Abstract
This is the first randomized controlled trial to evaluate non-inferiority of Prolonged Exposure (PE) delivered via home-based telehealth (HBT) compared to standard in-person (IP) PE. One-hundred thirty two Veterans recruited from a Southeastern Veterans Affairs Medical Center and affiliated University who met criteria for posttraumatic stress disorder (PTSD) were randomized to receive PE via HBT or PE via IP. Results indicated that PE-HBT was non-inferior to PE-IP in terms of reducing PTSD scores at post-treatment, 3 and 6 month follow-up. However, non-inferiority hypotheses for depression were only supported at 6 month follow-up. HBT has great potential to reduce patient burden associated with receiving treatment in terms of travel time, travel cost, lost work, and stigma without sacrificing efficacy. These findings indicate that telehealth treatment delivered directly into patients’ homes may dramatically increase the reach of this evidence-based therapy for PTSD without diminishing effectiveness.
Keywords: PTSD, Prolonged Exposure, Telemedicine, Non-Inferiority, RCT
Veterans are at high risk for repeated exposure to potentially traumatic events and subsequent risk of a broad range of mental health problems, including posttraumatic stress disorder (PTSD; Cohen et al., 2010; Fulton et al., 2015; Hoge et al., 2004; Hoge, Auchterlonie, & Milliken, 2006; Ramchand et al., 2015). Estimates of PTSD in veterans across eras range from 5 – 30% (Fulton et al., 2015; Hoge et al., 2004; Hoge et al., 2006; Iversen et al., 2005; Kang et al., 2003; Kulka et al., 1990; Ramchand et al., 2010; Seal et al., 2007). Fortunately, screening veterans for mental health problems is now routine (Wright et al., 2002), and those in need of help are more likely than ever to be identified. Moreover, mental health improves, and service use and costs are decreased when evidence based treatments such as Prolonged Exposure (PE; Foa et al., 1991; Foa et al., 1999; Foa et al., 2005) are offered and completed (Tuerk et al., 2013). Nonetheless, even though over 40% of those screening positive indicate that they want care for PTSD symptoms, and despite existence of effective and cost-reducing treatments, only 25% of those screening positive actually receive these services (Hoge et al., 2006). Stigma and logistics-based barriers likely play a role in low treatment utilization (Hoge et al., 2004; Kim et al., 2010). Thus, effective evidence based treatments for combat-related PTSD such as PE must be delivered by methods that address relevant barriers to care for military personnel and Veterans in order to optimize opportunities for broad dissemination.
Barriers to Seeking Treatment and a Potential Solution: Home-Based Telehealth
Veterans experience stigma associated with psychiatric conditions (Iversen et al., 2005). Among both active duty and veteran personnel who have experienced military culture, “succumbing” to PTSD may be perceived as a failure, a weakness, or as evidence of an innate deficiency of strength or leadership capability (Friedman, 2004). An attitude of “wanting to solve my own problems” has also been cited as a factor that prevents treatment seeking in earlier studies (Kulka et al., 1990). More obvious, logistical barriers to attending consecutive multiple weekly appointments also play a large role in preventing access to evidence-based PTSD care. Barriers range from difficulty accessing care due to parking issues in urban areas, travel time to and from appointments, and lost work time to difficulties in scheduling and location (Hoge et al., 2004). Such logistical problems are amplified for those commuting from rural areas (Beachler, Holloman, & Herman, 2003; Hogan, 2003).
Given these barriers, an alternative medium for service delivery is needed that addresses both stigma and logistical factors impeding access to care. “Hub and spoke” telehealth-delivered care was initially proposed as one such solution, with an expert or provider at centralized clinic delivering care to patients at satellite clinics. Indeed, such telehealth formats often come at a lower patient-side cost and with easier access for both patients and providers (Bose et al., 2001; Elford et al., 2000; Morland et al., 2010) and are effective means of service delivery (Bolton & Dorstyn, 2015). Several Department of Veterans Affairs (VA) and Department of Defense studies demonstrate that hub and spoke telehealth can be implemented within the existing system infrastructure (Shore, Goranson, & Lu, 2014; Tuerk et al., 2010; Williams et al., 2015), is cost effective (Fortney et al., 2005; Glueckauf, 2002; Jerome & Zaylor, 2000; Perednia & Allen, 1995), and is clinically effective (Morland et al., 2011). However, as patients must travel to satellite clinics, stigma and logistic barriers are still present in hub and spoke telehealth models. By contrast, home-based telehealth (HBT)-delivered psychotherapy may address these barriers to a higher degree, and initial work by our group demonstrates encouraging results (Acierno et al., 2016; Egede et al., 2015).
The Present Study
As noted earlier, HBT delivery of PE for PTSD may be one way to address stigma and logistical barriers to care that confront veterans. However, few studies have evaluated comparability (non-inferiority, specifically) of traditional, office based treatments with telehealth-delivered treatments (Bolton & Dorstn, 2015), particularly with complex diagnoses such as PTSD and rigorous psychotherapies such as PE. The distinction between psychotherapy delivered through standard telehealth, which almost always follows the hub and spoke model of care and psychotherapy delivered through HBT is an important one. HBT amplifies all advantages with respect to travel time, cost, and stigma, potentially obtained through standard telehealth, but lacks supportive infrastructure found in both traditional in-person care and satellite office-based telehealth care. Thus, the current study was designed to determine if HBT delivery of evidence based PE for PTSD, “is as good as” traditional in-person (IP) PE, in terms of standard measures of PTSD and major depression (MD), the latter of which was included as an outcome in keeping with existing treatment outcome research on PTSD (Foa et al., 1999; 2005).
Methods
Design
The current study used a between groups repeated measures randomized controlled design powered for non-inferiority conclusions. Participants were randomly assigned (1:1) to either HBT or office based IP delivery of the identical PE treatment (PE-HBT vs. PE-IP). Repeated assessments were conducted by blind interviewers at pre-treatment, post-treatment, 3-month follow-up, and 6-month follow-up. A non-inferiority approach was chosen for clinical outcome variables measuring PTSD and MD based on hypotheses derived from prior research on PTSD and satellite clinic based telehealth (Acierno et al., 2016; Tuerk et al., 2010). Specifically, we predicted that the mean treatment outcome difference scores of PE-IP minus PE-HBT would be within a priori defined confidence intervals (i.e., 90% one sided) demonstrating that PE-HBT is “as good as” PE-IP.
