Abstract
Background:
Botulinum toxin type A remains the most popular nonsurgical aesthetic treatment worldwide. Previous consensus statements have focused on Caucasians and on Koreans as generally representative of Asians. However, indications and dosages vary among different ethnic groups. This publication reports the results of a multidisciplinary, pan-Asian consensus focusing on incobotulinumtoxinA.
Methods:
A consensus group of plastic surgeons and dermatologists from Asia, Europe, and the United States convened for a live meeting in Asia, followed by a questionnaire-based Delphi procedure. Treatment of Asians in both their native countries and countries of migration was discussed.
Results:
For most items, the group achieved a majority consensus. A number of treatment indications, strategies, and dosages were identified in Asians, which are distinct to those previously described for Caucasians due to differences in facial morphotypes, anatomy, and cultural expectations. The group also formulated position statements for intradermal botulinum toxin type A (“mesotoxin”), body shaping with the calves as a paradigm, and reduction of parotid glands. While Asians have previously been considered a homogeneous group for the purposes of aesthetic treatment, this publication considers regional variations. A new classification of Asian facial morphotypes is proposed to aid treatment planning and implementation.
Conclusions:
This is the first pan-Asian consensus for aesthetic use of botulinum toxin type A. Its unique objective is to optimize treatment safety and efficacy for patients of complete or part-Asian ancestry in all regions. The recommendations for incobotulinumtoxinA may be extended with care to other botulinum toxin formulations.
The use of injectable botulinum toxin type A for aesthetic purposes has evolved rapidly over the past 2 decades. Previous consensus publications have provided guidelines for various formulations of botulinum toxin type A.1–7 Most of these publications focused on Caucasian subjects. A recent publication8 offered consensus recommendations from a group of Korean dermatologists. For this publication, an international group of plastic surgeons and dermatologists with expertise in injectables, from different Asian countries and also from 2 other continents with significant Asian populations, discussed aesthetic applications of botulinum toxin type A for Asian subjects and provided consensus recommendations.
Objectives and Statement of Need
The aims of this publication are to enable practitioners for the following:
To understand current, evidence-based, and experiential approaches to optimize botulinum toxin treatment outcomes for subjects of Asian ancestry from different regions of Asia and other countries in which they reside.
To recognize factors that influence patient counseling and planning of botulinum toxin treatment in Asian subjects, including key anatomical and functional considerations, specific factors related to age and gender, cultural ideals, and emerging trends.
To perform individualized pretreatment assessment, including analysis of facial morphotypes and target muscles, and implement effective strategies for site-specific treatment of Asian subjects with botulinum toxin, including selection of appropriate dosages and injection techniques.
To apply the above principles to pan-facial treatment with botulinum toxin to improve the proportions, shape, and contour of the youthful or aging Asian face.
Novel features of this publication include the following:
Use of muscular and/or bony landmarks to identify optimal toxin injection points. Soft tissue landmarks, which have been advocated in a previous Korean consensus document,8 may be less consistent and hence less accurate.
Distinction of toxin injection strategies for infraorbital rhytids from those for infraorbital eye opening.
Anatomically-based toxin injection strategies to achieve a preferred eyebrow shape in Asian females, including brow elevation, while avoiding the arched, “Samurai eyebrow” that is considered undesirable to Asians.
Anatomically-based injection strategy to target the lower rather than the upper portion of depressor anguli oris. This reflects pilot data from Korean cadaver dissections, showing a tendency for the modiolus to have a lower position than in Caucasians, and is with the aim of minimizing unwanted spread of toxin to other muscles controlling mobility of the mouth.
Proposal of a new, 3-point, pan-Asian classification of facial morphotypes to guide optimal treatment strategies with injectables.
Position statements for the following emerging treatment indications in Asia, with the caveat that further data are required to assess safety and efficacy from an evidence-based perspective: intradermal botulinum toxin (“mesotoxin”), body shaping, and injection of the parotid glands.
Consensus Group and Methodology
A meeting of 8 core aesthetics specialty experts from North America, Taiwan, South Korea, Singapore, Italy, and Germany (H.S., P-.H.H., N-.J.H., C.H.H., W.W., D.C., M.K., K.S.) was convened in Singapore on July 27, 2013. Participants were selected based on their experience in aesthetic use of botulinum toxin type A and in treating Asian subjects. The meeting was designed according to accepted guidelines for consensus initiatives9 and was accompanied by a pre-meeting questionnaire. Based on this questionnaire and the meeting proceedings, initial consensus recommendations were formulated. These recommendations were reviewed and revised in a Delphi-like procedure by the whole Pan-Asian Aesthetics Toxin Consensus Group, comprising the 8 faculty who were present at the live meeting, and 1 from China (Y.W.). The article was subsequently reviewed by a panel of 3 experts in the field of botulinum toxin type A: Drs. Benjamin Ascher (France), Derek Jones (United States), and Berthold Rzany (Germany). A majority consensus was achieved in 61 out of 84 (73%) of the investigated categories. Within these categories, a mean percentage expert consensus of 78% was observed.
Overview of Botulinum Toxin Type A Products
Several botulinum toxin type A formulations are approved for aesthetic use in Asia and elsewhere. A number are listed in Table 1.
Table 1.
Botulinum Toxin Type A Products Available In Asia
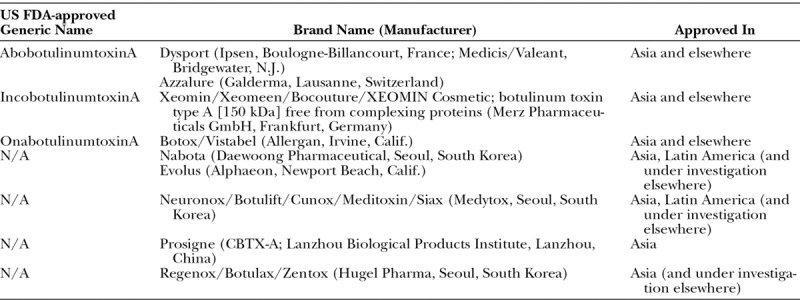
The dosage units and dose-response curves of different formulations are not directly comparable. However, dosing ratios exist that have been applied to daily practice. From a number of consensus and review publications, as well as a comparative clinical trial, clinical equivalence has been suggested at a unit ratio of 1:1 for aesthetic use of incobotulinumtoxinA and onabotulinumtoxinA.3,7,10 If extrapolating units of onabotulinumtoxinA or incobotulinumtoxinA to abobotulinumtoxinA, a ratio of 1:2.5 is considered appropriate, based on available data and clinical experience.11,12 The recommended doses within this document refer to incobotulinumtoxinA. The Pan-Asian Aesthetics Toxin Consensus Group considers it reasonable to extend these recommendations with care to other botulinum toxin type A formulations.
GENERAL CONSENSUS RECOMMENDATIONS FOR BOTULINUM TOXIN TYPE A TREATMENT
Patient-Tailored, Anatomically Appropriate Assessment and Treatment Planning
There is significant variability in the shape and function of many target muscles, between different populations, and even between individuals within one population. Determination of botulinum toxin type A injection sites should be based on muscular and bony landmarks rather than cutaneous ones. For instance, the eyebrows are a particularly unreliable cutaneous landmark, especially in women due to their propensity to modify eyebrow shape, eg, by tweezing or plucking. Treatment strategy should be based on the subject’s muscle mass, muscle shape, pattern of muscle activity, and what is aesthetically appropriate in the context of overall facial structure. Examination of the overlying soft tissues—fat and skin—is useful as an adjunct. Dosages are adjusted according to muscle activity and muscle mass, whereas muscle shape influences injection site placement.
