Abstract
Genomic medicine has revolutionized disease risk identification and subsequent risk reduction interventions. Skin cancer risk genomic feedback is a promising vehicle to raise awareness and protective behaviors in the general population, including Hispanics who are largely unaware of their risks. Yet, personalized genomics currently has limited reach. This study is the initial phase of a randomized controlled trial investigating the personal utility and reach of genomic testing and feedback for melanoma. Semi-structured cognitive interviews (N = 28), stratified across education level, were conducted to assess the comprehension and acceptability of translated skin cancer genomic risk education materials with Spanish-speaking Hispanic primary care patients. Overall, materials were comprehensible and acceptable with 33 of 246 terms/concepts identified as difficult. Common problems included translation challenges (e.g., peeling from sunburn), ambiguous concepts (e.g., healthcare system), and problematic terms (e.g., risk version). Aiming to expand the reach of genomic medicine across subpopulations that may benefit from it, necessary modifications were made to education materials to improve comprehensibility, acceptability, and cultural relevance.
Keywords: Cognitive interviews, Melanoma, Genetic testing, MC1R, Hispanics
Introduction
There is great potential for genomic medicine to revolutionize the personalization of disease risk and to optimize the adoption of clinical and behavioral recommendations designed to promote health (Graves et al. 2014). Despite this promise, genetic testing, whether offered directly to consumers or within a clinical context, has been shown to have limited reach and inequitable access (Green and Guyer 2011; Hindorff et al. 2009; Weitzel et al. 2011). Beneficiaries of learning personalized genetic information have traditionally been non-Hispanic white individuals at higher socioeconomic and education levels, with insurance coverage, and who have a high level of health literacy (Bloss et al. 2010). Members of racial and ethnic minority groups as well as those with lower education levels also stand to benefit from genomic technologies but are less likely to participate in genomic research or undergo genetic testing when offered (Bloss et al. 2010; Hensley Alford et al. 2011; Pagan et al. 2009; Suther and Kiros 2009). Yet, studies have also shown that members of underserved populations report great interest in genomics especially when information is presented in an accessible and relevant way to their sociocultural and behavioral characteristics (Kaphingst et al. 2015; Petruccio et al. 2008; Sussner et al. 2011; Torres et al. 2014). If genomic medicine is to make a significant difference in healthcare delivery and patient outcomes for all, it is critical that its efforts reach individuals who are known to have limited access to healthcare including those with low literacy and who are non-English speaking (Kaphingst and Goodman 2016).
In line with this vision, in 2015, the National Academy of Sciences, Engineering and Medicine convened experts in the field of genomics to a workshop on applying an implementation science approach to genomic medicine. Of critical importance was the discourse involving the need to address disparities in genomic research. Members stated: “In order to ensure equitable access to genomic medicine, greater efforts will be required to address health inequities across low income and minority groups. […] Genomics will only achieve its full potential to improve health when the advances it engenders become accessible to all.” (National Academy of Sciences 2016). Population-based efforts that maximize diversity and recruit outside traditional academic medical centers and beyond highly educated, non-Hispanic whites, and health conscious volunteers are needed to widen the reach of personal genomics in “real-world” settings. Accordingly, there is an emerging research base regarding genetic attitudes and preferences in underrepresented communities. In general, minority populations have been interested in genetic information but are less likely to access and use genetic testing (Halbert et al. 2012; Hamilton et al. 2016; Kaphingst et al. 2015). Individual (e.g., awareness, knowledge, attitudes, and beliefs) and system-level (e.g., health insurance, misuse of information, discrimination, and mistrust) factors contribute to this disparity (Kaphingst and Goodman 2016). Yet, recent research conducted with Hispanics suggest that when barriers to testing are removed (i.e., access and cost), a large proportion of them are very likely to pursue genetic risk assessment and testing and are also willing to share biospecimens for research purposes (Komenaka et al. 2016; Nodora et al. 2016). Consequently, culturally relevant outreach approaches that eliminate individual and systemic barriers to genetic risk assessment and testing are needed to bring genomics into diverse communities.
Efforts to ensure personalized genomics reach diverse communities must be linguistically appropriate and relevant. A first step to achieving this goal involves linguistic translation and transcreation. More broadly, health promotion messages are more effective when they undergo a process of transcreation and are made available in the target audience’s language (Wells et al. 2013). Transcreation goes beyond the linguistic translation of materials; its purpose is to conceptually recreate the text to meet the informational needs of the target population by including culturally relevant terminology, images, or themes (Simmons et al. 2011; Solomon et al. 2005). Following translation and transcreation, a critically important second step to conducting effective population-based science is to systematically test the comprehensibility and acceptability of educational materials with the target population. Cognitive interviewing is the “gold standard” procedure for appraising the comprehensibility and acceptability of newly developed content used in research (Willis 2005). The procedure allows patients to have an active voice in research by explicitly eliciting concerns and/or suggestions about the materials while assessing sociocultural relevance. Genomic medicine efforts can greatly benefit from having educational materials that are comprehensible and acceptable to a diverse audience, making cognitive interviews a particularly useful methodology to evaluate understanding of genomic information in minority populations.
