Abstract
Abiraterone suppresses intracrine androgen synthesis via inhibition of CYP17A1. However, clinical evidence suggests that androgen synthesis is not fully inhibited by abiraterone and the sustained androgen production may lead to disease relapse. In the present study, we identified AKR1C3, an important enzyme in the steroidogenesis pathway, as a critical mechanism driving resistance to abiraterone through increasing intracrine androgen synthesis and enhancing androgen signaling. We found that overexpression of AKR1C3 confers resistance to abiraterone while downregulation of AKR1C3 re-sensitizes resistant cells to abiraterone treatment. In abiraterone resistant prostate cancer cells, AKR1C3 is overexpressed and the levels of intracrine androgens are elevated. In addition, AKR1C3 activation increases intracrine androgen synthesis and enhances androgen receptor (AR) signaling via activating AR transcriptional activity. Treatment of abiraterone resistant cells with indomethacin, an AKR1C3 inhibitor, overcomes resistance and enhances abiraterone therapy both in vitro and in vivo by reducing the levels of intracrine androgens and diminishing AR transcriptional activity. These results demonstrate that AKR1C3 activation is a critical mechanism of resistance to abiraterone through increasing intracrine androgen synthesis and enhancing androgen signaling. Furthermore, this study provides a preclinical proof-of-principle for clinical trials investigating the combination of targeting AKR1C3 using indomethacin with abiraterone for advanced prostate cancer.
Keywords: prostate cancer, AKR1C3, abiraterone, indomethacin, intracrine androgens
Introduction
For patients with late-stage prostate cancer, the current standards of care are chemotherapeutic drugs such as docetaxel and cabazitaxel (1, 2), and/or next-generation anti-androgens such as enzalutamide and abiraterone (3, 4). Abiraterone inhibits CYP17A1 (5), resulting in the reduction of testosterone levels in advanced prostate cancer patients. While initially effective, most patients receiving abiraterone will progress in their disease by 15 months of treatment (4). The elucidation of adaptive resistance mechanisms and targeting against it to overcome the resistance are urgently needed.
Abiraterone resistance has been linked to re-activation of androgen receptor signaling in prostate cancer cells. This may be partially due to the presence of AR splice variants and mutation of the AR. Clinically, detection of AR-V7 in prostate cancer patients may indicate abiraterone resistance (6). Furthermore, the progesterone-activated T878A AR mutant is associated with resistance to abiraterone (7) and circulating tumor DNA extracted from plasma samples revealed that the L702H mutation in the ligand-binding domain of AR, which results in activation of the AR by glucocorticoids, might also induce abiraterone resistance (8). In addition to AR modification, increased expression of steroidogenic enzymes is another likely contributor to both prostate cancer progression and abiraterone resistance by increasing androgen levels and inducing AR activation. Mostaghel et al. detected a 1.3 – 4.5 fold increase in enzymes involved in steroidogenesis in abiraterone treated LuCaP cell lines, including CYP17A1, AKR1C3, HSD17B3, and SDR5A2 (9). Additionally, Chang et al. observed the 1245C mutation in HSD3B1 in abiraterone-resistant xenograft models leading to aberrant androgen production (10). AKR1C3 in particular is an important enzyme in the steroidogenesis pathway. Its activation contributes to CRPC drug resistance in patients treated with both abiraterone and enzalutamide and it has been suggested as a biomarker for assessing prostate cancer progression (11, 12). AKR1C3 facilitates the conversion of the weak androgens androstenedione (A′ dione) and 5α-androstanedione (5α-dione) to the more active androgens, testosterone and DHT, respectively and cannot be inhibited by abiraterone (13, 14). AKR1C3 is the major AKR1C isozyme in the human prostate (15) and elevated expression of this enzyme is associated with prostate cancer progression and aggressiveness (16, 17). AKR1C3 has also been identified as an AR co-activator (18). AKR1C3 is not detectable in normal prostatic epithelium, however it is highly elevated in metastasized prostate cancer (16, 17). In two independent prostate datasets in the Oncomine data base, AKR1C3 expression was correlated with Gleason score and recurrence status in prostate cancer patients (12).
Indomethacin (Indocin) is a non-steroidal anti-inflammatory drug that is commonly prescribed to reduce fever, pain, stiffness, and/or swelling due to a myriad of different causes. In addition to its function as a nonselective inhibitor of cyclooxygenase (COX) 1 and 2, studies have demonstrated that Indocin can inhibit AKR1C3 activity (19, 20). Other studies have shown that Indocin can increase the sensitivity of cancer cells to chemotherapeutics. Specifically, it was observed to increase the response of colon cancer cells to cisplatin and the response of melanoma cells to TRAIL-induced apoptosis (21, 22). Overexpression of AKR1C3 in prostate cancer cells confers resistance to enzalutamide and combination of Indocin and enzalutamide results in inhibition of enzalutamide-resistant tumor growth in xenografts (12). These data suggest that AKR1C3 activity is integral to the development of enzalutamide resistance in prostate cancer and that co-treatment with Indocin and enzalutamide is a viable method to overcome enzalutamide resistance. To date, however, the effects of Indocin on abiraterone resistance remain unknown.
In the present study, we utilized drug resistant prostate cancer cell lines to investigate the effects of AKR1C3 and Indocin on abiraterone resistance. We found that overexpression of AKR1C3 induces abiraterone resistance and that higher expression levels of AKR1C3 in drug resistant cells results in modification of androgen receptor (AR) signaling and regulated AR transcriptional activity. Chronic abiraterone acetate treatment in prostate cancer cells induced high levels of AKR1C3 and AR. Knockdown of AKR1C3 expression re-sensitized abiraterone resistant prostate cancer cells to abiraterone treatment. Furthermore, treatment of resistant cells with Indocin enhances abiraterone response both in vitro and in vivo. Data from this study further the understanding of abiraterone resistance in prostate cancer and provide the groundwork for the development of meaningful treatment strategies by targeting AKR1C3 using Indocin in combination with abiraterone in advanced prostate cancer patients.
Materials and Methods
Reagents and Cell Culture
LNCaP, VCaP and CWR22Rv1 cells were obtained from the American Type Culture Collection (ATCC, Manassas, VA). All experiments with cell lines were performed within 6 months of receipt from ATCC or resuscitation after cryopreservation. ATCC uses Short Tandem Repeat (STR) profiling for testing and authentication of cell lines. C4-2B cells were kindly provided and authenticated by Dr. Leland Chung, Cedars-Sinai Medical Center, Los Angeles, CA. VCaP cells were maintained in DMEM supplemented with 10% fetal bovine serum (FBS), 100 units/ml penicillin and 0.1 mg/ml streptomycin. Other cell lines were maintained in RPMI 1640 supplemented with 10% FBS, 100 units/ml penicillin and 0.1 mg/ml streptomycin. LNCaP-neo and LNCaP-AKR1C3 cells were generated by stable transfection of LNCaP cells with either empty vector pcDNA3.1 or pcDNA3.1 encoding AKR1C3 and were maintained in RPMI1640 medium containing 300 μg/mL G418. Cells resistant to enzalutamide were referred to as C4-2B MDVR (C4-2B enzalutamide resistant) as described before (12, 23). C4-2B cells were incubated with increasing concentrations of abiraterone acetate (1 μM ~ 20 μM) in RPMI1640 plus 10% FBS and stored for further analysis. The resistant cells were isolated and referred to as C4-2B AbiR (C4-2B abiraterone resistant) (24). Parental C4-2B cells were passaged alongside the abiraterone acetate treated cells as an appropriate control. C4-2B AbiR cells were maintained in 10 μM abiraterone acetate containing medium. All cells were maintained at 37°C in a humidified incubator with 5% carbon dioxide. Indocin was purchased from Sigma, Abiraterone was purchased from LKT Laboratories, Inc., Abiraterone acetate was purchased from AK Scientific Inc. All drugs were dissolved in DMSO and stored at −20°C.
