Supplemental Digital Content is available in the text.
Summary:
Migraine headaches are a debilitating disease that causes significant socioeconomic problems. One of the speculated etiologies of the generation of migraines is peripheral nerve irritation at different trigger points. The use of Onabotulinum toxin A (BOTOX), although initially a novel approach, has now been determined to be a valid treatment for chronic headaches and migraines as described in the Phase III Research Evaluating Migraine Prophylaxis Therapy trials that prompted the approval by the Food and Drug Administration for treatment of chronic migraines. The injection paradigm established by this trial was one of a broad injection pattern across large muscle groups that did not always correspond to the anatomical locations of nerves. The senior author developed the Anatomical Regional Targeted BOTOX injection paradigm as an alternative to the current injection model. This technique targets both the anatomical location of nerves known to have causal effects with migraines and the region where the pain localizes, to provide relief across a wide distribution of the peripheral nerve. This article serves as a guide to the Anatomical Regional Targeted injection technique, which, to our knowledge, is the first comprehensive BOTOX injection paradigm described in the literature for treatment of migraines that targets nerves and nerve areas rather than purely muscle groups. This technique is based on the most up-to-date anatomical and scientific studies and large-volume migraine surgery experience.
Migraine headaches are a common and disabling condition that affects roughly 18% of females and 6% of males worldwide.1 Often, these patients fail medical management and must look for more invasive treatment. One of these treatment options has been the injection of Onabotulinum toxin A (BOTOX), with growing evidence and Food and Drug Administration support for its use in the treatment of chronic migraines.2–4 The landmark Phase III Research Evaluating Migraine Prophylaxis Therapy (PREEMPT) trials2,3,5 demonstrated that BOTOX was effective in treating chronic migraines. However, the PREEMPT injection paradigm is less targeted, with injection into a broad muscle group rather than a more customized approach corresponding with the peripheral nerves. It uses both fixed and “follow-the-pain” injection sites, with additional specific “follow-the-pain” sites considered depending on individual symptoms. The “fixed-site” injection technique implemented in the PREEMPT trial did not consider the patient’s tender areas as a guide for an injection that corresponds to the anatomical location of the pain. Even the “follow-the-pain” approach described in the PREEMPT paradigm did not follow correct nerve anatomy as far as its surface topography and depth, nor did it correctly target the adjacent corresponding muscle.6
Based on the increased numbers of anatomical studies demonstrating the locations of muscles and nerves over the recent years in the plastic and reconstructive surgery literature,7–14 we noticed that several of the injection sites advocated in the PREEMPT study were not being done in the most precise topographical locations. Since the initial work by Guyuron on migraine surgery15 demonstrated that nerve compression can be involved in the genesis or worsening of migraines, the first generation of Guyuron-trained plastic surgeons has been injecting BOTOX for diagnostic and therapeutic purposes in anatomical locations that correspond to the topographical location and depth of these nerves.15–20 Ironically, recent research in the neurology literature has shown that BOTOX not only works solely via muscle paralysis but also has a direct action on the nerve itself, preventing the genesis of migraines.21,22 More recently, select neurologists have been injecting BOTOX in a more targeted and/or regional fashion but not in an anatomical fashion (Personal Communication: D. Friedman, 2014, 2015; B. Sorin, Plano Texas, North Texas Institute of Neurology & Headache, 2015; A. Lacy, Fort Worth, Tex., Cooks Children Hospital, 2016).
The quest to provide a better response rate to BOTOX in chronic migraine patients led the senior author (BA) to develop the “Anatomical,” “Regional,” and “Targeted” (ART) BOTOX injection paradigm for the treatment of both episodic and chronic migraine headaches. This technique stems from and expands upon the initial screening technique used preoperatively for surgical decompression,15 and focuses on 3 components: “Anatomical,” based on the surface anatomy of the corresponding nerves, the depth of the nerve, and the corresponding muscle around these nerves; “Regional,” a directed focus on the region of where the pain starts (i.e., occipital, temporal, frontal); and “Targeted,” based on the surface topography of the tender area, which at times may not fully correlate with the described and expected location due to anatomical variations.
The focal injection of BOTOX described by Guyuron, documented in migraine surgery publications, covers the zygomaticotemporal branch of the trigeminal nerve (ZTBTN), greater occipital nerve (GON), and corrugator muscle,16,23 but only for screening purposes. The only other references to this type of injection based on the anatomy and region of the pain is a review article by the senior author (BA) in 201224 and a prospective trial by Guyuron that evaluated the response of forehead migraines to fixed corrugator injections.19,20 Neither of these 2 articles included a comprehensive injection paradigm in all the necessary locations.