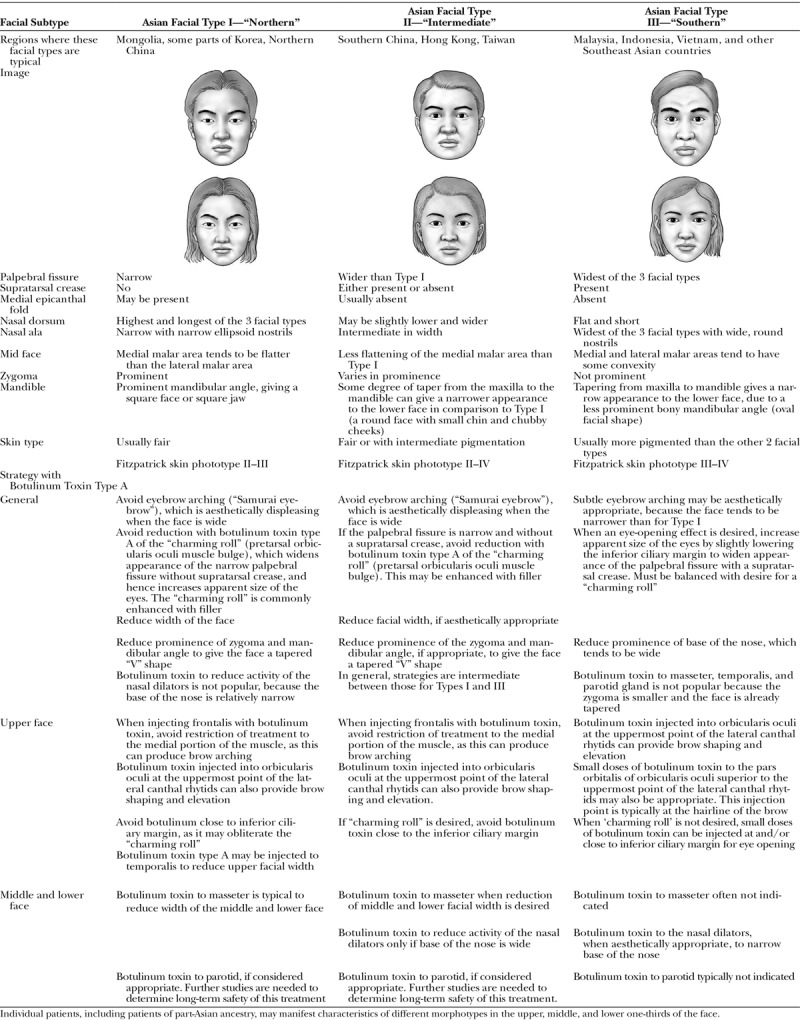
Asian Facial Morphotypes
Despite some informative publications on facial canons,13–16 facial types and aesthetic ideals for Asian subjects remain incompletely defined and are sometimes mistakenly presumed to be homogeneous. Asians are a notably heterogeneous group, and therefore cannot be treated as a uniform population. To guide patient-tailored treatment with toxin and fillers, we propose a new classification of 3 Asian facial morphotypes (Table 2). This is a consolidation of the varied morphotypes of Asian patients, with a focus on characteristics that are relevant to injectables treatment. In contrast to previous classifications, it is an integrative, pan-Asian classification, encompassing North and South Asians rather than addressing subpopulations such as Han Chinese. Patients originating from the Indian subcontinent or Middle East are not included, because their morphotypes and treatment do not fall within the scope of this publication. Additional, novel features of our classification include specific descriptions of the nasal dorsum for each facial type and a focus on mandibular prominence, which we feel is more accurate and of more value to treatment planning than the previously described lower facial width or facial “chubbiness.” Botulinum toxin injection strategy can be guided by the predominant facial type, in the context of overall facial morphology, geographic and cultural beauty ideals, and what is deemed attractive by the individual patient. For patients who manifest different morphotypes in the upper, middle, or lower one-thirds of the face, the predominant morphotype of a specific facial area may be considered when addressing it. Examples of different treatment strategies according to these distinct facial types are detailed in the relevant consensus recommendation sections below.
Table 2.
New Classification of 3 Asian Facial Morphotypes and Recommendations for Appropriate Treatment Strategies with Botulinum Toxin Type A
Aesthetic Ideals among Asians
For optimal treatment planning and outcomes, clinicians must acknowledge and address both the commonalities and variations in Asian ideals of beauty. A square or long female face is often considered to be unattractive.17 Traditionally, a round, full “moon” face was the hallmark of beauty, and many older individuals from Taiwan and China still consider this a sign of good fortune.18,19 In modern times, the ideal has shifted: Asian women who seek to modify their congenital characteristics with botulinum toxin type A most commonly wish to achieve a more pronounced taper from maxilla to mandible. This decreases prominence of the lower one-third of the face and imparts a ‘V’ shape in front profile. However, some specific geographic considerations are also germane. Although a more slender face is favored by many Taiwanese and Chinese,20,21 a face that is perceived as too narrow is deemed undesirable.20 The Korean ideal is notable for some unique features, including fuller, oval-shaped cheeks and a small chin with a 0.8–0.9 length ratio of glabellar to nasolabial angle to resemble a “baby” face.22 Through widespread media dissemination, this ideal has significantly influenced Japan, parts of China, and other Asian countries. The aesthetic ideals of Asian immigrants may be impacted by cultural overlays of the Asian or non-Asian countries in which they reside. Counseling of patients should therefore be based on their expressed desires, in the context of geographic and age-appropriate norms, and what is practically feasible given their baseline facial morphotypes.
Comparison of Asian and Caucasian Anatomy
Like others with Fitzpatrick skin phototypes III and above, Asians have been described as developing fewer age-related rhytids compared with the Caucasians. On the anecdotal basis of cadaver dissections, this has been attributed to a thicker dermis, increased fat above and deep to the superficial muscular aponeurotic system, and dense fat and fibrous connections between the superficial muscular aponeurotic system and deep parotidomasseteric fascia.23 Some members of the consensus group noted that considerations such as cumulative sun exposure and other aspects of lifestyle may also be relevant.
The mass of some muscles, such as the corrugators, tends to be lower in Asians than in Caucasians; the corrugators also tend to be shorter, narrower, and less hyperdynamic. These differences are considered to have a genetic basis,24 and perhaps also a cultural one due to variations in the frequency of specific facial expressions such as frowning.25 In contrast, Asians tend to have more developed masseter muscles than most Caucasians. Therefore, compared with Caucasian subjects, lower or higher doses of botulinum toxin type A may be appropriate for Asian subjects, depending on the facial area.
CONSENSUS RECOMMENDATIONS BY FACIAL AREA FOR TREATMENT WITH INCOBOTULINUMTOXINA
In all facial areas, primary treatment with botulinum toxin type A is indicated when excessive muscular contraction is the primary cause of what is observed and is to be addressed. When volume loss is the primary cause, injection of soft tissue fillers is the appropriate first intervention.26 Target muscles, aims, and considerations for specific facial areas are discussed below. Injection points, recommended dosage ranges, and the level of agreement (consensus definition) are provided in Tables 3–17. Levels of agreement were categorized as follows: ≤50% of experts agreed = no consensus; >50–75% of experts agreed = majoritarian agreement; >75–95% of experts agreed = consensus; >95% of experts agreed = strong consensus. The results are calculated as a percentage of the number of completed questionnaires for each category.
Table 3.
