Abstract
Background
The United States is experiencing an opioid overdose epidemic. Treatment use data from diverse racial/ethnic groups with opioid use disorder (OUD) are needed to inform treatment expansion efforts.
Methods
We examined demographic characteristics and behavioral health of persons aged ≥12 years that met criteria for past-year OUD (n=6,125) in the 2005–2013 National Surveys on Drug Use and Health (N=503,101). We determined the prevalence and correlates of past-year use of alcohol/drug use treatment and opioid-specific treatment to inform efforts for improving OUD treatment.
Results
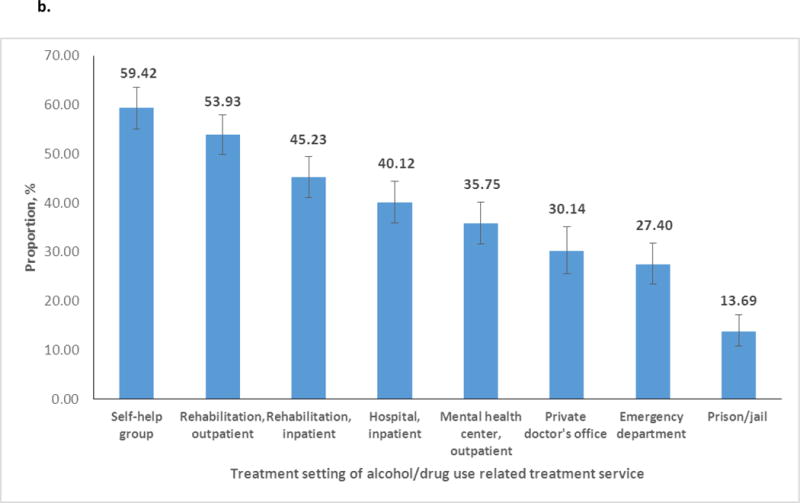
Among persons with OUD, 81.93% had prescription (Rx) OUD only, 9.75% had heroin use disorder (HUD) only, and 8.32% had Rx OUD+HUD. Persons with Rx OUD+HUD tended to be white, adults aged 18–49, males, or uninsured. The majority (80.09%) of persons with OUD had another substance use disorder (SUD), and major depressive episode (MDE) was common (28.74%). Of persons with OUD, 26.19% used any alcohol or drug use treatment, and 19.44% used opioid-specific treatment. Adolescents, the uninsured, blacks, native-Hawaiians/Pacific-Islanders/Asian-Americans, persons with Rx OUD only, and persons without MDE or SUD particularly underutilized opioid-specific treatment. Among alcohol/drug use treatment users, self-help group and outpatient rehabilitation treatment were commonly used services.
Conclusions
Most people with OUD report no use of OUD treatment. Multifaceted interventions, including efforts to access insurance coverage, are required to change attitudes and knowledge towards addiction treatment in order to develop a supportive culture and infrastructure to enable treatment-seeking. Outreach efforts could target adolescents, minority groups, and the uninsured to improve access to treatment.
Keywords: Heroin use disorder, Medication assisted treatment, Opioid use disorder, Prescription opioid misuse, Substance use treatment
1. INTRODUCTION
The opioid (opioid analgesics/heroin) overdose epidemic is among the most pressing public health issues in the United States (Volkow et al, 2014). However, substantial barriers exist for persons seeking medication-assisted treatment (MAT), including a limited number of MAT providers that treat opioid use disorder (OUD; Jones et al., 2015). To combat this opioid epidemic, the U.S. Department of Health and Human Services (USDHHS) has launched an opioid initiative to supporting efforts aimed at improving opioid prescribing practices, expanding use of naloxone to prevent overdoses, and extending use of MAT to treat OUD (Macrae et al., 2015). The USDHHS also released a new rule to allow qualified physicians to increase the number of patients with OUD they can treat with buprenorphine from 100 to 275 (Federal Register, 2016). Timely population-based data about persons with prescription (Rx) OUD or heroin use disorder (HUD) are needed to inform federal initiatives for improving access to MAT for population subgroups, including underserved racial/ethnic groups, to reduce opioid addiction. This paper considers both Rx OUD and HUD and focuses on unique aspects of opioid-specific treatment use among racial/ethnic groups.
