Abstract
Purpose
Appropriate medio-lateral (ML) stability is an important factor of good clinical outcome following total knee arthroplasty (TKA). We hypothesized that a newly introduced Bi-Cruciate Stabilized substituting (BCS) prosthesis reduces the medio-lateral instability in mid-flexion range. The purpose of this study was to measure the ML stability (varus ligament balance) using a new tensor device after implantation of BCS TKA and to analysis the association between varus ligament balance and clinical results after TKA.
Materials and methods
We evaluated 33 patients who underwent 39 Journey. 2. BCS TKA using the measured resection technique. We measured the gaps after implantation from extension to full flexion with reduced patella by constant distraction force with 120N. The varus ligament balance gap was defined as the gap calculated by subtracting from Lateral to medial component gap. The clinical results at 2years after operation was compared with intraoperative varus ligament balance.
Results
Varus ligament balance showed its maximum gap at full knee extension and 120° flexion. Varus ligament balance at 30°, 60° and 90° of flexion were significant differences in the varus ligament balance at full extension. (* p < 0.05). The varus ligament balance gap was negatively corrected with postoperative 2011 Knee society score (patient’s satisfaction) (r = 0.661, p = 0.001).
Conclusions
The most important findings of the present study are that BCS TKA can reduces the ML instability in mid-flexion range, and improve simultaneously the patient’s satisfaction.
Level of evidence
Therapeutic study, Level III.
Keywords: Total knee arthroplasty, Medio-lateral stability, Patient’s satisfaction
Normal knee kinematic presents internal rotation of tibia up to 80° of knee flexion, femoral external rotation (approximately 20°–30°), femoral roll-back motion, and smooth patella tracking when tibial tubercle meets femoral groove in line (the mechanism known as medial pivot movement). Previous study showed that in flexing of knee from 0 to 120° the medial femoral condyle moved little, the lateral moved posteriorly by 17 mm by analysing sections of distal femurs in the computer. 1 and, in passive motion of the normal cadaveric knee using MRI, the medial femoral tibial compartment is in the form of “ball in socket”, the lateral femoral tibial compartment is in the form of “Mixed rooling and spinning with four-bar linkage. 2 Recently, guided motion total knee arthroplasty (TKA) implants that induce medial pivot movement have been introduced to the market such as the implant with a 3°-equivalent step between femoral component and tibial polyethylene insert, and the tibial polyethylene insert with ball-in socket type medially and semi-compatible arch type laterally at the articulation surface. However, they were all ACL deficient knees, and whether induction of medial pivot motion will occur or not is unclear. Journey. 2. Bi-Cruciate Stabilized prosthesis has two cam-post mechanism, which substitute for the anterior cruciate ligament and posterior cruciate ligament, and asymmetrical geometry of the tibial plateau surface. Therefore Journey.2.BCS must acquire the medial compartment tightness to induce medial pivot motion during flexion and extension as well as normal knee. The joint gap after implantation was loose at the mid-flexion ranges, especially at 30° of flexion using posterior stabilized (PS) TKA. 3, 4 We hypothesized that a newly introduced Journey. 2. BCS reduces the medio-lateral (ML) instability in mid-flexion range. The purpose of this study was to measure the ML stability using a new tensor device after implantation and to analysis the association between ML instability and clinical results at years after operation.
1. Materaials and methods
From September. 2014 to July. 2015, primary total knee arthroplasty (TKA) were performed using Journey. 2. BCS [39 knees. tibial component (size: 3), tibial surface (size: 9): Smith&Nephew. Inc. Memphis, TN. USA]. Post-operative full length hip-knee-ankle angle (176°≧,184°≦); flex angle of femoral component (2°≦); posterior inclination of tibial component (3°>,7°<) and rotation angle of tibial component (except. 0 ± 2°) using Zed Knee (LEXI, Tokyo, Japan. Fig. 1) based on postoperative CT images were excluded. All patients have been pointed out pre-operative medial knee osteoarthritis. Major reasons for exclusion were lateral knee osteoarthritis, inflammatory arthritis, post-traumatic osteoarthritis, osteonecrosis of the knee. The pre-operative demographic deta of the patients are shown in Table 1
Fig. 1.
