Abstract
Background:
Onset of trigeminal neuralgia (TN) is uncommon in young adults with less favorable benefit from surgical interventions. The aim of this study was to evaluate the role of concomitant psychosomatic disorders in long-term surgical outcomes in this population.
Methods:
Twenty-one patients younger than 30 years of age were diagnosed initially as having medically refractory TN, and each patient underwent microvascular decompression (MVD) as initial surgical management. Correlation of clinical outcome and psychosomatic disorders (DSM-IV) was evaluated during a 15-year interval.
Results:
A total of 93 procedures were performed for the management of TN and subsequent iatrogenic craniofacial pain disorders. At a median of 81 months, 8 of 21 patients were free of facial pain. Fourteen patients with concomitant major depressive disorder (MDD) or other anxiety disorders underwent a higher median of procedures compared with 7 patients without known MDD or anxiety (4.5 versus 1 intervention, P = 0.038). Two of 14 patients who were diagnosed with MDD or other anxiety disorders were free of craniofacial pain, whereas 6 of 7 patients without mood or anxiety disorders were free of craniofacial pain (P = 0.0005). Thirteen patients developed treatment-related complications that required further surgical procedures. Presence of MDD or other anxiety disorders was associated with higher rate of complications (P = 0.026). One patient with past medical history of severe anxiety died of unknown causes.
Conclusions:
In young patients with TN, comorbid MDD or anxiety disorders was associated with seeking multiple invasive procedures in multiple academic centers with limited benefit and high rates of surgical induced complications.
Keywords: Anxiety, depression, surgical intervention, trigeminal neuralgia
INTRODUCTION
The incidence of trigeminal neuralgia (TN) increases with age, peaking by the 5th and 6th decades of life. However, a small incidence of TN occurs in the younger population as well.[3,35] Patients with refractory TN undergo microvascular decompression (MVD) or ablative procedures.[3,19,21,22,27] Data regarding the role of surgical management in the younger TN patient population are limited. In prior studies reporting the outcomes of MVD in the younger versus older patient population, a lower efficacy for MVD in the younger population has been reported, suggesting that vascular compression is not the main etiology of pain in this group.[2,24] A recent population-based cohort study revealed that depression and anxiety disorders are more common in patients with TN.[34] Further, several reports have demonstrated that facial pain could be controlled with antidepressants strategies.[8,13,17,20] suggesting that depression and anxiety could play an important role in the pathogenesis of pain in some patients with TN. In this report, our aim was to evaluate whether comorbid psychiatric disorders could predict long-term clinical outcome in young patients with TN.
