Abstract
Geographical clusters are defined as the occurrence of an unusual number of cases higher than expected in a given geographical area in a certain period of time. The aim of this study was to identify potential geographical clusters of specific selected congenital anomalies (CA) in Argentina. The cases were ascertained from 703,325 births, examined in 133 maternity hospitals in the 24 provinces of Argentina. We used the spatial scan statistic to determine areas of Argentina which had statistically significant elevations of prevalence. Prenatal diagnosis followed by referral of high-risk pregnancies to high complexity hospitals in a hospital-based surveillance system can create artifactual clusters. We assessed the referral bias by evaluating the prevalence heterogeneity within each cluster. Eight clusters of selected CAs with unusually high birth prevalence were identified: anencephaly, encephalocele, spina bifida, diaphragmatic hernia, talipes equinovarus, omphalocele, Cleft lip with or without cleft palate (CL/P), and Down syndrome. The clusters of Down syndrome and CL/P observed in this study match the previously reported clusters. These findings support local targeted interventions to lower the prevalence of the CAs and/or further research on the cause of each cluster. The clusters of spina bifida, anencephaly, encephalocele, omphalocele, congenital diaphragmatic hernia, and talipes equinovarus may be influenced by prenatal diagnosis and referral to high complexity hospitals.
Keywords: Congenital anomalies, Birth prevalence, Geographic clusters, National Network of Congenital Anomalies of Argentina (RENAC)
Introduction
Congenital anomalies (CAs) are morphological or functional alterations of prenatal etiology which are present from birth, even if detected later in life. Major morphological CAs have a significant effect on health and generally require medical or surgical treatment (e.g., cleft lip and palate, gastroschisis, spina bifida) (WHO 1996). In the last years in Argentina, media reports alleged high prevalence and geographic clusters of CAs, and postulated that these might be linked to exposure to environmental pollutants (i.e., pesticides). Anecdotal evidence from clinicians also suggests this possibility. We report on the results of a study setup in response to public concern to establish if there is a high prevalence of selected CAs in Argentina or any geographic cluster within the country.
Geographical clusters are defined as the occurrence of an unusual number of cases higher than expected in a given geographical area in a certain period of time. Many CAs can be prevented, and identification of clusters may provide an opportunity for targeted interventions designed to prevent specific CAs. Examining the geographic distribution of birth defects can also be useful in exploratory etiologic research. After the identification of a cluster, more specific research like a case-control study can be conducted to further assess the cause of the cluster. Specific studies of certain CAs may uncover possible environmental or genetic risk factors and assist with the generation of hypotheses about underlying causes of these conditions (Root et al. 2009). Previous studies evaluated clusters of selected CAs in different countries: orofacial clefts in the USA and South America (Cech et al. 2007; Poletta et al. 2007; Gili et al. 2015), gastroschisis in the USA (Root et al. 2009, 2011), anophtalmia in the UK (Dolk et al., 1998), sirenomelia in Colombia (Castilla et al., 2008), anorectal atresia/stenosis in China (Yuan et al. 2009), among others. The Latin-American Collaborative Study of Congenital Malformations (ECLAMC; Castilla and Orioli 2004) has previously evaluated clusters of several CAs in South American countries, including Argentina, using spatial scan statistics (Poletta et al. 2007; Gili et al. 2015).
Argentina is located in southern South America. It is a federal republic consisting of 24 jurisdictions or provinces. From a historical and geographical criterion, Argentina can be divided into five regions: Central (the most populous), Cuyo (west), Northwest, Northeast, and Patagonia (south). It has a population of 40,117,096 inhabitants, 89.4 % of whom live in urban areas. The continental part has an area of 2,800,000 km2, with a low population density of 14.4 people per square kilometer. Around 65 % of the population is concentrated in the central region provinces (INDEC 2010).
The aim of this study was to identify potential geographical clusters of specific selected CAs in Argentina. This is the first study with this aim that used data from the National Network of Congenital Abnormalities Argentina (RENAC), formerly known as National Registry of Congenital Anomalies (Groisman et al. 2013), a national hospital-based surveillance system.