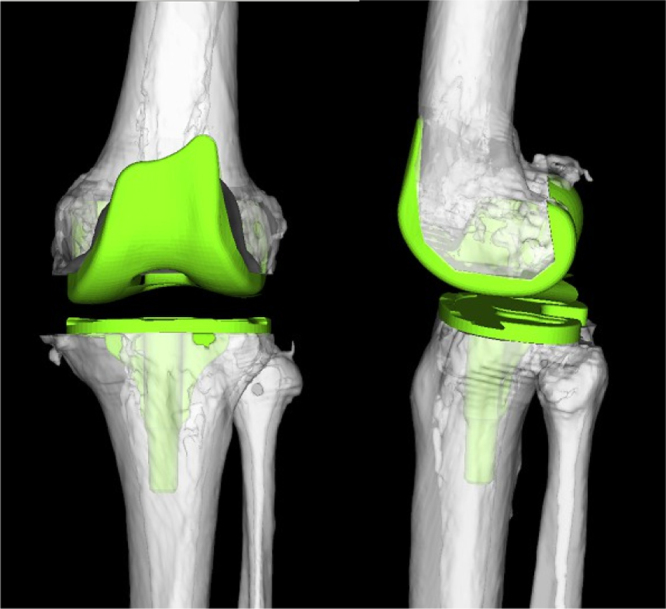
Photographs of Journey. 2. BCS TKA using Zed Knee (LEXI, Tokyo, Japan. Fig. 1) based on postoperative Computed tomography.
Table 1.
Patient’s demographic data.
| Parameter | Mean (SD) |
|---|---|
| Age (years) | 78 (6.5) |
| Male; female | 8; 31 |
| Height | 155 (12) |
| Body mass index | 24.4 (8.1) |
| Knee society score | |
| Knee score | 31.7 (17.1) |
| Function score | 39.8 (18.2) |
| Extension angle (degree) | −11 (8) |
| Flexion angle (degree) | 128 (19) |
| Pre-operative anatomical axis(degree) | 5.9 (5.2) varus |
| Post-operative anatomical axis(degree) | 5.2 (2.2) varus |
| Pre-operative mechanical axis(degree) | 14.2 (4.9) varus |
| Post-operative mechanical axis(degree) | 0.9 (1.2) varus |
1.1. Surgical procedure
In all cases, the TKA surgical procedure was performed by one author and was minimally invasive surgery, with a skin incision of 8–11 cm. The distal femoral cutting guide block was aligned using an intra-medullary guide, and the proximal tibia cutting block was aligned using an extramedullary guide. For the femur and tibia, a standard 6° valgus angle and posterior inclination 3° angle guide was used in all patients. The rotational alignment was adjusted to the surgical epi-condylar axis for the femoral component and medial third of tibia tuberosity at the level of patellar-tendon attachment for the tibia component. In addition, femoro-tibial rotational mismatch was reconfirmed at extension, and anterior pin fixation of tibial component trials was kept available (Fig. 2).
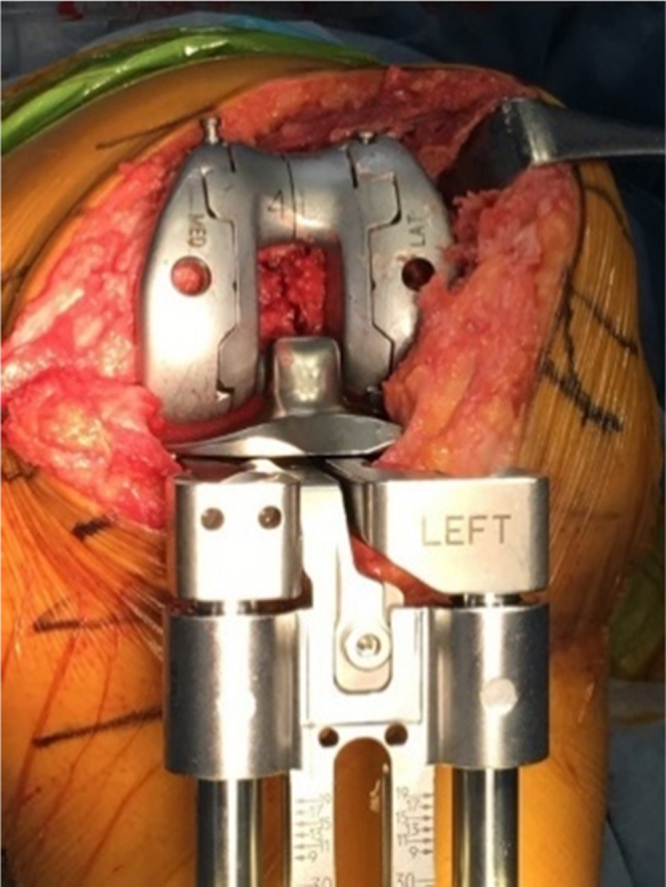
Fig. 2.