The ART injection approach adds focus to the delivery of BOTOX, thereby increasing its efficacy, decreasing complications, and minimizing oversaturation that could lead to BOTOX resistance.25–27 The technique is based off the theory introduced by works from our neurology colleagues that BOTOX works directly on the nerves to decrease migraine pain28,29 rather than an indirect effect by acting on the muscle alone. This technique has taken the initial Guyuron method15 of BOTOX injection and added to it additional injection sites based on newer data regarding migraine etiology and nerve anatomy,12–14,30 and the experience of the migraine BOTOX injection practice of the senior author,20 to form the first comprehensive, nerve-specific treatment for migraines.
Providing convincing evidence that the ART injection technique is better than the current paradigm advocated by the PREEMPT trial31 will require not only a large sample size with a standardized retrospective data review but also a robust prospective multicenter comparison trial similar in scope to the PREEMPT studies. The recent outcome of the senior author’s (BA) retrospective study, and the forthcoming prospective multicenter randomized trials, is beyond the scope of this article and will be presented in the neurology literature by us for comparison with the PREEMPT technique. Thus, the focus of this article is solely to demonstrate the senior author’s ART injection technique for both the plastic surgery and neurology community.
TECHNIQUE
All patients were seen by board-certified neurologists either before or after referral to our service. During the first visit, a diagnosis of chronic migraines (more than 15 headache days/mo or more than 8 migraine days/mo) is established along with documentation of failure of several classes of migraine medications. Based on these criteria, insurance approval for BOTOX injection in the plastic surgery office is almost always approved 2 to 3 weeks after the first visit.
After a detailed headache history is obtained, both the origin of pain and where the pain localizes to are determined, as the latter is often the only location initially mentioned unless the patient is specifically asked. The ZTBTN and supraorbital/supratrochlear nerve (SON/STN) injections are at fixed locations based on nerve and muscle anatomy. Injection variation in these areas based on a more specific “targeted” approach may increase complications of ptosis or diplopia. The variable site injections, based more on a targeted rather than “anatomical” approach, are the auriculotemporal (AT) nerve, GON, lesser occipital nerve (LON), tails of the GON/LON, and third occipital nerve (Table 1). Additionally, the ART technique targets both the primary and secondary trigger areas during the first injection visit because the goal of the injection is also to prevent the emergence of secondary “hidden” triggers32 several weeks later. This differs from both the initial technique used by Guyuron of “chasing the second or third trigger every couple of weeks” to prescreen patients for surgery5 and the “follow-the-pain” paradigm documented in the PREEMPT trials. The comprehensive ART technique is used as a treatment strategy alone and not necessarily a screening tool before surgery. For screening purposes before surgery, the author currently uses constellation of symptoms, nerve blocks, and region-specific ART injection when needed.
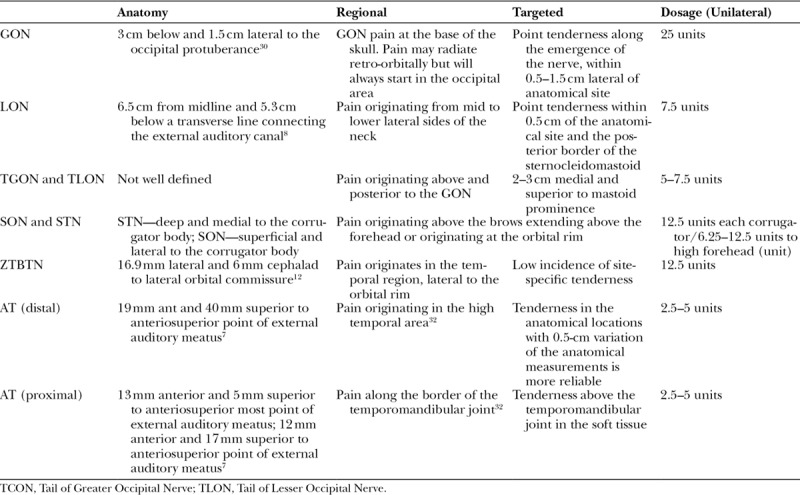
Table 1.