Participants and Recruitment
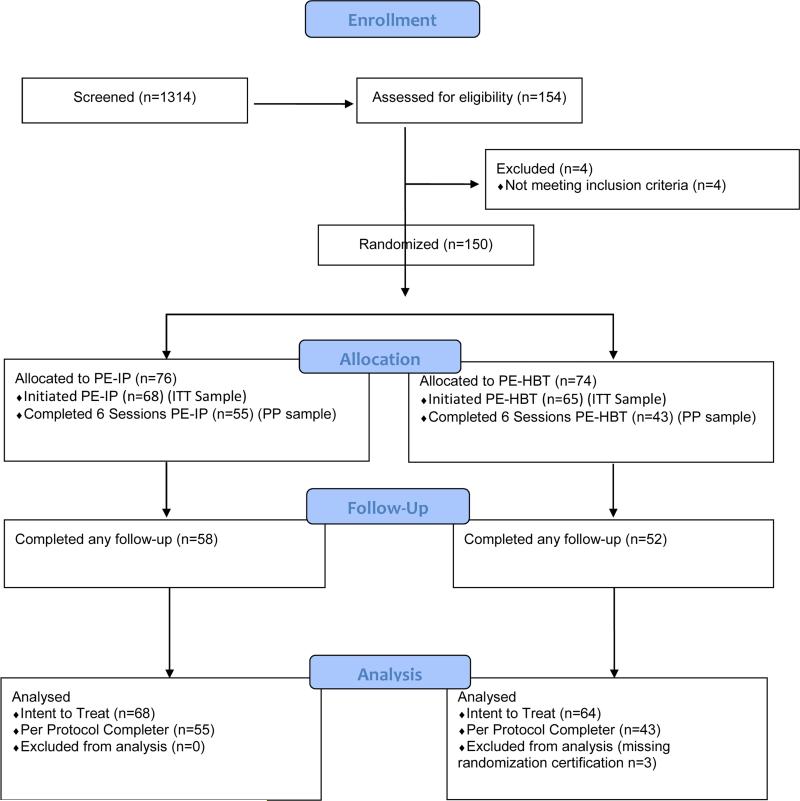
Participants were recruited from the Ralph H. Johnson Veterans Affairs Medical Center (VA) and the Medical University of South Carolina via provider referral to the VA PTSD clinic (see Figure 1 for CONSORT diagram). Data were collected November 2010 through April 2015. The Clinician Administered PTSD Scale (Blake et al., 1995) was used to determine PTSD eligibility and required that the criterion A event (i.e., the traumatic event) be combat-related. Individuals who were actively psychotic, acutely suicidal, or met criteria for current substance dependence, as determined by the Structured Clinical Interview for DSM-IV (SCID-IV; First, Spitzer, Gibbon, & Williams, 1997) were excluded from participation. To enhance generalizability of study findings, (a) veterans from each of the major conflicts comprising the majority of those served by the VA were included (i.e., OIF/OEF/OND, Persian Gulf, & Vietnam), and (b) participants receiving psychotropic medication or case management services for PTSD, mental health treatment for other psychiatric disorders, or those who met criteria for substance abuse were not excluded from participation. However, participants were asked to maintain their medication dosages at current levels and, in instances where medications were newly prescribed, required to wait four weeks for stabilization, at which point baseline measures were re-collected and study initiation commenced. Participant descriptions and demographics from the relatively larger Intent to Treat (ITT) sample (N = 132) are given in Table 1. Participants were predominantly male (n = 127), Black (n = 44) or White (n = 80), and married (n = 73). Just under half were employed (n = 55), and the average service connection rating, referring to compensated disability for injury suffered while in the military, was 53.5%.
Figure 1.
CONSORT 2016 Flow Diagram (PE)
Notes: PE-IP / PE-HBT: Prolonged Exposure In Person / Home Based Telehealth; ITT Intent to treat (at least 1 session completed); PP: Per Protocol (at least 6 sessions completed).
Table 1.
Sample Characteristics of the Overall ITT Sample Population at Baseline.
| Characteristics | Mean / Total N (SD / %) | PE-HBT n (%) | PE-IP n (%) | F or X2, p |
|---|---|---|---|---|
| Mean Age (years) | 41.8 (SD=14.5) | 40.7 (SD=14.9) | 42.9 (SD=14.1) | 0.74, 0.39 |
| Gender (%) | ||||
| Male | 127 (96.2) | 62 (98.4) | 65 (94.2) | 1.60, 0.37 |
| Female | 5 (3.8) | 1 (1.6) | 4 (5.8) | |
| Race/Ethnicity (%) | ||||
| White | 80 (60.6) | 39 (60.9) | 41 (60.3) | 1.16, 0.76 |
| Black | 44 (33.3) | 21 (32.8) | 23 (33.8) | |
| Hispanic | 7 (5.3) | 4 (6.3) | 3 (45.4) | |
| Others | 1 (0.8) | 0 (0.0) | 1 (1.5) | |
| Marital status (%) | ||||
| Never married | 30 (23.3) | 15 (23.8) | 15 (22.7) | 0.32, 0.96 |
| Married | 73 (56.6) | 36 (57.1) | 37 (56.1) | |
| Sep./Divorced | 23 (17.8) | 11 (17.5) | 12 (18.2) | |
| Widowed | 3 (2.3) | 1 (1.6) | 2 (3.0) | |
| Education (Years) | 12.4 (SD=4.6) | 12.2 (SD=4.9) | 12.5 (SD=4.4) | 0.09, 0.76 |
| Employed (%) | 55 (49.1) | 26 (48.1) | 29 (50.0) | 0.04, 0.50 |
| Baseline PCL | 59.2 (11.2) | 60.1 (11.3) | 58.3 (11.1) | 0.84, 0.36 |
| Basline BDI | 27.7 (12.1) | 27.5 (13.0) | 27.9 (11.4) | 0.01, 0.87 |
| War Theatre (%) | ||||
| OEF/OIF | 80 (60.6) | 38 (28.8) | 42 (31.8) | 0.06, 0.97 |
| Persian Gulf | 22 (16.7) | 11 (8.3) | 11 (8.3) | |
| Vietnam | 30 (22.7) | 14 (10.6) | 16 (12.1) | |
| Mean Service Connection Rating | 53.5 (SD=37.9) | 55.8 (SD=35.7) | 51.4 (SD=40.2) | 0.32, 0.57 |
Note: N's may differ across variables due to variable specific missing data. ± sd or %. Statistics are F-test for continuous variables (means) and chi-square for categorical (%) variables. PE-HBT: Prolonged Exposure-Home Based Telehealth; PE-IP: Prolonged Exposure-In Person; Sep: Separated; PCL: Post-traumatic Stress Disorder Checklist; BDI: Beck Depression Inventory; OEF: Operation Enduring Freedom; OIF: Operation Iraqi Freedom.
Measures
Clinician-Administered PTSD Scale (CAPS)-IV
The CAPS is a clinician-rated scale designed to diagnose current and lifetime PTSD (Blake et al., 1995). The CAPS has adequate internal consistency, inter-rater reliability, and test-retest reliability (Orsillo, Batten, & Hammond, 2001). In addition, the CAPS has adequate convergent validity with alternative measures of PTSD and adequate discriminant validity with respect to measures of depression and anxiety (Weathers & Litz, 1994). Finally, the diagnosis established by the CAPS compares well to alternative structured interviews (Weathers, Ruscio, & Keane, 1999), including the SCID (First et al., 1996). For this study, the CAPS was used to define inclusion criteria (i.e., PTSD diagnosis), not treatment response.