Photographs showing the tibia trial component. We have created to be able to fix pin in front of tibia component trial to avoid the rotational mismatch.
1.2. Joint gap after implantation (component gap)
The extension gap was measured with the femoral trial component using force-controlled compartment-specific ligament tensor device. The tensor device of three parts: an upper seesaw plate, a lower platform plate, and an extra-articular mainbody and presents two measurements: medial and lateral joint gap between the seesaw plate and the platform plate (Fig. 3). The upper plate has identical shape as polyethylene surface trial (size: 9) of Journey. 2. BCS (Fig. 4). The lower plate has 1 pin holes. One pins and the foot of the device firmly fixed the body of tensor device to the tibia (size: 3 of tibial component. Fig. 5). The surgeon can evaluate soft tissue balance under a constant joint distraction force between the seesaw plate and platform plate from 60N × 2 of ideal component gap of stiffness transition pointed by Heesterbeek.P.J.C after the reduction of patellar femoral joint. 5 The amount of force for pre-tensioning the gaps is based on clinical experience of more than 5 years. The medial and lateral component gap were defined as the gap calculated by subtracting the selected thickness of the tibial component. Medio-lateral stability (varus ligament balance) was defined as the gap calculated by subtracting from Lateral to medial component gap and were measured at full extension, 30°, 60°, 90°, 120° flexion. The measurements with the tensor device were obtained four times by one surgeon, and the average was used for data. All the patients followed the same post-operative rehabilitation protocol. This retrospective study was approved by the institutional review boards of our hospitals, and all patients were given informed consent.
Fig. 3.
Photographs showing the new tensor. The attachment can be interchangeable depending on the the same articular shapes as that the tibial liner, including anterior and posterior structure.
Fig. 4.

Photographs showing the new tensor. The upper plate has identical shape as polyethylene surface trial (size: 9) of Journey. 2. BCS.
Fig. 5.
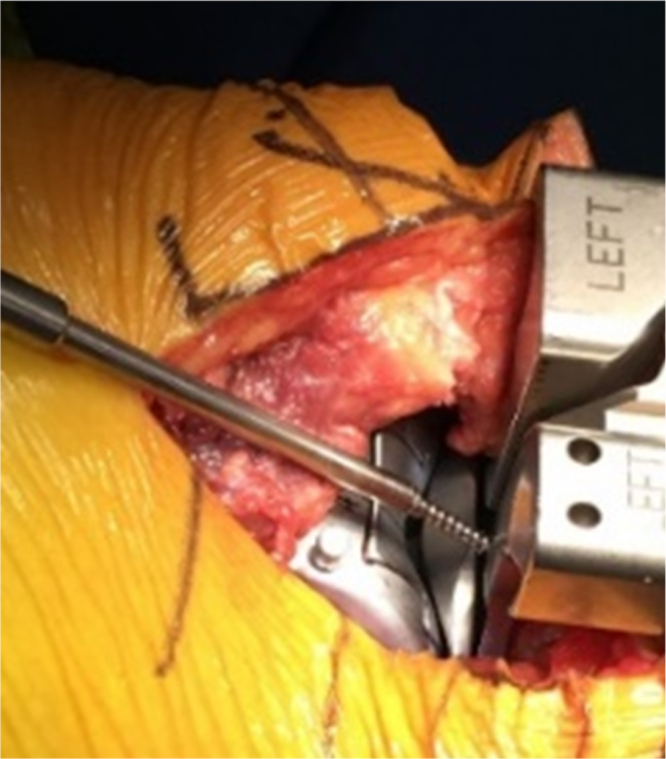
Photographs showing the new tensor. The lower plate has 1 pin holes. One pins and the foot of the device firmly fixed the body of tensor device to the tibia.