Consensus Recommendations for Treatment of Glabellar Rhytids with IncobotulinumtoxinA in Asian Patients
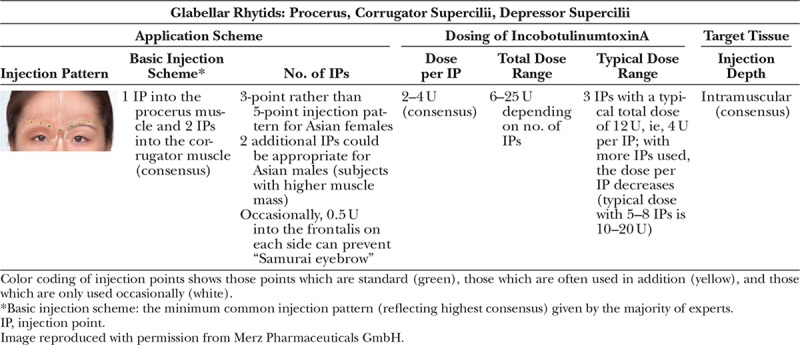
Table 17.
Consensus Recommendations for the “Nefertiti Neck Lift” and Treatment of Platysmal Bands with IncobotulinumtoxinA in Asian Patients
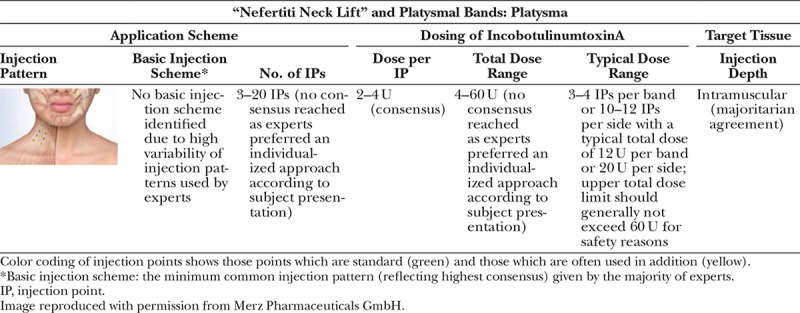
Table 4.
Consensus Recommendations for Treatment of Horizontal Forehead Rhytids with IncobotulinumtoxinA in Asian Patients
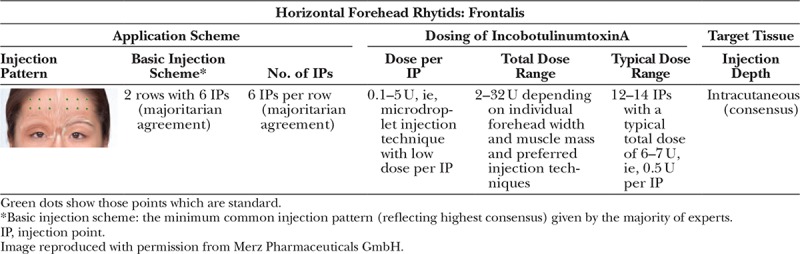
Table 5.
Consensus Recommendations for Eyebrow Shaping Using IncobotulinumtoxinA in Asian Patients
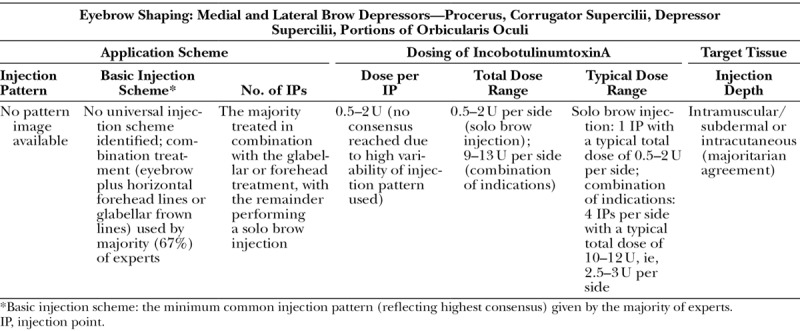
Table 6.
Consensus Recommendations for Treatment of Lateral Canthal Rhytids with IncobotulinumtoxinA in Asian Patients
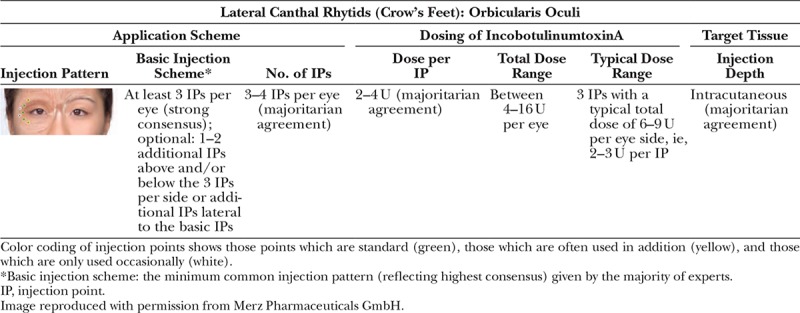
Table 7.
Consensus Recommendations for Treatment of Infraorbital Rhytids with IncobotulinumtoxinA in Asian Patients
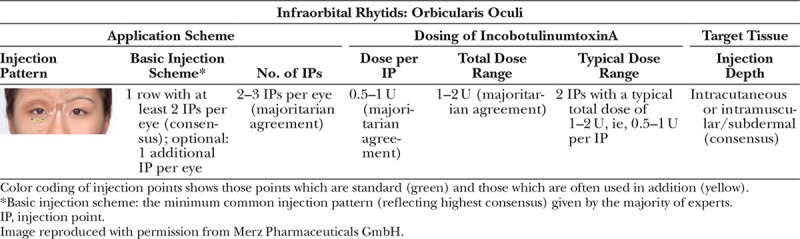
Table 8.
Consensus Recommendations for Infraorbital Eye Opening with IncobotulinumtoxinA in Asian Patients
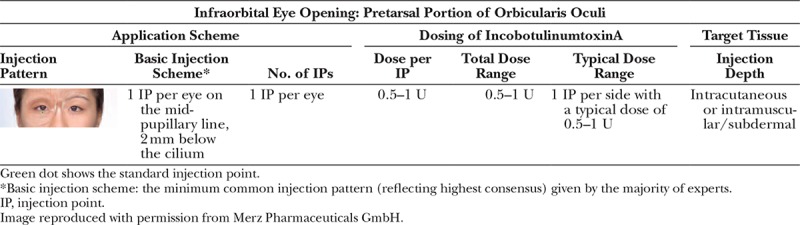
Table 9.
Consensus Recommendations for Treatment of Transverse Nasal Rhytids with IncobotulinumtoxinA in Asian Patients
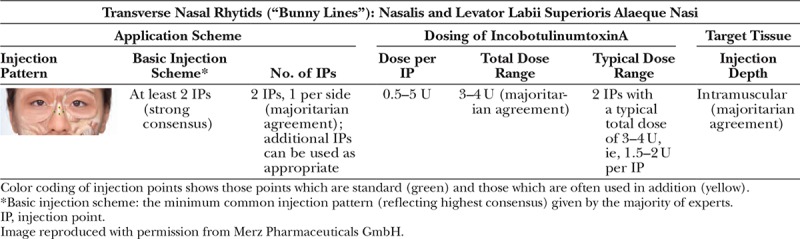
Table 10.
Consensus Recommendations for Treatment of Nasal Flare IncobotulinumtoxinA in Asian Patients
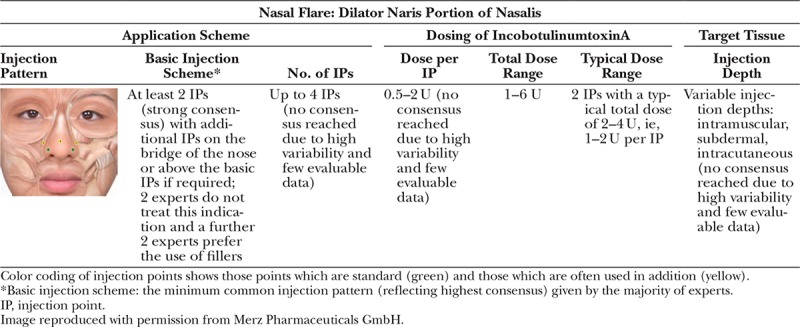
Table 11.