PTSD Checklist–Military (PCL-M)
The PCL-M is a 17-item measure designed to assess DSM-IV PTSD symptom severity (Weathers et al., 1993). The PCL has excellent internal consistency (α > .94) and excellent test-retest reliability in various populations (r = .96; Orsillo et al., 2001). In addition, the PCL demonstrates excellent convergent validity with alternative measures of PTSD (rs range from .77 to .93; Orsillo et al., 2001). Importantly, the PCL is also the most widely used PTSD outcome measure in the VA and demonstrates consistent dynamic change with effective PE treatment across numerous in-person studies (e.g., Goodson et al., 2013; Mouilso et al., 2015; Tuerk et al., 2011; Wolf et al., 2012; Yoder et al., 2012) and telehealth-related studies (e.g. Gros et al., 2011; Tuerk et al., 2010). Accordingly, the PCL served as the PTSD-related non-inferiority outcome for the study.
Beck Depression Inventory—2nd Edition (BDI)
The BDI 2nd edition is a 21-item measure designed to assess the cognitive, affective, behavioral, motivational, and somatic symptoms of depression in adults and adolescents (Beck, Steer, & Brown, 1996). The BDI-II has demonstrated excellent test-retest reliability over a 1-week interval (r = .93), excellent internal consistency (α < .92), and convergent and discriminant validity in multiple samples (Beck et al., 1996; Steer & Clark, 1997). The BDI served as the depression-related non-inferiority outcome for the study.
Procedures
All study procedures were approved by the University institutional review board and VA Medical Center Research and Development committee. Consented participants were randomly assigned to either PE-IP or PE-HBT. The randomization sequence was generated by the biostatistician (RK) using a permuted block randomization scheme with block size varied to minimize threats to blinded group assignment. The CONSORT diagram (see Figure 1) demonstrates the proportions of these groups that were randomized, completed at least one treatment session (the minimum to be included in ITT analyses), completed at least 6 treatment sessions (the minimum to be included in per protocol (PP) analyses) and completed at least one post treatment assessment.
Treatment, Therapists, & Treatment Fidelity
Both IP and HBT conditions followed the identical PE manual (Foa, Hembree, & Rothbaum, 2007), and all therapists delivered PE in both delivery formats. Treatment was comprised of 10-12, 1.5 hour sessions. Therapists were licensed master's level counselors who completed a 32-hour workshop-training program in PE and observed a senior-level clinician throughout a complete course of PE-IP and PE-HBT. Therapists met weekly with the third author for supervision throughout the duration of the study. All therapists provided equal proportions of PE-IP and PE-HBT treatment. Treatment fidelity was maintained at or above 90% across and within conditions, assessed through random sampling of 20% of therapy session audiotapes rated according to session-specific procedures directly corresponding to the PE treatment manual. Interviewers were masters level psychologists and were blind to condition for baseline, post-treatment, month 3 and month 6 follow-up data collection. However, therapists gathered PCL and BDI data for week 2, 4, 6, 8, and 10 time points as part of standard treatment procedures.
Experimental Conditions: PE-IP vs. PE-HBT
IP treatment was provided in the VA Medical Center PTSD outpatient treatment wing. Treatment sessions for the HBT condition were conducted using HIPAA compliant in-home videoconferencing software available free to VA Medical Center patients and providers. PE-HBT was provided via participants’ own equipment (e.g., home computer or tablet or even smartphone), or via equipment (videophones or tablets with high speed cellular internet plans) with pre-loaded videoconferencing software provided during the treatment phase by the research team. An assistant was available for technical support when needed, and conducted a pre-treatment test call with all patients. This pre-test procedure effectively resolved all software initiation issues. However, almost 80% of patients reported at least one bandwith (i.e., ‘frozen image’ problem) during at least one session, all of which were resolved by reconnection. Consistent with HBT policies, participants provided the address within which HBT sessions would take place in order to create a point of intervention should emergencies arise. Prior to session initiation, therapists acquired the direct (not 911) telephone line for the local emergency services dispatch for each patient's location. Emergency procedures for HBT are outlined by Gros, Veronee, Strachan, Ruggiero, and Acierno (2011) and begin with initiating local emergency service personnel response using the aforementioned direct telephone number. No participant required this, however.
Data Analytic Plan
The 90% one-sided confidence interval (90% CI) approach was used to evaluate noninferiority of PE-HBT compared to PE-IP mode of delivery. PE-HBT is judged to be “at least as good as” (noninferior to) PE-IP so long as difference in treatment means for PE-IP does not exceed that of PE-HBT by more than the a priori specified non-inferiority margin, delta (Δ). For the PTSD measure (PCL), the non-inferiority margin is given by the VA National Center for PTSD as 10-20 (Monson et al., 2008). However, we considered this range too liberal, and used the range of 8.8 derived through polling 12 published PTSD researchers and used in our first non-inferiority study (Acierno et al., 2016) of HBT. The commonly accepted clinically important effect size for the BDI is 5 points (Dworkin et al., 2008). With the CI approach (assuming order of subtraction is IP minus HBT), the non-inferiority of HBT can be declared if the lower bound of the 90% CI is less than −Δ, where −Δ for PCL and BDI are −8.8 and −5.0, respectively. The primary time points for assessing non-inferiority were immediate post-treatment and at 3- and 6-months follow-up.
Missing data were estimated using multiple imputation (SAS procedures MI and MIANALYZE; SAS V9.4, Cary, NC) with treatment, age, and observed values of the outcome variable (PCL, BDI) at all time points (baseline, even weeks 2-10, post, 3-, 6-months) included in the imputation model. The Markov Chain Monte Carlo (MCMC) method was used to convert nonmonotone missing data to a monotone pattern which was used for the final imputation step. A regression approach using a mixed effects model (SAS Proc Mixed) was used to estimate differences in outcome means and corresponding 90% CI at the primary time points (post-treatment, 3 month and 6 month follow-up). Consistent with non-inferiority (NI) analysis guidelines, we used the per-protocol (PP) sample for primary NI results and report confidence intervals rather than p-values (Schumi & Wittes, 2011).
In a secondary set of analyses using the ITT sample (comprising all 132 randomized participants who attended at least one session), a mixed effects modelling approach (MEM) was used to illustrate and compare the trajectories of longitudinal outcome means for PE-IP and PE-HBT over the full time course. The dependent variables in the MEM models were PCL and BDI, each used separately. The model included treatment, visit, visit-by-treatment (interaction term) as primary independent variables. Visit included measurement time points: baseline, weeks 2, 4, 6, 8, 10, post-treatment, 3 and 6 month follow-up. If a significant interaction term in the model is observed, this is considered evidence of non-parallel trajectories (differential rate of change by treatment group). An unstructured covariance was used and analyses were performed using SAS Proc Mixed (SAS v9.4).