Cell transfection and luciferase assay
AKR1C3 shRNA (TRCN0000026561 and TRCN0000025694) were purchased from Sigma. For luciferase assays, C4-2B MDVR cells (1×105 cells per well of 12-well plate) were transfected with 0.5 μg of pGL3-PSA6.0-Luc reporter plasmid or the control plasmid and subsequently treated with 20 μM Indocin. The luciferase activity was determined 48 hr after transfection using a dual-luciferase reporter assay system (Promega) as described previously (23).
Sample preparation and steroid analysis
The steroid extraction and analysis has been described previously (12, 25). Briefly, 100 million LNCaP-neo and LNCaP-AKR1C3 cells were cultured in serum and phenol red free RPMI1640 medium for 5 days. Fifty million C4-2B MDVR cells were cultured in serum and phenol red free RPMI1640 medium for 5 days and then treated with 20 μM Indocin for another 3 days. Subsequently, cells were suspended in 4 mL of a 1:1 water/methanol mixture. The suspension was homogenized, and the resulting homogenate was cooled on ice. The precipitated material was removed by centrifuging at high speed for 5 min, and the supernatant was removed and evaporated in a SpeedVaac (Labconco Inc.) followed by lyophilizer (Labconco Inc.). The residue was suspended in 150 μL of CH3OH/H2O (1:1), filtered through a 0.2 μm ultracentrifuge filter (Millipore inc.) and subjected to UPLC/MS-MS analysis. Samples were run in duplicate during UPLC-MS/MS analysis. Samples were placed in an Acquity sample manager which was cooled to 8 °C to preserve the analytes. Pure standards were used to optimize the UPLC-MS/MS conditions prior to sample analysis. The standard mixture was run before the first sample to prevent errors due to matrix effect and day-to-day instrument variations. In addition, immediately after the initial standard and before the first sample, two spiked samples were run to calibrate for the drift in the retention time of all analytes due to the matrix effect. After standard and spiked sample runs, a blank was injected to wash the injector and remove carry over effect.
Chromatin immunoprecipitation assay
C4-2B MDVR cells were transiently transfected with control shRNA or AKR1C3 shRNA (# 561 and # 694) for 3 days or treated with DMSO or Indocin for 2 days. DNA-AR protein complexes were cross-linked inside the cells by the addition of 1% formaldehyde. Whole-cell extracts were prepared by sonication, and an aliquot of the cross-linked DNA-protein complexes was immunoprecipitated by incubation with the AR-specific antibody (AR-441; Santa Cruz Biotechnology) overnight at 4°C with rotation. Chromatin-antibody complexes were isolated from solution by incubation with protein A/G agarose beads for 1 hour at 4°C with rotation. The bound DNA-protein complexes were washed and eluted from beads with elution buffer (1% SDS and 0.1 mol/L NaHCO3), crosslinking was reversed, and DNA was extracted. The resulting chromatin preparations were analyzed by PCR using primers spanning AREs of the PSA promoter as described previously (26). Isotype-matched IgG was used as control.
Western blot analysis
Cellular protein extracts were resolved on SDS–PAGE and proteins were transferred to nitrocellulose membranes. After blocking for 1 hour at room temperature in 5% milk in PBS/0.1% Tween-20, membranes were incubated overnight at 4°C with the indicated primary antibodies [AR (441,SC-7305, Santa Cruz Biotechnology, Santa Cruz, CA); AR (N20, SC-816, Santa Cruz Biotechnology, Santa Cruz, CA) AKR1C3 (A6229, Sigma); HSD3B (SC-28206, Santa Cruz Biotechnology, Santa Cruz, CA); Tubulin (T5168, Sigma-Aldrich, St. Louis, MO)]. Tubulin was used as loading control. Following secondary antibody incubation, immunoreactive proteins were visualized with an enhanced chemiluminescence detection system (Millipore, Billerica, MA).
Cell growth assay
C4-2B AbiR, C4-2B MDVR, CWR22Rv1 cells were seeded on 12-well plates at a density of 0.5×105 cells/well in RPMI 1640 media containing 10% FBS and transiently transfected with AKR1C3 shRNA or control shRNA and then treated with 10 μM abiraterone. Total cell numbers were counted after 3 days and the cell survival rate was normalized to the DMSO treatment for each group. LNCap-neo and LNCaP-AKR1C3 cells were treated with different concentrations of abiraterone for 48 hours. C4-2B parental and C4-2B AbiR cells were treated with different concentrations of abiraterone acetate and total cell numbers were counted on day 3. CWR22Rv1 cells were seeded on 12-well plates at a density of 0.5×105 cells/well in RPMI 1640 media containing 10% FBS and treated with DMSO, 20 μM Indocin, 10 μM abiraterone or their combination for 3 days. Total cell numbers were counted and the cell survival rate (%) was calculated. Cell survival rate (%) = (Treatment group cell number/Control group cell number) ×100.
Clonogenic Assay
C4-2 parental or C4-2B AbiR cells were treated with DMSO, 2.5 μM, 5 μM or 10 μM abiraterone acetate in media containing 10% FBS. Cells were plated at equal density (2000 cells/dish) in 100 mm dishes for 14 days. CWR22Rv1 cells were treated with 20 μM indocin with or without 10 μM abiraterone, and were plated at equal density (1500 cells/dish) in 100 mm dishes for 14 days. The medium was changed every 3 days. Colonies were rinsed with PBS before staining with 0.5% crystal violet/4% formaldehyde for 30 min and the numbers of colonies were counted.
Real-Time quantitative RT-PCR
Total RNAs were extracted using TriZOL reagent (Invitrogen). cDNAs were prepared after digestion with RNase-free RQ1 DNase (Promega). The cDNAs were subjected to real-time reverse transcription-PCR (RT-PCR) using Sso Fast Eva Green Supermix (Bio-Rad) according to the manufacturer’s instructions and as described previously (27). Each reaction was normalized by co-amplification of actin. Triplicates of samples were run on default settings of Bio-Rad CFX-96 real-time cycler. Primers used for Real-time PCR are: AKR1C3, 5′-gagaagtaaagctttggaggtcaca-3′(forward) and 5′-caacctgctcctcattattgtataaatga-3′(reverse); HSD3B, 5′-cgggcccaactcctacaag-3′ (forward) and 5′-ttttccagaggctcttcttcgt-3′(reverse); PSA, 5′-gccctgcccgaaagg-3′(forward) and 5′-gatccacttccggtaatgca-3′ (reverse); AR, 5′-cctggcttccgcaacttacac-3′(forward) and 5′-ggacttgtgcatgcggtactca-3′(reverse); NKX3.1, 5′-ccgagacgctggcagagacc-3′(forward) and 5′-gcttaggggtttggggaag-3′(reverse); and Actin, 5′-agaactggcccttcttggagg-3′(forward) and 5′-gtttttatgttcctctatggg-3′ (reverse).
Measurement of PSA
C4-2B MDVR cells were transiently transfected with AKR1C3 shRNA or control shRNA for 3 days, LNCaP-neo and LNCaP-AKR1C3 cells were cultured in CS-FBS conditions for 3 days and PSA level was measured using PSA ELISA Kit (KA0208, Abnova, Inc., Walnut, CA) according to the manufacturer’s instructions as described previously (28).
In vivo tumorigenesis assay
CWR22Rv1 cells (4×106) were mixed with matrigel (1:1) and injected subcutaneously into the flanks of 6–7 week male SCID mice. Tumor-bearing mice (tumor volume around 50–100 mm3) were randomized into four groups (5 mice in each group) and treated as follows: (1) vehicle control (5% Tween 80 and 5% ethanol in PBS, i.p.), (2) abiraterone acetate (200 mg/kg, p.o.), (3) indocin (3 mg/kg, i.p.), (4) abiraterone acetate (200 mg/kg, p.o.) + indocin (3 mg/kg, i.p.). Tumors were measured using calipers twice a week and tumor volumes were calculated using length × width2/2. Tumor tissues were harvested after 3 weeks of treatment.