Consensus Recommendations for Nasal Tip Elevation with IncobotulinumtoxinA in Asian Patients
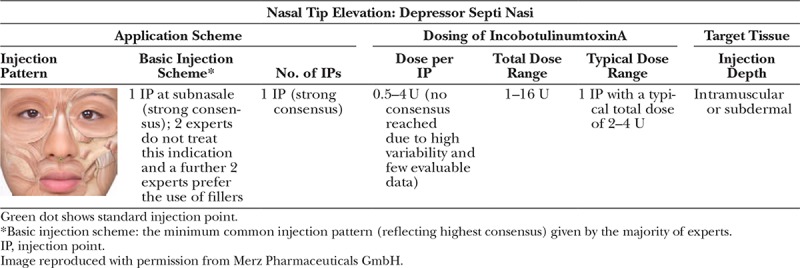
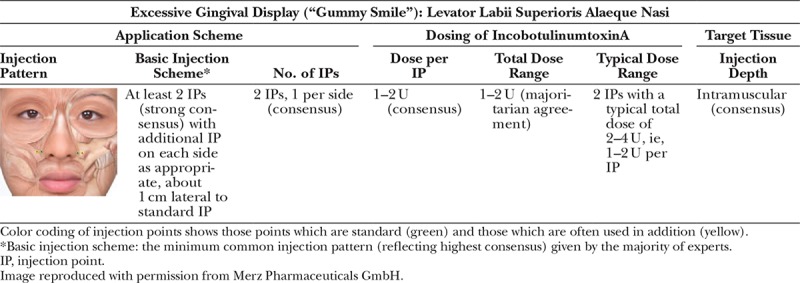
Table 12.
Consensus Recommendations for Treatment of Excessive Gingival Display with IncobotulinumtoxinA in Asian Patients
Glabellar Rhytids: Procerus, Corrugator Supercilii, Depressor Supercilii
Lower doses of botulinum toxin are appropriate for the many Asians who have a lower muscle mass and less hyperdynamic activity than Caucasians. If injection into the lateral aspect of shorter and narrower corrugator supercilii muscles is not indicated, this results in a 3-point injection pattern to the glabella, rather than the traditional 5-point pattern.
Horizontal Forehead Rhytids: Frontalis
The current trend for administering lower doses of botulinum toxin to the frontalis, due to its marked responsiveness, is magnified in Asians, many of whom have a lower muscle mass and less hyperdynamic activity than Caucasians.
Eyebrow Shaping: Medial and Lateral Brow Depressors—Procerus, Corrugator Supercilii, Depressor Supercilii, Portions of Orbicularis Oculi
The aim of all treatment of the eyebrows with botulinum toxin type A is to preserve or restore a natural-looking position. Female eyebrow “lifting” with botulinum toxin has been described extensively in publications with a Caucasian focus.27–31 However, prominently arched brows can make Asian faces look especially unnatural—due, in part, to their relatively greater width. The preferred brow shape for the Asian female is flatter and lower in the lateral two-thirds than has been traditionally advocated for Caucasians. Asians particularly dislike lateral brow arching, which is characterized as the ‘Samurai eyebrow’ and considered to convey anger.
Lateral Canthal Area (“Crow’s Feet”): Orbicularis Oculi
The recommended injection pattern depends on whether orbicularis oculi alone is the cause or zygomaticus is also being recruited. The general trend toward lower doses of botulinum toxin is again exemplified in Asians with lower muscle mass.
Infraorbital Rhytids: Orbicularis Oculi
Chinese patients, and some other patients of Asian descent, quite commonly seek reduction in infraorbital rhytids. If they wish to retain the pretarsal muscular bulge (“charming roll”), injection points should not be placed too close to the lower ciliary margin. The medial infraorbital area should be treated with caution and with low doses to avoid lower eyelid edema.6 Rhytids in this area can be injected subdermally with less than 0.5 U incobotulinumtoxinA at the junction of the preseptal and orbital portions of orbicularis oculi in the medial canthal line. As with all patients, the infraorbital area should not be injected if skin elasticity is poor, as this may result in aesthetic or functional impairment, eg, scleral show.
Infraorbital Eye Opening: Pretarsal Portion of Orbicularis Oculi
This procedure removes the pretarsal muscular bulge (“charming roll”). It is therefore contraindicated in Koreans and other Asians who consider the “charming roll” a hallmark of female beauty, and wish to retain it or enhance it with fillers. Injection of low doses of botulinum toxin to remove the pretarsal bulge and slightly lower the inferior ciliary margin is appropriate in patients with Type III (“Southern”) Asian faces who request it. It widens the palpebral aperture and, hence, appears to enlarge the eyes. This may be considered desirable in Southern Asian cultures, and also in Asian immigrants who have adopted the beauty norms of the non-Asian countries in which they reside.
Transverse Nasal Rhytids (“Bunny Lines”): Nasalis and Levator Labii Superioris Alaeque Nasi
It is beneficial to treat the nasalis and levator labii superioris alaeque nasi in conjunction with the glabella muscles, if there are significant wrinkles on the dorsum of the nose during animation. Rhytids caused by overcontraction of nasalis can be completely removed with botulinum toxin. However, activity of levator labii superioris alaeque nasi and the medial band of the orbicularis oculi cannot be fully obliterated, as this will cause aesthetic and functional impairment.
Nasal Flare: Dilator Naris Portion of the Nasalis
It is beneficial to treat other portions of nasalis in conjunction with the dilator naris if this is indicated by the pattern of muscular overcontraction during animation.
Nasal Tip Elevation: Depressor Septi Nasi
It is appropriate to treat the nasalis or levator labii superioris alaeque nasi in conjunction with the depressor septi nasi, if significant overactivity of all of these muscles during animation is the primary cause of nasal tip drooping.
Excessive Gingival Display (“Gummy Smile”): Levator Labii Superioris Alaeque Nasi
When primary treatment with botulinum toxin is indicated, the convergence point of levator labii superioris, levator labii superioris alaeque nasi, and zygomaticus minor can be targeted. As in all patients, care should be taken with placement of injection sites and dosage to avoid facial asymmetry or aesthetic impairment—in this case, of the smile.
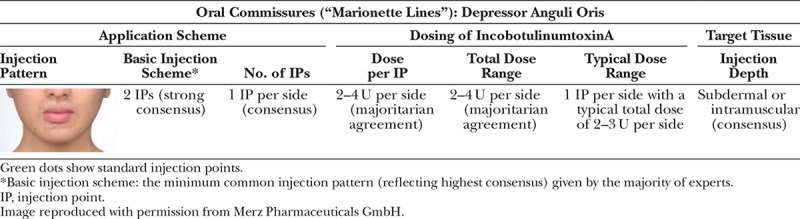
Oral Commissures (“Marionette Lines”): Depressor Anguli Oris
The modiolus, the point at which several facial muscles (including the depressor anguli oris) converge, was found to be lower than the intercheilion horizontal line in almost 60% of an 8-cadaver Korean dissection series (Table 13).32 Based on this, it is recommended that botulinum toxin should be injected into the lower part of the depressor anguli oris to minimize the risk of unwanted spread to other muscles responsible for movement of the corners of the mouth. As for all patients, care should be taken to avoid inadvertent targeting of depressor labii inferioris.
Table 13.