The present study describes the initial phase of a randomized controlled trial (NIH R01-CA181241)—The Skin Health Online for Melanoma: Better Risk Assessment (SOMBRA) study, which is investigating the personal utility and reach of genetic testing (melanocortin-1 receptor (MC1R)) for melanoma risk in Albuquerque, New Mexico, a city with a large proportion of Hispanics (see Hay et al., under review, 2016 for study design). Given accumulating evidence for common MC1R melanoma risk-increasing variants in individuals with varied skin types (Udayakumar and Tsao 2009), MC1R testing may have utility in raising melanoma risk awareness and risk reduction for a large proportion of the population, including Hispanics who are largely unaware of their risks (Santiago-Rivas and Wang 2014) and who commonly present for diagnosis and treatment with more advanced disease and poorer prognosis (Hu et al. 2009). Briefly, patients (English or Spanish-speaking) unselected for risk status are approached and randomized to an offer of online-delivered presentation of the risks and benefits of MC1R testing or wait-list control. For this initial phase of the trial, our primary objective was to evaluate the comprehension and acceptability of Spanish-translated skin cancer genomic risk education materials to be used in the trial.
Methods
Study design and goals
Semi-structured cognitive interviews were conducted to evaluate participants’ comprehension and the acceptability of SOMBRA skin cancer genomic risk education materials. Our intent was to ensure the cultural relevance of our materials in the population of interest: Spanish-speaking New Mexicans (Miller 2003; Schwarz et al. 2010). Our rigorous methodology accounts for the diverse influences found in the Albuquerque Spanish vernacular and documents terms that are difficult to understand and/or are culturally inappropriate.
Participants and eligibility
Patients at a southwest urban and university-affiliated primary care clinic in Albuquerque, NM were approached by project assistants (PAs) to assess study interest and eligibility. Patients were eligible for the study if they (a) spoke Spanish as their preferred language, (b) reported being fluent in Spanish, (c) were at least 18 years old, (d) had been a patient of the clinic for at least 2 years, and (e) were assigned to a primary care provider. Reasons for ineligibility were recorded. All eligible participants were consented and assigned a version of study materials to review alongside a PA. Participants were stratified by education level (less than high school vs. high school/equivalent or higher) and reviewed one of three versions of materials (Fig. 1).
Fig. 1.
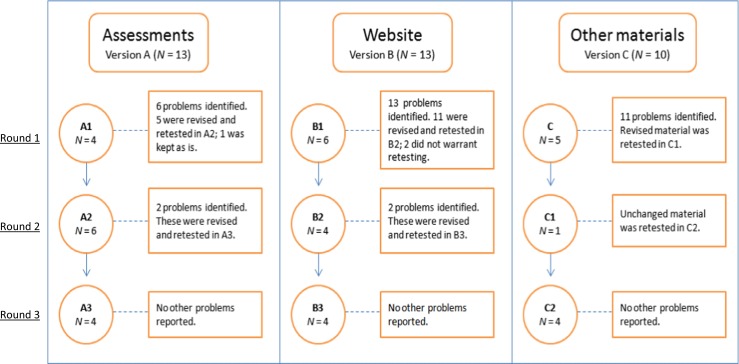
Cognitive interviews’ participant flow and identified problems. A total of 28 individual participants completed the cognitive interview phase; 13 individual participants completed versions A and B, respectively. To minimize patients’ time commitment, the material for versions A and B was split into two versions. For these versions, the number of participants in each round differ from the total number because one participant completed both A1 and A2, and another participant completed both B1 and B2. The same four participants completed versions A3, B3, and C2. A problem was defined as an issue identified by at least one participant, a project assistant, or the expert panel
Skin cancer genomic risk education materials
Our skin cancer genomic risk education materials comprised all materials participants encountered in SOMBRA. These covered (1) the baseline and follow-up questionnaires which contained validated and reliable instruments assessing participants attitudes and beliefs concerning skin cancer genetic risk, (2) the content for the SOMBRA website which included information on skin cancer and MC1R risk variants as well as ways to reduce one’s risk, and (3) all other miscellaneous study materials, including the skin cancer risk feedback brochure, letters to participants, flyers and study advertisements, and instructions for how to provide and return their saliva sample.
Translation approach
Spanish language translation efforts have traditionally relied on word-for-word, literal translations often sacrificing the overall intent of the translated item (Harkness et al. 2010). Beyond the translation process, it is recommended that several steps be taken involving empirical evaluation and pretesting of the translated materials to ensure quality and cultural relevance (Harkness et al. 2003). These steps are as follows: translation, review, adjudication, pretesting, and documentation (TRAPD) (Berrigan et al. 2010; Harkness et al. 2010). Following TRAPD guidelines, we utilized a team-based approach and multistep, iterative process to translation that addressed sociocultural as well as linguistic acceptability in our population of interest. First, the English-language skin cancer genomic risk education materials were translated into Spanish by a team at the Memorial Sloan Kettering Cancer Center (MSKCC) Linguistic and Cultural Competence Center, who also provided certificates of authenticity. Second, the target translations in conjunction with the sources (English) underwent rigorous review and adjudication by bilingual project staff. This included an iterative process where professional translations were revised by a bilingual project staff. Issues or discrepancies with the translated material were raised and discussed with the translation team. Staff discussed modifications to translated materials and made agreed-upon changes. Terms for which there was disagreement were flagged and turned into scripted probes during cognitive interviews. Third, we pretested the comprehensibility and acceptability of the newly translated items via cognitive interviewing with 28 Spanish-speaking primary care patients. Knowing that our initial translations were conducted in New York City, we took the essential step to cognitively test our materials in Albuquerque, our population setting of interest, to account for regional variability in Spanish. Lastly, we documented participants’ responses on paper and then transferred data into REDCap, an electronic data-reporting platform, and analyzed contents through in-depth qualitative data analysis.