Immunohistochemistry
Tumors were fixed by formalin. Paraffin embedded tissue blocks were dewaxed, rehydrated, and blocked for endogenous peroxidase activity. Antigen retrieval was performed in sodium citrate buffer (0.01 mol/L, pH 6.0) in a microwave oven at 1,000 W for 3 min and then at 100 W for 20 min. Nonspecific antibody binding was blocked by incubating with 10% fetal bovine serum in PBS for 30 min at room temperature. Slides were then incubated with anti-Ki-67 (at 1:500; NeoMarker) at 4°C overnight. Slides were then washed and incubated with biotin-conjugated secondary antibodies for 30 min, followed by incubation with avidin DH-biotinylated horseradish peroxidase complex for 30 min (Vectastain ABC Elite Kit, Vector Laboratories). The sections were developed with the diaminobenzidine substrate kit (Vector Laboratories) and counterstained with hematoxylin. Nuclear staining of cells was scored and counted in 5 different vision fields. Images were taken with an Olympus BX51 microscope equipped with DP72 camera.
Statistical Analysis
All data are presented as means ± standard deviation of the mean (SD). Statistical analyses were performed with Microsoft Excel analysis tools. Differences between individual groups were analyzed by one-way analysis of variance (ANOVA) followed by the Scheffé procedure for comparison of means. P < 0.05 was considered statistically significant.
Results
Overexpression of AKR1C3 confers resistance to abiraterone
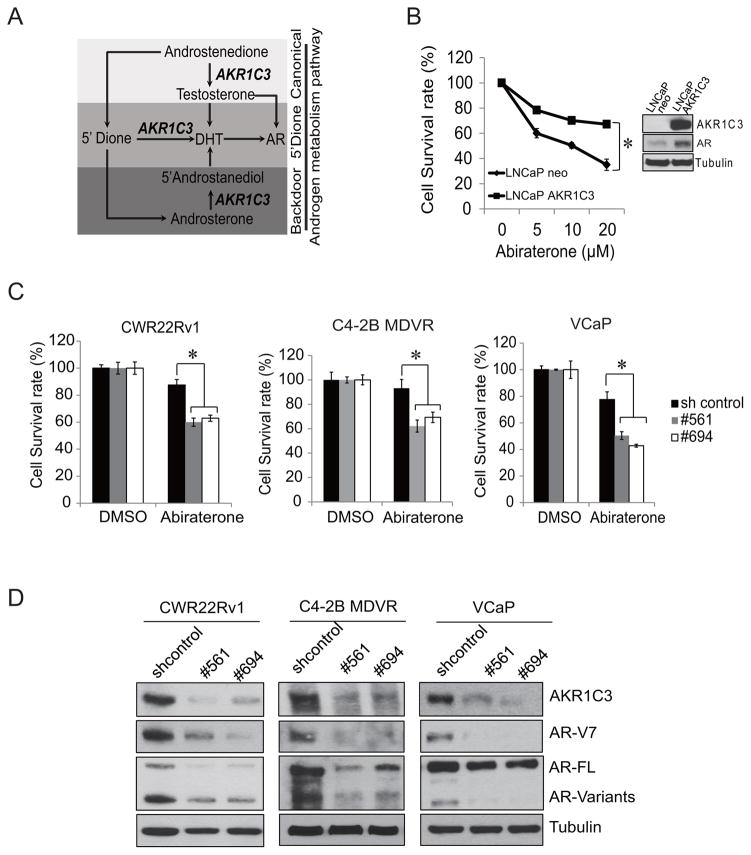
Abiraterone inhibits CYP17A1, resulting in the reduction of testosterone levels in advanced prostate cancer patients. However, the serum level of DHEA-S concentration is still in the high range, and may serve as an ample pool for intracrine androgen synthesis through AKR1C3 (29). AKR1C3 is one of the most important enzymes catalyzing androstenedione conversion to testosterone classically, and it also facilitates the 5′ dione and back door synthesis pathway by catalyzing 5α′ androstenedione and androsterone to 5′ androstanediol respectively which are then converted to DHT. Both testosterone and DHT activate the AR (Fig. 1A). To determine if AKR1C3 is able to induce abiraterone resistance in prostate cancer cells, LNCaP-neo and AKR1C3 overexpressing LNCaP-AKR1C3 cells were treated with different concentrations of abiraterone for 2 days and cell numbers were counted and cell survival rates were calculated. As shown in Fig. 1B, overexpression of AKR1C3 in LNCaP cells significantly induced abiraterone resistance in a dose dependent manner. Interestingly, overexpression of AKR1C3 in LNCaP cells also increased AR protein expression. To further confirm that AKR1C3 drives abiraterone resistance, CWR22Rv1, C4-2B MDVR and VCaP cells were transiently transfected with control shRNA or AKR1C3 shRNA (#561 and #694) and were subsequently treated with abiraterone for 3 days. Both C4-2B MDVR and CWR22Rv1 cells showed high resistance to abiraterone and VCaP cells had a moderate response to abiraterone treatment. Knockdown of AKR1C3 expression significantly enhanced the response to abiraterone in all cell lines (Fig. 1C). Knockdown of AKR1C3 expression also significantly decreased AR and AR variants expression (Fig. 1D). Taken together, these results demonstrated that overexpression of AKR1C3 in prostate cancer cells confers resistance to abiraterone.
Figure 1. Overexpression of AKR1C3 confers resistance to abiraterone.
A. AKR1C3 is involved in the canonical, 5-diol and backdoor pathways of androgen synthesis and activates AR. B. LNCaP-neo and LNCaP-AKR1C3 cells were treated with different concentrations of abiraterone for 2 days. Total cell numbers were counted and cell survival rate (%) was calculated. Whole cell lysates from LNCaP-neo and LNCaP-AKR1C3 cells were subjected to western blot (Inside panel). C. CWR22Rv1, C4-2B MDVR and VCaP cells were transiently transfected with AKR1C3 shRNA (#561 and #694). Following treatment with 10 μM abiraterone for 3 days, total cell numbers were counted and cell survival rate (%) was calculated. D. CWR22Rv1 cells, C4-2B MDVR and VCaP cells were transiently transfected with AKR1C3 shRNA (#561 and #694) for 3 days, AKR1C3, AR-V7 and AR expression were examined by western blot. * p<0.05.
