviewed by an interventionist during weekly phone calls. Key themes emphasized by interventionists across the weeks included: (1) developing a greater, more nuanced vocabulary for describing positive thoughts and feelings, (2) learning to identify and savor positive feelings and experiences, (3) learning to refocus on positive thoughts and feelings during PP activities if feeling distracted or dysphoric, and (4) utilizing novelty in completing the exercises: doing mental, physical, and social tasks that were not part of their usual routine.
During the in-hospital session, the interventionist outlined tips for completing the intervention (e.g., allowing adequate time to plan and complete exercises) and assigned the first exercise. Each subsequent week participants completed a 20–30 min phone session with their interventionist. On each call, the interventionist reviewed the previous week's exercise, explored positive thoughts and feelings associated with the exercise, gathered feedback about exercise ease and utility, and described and assigned the following week's exercise. In addition, the interventionist specifically discussed with the participant ways to incorporate and continue to use that week's skill regularly. Participants were also reminded to use the “toolbox” in their manual to record favorite skills and exercises for more regular use.
During the final phone call at week 8, participants developed a specific plan with their interventionist for continuing to use PP exercises and skills over the next several weeks. This plan could include repeating previously completed exercises or performing smaller adaptations more frequently. Participants also discussed specific ways to integrate favorite exercises into an ongoing future practice.
2.1.5 Training Procedures and Materials
The intervention was designed to be delivered by interventionists from a variety of disciplines with relatively little training. Study interventionists (in this case, doctoral-level psychologists and a masters-level social worker) were trained by senior members of the study team who had experience delivering PP interventions in prior studies. In trainings, interventionists completed PP background reading, observed sessions, completed all exercises with one another, and utilized role play activities. During the trial, sessions were recorded, and a fidelity scale (developed for the trial) was used to ensure consistency of intervention delivery. Fidelity focused on adherence to study procedures, emphasis of key themes (e.g., use of novelty, application of skills to daily life), and that other therapeutic techniques (e.g., cognitive-behavioral therapy) were not being used.
2.2 Proof-of-Concept Trial
To assess the feasibility and acceptability of the newly-created PP intervention and explore potential effects on proximal outcomes (positive affect, optimism, and psychological distress), we designed a one-arm proof-of-concept trial. Institutional Review Board (IRB) approval for this trial was obtained prior to any study procedures.
2.2.1 Study Criteria
Participants were enrolled from three inpatient cardiac units at an urban academic general hospital. Eligible patients were adults with (1) a primary admission diagnosis of ACS, diagnosed with standard definitions used in prior trials (Menzin et al. 2008), (2) suboptimal adherence to health behaviors, defined as total item score of < 15/18 on three items from the Medical Outcomes Study Specific Adherence Scale (MOS-SAS) (DiMatteo et al. 1992) that has been used in prior studies of cardiac patients (Bauer et al. 2012) regarding medication, physical activity, and diet recommendations over the prior month (this scale was used given that suboptimal adherence will be an inclusion criteria for future studies on behavior change), and (3) submaximal scores on the Positive and Negative Affect Schedule (PANAS) positive affect subscale (Watson et al. 1988) and Life Orientation Test-Revised (LOT-R; Scheier et al. 1994) for dispositional optimism. This final criterion prevented ceiling effects at baseline on these proximal psychological outcomes.
Exclusion criteria included: (1) cognitive deficits, assessed via a 6-item cognitive screen (Callahan et al. 2002), (2) inability to communicate in English, (3) medical conditions precluding participation in the weekly phone calls or that would to lead to death within 6 months, (4) patients not prescribed aspirin at discharge (a marker of health behavior), and (5) inability to participate in physical activity. The exclusions related to aspirin and physical activity were used because such patients would be ineligible for future planned trials that will objectively measure adherence to these behaviors.
2.2.2 Recruitment, Enrollment, and Weekly Intervention
Patients admitted for an ACS were identified from medical unit censuses. Study staff confirmed medical eligibility of potential participants. If patients were medically eligible and willing to be approached, a member of the research team described the study, assessed for inclusion and exclusion criteria, and obtained written informed consent. Patients were approached with a recruitment message that included a health-based rationale for studying ways to increase positive psychological constructs and a brief description of the intervention. In this single-arm trial, all participants received the PP intervention. The interventionist assigned the first exercise with the patient in-hospital and then conducted phone sessions with the participant in weeks 2–8.
2.2.3 Outcome Measures and Assessments
Data were collected at three time points. First, after enrollment and prior to initiation of the intervention, baseline sociodemographic and medical characteristics were collected via interview and medical record review, and baseline psychological status was assessed using validated self-report instruments. Second, each week during the intervention period, study interventionists recorded rates of exercise completion and ratings of exercise ease and utility. Participants were also asked to provide open-ended feedback about each exercise. Third, at 8 weeks, participants repeated the self-report psychological measures during a follow-up phone assessment.
2.2.4 Primary Outcomes: Feasibility and Acceptability
Feasibility was assessed by rates of PP exercise completion. The study interventionist recorded a session as completed if the participant had successfully finished all parts of the weekly exercise and completed the phone call. Regarding acceptability, each week participants rated exercise ease (“How easy was it to complete this exercise?”) and utility (“How helpful was this exercise?”) on 0–10 Likert scales. These items were used to establish mean ease and utility ratings for each specific exercise and across all exercises.