MATERIALS AND METHODS
Study population
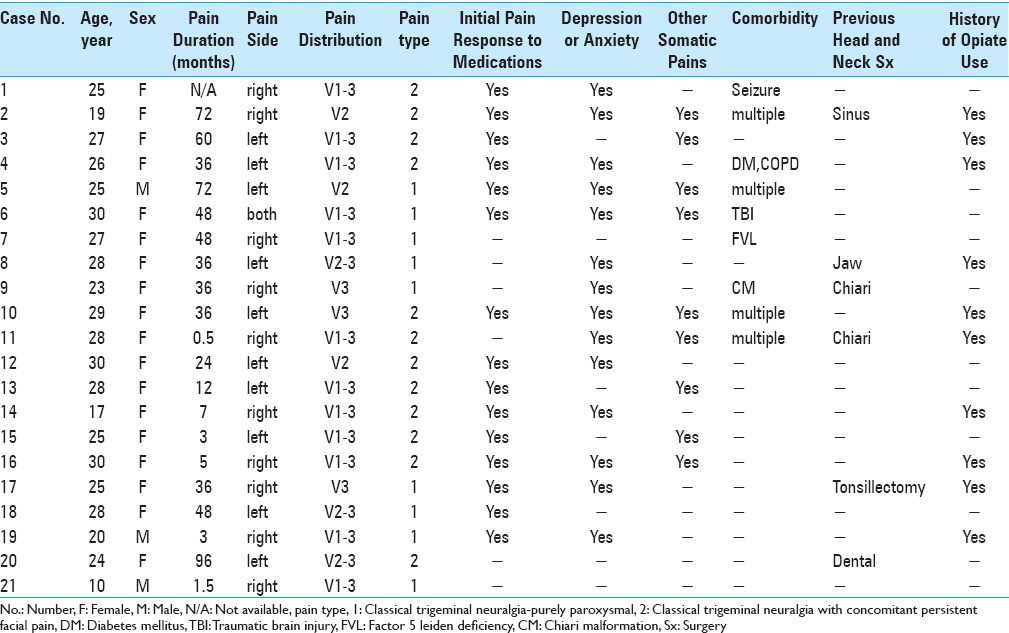
This study was conducted with the approval of the University of Pittsburgh Institutional Review Board. We retrospectively identified 25 medically refractory idiopathic TN patients, younger than 30 years of age, all of whom underwent initial MVD between January 2000 and December 2014. Four patients were lost to follow-up and 21 patients enrolled in study. No patient had an identified structural or demyelinating lesion as a cause of TN. Sixteen patients had at least some initial pain relief with medications. Four patients had poor response to medication, and one patient could not tolerate the side effects of medications. TN was categorized using Burchiel classification.[6] At the time of presentation, one patient presented with bilateral TN. One patient had undergone a prior MVD at another medical center. The median age at the time of pain onset was 23 years, and the median age at the time of surgical intervention was 26 years. Median follow-up for this registry was 81 months (6 to 182 months). General patient demographic information such as age, sex, general health conditions, and other comorbidities were collected as well as characteristics related to their TN and treatment including pain location, pain onset, Barrow Neurological Institute (BNI) pain classification post-treatment, duration of symptoms before first MVD, symptom progression, medications, therapeutic response to medical treatment, therapeutic response to MVD, TN-related comorbidities, surgical-related comorbidities, and presence of further surgical procedures. The patients’ presurgical demographics are shown in Table 1.
Table 1.
Patients demographics
Surgical technique
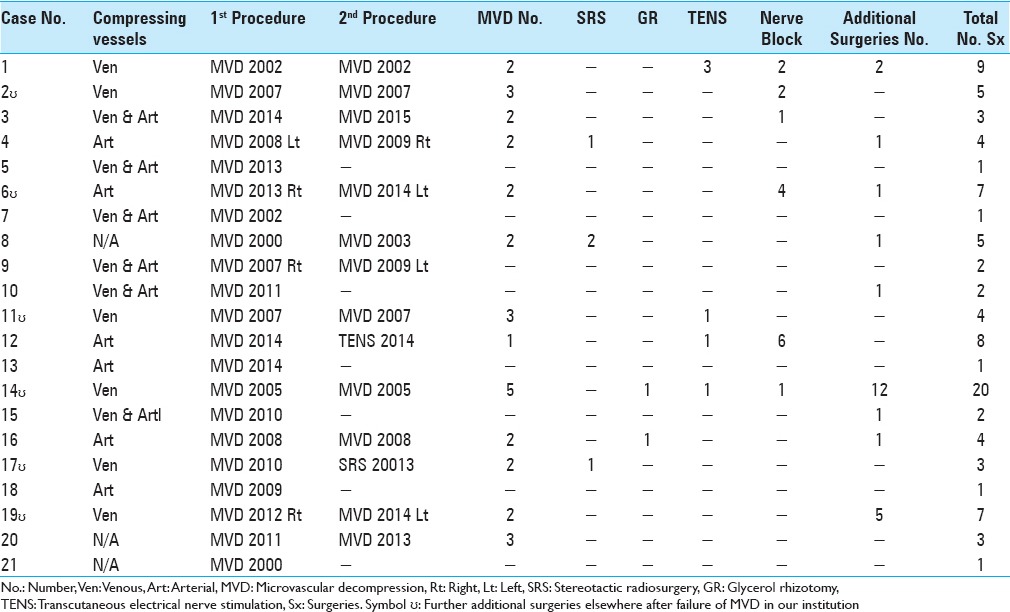
MVD was performed using the standard approach as described previously.[25] Briefly, a retromastoid incision was made behind the hairline, and a small retrosigmoid craniectomy was performed. The intersection of the transverse sinus and sigmoid sinuses was identified, and the dura was opened. After appropriate brain relaxation was achieved with CSF drainage, the cisternal portion of the trigeminal nerve was exposed and examined for vascular contact. Compressive arteries and veins were decompressed with soft implants or through elimination by electrocautery. Intraoperative findings are summarized in Table 2.
