Abstract
Introduction:
The complex anatomy and function of the native penis is difficult to surgically replicate. Metoidioplasty and radial forearm flap phalloplasty (RFFP) are the 2 most commonly utilized procedures for transgender neophallus construction.
Methods:
A MEDLINE search for metoidioplasty and RFFP in female-to-male genital reconstruction was performed. Primary outcome measures were subsequently compared. A systematic review was planned in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyse guidelines. Grading of Recommendations Assessment, Development and Evaluation (GRADE) was utilized to evaluate the quality of evidence.
Results:
Using Population, Intervention, Comparison and Outcomes tool criteria, a total of 188 articles were identified; 7 articles related to metoidioplasty and 11 articles related to RFFP met inclusion criteria. The GRADE quality of evidence was low to very low for all included studies. In studies examining metoidioplasty, the average study size and length of follow-up were 54 patients and 4.6 years, respectively (1 study did not report [NR]). Eighty-eight percent underwent a single-stage reconstruction (0 NR), 87% reported an aesthetic neophallus (3 NR), and 100% reported erogenous sensation (2 NR). Fifty-one percent of patients reported successful intercourse (3 NR), and 89% of patients achieved standing micturition (3 NR). In studies examining RFFP, the average study size and follow-up were 60.4 patients and 6.23 years, respectively (6 NR). No patients underwent single-stage reconstructions (8 NR). Seventy percent of patients reported a satisfactorily aesthetic neophallus (4 NR), and 69% reported erogenous sensation (6 NR). Forty-three percent reported successful penetration of partner during intercourse (6 NR), and 89% achieved standing micturition (6 NR). Compared with RFFP, metoidioplasty was significantly more likely to be completed in a single stage (P < 0.0001), have an aesthetic result (P = 0.0002), maintain erogenous sensation (P < 0.0001), achieve standing micturition (P = 0.001), and have a lower overall complication rate (P = 0.02).
Conclusions:
Although the current literature suggests that metoidioplasty is more likely to yield an “ideal” neophallus compared with RFFP, any conclusion is severely limited by the low quality of available evidence.
Gender dysphoria (DSM-V) is characterized by the experience of a profound incongruence between ones’ gender identity and birth anatomy (natal gender).1,2 Increasingly, gender-confirming surgery (GCS) is being initiated by gender-variant/gender- dysphoric patients who wish to align their physical body with their preferred gender identity. Along with this increasing demand comes a pressing need to better understand the medical and emotional issues affecting this patient population and a greater number of surgeons equipped to perform these reconstructions.3 Compared with the male-to-female transgender population (natal males being affirmed as females), female-to-male transgender patients (natal females being affirmed as males) are markedly underrepresented within the existing medical literature on transgender health needs and GCS.4,5 Given this discrepancy, far more information is available on the male-to-female transgender patient population—in terms of demographics, medical management, surgical techniques, and surgical outcomes—than for their female-to-male counterparts.6
For the natal female patient being affirmed as a male, GCSs primarily include male chest wall contouring (“top surgery”) and genital reconstruction (“bottom surgery”).7 In genital reconstruction, the neophallus is surgically fashioned in conjunction with other primary procedures—such as vaginectomy, hysterectomy–oophorectomy, and penile prosthesis insertion.8
To date, no study has sought to comprehensively assess patient-reported satisfaction with surgical outcomes. Similarly, the notion of an “ideal” bottom surgery outcome has not been articulated from the perspective of patients’ whose desires and preferences have scarcely been queried in a formal research capacity. In 1993, Hage and De Graaf9,10 described the “ideal” neophallus as one that is crafted reproducibly in a single-stage procedure, is aesthetically pleasing to the patient, has tactile and erogenous sensation, has a functional neourethra that permits standing urination, and confers minimal complications and donor-site morbidity. This list was subsequently amended by Monstrey et al11 who added the creation of an aesthetic neoscrotum. This notion of an “ideal” neophallus is repeatedly referenced throughout the existing medical literature.