Table Showing Regions, Patient Symptoms, and BOTOX Doses at Each Site and Corresponding Nerve That Is Targeted
FRONTAL SITES
For the SON/STN, the injection is based on the anatomy of the corrugator muscle.14,28 This site is adjusted slightly when the patient is asked to frown at the brow, showcasing its topographical anatomy (Fig. 1). Digital occlusion of the supratrochlear and supraorbital vessels during injection with the nondominant thumb is important as this will decrease the rate of “microhematomas,” which can lead to increased irritation around the nerves and potentially decreased response rate to BOTOX or increase in headaches.33 We do not feel the need for topical anesthetics, but an ice pack is used to cool the skin immediately before injections, as it is important to minimize any irritation caused by needles in migraine patients. The medial injection should be deeper and the lateral injection more superficial, considering the anatomy of the corrugator (Fig. 2). The previous neurology paradigms, adopted from the PREEMPT trials, depicted the medial head of the corrugator in an incorrect higher position.6 In addition, if the patient has tenderness on the inferior end of the orbital rim near the area of STN and SON emergence, BOTOX should not be injected over this area as there is a higher risk for lid ptosis due to proximity to the upper lid muscles, or even vertical diplopia in the event of leakage into the bony globe. Another method of injecting the corrugators is the lateral to medial approach with a single injection using a long needle, as described by Guyuron. However we feel that the point injection of the corrugators concentrates the BOTOX more around the SON and STN. (See video, Supplemental Digital Content 1, which demonstrates complete ART injection technique for frontal injection sites. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A345.)
Fig. 1.
Anatomical location of the corrugator.
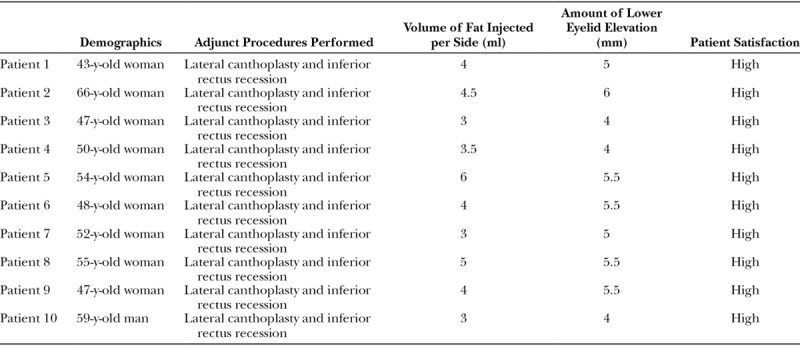
Fig. 2.
Frontal injection sites. Image showing the injection sites as they correlate over the corrugator muscle where the SON and STN transverse. The patient is asked to frown to assist in determining these locations. The paired injection sites superiorly target the high frontalis, and the dose is adjusted here based on the length of the forehead from 12.5 to 25 units.
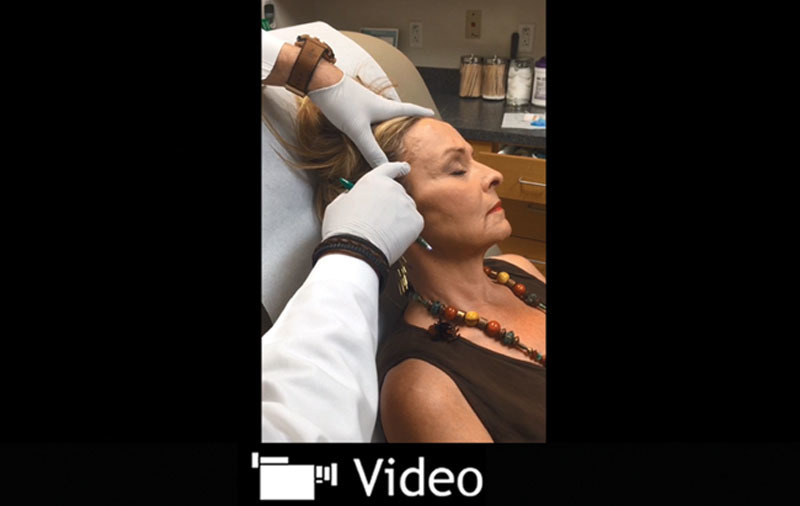
Video Graphic 1.

Frontal injection technique. See video, Supplemental Digital Content 1, which demonstrates complete ART injection technique for frontal injection sites. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A345.
Compared to the PREEMPT model, our injection of the frontalis muscle is higher (only into the upper 1/2), which theoretically should provide for a lower rate of eyebrow ptosis.34 The argument here is that frontalis injection is not targeting any specific compression areas or nerves. However, in our opinion, this is necessary not only to target the most distal aspects of the STN and SON nerves but also to relax the cephalic pull of the frontalis muscle. This would then decrease tension on the proximal STN and SON, which is potentially worsened by the superior pull of the frontalis muscle especially when it is compensating for eyelid ptosis.
TEMPORAL SITES
The ZTBTN is injected in an “anatomical” rather than “targeted” fashion because the tenderness reported by patients in this area is generally more diffuse rather than specific to the anatomical location of the nerve exit point from temporalis fascia. Because the anatomy of the nerve is very consistent in this area, an “anatomical” injection is sufficient. This point, described by Totonchi et al,12 is generally 1.7 mm lateral and 6 mm superior to the lateral canthus. This injection, initially described by Guyuron et al,16 is fanned out around the nerve into the temporalis muscle. We also inject a small amount of BOTOX into the space directly over the nerve exit point from the temporalis fascia to ensure that the superficial portion of the nerve that resides outside the temporalis is adequately exposed to BOTOX (Fig. 3). In our experience, a major drawback of the current neurologist injection paradigm is this nerve not being injected at the correct depth and location.