Material
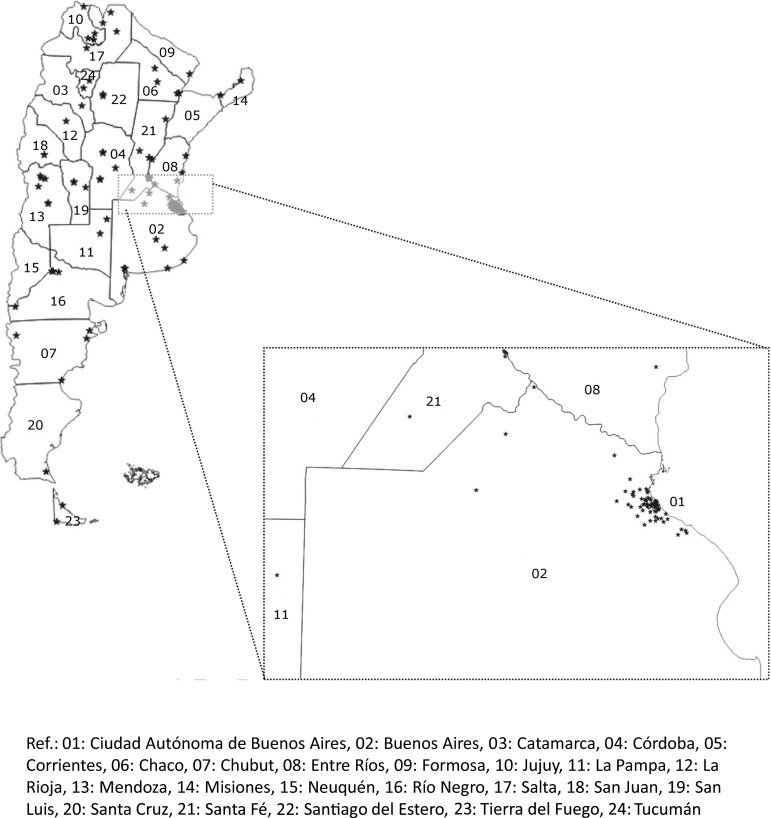
This observational descriptive study was performed with material obtained by the RENAC surveillance system since 2009 until 2013. The cases were ascertained from 703,325 births, examined in 133 maternity hospitals in the 24 provinces of Argentina (Fig. 1). The CAs included were those with major clinical impact and thought to be easily recognizable, consistently and accurately diagnosed. The following CAs were included anencephaly (ICD-10: Q00), spina bifida (ICD-10: Q05), encephalocele (ICD-10: Q01), Cleft lip with or without cleft palate (CL/P; ICD-10: Q36-Q37), cleft palate (CP; ICD-10: Q35), esophageal atresia (ICD-10: Q39.0-Q39.1), anorectal malformation (ICD-10: Q42), congenital diaphragmatic hernia (ICD-10: Q79.0), talipes equinovarus (ICD-10: Q66.0), talipes calcaneovalgus (ICD-10: Q66.1), omphalocele (ICD-10: Q79.2), gastroschisis (ICD-10: Q79.3), and Down syndrome (ICD-10: Q90). Cases included live births and stillbirths, equal or over 500 g. All clinical presentations (isolated and associated) were considered in the cluster analysis. We excluded from the analysis CAs that would not normally be identified in a standard physical examination and require diagnostic procedures (i.e., echocardiogram for definitive diagnosis of congenital heart defects).
Fig. 1.
The map of Argentina with the location of hospitals participating in the study
Methods
Birth prevalence of selected CAs was calculated considering Poisson’s distribution, with a 95 % confidence interval. For the geographic cluster analysis, we used the spatial scan statistic to determine areas of Argentina which had statistically significant elevations of prevalence (Kulldorff and Nagarwalla 1995; Kulldorff et al. 1998). This analysis uses information of the number of cases, number of total births, and the exact geographic location of each of the 133 RENAC’s maternity hospitals (defined by their geographic coordinates) and then tests several circular areas with different sizes and centered in each geographic point. Starting from an initial radius of 0, the area progressively enlarged by including more maternity hospitals and detecting significantly higher than expected birth prevalence of each selected anomaly. The null hypothesis stated that the birth prevalence for each selected anomaly was homogeneous in the whole RENAC population, and the alternative hypothesis assumed a higher risk within a given area, as compared with the birth prevalence observed outside that area. This test used the maximum likelihood ratio test statistic to determine those areas with the smallest probability for the observed unusual birth prevalence resulting from random sampling variation. The P value was obtained through multiple simulations by the Monte Carlo model of 9999 replications. The critical value for significance was set at P < 0.05. The cluster regions were not established “a priori”. The three restrictions introduced in our analysis were the following: (1) the number of births captured in a given area had to be more than 10,000 births to avoid birth prevalence variations due to a small number of births, (2) the diameter of the cluster area had to be less than 150 km to avoid excessively large clusters, and (3) the resulting areas did not overlap among them.