In the United States, an estimated 12.5 million people were past-year nonmedical Rx opioid users, and an estimated 0.8 million people were past-year heroin users in 2015 (Center for Behavioral Health Statistics and Quality [CBHSQ], 2016). Past-year Rx OUD is the second most prevalent illicit or nonmedical drug use disorder (DUD), affecting 2.0 million people aged ≥12 years; and 0.6 million persons aged ≥12 years had past-year HUD in 2015 (CBHSQ, 2016). The National Epidemiologic Survey on Alcohol and Related Conditions–III (NESARC-III) indicated that lifetime prevalence of DSM-IV Rx OUD among adults aged ≥18 rose from 1.4% in 2001–2002 to 2.9% in 2012–2013 (Saha et al., 2016). Whites and low-income adults had elevated odds of lifetime Rx OUD (Saha et al., 2016). Approximately 1% of the US adolescents aged 12–17, or 16% of adolescents that used Rx opioids nonmedically in the past year, had Rx OUD (Wu et al., 2008). In both adolescents and adults, having major depression was positively associated with the severity of Rx OUD (Wu et al., 2008, 2011a). Findings from the Treatment Episode Data Set (TEDS) indicated that the treatment admission rate for opioid use other than heroin was 167% higher in 2013 (57/per 100,000 population aged ≥12 years) than the rate in 2003 (21/per 100,000) (SAMHSA, 2015). The treatment admission rate for primary heroin use was 5% higher in 2013 (118/per 100,000 population aged ≥12 years) than the rates in 2003 (112/per 100,000) with a major increase among whites (SAMHSA, 2015). Overall, while prevalence of HUD is lower than Rx OUD nationally (CBHSQ, 2016), heroin use represented the majority (63%) of all opioid treatment admissions in TEDS (SAMHSA, 2014). The data reveal the importance of characterizing Rx OUD and HUD in treatment use research.
Of note, Rx opioid overdose death rates have increased progressively since around 1999 (Paulozzi, 2012). By around 2009, drug-involved overdose death rates (mainly Rx opioids) have passed motor vehicle traffic crash mortality rates (Paulozzi, 2012). Nearly half a million Americans died from drug overdoses during 2000–2014, and opioids/heroin were involved in 61% (28,647 deaths) of all drug overdose deaths in 2014 (Rudd et al., 2016). Between 2013 and 2014, significant increases in drug overdoses were found among both sexes, whites, and blacks. Heroin use also accounted for recent major increases in opioid overdose deaths (Rudd et al., 2016). Specifically, due to pharmacological similarities, availability, or high purity of heroin, Rx opioid overdoses are linked with a surge in heroin overdoses (Compton et al., 2016). Rx opioid misuse/OUD was positively associated with heroin use/HUD (Jones et al., 2015, 2016; Pollini et al., 2011). The odds of problematic heroin use indicators tended to be positively associated with frequent nonmedical opioid use across racial/ethnic groups, suggesting that all racial/ethnic groups should be a focus of intervention efforts to reduce opioid addiction (Martins et al., 2015).
Multiple factors have contributed to this opioid overdose epidemic, including availability of prescription and illicit opioids, unsafe prescribing of opioids, doctor shopping for opioids, and opiate diversion (Lev et al., 2016; Paulozzi, 2012). Opioid addiction is a chronic disease that often requires MAT for an adequate duration to facilitate recovery (Kampman and Jarvis, 2015; Volkow and McLellan, 2016). Expanding access to MAT and addiction services to reduce opioid overdoses and enhance recovery is a key emphasis in the federal initiatives (Macrae et al., 2015). Nonwhite racial/ethnic groups, which generally have lower income than whites and experience greater disparities in healthcare, are the fastest growing population in the United States (Colby and Ortman, 2015). To effectively combat the opioid epidemic, federal initiatives to expand access to OUD treatment should reach racial/ethnic and underserved groups. For example, low-income or lack of insurance was positively associated with having Rx OUD, and Rx OUD prevalence had increased among low-income or uninsured people as well as residents of large metropolitan areas (Jones et al., 2016). Among nonmedical Rx opioid users, the prevalence of heroin use had increased among whites and Hispanics (Martins et al., 2015).