2.2.5 Secondary Outcomes: Changes on Psychological Measures
As a secondary aim, we explored efficacy, defined as pre-post intervention changes on the following psychological measures: (1) positive affect (PANAS) (Watson et al. 1988), (2) optimism (LOT-R) (Scheier et al. 1994), and (3) anxiety and depression (Hospital Anxiety and Depression Scale [HADS]) (Bjelland et al. 2002), assessed as a total scale (HADS-T) and anxiety or depression subscales (HADS-A and HADS-D, respectively). We utilized these scales because the PANAS and LOT-R are well-validated scales that have been associated with cardiac outcomes (Scheier et al. 1999; Tindle et al. 2012; Hoen et al. 2013). The HADS was designed for patients with medical illness and has also been used in numerous studies of cardiac patients (Hevey et al. 2014; Huffman et al. 2014a).
2.3 Prospective TAU Cohort Enrollment
Given the potential for patients to have spontaneous improvement in psychological health in the weeks following an ACS, we chose to recruit a TAU cohort after completion of the proof-of-concept intervention study to assess the natural history of recovery from ACS and compare it to outcomes from the PP proof-of-concept trial. As part of TAU, patients received the hospital's Caring for Your Heart handbook with basic cardiovascular management tips and were free to receive any other treatment, including mental health treatment and cardiac rehabilitation (as were patients in the proof-of-concept trial).
We used the same process of patient identification, recruitment, and assessment (including self-report measures at baseline and 8 weeks) to enroll the prospective TAU cohort, but they received no active intervention or weekly calls. To best match the PP and TAU cohorts, we asked potential TAU participants whether they would have participated in an 8-week PP intervention; if they indicated that they would not have participated, they were not enrolled in the TAU comparison group.
2.4 Statistical Analysis and Study Hypotheses
For the primary study outcomes (feasibility and acceptability), we calculated proportions, means, and standard deviations using descriptive statistics. Regarding feasibility, our hypothesis was that a majority of participants (≥50 %) would complete over half of the exercises (≥f5/8). We selected this cutoff because this would result in the majority of participants completing nearly all (5/6) of the different PP exercises, given that the final two weeks repeated prior exercises.
Regarding acceptability, our hypothesis was that participants’ mean ratings would exceed 6/10 for ease and utility, meaning that the sessions would be deemed both more viable and more useful than not, a key acceptability threshold for moving forward. Though participants could have provided high scores due to social desirability, substantial variability in these ratings has been observed across different exercises within the same study (Huffman et al. 2014a), suggesting that participants were unlikely to indiscriminately give high ratings.
For pre-post changes in psychological outcome measures in the proof-of-concept trial (secondary outcome), we calculated effect size (ES; Cohen's d) for each measure by dividing the mean change in the measure by the pooled standard deviation of the measure at baseline and 8 weeks. We also explored pre-post differences using paired t tests. These tests were considered exploratory, as this pilot study was not powered to detect statistically significant changes. We hypothesized that we would observe a small to moderate effect of the PP intervention on pre-post scores, consistent with prior PP studies in medical cohorts (Cohn et al. 2014).
Finally, we compared mean changes in self-report measures over 8 weeks between PP and TAU groups via ES differences and exploratory independent-samples t tests. As with pre-post changes in the PP intervention group, our hypothesis was that we would observe small to moderate ES differences between groups favoring the PP intervention. All analyses were two-tailed and performed using Stata version 11.0 (StataCorp, College Station, TX).
3 Results
3.1 Proof-of-Concept Study
Twenty-three participants were eligible and enrolled in the proof-of-concept study (Table 2). There were no significant differences among those who enrolled and those who declined (n = 32) with respect to age, gender, and race/ethnicity (p > .10). Participants’ mean age was 60.4 years (SD = 11.7), 48 % were women, and this was the first ACS for 16 (70 %) patients. Of the 23 participants, 20 provided follow-up data and were included in analyses for secondary outcomes. In the TAU cohort, 25 participants were eligible and enrolled (Table 2); 22 provided follow-up data and were included in secondary between-group analyses.
Table 2.
Baseline characteristics of intervention and TAU cohorts
| Characteristic | Intervention (N = 23) | TAU (N = 25) |
|---|---|---|
| Sociodemographics (N [%] unless noted) | ||
| Age (years), M (SD) | 60.4 (11.7) | 65.2 (11.2) |
| Male | 12 (52) | 17 (68) |
| White | 18 (78) | 20 (80) |
| Admission diagnosis: MI | 15 (65) | 17 (68) |
| Length of stay (days), M (SD) | 3.7 (2.3) | 3.7 (2.8) |
| Married | 13 (56) | 18 (72) |
| Lives alone | 5 (22) | 3 (12) |
| Medical history | ||
| Charlson Medical Comorbidity Index, M (SD) | 2.2 (1.3) | 2.1 (1.4) |
| Body Mass Index, M (SD) | 29.3 (7.4) | 30.1 (5.3) |
| Diabetes mellitus type 2 | 4 (17) | 8 (32) |
| Current smoker | 5 (22) | 4 (16) |
| Hyperlipidemia | 17 (74) | 19 (76) |
| Hypertension(*) | 12 (52) | 19 (76) |
| Prior acute coronary syndrome | 7 (30) | 11 (44) |
| Peak troponin T (ng/ml), M (SD) | 2.2 (6.0) | 2.1 (2.9) |
| Left ventricular ejection fraction (%), M (SD) | 53.8 (13.9) | 58.6 (9.4) |
| Medications at discharge | ||
| Aspirin | 22 (96) | 25 (100) |
| Beta blocker | 22 (96) | 24 (96) |
| Angiotensin converting enzyme inhibitor/angiotensin receptor blocker | 13 (56) | 18 (72) |
| Antiplatelet agent | 21 (91) | 21 (84) |
| Statin(*) | 23 (100) | 21 (84) |
M mean, SD standard deviation
p < .10
3.1.1 Primary Outcomes: Feasibility and Acceptability
Out of 23 participants, 17 (74 %) completed ≥5 exercises, and the mean number of exercises completed was 6.5 (81 %). Participants’ mean rating of exercise ease was 7.4/10 (SD = 2.1), with mean individual exercise ratings ranging from 6.4 (Acts of Kindness) to 8.4/10 (Leveraging Past Success and Choice exercises). Mean utility rating across all exercises was 8.1 (SD = 1.6), with individual exercise ratings ranging from 7.6 (Personal Strengths and Enjoyable and Meaningful Activities) to 8.3 (Gratitude Letter). The two choice exercises had the highest rated utility (8.6/10), and participants most often chose the Gratitude for Positive Events and Gratitude Letter exercises to repeat. Among the three patients who did not continue in the intervention study, two were lost to follow-up and one withdrew due to medical factors.