Table 2.
Patients surgical procedures
Follow-up and data collection
The patient medical records were reviewed and pertinent information was recorded. Patients were contacted by telephone for additional information by two authors (SHM/BA) who did not provide patient care to any of the patients included. The results were analyzed in order to determine the clinical outcomes in this population following therapeutic interventions. Patients’ psychological history was reviewed retrospectively from medical records or contacting patients. Patients were specifically asked whether they underwent additional surgical procedures in other centers during the course of their pain history. Diagnosis of psychological disorder was made based on DSM-IV-TR criteria.[1]
RESULTS
Surgical approaches and clinical outcome
Patients in this series had a median of 3 procedures for the management of TN. For management of TN and surgically induced complications, 21 patients underwent 93 procedures. Four patients each had an additional MVD for TN onset on the contralateral side (three onsets of which developed post-initial ipsilateral MVD). Nine patients developed ipsilateral occipital neuralgia after MVD and underwent additional surgical interventions or nerve block. Patients’ operative procedures are shown in Table 2.
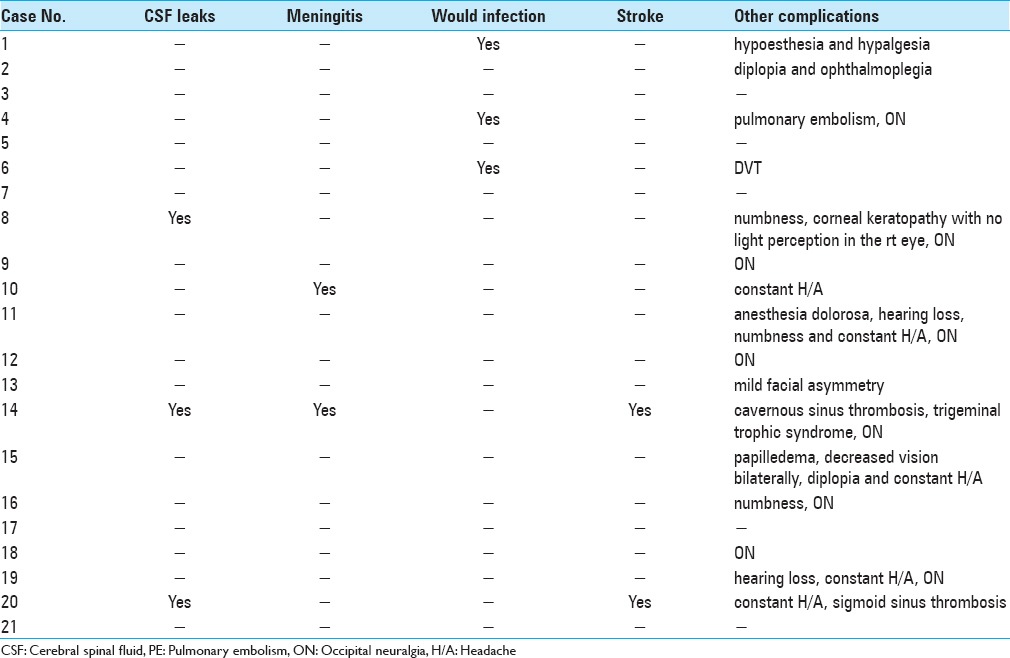
Fourteen patients initially responded to MVD with a median of 17 months of pain relief. Among the 14 patients with initial pain relief, 9 patients underwent additional interventions for management of pain recurrence, which was successful in 3 patients. At a median of 81-months follow-up, 8 patients were pain free. Thirteen patients suffered from side effects to interventions. While 2 patients had to leave college, another 4 had to stop their occupations due to intolerable pain. Furthermore, one patient was found dead in his apartment for an undisclosed reason 11 months after his last MVD. There were no statistically significance correlations between patients’ pain type, number of surgical interventions, and pain outcomes. Surgical outcomes and complications of patients are presented in Tables 3 and 4.
Table 3.