AKR1C3 regulates AR transcriptional activity in abiraterone resistant prostate cancer cells
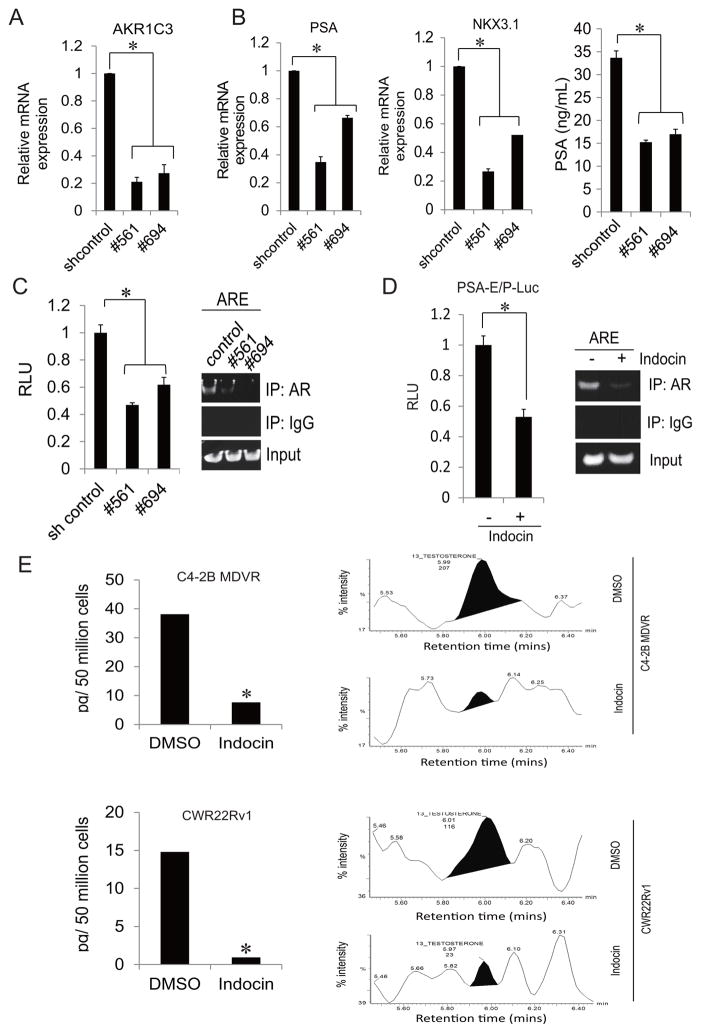
AKR1C3 is not only an important enzyme of androgen synthesis but also acts as an AR co-activator (18). To examine the influence of AKR1C3 on AR activity in C4-2B MDVR cells, AKR1C3 shRNA was transiently transfected into C4-2B MDVR cells. Knockdown of AKR1C3 expression significantly inhibited the expression of the AR target genes such as PSA and NKX3.1 (Fig. 2A and 2B). To further understand the mechanisms of AR transcriptional activity influenced by AKR1C3, a luciferase assay and ChIP assay were performed. As shown in Fig. 2C, knock down of AKR1C3 significantly inhibited PSA luciferase activity and reduced the recruitment of AR to the AREs (Androgen Responsive Elements). The results were confirmed by use of the AKR1C3 enzyme inhibitor Indocin (12). Treatment with Indocin significantly inhibited PSA luciferase activity and reduced the recruitment of AR to the AREs in C4-2B MDVR cells (Fig. 2D). We also examined testosterone levels in C4-2B MDVR cells treated with Indocin by LC-MS. As shown in Fig. 2E, Indocin significantly reduced testosterone levels in C4-2B MDVR and CWR22Rv1 cells.
Figure 2. AKR1C3 inhibition suppressed testosterone level and AR activity in prostate cancer.
A. C4-2B MDVR cells were transiently transfected with control shRNA or AKR1C3 shRNA (#561, #694) for 2 days. Total RNA was extracted and AKR1C3 mRNA level was examined by qRT-PCR. B. C4-2B MDVR cells were transiently transfected with control shRNA or AKR1C3 shRNA (#561, #694), Total RNA was extracted, PSA and NKX3.1 mRNA levels were examined by qRT-PCR, and the supernatants were collected and subjected to PSA ELISA. C. C4-2B MDVR cells were transiently transfected with control shRNA or AKR1C3 shRNA (#561, #694) with PSA-E/P-luc reporter. The luciferase activity was detected by dual luciferase reporter system (left) and whole cell lysates were subjected to ChIP assay (right). D. C4-2B MDVR cells were transiently transfected with PSA-E/P-luc reporter, followed by treatment with DMSO or 20 μM Indocin for 3 days. Luciferase activity was detected by dual luciferase reporter system (left) and whole cell lysates were subjected to ChIP assay (right). E. C4-2B MDVR (top) and CWR22Rv1 (bottom) cells were treated with DMSO or 20 μM Indocin in serum free, phenol red free RPMI1640 medium for 3 days. Fifty million cells were collected per treatment and testosterone level was examined by LC-MS. * p<0.05. Indocin: Indomethacin.
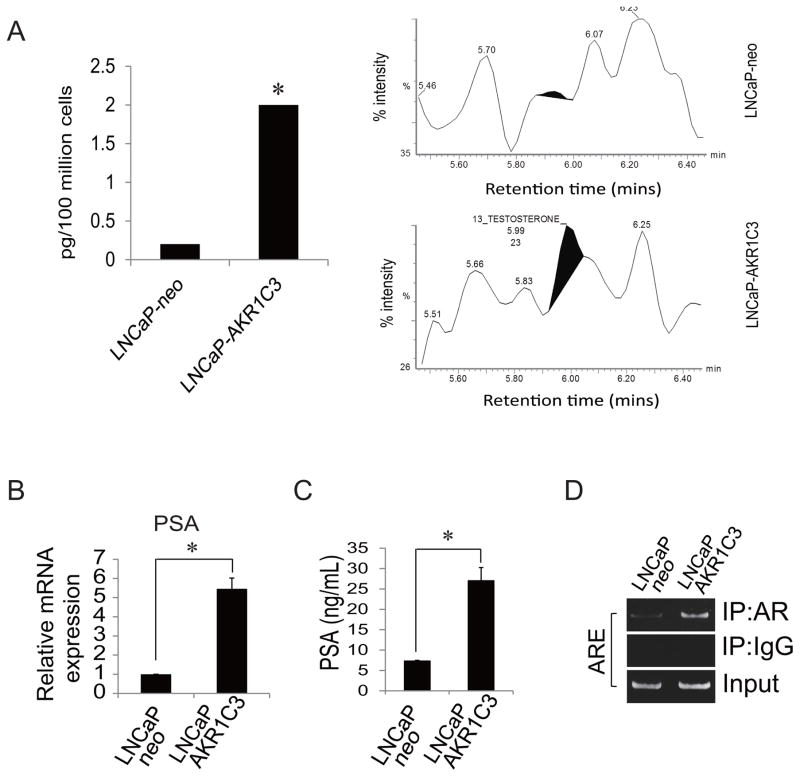
To examine if exogenous expression of AKR1C3 increases testosterone level and upregulates AR transcriptional activity, LNCaP-neo and LNCaP-AKR1C3 cells were cultured in phenol red free and serum free conditions for 3 days and testosterone levels were measured by LC-MS. LNCaP-AKR1C3 cells express significantly higher levels of testosterone than parental LNCaP cells (Fig. 3A). AR transcriptional activity was examined in LNCaP-neo and LNCaP-AKR1C3 cells by real-time PCR, western blot and ChIP assay. As shown in Fig. 3B-D, LNCaP-AKR1C3 cells express higher PSA at both the mRNA and protein level and exhibit enhanced AR recruitment to the PSA promoter compared to LNCaP-neo cells. This data suggests that AKR1C3 not only functions as a steroidogenesis enzyme that induces androgen production but also influences AR transcriptional activity, possibly through AR overexpression and AR co-activation, and thus conferring resistance to abiraterone.
Figure 3. Exogenous AKR1C3 promotes testosterone production and regulates AR transcriptional activity in prostate cancer.
A. LNCaP-neo and LNCaP-AKR1C3 cells were cultured in serum free, phenol red free RPMI1640 medium for 3 days. One hundred million cells were collected per group and testosterone level was examined by LC-MS. B. LNCaP-neo and LNCaP-AKR1C3 cells were cultured in CS-FBS conditions for 3 days, total RNA was extracted and PSA mRNA levels were examined by qRT-PCR, C. The supernatants were collected and PSA level was examined by PSA ELISA. D. LNCaP-neo and LNCaP-AKR1C3 cells were cultured in CS-FBS conditions for 3 days, whole cell lysates were subjected to ChIP assay. *p<0.05.