To inform interventions aimed at improving access to Rx OUD and HUD treatment use, we utilize the national sample from the 2005–2013 National Surveys on Drug Use and Health (NSDUH) to examine the prevalence and correlates of treatment use. We include both Rx OUD and HUD to provide fuller information about treatment needs for OUD. This analysis is among the first efforts to leverage national datasets and include both Rx OUD and HUD in an effort to produce newer estimates for opioid-specific treatment use by race/ethnicity. Among persons aged ≥12 years with past-year OUD, we determine their sociodemographic characteristics; calculate prevalence of behavioral health indicators; examine prevalence and correlates of past-year use of treatment for alcohol/drug use, drug use treatment, and opioid-specific treatment, respectively; and explore the location of treatment received among those accessing treatment in the past year. Given that male sex, middle age, white race, low income, non-metropolitan residence, other substance use disorder (SUD), and mental health problems are all positively associate with opioid overdose deaths (Paulozzi, 2012; Rudd et al., 2016); we examine the extent to which demographics, socioeconomic factors, and behavioral health status are associated with receipt of treatment.
2. METHODS
2.1. Data source
The NSDUH provides the primary source of national estimates of past-year OUD among civilian, noninstitutionalized persons aged ≥12 years (SAMHSA, 2006, 2014). Its target population included residents of households and persons in non-institutional group quarters (shelters, boarding houses, college dormitories, migratory workers’ camps, halfway houses) from 50 states and District of Columbia. NSDUH used stratified, multistage area probability sampling methods to select a representative sample of the U.S. population aged ≥12 years.
NSDUH data collection included screening of the eligible households for eligible participants and the conduct of the face-to-face household interview at the participant’s home. Computer-assisted personal interviewing, in which interviewers read less-sensitive questions to respondents and entered the respondents’ answers on the laptop, was employed to collect demographic information. Audio Computer-Assisted Self-Interviewing (ACASI), in which respondents read or listened to the questions on headphones and then entered their answers directly on the NSDUH laptop computer, was employed to provide respondents with a private mode for responding to questions about illicit drug use, mental health, and other sensitive behaviors (Turner et al., 1998).
A total of 503,101 persons aged ≥12 years were included in the public-use datasets from the 2005–2013 NSDUH (n=55,110–58,397/year). These surveys used similar designs to allow analysis of the pooled sample. Weighted response rates of household screening and interviewing for these years were 84–91% and 72–76%, respectively (SAMHSA, 2006, 2014). In the total sample, 0.79% (unweighted n=6,125) met criteria for past-year OUD (range: 0.69–0.89% in 2005–2013) that formed the analysis sample.
2.2. Study variables
We used Andersen’s healthcare utilization model to organize correlates of receipt of treatment (Andersen, 1995), which suggested that receipt of substance use treatment was influenced by persons’ predisposing or demographic (age, sex, race/ethnicity), enabling (e.g., insurance, income, population density of residence), and severity (e.g., comorbid SUD) factors (Rosenblatt et al., 2015; Wu et al., 2003, 2007).
2.2.1 Demographic and enabling variables
Respondents’ self-reported race/ethnicity, age, sex, total family income, population density of residence (large metropolitan, small metropolitan, non-metropolitan areas), and health insurance were included as covariates (Fleury et al., 2014; Wu et al., 2003, 2007). NSDUH defined mutually exclusive racial/ethnic groups based on respondents’ self-reported race and ethnicity: non-Hispanic white, non-Hispanic black, non-Hispanic native-American (American Indian/Alaska-native), non-Hispanic native-Hawaiian/Pacific-Islander, non-Hispanic Asian-American, mixed-race (>1 race), and Hispanic. We distinguished among private, public, and no insurance to understand their magnitude of association with treatment use (Dave and Mukerjee, 2011; Wu et al., 2003). We included a survey year variable to examine yearly variations in treatment use prevalence.
2.2.2 OUD
NSDUH assessments of nonmedical Rx opioid use included a detailed description of the drug class and a list of qualifying drugs. Nonmedical use of opioids was defined as any self-reported use of Rx pain relievers that was not prescribed for the respondent, or that the respondent took only for the experience or feeling they caused. Respondents were read the following statement: “These questions are about nonmedical use. We are not interested in your use of ‘over-the-counter’ pain relievers such as aspirin, Tylenol®, or Advil® that can be bought in drug stores or grocery stores without a doctor’s prescription.” Interviewers also showed a pill card to the respondents and read the following: “Card A shows pictures of some different kinds of prescription pain relievers and lists the names of some others. These pictures show only pills, but we are interested in your use of any form of Rx pain relievers that were not prescribed for you or that you took only for the experience or feeling they caused.” Respondents who used Rx opioids non-medically in the past year were assessed Rx opioid-specific abuse and dependence symptoms in the past year based on DSM-IV criteria (APA, 2000). Respondents who reported heroin use in the past year were assessed HUD. Consistent with DSM-IV definition, Rx opioid abuse included presence of ≥1 abuse symptom and absence of dependence, and Rx opioid dependence included presence of ≥3 dependence symptoms (APA, 2000). This sample logic was applied to define HUD. We combined Rx OUD with HUD into OUD (abuse or dependence).