Results
Baseline Scores and Dropout
Demographic characteristics and self-report measures of psychopathology were not significantly different for the PE-HBT and PE-IP treatment groups (Table 1). Approximately 19% of the PE-IP group dropped out (did not complete at least six therapy sessions) as compared to 32.8% of the PE-HBT group (χ2 = 3.23, p=0.072). We subsequently: (a) examined the overall average number of sessions received in both groups and found no statistically significant differences between PE-HBT (7.6 sessions; SD = 3.6 sessions) and PE-IP (8.6 sessions; SD=3.2 sessions) (F(1, 131) = 2.97, p = .09) in the overall ITT sample (N = 132); and (b) examined the average number of sessions completed prior to dropout in each group, and found no difference between conditions in the dropout sample (ITT – PP = 34) (PE-HBT: 3.1 sessions completed before dropout vs PE-IP: 2.9 sessions completed before dropout; F(1, 131) = 0.07, p = .80). Considering overall participants available for study, one hundred fifty individuals were randomized but intent to treat data were available for only 132 at post treatment and 110 at followup.
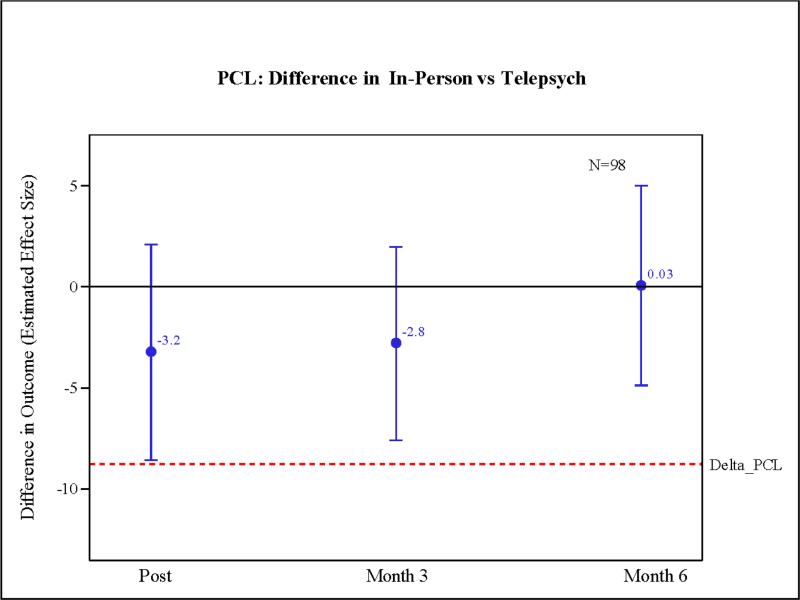
Non-Inferiority Comparisons
Figures 2 and 3 give the 90% one sided confidence intervals overlaid on the non-inferiority margin (Δ) line for PCL and BDI, respectively. Differences in treatment means and confidence intervals (90% CI) are given in terms of the PE-HBT group mean subtracted from the PE-IP group mean, with negative numbers indicating poorer performance for PE-HBT. In Figure 2, the lower limits of the 90% CI for PCL scores at post-treatment (M= −3.2; 90% CI: −8.6 to 2.1) 3 months (M= : −2.8; 90% CI: −7.6 to 2.0) and 6 months (M= 0.03; 90% CI: −4.9 to 5.0) were within (did not exceed) the pre-specified meaningful clinical difference (−Δ = −8.8) indicating, with respect to PCL outcome scores, PE-HBT was “as good as” PE-IP.
Figure 2.
PCL difference PE-HBT vs. PE-IP at post-treatment, 3 & 6 month follow-up.
Note: PE-HBT: Prolonged Exposure-Home Based Telehealth; PE-IP: Prolonged Exposure-In Person; PCL: Post-traumatic Stress Disorder Checklist; Inventory Order of subtraction PE-IP minus PE-HBT; negative difference indicates HBT mean higher than IP mean. Non-inferiority of HBT supported if lower limit of CI is not less than (extend beyond) delta.
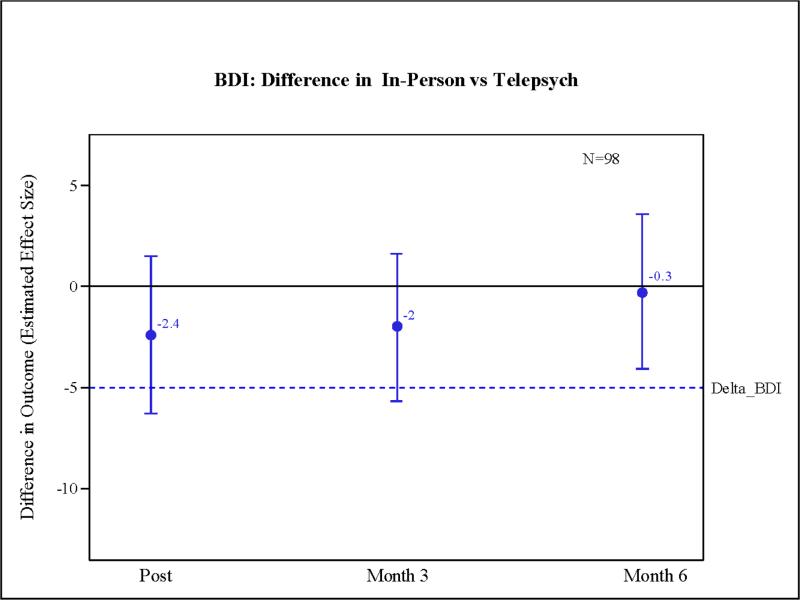
Figure 3.
BDI difference PE-HBT vs. PE-IP at post-treatment, 3 & 6 month followup.
Note: PE-HBT: Prolonged Exposure-Home Based Telehealth; PE-IP: Prolonged Exposure-In Person; BDI: Beck Depression Inventory Order of subtraction PE-IP minus PE-HBT; negative difference indicates HBT mean higher than IP mean. Non-inferiority of HBT supported if lower limit of CI is not less than (extend beyond) delta.
In contrast to findings for PTSD symptoms, the lower limit of the 90% CI for BDI scores (Figure 3) at post-treatment (M = −2.4; 90% CI: −6.3 to 1.5) and 3 month follow-up (M = −2.0; 90% CI: −5.7 to 1.6) fell slightly outside the pre-specified limit of non-inferiority (Δ = −5.0). However, scores between conditions were virtually identical (M= −0.3; 90% CI: −4.1 to 3.6) at 6 month follow-up.