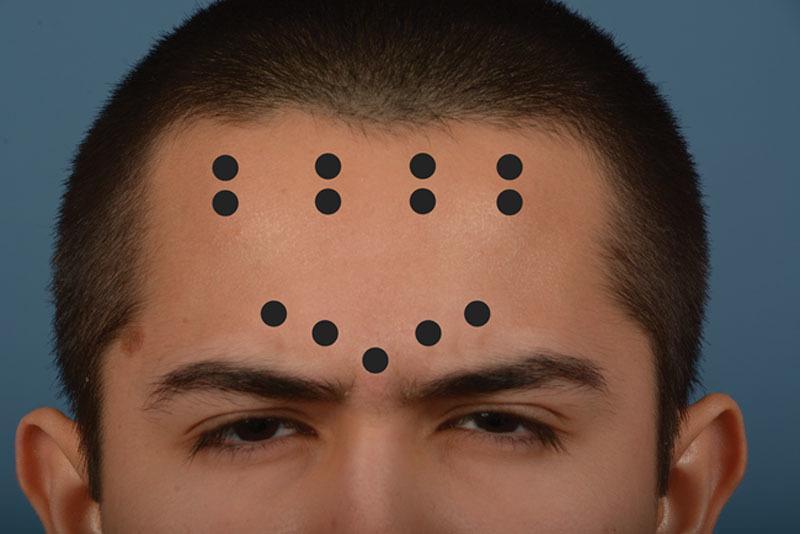
Fig. 3.
Temporal injection sites. Image showing the relationship of the AT (bright yellow), ZTBTN (dark yellow), and the anterior and posterior branches of the superficial temporal artery (red) to the temporal injection sites. The ZTBTN is on a different fascial plane than the AT and superficial temporal artery laterally. 1, ZTBTN injection site, which is commonly 1.5 cm behind the emergence of this nerve from the deep temporal fascia; 2, proximal AT corresponding to the fascial compression bands; 3, distal AT corresponding to the anterior temporal artery crossing the AT nerve.
The AT nerve is injected in a more “targeted” fashion in several areas, based on tenderness throughout the areas of nerve distribution, which may or may not roughly correlate to the known anatomical areas of compression7,9 (Video 2). (See video, Supplemental Digital Content 2, which demonstrates complete ART injection technique for temporal injection sites. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A346.) The main compression point is where the anterior superficial temporal artery crosses the distal branch of the nerve (site 5A).35 The second most common tender area, in our experience, is above constricting fibrous bands on the AT nerve directly superior to the temporomandibular joint (site 5B). Point tenderness here should not be confused with temporomandibular joint pain, which requires a different treatment. While recently described36,37 to confirm site 5A compression by the artery, we do not routinely use Doppler to find this point when we inject BOTOX. Although the use of Doppler can be very helpful for intraoperative localization of the artery and academic exercises, we feel that the added injection time with an often apprehensive migraine patient adds no value to the routine use of Doppler. Both the distal and proximal injection sites are based on maximal point tenderness during the clinical examination rather than a strict anatomical location (Video 3). (See video, Supplemental Digital Content 3, which demonstrates the author’s evolved injection of the AT proximal and distal sites. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A347.)
Video Graphic 2.

Temporal Injection technique. See video, Supplemental Digital Content 2, which demonstrates complete ART injection technique for temporal injection sites. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A346.
Video Graphic 3.
Auriculotemporal injection technique. See video, Supplemental Digital Content 3, which demonstrates the author’s evolved injection of the AT proximal and distal sites. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A347.
As we described in a previous publication,35 these areas can vary slightly and rely on point tenderness to target drug delivery more effectively.