Other behavioral health (need) variables: Like OUD, respondents who reported alcohol or other drug use in the past year were then assessed by substance-specific questions designed to operationalize DSM-IV criteria for abuse of or dependence on each individual substance class (cannabis, cocaine, hallucinogens, inhalants, stimulants/amphetamines, tranquilizers, or sedatives). Current nicotine dependence was assessed by Nicotine Dependence Syndrome Scale (NDSS) and Fagerström Test of Nicotine Dependence (FTND) (Heatherton et al., 1991; Shiffman et al., 2004). NSDUH categorized respondents as having nicotine dependence in the past month if they met criteria for dependence as specified by either NDSS or FTND. Due to the association between major depression and nonmedical opioid use, we examined past-year major depressive episodes (MDE) as a correlate of treatment use (Wu et al., 2010). Assessments for MDE were based on DSM-IV criteria (Kessler et al., 2004, 2010).
Substance use treatment: Respondents’ treatment use was assessed by separate questions that asked about the receipt of treatment for use of alcohol or drugs and for any drug (e.g., “During the past 12 months, that is since [DATE FILL] have you received treatment or counseling for your use of alcohol or any drug, not counting cigarettes?”). Among respondents who reported the receipt of treatment or counseling for drug use, the survey assessed drug-specific treatment use during their most recent treatment use. Opioid-specific treatment included the receipt of treatment or counseling for the respondent’s use of Rx opioids or heroin. Among respondents who reported the receipt of alcohol/drug treatment in the past year, we examined their treatment locations: hospital (inpatient), alcohol/drug rehabilitation facility (inpatient, outpatient), mental health facility (outpatient), emergency department, private doctor’s office, self-help group (Alcoholics Anonymous, Narcotics Anonymous), and prison/jail.
2.3. Data analysis
We examined racial/ethnic differences in the distributions of demographics, MDE, and SUDs among adults with OUD. To inform patient identification and intervention, we used descriptive and logistic regression analyses to characterize differences between Rx OUD and HUD with respect to respondents’ demographics, MDE, and SUDs. We calculated prevalence of treatment use (alcohol or drug, drug, opioid) and location. We conducted logistic regression to identify factors associated with treatment use. All analyses took into account the NSDUH’s complex designs (weighting, clustering; StataCorp, 2013). All results are weighted estimates except for sample size.
3. RESULTS
3.1. Demographic characteristics of persons with OUD (Table 1)
Table 1.
Characteristics of persons aged ≥12 years with past-year opioid use disorder: 2005–2013 NSDUH
| Race/ethnicity | Total | White | Black | Native-American | Native-Hawaiian/ Pacific-Islander/ Asian-American‡ |
Mixed-Race | Hispanic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Sample size, unweighted | n=6,125 | n=4,361 | n=459 | n=141 | n=99 | n=266 | n=799 | ||||||
|
| |||||||||||||
| Weighted % | % (SE) | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI |
| Age in years | |||||||||||||
| 12–17 | 11.66 (0.47) | 10.66 | 9.73–11.65 | 11.73 | 9.27–14.74 | 12.72 | 7.45–20.88 | 10.29 | 5.09–19.70 | 22.83 | 15.46–32.36 | 15.74 | 12.88–19.10 |