Abiraterone resistant prostate cancer cells express higher levels of AKR1C3
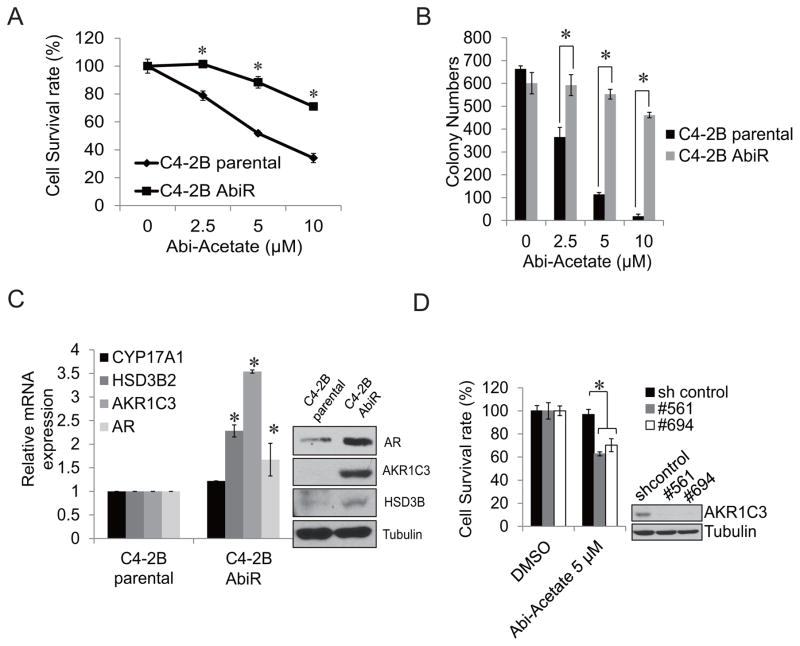
To further confirm our hypothesis that AKR1C3 plays a pivotal role in abiraterone resistance, we generated an abiraterone acetate resistant prostate cancer cell line by continuous culture of C4-2B cells in media containing abiraterone acetate. As shown in Fig. 4A, after 12 months of being cultured in media containing abiraterone acetate, C4-2B AbiR cells exhibited more resistance to abiraterone acetate treatment than C4-2B parental cells. Abiraterone acetate significantly suppressed cell growth in C4-2B parental cells in a dose dependent manner, while abiraterone acetate had moderate effect on C4-2B AbiR cells. This result was also confirmed by clonogenic assay. Abiraterone acetate significantly inhibited the number of colonies in C4-2B parental cells in a dose dependent manner compared to C4-2B AbiR cells (Fig 4B). C4-2B AbiR cells express higher levels of AKR1C3 mRNA and protein than C4-2B parental cells (Fig. 4C). C4-2B AbiR cells also express higher levels of AR protein than C4-2B parental cells. Next, we examined if knockdown of AKR1C3 expression in C4-2B AbiR cells could re-sensitize these cells to abiraterone. Knockdown of AKR1C3 expression using two different AKR1C3 shRNA significantly re-sensitized C4-2B AbiR cells to abiraterone treatment (Fig. 4D). These data suggest chronic abiraterone treatment induces AKR1C3 overexpression, which in turn confers resistance to abiraterone.
Figure 4. Abiraterone resistant prostate cancer cells express higher levels of AKR1C3.
A. C4-2B parental cells and C4-2B AbiR cells were treated with different concentration of abiraterone acetate in RPMI 1640 media containing 10% FBS, total cell numbers were counted and cell survival rate was calculated on day 3. B. The clonogenic ability of C4-2B parental and C4-2B AbiR cells treated with 2.5 μM, 5 μM or 10 μM abiraterone acetate. The colonies were counted and results are presented as means ± SD of 2 experiments performed in duplicate, C. C4-2B parental cells and C4-2B MDVR cells were cultured in RPMI 1640 media containing 10% FBS for 3 days, total RNA was extracted and AKR1C3, CYP17A1, HSD3B2 and AR mRNA levels were analyzed by qRT-PCR. Whole cell lysates were immunoblotted with the indicated antibodies. D. C4-2B AbiR cells were transiently transfected with AKR1C3 shRNA (#561 and #694). Following treatment with 5 μM abiraterone acetate for 3 days, total cell numbers were counted and cell survival rate (%) was calculated. Knockdown effects were examined by western blot. Abi: Abiraterone. * P<0.05
Targeting AKR1C3 with Indocin enhances abiraterone treatment in vitro and in vivo
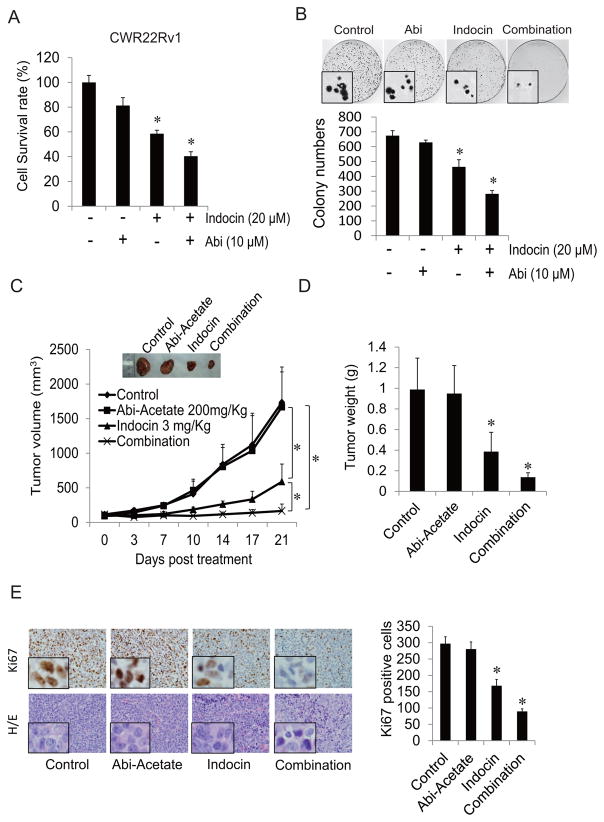
To examine if targeting AKR1C3 enhances abiraterone treatment, we treated CWR22Rv1 cells with Indocin, an AKR1C3 inhibitor (12), in conjunction with abiraterone. CWR22Rv1 cells were treated with 20 μM Indocin with or without 10 μM abiraterone for 3 days and total cell numbers were counted. As shown in Fig. 5A, 10 μM abiraterone had limited effects on cell growth, 20 μM Indocin inhibited cell growth, and the combination treatment further inhibited cell growth. These results were also confirmed by clonogenic assay: Indocin combined with abiraterone further inhibited colony numbers and reduced colony size in CWR22Rv1 cells compared to either treatment on its own (Fig. 5B).
Figure 5. Indocin enhances abiraterone treatment in vitro and in vivo.
A. CWR22Rv1cells were treated with 20 μM Indocin with or without 10 μM abiraterone for 2 days and total cell numbers were counted and cell survival rate was calculated. B. CWR22Rv1cells were treated with 20 μM Indocin with or without 10 μM abiraterone and clonogenic assays were performed; colonies were counted and results are presented as means ± SD of 2 experiments performed in duplicate, the representative pictures were taken under a microscope, C. Mice bearing CWR22Rv1 xenografts were treated with vehicle control, abiraterone acetate (200 mg/Kg p.o), Indocin (3mg/Kg i.p) or their combination for 3 weeks. Tumor volumes were measured twice weekly. D. Each group of tumors was weighed. E. IHC staining of Ki67 in each group was performed and quantified. *p<0.05. Abi: Abiraterone, Indocin: Indomethacin.
To test if inhibition of AKR1C3 activity enhances abiraterone treatment in vivo, a CWR22Rv1 xenograft model was developed. As shown in Fig. 5C and 5D, CWR22Rv1 tumors were resistant to abiraterone. Treatment with Indocin alone significantly inhibited tumor growth and combination of abiraterone and Indocin further inhibited tumor growth compared to either treatment alone. Indocin inhibited Ki67 expression while combination treatment further lowered Ki67 expression (Fig. 5E). These data demonstrate that inhibition of AKR1C3 activity by Indocin overcomes abiraterone resistance, providing preclinical data to support further clinical development of combination therapy of abiraterone and Indocin to treat advanced prostate cancer.