Patients clinical outcome
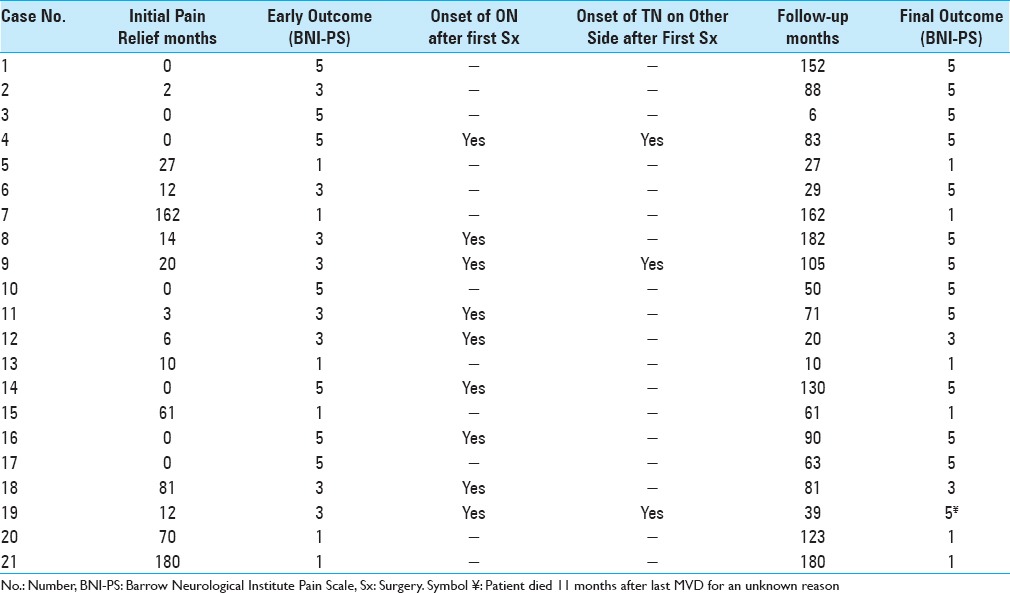
Table 4.
Surgical induced complications
Effect of additional depression and anxiety disorders in pain control
Reviewing the medical records, aside from facial pain, 17 patients were diagnosed with additional major depressive disorder (MDD), anxiety disorders, or somatic pain disorders (DSM IV-TR). Nine patients had concomitant MDD, of which 7 were on antidepressant medications. Eleven patients had other anxiety disorders, of which 8 were on antianxiety medications. Four patients were diagnosed with fibromyalgia, and 3 patients reported severe migraine prior to initial surgery.
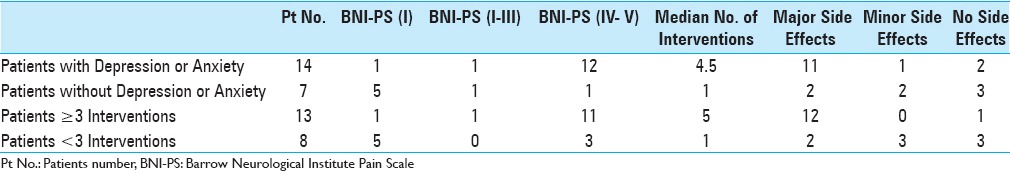
Patients with concomitant MDD and GAD underwent a median of 4.5 versus 1 invasive intervention for patients without comorbid psychiatric disorder (P = 0.038, Fisher's exact test). TN was relieved with and without medication in only 2 of the 14 patients with such disorders; however, in 6 out of the 7 patients without known MDD or GAD, TN was relieved with or without medication (P = 0.0005, Fisher's exact test). Presence of depression or other anxiety disorders was also associated with higher rate of surgical induced complications (P = 0.026, Fisher's exact test). Pain intensity score in relation to number of therapeutic interventions in association with other somatic pain syndromes, MDD, GAD, and complications are summarized in Table 5.
Table 5.