Consensus Recommendations for Treatment of Oral Commissures (“Marionette Lines”) with IncobotulinumtoxinA in Asian Patients
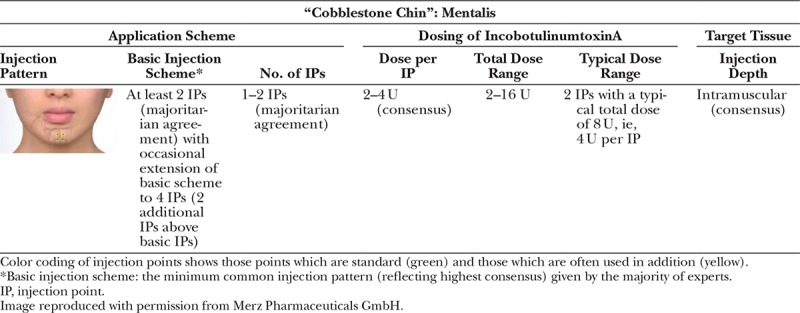
“Cobblestone Chin”: Mentalis
In many Asians, mentalis hyperactivity is secondary to congenital, bony retrusion of the chin (Table 14). This can worsen with age and as volume loss occurs. As for all patients, care should be taken to avoid inadvertent targeting of depressor labii inferioris.
Table 14.
Consensus Recommendations for Treatment of “Cobblestone Chin” with IncobotulinumtoxinA in Asian Patients
Square Jaw: Masseter
Injection of botulinum toxin type A for square jaw has been an established paradigm in Asia for more than 10 years (Table 15).33 Appropriate subjects for treatment have significant masseteric muscle volume, rather than bony prominence of the mandibular angle. Factors that contribute to masseteric hypertrophy include jaw clenching and bruxism, and habitual chewing of gum or hard, dried food.34 One-sided chewing can lead to asymmetric masseteric hypertrophy. Bilateral injection of the masseter muscles decreases their prominence and produces tapering of the lower face. Repeated, high-dose injections over several years can result in chronic muscular atrophy. Muscle volume is a key determinant of botulinum toxin dose, together with regional and cultural variations in the degree of taper that is considered attractive. Lower facial shape can be improved even in individuals who start with a normal muscle thickness of 0.8 cm.35
Table 15.
Consensus Recommendations for Treatment of Square Jaw with IncobotulinumtoxinA in Asian Patients
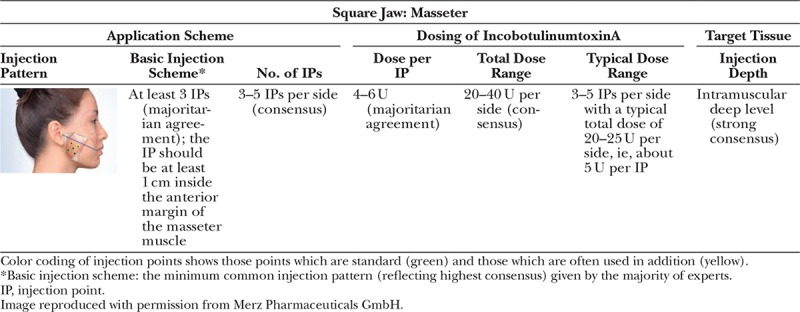
When targeting the masseters, both the onset and peak of effect become apparent significantly later than with other muscles. A decrease in masseteric volume typically starts to become apparent 2 weeks post injection, and the effect continues to develop over the ensuing 1–3 months.36,37 The peak of muscle atrophy is usually reached by 3 months after injection. Muscle volume is usually restored to some extent at 6 months36 and may approach its pretreatment state by 10–12 months after injection. Variation in the duration of effect depends on the individual’s personal habits, such as bruxism, unconscious jaw clenching, and excessive chewing. There are reports of results lasting for more than 1 or 2 years, even after only 1 session of botulinum toxin type A treatment.33 This extended duration of effect has been noted particularly in subjects who have the acquired form of masseteric hypertrophy, avoid excessive chewing, and do not have the habit of jaw clenching. In a proportion of subjects, mild temporary muscular weakness following treatment may manifest as difficulty in chewing; this generally passes and chewing returns to normal force within 3 months.38
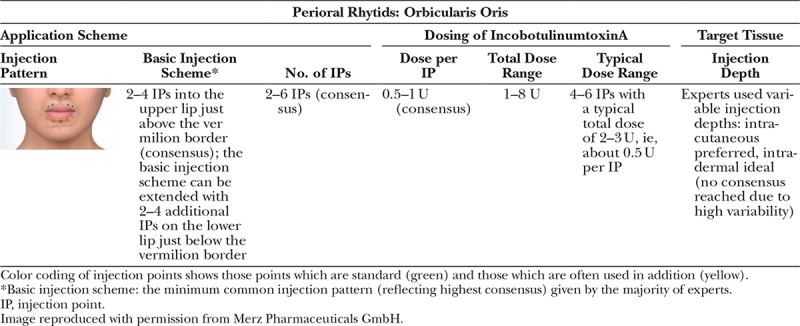
Perioral Rhytids: Orbicularis Oris
As in all patients, careful placement of injection sites and low doses of botulinum toxin are advised (Table 16). Treatment should be performed with caution in Asian patients with a congenitally long philtrum and protruding upper lip, as it may lead to further elongation of the philtrum.
Table 16.
Consensus Recommendations for Treatment of Perioral Rhytids with IncobotulinumtoxinA in Asian Patients
“Nefertiti Neck Lift” and Platysmal Bands: Platysma
Small cadaver dissection series have provided an anatomic rationale for the anecdotal observation that Asians are less likely than Caucasians to develop platysmal bands (Table 17).23 Targeting the portion of platysma that is close to the mandibular insertion (“Nefertiti neck lift”) is popular in Asian subjects.39 Some members of the consensus group noted anecdotally that Asians are quite likely to possess the palpable muscle mass in this area that is a predictor of favorable response.
POSITION STATEMENTS
The Pan-Asian Aesthetics Toxin Consensus Group formulated position statements for the following emerging treatment indications, with the caveat that further data must be accrued to fully assess safety and efficacy from an evidence-based perspective.
Intradermal Botulinum Toxin (“Mesotoxin,” “Dermotoxin,” etc.)
Injection of botulinum toxin type A in the dermal-subdermal layer40 has been reported anecdotally to produce improvement in skin texture and turgor, and reduction in sebum production and pore prominence.41–43 The reported presence of intracutaneous acetylcholine receptors, eg, on sebaceous glands,44 provides a possible mechanism for the observations of improved skin texture.40 Recently, the reduction of sebum production in patients with oily skin following intradermal botulinum toxin type A injection was objectively demonstrated.45
The consensus group discussed the possibility that needle insertion into the skin, rather than botulinum toxin itself, might be sufficient to produce at least some of the beneficial effects.46 They considered it debatable whether the postulated effects are truly due to an intradermal mechanism of action or to the spread of botulinum toxin to underlying and adjacent muscles. From an evidence-based perspective, large, placebo-controlled trials would be required to evaluate the efficacy of intradermal botulinum toxin injection. Because toxin spreads in a 3-dimensional manner from its point of injection, effects on the musculature or the skin cannot be considered in isolation. Intracutaneous injection of botulinum toxin type A has been described as a strategy to preferentially target the superficial portions of the underlying muscles, and hence to achieve efficacy without impairment of function.26
Body Shaping
Although the popularity of body shaping with botulinum toxin type A is reportedly increasing in Asian subjects, it is still dwarfed by facial use. The most commonly described treatment is injection of the calves.47 Asians tend to have short legs relative to their torsos.48 Thick calves further accentuate this physical disproportion, and women dislike the stocky, inelegant appearance this gives them.48 Injection into upper body muscles, such as the deltoids, has also been described to decrease circumference of the upper arms.47
The aim of injecting botulinum toxin type A into the calves is to produce atrophy. Based on clinical experience, 60–100 U incobotulinumtoxinA is typically injected into the head of each gastrocnemius at up to 25 injection sites (Fig. 1). For the upper arms, 50 U incobotulinumtoxinA are typically injected into each deltoid and 50 U incobotulinumtoxinA into the upper part of each trapezius.