Discussion
Intratumoral androgen biosynthesis is well characterized as a mechanism of CRPC (30–33). Many enzymes are involved in androgen synthesis, including CYP17A1, AKR1C3 and HSD3B. CYP17A1 can be inhibited by abiraterone in clinical treatments (4, 34). However, serum levels of androgens are still high in some patients treated with abiraterone, suggesting that inhibition of androgen synthesis by abiraterone is incomplete, and sustained steroidogenesis contributes to resistance (10, 35, 36). In this study, we demonstrated that AKR1C3 is overexpressed in abiraterone resistant prostate cancer cells. Overexpression of AKR1C3 increases intracrine androgens and AR expression and induces abiraterone resistance, while down regulation of AKR1C3 sensitizes resistant cells to abiraterone treatment. Furthermore, we demonstrated that Indocin (an AKR1C3 inhibitor) inhibits the levels of intracrine androgens, suppresses AR and AR variants expression and overcomes abiraterone resistance and enhances abiraterone treatment both in vitro and in vivo.
Abiraterone inhibits CYP17A1, resulting in the reduction of testosterone levels in advanced prostate cancer patients. However, the serum level of DHEA-S is still in the high range, and may serve as an ample pool for intracrine androgen synthesis (29). Many enzymes involved in androgen synthesis, including AKR1C3 and HSD3B, are elevated in abiraterone resistant C4-2B AbiR cells. AKR1C3 is one of the most important enzymes in androgen synthesis; it catalyzes the reduction of 5α-dihydrotestosterone to 5α-androstane-3α,17β-dior by its 3α-HSD activity and conversion of androstenedione to testosterone by its 17β-HSD activity (16). We showed that the levels of intracrine androgens are elevated in AKR1C3 overexpressing LNCaP-AKR1C3 cells compared to their parental cells, suggesting that AKR1C3 activation results in an increase in androgen synthesis in these cells.
In addition to its function as a critical enzyme in intracrine androgen synthesis, AKR1C3 also catalyzes the formation of prostaglandin (PG) F2α and 11β-PGF2α from PGH2 and PGD2, respectively. The PGF2α and 11β-PGF2α can inactivate proliferator peroxisome activator receptor gamma (PPARγ) and displays anti-proliferative effects (37). Recently, the AKR1C3 has been found to directly interact with E3 ubiquitin ligase siah2 and control its stabilization, and thus regulate the siah2 dependent AR signaling (38). Furthermore, AKR1C3 has been found to specifically interact with the AR and is recruited to the ARE on the promoter of androgen responsive genes. AKR1C3 co-activating the AR in prostate cancer tissue might magnify androgen effects (18). This makes the fact that AKR1C3 is pharmacologically targetable in prostate cancer highly important.
AR deregulation has been found in 80% of CRPC patients (39). AR overexpression can confer AR hypersensitivity to low levels of androgen and may contribute to drug resistance (40). In the present study, we found that AR is overexpressed in abiraterone resistant C4-2B-AbiR and AKR1C3 overexpressing LNCaP-AKR1C3 cells. Knockdown of AKR1C3 expression down regulates full length AR as well as AR variants expression in these abiraterone resistant cell lines, suggesting that AKR1C3 regulates AR and AR varinats expression. The effects of altered AKR1C3 expression on androgen signaling can be due to a number of potential mechanisms including changes in AR and AR variants expression (41, 42) (43), changes in cellular concentration of androgens (12), and/or AKR1C3 functions as a coregulator for AR (18). Taken together, AKR1C3 is not only an enzyme that catalyzes testosterone synthesis but also affects AR expression and/or functions as an AR co-activator to regulate AR activity.
Both abiraterone and enzalutamide are FDA approved. However, when a patient becomes resistant to one drug, the subsequent response rate to the other drug is 20% or less (43–45). This suggests common resistance mechanisms exist for the observed cross resistance. In previous studies, we demonstrated that AKR1C3 activation increases intracrine androgens and confers resistance to enzalutamide (12). Here we showed that AKR1C3 activation also induces resistance to abiraterone. Thus AKR1C3 activation could represent a common resistance mechanism for cross resistance between enzalutamide and abiraterone. We showed that enzalutamide resistant C4-2B MDVR cells are resistant to abiraterone treatment, knocking down AKR1C3 expression blocked the recruitment of AR to the AREs and reduced the levels of intracrine androgens, thus re-sensitizing the cells to abiraterone treatment. These results further the understanding of cross-resistance between abiraterone and enzalutamide in prostate cancer, and provide the groundwork for the development of meaningful treatment strategies by targeting AKR1C3 to enhance next generation anti-androgen therapies.
Indocin, a non-steroidal anti-inflammatory drug (NSAID) used for reducing fever, pain and inflammation, has been shown to inhibit AKR1C3 activity (12, 46). Indocin blocks AKR1C3 function through binding with the AKR1C3 active site (20). Indocin exhibits a strong selectivity for AKR1C3 (8.2 μM) over AKR1C1 and AKR1C2 (over 100 μM) (46). Recently, several derivatives of Indocin, as well as other compounds, were developed that exhibit higher potency to inhibit AKR1C3 activity (47, 48). These, in addition to baccharin (49) and other more specific AKR1C3 inhibitors such as (3-(4-(Trifluoromethyl)phenylamino)benzoic acid) have been identified and characterized (48). We showed that Indocin is able to inhibit the levels of intracrine androgens in C4-2B MDVR cells and CWR22Rv1 cells and suppress prostate cancer tumor growth and enhance enzalutamide and abiraterone treatment, suggesting that Indocin is more potent than SN33638, an inhibitor of AKR1C3, which has limited activity in the inhibition of testosterone production and cell proliferation (50). Indocin has been on the market and safely taken by patients, including prostate cancer patients, for decades. Together, this study and the previous report of Indocin synergizing with enzalutamide therapy, pave the way for the development of Indocin as a potential treatment strategy to block AKR1C3 activation to overcome treatment resistance and enhance the therapeutic effect of enzalutamide and abiraterone.
In summary, we have identified AKR1C3 activation as a critical mechanism of resistance to abiraterone through increasing intracrine androgen synthesis and enhancing androgen signaling. Furthermore, this study provides a preclinical proof-of-principle for clinical trials investigating combination treatment of Indocin with abiraterone for advanced prostate cancer.
Acknowledgments
Financial Information: This work was supported in part by grants NIH/NCI CA140468, CA168601, CA179970 (A.C. Gao), DOD PC130062 (A.C. Gao), and US Department of Veterans Affairs, ORD VA Merits I01BX0002653 (A.C. Gao).
Abbreviations
- 5α-dione
5α-androstanedione
- Abi
Abiraterone
- AbiR
Abiraterone resistance
- AR
Androgen receptor
- A′ dione
Androstenedione
- Cox
Cyclooxygenase
- DHEA-S
Dehydroepiandrosterone sulfate
- Enza
Enzalutamide
- FBS
Fetal bovine serum
- Indocin
Indomethacin
- MDVR
Enzalutamide resistance
- NSAID
Nonsteroidal anti-inflammatory drug
- PG
Prostaglandin
- PPARγ
Peroxisome proliferator-activated receptor gamma
- PSA
Prostate-specific antigen
- SCID
Severe combined immunodeficiency
Footnotes
Conflict of Interest Statement: CL, WL, and ACG are co-inventors of a patent application covering the use of combination of indomethacin and abiraterone. CPE has received commercial research grant, honoraria and consultant fee from Medivation/Astellas.