We examined the birth prevalence heterogeneity within each cluster with Cochran’s Q test, at a significance level of P < 0.05. Heterogeneous clusters are more likely influenced by referral bias because one or more of the high complexity hospitals within the cluster could be responsible for the detected prevalence increase in the cluster area.
Results
During the study period, RENAC covered 18.75 % of birth of the country. Among 703,422 births included, 11,373 cases with major CAs were detected. The birth prevalence of major CAs was 1.62 (CI 95 % 1.59–1.65). We present the birth prevalence of the 13 specific selected anomalies in Table 1. Prenatal diagnosis was higher for encephalocele (74 %), anencephaly (71 %), omphalocele (71 %), and congenital diaphragmatic hernia (64 %).
Table 1.
Birth prevalence of selected congenital anomalies per 10,000 births, RENAC Argentina, 2009–2013
| Congenital anomaly | Cases | Prevalence (CI 95 %) |
|---|---|---|
| Anencephaly | 212 | 3.0 (2.6–3.4) |
| Encephalocele | 97 | 1.4 (1.1–1.7) |
| Spina bifida | 389 | 5.5 (5.0–6.1) |
| Diaphragmatic hernia | 225 | 3.2 (2.8–3.6) |
| Talipes equinovarus | 484 | 6.9 (6.3–7.5) |
| Talipes calcaneovalgus | 89 | 1.3 (1.0–1.6) |
| Gastroschisis | 600 | 8.5 (7.9–9.2) |
| Omphalocele | 167 | 2.4 (2.0–2.8) |
| Cleft lip with or without cleft palate | 826 | 11.7 (11.0–12.6) |
| Cleft palate | 220 | 3.1 (2.7–3.6) |
| Down syndrome | 1220 | 17.3 (16.4–18.3) |
| Esophageal atresia | 230 | 3.3 (2.9–3.7) |
| Anorectal malformation | 231 | 3.3 (2.9–3.7) |
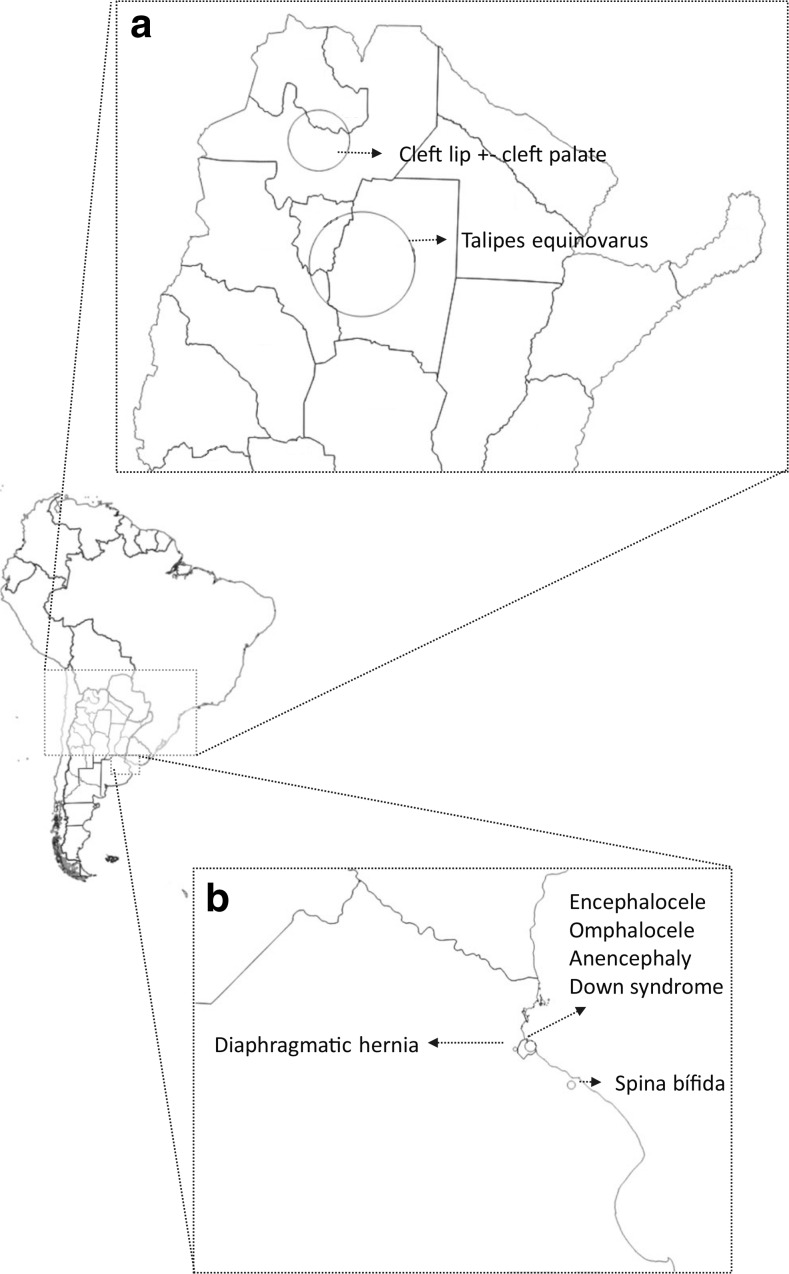
Eight clusters of selected CAs with unusually high birth prevalence were identified: anencephaly, encephalocele, spina bifida, diaphragmatic hernia, talipes equinovarus, omphalocele, CL/P, and Down syndrome (Table 2; Fig. 2). From the eight identified clusters, six are located in the Central region, in the metropolitan area of the City of Buenos Aires. In this study, we included 317,531 births from 67 hospitals of this area, covering 45 % of births of the whole study.