| 18–25 | 31.70 (1.03) | 34.43 | 32.27–36.65 | 20.37 | 14.83–27.31 | 22.14 | 12.90–35.32 | 28.83 | 15.35–47.51 | 37.64 | 27.08–49.54 | 25.62 | 20.71–31.24 |
| 26–34 | 24.25 (1.01) | 26.15 | 23.67–28.78 | 17.10 | 11.33–24.99 | 13.42 | 6.50–25.71 | 9.06 | 3.41–21.93 | 12.67 | 6.56–23.07 | 23.45 | 17.52–30.63 |
| 35–49 | 20.85 (1.13) | 19.52 | 17.26–22.00 | 27.95 | 21.14–35.95 | 20.02 | 9.37–37.74 | 50.21 | 28.54–71.80 | 26.15 | 13.12–45.36 | 18.49 | 13.78–24.34 |
| 50+ | 11.53 (1.38) | 9.25 | 6.68–12.68 | 22.85 | 14.61–33.89 | 31.70 | 15.48–54.05 | 1.61 | 0.21–11.43 | 0.71 | 0.16–3.06 | 16.71 | 10.37–25.79 |
|
| |||||||||||||
| Sex | |||||||||||||
| Male | 57.39 (1.13) | 57.26 | 54.92–59.57 | 53.09 | 43.66–62.30 | 54.53 | 35.03–72.73 | 63.14 | 47.02–76.78 | 40.36 | 28.87–53.02 | 62.22 | 55.14–68.81 |
| Female | 42.61 (1.13) | 42.74 | 40.43–45.08 | 46.91 | 37.70–56.34 | 45.47 | 27.27–64.97 | 36.86 | 23.22–52.98 | 59.64 | 46.98–71.13 | 37.78 | 31.19–44.86 |
|
| |||||||||||||
| Total annual family | |||||||||||||
| <$50,000 | 67.12 (1.16) | 62.98 | 60.36–65.53 | 83.78 | 77.75–88.41 | 88.98 | 81.13–93.82 | 58.89 | 41.38–74.40 | 71.48 | 58.15–81.88 | 76.44 | 70.11–81.77 |
| $50,000–$74,999 | 13.50 (0.71) | 14.94 | 13.25–16.80 | 6.54 | 3.87–10.84 | 6.03 | 2.95–11.94 | 19.43 | 9.87–34.69 | 8.59 | 4.81–14.87 | 11.02 | 7.43–16.04 |
| $75,000+ | 19.37 (0.91) | 22.08 | 20.11–24.19 | 9.69 | 5.64–16.15 | 4.99 | 2.10–11.38 | 21.68 | 7.88–47.24 | 19.93 | 10.48–34.62 | 12.54 | 8.68–17.78 |
|
| |||||||||||||
| Population density | |||||||||||||
| Large metropolitan | 49.99 (1.04) | 45.73 | 43.44–48.03 | 62.38 | 53.96–70.11 | 24.56 | 12.96–41.59 | 75.14 | 61.52–85.10 | 47.85 | 34.52–61.49 | 63.00 | 55.96–69.52 |
| Small metropolitan | 43.97 (1.01) | 47.72 | 45.51–49.93 | 31.21 | 24.35–39.01 | 47.97 | 32.27–64.09 | 24.86 | 14.90–38.48 | 47.89 | 35.02–61.04 | 34.78 | 28.42–41.74 |
| Nonmetropolitan | 6.04 (0.50) | 6.56 | 5.59–7.68 | 6.41 | 2.07–18.12 | 27.46 | 12.00–51.26 | 0 | …… | 4.26 | 1.56–11.14 | 2.22 | 1.09–4.49 |
|
| |||||||||||||
| Health insurance | |||||||||||||
| Private | 40.97 (1.13) | 43.76 | 41.28–46.28 | 27.88 | 20.76–36.33 | 28.94 | 13.64–51.24 | 66.23 | 48.55–80.30 | 38.35 | 27.13–50.98 | 32.93 | 26.54–40.02 |
| Public | 28.98 (1.21) | 25.03 | 22.79–27.42 | 49.40 | 39.81–59.03 | 51.66 | 35.64–67.34 | 21.27 | 8.21–44.94 | 41.69 | 28.23–56.51 | 33.70 | 27.48–40.54 |
| None | 30.05 (1.16) | 31.21 | 28.68–33.85 | 22.72 | 16.61–30.26 | 19.40 | 9.04–36.82 | 12.50 | 5.92–24.49 | 19.96 | 11.97–31.39 | 33.37 | 27.31–40.04 |
|
| |||||||||||||
| Opioid use disorder* | |||||||||||||
| Opioid abuse | 24.73 (1.00) | 20.70 | 18.89–22.64 | 31.10 | 23.82–39.46 | 21.81 | 12.50–35.24 | 46.19 | 27.52–65.99 | 20.52 | 12.73–31.35 | 39.24 | 32.98–45.88 |
| Opioid dependence | 75.27 (1.00) | 79.30 | 77.36–81.11 | 68.90 | 60.54–76.18 | 78.19 | 64.76–87.50 | 53.81 | 34.01–72.48 | 79.48 | 68.65–87.27 | 60.76 | 54.12–67.02 |
|
| |||||||||||||
| Rx opioid use disorder, yes | 90.08 (0.66) | 91.88 | 90.55–93.04 | 82.12 | 75.64–87.16 | 95.36 | 86.76–98.47 | 98.85 | 94.62–99.76 | 85.95 | 65.89–95.09 | 84.74 | 78.26–89.55 |
|
| |||||||||||||
| Heroin use disorder, yes | 18.19 (0.90) | 17.72 | 15.81–19.80 | 23.29 | 17.22–30.70 | 6.34 | 2.54–14.96 | 3.94 | 1.19–12.21 | 21.23 | 10.71–37.72 | 19.97 | 14.93–26.18 |
SE: standard error; CI: confidence interval.