1.3. Assessment of correlations and statistical analysis
The correlations between intraoperative mediaolateral component gap, varus ligament balance using a new tensor device and post-operative flexion angle were evaluated. All measurements were expressed in the format of mean ± standard deviation. Pearson correlation coefficient was utilized to analyze the strength of correlation (version 24.0; SPSS, Chicago, IL). Analysis of variance (ANOVA) with post hoc Turkey test was used. This study was approved by the institutional review board of our facility, and every patient in this study submitted the informed consent.
2. Results
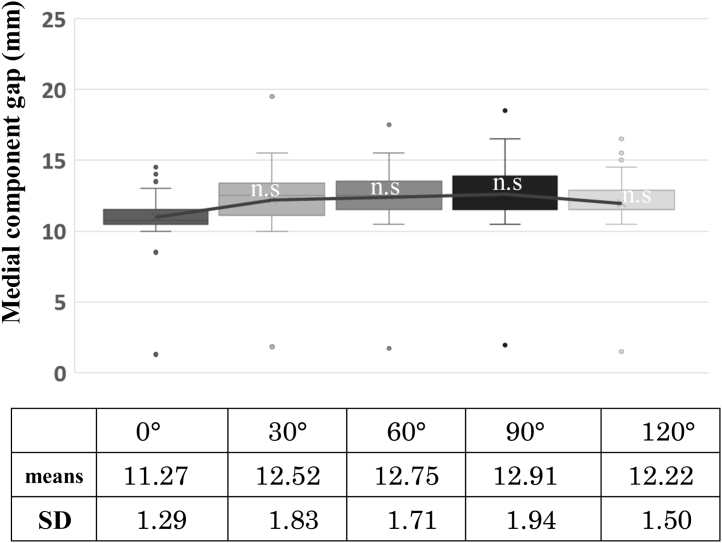
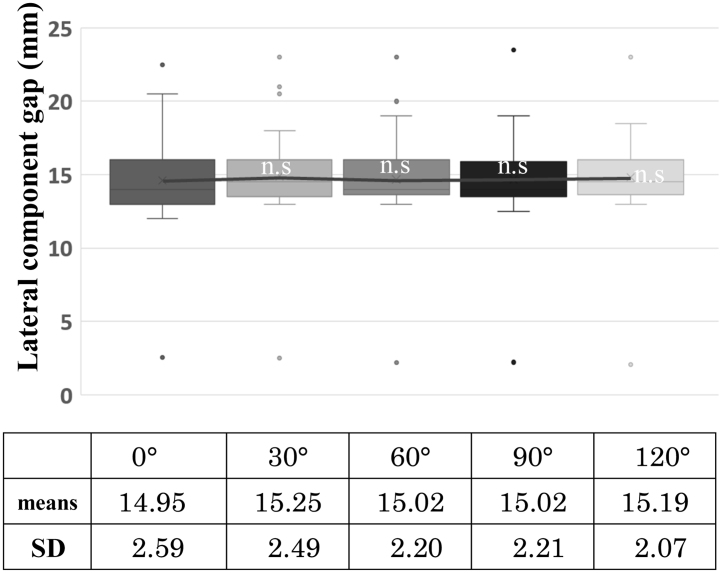
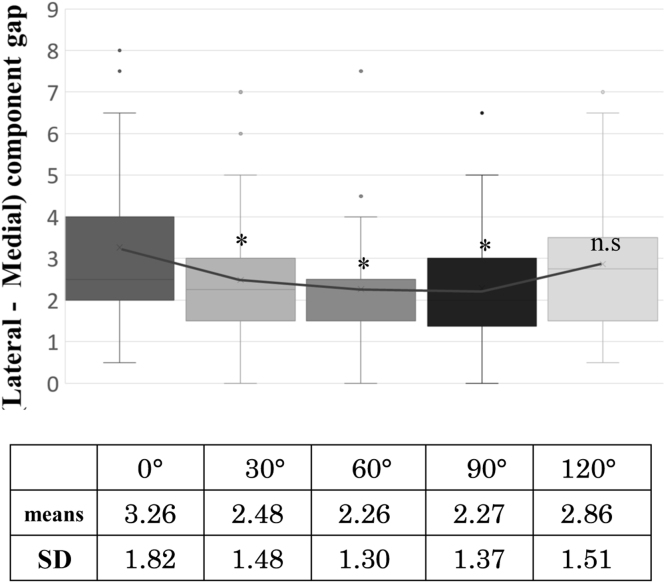
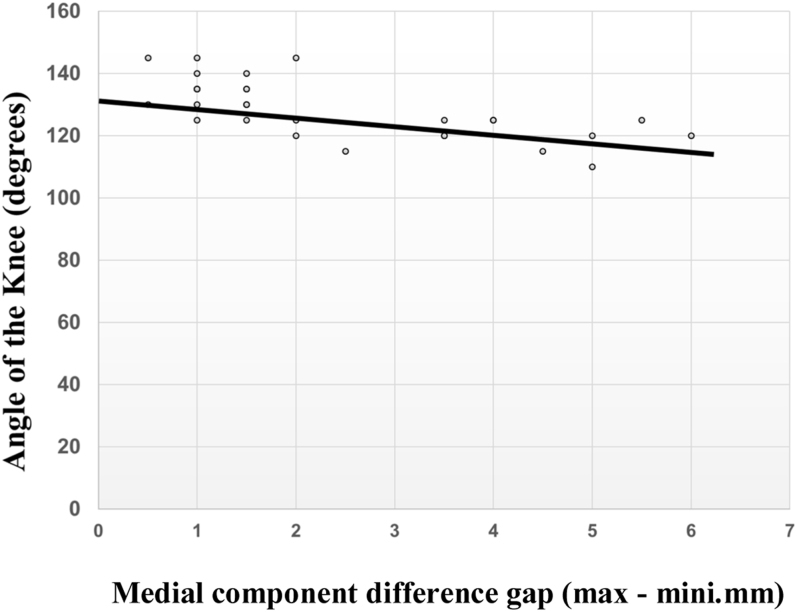
The mean medial component gaps were 12.3 ± 1.6 mm (Fig. 6) and the lateral component gaps were 15.0 ± 2.31 mm (Fig. 7). There were not significant differences in the mediolateral joint gap during full extension to 120° flexion (n.s vs full extension). Varus ligament balance showed its maximum gap at full knee extension and 120° flexion. No mid-flexion instability was observed at 30°, 60° and 90° of flexion (Fig. 8). There were significant differences in the mediolateral joint gap during full extension to 120° flexion (n.s vs full extension). Medial tightness, defined as the value of maximum medial component gap subtracted by its