Abstract
Background:
Iatrogenic injury to the vertebral artery is a rare but potential complication of cervical spine surgery. Previous authors have commented on the use of flow-diverting stents for treatment of aneurysms of the V3 segment of the vertebral artery.
Case Description:
Here, we report a case in which injury occurred at the V2 segment of the vertebral artery with the development of a pseudoaneurysm, which was found on angiography. After decompressing the spinal cord from an epidural hematoma, the pseudoaneurysm was treated by deploying two Pipeline flow-diverting stents (Medtronic, Minneapolis, MN). Obliteration of the pseudoaneurysm was noted on follow-up angiography 4 days after the treatment.
Conclusion:
This case highlights a unique treatment at a region which, to our knowledge, has not been mentioned in the literature.
Keywords: Iatrogenic complication, Pipeline embolization device, pseudoaneurysm, V2 segment, vertebral artery
INTRODUCTION
Although rare, iatrogenic injury to the vertebral artery (VA) during cervical spine surgery poses potentially life-threatening risk to patients. Resultant hemorrhage as well as infarction secondary to VA injury constitute potential causes of intraoperative death. Subsequent formation of a VA pseudoaneurysm at the site of injury places the patient at risk for future emergent complications such as aneurysmal rupture.[1,4] Prior to advances in endovascular techniques, treatment of VA injury relied on an open surgical approach – primary microvascular repair and vessel ligation – that was associated with high morbidity and mortality.[1] With the advent of coil embolization, balloon-assisted coil embolization, and flow-diverting stents, treatment of VA pseudoaneurysms has shifted toward these minimally invasive endovascular techniques.[6]
Endovascular flow-diversion technology utilizes a high-density mesh stent at the site of aneurysm, thereby diverting blood flow from the aneurysmal sac and maintaining the patency of the parent vessel. In addition, the mesh provides a scaffold for the subsequent endothelialization of the aneurysm neck, ultimately aiding in the isolation and obliteration of the aneurysm.[3,6] These flow-diverting stents have been investigated in the context of cerebral aneurysms, most commonly those stemming from the internal carotid artery (ICA).[3] Thus far, the use of flow-diverting stents for the treatment of ICA aneurysms has been promising, yielding low complication rates and high rates of complete angiographic occlusion of the aneurysm at 6-month follow-up.[3,6] However, the use of flow-diverting stents for the treatment of pseudoaneurysms arising from the VAs, specifically the V3 segment, have only recently been described.[1,5] Here, we present a case of successful treatment of an iatrogenic pseudoaneurysm within the V2 segment using a flow-diverting stent.
CASE REPORT
The patient (age in the early 60s) underwent treatment of multilevel cervical stenosis with a C3-7 anterior cervical discectomy and fusion (ACDF). During the course of the procedure, the surgeon encountered copious bleeding during end-plate preparation of the C5-6 level. There was concern for VA injury, which was controlled with Surgiflo hemostatic matrix (Ethicon, Somerville, NJ, USA) and Gelfoam (Pfizer, New York City, NY, USA) packing to tamponade the hemorrhage. After hemostasis was obtained, the plate was placed and normal wound closure ensued. The patient was subsequently transferred to the intensive care unit (ICU) for observation after the completion of the procedure.
While in the ICU, the patient developed progressive quadriparesis within 36 hours of the procedure. Work-up, including magnetic resonance imaging of the cervical spine and computed tomographic angiography of the neck, showed ventral cord compression at the C5-6 level as a result of a ventral epidural hematoma [Figure 1]. The patient was immediately taken back to the operating room for decompression of the spinal cord and revision of the ACDF procedure. From the operating room, the patient was taken to the angiography suite. Cerebral angiography was performed, which revealed the presence of a 0.5 mm × 0.85 mm pseudoaneurysm in the V2 segment on the left side [Figure 2]. Subsequently, two Pipeline embolization devices, 4 × 18 mm and 4 × 20 mm in size, were deployed across the pseudoaneurysm, completely covering the lesion. Follow-up angiography 4 days later demonstrated no evidence of residual pseudoaneurysm [Figure 3], and the patient's quadriparesis gradually improved over the next week. Clinical follow-up occurred 9 months later, with the patient demonstrating significant improvement in function and minimal right-upper extremity weakness.