Table 2.
Identified clusters with unusually high birth prevalence in Argentina, 2009–2013
| Congenital anomaly | Centroid coordinates (i) | Radius (ii) | Region (iii) | Cities (iv) | Hospitals (v) | Cases (vi) | Births (vii) | BP (viii) | RR (ix) | LHR (x) | P (xi) | P value for heterogeneity Cochran’s Q test |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diaphragmatic hernia | 34.625181 S, 58.555990 W | 1.88 km | Central region | 2 | 2 | 22 | 15,383 | 14.3 | 4.85 | 16.55 | <0.001 | 0.435 |
| Encephalocele | 34.589078 S, 58.400233 W | 5.32 km | Central region | 1 | 9 | 25 | 50,049 | 5.00 | 4.53 | 16.03 | <0.001 | 0.006 |
| Omphalocele | 34.589078 S, 58.400233 W | 5.09 km | Central region | 1 | 8 | 35 | 42,520 | 8.23 | 4.12 | 20.70 | <0.001 | <0.001 |
| Spina bífida | 34.895851 S, 57.948282 W | 3.80 km | Central region | 1 | 2 | 22 | 10,859 | 20.26 | 3.82 | 12.91 | <0.001 | <0.001 |
| Anencephaly | 34.589078 S, 58.400233 W | 5.09 km | Central region | 1 | 8 | 109 | 42,520 | 25.63 | 2.89 | 41.07 | <0.01 | <0.001 |
| Talipes equinovarus | 27.729279 S, 64.239497 W | 139.4 km | Northwest region | 3 | 3 | 68 | 52,112 | 13.05 | 2.04 | 12.55 | <0.001 | 0.001 |
| Cleft lip with or without cleft palate | 24.772172 S, 65.414777 W | 81.16 km | Northwest region | 2 | 3 | 77 | 41,305 | 18.64 | 1.65 | 7.62 | <0.05 | 0.940 |
| Down syndrome | 34.589078 S, 58.400233 W | 5.32 km | Central region | 1 | 9 | 125 | 50,049 | 24.98 | 1.49 | 8.03 | <0.05 | <0.001 |
(i) Location of the centroid by geographic coordinates; (ii) radius length; (iii) country region, (iv) number of included cities, (v) number of maternity hospitals, (vi) ascertained cases; (vii) examined births in the cluster; (viii) BP: birth prevalence × 10,000 births; (ix) relative risk (RR); (x) logarithm likelihood ratio value (log LHR); (xi) P value using the likelihood ratio test statistics
Fig. 2.