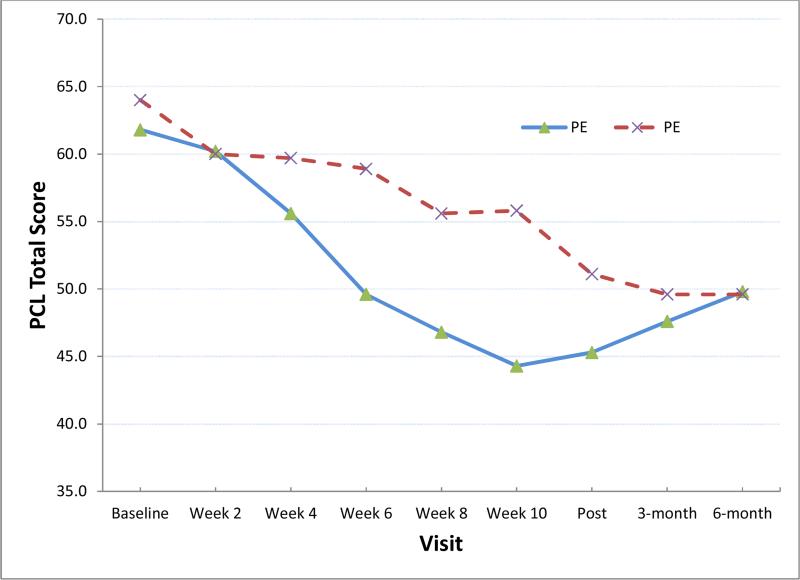
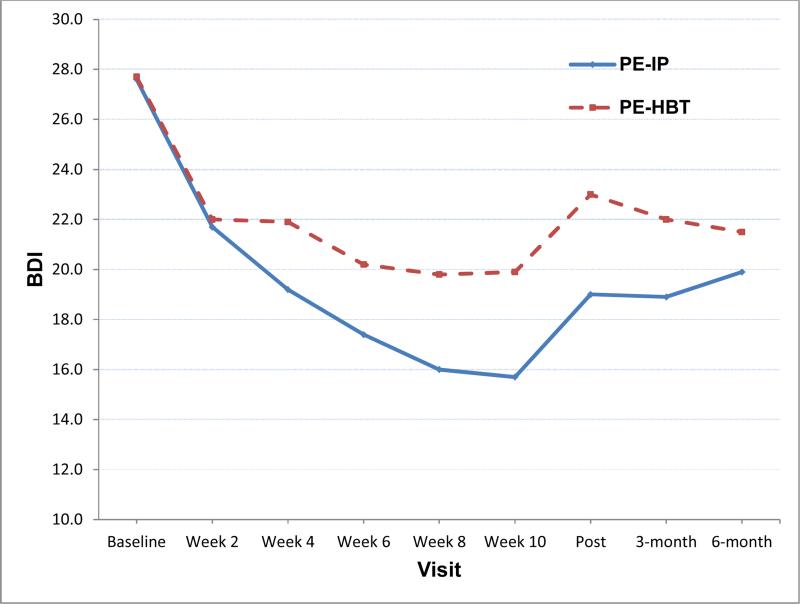
Secondary analyses described the longitudinal trajectory of outcome using the ITT sample to characterize the overall intervention effect, as ITT samples are characteristically used for this purpose. Note that Figures 4 and 5 illustrate the modeled time course of PCL and BDI means, respectively. For both PCL and BDI, we found no statistically significant time-by-visit interaction and no significant treatment main effect, indicating that treatment groups had similar rates of improvement over time for PCL (PE-IP slope=−1.9, p<0.0001; PE-HBT slope=−1.8, p<0.0001) and BDI (PE-IP slope=−1.2, p<0.0001; PE-HBT slope=−0.8, p=0.004). We also found no statistically significant treatment differences in outcomes (effect sizes) at the primary post, 3-, and 6-month time points for the linear MMRM model.
Figure 4.
Trajectory of PCL Modeled Means for ITT Sample (n=132)
Note: PE-HBT: Prolonged Exposure-Home Based Telehealth; PE-IP: Prolonged Exposure-In Person; PCL: Post-traumatic Stress Disorder Checklist. Least squares means from mixed effects model with unstructured covariance. For linear model: Treatment main effect, p=0.1159; time main effect, p<0.0001, Treatment-by-time interaction, p=0.1307. p-values at immediate post, 3- and 6-months: 0.2478, 0.4437, 0.9753, respectively.
Figure 5.
Trajectory of BDI Modeled Means for ITT Sample (n=132)
Note: PE-HBT: Prolonged Exposure-Home Based Telehealth; PE-IP: Prolonged Exposure-In Person; BDI: Beck Depression Inventory. Least squares means from mixed effects model with unstructured covariance. For linear model: Treatment main effect, p=0.1922; time main effect, p<0.0001, Treatment-by-time interaction, p=0.4703. P-values at immediate post, 3- and 6-months: 0.1513, 0.2079, 0.5480, respectively.
For comparability with other treatment outcome studies, we also report calculated effect sizes (d) for time. As noted above, there were no between group differences in either slope, or effect size at each time point. Thus, in the absence of differences across conditions, overall effect sizes across major time assessment points (i.e., baseline compared to post-treatment, 3 and 6 month follow-ups) were calculated with the ITT sample for PCL scores using pooled standard deviations at each time point (baseline PCL M = 59.1, SD = 11.2; post-treatment PCL M 43.4, SD = 14.2; month 3 PCL M = 44.8, SD = 10.5; month 6 PCL M = 46.5, SD = 13.8), yielding a baseline - post treatment effect size d = 1.24 (90% CI = 1.02 – 1.46); a baseline - month 3 effect size d = 1.32 (90% CI = 1.10 – 1.55), and a baseline – month 6 effect size d = 1.04 (90% CI = 0.83 – 1.26).
Discussion
The major study hypothesis that PE delivered by HBT would be ‘as good as’ the same treatment delivered in person was largely supported in terms of PTSD symptom response by non-inferiority analyses at all time points. However, non-inferiority hypotheses for depression were only supported at 6 month follow-up, with PE-HBT performing more poorly than PE-IP with respect to BDI scores at post-treatment and 3 month follow-up. This may be due to the focus of PE on PTSD symptoms, and this focus may be relatively enhanced when conducting treatment via HBT compared to in person settings, where opportunities for incidental attention to depression symptoms and their alleviation may be more frequent. In addition, the increased activities necessary to engage in in person psychotherapy may well have acted as a form of behavioral activation, enhancing the the in person condition's antidepressant effect. Overall, these findings build on those of previous investigations indicating non-inferiority of HBT delivered therapies relative to in-person treatment (Acierno et al., 2016; Bolton & Dorstyn, 2015; Maieritsch et al., 2015; Morland et al., 2015), and support the notion that this medium is tenable for delivering evidence based treatments for complex conditions such as PTSD. These findings are promising for veterans who encounter significant barriers to receiving PTSD-related treatment at the VA or at community based outpatient clinics.