OCCIPITAL SITES
The GON is injected in both an “anatomical” and “targeted” fashion, as the nerve exit point from the semispinalis capitis (a 1.5-cm diameter circle approximately 3 cm below and 1.5 cm lateral to the occipital protuberance) has been well described30 and may correlate to the point of maximum tenderness. However, in our experience, the tender area is usually 0.5 to 1 cm lateral to this exit point, likely because of further irritation and compression by the nuchal line and greater occipital vessels. When injecting this nerve, it is paramount to inject deep enough to pierce the trapezius fascia delivering the drug in the same space that the nerve resides. This injection is significantly deeper than the PREEMPT paradigm occipital injections and another major advantage to the ART technique. Instead of a 30-gauge needle, a longer and sturdier 27-gauge needle is used, which makes it easier to pierce the trapezius fascia. The LON is similarly injected in both an “anatomical” and “targeted” fashion, with injections modified to conform to the point of maximal tenderness commonly within 0.5 cm of the described anatomical landmark posterior to the sternocleidomastoid.11 Additionally, there can be point tenderness in the distal “tail of the GON or LON” as they course over the mastoid and the superior/medial areas of the ear, where they can intertwine with the terminal branches of the occipital artery. (We have not had any issues injecting close to the vessels in the occipital area. In the case of a small amount of bleeding, immediate direct pressure is used for several minutes. This is in contrast to the corrugator area, where aggressive direct pressure should be avoided to prevent ptosis.) This injection is done in more of a “targeted” fashion, chasing the tender tail of the GON and LON. The third occipital nerve is injected far less commonly, also in an “anatomical”8 and “targeted” fashion, depending on the severity of headache pain localizing from this area (Fig. 4). Recent studies show that the third occipital nerve is much less commonly involved in the pathogenesis of migraines.38 Unlike the PREEMPT paradigm, there is no injection into the trapezius muscle lower on the neck where no real distinct nerve sites are located (Video 4). (See video, Supplemental Digital Content 4, which demonstrates the complete ART injection technique for occipital injection sites. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A349.)
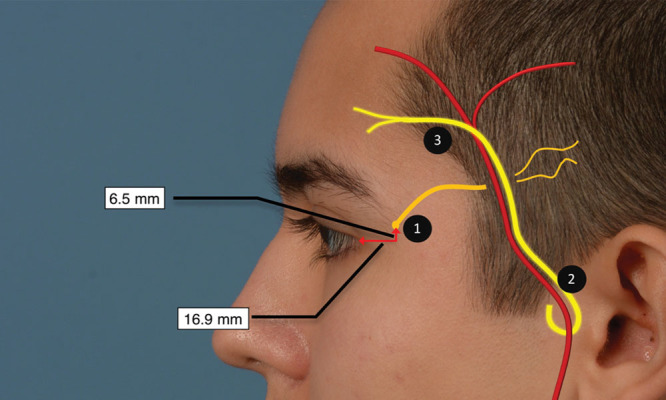
Fig. 4.
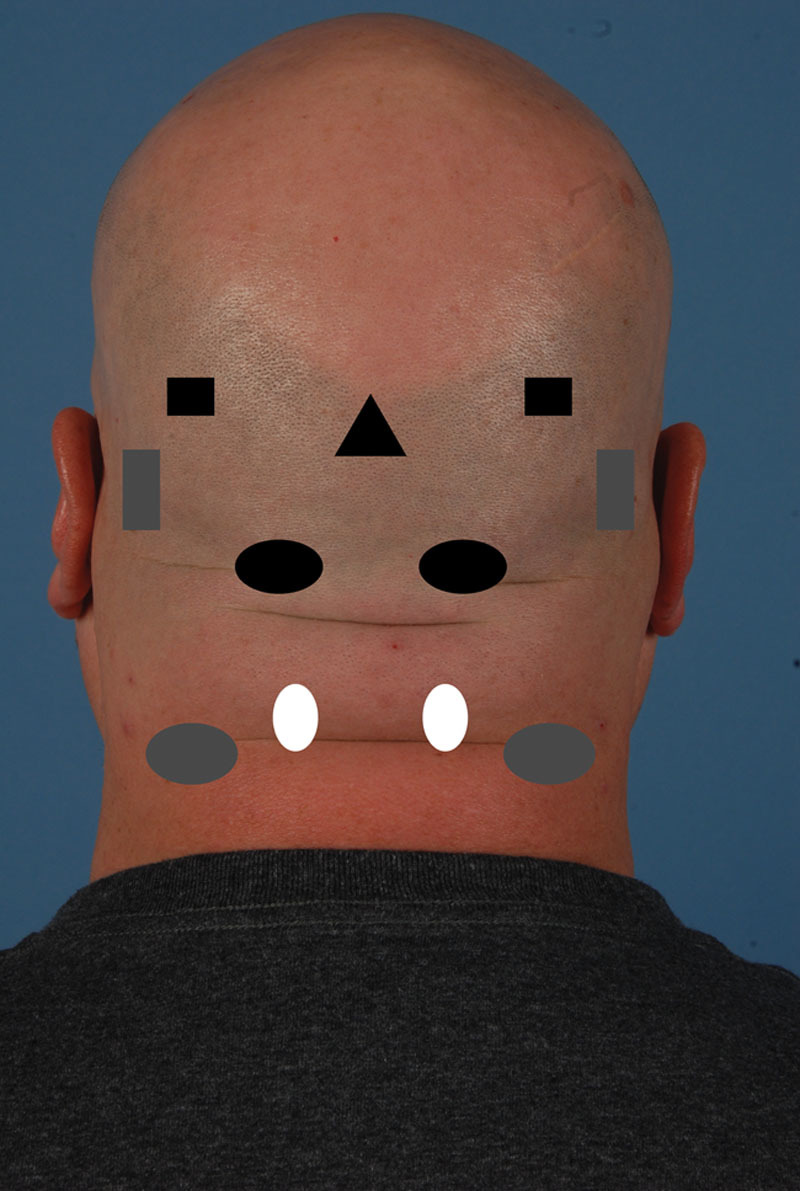
Occipital injection sites. Image showing the occipital injection sites. Occipital protuberance (triangle), GON (black oval), tail of GON (black square), LON (gray oval), tail of LON (gray square), third occipital nerve (white circle). The third occipital nerve site is rarely injected as the patient usually does not have tenderness over this site.