Interviewer training
Prior to study initiation, PAs attended a 2-day, scenario-based training led by co-authors with expertise in qualitative methodology (VMR, JLH, and KZ). The training focused on how to successfully recruit and interview participants as well as how to apply probes during interviews. PAs were Master’s level research associates, bilingual in Spanish and English, and with extensive experience in conducting interviews with our population of interest. PAs attended weekly meetings with the associate director of the UNM Comprehensive Cancer Center’s Behavioral Measurement and Population Sciences Shared Resource as well as weekly meetings to discuss interviewing issues and ongoing recruitment.
Overall procedures
PAs approached patients waiting for their doctor’s appointment using a standardized script. Patients willing and eligible to participate completed the cognitive interview, which on average lasted approximately 45 min. Interviews were conducted until each of the items was evaluated by at least two participants. Each PA kept detailed notes on responses during the interviews. After completion, participants received a $20 gift card as compensation for their time and valued contributions. All study procedures and materials were approved by the University of New Mexico (UNM) institutional review board.
Participants reviewed the materials and were asked two standard probes for each item or section reviewed. We first asked participants whether the item/section was difficult to understand (¿Difícil de entender?). An affirmative answer to this first probe triggered a second probe that gave participants the option of providing additional comments, suggestions for alternate terms or phrasing, or any other feedback if they so desired (¿Sugerencias?). In addition to these standard probes, we used a combination of conditional and scripted probes during interviews (Willis 2005). PAs were trained to employ conditional probes in reaction to any hesitations, spontaneous patient comments about items, or non-verbal expressions signaling meaningful responses (e.g., confusion, uncertainty, and offense). These conditional probes were semi-scripted with interviewers having access to a conditional probe guide to facilitate interviews (Table 1). Scripted probes, however, were administered systematically to all participants. These were developed a priori to elicit direct feedback on items the translation team identified as potentially difficult. Recruitment and data collection issues were discussed in weekly team conference calls.
Table 1.
Study probes
| Standard probes | |||
| ¿Difícil de entender? | Difficult to understand? | ||
| ¿Sugerencias? | Suggestions? | ||
| Scripted probes | |||
| ¿Qué significa para usted la frase “ni en acuerdo ni en desacuerdo” de la manera en que se usa en ésta pregunta? | What does “neither agree nor disagree” mean to you as it is used in this question? | ||
| ¿Qué significa para usted la palabra “descamación” de la manera en que se usa en ésta pregunta? | What does “descamación” mean to you as it is used in this question? | ||
| ¿Cuál sería un mejor término o palabra? | Can you think of a better term or word? | ||
| ¿Qué significa para usted la palabra “descarapela” de la manera en que se usa en ésta pregunta? | What does “descarapela” mean to you as it is used in this question? | ||
| ¿Qué significa para usted la palabra “archivo” de la manera en que se usa en ésta pregunta? | What does “archivo” mean to you as it is used in this question? | ||
| ¿Cuál sería un mejor término o palabra? | What would be a better term or word? | ||
| Conditional probes | |||
| Condition | Behavioral indicators | Spanish probe | English translation |
| Uncertainty | |||
| Non-verbal | Non-verbal cues: e.g., sighing, shrug of shoulders, eye rolls, or other indications of frustration. | Me parece que está un poco inseguro (frustrado) con esta pregunta. ¿Me podría decir por qué? | You seem to be somewhat uncertain (frustrated) with this question. If so, can you tell me why? |
| Uses explicit cues: e.g., “um” and “ah,” | |||
| Answers after a period of silence. | Le tomó un poco de tiempo el contestar la pregunta. ¿En qué estaba pensando? | You took a little while to answer that question. What were you thinking about? | |
| Verbal | Changes their answer. | ¿Qué lo llevó a cambiar su contestación? | What caused you to change your answer? |
| Cannot answer or does not know the answer. | ¿Qué estaba pasando por su mente cuando trataba de contestar la pregunta? | What was going through your mind as you tried to answer the question? | |
| Requests information instead of providing an answer. | ¿Si no estuviera aquí para contestarle, que usted hubiese pensado que significaba? | If I were not available to answer, what would you decide it means? | |
| ¿Cree que tiene otros significados? | Are there different things you think it might mean? What sorts of things? | ||
| ¿Cómo qué? | |||
| Misunderstanding | |||
| Verbal | Verbal report implies misunderstanding of the term; e.g., off topic and irrelevant answer | Clarifique la comprención del término usado. Si parece que el participante malentendió la palabra, explore el término. | Clarify respondent’s understanding of the particular term used. If the respondent appeared to misunderstand a word, probe the term. |
| ¿Qué significa la palabra “xyz” para usted? | What does “xyz” mean to you? | ||
| Verbal report implies that the concept is ambiguous or confusing; e.g., “I am not sure what this means;” “I do not know what you are asking” | Explique lo que significan la palabra o término usado y pregunte: | Explain what is meant by the term/concept and ask: | |
| ¿Puede pensar en alguna otra palabra que sea mejor o más entendible? | Can you think of another word/phrase that would be better or clearer? | ||
| ¿Cómo usted diría “xyz” en sus propias palabras? | How would you say “xyz” in your own words? | ||
| Verbal report indicates that the participant has answered the question rather than letting the PA know if it is not clear or does not make sense. | Recuerde que lo que necesitamos es que nos diga si la palabra o frase no está clara o no le hace sentido. | Remember that we need your advice on what words or phrases are not clear. | |
Cognitive interviews procedures
Given the large amount of educational materials needing cognitive testing, we chose to divide the material into smaller versions to limit participant burden. The material included in these versions was sub-divided into smaller sections which we call items. As seen in Fig. 1, participants were assigned to review one of three versions: version A included individual items from the baseline and follow-up assessments (92 items); version B included the material to be presented on the SOMBRA website (121 items); and version C included miscellaneous materials, such as the skin cancer risk feedback brochure, letters to participants, instructions to provide saliva sample, and study advertisements (33 items). To keep interviews to approximately 45 min, a decision was made to further split the material presented in versions A and B into two sub-versions (e.g., A1 and A2) after the first two participants completed procedures. Three rounds of cognitive interviews were performed. Items that had reached saturation (i.e., no additional problems or issues identified after at least two participants viewed them and the expert panel agreed saturation was reached were discontinued from further retesting; Willis 2005). For the third and final iterative round of interviews, the same four participants reviewed a combined set of materials which included revised items needing retesting from all three versions (i.e., A3, B3, and C2).