Role of Depression and Anxiety in TN outcome
DISCUSSION
This report provides additional evidence that MVD and further surgical procedures failed to provide pain relief in a majority of younger patients diagnosed with TN. Similar results have been reported elsewhere.[24] A lower response to multiple surgical interventions and a high incidence of new facial pain syndromes after surgical procedures suggests that vascular compression may not be the primary or sole etiology in this population, as formerly proposed.[3] The presence of additional MDD, GAD, higher rates of opiate consumption, and higher rates of patient's undergoing multiple surgical procedures in several different institutions suggests that TN symptoms in younger patients may be a part of psychological factors affecting other medical conditions (DSM-5).[10] The essential feature of psychological factors affecting other medical conditions is the “presence of one or more clinically significant psychological or behavioral factors that adversely affect a medical condition by increasing the risk for suffering, death, or disability. These factors can adversely affect the medical condition by influencing its course or treatment, by constituting an additional well-established health risk factor, or by influencing the underlying pathophysiology to precipitate or exacerbate symptoms to necessitate medical attention.” (DSM-5) Hence, we argue that it is critical, especially in young patients with TN and comorbid psychiatric illness, to look beyond vascular compression as the sole etiology of distress in these patients.
In 1947 and 1951, McElin and Horton followed by Engel, respectively, suggested that atypical facial pain was a secondary manifestation of primary psychiatric disturbances in two separate studies.[8,20] In 1949, Janjigian et al. reported three cases of TN apparently cured by electroshock therapy.[13] In 1966, Lascelles performed the first clinical trial showing patients with known symptoms of depression coinciding with atypical facial pain, administration of antidepressants resulted in complete pain relief in majority of patients.[17] In 1984, Feinmann et al. reported that antidepressants in the absence of diagnosed psychiatric disorders in patients with facial pain resulted in 81% being pain free, and minimal surgical intervention for facial pain was a positive predictor of pain relief.[9] In general, patients with any pain and comorbid MDD have a worse prognosis in pain control compared with patients without MDD;[11,12,16,18,26,28,29,31] pain control appears to be more achievable when MDD is also under control in such patients.[15,17,33] Nevertheless patients with psychiatric disorders more often seek care for somatic pain.[16] This could be due to the proposed common biological pathway mediating pain and depression in the central nervous system.[23]
The exacerbatory effects of depression on the severity of painful stimuli may be of particular importance for patients with TN.[4,7,16,32] Due to the severity of pain, depressed TN patients may be even more inclined to undergo invasive procedures if their TN remains uncontrolled.[14,30] MVD, as the most durable invasive treatment for TN, has a high reported success rate in several studies composed of adults primarily aged 5 to 87 years (median: 57 years).[3,5] However, if TN is refractory to MVD, patients often elect to undergo additional procedures because of their inability to tolerate the pain of TN. It has been reported that, in the setting of failed initial MVD, repeat MVD has a lower efficacy of affording patient pain relief.[3] In a younger patient population, pain and depression coupled with repeated surgeries that fail to provide pain relief from TN has severe consequences. In this study, we show that, in patients with comorbid psychiatric illness, the majority of the additional surgical interventions, following an initial procedure that did not provide pain relief, were performed in other institutions. Yet none of those were beneficial and increased the number of surgical procedures often leading to additional surgical complications.
Study limitations
While our results demonstrate an important concept in the management of young patients with TN, this study did not have a nonintervention control group. However, the absence of a nonintervention control group was unavoidable due to ethical considerations. More important, because our study was cross-sectional and our analyses correlational, we cannot address causality, whether MDD or GAD onset occurred before, after, or concurrently with TN onset in our patient population. In addition, our patients’ population due to rare incidence of TN in young individuals was small. Furthermore, due to separation of two primary surgeons from the University, it is not clear whether some of these patients were misdiagnosed with TN, while they might have actually suffered from atypical facial pain.
CONCLUSION
Our results suggest that in the presence of MDD and anxiety disorders younger patients with TN seek multiple invasive procedures in different institutions with limited benefit. Therefore, management of these patients should include an initial psychiatric evaluation and appropriate treatment, if needed, before initial surgery is recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Seyed H. Mousavi, Email: mousavish@upmc.edu.
Raymond F. Sekula, Email: sekularf@upmc.edu.
Ariel Gildengers, Email: gildengersag@upmc.edu.
Paul Gardner, Email: gardpa@upmc.edu.