Opioid use disorder included Rx opioid or heroin use disorder in the past year.
Estimates are preliminary due to sample size.
Among persons with past-year OUD (n=6,125), three-fourths met criteria for DSM-IV opioid dependence. More whites (79.30%) than blacks (68.90%), native-Hawaiians/Pacific-Islanders/Asian-Americans (53.81%), and Hispanics (60.76%) had opioid dependence.
A high proportion of persons with OUD were whites (72.29%; blacks 9.23%, Hispanics 13.82%, others 4.66%), adults aged 18–34 (55.95%), males (57.39%), persons with low income (<$50,000; 67.12%), residents of large metropolitan areas (49.99%), or privately insured persons (40.97%). Compared with whites, mixed-race persons and Hispanics included more adolescents, and native-Americans included a higher proportion of older adults aged ≥50. Among mixed-race persons, there was a higher proportion of females than males. The vast majority of blacks (83.78%), native-Americans (88.98%), and Hispanics (76.44%) were in the lowest income group. A high proportion of blacks, native-Hawaiians/Pacific-Islanders/Asian-Americans, and Hispanics resided in large metropolitan areas. A high proportion of native-Americans lived in nonmetropolitan areas. All non-white groups except for native-Hawaiians/Pacific-Islanders/Asian-Americans had higher proportions of public insurance than whites.
3.2. Behavioral health indicators (Table 2)
Table 2.
Prevalence of major depressive episode and substance use disorders among persons aged ≥12 years with past-year opioid use disorder: 2005–2013 NSDUH
| Race/ethnicity | Total | White | Black | Native-American | Native-Hawaiian/ Pacific-Islander/ Asian-American‡ |
Mixed-Race | Hispanic | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size, unweighted | n=6,125 | n=4,361 | n=459 | n=141 | n=99 | n=266 | n=799 | ||||||
|
| |||||||||||||
| Weighted % | % (SE) | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI |
| Major depressive episode†* | |||||||||||||
| Yes | 28.74 (1.08) | 30.34 | 27.89–32.91 | 23.32 | 16.72–31.54 | 23.09 | 13.22–37.17 | 12.98 | 5.89–26.24 | 34.62 | 22.54–49.06 | 25.84 | 20.41–32.13 |
|
| |||||||||||||
| Other substance use disorder (tobacco, alcohol, other drugs) | |||||||||||||
| Yes | 80.09 (0.83) | 83.39 | 81.57–85.07 | 73.68 | 66.99–79.43 | 88.43 | 72.46–95.69 | 37.11 | 20.78–57.04 | 83.31 | 73.27–90.09 | 72.04 | 64.71–78.36 |
|
| |||||||||||||
| Alcohol or other drug use disorder† | |||||||||||||
| Yes | 60.51 (1.01) | 61.45 | 59.13–63.72 | 56.78 | 48.46–64.74 | 74.52 | 58.12–86.04 | 33.10 | 18.39–52.07 | 64.42 | 51.08–75.85 | 60.27 | 52.48–67.57 |
|
| |||||||||||||
| Nicotine dependence‡ | |||||||||||||
| Yes | 53.02 (1.21) | 57.65 | 54.80–60.45 | 49.19 | 40.36–58.06 | 53.64 | 33.97–72.23 | 14.45 | 6.26–29.93 | 50.90 | 38.62–63.07 | 36.89 | 29.69–44.71 |
|
| |||||||||||||
| Alcohol use disorder† | |||||||||||||