3.1.2 Secondary Outcomes: PP Intervention Group Pre-post Changes on Psychological Constructs
In the PP intervention (n = 20), there was a moderate effect size improvement of positive affect (PANAS: 35.1 [baseline] to 38.2 [follow-up]), d = .46; p = .053). There were likewise moderate effect size improvements on total anxiety and depression (HADS-T: 13.4 [baseline] to 9.0 [follow-up]; d = .69; p = .008), anxiety subscale (HADS-A: 8.5 [baseline] to 5.7 [follow-up]; d = .66; p = .002) and depression subscale (HADS-D: 4.9 [baseline] to 3.3 [follow-up]; d = .46; p = .06). In contrast, dispositional optimism remained essentially unchanged (LOT-R: 23.5 [baseline] to 23.0 [follow-up]; d = .08; p > .10). TAU participants had minimal change on psychological outcomes (all ps > .10; Table 3).
Table 3.
Pre-post changes in study outcomes over 8 weeks in the PP intervention and TAU cohorts
| Measure | Baseline scores M (SD) | 8 week follow-up scores M (SD) | Change from baseline to 8 weeks | ES (d) |
|---|---|---|---|---|
| PP intervention cohort (n = 20) | ||||
| PANAS (positive affect) | 35.1 (7.9) | 38.2 (8.6) | 3.1(*) | .46 |
| LOT-R (dispositional optimism) | 23.5 (4.8) | 23.0 (5.8) | –.50 | .08 |
| HADS-T° (total negative psychological health) | 13.4 (8.9) | 9.0 (5.6) | –4.4* | .69 |
| HADS-A° (anxiety) | 8.5 (5.9) | 5.7 (4.6) | –2.8* | .66 |
| HADS-D° (depression) | 4.9 (3.9) | 3.3 (4.1) | –1.6(*) | .46 |
| TAU cohort (n = 22) | ||||
| PANAS (positive affect) | 36.7 (7.6) | 36.3 (7.3) | –.40 | .01 |
| LOT-R (dispositional optimism) | 24.9 (3.7) | 25.9 (3.7) | 1.0 | .30 |
| HADS-T (total negative psychological health) | 8.5 (6.7) | 8.6 (5.8) | .10 | .02 |
| HADS-A (anxiety) | 4.7 (4.1) | 4.4 (3.5) | –.30 | .09 |
| HADS-D (depression) | 3.8 (3.4) | 4.3 (3.1) | .50 | .21 |
M mean, SD standard deviation, ES effect size (Cohen's d, absolute value), HADS Hospital Anxiety and Depression Scale, LOT-R Life Orientation Test-Revised, PANAS Positive and Negative Affect Schedule
p < .10
p < .01 on paired t test
n = 19
3.1.3 Secondary Outcomes: PP Versus TAU Comparisons on Psychological Constructs
As shown in Fig. 2, relative to TAU participants, PP participants had a superior trajectory in positive affect with a 3.1 point improvement compared to a .40 point decrease among TAU participants (effect size difference d = .47; t(40) = –1.70, p = .097). Similarly, PP participants had a 4.4 point reduction (improvement) on the combined measure of anxiety/depression compared to a .10 point increase in TAU participants (d = .71; t(39) = 2.44, p = .019). For the anxiety, there was a 2.8 point improvement in PP participants versus a .30 point improvement in TAU participants (d = .57; t(39) = 2.01, p = .051). For the depression, there was a 1.6 point improvement in PP participants compared to a .50 point improvement in TAU participants (d = .67; t(39) = 2.27, p = .029). TAU participants had non-significantly greater improvement (1.0 points) in dispositional optimism compared to PP participants (–.50 points) with a small ES difference (d = .38; t(40) = 1.03, p > .10).
Fig. 2.
Pre-post intervention changes for PP intervention cohort versus TAU cohort on positive affect, anxiety, depression, and optimism
3.2 Feedback from Proof-of-Concept Study
Each week, PP participants were asked open-ended questions about what was useful and what was challenging about each exercise. Table 4 summarizes relevant themes from participant responses and provides representative quotes. Positive comments focused on how the PP exercises reduced stress, improved mood, promoted awareness of positive events in daily life, provided a structure to organize thoughts, and encouraged reflection. Several participants found that the exercises that focused on personal strengths and acknowledging past successes also fostered greater self-esteem, optimism, and feelings of efficacy and confidence. The most common feedback regarding the challenging or less appealing aspects of the intervention focused on the amount of time some exercises took to complete, or feeling unable due to health limitations, especially those requiring action, such as acts of kindness or completing meaningful activities.
Table 4.