Analytic approach
Our analytic approach went beyond linguistic translation to evaluate the comprehensibility and acceptability of materials through in-depth cognitive interviews. Guided by our prior experience conducting genetics research with low literacy populations (Drake et al. 2016; Kaphingst et al. 2015) as well as Spanish-speakers (Hay et al. 2016) decisions were made to either modify problematic terms or re-test them “as is.” Two parallel processes triggered modifications of study materials: an expert opinion panel and participant feedback gathered during interviews. At the mid-point of cognitive interviews, a consensus meeting was held with a multidisciplinary team composed of experts in qualitative data analysis (VMR and JLH), linguistic translation (CJG), health and genetic literacy (KK), anthropology (KH), and the SOMBRA study (ER and KZ). All items were reviewed with particular attention given to items for which two or more patients reported problems, considering the specific nature of the problems and characteristics of the participant (e.g., education level). This information was used to determine whether revisions were needed based on participant feedback and to draft a revised version of the item to be used in subsequent testing. Potential problems raised by participants, PAs, or the expert panel were evaluated for revision. This approach was chosen based on published guidance (Willis 2005; Willis et al. 2008), which asserts that even a single problem can dictate the need for adaptation. The study was considered complete when no further information warranting adaptation or additional testing was generated for any item/section.
Detailed field notes written during and after interviews were entered directly into REDCap. Documentation from REDCap was used to prepare structured reports of each interview. Each participant report included (1) participant demographics (i.e., education level and gender); (2) full item-by-item results; (3) interviewer comments about participant body language or questions raised during the interview; and (4) a description of problems related to each item or section. Section-level summaries were created for each version of the skin cancer genomic risk education materials based on aggregate data from all interview reports. These structured summaries, or tally tables, documented the frequency of problems experienced by participants at the item/section level as well as the specific nature of those problems, the education level of the participants experiencing those problems, and the final resolution.
Results
Study participants
From August to November 2015, a total of 68 primary care patients were approached by PAs to assess study interest and eligibility. Twenty-two (32%) patients refused participation and 18 (27%) were ineligible. Reasons for ineligibility included the following: Spanish not being their preferred language (n = 4), not fluent in Spanish (n = 1), not 18 years or older (n = 1), and not being a patient of the clinic (n = 12). A total of 28 (41%) patients were interested and eligible to participate and enrolled in the study. The sample was largely female (n = 20; 71%) with an average age of 61 years (SD = 12.7). We met our stratification goal with a little over half of participants (n = 15; 57%) reporting a lower level of education (less than high school) and 13 patients (43%) reporting a higher education level (high school/equivalent or higher). All but one participant reported being of Hispanic, Latino, or Spanish origin (96%) with the majority self-identifying as Mexican (n = 16), followed by Hispanic (n = 6), Mexican-American (n = 2), Chicano/a (n = 1), Latino/a (n = 1), and Cuban (n = 1). The remaining participant did not answer the question about ethnicity but racially self-identified as white.
Cognitive interviews findings
Any issue raised by at least one participant, a PA, or the expert panel was evaluated for revision and labeled as a problem. Problems included but were not limited to problematic terms, confusing response choices or procedures, and ambiguous concepts (Table 2). Overall, participants comprehended the material well and reported few problems. Across versions, a total of 33 problems (out of 246 items) were identified (Table 3).
Table 2.
Number of identified problems by translation target
| Problem types | Number of problems |
|---|---|
| Translation problem | 10 |
| Interviewer difficulty | 0 |
| Problematic term | 9 |
| Ambiguous concept | 11 |
| Overly complex question | 2 |
| Double barreled question | 0 |
| Questionnaire effects over multiple items | 0 |
| Response selection | 1 |
| Total no. of problems | 33 |
Table 3.