The map of Argentina with detail of the detected clusters
Discussion
CAs prevalence fluctuates in populations over space and time, which can create the appearance of clusters. CAs surveillance systems can serve as important resources when investigating these occurrences because they continuously and systematically monitor CAs prevalence. Clusters’ search is part of the RENAC routine of public health surveillance of CAs. Major CAs are particularly well suited to this type of geographic analyses because the lag time between exposure to environmental and the development of the birth defect outcome is relatively short. This situation minimizes the potential bias introduced when study subjects move during the exposure period and allows for stronger hypotheses about the area-level factors that may cause the disease. Understanding the geographic distribution of diseases with a long latency period (e.g., cancer) may be less informative because study subjects are much more likely to move several times between exposure and diagnosis of the disease. Geographic variation of the prevalence may reflect joint contributions of environmental and genetic factors to the occurrence of the selected birth defects (Root et al. 2009).
The birth prevalence for major CAs was within expected rates (1–3 %). Regarding the prevalence of the selected CAs in the total sample (Table 1), we have previously reported a higher prevalence of gastroschisis and CL/P in the RENAC when compared with Eurocat (Groisman et al. 2013). The higher prevalence of gastroschisis could be attributed to higher prevalence of teenage pregnancy in Argentina (United Nations, 2015) because young maternal age is a well-known risk factor for gastroschisis (Rasmussen et al. 2008). The higher frequency of a CL/P could be explained by the Amerindian component (Poletta et al. 2007; Gili et al. 2015) and the lower socioeconomic level present in some regions of the country, risk factors previously associated with this anomaly (Pawluk et al. 2014).
For Down syndrome, spina bifida, anencephaly, encephalocele, omphalocele, and talipes equinovarus, we found heterogeneity within the clusters. Although we did not find heterogeneity within the congenital diaphragmatic hernia cluster, the hospitals in that cluster are well-known referral centers for prenatally detected cases. Therefore, we consider that these clusters could be influenced by referral bias due to prenatal diagnosis and referral to one or more high complexity hospitals within the clusters.
Regarding Down syndrome, advanced maternal age (greater or equal than 35 years old) is a well-known risk factor for aneuploidy (Meredith et al. 1978). The cluster we found is located in the City of Buenos Aires and it could be associated with a higher maternal age when comparing this city with the rest of the country. The proportion of mothers with age of 35 or more in the City of Buenos Aires is the highest in the country (26.9 % in the City of Buenos Aires versus 15.5 % in the rest of the country) (National Ministry of Health 2014). The ECLAMC previously reported a higher prevalence of Down syndrome located in the same region (Campaña et al. 2010). The finding of this cluster could be used to target educational interventions about advanced maternal age as a risk factor for aneuploidy and other adverse reproductive outcomes.
Most cases with oral clefts have multifactorial origin, although there are some genetic syndromes. Among the teratogenic causes, it has been reported that the immunosuppressant mycophenolate (CL/P), corticosteroids (CP), and lamotrigine (CL/P and CP) are associated with oral clefts. There is strong evidence of increased risk of oral clefts after prenatal exposure to tobacco (Hackshaw et al. 2011). A cluster identified in Texas showed suggestive evidence of an association between elevated radiation levels in tap water and elevated cleft birth prevalence rates (Cech et al. 2007). There is evidence that periconceptional supplementation with multivitamins including folic acid decreases the CL/P risk in the offspring (Johnson and Little 2008). There are several reports of strong geographical differences: prevalence of CL/P is high in parts of Latin America and Asia (China, Japan). The CL/P cluster found in this study is located in the Northwest of Argentina, similar to the previously reported by the ECLAMC (Poletta et al. 2007). In that study, Amerindian ethnic background was found associated to the higher risk. Another geographical analysis from the ECLAMC in Argentina showed a higher prevalence of CL/P in a cluster of low socio-economic level, which included the same region (Pawluk et al. 2010). A case control study from the ECLAMC also showed a higher risk of CL/P in mothers with low socioeconomic level (Pawluk et al. 2014). In brief, the Northwest region presents a population structure, with a higher Amerindian component and socioeconomic differences that could partly explain the high frequency observed. We did not find heterogeneity in this cluster, which could indicate a lower influence of the referral bias.
Two previous studies by the ECLAMC reported a cluster of orofacial clefts in the Patagonia region (Poletta et al. 2007; Campaña et al. 2010), the southern region of Argentina. This cluster was not found in our study. The reason could be that the cluster reported by ECLAMC included part of Chile, the neighboring country, and have an overrepresentation of the western area of Patagonia (the Andes area); while RENAC only includes Argentina and hospitals both from the western and eastern Patagonia. Another explanation could be that the number of births from the Patagonia region in the study period was low, and it may require more births under surveillance to find that cluster.