Qualitative feedback from participants in the proof-of-concept study
| What was helpful about this exercise? | What was difficult about this exercise? | ||
|---|---|---|---|
| Theme | Participant quote | Theme | Participant quote |
| Promoted a positive outlook | “[This exercise] helped me to evaluate my past and plan for a healthy future” | Exercises were time consuming | “Having three different things to think about was hard and challenging...too much to do in one week” |
| Boosted self-esteem | “I never thought of myself as strong, persistent and determined and it's a good thing to think of myself this way” | Health restrictions impacted difficulty of exercise | “Harder to do than the other exercises; partly because of [my] current health restrictions and limited interaction with others due to recovery” |
| Increased sense of purpose | “[It] helped me to feel useful at a time when I would otherwise feel helpless” | Some exercises were mentally challenging | “[The exercise] took a lot of thought. It was pretty challenging” “Some of the questions were difficult” |
4 Discussion
This paper presents the theory, background, methods, and preliminary proof-of-concept findings for a PP intervention in hospitalized ACS patients. We successfully developed the PP intervention structure, participant and interventionist manuals, training procedures, and assessment batteries. The intervention met a priori feasibility and acceptability thresholds, with high rates of PP exercise completion (81 %) and favorable participant ratings of exercise ease and utility. There were moderate effect size improvements on positive affect, total negative psychological health, anxiety, and depression—but not optimism—on pre-post assessments and when compared to a prospectively recruited TAU sample. The observed findings represent a promising first step in determining whether similar interventions can ultimately improve downstream outcomes such as cardiac health behaviors and clinical events, though additional studies are needed to assess whether the intervention can modify these key outcomes.
These findings are generally consistent with the literature on PP interventions in medical populations. A small positive affect induction study used a similar design (single-arm study followed by prospectively recruited control cohort) and PP-related exercises in HIV patients (Moskowitz et al. 2012). This study led to improvements in positive and negative affect. A pilot study of a randomized PP trial in patients with type 2 diabetes led to improvement of depression, though not daily positive or negative affect, compared to an emotion-reporting control condition (Cohn et al. 2014). In cardiac patients, a simpler non-customized PP intervention in recently hospitalized patients was feasible and well-accepted (Huffman et al. 2011). Finally, three linked randomized studies of an intervention that used positive affect induction, self-affirmation, and random provision of small gifts among patients with asthma, coronary disease, or hypertension resulted in improvements in health behaviors in some but not all studies (Mancuso et al. 2012; Ogedegbe et al. 2012; Peterson et al. 2012). Our work builds on prior PP literature in several ways. This is the first study to specifically focus on ACS patients, it tests the feasibility of PP interventions in acutely ill patients at high risk for subsequent adverse medical events and mortality.
We specifically chose in-hospital enrollment for several reasons. First, as noted, hospitalization for an ACS may represent a window during which patients may be more receptive to psychological and behavioral changes and interventions (Katz et al. 2009). Proactively recruiting patients during hospitalization, as opposed to typical recruitment procedures that ask interested people to contact a study team, also allowed us to enroll patients who may not otherwise have known about or been interested in research. Furthermore, this approach also allowed enrollment of patients who lived and received treatment in a wide catchment area. The hospital setting also allowed for an in-depth, in-person meeting to explain the intervention, form an alliance, and assign an initial exercise. Finally, hospitalized ACS patients represent a high-yield cohort, given their substantial rates of readmission, poor functioning, and mortality (Kolansky 2009; Menzin et al. 2008).
We elected to deliver this intervention by phone post-discharge (rather than in-person or via internet) to enhance the accessibility of this intervention. Patients recently hospitalized for an ACS may have significant functional limitations, transportation challenges, or insufficient time to attend in-person visits (Chiu and Wray 2011; Lawton et al. 2005; Khoza and Kortenbout 1995). In qualitative interviews with ACS patients, many expressed a preference for phone over internet because it allows for a more personal connection (Huffman et al. 2014b). Furthermore, some patients do not have internet access, especially those of lower socioeconomic status (Carroll et al. 2005; Kind et al. 2005).
As internet penetrance increases in developed countries and among harder-to-reach populations (Miniwatts 2015), pursuing an internet or smartphone-based intervention in future studies is warranted. PP exercises have been delivered via internet in healthy persons and patients with chronic disease to good effect (Seligman et al. 2005; Cohn et al. 2014), and it may be that the core elements of this intervention could also be adapted to internet delivery or an smartphone application-based intervention.
These advantages of hospital enrollment and a phone-based intervention must be balanced against a somewhat low enrollment rate (fewer than 50 % of approached patients enrolled). Some patients noted limited time to take study calls, medical/functional concerns, and needing time to transition to post-hospitalization life. Future methods to improve enrollment could include the option to initiate the intervention after discharge to allow time for adjustment and recovery, and offering an alternative internet-based option that may be preferred by some younger or busier patients (Cohn et al. 2014). However, once enrolled, approximately three-quarters of participants completed a majority of the exercises and only three participants dropped out, suggesting that participants were successfully engaged throughout the study.
Though we saw substantial changes in positive affect, depression, and anxiety in both pre-post assessments and when the PP cohort was compared to the TAU cohort, we saw little improvement in optimism, with a mean .75 point change across groups. One potential reason is that the dispositional nature of optimism, especially as measured by the LOT-R, is often considered a more stable trait than positive affect, depression, or anxiety (Schou et al. 2005). As such, this specific construct may be less responsive to change than the other three psychological outcome measures that are linked to cardiac outcomes (Scheier et al. 1999; Tindle et al. 2012; Hoen et al. 2013; Hevey et al. 2014), and a longer follow-up or intervention period might be required to modify this more enduring construct. Another possibility, given the small to medium effect size difference, is that indeed PP has inferior effects on optimism compared to usual care. Of note, there is no established measure of state optimism. Whether such a measure would be responsive to change and predict cardiac outcomes remains unknown and is an important area of future measure development.
This intervention and proof-of-concept trial had several limitations. Participants were enrolled from a single academic medical center and 78 % were White, potentially limiting generalizability. We did not record some participant characteristics (e.g., educational status, socioeconomic status) and did not record cardiac rehabilitation participation, though most patients would not initiate cardiac rehabilitation until roughly 6–8 weeks post-discharge, when the intervention was nearly complete. Also, this intervention was not compared to a concurrently recruited control condition or an attention-matched control, and there is not yet evidence that it can impact health behaviors or cardiac outcomes.