Metoidioplasty and radial forearm free flap phalloplasty are the 2 most common surgical techniques utilized in genital reconstruction for the female-to-male transgender patient.10,12 Metoidioplasty involves the creation of a neophallus from the female clitoris, which is often hypertrophied by the effects of hormonal stimulation.10,12 Advantages of this technique include “like-with-like” penile reconstruction, a limited local donor site, and the ability to achieve erectile rigidity without a prosthesis. However, the resultant neophallus is often shorter and smaller than in other techniques, potentially compromising sexual function and capacity for standing micturition.13,14
Radial forearm free flap phalloplasty (RFFP) is considered the workhorse technique in transgender phalloplasty.11 RFFP is advantageous for its capacity to produce a longer and thicker neophallus with good aesthetic results. Disadvantages include a large and potentially stigmatizing donor site, the need for erectile prostheses for successful penetration of partner, and difficulty with urethroplasty because of a longer, pendulous neourethra.11,15
The existing literature on outcomes in female-to-male transgender genital reconstruction is profoundly lacking. To date, no study has sought to directly assess how outcomes differ by and across individual techniques, and no standardized system of evaluation has been developed to critically assess surgical outcomes. Without comparative studies and/or a standardized system to evaluate outcomes, it is difficult to determine which technique is most capable of producing a neophallus close to the “ideal” standard described by Hage and De Graaf.9 For this reason, we set out to examine the existing literature on outcomes in metoidioplasty and RFFP in the context of GCS and to investigate which procedure is most likely to procure an outcome closest to the “ideal” standards described by Hage and De Graaf.9
METHODS
Using PICOS criteria, we identified patients as those undergoing female-to-male transgender phalloplasty with an intervention of either metoidioplasty or radial forearm flap phalloplasty, the comparator being the success of the phalloplasty procedure in these patients. In accordance with description of the “ideal” neophallus by Hage and De Graaf,9 the following primary outcome measures were utilized: proportion of reconstructions performed in a single-stage, degree of aesthetic satisfaction and erogenous/tactile sensation, rate of neourethral stricture and fistulas, proportion of patients able to successfully penetrate partner during intercourse, rate of standing micturition, and rates of donor-site morbidity and overall complications. A systematic review was carried out in accordance with PRISMA guidelines. A MEDLINE search was performed using the search terms “metoidioplasty,” “metaidoioplasty,” and “radial forearm flap phalloplasty” (Fig. 1).
Fig. 1.
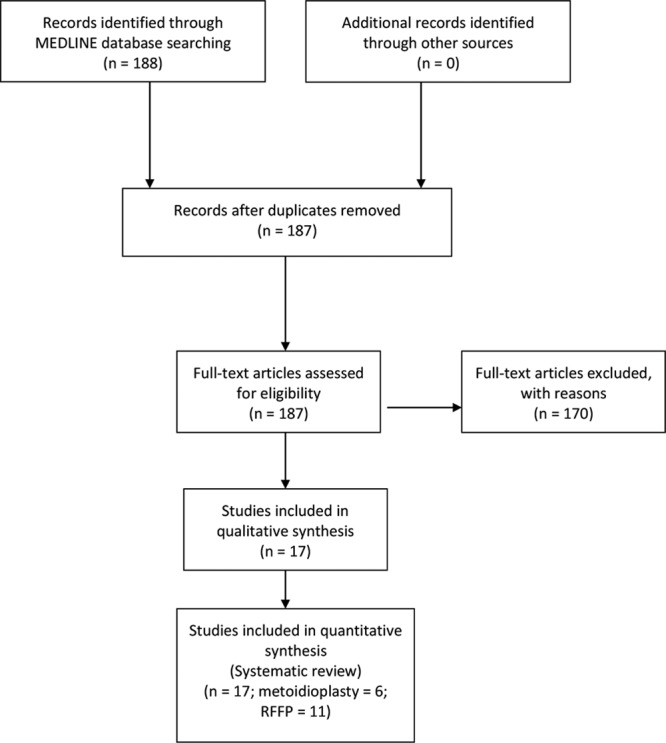
Flow diagram depicting search strategy and article selection.