The prevalence of neural tube defects (NTD) varies depending on geographic region. A high prevalence of NTD is described in Mexico, Ireland, Wales, Egypt, and Lebanon (Gorlin et al. 2001). Hispanics consistently had a higher prevalence of NTD compared with the other racial/ethnic groups. Different risk factors have been identified for the occurrence of NTD, such as maternal obesity, pregestational diabetes, anticonvulsants, low socioeconomic status, multiple births, female sex and, especially, low folic acid intake (Rimoin D et al. 2006). The intake of periconceptional folic acid is a well-known protective factor for NTD. In Argentina, folic acid fortification of wheat flour is compulsory by a national law since 2002 with a dose of 2.2 mg/kg. The ECLAMC previously reported a higher prevalence of spina bifida located in the same region (Campaña et al. 2010). The finding of the spina bifida and encephalocele cluster in Argentina could be used to develop further research, looking for risk factors at the individual level. Also, it is useful to target interventions for the population of that cluster such as providing nutrition education to women of childbearing age that could result in increased dietary folate consumption and greater compliance with vitamin supplementation (Gordon et al. 2003).
The cluster of anencephaly is located in the City of Buenos Aires, the capital city of Argentina, which include hospitals with more infrastructure and technology than the rest of country to receive high-risk pregnancies. Also, for anencephaly, there is a special situation in the City of Buenos Aires because there is a local law that allows elective termination of pregnancy of prenatally detected cases with lethal birth defects from 24 gestational weeks. This probably increases referral of prenatally detected cases of anencephaly to the hospitals of this city (Law number 1044, 2003).
Regarding talipes equinovarus, the etiology is poorly understood, generally considered to be multifactorial. The prevalence reported by different surveillance systems varies considerably (ICBDSR 2012). There is evidence for environmental contribution of smoking (Werler et al. 2015). One of the provinces (Tucumán) partially included in this cluster has a greater than average prevalence of smoking and could benefit with interventions targeted to tobacco control (National Ministry of Health 2011).
Congenital diaphragmatic hernia is defined by the presence of an orifice in the diaphragm, more often the left and posterolateral that permits the herniation of abdominal contents into the thorax. The causes of congenital diaphragmatic hernia are largely unknown. Most cases are isolated, but associated malformations are often observed, sometimes as components of genetic syndromes. Omphalocele is frequently associated with aneuploidy (30 %), with two-thirds of cases, there are other structural anomalies. Among the CAs analyzed, omphalocele had a low frequency. The random variation of low-frequency anomalies could generate an artifactual cluster. Besides the likely influence of the referral bias and the random variation of low frequency anomalies, we could not find a clear explanation for the congenital diaphragmatic hernia and the omphalocele clusters.
Limitations
One limitation of this study is that it tested for unusual patterns within circles, though these patterns may not be circular in nature. We are not able with this test to determine the exact boundaries of the area where the unusual rates occurred.
Since this is an ecological analysis, we cannot say that the whole population living within the cluster area has the same risk for giving birth to an infant with the selected CA. Women have varying levels of risk, which depend on their individual characteristics, behaviors, and family histories. However, the presence of the cluster suggests that a risk factor, of environmental or genetic origin, may exist in that area. We cannot rule out the possibility that some of the spatial variation detected was due to residual spatial confounding. Spatial confounding occurs when there is an uneven spatial distribution of an uncontrolled risk factor.
Biased case ascertainment is always a concern in hospital-based settings when compared with population-based databases. However, in this study, we compared the prenatal diagnosis inside the cluster with the outside to identify those clusters influenced by referral bias. Since RENAC is a hospital-based system, the prevalence was calculated using data from the number of cases (numerator) and births (denominator) in the included hospitals. We lack information about the residence of the mothers of the denominator. Therefore, it is not possible to analyze the data according to maternal residence during pregnancy, which would be more related to environmental exposures.
Although RENAC now covers 42.4 % of births in the country, the coverage during the study period was lower. This lower coverage could influence the results of the study, generating artifactual clusters or preventing detection of real clusters.
Strengths
We used a spatial scan statistic because it does not require a priori knowledge of the geographic location or size of a cluster before conducting the analysis, thereby ameliorating the problem of pre-selection bias.