Identified problems and resolutions
| Original version | Modified version | Reason(s) for the modification/unmodification | ||
|---|---|---|---|---|
| English | Spanish | English | Spanish | |
| Sun exposure | Exposición solar | Being in the sun | Estar en el sol | The term “sun exposure” was changed to improve comprehensibility of the concept. |
| Sunglasses | Gafas de sol | Sunglasses | Lentes de sol | The word “gafas” was substituted for “lentes” as it is a more comprehensible term. |
| Peeling | Descamación | Peeling | Descarapelar | The term “descamación” was changed to improve comprehensibility of the term. |
| Healthcare system | El sistema de salud | Healthcare system (e.g., medical clinics, doctors, nurses, dentists, and many other health professionals) | El sistema de salud (ej. clínicas de salud, doctores, médicos, enfermeras, dentistas, y muchos otros profesionales de la salud) | To clarify that the healthcare systems include a variety of healthcare professionals. |
| Health care providers | Proveedores de atención médica | Health care providers (e.g., doctors, nurses, physician assistants) | Proveedores de atención médica (ej. doctores, enfermeras, médicos) | To clarify that healthcare providers include doctors, physician assistants, and/or nurses. |
| Risk version | Versión de riesgo | Risk type | Tipo de riesgo | The term was revised by expert opinion panel to improve comprehensibility of the concept. |
| Kit | Kit | Kit | Kit (equipo de materiales) | The parenthetical phrase was included to provide additional context for the term. |
| Click | Pulse (haga clic) | Click | Haga clic | The word “pulse” was removed and a more acceptable term “haga clic” was kept. |
| Remove | Extraiga | Remove | Saque | The word “extraiga” was substituted for “saque” as it is a more comprehensible term for patients. |
| Family history | Historial familiar | Health of your relatives (family history) […]. By family we mean your parents, siblings, and grandparents. | Historial médico de su familia […]. Al decir familia nos referimos a sus padres, hermanos/as, o abuelos. | To clarify that the family include parents, siblings, and grandparents. |
| Response anchor: ‘Neither agree nor disagree’ | ‘Ni en acuerdo ni en desacuerdo’ | ‘Neither agree nor disagree (I do not agree but I am also not in disagreement)’ | ‘Ni en acuerdo ni en desacuerdo (No estoy en acuerdo pero tampoco en desacuerdo)’ | Added prompt in parenthesis for PAs to read if participant shows signs of confusion. |
| Typically | Típicamente | – | – | Given its commonality in the Spanish vernacular, this term was kept unchanged. |
| Gender | Género | Gender (man or woman) | Género (hombre o mujer) | The parenthetical phrase was included to provide additional context for the term. |
| How much did finding out your test results make you feel…? | ¿Qué tan ____ se sintió al saber de los resultados de las pruebas? | – | – | Added PA prompt to read question stem for each response item. |
| • Nervous | • Nervioso/a | |||
| • Relieved, etc. | • Aliviado/a, ect. | |||
| During the conversations that you had about skin cancer risk, did you talk about …? | Durante la conversación que tuvo sobre el riesgo de cáncer de la piel, ¿habló de…? | - | - | Added PA prompt to read question stem for each response item. |
| • Who had skin cancer | • Quién tenia cancer de la piel en su familia | |||
| • Your own risk of getting skin cancer, etc. | • Su propio riesgo de desarrollar cáncer de la piel, ect. | |||
| Skin cancer | Cáncer de piel | Skin cancer | Cáncer de la piel | The term “cancer de piel” was changed to a more accepted term by our target population. |
| Because | Puesto | Because | Porque | The term “puesto” was changed to a more accepted term by our target population. |
| Change your mind | Cambia de parecer | Change your mind | Cambia de opinión | The term “cambia de parecer” was changed to a more accepted term by our target population. |
| Response anchors: “Very unlikely” to “Very likely” | “Muy improbable” a “muy probable” | – | – | The response anchors were kept in their original form as they were comprehensible upon retesting. |
| Logout | Cerrar sesión | – | – | Term remained unchanged as it is a commonly used technical term among internet users, with no other viable translation. |
| Home | Inicio | – | – | Term remained unchanged as it is a commonly used technical term among internet users, with no other viable translation. |
| Gene | Gen | – | – | The definition for the term “gene” offered in the website glossary was revised to increase comprehensibility. |
| List | Enumeran | – | – | Given its commonality in the Spanish vernacular, this term was kept unchanged. |
| DNA | ADN | – | – | The definition for the term “DNA” offered in the website glossary was revised to increase comprehensibility. |
| MC1R | MC1R | – | – | The definition for the term “MC1R” was added to the website glossary to increase comprehensibility. |
| Supplements | Suplementos | – | – | The term “suplementos” was removed to improve comprehensibility of the material. |
| Bubbled | Acolchado (burbuja) | – | – | Given its commonality in the Spanish vernacular, this term was kept unchanged. |
A total of 13 participants reviewed version A (assessments). Six problems were identified by participants during A1 data collection. Of these, all but one was revised and re-tested in A2. Problematic terms included “exposición solar” (sun exposure) and “descamación” (peeling from sunburn) with participants not understanding the terms or suggesting different wording. These terms were changed to “estar en el sol” (being in the sun) and “descarapelar” (peeling from sunburn), respectively. Of note, our translated term for sun exposure was correctly translated and perfectly equivalent; however, lack of understanding may have been due to low literacy or regional variation in the use of Spanish words. The one problem that was not retested was a term that only one participant did not understand (típicamente or typically). Due to the commonality of this term in the Spanish vernacular, the expert panel decided to keep this item unchanged. During the second round of interviews (A2), the revised items were understood by participants; however, two other problems related to procedural issues were identified by PAs. For example, PAs noted that even though two participants reported understanding the phrasing of a survey item assessing their communication with others about their skin cancer risk, they did not understand the structure of the item; specifically, the participants did not understand that there were different options or responses that could be chosen to answer the item. In response to this feedback, we added prompts to remind the PAs to re-read the question stem before each possible answer choice. After this change was made, no further difficulties were reported (A3).