Video Graphic 4.

Occipital injection technique. See video, Supplemental Digital Content 4, which demonstrates the complete ART injection technique for occipital injection sites. This video is available in the “Related Videos” section of the Full-Text article on PRSGlobalOpen.com or available at http://links.lww.com/PRSGO/A349.
A majority of our patients receive the standard PREEMPT dose of 155 units of BOTOX, but in a more efficient way. In the select patients who only have a single trigger point or single “region” involved, we will use less than the standard dose and only target what is needed. However, we still adhere to the site-specific injection techniques listed above and do not simply “follow the pain” unless it corresponds with the above ART injection paradigm.
CONCLUSIONS
The ART BOTOX injection technique is the first, to our knowledge, that describes a comprehensive migraine treatment strategy that targets BOTOX injections around the nerve and the various nerve regions, rather than an imprecise dispersed fashion throughout multiple muscle groups.6,31 The ART injection technique is less of a “shotgun” approach than in the PREEMPT trials,6 yet it is more comprehensive than the targeted approach initially described by Guyuron for screening purposes. The ART injection paradigm is not a screening tool, and both the surgeon and the patient should understand that the goal of this technique is a comprehensive treatment of the migraines with BOTOX.
By injecting closer to the nerves to target known anatomical sites of nerve irritation and focusing on regional sites of pain, the BOTOX injector can provide migraine patients with more pain relief, decreased complications from overinjection, potentially less BOTOX tolerance, overall increased patient satisfaction, and decreased attrition due to complications and the potentially poorer response of diffuse injections. This method of injection may even prove useful in episodic migraines, which is currently thought to not be as responsive to the PREEMPT paradigm. Future prospective trials comparing this technique with the PREEMPT technique will definitively determine whether the senior authors’ paradigm is validated for long-term use. Our current retrospective data, which is being considered for publication, may serve as a pilot guide to any future large prospective trials.
PATIENT CONSENT
Patients provided written consent for the use of their images.
Supplementary Material
Footnotes
Presented at the 3rd Annual International Congress of Interventional Pain Medicine & 5th Annual Congress of ISRAPM, September 22–October 7, 2012, Tehran, Iran; 37th Annual State Conference of Texas Association of Perianesthesia Nurses (TAPAN), October 11, 2013, Garland, Tex; 18th Annual Dallas Cosmetic Symposium Westin Galleria, March 5, 2015, Dallas, Tex.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid by PRS Global Open at the Discretion of the Editor-in-Chief.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.Lipton RB, Bigal ME, Diamond M, et al. AMPP Advisory Group. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343–349. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 2.Aurora SK, Dodick DW, Turkel CC, et al. PREEMPT 1 Chronic Migraine Study Group. OnabotulinumtoxinA for treatment of chronic migraine: results from the double-blind, randomized, placebo-controlled phase of the PREEMPT 1 trial. Cephalalgia. 2010;30:793–803. doi: 10.1177/0333102410364676. [DOI] [PubMed] [Google Scholar]
- 3.Dodick DW, Turkel CC, DeGryse RE, et al. PREEMPT Chronic Migraine Study Group. OnabotulinumtoxinA for treatment of chronic migraine: pooled results from the double-blind, randomized, placebo-controlled phases of the PREEMPT clinical program. Headache. 2010;50:921–936. doi: 10.1111/j.1526-4610.2010.01678.x. [DOI] [PubMed] [Google Scholar]
- 4.Lipton RB, Varon SF, Grosberg B, et al. OnabotulinumtoxinA improves quality of life and reduces impact of chronic migraine. Neurology. 2011;77:1465–1472. doi: 10.1212/WNL.0b013e318232ab65. [DOI] [PubMed] [Google Scholar]