Only articles that described techniques in the context of female-to-male transgender genital reconstruction were considered for review; articles describing these techniques in the context of male penile reconstruction after trauma, or for extirpative procedures, were excluded. Irrespective of the technique, articles had to detail the reconstruction of some portion of the entire neophallus, including the skin/soft tissue component and the urethral component. Articles that described a technique only for a component reconstruction, such as radial forearm flap utilized solely for neourethral construction, were excluded. Variations in the technique were allowed and not considered cause for exclusion. For example, articles examining both fasciocutaneous and osseofasciocutaneous radial forearm flap phalloplasties were included in our analysis. Single case reports were excluded. Articles selected for inclusion were reviewed for demographics (number of subjects per study, etc), followed by outcome parameters. GRADE was utilized to evaluate the quality of evidence. Data were extracted through a careful review of individual articles.
Descriptive statistics and mean values were used to describe results for examined parameters in all studies on metoidioplasty and radial forearm flap phalloplasty, respectively. Collective outcomes for the 2 techniques were subsequently compared. Student t tests were used to analyze binary data sets. Chi-square analysis was used to compare proportional responses. P values of less than 0.05 were deemed significant. Of note, there was no funding for this review.
RESULTS
A total of 188 relevant articles were identified. Seven articles related to metoidioplasty13,14,16–20 and 11 articles related to RFFP11,15,21–29 met inclusion criteria for subsequent analysis. One article related to metoidioplasty17 included patients who were subsequently incorporated into an additional study carried out with more patients and a lengthier follow-up period.18 The study reporting early results was therefore excluded from analysis (Fig. 1). Notably, all of the included studies were assigned either low or very low-quality ratings in accordance with the GRADE approach.30
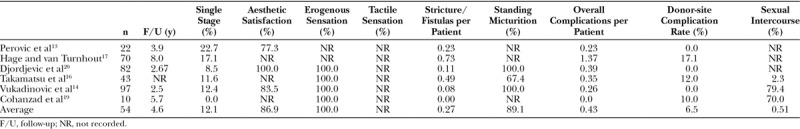
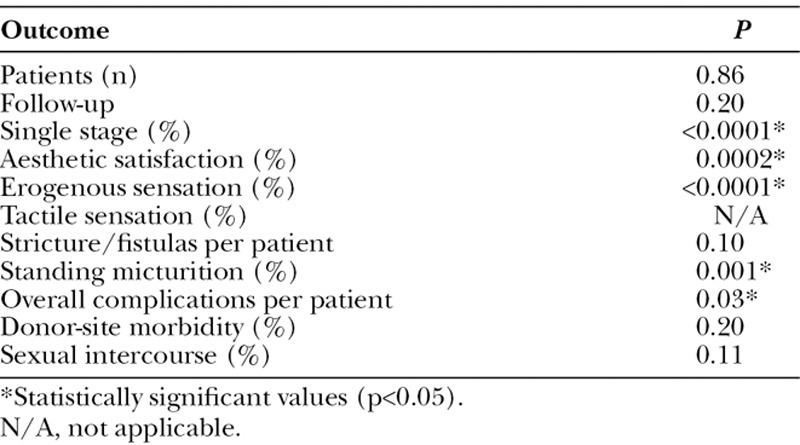
In studies examining metoidioplasty, the average sample size and follow-up period were 54.0 patients and 4.6 years, respectively (1 study did not report [NR] the follow-up period). Approximately 88% of patients underwent single-stage reconstructions (0 NR). Eighty-seven percent of patients reported a satisfactorily aesthetic neophallus (3 NR), 100% of patients reported erogenous sensation (2 NR), and no studies reported tactile sensation (7 NR). Fifty-one percent of patients reported successful penetration of partner during intercourse (3 NR), and 89.1% reported standing micturition (3 NR). The average number of strictures and/or fistulae per patient was 0.27 (0 NR), whereas the average overall rate of complications per patient was 0.43 (0 NR). Donor-site morbidity was 6.5% (0 NR; Table 1).
Table 1.