Our findings are in line with those of existing randomized controlled trials comparing telehealth delivered treatment with in person treatment of PTSD (although there are very few of these studies with veterans). For example, Morland et al. (2013) followed the hub and spoke model of care (satellite office based telehealth) to deliver therapy to groups of veterans with PTSD and found the modality to be non-inferior to in person treatment in a sample of 125 veterans. However, unlike Morland et al. (2013), PTSD treatment gains following HBT were largely maintained in this study. Similarly, in a very small randomized controlled trial with 18 participants, Zeimba, et al. (2014) showed similar gains for in-person and satellite office telehealth treated veterans. Maieritsch et al. (2015) also compared the hub and spoke version of telehealth delivered treatment with in person treatment of PTSD and found similar outcomes for both treatment deliveries. However, they noted that HBT should be considered due to significant barriers to treatment delivery using the hub and spoke model, including requirements of space for a therapist at one site, space for the patient at the second site, and patient travel time. Thus, our findings extend prior hub and spoke telehealth findings to HBT delivered care, which may alleviate more barriers than traditional hub and spoke models of telehealth. Note also that none of these studies used PE as the treatment examined. Instead, other effective cognitive behavioral treatments were used including cognitive processing therapy. Therefore, this is the first study to examine high-fidelity PE delivered over HBT. This is an important distinction because therapists may be more reluctant to deliver PE over HBT due to potential difficulties with imaginal exposures and in vivo exposures. However, the findings from this study should alleviate any of these potential therapist concerns.
Indeed, a secondary finding worthy of comment is the fact that effect size analyses indicated that PE produced long-term PTSD symptom improvement, albeit at levels somewhat less that those observed in prior studies (Foa e al., 2005). These clinically significant improvements were evident even though we went to great lengths to approximate the ‘real world’ context of a VA PTSD clinic and its clinicians. Specifically, our recruitment criteria were the same as those of the VA clinic from which we recruited, and the wide inclusion / narrow exclusion criteria (i.e., CAPS positive for PTSD, non-acutely psychotic, not acutely suicidal, non-substance dependent) meant that our patient population evinced many variations of symptom intensity, frequency, course, motivation for treatment, and comorbidities of both a health and mental health nature among other factors that most certainly affect treatment effectiveness. These factors are typically filters for inclusion in protocol based treatment outcome research. This, combined with our purposeful use of masters level clinicians rather than highly specialized clinicians, dramatically increased the real world generalizability of our findings.
There are several strengths of the present study. Most importantly, this is the first demonstration of non-inferiority of PE delivered via HBT for PTSD symptoms. Second, the patient sample was relatively ‘unfiltered’, and our inclusion / exclusion criteria were no different from that of the VA PTSD clinic from which participants were recruited. Third, our therapists were typical of the VA, and thus, our findings have extremely high real world relevance and show that the logistical advantage of HBT over ‘hub and spoke’ versions of telehealth do not come at a high cost to treatment effectiveness.
Limitations
The study also contains several limitations. First, due to ethical concerns associated with using control treatments with veterans with PTSD, the study lacked a third group of participants receiving an alternative intervention to compare PE-HBT with a standard control-group treatment (e.g., Supportive Counseling via HBT). Although this would not have provided relevant information for non-inferiority analyses, it would have provided comparative effectiveness data allowing us to isolate the treatment medium from the PE treatment, per se. Second, the number of those completing six or more sessions (i.e., the PP sample) was significantly lower than the ITT sample, and such discrepancy could lessen reliability of the findings. Relatedly, there was limited power to assess differential dropout. In addition, all participants in both groups were required to be willing to attend sessions in person prior to randomization, thereby limiting generalization to the more rural / geographically distant population for whom this modality is most relevant. Further, prior treatment and prior treatment failure were not assessed, and the impact of prior treatment on the effectiveness of in person vs HBT delivered PE is unknown. Another limitation involves the dependent measures. While it is common to use continuous measures of psychopathology as primary outcome variables, post-treatment CAPS data would have offered complimentary diagnostic level information regarding non-inferiority of treatment modality. Additionally, although miniority status was well represented, gender was not, with only 5 female veterans included in the study. A further weakness involves limited generalizability of results from this combat sample of largely male veterans to the general population of civilians who may receive PE treatment. Finally, a major concern with HBT involves access to emergency resources that may be more often available in clinic settings. The scope of the present investigation was limited in that these concerns and the parameters under which they are more or less likely to become manifest were not studied.
Highlights.
Prolonged Exposure (PE) decreases posttraumatic stress disorder (PTSD) symptoms
Home-based telemedicine (HBT) was compared to in person (IP) delivery of PE
HBT-PE was non-inferior to IP-PE in terms of PTSD symptoms at post, 3 and 6 month followup points
HBT-PE was non-inferior to IP-PE in depression symptoms at 6-month follow-up only
HBT-PE can increase the reach of this evidence-based treatment for PTSD
Acknowledgements
This research was supported by the Department of Veterans Affairs Health Services Research and Development grant #HX00152 (PI: Acierno) and by the South Carolina Clinical & Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina through NIH/NCATS Grant Number UL1 TR001450. Manuscript preparation was partially supported by a grant from the National Institute of Mental Health (T32 MH18869; PIs: Kilpatrick & Danielson).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
Several authors are core and affiliate members of the Ralph H. Johnson VAMC Center of Innovation (CoIN 13–418; PI: Egede): Health Equity and Rural Outreach Innovation Center (HEROIC). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. There are no conflicts of interest to disclose for any of the authors.