References
- 1.Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. The New England journal of medicine. 2004;351:1502–12. doi: 10.1056/NEJMoa040720. [DOI] [PubMed] [Google Scholar]
- 2.de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147–54. doi: 10.1016/S0140-6736(10)61389-X. [DOI] [PubMed] [Google Scholar]
- 3.Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. The New England journal of medicine. 2012;367:1187–97. doi: 10.1056/NEJMoa1207506. [DOI] [PubMed] [Google Scholar]
- 4.de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and increased survival in metastatic prostate cancer. The New England journal of medicine. 2011;364:1995–2005. doi: 10.1056/NEJMoa1014618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haidar S, Ehmer PB, Barassin S, Batzl-Hartmann C, Hartmann RW. Effects of novel 17alpha-hydroxylase/C17, 20-lyase (P450 17, CYP 17) inhibitors on androgen biosynthesis in vitro and in vivo. The Journal of steroid biochemistry and molecular biology. 2003;84:555–62. doi: 10.1016/s0960-0760(03)00070-0. [DOI] [PubMed] [Google Scholar]
- 6.Antonarakis ES, Lu CX, Wang H, Luber B, Nakazawa M, Roeser JC, et al. AR-V7 and Resistance to Enzalutamide and Abiraterone in Prostate Cancer. New Engl J Med. 2014;371:1028–38. doi: 10.1056/NEJMoa1315815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen EJ, Sowalsky AG, Gao S, Cai C, Voznesensky O, Schaefer R, et al. Abiraterone treatment in castration-resistant prostate cancer selects for progesterone responsive mutant androgen receptors. Clin Cancer Res. 2015;21:1273–80. doi: 10.1158/1078-0432.CCR-14-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Romanel A, Gasi Tandefelt D, Conteduca V, Jayaram A, Casiraghi N, Wetterskog D, et al. Plasma AR and abiraterone-resistant prostate cancer. Science translational medicine. 2015;7:312re10. doi: 10.1126/scitranslmed.aac9511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mostaghel EA, Marck BT, Plymate SR, Vessella RL, Balk S, Matsumoto AM, et al. Resistance to CYP17A1 inhibition with abiraterone in castration-resistant prostate cancer: induction of steroidogenesis and androgen receptor splice variants. Clinical cancer research: an official journal of the American Association for Cancer Research. 2011;17:5913–25. doi: 10.1158/1078-0432.CCR-11-0728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang KH, Li R, Kuri B, Lotan Y, Roehrborn CG, Liu J, et al. A gain-of-function mutation in DHT synthesis in castration-resistant prostate cancer. Cell. 2013;154:1074–84. doi: 10.1016/j.cell.2013.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tian Y, Zhao L, Zhang H, Liu X, Zhao L, Zhao X, et al. AKR1C3 overexpression may serve as a promising biomarker for prostate cancer progression. Diagn Pathol. 2014;9:42. doi: 10.1186/1746-1596-9-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu C, Lou W, Zhu Y, Yang JC, Nadiminty N, Gaikwad NW, et al. Intracrine Androgens and AKR1C3 Activation Confer Resistance to Enzalutamide in Prostate Cancer. Cancer research. 2015;75:1413–22. doi: 10.1158/0008-5472.CAN-14-3080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labrie F, Luu-The V, Lin SX, Labrie C, Simard J, Breton R, et al. The key role of 17 beta-hydroxysteroid dehydrogenases in sex steroid biology. Steroids. 1997;62:148–58. doi: 10.1016/s0039-128x(96)00174-2. [DOI] [PubMed] [Google Scholar]
- 14.Bauman DR, Steckelbroeck S, Williams MV, Peehl DM, Penning TM. Identification of the major oxidative 3alpha-hydroxysteroid dehydrogenase in human prostate that converts 5alpha-androstane-3alpha,17beta-diol to 5alpha-dihydrotestosterone: a potential therapeutic target for androgen-dependent disease. Mol Endocrinol. 2006;20:444–58. doi: 10.1210/me.2005-0287. [DOI] [PubMed] [Google Scholar]
- 15.Penning TM, Burczynski ME, Jez JM, Hung CF, Lin HK, Ma H, et al. Human 3alpha-hydroxysteroid dehydrogenase isoforms (AKR1C1-AKR1C4) of the aldo-keto reductase superfamily: functional plasticity and tissue distribution reveals roles in the inactivation and formation of male and female sex hormones. Biochem J. 2000;351:67–77. doi: 10.1042/0264-6021:3510067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stanbrough M, Bubley GJ, Ross K, Golub TR, Rubin MA, Penning TM, et al. Increased expression of genes converting adrenal androgens to testosterone in androgen-independent prostate cancer. Cancer Res. 2006;66:2815–25. doi: 10.1158/0008-5472.CAN-05-4000. [DOI] [PubMed] [Google Scholar]
- 17.Wako K, Kawasaki T, Yamana K, Suzuki K, Jiang S, Umezu H, et al. Expression of androgen receptor through androgen-converting enzymes is associated with biological aggressiveness in prostate cancer. Journal of clinical pathology. 2008;61:448–54. doi: 10.1136/jcp.2007.050906. [DOI] [PubMed] [Google Scholar]
- 18.Yepuru M, Wu Z, Kulkarni A, Yin F, Barrett CM, Kim J, et al. Steroidogenic enzyme AKR1C3 is a novel androgen receptor-selective coactivator that promotes prostate cancer growth. Clinical cancer research: an official journal of the American Association for Cancer Research. 2013;19:5613–25. doi: 10.1158/1078-0432.CCR-13-1151. [DOI] [PubMed] [Google Scholar]
- 19.Liedtke AJ, Adeniji AO, Chen M, Byrns MC, Jin Y, Christianson DW, et al. Development of potent and selective indomethacin analogues for the inhibition of AKR1C3 (Type 5 17beta-hydroxysteroid dehydrogenase/prostaglandin F synthase) in castrate-resistant prostate cancer. J Med Chem. 2013;56:2429–46. doi: 10.1021/jm3017656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lovering AL, Ride JP, Bunce CM, Desmond JC, Cummings SM, White SA. Crystal structures of prostaglandin D(2) 11-ketoreductase (AKR1C3) in complex with the nonsteroidal anti-inflammatory drugs flufenamic acid and indomethacin. Cancer research. 2004;64:1802–10. doi: 10.1158/0008-5472.can-03-2847. [DOI] [PubMed] [Google Scholar]
- 21.Brunelli C, Amici C, Angelini M, Fracassi C, Belardo G, Santoro MG. The non-steroidal anti-inflammatory drug indomethacin activates the eIF2alpha kinase PKR, causing a translational block in human colorectal cancer cells. The Biochemical journal. 2012;443:379–86. doi: 10.1042/BJ20111236. [DOI] [PubMed] [Google Scholar]
- 22.Tse AK, Cao HH, Cheng CY, Kwan HY, Yu H, Fong WF, et al. Indomethacin sensitizes TRAIL-resistant melanoma cells to TRAIL-induced apoptosis through ROS-mediated upregulation of death receptor 5 and downregulation of survivin. The Journal of investigative dermatology. 2014;134:1397–407. doi: 10.1038/jid.2013.471. [DOI] [PubMed] [Google Scholar]
- 23.Liu C, Lou W, Zhu Y, Nadiminty N, Schwartz C, Evans CP, et al. Niclosamide inhibits androgen receptor variants expression and overcomes Enzalutamide resistance in castration resistant prostate cancer. Clinical cancer research: an official journal of the American Association for Cancer Research. 2014 doi: 10.1158/1078-0432.CCR-13-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu C, Armstrong C, Zhu Y, Lou W, Gao AC. Niclosamide enhances abiraterone treatment via inhibition of androgen receptor variants in castration resistant prostate cancer. Oncotarget. 2016 doi: 10.18632/oncotarget.8493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gaikwad NW. Ultra performance liquid chromatography-tandem mass spectrometry method for profiling of steroid metabolome in human tissue. Analytical chemistry. 2013;85:4951–60. doi: 10.1021/ac400016e. [DOI] [PubMed] [Google Scholar]