Despite these limitations, this straightforward, novel PP intervention for patients with serious medical illness had beneficial effects on depression, anxiety, and positive affect at a critical time period. Next-step studies can examine the impact of the intervention on health behaviors, given that positive psychological constructs are linked to greater participation in specific health behaviors (e.g., physical activity) that can reduce post-ACS mortality (DuBois et al. 2012; Gehi et al. 2007). Future studies can also determine whether PP interventions are most effective as stand-alone treatments or when combined with established health behavior techniques, such as motivational interviewing, that may boost motivation, reduce ambivalence, and enhance self-efficacy.
Acknowledgments
This work was supported by the National Institutes of Health (NIH) Grant R01HL113272.
Appendix
Appendix: Manual Table of Contents
| Study Calendar | 4 |
| Introduction | 5 |
| List of 12 Emotions | 11 |
| Week One (Gratitude for Positive Events) | 13 |
| Week Two (Personal Strengths) | 21 |
| Week Three (Gratitude Letter) | 28 |
| Week Four (Enjoyable and Meaningful Activities) | 35 |
| Week Five (Remembering Past Success) | 43 |
| Week Six (Acts of Kindness) | 50 |
| Week Seven—Choice 1 (Exercise of Your Choice) | 58 |
| Week Eight—Choice 2 (Exercise of Your Choice) | 64 |
| Next Steps | 69 |
| Positive Activity Schedule | 73 |
| Toolbox of Best Activities | 75 |
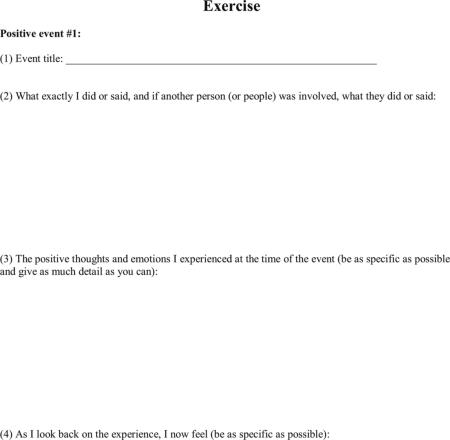
Sample Exercise
Introduction
In this exercise, we will focus on identifying and re-experiencing three positive events that happened in the past week. People often focus on negative events but less frequently pay attention to good things that happen. It makes sense to analyze bad events so that we can learn from them and avoid them in the future. However, it can be easy to overdo this focus on the negative, and this can impact one's health. One way to keep this from happening is to develop our ability to think about the good in life.
Most of us are not nearly as good at savoring and appreciating good events as we are at analyzing bad events, so this is a skill that needs practice. As you become better at focusing on the good in your life, it may become easier to feel even more grateful for what you have and more hopeful about the future.
The following exercise will ask you to identify three good things in your life that occurred in the past week. We recognize that this has been a very serious (and probably very stressful) time for you, and as a result, you may have barely noticed anything positive happening during the stress of the week. However, by looking back carefully and specifically searching for good things that may have happened, you may be surprised to find that there were small (or even large) positive events and blessings to be counted.
I am in the hospital for a heart problem—how can I possibly identify good things that are happening in my life?
At first, it can seem hard to identify positive events during a medical crisis. However, this is one reason we do this exercise first: now may be the most important time to remember that good things—even small ones—can happen, even in the midst of serious medical issues. As you get skilled at focusing your attention on pleasant moments that happen during the day—a kind gesture from someone, a greatly-appreciated visit, good news about family or friends— you may find the good things in your life becoming much more obvious.
Instructions
Take 10–15 min to complete this exercise. Use this time to write down three positive things that happened this week. Use the space on the next pages to write about the events—it is important that you have a written record of your thoughts on paper. The things you list can be relatively small in importance (“I enjoyed my lunch today”) or relatively large in importance (“I'm feeling much better after my procedure”). They can be related to your hospitalization or heart problem, or completely separate.
As you write, please follow these instructions:
Give the event a title (e.g., “sister remembered my birthday”)
Write down exactly what happened in as much detail as possible, including what you did or said, and if other people were involved, what they did or said.
Record how this event made you feel at the time. Use the most specific positive emotional words that you can think of to describe how you felt: Joy? Satisfaction? Relief?
Record how this event makes you feel now as you remember it.
Some important tips:
The goal of the exercise is to remember the good event and then enjoy the positive emotions that come with it. Don't analyze the event itself in too much detail—the important thing here is being able to:
Take your time to experience and savor the positive emotion, and then
Name and describe that positive feeling (like joy, pride, relief, or contentment) as specifically as possible—not just that you felt “good”.
Refer to the list of positive emotions (page 11) to help you describe the good feelings you experienced.
You may also find yourself wanting to write something like “I felt less stressed.” It's good to note this but try to describe the feeling or thought using positive emotions and words. So, for example, instead of writing “I felt less stressed,” you might write “I felt a little bit of relief.”
Focus on the positive. If you find yourself focusing on negative feelings or emotions, turn your mind from the negative feeling and refocus yourself on the good event and the positive feelings that came along with it. This can take effort, but it gets easier with practice and can make a real difference in how you feel.
Footnotes
Compliance with Ethical Standards
Conflicts of interest The authors have no conflicts of interest to report and there were no other funding sources.