minimum value, showed strong negative correlation with knee flexion angle at post-operative 2 years (r = − 0.688, P < 0.001, Fig. 9). Varus ligament balance showed a negative correlation at post-operative 2 years (r = − 0.425, P < 0.002, Fig. 10). The varus ligament balance with 30,60° of flexion angles was negatively corrected with postoperative 2011 Knee society score (patient’s satisfaction) (r = − 0.670, p < 0.002, Fig. 11. r = − 0.430, p < 0.001, Fig. 12).
Fig. 6.
Graphs showing the medial component gap. The medial component gap was nearly constant at 12.3 ± 1.6mm(SD) from the extension to flexion angle of the knee. There were not significant differences in the medial joint gap during full extension to 120° flexion (n.s vs full extension). Means and SD were provided.
Fig. 7.
Graphs showing the lateral component gap. The lateral component gap was 15.3 ± 2.31 mm(SD) from the extension to flexion angle of the knee. There were not significant differences in the lateral joint gap during full extension to 120° flexion (n.s vs full extension). Means and SD were provided.
Fig. 8.
Graphs showing Varus ligament balance (lateral-medial component gap). The gap was dilated in extension and 120 °flexion angle of the knee. Varus ligament balance at 30°, 60° and 90° of flexion were significant differences in the varus ligament balance at full extension. * p < 0.05). The mid-flexion was not recognized the instability of knee.