L. Dade Lunsford, Email: lunsld@upmc.edu.
REFERENCES
- 1.American Psychiatric Association, American Psychiatric Association. Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Bahgat D, Ray DK, Raslan AM, McCartney S, Burchiel KJ. Trigeminal neuralgia in young adults. J Neurosurg. 2011;114:1306–11. doi: 10.3171/2010.10.JNS10781. [DOI] [PubMed] [Google Scholar]
- 3.Barker FG, 2nd, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD. The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med. 1996;334:1077–83. doi: 10.1056/NEJM199604253341701. [DOI] [PubMed] [Google Scholar]
- 4.Betrus PA, Elmore SK, Hamilton PA. Women and somatization: Unrecognized depression. Health Care Women Int. 1995;16:287–97. doi: 10.1080/07399339509516182. [DOI] [PubMed] [Google Scholar]
- 5.Broggi G, Ferroli P, Franzini A, Servello D, Dones I. Microvascular decompression for trigeminal neuralgia: Comments on a series of 250 cases, including 10 patients with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2000;68:59–64. doi: 10.1136/jnnp.68.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burchiel KJ. A new classification for facial pain. Neurosurgery. 2003;53:1164–6. doi: 10.1227/01.neu.0000088806.11659.d8. [DOI] [PubMed] [Google Scholar]
- 7.Burton AK, Tillotson KM, Main CJ, Hollis S. Psychosocial predictors of outcome in acute and subchronic low back trouble. Spine. 1995;20:722–8. doi: 10.1097/00007632-199503150-00014. [DOI] [PubMed] [Google Scholar]
- 8.Engel GL. Primary atypical facial neuralgia; an hysterical conversion symptom. Psychosom Med. 1951;13:375–96. doi: 10.1097/00006842-195111000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Feinmann C, Harris M, Cawley R. Psychogenic facial pain: Presentation and treatment. Br Med J. 1984;288:436–8. doi: 10.1136/bmj.288.6415.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.First MB. Diagnostic and statistical manual of mental disorders, 5 th edition, and clinical utility. J Nerv Ment Dis. 2013;201:727–9. doi: 10.1097/NMD.0b013e3182a2168a. [DOI] [PubMed] [Google Scholar]
- 11.Gureje O, Simon GE, Von Korff M. A cross-national study of the course of persistent pain in primary care. Pain. 2001;92:195–200. doi: 10.1016/s0304-3959(00)00483-8. [DOI] [PubMed] [Google Scholar]
- 12.Holroyd KA, Stensland M, Lipchik GL, Hill KR, O’Donnell FS, Cordingley G. Psychosocial correlates and impact of chronic tension-type headaches. Headache. 2000;40:3–16. doi: 10.1046/j.1526-4610.2000.00001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Janjigian ER. Report of three cases of trigeminal neuralgia apparently cured by electroshock therapy. Am J Psychiatry. 1949;106:143. doi: 10.1176/ajp.106.2.143. [DOI] [PubMed] [Google Scholar]
- 14.Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R, et al. Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162:304–10. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- 15.Katon W, Ries RK, Kleinman A. A prospective DSM-III study of 100 consecutive somatization patients. Compr Psychiatry. 1984;25:305–14. doi: 10.1016/0010-440x(84)90063-4. [DOI] [PubMed] [Google Scholar]
- 16.Lamb SE, Guralnik JM, Buchner DM, Ferrucci LM, Hochberg MC, Simonsick EM, et al. Factors that modify the association between knee pain and mobility limitation in older women: The Women's Health and Aging Study. Ann Rheum Dis. 2000;59:331–7. doi: 10.1136/ard.59.5.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lascelles RG. Atypical facial pain and depression. Br J Psychiatry. 1966;112:651–9. doi: 10.1192/bjp.112.488.651. [DOI] [PubMed] [Google Scholar]
- 18.Leino P, Magni G. Depressive and distress symptoms as predictors of low back pain, neck-shoulder pain, and other musculoskeletal morbidity: A 10-year follow-up of metal industry employees. Pain. 1993;53:89–94. doi: 10.1016/0304-3959(93)90060-3. [DOI] [PubMed] [Google Scholar]