- 5.Aurora SK, Dodick DW, Diener HC, et al. OnabotulinumtoxinA for chronic migraine: efficacy, safety, and tolerability in patients who received all five treatment cycles in the PREEMPT clinical program. Acta Neurol Scand. 2014;129:61–70. doi: 10.1111/ane.12171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blumenfeld A, Silberstein SD, Dodick DW, et al. Method of injection of onabotulinumtoxinA for chronic migraine: a safe, well-tolerated, and effective treatment paradigm based on the PREEMPT clinical program. Headache. 2010;50:1406–1418. doi: 10.1111/j.1526-4610.2010.01766.x. [DOI] [PubMed] [Google Scholar]
- 7.Chim H, Okada HC, Brown MS, et al. The auriculotemporal nerve in etiology of migraine headaches: compression points and anatomical variations. Plast Reconstr Surg. 2012;130:336–341. doi: 10.1097/PRS.0b013e3182589dd5. [DOI] [PubMed] [Google Scholar]
- 8.Dash KS, Janis JE, Guyuron B. The lesser and third occipital nerves and migraine headaches. Plast Reconstr Surg. 2005;115:1752–1758. doi: 10.1097/01.prs.0000161679.26890.ee. discussion 1759. [DOI] [PubMed] [Google Scholar]
- 9.Janis JE, Hatef DA, Ducic I, et al. Anatomy of the auriculotemporal nerve: variations in its relationship to the superficial temporal artery and implications for the treatment of migraine headaches. Plast Reconstr Surg. 2010;125:1422–1428. doi: 10.1097/PRS.0b013e3181d4fb05. [DOI] [PubMed] [Google Scholar]
- 10.Janis JE, Hatef DA, Thakar H, et al. The zygomaticotemporal branch of the trigeminal nerve: Part II. Anatomical variations. Plast Reconstr Surg. 2010;126:435–442. doi: 10.1097/PRS.0b013e3181e094d7. [DOI] [PubMed] [Google Scholar]
- 11.Lee M, Brown M, Chepla K, et al. An anatomical study of the lesser occipital nerve and its potential compression points: implications for surgical treatment of migraine headaches. Plast Reconstr Surg. 2013;132:1551–1556. doi: 10.1097/PRS.0b013e3182a80721. [DOI] [PubMed] [Google Scholar]
- 12.Totonchi A, Pashmini N, Guyuron B. The zygomaticotemporal branch of the trigeminal nerve: an anatomical study. Plast Reconstr Surg. 2005;115:273–277. [PubMed] [Google Scholar]
- 13.Webster RC, Gaunt JM, Hamdan US, et al. Supraorbital and supratrochlear notches and foramina: anatomical variations and surgical relevance. Laryngoscope. 1986;96:311–315. doi: 10.1288/00005537-198603000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Guyuron B, Varghai A, Michelow BJ, et al. Corrugator supercilii muscle resection and migraine headaches. Plast Reconstr Surg. 2000;106:429–434. doi: 10.1097/00006534-200008000-00030. discussion 435–437. [DOI] [PubMed] [Google Scholar]
- 15.Guyuron B. Surgical Management of Migraine Headaches. St. Louis, MO: Mosby; 2000. [Google Scholar]
- 16.Guyuron B, Tucker T, Davis J. Surgical treatment of migraine headaches. Plast Reconstr Surg. 2002;109:2183–2189. doi: 10.1097/00006534-200206000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Amirlak B. Use of targeted BOTOX and surgery in chronic migraines.. In: 3rd Annual International Congress of Interventional Pain Medicine; Tehran, Iran. 2010. [Google Scholar]
- 18.Amirlak B. Treatment of migraine headaches with Botox and surgery.. In: Annual State Conference of Texas Association of Perianesthesias Nurses (TAPAN); October 11, 2013; Grapevine, Texas. [Google Scholar]
- 19.Behmand RA, Tucker T, Guyuron B. Single-site botulinum toxin type A injection for elimination of migraine trigger points. Headache. 2003;43:1085–1089. doi: 10.1046/j.1526-4610.2003.03210.x. [DOI] [PubMed] [Google Scholar]
