A 52-year-old man who had hypoglycaemia for 8 years was found to have endogenous hyperinsulinism indicating an insulinoma. Abdominal MRI, CT perfusion, endoscopic ultrasonography, and 99mTc-HYNIC-TOC SPECT/CT were negative. Thus, the patient was referred for 68Ga-NOTA-exendin-4 PET/CT with the approval of the Institutional Review Board of our hospital.
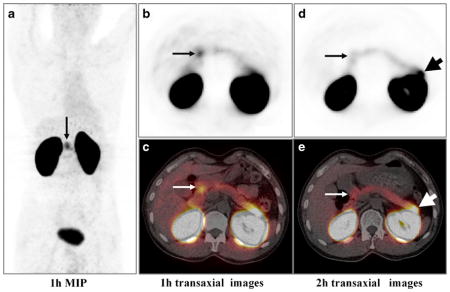
As well as the intense physiological distribution in the kidneys and bladder due to urinary excretion, moderately elevated uptake is apparent in the proximal duodenum (a–c long arrows, SUVmax 5.2) and pancreas (SUVmax 2.9) at 1 h after injection of 68Ga-NOTA-exendin-4. Because visualization of the pancreas tail was significantly influenced by the intense radioactivity in the left kidney, the patient was reimaged at 2 h after injection. A lesion with intense uptake (SUVmax 20.7) was clearly seen in the pancreas tail (d, e short arrows). Interestingly, radioactivity in the proximal duodenum significantly decreased (d, e long arrows, SUVmax 2.3) while the appearance of the normal pancreas remained unchanged.
The patient recovered from hypoglycemia after surgical removal of the pancreas tail insulinoma (WHO grade 1). Intraoperative ultrasonography excluded a duodenal tumor.
Glucagon-like peptide-1 receptor (GLP-1R) is highly overexpressed in insulinoma [1, 2]. SPECT/CT imaging of GLP-1R using 111In-labelled or 99mTc-labelled exendin-4 has been shown to be highly accurate in the detection of insulinoma [2–4]. However, PET/CT imaging of GLP-1R has rarely been reported [5]. We present the first successful use of 68Ga-NOTA-exendin-4 PET/CT for the identification of an occult insulinoma that could not be detected by other standard imaging methods. 68Ga-NOTA-exendin-4 also shows great potential for evaluation of pancreatic physiology due to its uptake, presumably, by islet cells.
Acknowledgments
This work was partly supported by a Special Scientific Research Fund for Public Welfare Professions of China (201402001) and NIBIB intramural research program.
Footnotes
Conflicts of interest: None.
Contributor Information
Yaping Luo, Department of Nuclear Medicine, Chinese Academy of Medical Sciences and Peking Union Medical College Hospital, Beijing 100730, People’s Republic of China.
Miao Yu, Department of Endocrinology, Chinese Academy of Medical Sciences and Peking Union Medical College Hospital, Beijing 100730, People’s Republic of China.
QingQing Pan, Department of Nuclear Medicine, Chinese Academy of Medical Sciences and Peking Union Medical College Hospital, Beijing 100730, People’s Republic of China.
Wenming Wu, Department of General Surgery, Chinese Academy of Medical Sciences and Peking Union Medical College Hospital, Wangfujing, Dongcheng District, Beijing 100730, People’s Republic of China.
Taiping Zhang, Department of General Surgery, Chinese Academy of Medical Sciences and Peking Union Medical College Hospital, Wangfujing, Dongcheng District, Beijing 100730, People’s Republic of China.
Dale O. Kiesewetter, Laboratory of Molecular Imaging and Nanomedicine, National Institute of Biomedical Imaging and Bioengineering, National Institutes of Health, Bethesda, MD 20892, USA
Zhaohui Zhu, Department of Nuclear Medicine, Chinese Academy of Medical Sciences and Peking Union Medical College Hospital, Beijing 100730, People’s Republic of China.
Fang Li, Department of Nuclear Medicine, Chinese Academy of Medical Sciences and Peking Union Medical College Hospital, Beijing 100730, People’s Republic of China.
Xiaoyuan Chen, Laboratory of Molecular Imaging and Nanomedicine, National Institute of Biomedical Imaging and Bioengineering, National Institutes of Health, Bethesda, MD 20892, USA.
Yupei Zhao, Department of General Surgery, Chinese Academy of Medical Sciences and Peking Union Medical College Hospital, Wangfujing, Dongcheng District, Beijing 100730, People’s Republic of China.
References
- 1.Korner M, Stockli M, Waser B, Reubi JC. GLP-1 receptor expression in human tumors and human normal tissues: potential for in vivo targeting. J Nucl Med. 2007;48:736–43. doi: 10.2967/jnumed.106.038679. [DOI] [PubMed] [Google Scholar]
- 2.Korner M, Christ E, Wild D, Reubi JC. Glucagon-like peptide-1 receptor overexpression in cancer and its impact on clinical applications. Front Endocrinol. 2012;3:158. doi: 10.3389/fendo.2012.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christ E, Wild D, Forrer F, Brandle M, Sahli R, Clerici T, et al. Glucagon-like peptide-1 receptor imaging for localization of insulinomas. J Clin Endocrinol Metab. 2009;94:4398–405. doi: 10.1210/jc.2009-1082. [DOI] [PubMed] [Google Scholar]
- 4.Sowa-Staszczak A, Pach D, Mikolajczak R, Macke H, Jabrocka-Hybel A, Stefanska A, et al. Glucagon-like peptide-1 receptor imaging with [Lys40(Ahx-HYNIC-99mTc/EDDA)NH2]-exendin-4 for the detection of insulinoma. Eur J Nucl Med Mol Imaging. 2013;40:524–31. doi: 10.1007/s00259-012-2299-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eriksson O, Velikyan I, Selvaraju RK, Kandeel F, Johansson L, Antoni G, et al. Detection of metastatic insulinoma by positron emission tomography with [68Ga]exendin-4 – a case report. J Clin Endocrinol Metab. 2014;99(5):1519–24. doi: 10.1210/jc.2013-3541. [DOI] [PMC free article] [PubMed] [Google Scholar]