Thirteen participants completed cognitive interviews for version B (website). Although the website content was, for the most part, comprehensible, a total of 13 problems were identified by participants or the expert panel in the first round of interviews (B1). Problematic terms were related to (a) standard elements typically found on a website, for example, the terms “inicio” (home) and “cerrar sesión” (logout); (b) ambiguity about certain concepts, such as what was meant by “proveedores de atención” (healthcare providers) and “kit” (kit); and (c) Likert scale response anchors including those from “muy improbable–muy probable” (very unlikely to very likely). In some cases, the wording was unchanged but was retested to confirm comprehension (i.e., home/logout and very likely/unlikely). For items that represented an ambiguous concept, we added a parenthetical explanation next to the original word or phrase. For example, for “healthcare providers,” we added the following clarifying statement: “(doctors, nurses, and physician assistants).” Two remaining items were deemed to not warrant retesting due to minimal difficulties with comprehension (“pulse” (click) and “enumeran” (list)). Participants in this round also identified the term sun exposure as problematic, resulting in the same change as described above. Following modifications, B2 participants reported good understanding of the material; however, to maximize comprehension, our expert panel agreed to make changes to the definitions and explanations of two genetic terms: genes and DNA. The original definition for the term gene, “A section of DNA that carries information about how a feature of a living thing looks and works, such as eye color or hair color in people.”, was modified to “Genes are short sections of DNA that affect how a living thing looks and works. Some genes affect physical traits like eye color. Others affect the chances of getting diseases like cancer.” As for DNA, the original definition stated: “The material that carries information about how a living thing will look and how it will work.” This was changed to “DNA is the material in living things that carries information about how they look and work. There is DNA in all parts of your body, including your saliva.” No further issues or difficulties were identified (B3).
Lastly, ten participants completed cognitive interviews for version C (miscellaneous materials). Eleven problems were identified by participants or the expert panel, and these were either revised for further testing (e.g., “extraiga” changed to “saque” meaning to remove) or retested in their original form (e.g., “acolchado” meaning bubbled). Recurring problems noted in previous version materials were also identified here: “sun exposure,” “genes”, and “kit.” To improve comprehension of genetic material for this population, the term risk version was changed to “risk type” and the gene MC1R was added to the website glossary. The most common translation problem encountered by these participants was the term for sun glasses originally translated as “gafas de sol.” Although participants understood the concept, four out of five patients suggested modifying the term to a more familiar one: “lentes de sol.” Further clarification was provided in the form of parenthetical explanations for the following terms: “historial familiar” (family history) and “proveedor de atención primaria” (primary care provider). Following these modifications, no additional problems or difficulties were reported.
Discussion
Translating genetic information to diverse populations raises significant but addressable challenges. On the one hand, research has shown that racial and ethnic minority groups vary in their understanding and linguistic elaboration of genetic concepts (Kaphingst and Goodman 2016). As a result, there is a great need for the development of low literacy, multi-lingual skin cancer genomic risk education materials. On the other hand, moving from a high resource, time intensive genetic counseling approach to greater reliance on other more generalizable channels for genomic information dissemination (e.g., the Internet), may be a promising vehicle to make genomics information more accessible. In line with the patient-centered medicine movement and its implications for patients’ engagement and activation toward prevention and treatment, it is essential that advances in genomics reach underserved populations to minimize widening health disparities. While the potential is great, the challenge is to develop, confirm, and validate such efforts with detailed input from the target population.
Overall, the translation and transcreation approach used to develop the Spanish skin cancer genomic risk education materials for SOMBRA was successful as demonstrated by a minimal number of problems identified through cognitive interviews. Feedback gathered from participants, PAs, and the expert panel led to important adaptations, however, that improved the comprehensibility and cultural relevance of our materials. Participants encountered some difficulty with various translations regarding the American healthcare jargon (i.e., healthcare provider and healthcare system) as well as various genetic concepts (i.e., gene, DNA, and risk version). The most common problem encountered was related to concepts that were considered ambiguous in some way—that is, when the participant appeared confused or not entirely sure what was meant by a term. We addressed these types of problems by providing further explanation in the form of a parenthesis immediately following the term or by adding a prompt for our interviewers to provide verbal clarification. Based on recommendations by our expert panel, we also added these ambiguous terms to our website glossary (e.g., gene and DNA) in order to have an additional place where participants could get more information. Another type of problem commonly identified during interviews was “problematic terms.” These were terms that were not comprehensible as used in context or terms that were too complex for some participants. For example, the term “risk version (versión de riesgo)” as it pertains to genetic risk was found to be unclear and therefore it was modified. These types of problems were discussed extensively by our expert panel and modifications were made to simplify the language and improve comprehension.
Another common problem involved the actual Spanish translation of terms. Basic Spanish is typically understood across regions, yet there are regional idioms and expressions that are specific to certain sub-ethnic groups or individuals living in a particular geographical area (Bills and Vigil 2008). Accordingly, participants in our study identified several terms or phrases, such as “peeling (descamación)” and “sunglasses (gafas de sol),” for which the translation was not frequently used or accepted in the Albuquerque Spanish vernacular. Participants suggested different wording (e.g., “descarapelar” and “lentes de sol”), which in turn improved acceptability and cultural relevance of the terms. Of note, most of our translated materials were comprehensible and understandable to our participants. However, it is critical that research efforts with Spanish-speaking participants address the linguistic regionalisms of the target population as these are prevalent and vital to maintaining cultural relevance as well as ensuring understanding of healthcare jargon. Addressing the comprehensibility of the colloquial language used to explain difficult concepts, like genetic terms, taking into account regional challenges in Spanish is a promising vehicle through which genetics education can be made readily accessible.