Fig. 9.
Graphs showing the relationship between medial component difference gap (max-mini) and post-operative angle of the knee. The medial component difference gap (max-mini) was negatively corrected with postoperative knee flexion angle (r = −0.668, p < 0.001).
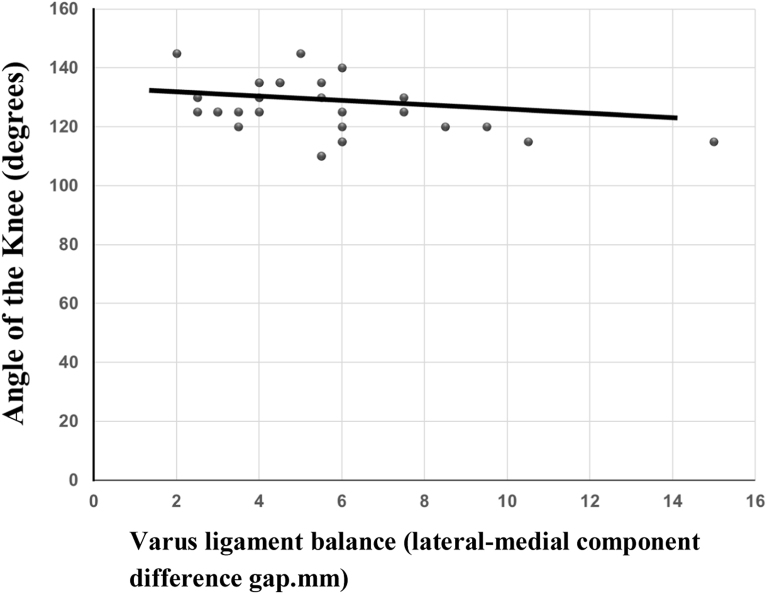
Fig. 10.
Graphs showing the relationship between varus ligament balance (lateral-medial component gap)and post-operative angle of the knee. The Varus ligament balance was negatively corrected with postoperative knee flexion angle (r = 0.425, p < 0.002).
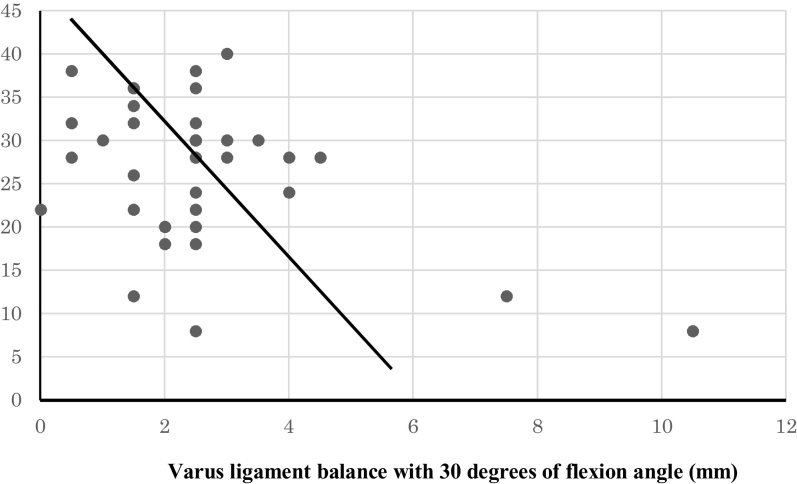
Fig. 11.
Graphs showing the relationship between varus ligament balance with 30° of flexion angle and patient’s satisfaction. The Varus ligament balance was strong negatively corrected with postoperative knee flexion angle (r = 0.670, p < 0.002).