The analysis included 703,325 births, which makes it a suitable sample for the use of spatial statistics in searching for endemic geographic regions. Data were collected without knowledge of the working hypothesis, which was applied to material stored in the RENAC data base. The RENAC combines two strengths: high quality of diagnosis made by neonatologist following standardized procedures and high coverage.
Maps used in conjunction with statistical tests for clustering can be useful to health researchers for focusing attention on areas for further investigation. These types of maps are useful for showing general patterns of disease and to generate hypotheses regarding the role of environmental, genetic, or lifestyle factors in the etiology of a disease.
Conclusion
The clusters of Down syndrome and CL/P observed in this study match the previously reported clusters by the ECLAMC with a different sample and time period (Poletta et al. 2007; Campaña et al. 2010). These findings support local targeted interventions to lower the prevalence of the CAs and/or further research on the cause of each cluster. The clusters of spina bifida, anencephaly, encephalocele, omphalocele, congenital diaphragmatic hernia, and talipes equinovarus may be influenced by prenatal diagnosis and referral to high complexity hospitals.
Compliance with ethical standards
Conflict of interests
The authors declare that they have no conflict of interest.
Funding
This study was supported by the National Center of Medical Genetics, and the National Program of Rare Diseases and Congenital Anomalies, National Ministry of Health. It was supported by grants from the Agencia Nacional de Promoción Científica y Técnológica, National Ministry of Science and Technology, Buenos Aires, Argentina (PICTO 2011-0147) and the National Ministry of Health (Becas Salud Investiga).
Consent
This article does not contain any studies with human participants or animals performed by any of the authors. This study uses aggregated and anonymous data from a public health surveillance system (RENAC).
References
- Campaña H, Pawluk MS, López Camelo JS y Grupo de Estudio del ECLAMC (2010). Prevalencia al nacimiento de 27 anomalías congénitas seleccionadas, en 7 regiones geográficas de la Argentina. Arch. Argent. pediatr. vol.108 no.5 [DOI] [PubMed]
- Castilla EE, Orioli IM, ECLAMC The Latin-American collaborative study of congenital malformations. Community Genet. 2004;7:76–94. doi: 10.1159/000080776. [DOI] [PubMed] [Google Scholar]
- Castilla EE, Mastroiacovo P, López-Camelo JS, Saldarriaga W, Isaza C, Orioli IM (2008). Sirenomelia and cyclopia cluster in Cali, Colombia. Am J Med Genet A. 15;146A(20):2626-36. [DOI] [PubMed]
- Cech I, Burau KD, Walston J. Spatial distribution of orofacial cleft defect births in Harris County, Texas, 1990 to 1994, and historical evidence for the presence of low-level radioactivity in tap water. South Med J. 2007;100(6):560–569. doi: 10.1097/SMJ.0b013e31802f7d38. [DOI] [PubMed] [Google Scholar]
- Dolk H, Busby A, Armstrong BG, Walls PH (1998). Geographical variation in anophthalmia and microphthalmia in England, 1988-94. BMJ. 3;317(7163):905-9. [DOI] [PMC free article] [PubMed]
- Gili JA, Poletta FA, Pawluk M, Gimenez LG, Campaña H, Castilla E, López-Camelo JS (2015). High birth prevalence rates for congenital anomalies in South American regions. Epidemiology. Sep;26(5) [DOI] [PubMed]
- Gordon TE, Leeth EA, Nowinski CJ, MacGregor SN, Kambich M, Silver RK. Geographic and temporal analysis of folate-sensitive fetal malformations. J Soc Gynecol Investig. 2003;10(5):298–301. doi: 10.1016/S1071-5576(03)00086-8. [DOI] [PubMed] [Google Scholar]
- Gorlin RJ, Cohen MM, Hennekam R (2001). Syndromes of the head and the neck, Oxford University Press
- Groisman B, Bidondo MP, Barbero P, Gili JA, Liascovich R, Task Force RENAC. RENAC: National Registry of Congenital Anomalies of Argentina. Arch Argent Pediatr. 2013;111(6):484–494. doi: 10.5546/aap.2013.eng.484. [DOI] [PubMed] [Google Scholar]