Lessons learned and recommendations
Establishing the comprehensibility and cultural relevance of skin cancer genomic risk information is a critical step in mounting a randomized controlled trial examining reach and utility of skin cancer genomic testing in primary care. First, the process of language translation and transcreation is critical if we are to be responsive to the needs of specific populations. Second, selecting and training interviewers (PAs) that were not only fluent in Spanish but familiar with Albuquerque and its regionalisms was of utmost importance. Our PAs were integral members of our expert panel and provided valuable insights on the attitudes and preferences of the population we set to recruit in the larger trial. Third, planning for adequate time and resources for this effort was vital to success. Fourth, having expertise concerning the local linguistic culture, as well as genomic literacy, anthropology, health psychology, and molecular epidemiology aided in a multidisciplinary and nuanced perspective on our genomic risk education materials. Finally, expertise in qualitative behavioral research and in conducting and analyzing cognitive interviews was also critical to the successful execution and analysis of cognitive interviews.
Conclusions
The translation of personalized genomics into real-world, general population application is necessary (Green and Guyer 2011) but understudied (McBride et al. 2010). With the advent of personalized genomics for various cancers and its implications for prevention and treatment recommendations, it is imperative that research examines the impact of such advances on diverse populations to minimize existing health disparities. Accordingly, we argue that the field of skin cancer prevention is ready for public health prevention efforts that utilize genomic indicators and the time to develop genomic risk educational materials that are acceptable and relevant for Spanish speakers is now.
Confirming the comprehensibility of our skin cancer genomic risk education materials is consistent with (1) move toward broadened access to genomic technologies, (2) patient-centered medicine, and (3) efforts to maximize patient engagement and healthcare access in general. Furthermore, simultaneous exploration of basic science questions and behavioral outcomes—like we do in SOMBRA—will yield more translatable and accessible research to underserved populations (McBride et al. 2015). As genomic information increases, we have a concomitant need to engage our patients’ and research participants’ perspectives which will further accelerate the relevance and use of our findings in the future.
Compliance with ethical standards
Funding/support
This work was supported by the National Cancer Institute’s Research Grant (R01 CA181241-01A1) and Support/Core Grant (P30 CA008748). Dr. Rodríguez was supported by a training grant (T32 CA009461).
Conflict of interest
Vivian M. Rodríguez declares that she has no conflict of interest. Erika Robers declares that she has no conflict of interest. Kate Zielaskowski declares that she has no conflict of interest. C. Javier González declares that he has no conflict of interest. Keith Hunley declares that he has no conflict of interest. Kimberly A. Kaphingst declares that she has no conflict of interest. Dolores D. Guest declares that she has no conflict of interest. Andrew Sussman declares that he has no conflict of interest. Kirsten A. Meyer White declares that she has no conflict of interest. Matthew R. Schwartz declares that he has no conflict of interest. Jennie Greb declares that she has no conflict of interest. Yvonne Talamantes declares that she has no conflict of interest. Jessica Bigney declares that she has no conflict of interest. Marianne Berwick declares that she has no conflict of interest. Jennifer L. Hay declares that she has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- Berrigan D, Forsyth BH, Helba C, Levin K, Norberg A, Willis GB. Cognitive testing of physical activity and acculturation questions in recent and long-term Latino immigrants. BMC Public Health. 2010;10:481. doi: 10.1186/1471-2458-10-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bills GD, Vigil NA. The Spanish language of New Mexico and Southern Colorado: a linguistic atlas. Albuquerque: University of New Mexico Press; 2008. [Google Scholar]
- Bloss CS, Ornowski L, Silver E, Cargill M, Vanier V, Schork NJ, Topol EJ. Consumer perceptions of direct-to-consumer personalized genomic risk assessments. Genetics in Medicine. 2010;12:556–566. doi: 10.1097/GIM.0b013e3181eb51c6. [DOI] [PubMed] [Google Scholar]
- Drake BF, et al. Development of plain language supplemental materials for the Biobank informed consent process. Journal of Cancer Education: the Official Journal of the American Association for Cancer Education. 2016 doi: 10.1007/s13187-016-1029-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graves KD, Hay JL, O'Neill SC. The promise of using personalized genomic information to promote behavior change: is the debate over, or just beginning? Personalized Medicine. 2014;11:173–185. doi: 10.2217/pme.13.110. [DOI] [PubMed] [Google Scholar]
- Green ED, Guyer MS. Charting a course for genomic medicine from base pairs to bedside. Nature. 2011;470:204–213. doi: 10.1038/nature09764. [DOI] [PubMed] [Google Scholar]
- Halbert CH, Kessler L, Collier A, Weathers B, Stopfer J, Domchek S, McDonald JA. Low rates of African American participation in genetic counseling and testing for BRCA1/2 mutations: racial disparities or just a difference? J Genet Couns. 2012;21:676–683. doi: 10.1007/s10897-012-9485-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton JG, et al. Genetic testing awareness and attitudes among Latinos: exploring shared perceptions and gender-based differences. Public Health Genomics. 2016;19:34–46. doi: 10.1159/000441552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness JA, Villar A, Edwards B, et al. Translation, adaptation, and design. In: Harkness JA, et al., editors. Survey methods in multinational, multicultural and multiregional contexts. Hoboken, NJ: Wiley; 2010. pp. 117–140. [Google Scholar]