Demographics and Outcomes in Included Studies Examining Metoidioplasty for Female-to-male Transgender Genital Reconstruction
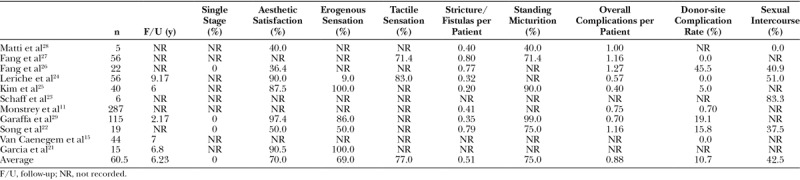
In studies examining radial forearm flap phalloplasty, the average sample size and length of follow-up period were 60.4 patients and 6.23 years (6 NR), respectively. No patients had a single-stage reconstruction (8 NR), yet 70% reported a satisfactorily aesthetic neophallus (4 NR). Sixty-nine percent of patients reported erogenous sensation (6 NR), and 77% reported tactile sensation (9 NR). Forty-three percent of patients reported successful penetration of partner during intercourse (6 NR), and 75% reported standing micturition (6 NR). The average number of strictures and/or fistulae per patient was 0.51 (4 NR), whereas the average overall rate of complications per patient was 0.88 (3 NR). Donor-site morbidity was 11% (3 NR; Table 2).
Table 2.
Demographics and Outcomes in Included Studies Examining Radial Forearm Flap Phalloplasty for Female-to-male Transgender Genital Reconstruction
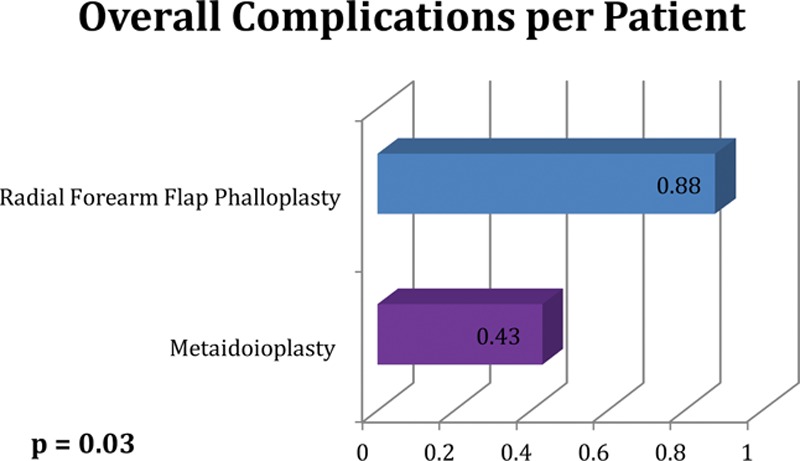
Comparing the 2 groups, sample size (P = 0.86) and follow-up (P = 0.20) were equivalent. Compared with RFFP, metoidioplasty was significantly more likely to be completed in a single stage (P < 0.0001), to have an aesthetic result (P = 0.0002), maintain erogenous sensation (P < 0.0001), report standing micturition (P = 0.001), and have a lower overall complication rate (P = 0.03; Figs. 2, 3). Outcomes for urethral stricture/fistulae (P = 0.08), donor-site morbidity (P = 0.11), and the number of patients reporting successful penetration of partner during intercourse (P = 0.1061) were similar. Since no metoidioplasty study explicitly reported on tactile sensation, these outcome measures could not be compared (Table 3).
Fig. 2.
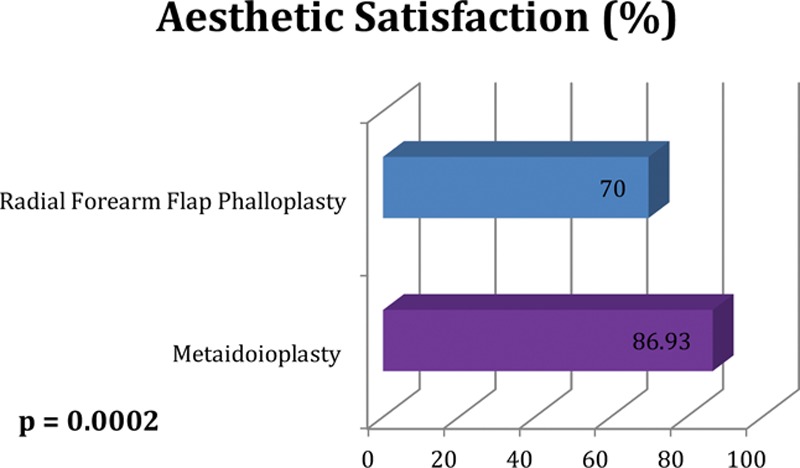
Collective aesthetic satisfaction ratings compared for patients undergoing metoidioplasty versus radial forearm flap phalloplasty.