References
- Acierno R, Gros DF, Ruggiero KJ, Hernandez-Tejada MA, Knapp RG, Lejuez CW, Tuerk PW. Behavioral activation and therapeutic exposure for posttraumatic stress disorder: A non-inferiority trial of treatment delivered in person vs. home-based telehealth. Depression and Anxiety, Advanced online publication. 2016 doi: 10.1002/da.22476. doi: 10.1002/da.22476. [DOI] [PubMed] [Google Scholar]
- Beachler M, Holloman C, Herman J. Southern rural access program: An overview. Journal of Rural Health. 2003;19:301–307. doi: 10.1111/j.1748-0361.2003.tb01048.x. doi: 10.1111/j.1748-0361.2003.tb00645.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II. Harcourt Assessment; San Antonio, TX: 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Jaloupek DG, Gusman FD, CHarney DS, Keane TM. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. doi: 10.1007/bf02105408. [DOI] [PubMed] [Google Scholar]
- Bolton A, Dorstyn D. Telepsychology for posttraumatic stress disorder: A systematic review. Journal of Telemedicine and Telecare. 2015;21:254–267. doi: 10.1177/1357633X15571996. doi: 10.1177/1357633x15571996. [DOI] [PubMed] [Google Scholar]
- Bose U, McLaren P, Riley A, Mohammedali A. The use of telepsychiatry in the brief counseling of non-psychotic patients from an inner-London general practice. Journal of Telemedicine and Telecare. 2001;7:8–10. doi: 10.1177/1357633X010070S103. doi: 10.1177/1357633x010070s103. [DOI] [PubMed] [Google Scholar]
- Cohen B, Gima K, Bertenthal D, Kim S, Marmar CR, Seal KH. Mental health diagnoses and use of VA non-mental health medical services among returning OIF/OEF veterans. Journal of General Internal Medicine. 2010;25:18–24. doi: 10.1007/s11606-009-1117-3. doi: 10.1007/s11606-009-1117-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin RH, Turk DC, Wyrwich KW, Beaton D, Cleeland CS, Farrar JT, McDermott MP. Consensus statement: Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. Journal of Pain. 2008;9:105–121. doi: 10.1016/j.jpain.2007.09.005. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- Egede LE, Acierno R, Knapp RG, Lejuez C, Hernandez-Tejada M, Payne EH, Frueh BC. Psychotherapy for depression in older veterans via telemedicine: A randomised, open-label, non-inferiority trial. Lancet Psychiatry. 2015;2:693–701. doi: 10.1016/S2215-0366(15)00122-4. doi: 10.1016/s2215-0366(15)00122-4. [DOI] [PubMed] [Google Scholar]
- Elford R, White H, Bowering R, Ghandi A, Maddiggan B, John KS. A randomized, controlled trial of child psychiatric assessments conducted using videoconferencing. Journal of Telemedicine and Telecare. 2000;6:73–82. doi: 10.1258/1357633001935086. doi: 10.1258/1357633001935086. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV) American Psychiatric Press, Inc.; Washington, D.C.: 1996. 1996. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67:194–200. doi: 10.1037//0022-006x.67.2.194. doi: 10.1037/0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa E, Hembree E, Cahill S, Rauch SAM, Riggs DS, Feeny NC, Yadin E. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. doi: 10.1037/0022-006x.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO. Prolonged exposure therapy for PTSD. Oxford University; New York: 2007. [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. doi: 10.1037/0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Fortney J, Maciejewski M, Warren J, Burgess JF. Does improving geographic access to VA primary care services impact patients' patterns of utilization and costs? Inquiry. 2005;42:29–42. doi: 10.5034/inquiryjrnl_42.1.29. doi: 10.5034/inquiryjrnl_42.1.29. [DOI] [PubMed] [Google Scholar]
- Friedman M. Acknowledging the psychological cost of war. New England Journal of Medicine. 2004;351:75–78. doi: 10.1056/NEJMe048129. doi: 10.1056/nejme048129. [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner RH, Schry AR, Hair LP, Feeling N, Elbogen E, Beckham JC. The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans: A meta-analysis. Journal of Anxiety Disorders. 2015;31:98–107. doi: 10.1016/j.janxdis.2015.02.003. doi: 10.1016/j.janxdis.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Glueckauf R. Telehealth and chronic disabilities: New frontier for research and development. Rehabilitation Psychology. 2002;47:3–7. doi: 10.1037/0090-5550.47.1.3. [Google Scholar]
- Goodson JT, Lefkowitz CM, Helstrom AW, Gawrysiak MJ. Outcomes of prolonged exposure therapy for veterans with posttraumatic stress disorder. Journal of Traumatic Stress. 2013;26:419–425. doi: 10.1002/jts.21830. doi: 10.1002/jts.21830. [DOI] [PubMed] [Google Scholar]
- Gros DF, Veronee K, Strachan M, Ruggiero KJ, Acierno R. Managing suicidality in home-based telehealth. Journal of Telemedicine and Telecare. 2011;17(6):332–335. doi: 10.1258/jtt.2011.101207. [DOI] [PubMed] [Google Scholar]
- Gros DF, Yoder M, Tuerk PW, Lozano BE, Acierno R. Exposure therapy for PTSD delivered to veterans via telehealth: Predictors of treatment completion and outcome and comparison to treatment delivered in person. Behavior Therapy. 2011;42(2):276–283. doi: 10.1016/j.beth.2010.07.005. [DOI] [PubMed] [Google Scholar]
- Hogan MF. The president's new freedom commission: recommendations to transform mental health care in America. Psychiatric Services. 2003;54:1467–1474. doi: 10.1176/appi.ps.54.11.1467. doi: 10.1176/appi.ps.54.11.1467. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–1032. doi: 10.1001/jama.295.9.1023. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Iversen A, Dyson C, Smith N, Greenberg N, Walwyn R, Unwin C, Wessely S. ‘Goodbye and good luck’: The mental health needs and treatment experiences of British ex-service personnel. British Journal of Psychiatry. 2005;186:480–486. doi: 10.1192/bjp.186.6.480. doi: 10.1192/bjp.186.6.480. [DOI] [PubMed] [Google Scholar]
- Jerome LW, Zaylor C. Cyberspace: Creating a therapeutic environment for telehealth applications. Professional Psychology: Research and Practice. 2000;31:478–483. doi: 10.1037/0735-7028.31.5.478. [Google Scholar]
- Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: A population-based survey of 30,000 veterans. American Journal of Epidemiology. 2003;157:141–148. doi: 10.1093/aje/kwf187. doi: 10.1093/aje/kwf187. [DOI] [PubMed] [Google Scholar]
- Keane T, Wolfe J. Comorbidity in PTSD: An analysis of community and clinical studies. Journal of Applied Social Psychology. 1990;20:1776–1788. doi: 10.1111/j.1559-1816.1990.tb01511.x. [Google Scholar]
- Kim PY, Thomas JL, Wilk JE, Castro C, Hoge C. Stigma, barriers to care, and use of mental health services among active duty and national guard soldiers after combat. Psychiatric Services. 2010;61:582–588. doi: 10.1176/ps.2010.61.6.582. doi: 10.1176/appi.ps.61.6.582. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WA, Fairbanks JA, Hough RL, Jordan BK, Marmar CR, Cranston AS. Trauma and the Vietnam War generation: Report of findings from the National Vietnam Veterans Readjustment Study. Brunner/Mazel; New York: 1990. [Google Scholar]