- 19.Lunsford LD. Treatment of tic douloureux by percutaneous retrogasserian glycerol injection. JAMA. 1982;248:449–53. [PubMed] [Google Scholar]
- 20.Mc ET, Horton BT. Atypical face pain; a statistical consideration of 66 cases. Ann Intern Med. 1947;27:749–68. doi: 10.7326/0003-4819-27-5-749. [DOI] [PubMed] [Google Scholar]
- 21.Mousavi SH, Niranjan A, Huang MJ, Laghari FJ, Shin SS, Mindlin JL, et al. Early radiosurgery provides superior pain relief for trigeminal neuralgia patients. Neurology. 2015;85:2159–65. doi: 10.1212/WNL.0000000000002216. [DOI] [PubMed] [Google Scholar]
- 22.Mullan S, Lichtor T. Percutaneous microcompression of the trigeminal ganglion for trigeminal neuralgia. J Neurosurg. 1983;59:1007–12. doi: 10.3171/jns.1983.59.6.1007. [DOI] [PubMed] [Google Scholar]
- 23.Rainville P, Duncan GH, Price DD, Carrier B, Bushnell MC. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science. 1997;277:968–71. doi: 10.1126/science.277.5328.968. [DOI] [PubMed] [Google Scholar]
- 24.Resnick DK, Levy EI, Jannetta PJ. Microvascular decompression for pediatric onset trigeminal neuralgia. Neurosurgery. 1998;43:804–7. doi: 10.1097/00006123-199810000-00047. [DOI] [PubMed] [Google Scholar]
- 25.Sekula RF, Marchan EM, Fletcher LH, Casey KF, Jannetta PJ. Microvascular decompression for trigeminal neuralgia in elderly patients. J Neurosurg. 2008;108:689–91. doi: 10.3171/JNS/2008/108/4/0689. [DOI] [PubMed] [Google Scholar]
- 26.Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341:1329–35. doi: 10.1056/NEJM199910283411801. [DOI] [PubMed] [Google Scholar]
- 27.Sweet WH. Controlled thermocoagulation of trigeminal ganglion and rootlets for differential destruction of pain fibers: Facial pain other than trigeminal neuralgia. Clin Neurosurg. 1976;23:96–102. doi: 10.1093/neurosurgery/23.cn_suppl_1.96. [DOI] [PubMed] [Google Scholar]
- 28.Taenzer P, Melzack R, Jeans ME. Influence of psychological factors on postoperative pain, mood and analgesic requirements. Pain. 1986;24:331–42. doi: 10.1016/0304-3959(86)90119-3. [DOI] [PubMed] [Google Scholar]
- 29.Terry EL, DelVentura JL, Bartley EJ, Vincent AL, Rhudy JL. Emotional modulation of pain and spinal nociception in persons with major depressive disorder (MDD) Pain. 2013;154:2759–68. doi: 10.1016/j.pain.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Verdejo-Garcia A, Lopez-Torrecillas F, Calandre EP, Delgado-Rodriguez A, Bechara A. Executive function and decision-making in women with fibromyalgia. Arch Clin Neuropsychol. 2009;24:113–22. doi: 10.1093/arclin/acp014. [DOI] [PubMed] [Google Scholar]
- 31.Von Korff M, Le Resche L, Dworkin SF. First onset of common pain symptoms: A prospective study of depression as a risk factor. Pain. 1993;55:251–8. doi: 10.1016/0304-3959(93)90154-H. [DOI] [PubMed] [Google Scholar]
- 32.Wells KB, Golding JM, Burnam MA. Affective, substance use, and anxiety disorders in persons with arthritis, diabetes, heart disease, high blood pressure, or chronic lung conditions. Gen Hosp Psychiatry. 1989;11:320–7. doi: 10.1016/0163-8343(89)90119-9. [DOI] [PubMed] [Google Scholar]
- 33.Wilson DR, Widmer RB, Cadoret RJ, Judiesch K. Somatic symptoms. A major feature of depression in a family practice. J Affect Disord. 1983;5:199–207. doi: 10.1016/0165-0327(83)90042-3. [DOI] [PubMed] [Google Scholar]
- 34.Wu TH, Hu LY, Lu T, Chen PM, Chen HJ, Shen CC, et al. Risk of psychiatric disorders following trigeminal neuralgia: A nationwide population-based retrospective cohort study. J Headache Pain. 2015;16:64. doi: 10.1186/s10194-015-0548-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ. 2015;350:h1238. doi: 10.1136/bmj.h1238. [DOI] [PubMed] [Google Scholar]