Fig. 3.
Collective overall complications per patient compared for patients undergoing metoidioplasty versus radial forearm flap phalloplasty.
Table 3.
P Values for Comparison of Outcomes in Included Studies Examining Metoidioplasty and Radial Forearm Flap Phalloplasty
DISCUSSION
An increasing portion of the transgender patient population is pursuing GCS.3 Surgical procedures for the natal female being affirmed as male primarily include male chest wall reconstruction (“top” surgery) and genital reconstruction (“bottom surgery”) to surgically construct a neophallus.7
According to Hage and De Graaf9,10, the “ideal” neophallus is crafted reproducibly in a single-stage procedure, is aesthetic, has tactile and erogenous sensation, has a functional neourethra to permit standing urination, and is associated with minimal complications and donor-site morbidity. Despite recent advances, no singular surgical technique is yet capable of effectively and reliably meeting all of these goals. In this study, these guidelines were utilized to approximate the “ideal” neophallus, as there are strikingly little data on what transgender patients consider “ideal” in neophallus reconstruction.
Surgical techniques for genital reconstruction can be broadly divided into 3 categories—metoidioplasty, pedicled flap phalloplasty, and free flap phalloplasty.10 Although innumerable procedures within these broad categories exist, 2 of the most commonly performed methods of female-to-male genital reconstruction are metoidioplasty and radial free forearm flap.10,11
Metoidioplasty is the creation of a neophallus from a clitoris that is often hypertrophied by the effects of hormonal therapy.10,12,13,18 Metoidioplasty is advantageous for its capacity to yield “like-with-like” glans reconstruction with tactile and erogenous clitoral tissue, sufficient erectile rigidity without a prosthesis, scarring that is limited to the perineum, and shorter operative times.5,12,13,20,31 The metoidioplasty-constructed neophallus is often shorter and smaller compared with other techniques; as a result, functional limitations can include difficulty with standing micturition and sexual penetration.12–14,32 Though sometimes touted as a single-stage procedure, a series by Hage and van Turnhout17 found that, on average, 2.6 procedures were required before a metoidioplasty reconstruction was considered complete.
The radial free forearm flap may be considered the flap of choice in female-to-male transgender phalloplasty.2,9,11,15,33–35 Multiple flap modifications are available, including construction of an osteofasciocutaneous flap.15,25 Purported advantages of the radial forearm flap, in all of its iterations, include the size and aesthetics of the resultant neophallus and its capacity for reinnervation. Donor-site morbidity, including stigma related to scarring, is regarded as its principle disadvantage.15,32 Despite this, Van Caenegem et al15 reported acceptable aesthetics and functional donor-site outcomes after radial forearm flap phalloplasty. In both metoidioplasty and RFFP, urologic complications related to neourethral fistulae and strictures are the most common.11–14,17,25
The components of an “ideal” neophallus should not be privileged over the preferences and priorities of patients, and technique selection should be personal and individualized on a per-patient basis. All patients should be counseled on the advantages and disadvantages of available techniques, especially on how each technique fares in relation to patient priorities and their desired surgical outcome. In this regard, there is no true “standard” technique for neophallus creation. However, irrespective of the technique, data on surgical outcomes in female-to-male transgender genital reconstruction are sparse, and few studies have sought to compare outcomes across individual techniques. For this reason, the authors reviewed the current literature to determine which of the 2 most commonly utilized techniques—metoidioplasty and RFFP—is more likely to yield the “ideal” neophallus described by Hage and De Graaf.9,10
Compared with patients who underwent radial forearm phalloplasty, metoidioplasty patients were found to be more likely to undergo a single-stage procedure, more likely to retain erogenous sensation, more likely to achieve standing micturition, and less likely to suffer complications. Outcomes for urethral stricture/fistulae, donor-site morbidity, and penetration of partner during intercourse were similar in both groups. Because no metoidioplasty study explicitly reported on tactile sensation, outcomes for tactile sensation could not be compared. Altogether, these comparisons suggest that the metoidioplasty procedure is, overall, more likely than RFFP to yield outcomes close to the “ideal” neophallus described by Hage and De Graaf.9,10 However, the exceedingly low-quality evidence of the existing literature ultimately tempers these conclusions.