Figure 1.
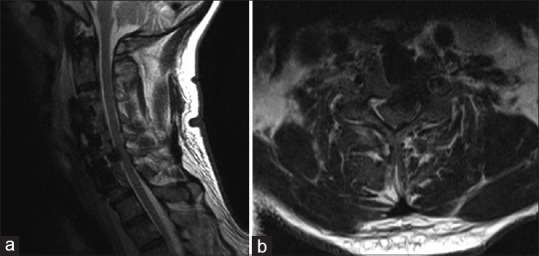
(a) Sagittal T2-weighted magnetic resonance image of the cervical spine demonstrating epidural hematoma and ventral cord compression; (b) axial T2-weighted magnetic resonance image showing ventral hematoma and cord compression
Figure 2.

Left vertebral artery injection, (a) anteroposterior (with inset) and (b) posterior views, demonstrating a very small, posteromedially projecting pseudoaneurysm in the V2 segment (arrows)
Figure 3.
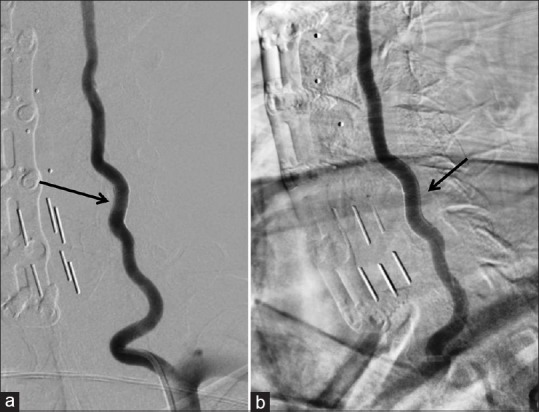
Digital subtraction angiography of the left vertebral artery after the deployment of two Pipeline embolization devices (a, anteroposterior; b, lateral). Previously seen pseudoaneurysm is no longer visible (arrows)
DISCUSSION
In previous descriptions of VA pseudoaneurysms treated with flow-diverting stents, the aneurysms were located at the V3 segment of the VA, an area more anatomically prone to injury than other VA segments due to its tortuosity, its course along the posterior arch of C1, and its location beyond the protection of the transverse cervical foramina of C2-C6.[5] This case demonstrates the efficacy of Pipeline embolization in the V2 segment for a pseudoaneurysm located at the level of C5-C6. Iatrogenic injuries due to anterior cervical spine surgery at the level of V2, as was the case with our patient, are exceptionally rare, occurring in 0.5% of procedures according to a series analysis by Tang and Rao.[8] Despite their rarity, the severity of complications, including the potential for rupture, warrants treatment.
The etiology of pseudoaneurysm formation provides a rationale for flow-diversion stenting as a modality of treatment. In an iatrogenic pseudoaneurysm caused by a direct penetrating injury to the vessel, friable connective tissue beyond the vessel comprises the aneurysmal sac.[1,2] The use of other endovascular techniques, such as coil embolization or stent-coiling, exposes the weak connective tissue of the aneurysmal sac to direct manipulation, potentially increasing the risk for rupture.[1,2,5] Furthermore, for pseudoaneurysms with fusiform morphology (i.e., lacking a true neck), use of a flow-diverting stent across the aneurysmal site avoids the difficulties encountered when attempting to coil embolize a diffusely enlarged vessel. Although the treatment of VA pseudoaneurysms with these stents seems to be a rational approach, the most supported use of flow-diversion stenting is for supra and paraclinoid regions of the ICA.[3] Aneurysm treatment in the VAs has been reported; however, the morbidity, mortality, and long-term efficacy of this technique in the posterior circulation remain unknown. The success of flow-diversion stenting in the supra and paraclinoid regions of the ICA is attributed in part to large artery caliber and lack of perforating vessels. As the flow-diverting stent is partially occlusive, advancing the device across perforators generates risk for ischemic complications.[7] Indeed, flow-diversion stenting in the VAs carries a higher risk of ischemic complication.[3] Although the present case study demonstrates the viability of flow-diversion stent placement in the V2 segment of the VA for pseudoaneurysm treatment, continued investigation is needed to determine its safety for use in the posterior cerebral circulation.