- Hackshaw A, Rodeck C, Boniface S. Maternal smoking in pregnancy and birth defects: a systematic review based on 173,687 malformed cases and 11.7 million controls. Hum Reprod Update. 2011;17(5):589–604. doi: 10.1093/humupd/dmr022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICBDSR - International Clearinghouse Centre for Birth Defects (2014). Annual reports: 2012. Available at: http://www.icbdsr.org/filebank/documents/ar2005/Report2012.pdf
- INDEC (2010). National Institute for Statistics and Census. National census 2010. www.indec.gov.ar
- Johnson CY, Little J. Folate intake, markers of folate status and oral clefts: is the evidence converging? Int J Epidemiol. 2008;37(5):1041–1058. doi: 10.1093/ije/dyn098. [DOI] [PubMed] [Google Scholar]
- Kulldorff M, Athas WF, Feurer EJ, Miller BA, Key Sep CR. Evaluating cluster alarms: a space-time scan statistic and brain cancer in Los Alamos, New Mexico. Am J Public Health. 1998;88:1377–1380. doi: 10.2105/AJPH.88.9.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulldorff M, Nagarwalla N (1995). Spatial disease clusters: detection and inference. Stat Med. 30;14(8):799-810. [DOI] [PubMed]
- Law number 1044 (2003) of the Autonomous City of Buenos Aires. Available at www.cedom.gov.ar/es/legislacion/normas/leyes/ley1044.html
- Meredith R, Taylor AI, Ansi FM (1978). High risk of Down’s syndrome at advanced maternal age. Lancet. 11;1(8063):564-5. [DOI] [PubMed]
- Pawluk MS, Hebe C, López Camelo Jorge S. Agregados geográficos, condición socioeconómica y prevalencia de anomalías congénitas en Argentina. J Basic Appl Gen. 2010;21(1):49–59. [Google Scholar]
- Pawluk MS, Campaña H, Gili JA, Comas B, Giménez LG, Villalba MI, Scala SC, Poletta FA, López Camelo JS. Adverse social determinants and risk for congenital anomalies. Arch Argent Pediatr. 2014;112(3):215–223. doi: 10.5546/aap.2014.eng.215. [DOI] [PubMed] [Google Scholar]
- Poletta FA, Castilla EE, Orioli IM, Lopez-Camelo JS. (2007) Regional analysis on the occurrence of oral clefts in South America. Am J Med Genet A. 15;143A(24):3216-27. [DOI] [PubMed]
- Rasmussen SA, Frías JL. Non-genetic risk factors for gastroschisis (2008). Am J Med Genet C Semin Med Genet. 15;148C(3):199-212. [DOI] [PubMed]
- Rimoin D, Connor JM, Pyeritz R, Korf B (2006), Emery and Rimoin’s principles and practice of medical genetics, Elsevier.
- Root ED, Meyer RE, Emch M. Socioeconomic context and gastroschisis: exploring associations at various geographic scales. Soc Sci Med. 2011;72(4):625–633. doi: 10.1016/j.socscimed.2010.11.025. [DOI] [PubMed] [Google Scholar]
- Root ED, Meyer RE, Emch ME. Evidence of localized clustering of gastroschisis births in North Carolina, 1999–2004. Soc Sci Med. 2009;68(8):1361–1367. doi: 10.1016/j.socscimed.2009.01.034. [DOI] [PubMed] [Google Scholar]
- UN Statistics Division (2015) Live births by age of mother and sex of child bred, general and age-specific fertility rates: latest available year, 2000–2009. Available at http://unstats.un.org/unsd/demographic/products/dyb/dyb2009-2010.htm
- National Ministry of health (2014), Vital Statistics. Dirección de Estadísticas e Información de Salud (DEIS), Estadísticas Vitales, Información Básica Año 2014.
- National Ministry of Health of Argentina (2011), Second national risk factors survey.
- Werler MM, Yazdy MM, Kasser JR, Mahan ST, Meyer RE, Anderka M, Druschel CM, Mitchell AA. Maternal cigarette, alcohol, and coffee consumption in relation to risk of clubfoot. Paediatr Perinat Epidemiol. 2015;29(1):3–10. doi: 10.1111/ppe.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (1996) Control of hereditary diseases. Report of a WHO Scientific Group. WHO Technical Report Series 865 [PubMed]
- Yuan P, Qiao L, Dai L, Wang YP, Zhou GX, Han Y, Liu XX, Zhang X, Cao Y, Liang J, Zhu J (2009). Spatial distribution patterns of anorectal atresia/stenosis in China: use of two-dimensional graph-theoretical clustering. World J Gastroenterol. 14;15(22):2787-93. [DOI] [PMC free article] [PubMed]