The fact that metoidioplasty patients were found to be more likely to undergo a single-stage reconstruction and to retain erogenous sensation is relatively unsurprising. In metoidioplasty, the clitoris is converted to the glans penis, which should supply excellent erogenous sensation.10,12,13,18 By extension, as the metoidioplasty procedure utilizes local, sensate tissue for reconstruction, one would expect a greater number of patients in the metoidioplasty group (as opposed to the RFFP group) to retain high-quality tactile sensation. Similarly, free flap phalloplasty procedures are often times deliberately performed in multiple stages, giving metoidioplasty an edge in the category of single-stage reconstructions. Donor-site complications also trended toward favoring metoidioplasty. Yet, unlike for overall complication rates, donor-site morbidity was not statistically significant.
It is, however, surprising that studies evaluating metoidioplasty reported significantly better aesthetic results compared with radial forearm phalloplasty. This could be taken to indicate that the increased size with RFFP is not necessarily as important to patients as are other aesthetic parameters. On the other hand, however, it should be noted that within the studies we reviewed, reports of aesthetic satisfaction were not well defined. In most cases, the degree of aesthetic satisfaction was determined via a singular “yes” or “no” question posed to the patient. Furthermore, the fact that the percentage of patients who reported successful penetration of partner during intercourse was similar between the metoidioplasty and RFFP groups is likewise surprising because one might expect the comparatively small size of the metoidioplasty-constructed neophallus to limit the capacity for penetration. Ultimately, both parameters—satisfaction with aesthetic result and successful penetration of partner during intercourse—are worthy of future research investigation. To improve our understanding of aesthetic outcome parameters in particular, future studies should strive to incorporate a more nuanced, sensitive instrument to measure all aspects of patient-reported satisfaction with post-op neophallus aesthetics. This study is further limited by publication and patient selection biases inherent in all of the studies reviewed.
It must be noted that no study meeting our inclusion criteria provided data on “every” aspect of the “ideal” neophallus. This, again, highlights the lack of existing evidence on outcomes in female-to-male transgender genital reconstruction. High-quality studies that emphasize patient-reported outcome measures are necessary to advance our understanding of genital reconstruction in this unique patient population. In addition, researchers should develop a standardized system of measurement to facilitate direct comparisons of outcomes across techniques. In the final GRADE scoring, the overall quality of evidence included in this review is considered very low (score 0).36 In the future, substantial research attention should be directed toward evaluating the tenets of the “ideal” neophallus using patient-reported outcome ratings and survey-based data obtained from this patient population. Until then, the parameters of the “ideal” neophallus espoused by Hage and De Graaf9 remain the most established and reproducible means of gauging success in neophallus construction.
To summarize, there is a remarkable paucity of high-quality, comparative data on surgical outcomes in female-to-male transgender genital reconstruction. Significantly, all of the studies included herein received GRADE scores ranging from low to very low. Although the current literature suggests that metoidioplasty is more likely than radial free forearm flap phalloplasty to yield an “ideal” neophallus, any conclusion is severely limited by the exceedingly low quality of available evidence. As the number of transgender patients seeking GCS continues to increase, the need for high-quality research studies that emphasize patient-reported outcome metrics and a universal method of evaluation remains stark.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
Presented at Plastic Surgery The Meeting 2016 in Los Angeles, Calif, September 23–27, 2016.