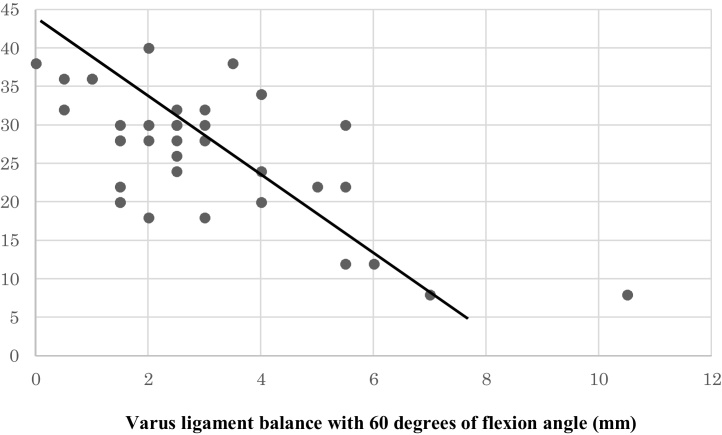
Fig. 12.
Graphs showing the relationship between varus ligament balance with 60° of flexion angle and patient’s satisfaction. The Varus ligament balance was negatively corrected with postoperative knee flexion angle (r = 0.430, p < 0.001).
3. Discussion
To the best of our knowledge, this is the first report which analyzed the relationship between varus ligament balance and clinical results after implantation of femoral component trial, patellar component trial, and as polyethylene surface trial as identical shape of Journey. 2. BCS. The most important findings of this study were that the medial component gap after implantation was constant throughout range of motion in Journey.2.BCS TKA, therefore revealed the acquisition of medial tightness that is required for medial pivot movement. Subjects could achieve post-operative flexion of 120°or more when the medial tightness showed 2 mm or less. A newly BCS TKA improve medio-lateral instability in mid-flexion range and improve patient’s satisfaction. The anterior shift of femoral component relative to tibial component, triggered by anterior cam’s anterior stabilizing mechanism of Journey.2.BCS TKA, did not cause decreases in the mediolateral component gap at full knee extension due to projection of component against capsule, and revealed the same physiological lateral laxity as normal knees. None of our cases required medial release to equalize medial component gap with lateral. No instability was identified at mid-flexion range, which can be found in conventional PS TKA. The varus ligament balance with 4 mm or more showed to decrease post-operative flexion. The result also suggested the reduced amount of rollback of femoral component due to changes in the contact area of anterior and posterior cam with a post. The advantage of this study was to use the specially designed tensor device which had the same design as Journey.2.BCS TKA fairly reproduce the conditions after implantation. We discussed that BCS TKA fairly reproduce the coronal laxity of the healthy knee, possibly due to the asymmetric cam mechanism and is a prosthesis that can be expected to improve patient’s satisfaction. Recent report by kurita et al., 6 has shown that the postoperative knee joint kinematics especially in the midflexion range was influenced by the sharpe of articulating surface of TKA. We believed that our study reproduced the joint gap kinenmatics after implantation. Bi-cruciate substituting TKA (Journey.BCS), the former model of Journey.2.BCS design demonstates femoral rollback at 90° with an average of 14 mm for the MFC and 23 mm for the LFC, and 10°internal tibial rotation. 7, 8, 9 Additionally, it provides increased sagittal stability during early flexion and an improved pivot shift (indicating improved anterior stabilization). But, Luycks et al. documented the major revision rate of 2.0% to induce friction between iliotibial band and femoral component with the grater rotational allowance after implantation of the Journey.BCS. 10 In addition, the study on the comparison of Journey. BCS and Genesis II PS (PS TKA, Smith & Nephew Inc.: Memphis, TN) found no clinical significance in the maximum flexion angle at post-operative 2years follow-up. 11 Mugnai et al. reported a comparison of Journey. BCS and Non-restrictive Geometry (NRG: posterior – stabilized knee system. Stryker Orthopedics. Inc, Mahwah, NJ) in post-operative 29 months, and showed the onset of post-operative stiff knee of 2.7% in Journey BCS versus 0.5% in NRG. The onset of stiff knee, Mungnai et al., was triggered by the emergence of intra-articular fibrillizations caused by them mechanical stress towards soft tissue due to excessive rollback of femoral component. 12 The current study has also experienced the same issue as Journey 1 BCES among approximately 2% of our subjects (2 out of 94) due to the anterior shift of femoral component relative tibial component due to the anterior supporting mechanism of anterior cam. Further countermeasures are required to be taken in the future cases.
There are several limitations to this study.