References
- Aspinwall LG, Tedeschi RG. The value of positive psychology for health psychology: Progress and pitfalls in examining the relation of positive phenomena to health. Annals of Behavioral Medicine. 2010;39(1):4–15. doi: 10.1007/s12160-009-9153-0. [DOI] [PubMed] [Google Scholar]
- Auer R, Gaume J, Rodondi N, Cornuz J, Ghali WA. Efficacy of in-hospital multidimensional interventions of secondary prevention after acute coronary syndrome: A systematic review and meta-analysis. Circulation. 2008;117(24):3109–3117. doi: 10.1161/CIRCULATIONAHA.107.748095. [DOI] [PubMed] [Google Scholar]
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosomatic Medicine. 2004;66(6):802–813. doi: 10.1097/01.psy.0000146332.53619.b2. [DOI] [PubMed] [Google Scholar]
- Bauer LK, Caro MA, Beach SR, Mastromauro CA, Lenihan E, Januzzi JL, et al. Effects of depression and anxiety improvement on adherence to medication and health behaviors in recently hospitalized cardiac patients. American Journal of Cardiology. 2012;109(9):1266–1271. doi: 10.1016/j.amjcard.2011.12.017. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized Trial. Journal of the American Medical Association. 2003;289(23):3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. Journal of Psychosomatic Research. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Boehm JK, Kubzansky LD. The heart's content: The association between positive psychological well-being and cardiovascular health. Psychological Bulletin. 2012;138(4):655–691. doi: 10.1037/a0027448. [DOI] [PubMed] [Google Scholar]
- Boehm JK, Williams DR, Rimm EB, Ryff C, Kubzansky LD. Association between optimism and serum antioxidants in the midlife in the United States study. Psychosomatic Medicine. 2013;75(1):2–10. doi: 10.1097/PSY.0b013e31827c08a9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health. 2013;13:119. doi: 10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwers C, Mommersteeg PM, Nyklicek I, Pelle AJ, Westerhuis BL, Szabo BM, et al. Positive affect dimensions and their association with inflammatory biomarkers in patients with chronic heart failure. Biological Psychology. 2013;92(2):220–226. doi: 10.1016/j.biopsycho.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Browning C, Sims J, Kendig H, Teshuva K. Predictors of physical activity behavior in older community-dwelling adults. Journal of Allied Health. 2009;38(1):8–17. [PubMed] [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40(9):771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- Carroll AE, Rivara FP, Ebel B, Zimmerman FJ, Christakis DA. Household computer and internet access: The digital divide in a pediatric clinic population. AMIA annual symposium proceedings. 2005:111–115. [PMC free article] [PubMed] [Google Scholar]
- Celano CM, Huffman JC. Depression and cardiac disease: A review. Cardiology in Review. 2011;19(3):130–142. doi: 10.1097/CRD.0b013e31820e8106. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Boutin-Foster C, Mancuso CA, Peterson JC, Ogedegbe G, Briggs WM, et al. Randomized controlled trials of positive affect and self-affirmation to facilitate healthy behaviors in patients with cardiopulmonary diseases: Rationale, trial design, and methods. Contemporary Clinical Trials. 2007;28(6):748–762. doi: 10.1016/j.cct.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosomatic Medicine. 2008;70(7):741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- Chiu CJ, Wray LA. Gender differences in functional limitations in adults living with type 2 diabetes: Biobehavioral and psychosocial mediators. Annals of Behavioral Medicine. 2011;41(1):71–82. doi: 10.1007/s12160-010-9226-0. [DOI] [PubMed] [Google Scholar]
- Chocron S, Etievent JP, Viel JF, Dussaucy A, Clement F, Kaili D, et al. Preoperative quality of life as a predictive factor of 3-year survival after open heart operations. Annals of Thoracic Surgery. 2000;69(3):722–727. doi: 10.1016/s0003-4975(99)01329-6. [DOI] [PubMed] [Google Scholar]
- Chow CK, Jolly S, Rao-Melacini P, Fox KA, Anand SS, Yusuf S. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation. 2010;121(6):750–758. doi: 10.1161/CIRCULATIONAHA.109.891523. [DOI] [PubMed] [Google Scholar]
- Cohn MA, Pietrucha ME, Saslow LR, Hult JR, Moskowitz JT. An online positive affect skills intervention reduces depression in adults with type 2 diabetes. Journal of Positive Psychology. 2014;9(6):523–534. doi: 10.1080/17439760.2014.920410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo MR, Hays RD, Sherbourne CD. Adherence to cancer regimens: Implications for treating the older patient. Oncology. 1992;6(2 Suppl):50–57. [PubMed] [Google Scholar]
- DuBois CM, Beach SR, Kashdan TB, Nyer MB, Park ER, Celano CM, et al. Positive psychological attributes and cardiac outcomes: Associations, mechanisms, and interventions. Psychosomatics. 2012;53(4):303–318. doi: 10.1016/j.psym.2012.04.004. [DOI] [PubMed] [Google Scholar]
- DuBois CM, Lopez OV, Beale EE, Healy BC, Boehm JK, Huffman JC. Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: A systematic review. International Journal of Cardiology. 2015;195:265–280. doi: 10.1016/j.ijcard.2015.05.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbach A, Labroo AA. Be better or be merry: How mood affects self-control. Journal of Personality and Social Psychology. 2007;93(2):158–173. doi: 10.1037/0022-3514.93.2.158. [DOI] [PubMed] [Google Scholar]
- Gander F, Proyer RT, Ruch W, Wyss T. Strength-based positive interventions: Further evidence for their potential in enhancing well-being and alleviating depression [Peer Reviewed]. Journal of Happiness Studies. 2013;14(4):1241–1259. [Google Scholar]