REFERENCES
- 1.Snaith P. Gender dysphoria. Adv Psychiatr Treat. 1998;4:356–359. [Google Scholar]
- 2.Gooren LJ. Care of transsexual persons. N Engl J Med. 2011;364:2559–2560. doi: 10.1056/NEJMc1104884. [DOI] [PubMed] [Google Scholar]
- 3.Meier SC, Labuski CM. Demographics of the transgender population. In: Baumle AK, editor. In: International Handbook on the Demography of Sexuality. The Netherlands: Springer; 2013. pp. 289–327. [Google Scholar]
- 4.van Kesteren PJ, Gooren LJ, Megens JA. An epidemiological and demographic study of transsexuals in The Netherlands. Arch Sex Behav. 1996;25:589–600. doi: 10.1007/BF02437841. [DOI] [PubMed] [Google Scholar]
- 5.Morrison SD, Perez MG, Nedelman M, et al. Current state of female-to-male gender confirming surgery. Curr Sex Heal Reports. 2015;7:38–48. [Google Scholar]
- 6.Garber M. Spare parts: the surgical construction of gender. In: Abelove H, Barale MA, Halperin DM, editors. In: The Lesbian and Gay Studies Reader. New York: Routledge; 1993. pp. 321–336. [Google Scholar]
- 7.Monstrey SJ, Ceulemans P, Hoebeke P. Sex reassignment surgery in the female-to-male transsexual. Semin Plast Surg. 2011;25:229–244. doi: 10.1055/s-0031-1281493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sutcliffe PA, Dixon S, Akehurst RL, et al. Evaluation of surgical procedures for sex reassignment: a systematic review. J Plast Reconstr Aesthet Surg. 2009;62:294–306. doi: 10.1016/j.bjps.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 9.Hage JJ, De Graaf FH. Addressing the ideal requirements by free flap phalloplasty: some reflections on refinements of technique. Microsurgery. 1993;14:592–598. doi: 10.1002/micr.1920140910. [DOI] [PubMed] [Google Scholar]
- 10.Neligan PC, Warren RJ, Van Beek A. In: Plastic Surgery. 3rd ed. Vol 4. London: Elsevier Saunders; 2013. “Reconstruction of male genital defects.”; pp. 297–325. [Google Scholar]
- 11.Monstrey S, Hoebeke P, Selvaggi G, et al. Penile reconstruction: is the radial forearm flap really the standard technique? Plast Reconstr Surg. 2009;124:510–518. doi: 10.1097/PRS.0b013e3181aeeb06. [DOI] [PubMed] [Google Scholar]
- 12.Stojanovic B, Djordjevic ML. Anatomy of the clitoris and its impact on neophalloplasty (metoidioplasty) in female transgenders. Clin Anat. 2015;28:368–375. doi: 10.1002/ca.22525. [DOI] [PubMed] [Google Scholar]
- 13.Perovic SV, Djordjevic ML. Metoidioplasty: a variant of phalloplasty in female transsexuals. BJU Int. 2003;92:981–985. doi: 10.1111/j.1464-410x.2003.04524.x. [DOI] [PubMed] [Google Scholar]
- 14.Vukadinovic V, Stojanovic B, Majstorovic M, et al. The role of clitoral anatomy in female to male sex reassignment surgery. ScientificWorldJournal. 2014;2014:437378. doi: 10.1155/2014/437378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Caenegem E, Verhaeghe E, Taes Y, et al. Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. J Sex Med. 2013;10:1644–1651. doi: 10.1111/jsm.12121. [DOI] [PubMed] [Google Scholar]
- 16.Takamatsu A, Harashina T. Labial ring flap: a new flap for metaidoioplasty in female-to-male transsexuals. J Plast Reconstr Aesthet Surg. 2009;62:318–325. doi: 10.1016/j.bjps.2008.11.038. [DOI] [PubMed] [Google Scholar]
- 17.Hage JJ, van Turnhout AA. Long-term outcome of metaidoioplasty in 70 female-to-male transsexuals. Ann Plast Surg. 2006;57:312–316. doi: 10.1097/01.sap.0000221625.38212.2e. [DOI] [PubMed] [Google Scholar]
- 18.Hage JJ. Metaidoioplasty: an alternative phalloplasty technique in transsexuals. Plast Reconstr Surg. 1996;97:161–167. doi: 10.1097/00006534-199601000-00026. [DOI] [PubMed] [Google Scholar]
- 19.Cohanzad S. Extensive metoidioplasty as a technique capable of creating a compatible analogue to a natural penis in female transsexuals. Aesthetic Plast Surg. 2016;40:130–138. doi: 10.1007/s00266-015-0607-4. [DOI] [PubMed] [Google Scholar]