First, this is a case-series study with a lack of conrtol subjects. Second, this study was limited to the medial knee osteoarthritis in which surgery had been performed with Journey. 2. BCS TKA, therefore, valgus knee and other diseases cannot be generalized by our results. Third, there is a possibility that the thickness of cement mantle, because component gap was measured before cementing.
4. Conclusion
Journey 2 BCS which substitutes the function of ACL and PCL (anterior and posterior cam post) can acquire the medio-lateral stability in mid-flexion range and the medial tightness that induces the same medial pivot movement as the normal knees, and improve simultaneously the patient’s satisfaction.
Conflict of interest
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Acknowledgement
The authors thank Hiroaki Suzuki and Eriko Kuroiwa for their assistance in this study.
References
- 1.Kurosawa H., Walker P., Abe S., Garg A., Hunter T. Geometry and motion of the knee for implant and prosthetic design. J Biomech. 1985;18(7):487–499. doi: 10.1016/0021-9290(85)90663-3. [DOI] [PubMed] [Google Scholar]
- 2.Pinskerova V., Iwaki H., Freeman M.A.R. The shapes and relative movements of the femur and tibia at the knee. Orthopade. 2000;29(1):S3–S5. doi: 10.1007/pl00003679. [DOI] [PubMed] [Google Scholar]
- 3.Minoda Y., Nakagawa S., Sugama R., Ikawa T., Noguchi T., Hirakawa M. Midflexion laxity after implantation was influenced by the joint gap balance before implantation in TKA. J Arthroplast. 2015;30:762–765. doi: 10.1016/j.arth.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 4.Minoda Y., Nakagawa S., Sugama R. Intraoperative assessment of midflexion laxity in total knee prosthesis. Knee. 2015;21:810–814. doi: 10.1016/j.knee.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 5.Heesterbeek P.J.C., Haffner N., Wymenga A.B., Stifter J., Ritschl P. Patient-related factors influence stiffness of the soft tissue complex during intraoperative gap balancing in cruciate-retaining total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015 doi: 10.1007/s00167-015-3694-5. [Epub ahead of print:] [DOI] [PubMed] [Google Scholar]
- 6.Kurita M., Tomita T., Yamazaki T. In vivo kinematics of high-flex mobile-bearing total knee arthroplasty, with a new post-cam design, in deep knee bending motion. Int Orthop. 2012;36(12):2465–2471. doi: 10.1007/s00264-012-1673-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Victor J., Mueller J.K., Komistek R.D., Sharma A., Nadaud M.C., Bellemans J. In vivo kinematics after a cruciate-substituting TKA. Clin Orthop Relat Res. 2010;468(3):807–814. doi: 10.1007/s11999-009-1072-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Catani F., Ensini A., Belvedere C. In vivo kinematics and kinetics of a bi-cruciate substituting total knee arthroplasty. J orthop Res. 2009;27(12):1569–1575. doi: 10.1002/jor.20941. [DOI] [PubMed] [Google Scholar]
- 9.Victor J., Bellemans J. Physiologic kinematics as a concept for better flexion in TKA. Clin Orthop Relat Res. 2006;452:53–58. doi: 10.1097/01.blo.0000238792.36725.1e. [DOI] [PubMed] [Google Scholar]
- 10.Luyckx L., Luyckx T., Bellemans J. Iliotibial band traction syndrome in guided motion TKA. A new clinical entity after TKA. Acta Orthop Belg. 2010;76:507–512. [PubMed] [Google Scholar]
- 11.Schimmel J.J.P., Defoort K.C., Heesterbeek P.J.C., Wymenga A.B., Jacobs W.C.H., van Hellemondt G.G. Bicruciate substituting design does not improve maximal flexion in total knee arthroplasty. J Bone Joint Surg Am. 2014;96(81):1–8. doi: 10.2106/JBJS.M.00277. [DOI] [PubMed] [Google Scholar]
- 12.Mugnai Raffale, Digennaro Vitantonio, Ensini Andrea, Leardini Alberto, Catani Fabio. Can TKA design affect the clinical outcomes? Comparison between two guided-motion systems. Knee Surg Sports Traumatol Arthrosc. 2014;22:581–589. doi: 10.1007/s00167-013-2509-9. [DOI] [PubMed] [Google Scholar]