Fig. 1.
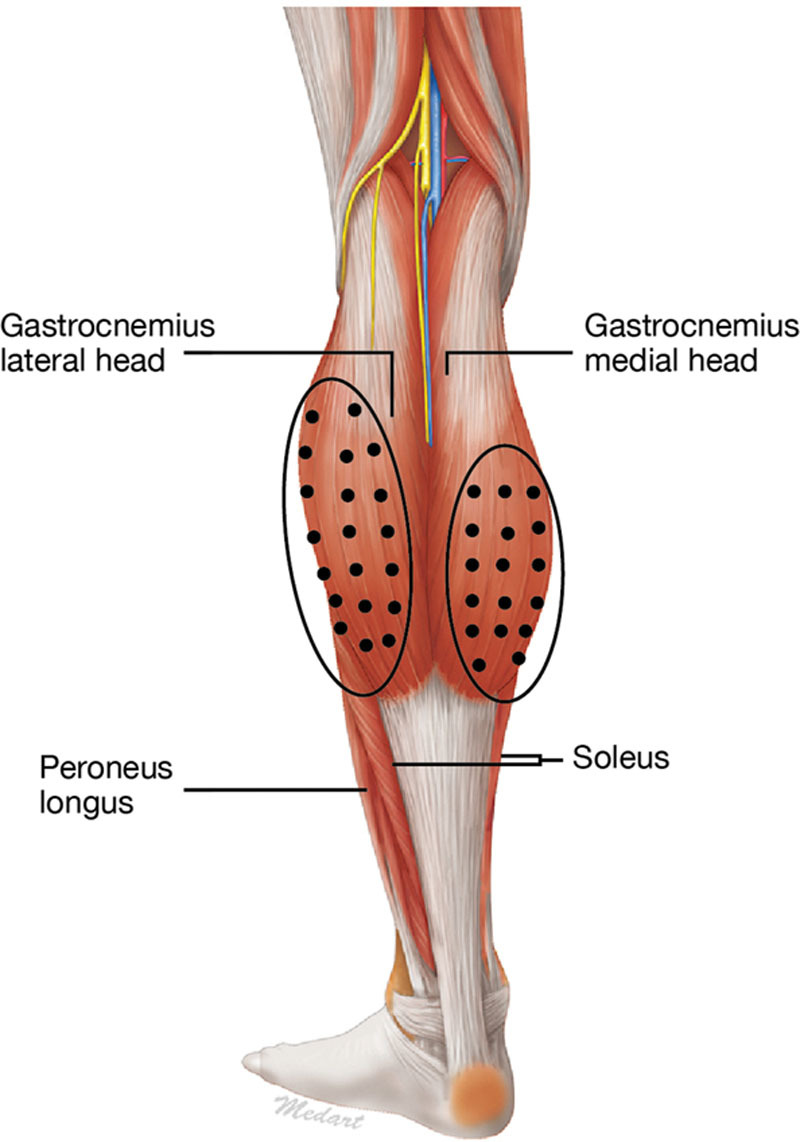
Suggested injection sites of the gastrocnemius muscles for calf shaping according to the position statement. A total of 15–25 IPs are commonly used with a dose of 4 U per injection point and a total dose of 60–100 U for the head of each gastrocnemius muscle. The injection level should be intramuscular. Reproduced with permission from Seo K, Botulinum Toxin for Asians; Jeju, South Korea: Jeju, Korea: Seoul Medical Publishing Ltd.; 2014.
As with treatment of the masseters, onset of atrophy becomes apparent 1–2 weeks post injection and reaches maximum effect by 2–3 months. The muscle returns to approximately half its original volume after 5–6 months and approaches its previous state approximately 10–12 months after injection. If the subject avoids active exercise of the treated muscle, a return to pretreatment muscle volume can be prevented. Clinical experience indicates that repeated injections over several years can also result in chronic muscular atrophy. The consensus group added the caveat that it does not consider functional impairment to be an acceptable result of cosmetic treatment with botulinum toxin.
Reduction of the Parotid Glands
Enlarged parotid glands can contribute to a square-shaped lower face.48 Because acetylcholine acts as the neurotransmitter in salivary glands as it does in the neuromuscular junction, it can be blocked by botulinum toxin type A.49 Injection of an enlarged or protruding parotid gland can reduce the width of the lower face, as an adjunct to treatment of the masseter muscles.50,51 Injection of the parotid gland seldom results in a dry mouth, as the majority of salivary production (71% in one report52) comes from the submandibular gland. The most protruding part of the parotid gland around the mandibular angle is the preferred injection site. Based on clinical experience, 4–6 injection points are typically used for the parotid gland with a dose of 4–6 U incobotulinumtoxinA per injection site (Fig. 2). Injection of botulinum toxin in very thin subjects with an obvious submandibular salivary gland can improve lines on the neck.
Fig. 2.

Suggested parotid gland injection sites for gland reduction according to the position statement. A total of 4–6 IPs with a dose of 4–6 U per IP is suggested giving a total dose of approximately 30 U (20–40 U) depending on the volume of the parotid gland. The level of injection is intraglandular. IP, injection point. Reproduced with permission from Seo K, Botulinum Toxin for Asians; Jeju, Korea: Seoul Medical Publishing Ltd.; 2014.
CONCLUSIONS
Given the rapid rise in demand for cosmetic procedures in Asia and the global migration of Asians, these recommendations are germane to physicians throughout the world. When planning and implementing treatment with botulinum toxin type A, it must be understood that anatomic and cultural differences exist not only between Asians and Caucasians, but also among Asians. In addition, it is important to appreciate that Asians seek botulinum toxin treatment for cosmetic enhancement and for rejuvenation. The aim of these consensus recommendations is to provide guidelines for optimal treatment of Asians across a full range of indications.
ACKNOWLEDGMENTS
We thank Dr. Benjamin Ascher, Dr. Derek Jones, and Dr. Berthold Rzany for their critical review of the manuscript, and Scientific Communications & Information, Oxford, United Kingdom for editorial support and assistance with formatting of the manuscript and figures. Merz Pharmaceuticals GmbH supported this assistance, the Pan-Asian Aesthetics Toxin Consensus Group meeting, and the creation of these recommendations. The content of the publication reflects the opinions and experiences of the experts.
Footnotes
Disclosure: Hema Sundaram, MD, has served as a clinical investigator and/or consultant for Allergan, CosmoFrance, Daewoong, Evolus/Strathspey Crown, Galderma, Institut Biochimique SA, Ipsen, JuvaPlus, Kythera, Merz Pharmaceuticals, Suneva and Teoxane. Po-Han Huang, MD, serves as a clinical investigator for Galderma and a consultant for Merz Pharmaceuticals. Nai-Jen Hsu, MD, has collaborated with Q-Med/Galderma on several clinical studies and has been a consultant for Merz Pharmaceuticals. Chang Hun Huh, MD, PhD, serves as a clinical investigator for Medytox, Valeant Aesthetics, Solstice Neurosciences, LG Life Sciences, Revance Therapeutics, GlaxoSmithKline, Merck Sharp & Dohme, and Skin MD and a consultant for Merz Pharmaceuticals. Woffles T. L. Wu, MD, sits on advisory boards for Allergan, Galderma, and Merz Pharmaceuticals and has received honoraria for attending advisory board meetings and delivering local and international workshops and lectures. Yan Wu, MD, PhD, serves as a clinical investigator for Allergan, GlaxoSmithKline, Lanzhou Biological Products Institute, and Freda Biopharm (Shandong hyaluronic acid filler). Daniel Cassuto, MD, has served as a clinical investigator and/or consultant for CosmoFrance, Galderma, HaoHai Healthcare, Institut Biochimique SA, Ipsen, JuvaPlus and Merz Pharmaceuticals. Martina J. Kerscher, MD, serves as a clinical investigator and has collaborated with Merz Pharmaceuticals, Q-Med, Laboratoires Pierre Fabre SA, and Kythera on several clinical studies. Kyle Koo-Il Seo, MD, PhD, serves as a clinical investigator and/or consultant for Allergan, Merz Pharmaceuticals, Q-Med/Galderma, Medytox, LG Life Sciences, and Daewoong. The Article Processing Charge was paid for by Merz Pharmaceuticals.