- 20.Becker D, Amirlak B. Beyond beauty: onobotulinumtoxin A (BOTOX®) and the management of migraine headaches. Anesth Pain Med. 2012;2:5–11. doi: 10.5812/aapm.6286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramachandran R, Yaksh TL. Therapeutic use of botulinum toxin in migraine: mechanisms of action. Br J Pharmacol. 2014;171:4177–4192. doi: 10.1111/bph.12763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burstein R, Zhang X, Levy D, et al. Selective inhibition of meningeal nociceptors by botulinum neurotoxin type A: therapeutic implications for migraine and other pains. Cephalalgia. 2014;34:853–869. doi: 10.1177/0333102414527648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guyuron B, Kriegler JS, Davis J, et al. Comprehensive surgical treatment of migraine headaches. Plast Reconstr Surg. 2005;115:1–9. [PubMed] [Google Scholar]
- 24.Amirlak B. Discussion: outcome comparison of endoscopic and transpalpebral decompression for treatment of frontal migraine headaches. Plast Reconstr Surg. 2012;129:1120–1122. doi: 10.1097/PRS.0b013e3182519dd9. [DOI] [PubMed] [Google Scholar]
- 25.Sankhla C, Jankovic J, Duane D. Variability of the immunologic and clinical response in dystonic patients immunoresistant to botulinum toxin injections. Mov Disord. 1998;13:150–154. doi: 10.1002/mds.870130128. [DOI] [PubMed] [Google Scholar]
- 26.Kessler KR, Skutta M, Benecke R. Long-term treatment of cervical dystonia with botulinum toxin A: efficacy, safety, and antibody frequency. German Dystonia Study Group. J Neurol. 1999;246:265–274. doi: 10.1007/s004150050345. [DOI] [PubMed] [Google Scholar]
- 27.Naumann M, Carruthers A, Carruthers J, et al. Meta-analysis of neutralizing antibody conversion with onabotulinumtoxinA (BOTOX®) across multiple indications. Mov Disord. 2010;25:2211–2218. doi: 10.1002/mds.23254. [DOI] [PubMed] [Google Scholar]
- 28.Dirnberger F, Becker K. Surgical treatment of migraine headaches by corrugator muscle resection. Plast Reconstr Surg. 2004;114:652–657. doi: 10.1097/01.prs.0000131906.27281.17. discussion 658. [DOI] [PubMed] [Google Scholar]
- 29.Barbanti P, Egeo G, Fofi L, et al. Rationale for use of onabotulinum toxin A (BOTOX) in chronic migraine. Neurol Sci. 2015;36(Suppl 1):29–32. doi: 10.1007/s10072-015-2195-0. [DOI] [PubMed] [Google Scholar]
- 30.Mosser SW, Guyuron B, Janis JE, et al. The anatomy of the greater occipital nerve: implications for the etiology of migraine headaches. Plast Reconstr Surg. 2004;113:693–697. doi: 10.1097/01.PRS.0000101502.22727.5D. [DOI] [PubMed] [Google Scholar]
- 31.Liberini P, Pari E, Gazzina S, et al. Technique of injection of onabotulinumtoxin A for chronic migraine: the PREEMPT injection paradigm. Neurol Sci. 2014;35(Suppl 1):41–43. doi: 10.1007/s10072-014-1740-6. [DOI] [PubMed] [Google Scholar]
- 32.Punjabi A, Brown M, Guyuron B. Emergence of secondary trigger sites after primary migraine surgery. Plast Reconstr Surg. 2016;137:712e–716e. doi: 10.1097/PRS.0000000000002011. [DOI] [PubMed] [Google Scholar]
- 33.Larson K, Lee M, Davis J, et al. Factors contributing to migraine headache surgery failure and success. Plast Reconstr Surg. 2011;128:1069–1075. doi: 10.1097/PRS.0b013e31822b61a1. [DOI] [PubMed] [Google Scholar]
- 34.Monheit G. Neurotoxins: current concepts in cosmetic use on the face and neck–upper face (Glabella, Forehead, and Crow’s Feet). Plast Reconstr Surg. 2015;136:72S–75S. doi: 10.1097/PRS.0000000000001771. [DOI] [PubMed] [Google Scholar]
- 35.Sanniec K, Borsting E, Amirlak B. Decompression-avulsion of the auriculotemporal nerve for treatment of migraines and chronic headaches. Plast Reconstr Surg Glob Open. 2016;4:e678. doi: 10.1097/GOX.0000000000000663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guyuron B, Nahabet E, Khansa I, et al. The current means for detection of migraine headache trigger sites. Plast Reconstr Surg. 2015;136:860–867. doi: 10.1097/PRS.0000000000001572. [DOI] [PubMed] [Google Scholar]
- 37.Guyuron B, Riazi H, Long T, et al. Use of a Doppler signal to confirm migraine headache trigger sites. Plast Reconstr Surg. 2015;135:1109–1112. doi: 10.1097/PRS.0000000000001102. [DOI] [PubMed] [Google Scholar]
- 38.Lee M, Lineberry K, Reed D, et al. The role of the third occipital nerve in surgical treatment of occipital migraine headaches. J Plast Reconstr Aesthet Surg. 2013;66:1335–1339. doi: 10.1016/j.bjps.2013.05.023. [DOI] [PubMed] [Google Scholar]