Our experience shows that the use of flow-diverting stents, characterized and indicated for use in the ICA, appear to be a viable option for the treatment of iatrogenic pseudoaneurysms located in the V2 segment of the VA.
Financial support and sponsorship
Nil.
Conflicts of interest
Levy: Shareholder/ownership interests–Intratech Medical Ltd., Blockade Medical LLC, NeXtGen Biologics. Principal investigator: Covidien US SWIFT PRIME Trials. Honoraria–Covidien. Consultant–Pulsar, Blockade Medical. Advisory Board-Stryker, NeXtGen Biologics, MEDX. Other financial support–Abbott for carotid training sessions.
Acknowledgments
The authors thank Paul H. Dressel, BFA for preparation of the illustrations and Carrie Owens MSILS and Debra J. Zimmer for editorial assistance.
Footnotes
Contributor Information
Hakeem J. Shakir, Email: hshakir@ubns.com.
Patrick J. Rooney, Email: prooney@buffalo.edu.
Leonardo Rangel-Castilla, Email: leonardo.rangel-castilla@wayne.edu.
Parham Yashar, Email: Yasharpmd@gmail.com.
Elad I. Levy, Email: elevy@ubns.com.
REFERENCES
- 1.Ambekar S, Sharma M, Smith D, Cuellar H. Successful treatment of iatrogenic vertebral pseudoaneurysm using Pipeline embolization device. Case Rep Vasc Med 2014. 2014:341748. doi: 10.1155/2014/341748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amenta PS, Starke RM, Jabbour PM, Tjoumakaris SI, Gonzalez LF, Rosenwasser RH, et al. Successful treatment of a traumatic carotid pseudoaneurysm with the Pipeline stent: Case report and review of the literature. Surg Neurol Int. 2012;3:160. doi: 10.4103/2152-7806.105099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Briganti F, Leone G, Marseglia M, Mariniello G, Caranci F, Brunetti A, et al. Endovascular treatment of cerebral aneurysms using flow-diverter devices: A systematic review. Neuroradiol J. 2015;28:365–75. doi: 10.1177/1971400915602803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi JW, Lee JK, Moon KS, Kim YS, Kwak HJ, Joo SP, et al. Endovascular embolization of iatrogenic vertebral artery injury during anterior cervical spine surgery: Report of two cases and review of the literature. Spine. 2006;31:E891–4. doi: 10.1097/01.brs.0000244614.84685.c2. [DOI] [PubMed] [Google Scholar]
- 5.Dolati P, Eichberg DG, Thomas A, Ogilvy CS. Application of Pipeline Embolization Device for Iatrogenic Pseudoaneurysms of the Extracranial Vertebral Artery: A Case Report and Systematic Review of the Literature. Cureus. 2015;7:e356. doi: 10.7759/cureus.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krishna C, Sonig A, Natarajan SK, Siddiqui AH. The expanding realm of endovascular neurosurgery: Flow diversion for cerebral aneurysm management. Methodist Debakey Cardiovasc J. 2014;10:214–9. doi: 10.14797/mdcj-10-4-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pierot L. Flow diverter stents in the treatment of intracranial aneurysms: Where are we? J Neuroradiol. 2011;38:40–6. doi: 10.1016/j.neurad.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Tang S, Rao R. Perioperative and approach-related complications associated with anterior cervical surgery. Semin Spine Surg. 2009;21:148–55. [Google Scholar]