REFERENCES
- 1.Ascher B, Talarico S, Cassuto D, et al. International consensus recommendations on the aesthetic usage of botulinum toxin type A (Speywood Unit)–Part II: Wrinkles on the middle and lower face, neck and chest. J Eur Acad Dermatol Venereol. 2010;24:1285–1295. doi: 10.1111/j.1468-3083.2010.03728.x. [DOI] [PubMed] [Google Scholar]
- 2.Ascher B, Talarico S, Cassuto D, et al. International consensus recommendations on the aesthetic usage of botulinum toxin type A (Speywood Unit)–Part I: Upper facial wrinkles. J Eur Acad Dermatol Venereol. 2010;24:1278–1284. doi: 10.1111/j.1468-3083.2010.03631.x. [DOI] [PubMed] [Google Scholar]
- 3.Carruthers A, Kane MA, Flynn TC, et al. The convergence of medicine and neurotoxins: a focus on botulinum toxin type A and its application in aesthetic medicine–a global, evidence-based botulinum toxin consensus education initiative: part I: botulinum toxin in clinical and cosmetic practice. Dermatol Surg. 2013;39(3 Pt 2):493–509. doi: 10.1111/dsu.12147. [DOI] [PubMed] [Google Scholar]
- 4.Carruthers J, Fagien S, Matarasso SL Botox Consensus Group. Consensus recommendations on the use of botulinum toxin type a in facial aesthetics. Plast Reconstr Surg. 2004;114(6 Suppl):1S–22S. doi: 10.1097/01.PRS.0000144795.76040.D3. [DOI] [PubMed] [Google Scholar]
- 5.Carruthers J, Fournier N, Kerscher M, et al. The convergence of medicine and neurotoxins: a focus on botulinum toxin type A and its application in aesthetic medicine–a global, evidence-based botulinum toxin consensus education initiative: part II: incorporating botulinum toxin into aesthetic clinical practice. Dermatol Surg. 2013;39(3 Pt 2):510–525. doi: 10.1111/dsu.12148. [DOI] [PubMed] [Google Scholar]
- 6.Carruthers JD, Glogau RG, Blitzer A Facial Aesthetics Consensus Group Faculty. Advances in facial rejuvenation: botulinum toxin type a, hyaluronic acid dermal fillers, and combination therapies–consensus recommendations. Plast Reconstr Surg. 2008;121(5 Suppl):5S–30S. doi: 10.1097/PRS.0b013e31816de8d0. quiz 31S. [DOI] [PubMed] [Google Scholar]
- 7.Poulain B, Trevidic P, Clave M, et al. Clinical equivalence of conventional OnabotulinumtoxinA (900 KDa) and IncobotulinumtoxinA (neurotoxin free from complexing proteins - 150 KDa): 2012 multidisciplinary French consensus in aesthetics. J Drugs Dermatol. 2013;12:1434–1446. [PubMed] [Google Scholar]
- 8.Ahn BK, Kim YS, Kim HJ, et al. Consensus recommendations on the aesthetic usage of botulinum toxin type A in Asians. Dermatol Surg. 2013;39:1843–1860. doi: 10.1111/dsu.12317. [DOI] [PubMed] [Google Scholar]
- 9.AGREE Next Steps Consortium. The AGREE II Instrument. Available at: http://www.agreetrust.org. Accessed January 16, 2014.
- 10.Sattler G, Callander MJ, Grablowitz D, et al. Noninferiority of incobotulinumtoxinA, free from complexing proteins, compared with another botulinum toxin type A in the treatment of glabellar frown lines. Dermatol Surg. 2010;36(Suppl 4):2146–2154. doi: 10.1111/j.1524-4725.2010.01706.x. [DOI] [PubMed] [Google Scholar]
- 11.Karsai S, Raulin C. Current evidence on the unit equivalence of different botulinum neurotoxin A formulations and recommendations for clinical practice in dermatology. Dermatol Surg. 2009;35:1–8. doi: 10.1111/j.1524-4725.2008.34375.x. [DOI] [PubMed] [Google Scholar]
- 12.Kane M, Donofrio L, Ascher B, et al. Expanding the use of neurotoxins in facial aesthetics: a consensus panel’s assessment and recommendations. J Drugs Dermatol. 2010;9(1 Suppl):s7–s22, quiz s23–s25. [PubMed] [Google Scholar]
- 13.Le TT, Farkas LG, Ngim RC, et al. Proportionality in Asian and North American Caucasian faces using neoclassical facial canons as criteria. Aesthetic Plast Surg. 2002;26:64–69. doi: 10.1007/s00266-001-0033-7. [DOI] [PubMed] [Google Scholar]
- 14.Porter JP, Lee JI. Facial analysis: maintaining ethnic balance. Facial Plast Surg Clin North Am. 2002;10:343–349. doi: 10.1016/s1064-7406(02)00030-5. [DOI] [PubMed] [Google Scholar]
- 15.Sim RS, Smith JD, Chan AS. Comparison of the aesthetic facial proportions of southern Chinese and white women. Arch Facial Plast Surg. 2000;2:113–120. doi: 10.1001/archfaci.2.2.113. [DOI] [PubMed] [Google Scholar]
- 16.Wang D, Qian G, Zhang M, et al. Differences in horizontal, neoclassical facial canons in Chinese (Han) and North American Caucasian populations. Aesthetic Plast Surg. 1997;21:265–269. doi: 10.1007/s002669900123. [DOI] [PubMed] [Google Scholar]
- 17.Sundaram H, Carruthers J. The glabella and central brow. In: Carruthers J, Carruthers A, editors. In: Procedures in Cosmetic Dermatology: Soft Tissue Augmentation. 3rd Edition. Amsterdam: Elsevier Saunders; 2013. pp. 88–99. [Google Scholar]
- 18.Webster R. Face Reading Quick and Easy. Woodbury, Minn.: Llewellyn Publications; 2012. [Google Scholar]
- 19.Chen X. The Full Textbook of Face Reading. Tainan, Taiwan: Da Fu Publishing Co; 1994. [Google Scholar]
- 20.Chen Y-J, Huang T-H, Kao C-T. Perception of ethnic Chinese facial esthetics in Taiwan - a pilot study. J Dent Sci. 2007;2:75–87. [Google Scholar]
- 21.Rhee SC. The average Korean attractive face. Aesthetic Plast Surg. 2006;30:729–730. doi: 10.1007/s00266-006-0157-x. [DOI] [PubMed] [Google Scholar]
- 22.Lee JS, Kim HK, Kim YW. Anthropometric analysis of the attractive and normal faces in Korean female. J Korean Soc Plast Reconstr Surg. 2004;31:526–531. [Google Scholar]
- 23.Sykes JM. Management of the aging face in the Asian patient. Facial Plast Surg Clin North Am. 2007;15:353–60, vi. doi: 10.1016/j.fsc.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 24.Yang HM, Kim HJ. Anatomical study of the corrugator supercilii muscle and its clinical implication with botulinum toxin A injection. Surg Radiol Anat. 2013;35:817–821. doi: 10.1007/s00276-013-1174-5. [DOI] [PubMed] [Google Scholar]