- Gehi AK, Ali S, Na B, Whooley MA. Self-reported medication adherence and cardiovascular events in patients with stable coronary heart disease: The heart and soul study. Archives of Internal Medicine. 2007;167(16):1798–1803. doi: 10.1001/archinte.167.16.1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giltay EJ, Geleijnse JM, Zitman FG, Buijsse B, Kromhout D. Lifestyle and dietary correlates of dispositional optimism in men: The Zutphen Elderly Study. Journal of Psychosomatic Research. 2007;63(5):483–490. doi: 10.1016/j.jpsychores.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Glassman AH, O'Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Jr, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288(6):701–709. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: A clinical review. European Heart Journal. 2014;35(21):1365–1372. doi: 10.1093/eurheartj/eht462. [DOI] [PubMed] [Google Scholar]
- Hevey D, McGee HM, Horgan JH. Comparative optimism among patients with coronary heart disease (CHD) is associated with fewer adverse clinical events 12 months later. Journal of Behavioral Medicine. 2014;37(2):300–307. doi: 10.1007/s10865-012-9487-0. [DOI] [PubMed] [Google Scholar]
- Hoen PW, Denollet J, de Jonge P, Whooley MA. Positive affect and survival in patients with stable coronary heart disease: Findings from the Heart and Soul Study. Journal of Clinical Psychiatry. 2013;74(7):716–722. doi: 10.4088/JCP.12m08022. [DOI] [PubMed] [Google Scholar]
- Huffman JC, DuBois CM, Healy BC, Boehm JK, Kashdan TB, Celano CM, et al. Feasibility and utility of positive psychology exercises for suicidal inpatients. General Hospital Psychiatry. 2014a;36(1):88–94. doi: 10.1016/j.genhosppsych.2013.10.006. [DOI] [PubMed] [Google Scholar]
- Huffman JC, DuBois CM, Mastromauro CA, Moore SV, Suarez L, Park ER. Positive psychological states and health behaviors in acute coronary syndrome patients: A qualitative study. Journal of Health Psychology. 2014b doi: 10.1177/1359105314544135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, Mastromauro CA, Boehm JK, Seabrook R, Fricchione GL, Denninger JW, et al. Development of a positive psychology intervention for patients with acute cardiovascular disease. Heart International. 2011;6(2):e14. doi: 10.4081/hi.2011.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, Moore SV, DuBois CM, Mastromauro CA, Suarez L, Park ER. An exploratory mixed methods analysis of adherence predictors following acute coronary syndrome. Psychol Health Med. 2015;20(5):541–550. doi: 10.1080/13548506.2014.989531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda A, Schwartz J, Peters JL, Fang S, Spiro A, 3rd, Sparrow D, et al. Optimism in relation to inflammation and endothelial dysfunction in older men: the VA Normative Aging Study. Psychosomatic Medicine. 2011;73(8):664–671. doi: 10.1097/PSY.0b013e3182312497. [DOI] [PubMed] [Google Scholar]
- Jiang W, O'Connor C, Silva SG, Kuchibhatla M, Cuffe MS, Callwood DD, et al. Safety and efficacy of sertraline for depression in patients with CHF (SADHART-CHF): A randomized, double-blind, placebo-controlled trial of sertraline for major depression with congestive heart failure. American Heart Journal. 2008;156(3):437–444. doi: 10.1016/j.ahj.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz DA, Graber M, Birrer E, Lounsbury P, Baldwin A, Hillis SL, et al. Health beliefs toward cardiovascular risk reduction in patients admitted to chest pain observation units. Academic Emergency Medicine. 2009;16(5):379–387. doi: 10.1111/j.1553-2712.2009.00383.x. [DOI] [PubMed] [Google Scholar]
- Kelloniemi H, Ek E, Laitinen J. Optimism, dietary habits, body mass index and smoking among young Finnish adults. Appetite. 2005;45(2):169–176. doi: 10.1016/j.appet.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Khoza SR, Kortenbout W. An investigation of compliance in type II diabetic patients attending clinic at Church of Scotland hospital. Curationis. 1995;18(4):10–14. doi: 10.4102/curationis.v18i4.1367. [DOI] [PubMed] [Google Scholar]
- Kind T, Huang ZJ, Farr D, Pomerantz KL. Internet and computer access and use for health information in an underserved community. Ambulatory Pediatrics. 2005;5(2):117–121. doi: 10.1367/A04-107R.1. [DOI] [PubMed] [Google Scholar]
- Kolansky DM. Acute coronary syndromes: morbidity, mortality, and pharmacoeconomic burden. American Journal of Managed Care. 2009;15(2 Suppl):S36–S41. [PubMed] [Google Scholar]
- Konstam V, Salem D, Pouleur H, Kostis J, Gorkin L, Shumaker S, et al. Baseline quality of life as a predictor of mortality and hospitalization in 5,025 patients with congestive heart failure. SOLVD Investigations. Studies of Left Ventricular Dysfunction Investigators. American Journal of Cardiology. 1996;78(8):890–895. doi: 10.1016/s0002-9149(96)00463-8. [DOI] [PubMed] [Google Scholar]
- Krumholz HM, Peterson ED, Ayanian JZ, Chin MH, DeBusk RF, Goldman L, et al. Report of the National Heart, Lung, and Blood Institute working group on outcomes research in cardiovascular disease. Circulation. 2005;111(23):3158–3166. doi: 10.1161/CIRCULATIONAHA.105.536102. [DOI] [PubMed] [Google Scholar]
- Laerum E, Johnsen N, Smith P, Larsen S. Myocardial infarction may induce positive changes in life-style and in the quality of life. Scandinavian Journal of Primary Health Care. 1988;6(2):67–71. doi: 10.3109/02813438809009293. [DOI] [PubMed] [Google Scholar]
- Lawton J, Parry O, Peel E, Douglas M. Diabetes service provision: A qualitative study of newly diagnosed type 2 diabetes patients’ experiences and views. Diabetic Medicine. 2005;22(9):1246–1251. doi: 10.1111/j.1464-5491.2005.01619.x. [DOI] [PubMed] [Google Scholar]