- 26.Liu C, Zhu Y, Lou W, Cui Y, Evans CP, Gao AC. Inhibition of constitutively active Stat3 reverses enzalutamide resistance in LNCaP derivative prostate cancer cells. The Prostate. 2014;74:201–9. doi: 10.1002/pros.22741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu C, Nadiminty N, Tummala R, Chun JY, Lou W, Zhu Y, et al. Andrographolide targets androgen receptor pathway in castration-resistant prostate cancer. Genes Cancer. 2011;2:151–9. doi: 10.1177/1947601911409744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu C, Lou W, Armstrong C, Zhu Y, Evans CP, Gao AC. Niclosamide suppresses cell migration and invasion in enzalutamide resistant prostate cancer cells via Stat3-AR axis inhibition. The Prostate. 2015;75:1341–53. doi: 10.1002/pros.23015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tamae D, Mostaghel E, Montgomery B, Nelson PS, Balk SP, Kantoff PW, et al. The DHEA-sulfate depot following P450c17 inhibition supports the case for AKR1C3 inhibition in high risk localized and advanced castration resistant prostate cancer. Chemico-biological interactions. 2015;234:332–8. doi: 10.1016/j.cbi.2014.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cai C, Chen S, Ng P, Bubley GJ, Nelson PS, Mostaghel EA, et al. Intratumoral de novo steroid synthesis activates androgen receptor in castration-resistant prostate cancer and is upregulated by treatment with CYP17A1 inhibitors. Cancer research. 2011;71:6503–13. doi: 10.1158/0008-5472.CAN-11-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ishizaki F, Nishiyama T, Kawasaki T, Miyashiro Y, Hara N, Takizawa I, et al. Androgen deprivation promotes intratumoral synthesis of dihydrotestosterone from androgen metabolites in prostate cancer. Scientific reports. 2013;3:1528. doi: 10.1038/srep01528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Locke JA, Guns ES, Lubik AA, Adomat HH, Hendy SC, Wood CA, et al. Androgen levels increase by intratumoral de novo steroidogenesis during progression of castration-resistant prostate cancer. Cancer research. 2008;68:6407–15. doi: 10.1158/0008-5472.CAN-07-5997. [DOI] [PubMed] [Google Scholar]
- 33.Mohler JL, Titus MA, Bai S, Kennerley BJ, Lih FB, Tomer KB, et al. Activation of the androgen receptor by intratumoral bioconversion of androstanediol to dihydrotestosterone in prostate cancer. Cancer research. 2011;71:1486–96. doi: 10.1158/0008-5472.CAN-10-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. The New England journal of medicine. 2013;368:138–48. doi: 10.1056/NEJMoa1209096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Attard G, Reid AH, Auchus RJ, Hughes BA, Cassidy AM, Thompson E, et al. Clinical and biochemical consequences of CYP17A1 inhibition with abiraterone given with and without exogenous glucocorticoids in castrate men with advanced prostate cancer. J Clin Endocrinol Metab. 2012;97:507–16. doi: 10.1210/jc.2011-2189. [DOI] [PubMed] [Google Scholar]
- 36.Li Z, Bishop AC, Alyamani M, Garcia JA, Dreicer R, Bunch D, et al. Conversion of abiraterone to D4A drives anti-tumour activity in prostate cancer. Nature. 2015 doi: 10.1038/nature14406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Desmond JC, Mountford JC, Drayson MT, Walker EA, Hewison M, Ride JP, et al. The aldo-keto reductase AKR1C3 is a novel suppressor of cell differentiation that provides a plausible target for the non-cyclooxygenase-dependent antineoplastic actions of nonsteroidal anti-inflammatory drugs. Cancer research. 2003;63:505–12. [PubMed] [Google Scholar]
- 38.Fan L, Peng G, Hussain A, Fazli L, Guns E, Gleave M, et al. The Steroidogenic Enzyme AKR1C3 Regulates Stability of the Ubiquitin Ligase Siah2 in Prostate Cancer Cells. The Journal of biological chemistry. 2015;290:20865–79. doi: 10.1074/jbc.M115.662155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Linja MJ, Savinainen KJ, Saramaki OR, Tammela TL, Vessella RL, Visakorpi T. Amplification and overexpression of androgen receptor gene in hormone-refractory prostate cancer. Cancer research. 2001;61:3550–5. [PubMed] [Google Scholar]
- 40.Waltering KK, Helenius MA, Sahu B, Manni V, Linja MJ, Janne OA, et al. Increased expression of androgen receptor sensitizes prostate cancer cells to low levels of androgens. Cancer research. 2009;69:8141–9. doi: 10.1158/0008-5472.CAN-09-0919. [DOI] [PubMed] [Google Scholar]
- 41.Cai C, He HH, Chen S, Coleman I, Wang H, Fang Z, et al. Androgen receptor gene expression in prostate cancer is directly suppressed by the androgen receptor through recruitment of lysine-specific demethylase 1. Cancer cell. 2011;20:457–71. doi: 10.1016/j.ccr.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cai C, Wang H, Xu Y, Chen S, Balk SP. Reactivation of androgen receptor-regulated TMPRSS2:ERG gene expression in castration-resistant prostate cancer. Cancer research. 2009;69:6027–32. doi: 10.1158/0008-5472.CAN-09-0395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mitsiades N, Sung CC, Schultz N, Danila DC, He B, Eedunuri VK, et al. Distinct patterns of dysregulated expression of enzymes involved in androgen synthesis and metabolism in metastatic prostate cancer tumors. Cancer research. 2012;72:6142–52. doi: 10.1158/0008-5472.CAN-12-1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bianchini D, Lorente D, Rodriguez-Vida A, Omlin A, Pezaro C, Ferraldeschi R, et al. Antitumour activity of enzalutamide (MDV3100) in patients with metastatic castration-resistant prostate cancer (CRPC) pre-treated with docetaxel and abiraterone. European journal of cancer. 2014;50:78–84. doi: 10.1016/j.ejca.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 45.Azad AA, Eigl BJ, Murray RN, Kollmannsberger C, Chi KN. Efficacy of enzalutamide following abiraterone acetate in chemotherapy-naive metastatic castration-resistant prostate cancer patients. European urology. 2015;67:23–9. doi: 10.1016/j.eururo.2014.06.045. [DOI] [PubMed] [Google Scholar]
- 46.Byrns MC, Jin Y, Penning TM. Inhibitors of type 5 17beta-hydroxysteroid dehydrogenase (AKR1C3): overview and structural insights. The Journal of steroid biochemistry and molecular biology. 2011;125:95–104. doi: 10.1016/j.jsbmb.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adeniji AO, Chen M, Penning TM. AKR1C3 as a target in castrate resistant prostate cancer. The Journal of steroid biochemistry and molecular biology. 2013;137:136–49. doi: 10.1016/j.jsbmb.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Adeniji AO, Twenter BM, Byrns MC, Jin Y, Chen M, Winkler JD, et al. Development of potent and selective inhibitors of aldo-keto reductase 1C3 (type 5 17beta-hydroxysteroid dehydrogenase) based on N-phenyl-aminobenzoates and their structure-activity relationships. Journal of medicinal chemistry. 2012;55:2311–23. doi: 10.1021/jm201547v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Endo S, Matsunaga T, Kanamori A, Otsuji Y, Nagai H, Sundaram K, et al. Selective inhibition of human type-5 17beta-hydroxysteroid dehydrogenase (AKR1C3) by baccharin, a component of Brazilian propolis. Journal of natural products. 2012;75:716–21. doi: 10.1021/np201002x. [DOI] [PubMed] [Google Scholar]
- 50.Yin YD, Fu M, Brooke DG, Heinrich DM, Denny WA, Jamieson SM. The Activity of SN33638, an Inhibitor of AKR1C3, on Testosterone and 17beta-Estradiol Production and Function in Castration-Resistant Prostate Cancer and ER-Positive Breast Cancer. Frontiers in oncology. 2014;4:159. doi: 10.3389/fonc.2014.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]