- Monson CM, Gradus JL, Young-Xu Y, Schnurr PP, Price JL, Schumm JA. Change in posttraumatic stress disorder symptoms: Do clinicians and patients agree? Psychological Assessment. 2008;20:131–138. doi: 10.1037/1040-3590.20.2.131. doi: 10.1037/1040-3590.20.2.131. [DOI] [PubMed] [Google Scholar]
- Morland LA, Greene CJ, Rosen CS, Foy D, Reilly, Shore J, He Q, Frueh C. Telemedicine for anger management therapy in a rural population of combat veterans with posttraumatic stress disorder: A randomized noninferiority trial. Journal of Clinical Psychiatry. 2010;71:855–863. doi: 10.4088/JCP.09m05604blu. doi: 10.4088/jcp.09m05604blu. [DOI] [PubMed] [Google Scholar]
- Morland L, Hynes A, Mackintosh MA, Resick PA, Chard KM. Group cognitive processing therapy delivered to veterans via telehealth: A pilot cohort. Journal of Traumatic Stress. 2011;24:465–469. doi: 10.1002/jts.20661. doi: 10.1002/jts.20661. [DOI] [PubMed] [Google Scholar]
- Morland L, Raab M, Mackintosh M, Rosen CS, Dismuke CE, Greene CJ, Frueh BC. Telemedicine: A cost-reducing means of delivering psychotherapy to rural combat veterans with PTSD. Telemedicine and e-Health. 2013;19:754–759. doi: 10.1089/tmj.2012.0298. doi: 10.1089/tmj.2012.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouilso ER, Tuerk PW, Schnurr PP, Rauch SAM. Addressing the gender gap: Prolonged exposure for PTSD in veterans. Psychological Services. 2016;13:308–316. doi: 10.1037/ser0000040. doi: 10.1037/ser0000040. [DOI] [PubMed] [Google Scholar]
- Orsillo S, Batten S, Hammond C. Acute stress disorder and posttraumatic stress disorder: A brief overview and guide to assessment. In: Antony M, Orsillo S, Roemer L, editors. Practitioner's guide to empirically based measures of anxiety AABT clinical assessment series. Springer; US: 2001. pp. 245–54. [Google Scholar]
- Perednia D, Allen A. Telemedicine technology and clinical applications. Journal of the American Medical Association. 1995;273:483–488. doi: 10.1001/jama.1995.03520300057037. [PubMed] [Google Scholar]
- Ramchand R, Rudavsky R, Grant S, Tanielian T, Jaycox L. Prevalence of, risk factors for, and consequences of posttraumatic stress disorder and other mental health problems in military populations deployed to Iraq and Afghanistan. Current Psychiatry Reports. 2015;17:1–11. doi: 10.1007/s11920-015-0575-z. doi: 10.1007/s11920-015-0575-z. [DOI] [PubMed] [Google Scholar]
- Ramchand R, Schell TL, Karney BR, Osilla KC, Burns RM, Caldarone LB. Disparate prevalence estimates of PTSD among service members who served in Iraq and Afghanistan: Possible explanations. Journal of Traumatic Stress. 2010;23:59–68. doi: 10.1002/jts.20486. doi: 10.1002/jts.20486. [DOI] [PubMed] [Google Scholar]
- Seal KH, Bertenthal D, Miner CR, Sen S, Marmar S. Bringing the war back home: Mental health disorders among 103, 788 U.S. veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Archives of Internal Medicine. 2007;167:476–482. doi: 10.1001/archinte.167.5.476. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- Schumi J, Wittes JT. Through the looking glass: Understanding non-inferiority. Trials. 2011;12:106–118. doi: 10.1186/1745-6215-12-106. doi: 10.1186/1745-6215-12-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shore P, Goranson A, Lu M. Meeting veterans where they're @: A VA home-based telemental health (HBTMH) pilot program. International Journal of Psychiatry in Medicine. 2014;48:5–17. doi: 10.2190/PM.48.1.b. doi: 10.2190.pm.48.1.b. [DOI] [PubMed] [Google Scholar]
- Steer RA, Clark DA. Psychometric characteristics of the Beck Depression Inventory-II with college students. Measurement and Evaluation in Counseling and Development. 1997;30:128–136. doi: 10.1080/13651500510014800. [Google Scholar]
- Tuerk PW, Wangelin B, Rauch SAM, Dismuke CE, Yoder M, Myrick H, Eftekhari A, Acierno R. Health service utilization before and after evidence-based treatment for PTSD. Psychological Services. 2013;10:401–409. doi: 10.1037/a0030549. doi: 10.1037/a0030549. [DOI] [PubMed] [Google Scholar]
- Tuerk PW, Yoder M, Grubaugh A, Myrick H, Hamner M, Acierno R. Prolonged exposure therapy for combat-related posttraumatic stress disorder: An examination of treatment effectiveness for veterans of the wars in Afghanistan and Iraq. Journal of Anxiety Disorders. 2011;25:397–403. doi: 10.1016/j.janxdis.2010.11.002. doi: 10.1016/j.janxdis.2010.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuerk P, Yoder M, Ruggiero KJ, Gros DF, Acierno R. A pilot study of prolonged exposure therapy for posttraumatic stress disorder delivered via telehealth technology. Journal of Traumatic Stress. 2010;23:116–123. doi: 10.1002/jts.20494. doi: 10.1002/jts.20494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, Vasterling JJ. Validation of scales from the deployment risk and resilience inventory in a sample of Operation Iraqi Freedom veterans. Assessment. 2008;15:391–403. doi: 10.1177/1073191108316030. doi: 10.1177/1073191108316030. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT. Psychometric properties of the clinician-administered PTSD scale, CAPS-1. PTSD Research Quarterly. 1994;5:2–6. doi: 10.1037/e572192010-003. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist: reliability, validity and diagnostic utility. Annual meeting of the International Society for Traumatic Stress Studies; San Antonio, TX: 1993. [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Assessment. 1999;11:124–133. doi: 10.1037/1040-3590.11.2.124. [Google Scholar]
- Williams J, Tuerk P, Acierno R. Common elements of the expert consensus guidelines for clinical videoconferencing. In: Tuerk P, Shore P, editors. Clinical videoconferencing in telehealth. Springer International Publishing; Switzerland: 2015. pp. 55–67. [Google Scholar]
- Wolf GK, Strom TQ, Kehle SM, Eftekhari A. A preliminary examination of prolonged exposure therapy with Iraq and Afghanistan veterans with a diagnosis of posttraumatic stress disorder and mild to moderate traumatic brain injury. Journal of Head Trauma Rehabilitation. 2012;27:26–32. doi: 10.1097/HTR.0b013e31823cd01f. doi: 10.1097/HTR.0b013e31823cd01f. [DOI] [PubMed] [Google Scholar]
- Wright KM, Huffman AH, Adler AB, Castro CA. Psychological screening program overview. Military Medicine. 2002;167:858–861. doi: 10.1037/e623152007-001. [PubMed] [Google Scholar]
- Yoder M, Tuerk PW, Price M, Grubaugh AL, Strachan M, Myrick H, Acierno R. Prolonged exposure therapy for combat-related posttraumatic stress disorder: Comparing outcomes for veterans of different wars. Psychological Services. 2012;9:16–25. doi: 10.1037/a0026279. doi: 10.1037/a002627. [DOI] [PMC free article] [PubMed] [Google Scholar]