- 25.Tzou CH, Giovanoli P, Ploner M, et al. Are there ethnic differences of facial movements between Europeans and Asians? Br J Plast Surg. 2005;58:183–195. doi: 10.1016/j.bjps.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 26.Sundaram H, Signorini M, Liew S, et al. Global Aesthetics Consensus: Botulinum Toxin Type A – Evidence-Based Review, Emerging Concepts, and Consensus Recommendations for Aesthetic Use, Including Updates on Complications. Plast Reconstr Surg. 2016;137:518e–529e. doi: 10.1097/01.prs.0000475758.63709.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frankel AS, Kamer FM. Chemical browlift. Arch Otolaryngol Head Neck Surg. 1998;124:321–323. doi: 10.1001/archotol.124.3.321. [DOI] [PubMed] [Google Scholar]
- 28.Huilgol SC, Carruthers A, Carruthers JD. Raising eyebrows with botulinum toxin. Dermatol Surg. 1999;25:373–375, discussion 376. doi: 10.1046/j.1524-4725.1999.08286.x. [DOI] [PubMed] [Google Scholar]
- 29.Kornstein AN. Soft-tissue reconstruction of the brow with Restylane. Plast Reconstr Surg. 2005;116:2017–2020. doi: 10.1097/01.prs.0000191170.92779.a3. [DOI] [PubMed] [Google Scholar]
- 30.Sundaram H, Kiripolsky M. Nonsurgical rejuvenation of the upper eyelid and brow. Clin Plast Surg. 2013;40:55–76. doi: 10.1016/j.cps.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 31.Carruthers A, Carruthers J. Eyebrow height after botulinum toxin type A to the glabella. Dermatol Surg. 2007;33(1 Spec No):S26–S31. doi: 10.1111/j.1524-4725.2006.32328.x. [DOI] [PubMed] [Google Scholar]
- 32.Hu K, Yang S, Kwak H, et al. Location of the modiolous and the morphologic variations of the risorius and zygomaticus major muscle related to the facial expression in Koreans. Korean J Phys Anthropol. 2005;18:1–11. [Google Scholar]
- 33.Kim NH, Chung JH, Park RH, et al. The use of botulinum toxin type A in aesthetic mandibular contouring. Plast Reconstr Surg. 2005;115:919–930. doi: 10.1097/01.prs.0000153236.79775.a0. [DOI] [PubMed] [Google Scholar]
- 34.Mandel L, Tharakan M. Treatment of unilateral masseteric hypertrophy with botulinum toxin: case report. J Oral Maxillofac Surg. 1999;57:1017–1019. doi: 10.1016/s0278-2391(99)90029-0. [DOI] [PubMed] [Google Scholar]
- 35.Xu JA, Yuasa K, Yoshiura K, et al. Quantitative analysis of masticatory muscles using computed tomography. Dentomaxillofac Radiol. 1994;23:154–158. doi: 10.1259/dmfr.23.3.7835516. [DOI] [PubMed] [Google Scholar]
- 36.Yu CC, Chen PK, Chen YR. Botulinum toxin a for lower facial contouring: a prospective study. Aesthetic Plast Surg. 2007;31:445–451. doi: 10.1007/s00266-007-0081-8. discussion 452. [DOI] [PubMed] [Google Scholar]
- 37.Kim HJ, Yum KW, Lee SS, et al. Effects of botulinum toxin type A on bilateral masseteric hypertrophy evaluated with computed tomographic measurement. Dermatol Surg. 2003;29:484–489. doi: 10.1046/j.1524-4725.2003.29117.x. [DOI] [PubMed] [Google Scholar]
- 38.Kim KS, Byun YS, Kim YJ, et al. Muscle weakness after repeated injection of botulinum toxin type A evaluated according to bite force measurement of human masseter muscle. Dermatol Surg. 2009;35:1902–1906. doi: 10.1111/j.1524-4725.2009.01319.x. [DOI] [PubMed] [Google Scholar]
- 39.Levy PM. The ‘Nefertiti lift’: a new technique for specific re-contouring of the jawline. J Cosmet Laser Ther. 2007;9:249–252. doi: 10.1080/14764170701545657. [DOI] [PubMed] [Google Scholar]
- 40.Wu WT. Innovative uses of botox and the Woffles lift. In: Panfilov D, editor. In: Aesthetic Surgery of the Facial Mosaic. Berlin: Springer; 2006. pp. 636–649. [Google Scholar]
- 41.Chang SP, Tsai HH, Chen WY, et al. The wrinkles soothing effect on the middle and lower face by intradermal injection of botulinum toxin type A. Int J Dermatol. 2008;47:1287–1294. doi: 10.1111/j.1365-4632.2008.03895.x. [DOI] [PubMed] [Google Scholar]
- 42.Rose AE, Goldberg DJ. Safety and efficacy of intradermal injection of botulinum toxin for the treatment of oily skin. Dermatol Surg. 2013;39(3 Pt 1):443–448. doi: 10.1111/dsu.12097. [DOI] [PubMed] [Google Scholar]
- 43.Shah AR. Use of intradermal botulinum toxin to reduce sebum production and facial pore size. J Drugs Dermatol. 2008;7:847–850. [PubMed] [Google Scholar]
- 44.Kurzen H, Wessler I, Kirkpatrick CJ, et al. The non-neuronal cholinergic system of human skin. Horm Metab Res. 2007;39:125–135. doi: 10.1055/s-2007-961816. [DOI] [PubMed] [Google Scholar]
- 45.Li ZJ, Park SB, Sohn KC, et al. Regulation of lipid production by acetylcholine signalling in human sebaceous glands. J Dermatol Sci. 2013;72:116–122. doi: 10.1016/j.jdermsci.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 46.Kapoor R, Shome D, Jain V, et al. Facial rejuvenation after intradermal botulinum toxin: is it really the botulinum toxin or is it the pricks? Dermatol Surg. 2010;36(Suppl 4):2098–2105. doi: 10.1111/j.1524-4725.2010.01703.x. [DOI] [PubMed] [Google Scholar]
- 47.Seo KK, Lee W. Medytoxin/Neuronox®. In: Carruthers J CA, editor. In: Botulinum Toxin. Philadelphia, Pa.: Elsevier; 2012. pp. 52–58. [Google Scholar]
- 48.Wu WT. Facial and lower limb contouring. In: Benedetto A, editor. In: Botulinum Toxins in Clinical Aesthetic Practice. Boca Raton: CRC Press; 2011. pp. 206–222. [Google Scholar]
- 49.Teymoortash A, Sommer F, Mandic R, et al. Intraglandular application of botulinum toxin leads to structural and functional changes in rat acinar cells. Br J Pharmacol. 2007;152:161–167. doi: 10.1038/sj.bjp.0707375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu WT. Botox facial slimming/facial sculpting: the role of botulinum toxin-A in the treatment of hypertrophic masseteric muscle and parotid enlargement to narrow the lower facial width. Facial Plast Surg Clin North Am. 2010;18:133–140. doi: 10.1016/j.fsc.2009.11.014. [DOI] [PubMed] [Google Scholar]
- 51.Bae GY, Yune YM, Seo K, et al. Botulinum toxin injection for salivary gland enlargement evaluated using computed tomographic volumetry. Dermatol Surg. 2013;39:1404–1407. doi: 10.1111/dsu.12247. [DOI] [PubMed] [Google Scholar]
- 52.Elluru RG. Physiology of the salivary glands. In: Flint P, Haughey B, Lund V, et al., editors. In: Cummings Otolaryngology. Philadelphia, Pa: Mosby Elsevier; 2010. Chapter 84. [Google Scholar]