- Lesperance F, Frasure-Smith N, Koszycki D, Laliberte MA, van Zyl LT, Baker B, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: The Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial. Journal of the American Medical Association. 2007;297(4):367–379. doi: 10.1001/jama.297.4.367. [DOI] [PubMed] [Google Scholar]
- Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, et al. Depression as a risk factor for coronary artery disease: Evidence, mechanisms, and treatment. Psychosomatic Medicine. 2004;66(3):305–315. doi: 10.1097/01.psy.0000126207.43307.c0. [DOI] [PubMed] [Google Scholar]
- Lichtman JH, Froelicher ES, Blumenthal JA, Carney RM, Doering LV, Frasure-Smith N, et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: Systematic review and recommendations: A scientific statement from the American Heart Association. Circulation. 2014;129(12):1350–1369. doi: 10.1161/CIR.0000000000000019. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, Layous K. How do simple positive activities increase well-being? [Peer Reviewed]. Current Directions in Psychological Science. 2013;22(1):57–62. [Google Scholar]
- Lyubomirsky S, Sheldon KM, Schkade D. Pursuing happiness: The architecture of sustainable change. Review of General Psychology. 2005;9:111–131. [Google Scholar]
- Mancuso CA, Choi TN, Westermann H, Wenderoth S, Hollenberg JP, Wells MT, et al. Increasing physical activity in patients with asthma through positive affect and self-affirmation: A randomized trial. Archives of Internal Medicine. 2012;172(4):337–343. doi: 10.1001/archinternmed.2011.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzin J, Wygant G, Hauch O, Jackel J, Friedman M. One-year costs of ischemic heart disease among patients with acute coronary syndromes: Findings from a multi-employer claims database. Current Medical Research and Opinion. 2008;24(2):461–468. doi: 10.1185/030079908x261096. [DOI] [PubMed] [Google Scholar]
- Miniwatts Internet world statistics, 2014; Internet usage statistics: The internet big picture. 2015 http://www.internetworldstats.com/stats.htm, August 11, 2015.
- Moskowitz JT, Hult JR, Duncan LG, Cohn MA, Maurer S, Bussolari C, et al. A positive affect intervention for people experiencing health-related stress: Development and non-randomized pilot test. J Health Psychol. 2012;17(5):676–692. doi: 10.1177/1359105311425275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- Ogedegbe GO, Boutin-Foster C, Wells MT, Allegrante JP, Isen AM, Jobe JB, et al. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Archives of Internal Medicine. 2012;172(4):322–326. doi: 10.1001/archinternmed.2011.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson JC, Charlson ME, Hoffman Z, Wells MT, Wong SC, Hollenberg JP, et al. A randomized controlled trial of positive-affect induction to promote physical activity after percutaneous coronary intervention. Archives of Internal Medicine. 2012;172(4):329–336. doi: 10.1001/archinternmed.2011.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressman S, Cohen S. Does positive affect influence health? Psychological Bulletin. 2005;131(6):925–971. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- Ryff CD, Singer BH, Dienberg Love G. Positive health: Connecting well-being with biology. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 2004;359(1449):1383–1394. doi: 10.1098/rstb.2004.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Matthews KA, Owens JF, Schulz R, Bridges MW, Magovern GJ, et al. Optimism and rehospitalization after coronary artery bypass graft surgery. Archives of Internal Medicine. 1999;159(8):829–835. doi: 10.1001/archinte.159.8.829. [DOI] [PubMed] [Google Scholar]
- Schou I, Ekeberg O, Sandvik L, Ruland CM. Stability in optimism-pessimism in relation to bad news: A study of women with breast cancer. Journal of Personality Assessment. 2005;84(2):148–154. doi: 10.1207/s15327752jpa8402_04. [DOI] [PubMed] [Google Scholar]
- Seligman ME, Steen TA, Park N, Peterson C. Positive psychology progress: Empirical validation of interventions. American Psychologist. 2005;60(5):410–421. doi: 10.1037/0003-066X.60.5.410. [DOI] [PubMed] [Google Scholar]
- Shepperd JA, Maroto JJ, Pbert LA. Dispositional optimism as a predictor of health changes among cardiac patients. Journal of Research in Personality. 1996;10:34–42. [Google Scholar]
- Sin NL, Lyubomirsky S. Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: A practice-friendly meta-analysis. Journal of Clinical Psychology. 2009;65(5):467–487. doi: 10.1002/jclp.20593. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Dockray S, Wardle J. Positive affect and psychobiological processes relevant to health. Journal of Personality. 2009;77(6):1747–1776. doi: 10.1111/j.1467-6494.2009.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behaviour in community-dwelling older people: Associations with healthy ageing. British Journal of Health Psychology. 2006;11(Pt 1):71–84. doi: 10.1348/135910705X42850. [DOI] [PubMed] [Google Scholar]
- Sud A, Kline-Rogers EM, Eagle KA, Fang J, Armstrong DF, Rangarajan K, et al. Adherence to medications by patients after acute coronary syndromes. Annals of Pharmacotherapy. 2005;39(11):1792–1797. doi: 10.1345/aph.1G249. [DOI] [PubMed] [Google Scholar]
- Tindle H, Belnap BH, Houck PR, Mazumdar S, Scheier MF, Matthews KA, et al. Optimism, response to treatment of depression, and rehospitalization after coronary artery bypass graft surgery. Psychosomatic Medicine. 2012;74(2):200–207. doi: 10.1097/PSY.0b013e318244903f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Archives of Internal Medicine. 2000;160(12):1818–1823. doi: 10.1001/archinte.160.12.1818. [DOI] [PubMed] [Google Scholar]