- Hay JL, Brennessel D, Kemeny MM, Lubetkin EI. Examining intuitive cancer risk perceptions in Haitian-Creole and Spanish-speaking populations. J Transcult Nurs. 2016;27:368–375. doi: 10.1177/1043659614561679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensley Alford S, McBride CM, Reid RJ, Larson EB, Baxevanis AD, Brody LC. Participation in genetic testing research varies by social group. Public Health Genomics. 2011;14:85–93. doi: 10.1159/000294277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindorff LA, Sethupathy P, Junkins HA, Ramos EM, Mehta JP, Collins FS, Manolio TA. Potential etiologic and functional implications of genome-wide association loci for human diseases and traits. Proc Natl Acad Sci U S A. 2009;106:9362–9367. doi: 10.1073/pnas.0903103106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu S, Parmet Y, Allen G, Parker DF, Ma F, Rouhani P, Kirsner RS. Disparity in melanoma: a trend analysis of melanoma incidence and stage at diagnosis among whites, Hispanics, and blacks in Florida. Arch Dermatol. 2009;145:1369–1374. doi: 10.1001/archdermatol.2009.302. [DOI] [PubMed] [Google Scholar]
- Kaphingst KA, Goodman MS. Importance of race and ethnicity in individuals' use of and responses to genomic information. Personalized Medicine. 2016;13:1–4. doi: 10.2217/pme.15.39. [DOI] [PubMed] [Google Scholar]
- Kaphingst KA, Stafford JD, McGowan LD, Seo J, Lachance CR, Goodman MS. Effects of racial and ethnic group and health literacy on responses to genomic risk information in a medically underserved population. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2015;34:101–110. doi: 10.1037/hea0000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komenaka IK, et al. Participation of low-income women in genetic cancer risk assessment and BRCA 1/2 testing: the experience of a safety-net institution. Journal of Community Genetics. 2016;7:177–183. doi: 10.1007/s12687-015-0257-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Abrams LR, Koehly LM. Using a historical lens to envision the next generation of genomic translation research. Public Health Genomics. 2015;18:272–282. doi: 10.1159/000435832. [DOI] [PubMed] [Google Scholar]
- McBride CM, et al. Future health applications of genomics: priorities for communication, behavioral, and social sciences research. Am J Prev Med. 2010;38:556–565. doi: 10.1016/j.amepre.2010.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academy of Sciences, Engineering, and Medicine (2016) Applying an implementation science approach to genomic medicine: workshop summary. Washington, DC. doi:107226/23403 [PubMed]
- Nodora JN et al (2016) Biospecimen sharing among Hispanic women in a safety-net clinic: implications for the precision medicine initiative. J Natl Cancer Inst:109. doi:10.1093/jnci/djw201 [DOI] [PMC free article] [PubMed]
- Pagan JA, Su D, Li L, Armstrong K, Asch DA. Racial and ethnic disparities in awareness of genetic testing for cancer risk. Am J Prev Med. 2009;37:524–530. doi: 10.1016/j.amepre.2009.07.021. [DOI] [PubMed] [Google Scholar]
- Petruccio C, et al. Healthy choices through family history: a community approach to family history awareness. Community Genetics. 2008;11:343–351. doi: 10.1159/000133306. [DOI] [PubMed] [Google Scholar]
- Santiago-Rivas M, Wang C (2014) Sun protection beliefs among Hispanics in the US 2014:161960 doi: 10.1155/2014/161960 [DOI] [PMC free article] [PubMed]
- Simmons VN, et al. Transcreation of validated smoking relapse-prevention booklets for use with Hispanic populations. J Health Care Poor Underserved. 2011;22:886–893. doi: 10.1353/hpu.2011.0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon FM, Eberl-Lefko AC, Michaels M, Macario E, Tesauro G, Rowland JH. Development of a linguistically and culturally appropriate booklet for Latino cancer survivors: lessons learned. Health Promot Pract. 2005;6:405–413. doi: 10.1177/1524839905278447. [DOI] [PubMed] [Google Scholar]
- Sussner KM, et al. Ethnic, racial and cultural identity and perceived benefits and barriers related to genetic testing for breast cancer among at-risk women of African descent in New York City. Public Health Genomics. 2011;14:356–370. doi: 10.1159/000325263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suther S, Kiros GE. Barriers to the use of genetic testing: a study of racial and ethnic disparities. Genetics in Medicine: Official Journal of the American College of Medical Genetics. 2009;11:655–662. doi: 10.1097/GIM.0b013e3181ab22aa. [DOI] [PubMed] [Google Scholar]
- Torres SM, Ramos M, Leverence R, Bowen D, Berwick M, Hay J. A pilot study of skin cancer risk reduction behaviors, cancer communicatin, and skin cancer beliefs in Hispanics California. Journal of Health Promotion. 2014;12:95–100. [Google Scholar]
- Udayakumar D, Tsao H. Moderate- to low-risk variant alleles of cutaneous malignancies and nevi: lessons from genome-wide association studies. Genome Medicine. 2009;1:95. doi: 10.1186/gm95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzel JN, Blazer KR, MacDonald DJ, Culver JO, Offit K. Genetics, genomics, and cancer risk assessment: state of the art and future directions in the era of personalized medicine CA. A Cancer Journal for Clinicians. 2011;61:327–359. doi: 10.3322/caac.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KJ, et al. Feasibility trial of a Spanish-language multimedia educational intervention. Clinical Trials (London, England) 2013;10:767–774. doi: 10.1177/1740774513495984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willis G. Cognitive interviewing: a tool for improving questionnaire design. Thousand Oaks, CA: SAGE Publications, Inc.; 2005. [Google Scholar]
- Willis G, Lawrence D, Hartman A, Stapleton Kudela M, Levin K, Forsyth B. Translation of a tobacco survey into Spanish and Asian languages: the tobacco use supplement to the current population survey. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2008;10:1075–1084. doi: 10.1080/14622200802087572. [DOI] [PMC free article] [PubMed] [Google Scholar]