- 20.Djordjevic ML, Stanojevic D, Bizic M, et al. Metoidioplasty as a single stage sex reassignment surgery in female transsexuals: Belgrade experience. J Sex Med. 2009;6:1306–1313. doi: 10.1111/j.1743-6109.2008.01065.x. [DOI] [PubMed] [Google Scholar]
- 21.Garcia MM, Christopher NA, De Luca F, et al. Overall satisfaction, sexual function, and the durability of neophallus dimensions following staged female to male genital gender confirming surgery: the Institute of Urology, London U.K. experience. Transl Androl Urol. 2014;3:156–162. doi: 10.3978/j.issn.2223-4683.2014.04.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Song C, Wong M, Wong CH, et al. Modifications of the radial forearm flap phalloplasty for female-to-male gender reassignment. J Reconstr Microsurg. 2011;27:115–120. doi: 10.1055/s-0030-1268210. [DOI] [PubMed] [Google Scholar]
- 23.Schaff J, Papadopulos NA. A new protocol for complete phalloplasty with free sensate and prelaminated osteofasciocutaneous flaps: experience in 37 patients. Microsurgery. 2009;29:413–419. doi: 10.1002/micr.20647. [DOI] [PubMed] [Google Scholar]
- 24.Leriche A, Timsit MO, Morel-Journel N, et al. Long-term outcome of forearm flee-flap phalloplasty in the treatment of transsexualism. BJU Int. 2008;101:1297–1300. doi: 10.1111/j.1464-410X.2007.07362.x. [DOI] [PubMed] [Google Scholar]
- 25.Kim SK, Lee KC, Kwon YS, et al. Phalloplasty using radial forearm osteocutaneous free flaps in female-to-male transsexuals. J Plast Reconstr Aesthet Surg. 2009;62:309–317. doi: 10.1016/j.bjps.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 26.Fang RH, Kao YS, Ma S, et al. Phalloplasty in female-to-male transsexuals using free radial osteocutaneous flap: a series of 22 cases. Br J Plast Surg. 1999;52:217–222. doi: 10.1054/bjps.1998.3027. [DOI] [PubMed] [Google Scholar]
- 27.Fang RH, Lin JT, Ma S. Phalloplasty for female transsexuals with sensate free forearm flap. Microsurgery. 1994;15:349–352. doi: 10.1002/micr.1920150512. [DOI] [PubMed] [Google Scholar]
- 28.Matti BA, Matthews RN, Davies DM. Phalloplasty using the free radial forearm flap. Br J Plast Surg. 1988;41:160–164. doi: 10.1016/0007-1226(88)90044-6. [DOI] [PubMed] [Google Scholar]
- 29.Garaffa G, Christopher NA, Ralph DJ. Total phallic reconstruction in female-to-male transsexuals. Eur Urol. 2010;57:715–722. doi: 10.1016/j.eururo.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 30.The Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011. [Google Scholar]
- 31.Gates G. How Many People Are Lesbian, Gay, Bisexual, and Transgender? Los Angeles, CA: Williams Institute, UCLA School of Law; 2011. [Google Scholar]
- 32.Selvaggi G, Dhejne C, Landen M, et al. The 2011 WPATH standards of care and penile reconstruction in female-to-male transsexual individuals. Adv Urol. 2012;2012:581712. doi: 10.1155/2012/581712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gottlieb LJ, Levine LA. A new design for the radial forearm free-flap phallic construction. Plast Reconstr Surg. 1993;92:276–283. discussion 284. [PubMed] [Google Scholar]
- 34.Gilbert DA, Jordan GH, Devine CJ, Jr, et al. Microsurgical forearm “cricket bat-transformer” phalloplasty. Plast Reconstr Surg. 1992;90:711–716. doi: 10.1097/00006534-199210000-00027. [DOI] [PubMed] [Google Scholar]
- 35.Hage JJ, Winters HA, Van Lieshout J. Fibula free flap phalloplasty: modifications and recommendations. Microsurgery. 1996;17:358–365. doi: 10.1002/(SICI)1098-2752(1996)17:7<358::AID-MICR3>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 36.Atkins D, Best D, Briss PA, et al. GRADE Working Group. “Grading quality of evidence and strength of recommendations.”. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]