| Yes | 40.93 (0.98) | 41.17 | 39.00–43.39 | 35.01 | 28.01–42.73 | 54.89 | 39.05–69.80 | 19.35 | 8.68–37.74 | 43.26 | 32.53–54.65 | 45.11 | 38.14–52.27 |
|
| |||||||||||||
| Other drug use disorder†** | |||||||||||||
| Yes | 43.22 (1.01) | 43.38 | 41.13–45.67 | 43.65 | 35.93–51.70 | 47.50 | 30.70–64.89 | 18.38 | 9.77–31.89 | 53.06 | 39.82–65.88 | 44.09 | 36.58–51.89 |
|
| |||||||||||||
| Cannabis use disorder† | |||||||||||||
| Yes | 22.32 (0.70) | 21.76 | 20.23–23.39 | 17.33 | 12.83–22.99 | 30.82 | 16.39–50.30 | 11.45 | 5.32–22.96 | 27.32 | 19.90–36.26 | 28.76 | 22.81–35.55 |
|
| |||||||||||||
| Tranquilizer use disorder† | |||||||||||||
| Yes | 13.99 (0.70) | 14.54 | 13.10–16.10 | 13.70 | 8.37–21.61 | 15.54 | 7.09–30.72 | 2.91 | 0.95–8.60 | 12.26 | 8.18–17.96 | 12.92 | 8.04–20.11 |
|
| |||||||||||||
| Cocaine use disorder† | |||||||||||||
| Yes | 15.25 (0.94) | 14.49 | 12.76–16.40 | 21.46 | 14.90–29.89 | 10.01 | 4.83–19.60 | 2.21 | 0.69–6.87 | 20.31 | 9.52–38.17 | 16.79 | 11.79–23.35 |
|
| |||||||||||||
| Stimulant use disorder† | |||||||||||||
| Yes | 9.28 (0.80) | 9.79 | 8.24–11.61 | 8.67 | 3.74–18.83 | 6.72 | 2.81–15.20 | 3.44 | 1.24–9.20 | 8.24 | 5.62–11.92 | 8.11 | 4.45–14.34 |
|
| |||||||||||||
| Hallucinogen use disorder† | |||||||||||||
| Yes | 5.25 (0.38) | 4.78 | 4.06–5.60 | 6.26 | 3.88–9.94 | 3.81 | 1.42–9.84 | 0.87 | 0.16–4.45 | 8.52 | 4.85–14.54 | 7.46 | 4.68–11.70 |
|
| |||||||||||||
| Sedative use disorder† | |||||||||||||
| Yes | 3.51 (0.43) | 3.24 | 2.43–4.32 | 4.40 | 2.12–8.91 | 11.33 | 3.88–28.81 | 2.77 | 0.83–8.90 | 3.10 | 1.80–5.29 | 3.77 | 1.56–8.82 |
|
| |||||||||||||
| Inhalant use disorder† | |||||||||||||
| Yes | 2.22 (0.22) | 1.96 | 1.52–2.53 | 2.06 | 1.05–3.99 | 2.83 | 1.11–7.03 | 4.77 | 1.51–14.03 | 3.51 | 1.67–7.21 | 3.14 | 1.93–5.08 |
In the past year.
In the past month.
The sample was 5,977 (148 respondents with missing data on major depressive episode were excluded).
Other drug included cannabis, tranquilizer, cocaine, stimulant, hallucinogen, sedative, or inhalant use disorder. SE: standard error; CI: confidence interval.
Estimates are preliminary due to sample size. Boldfaced: The estimate in that group differed from the estimate among whites (P<0.05).
Among persons with OUD, 28.74% had MDE, 53.02% had nicotine dependence, 40.93% had alcohol use disorder (AUD), and 43.22% had ≥1 other DUD (cannabis 22.32%, tranquilizer 13.99%, cocaine 15.25%, stimulant 9.28%, hallucinogen 5.25%, sedative 3.51%, inhalant 2.22%).
Overall, 80.09% of persons with OUD had another SUD (tobacco, alcohol, drug), which was more prevalent among whites (83.39%) than Hispanics (72.04%). Nicotine dependence was more common among whites (57.65%) than Hispanics (36.89%). Compared with whites, prevalence of MDE and most SUDs was lower among native-Hawaiians/Pacific-Islanders/Asian-Americans.
3.3. Differences between HUD and Rx OUD among persons with OUD (Table 3)
Table 3.
Adjusted odds ratios (AORs) of Rx opioid and heroin use disorders among persons aged ≥12 years with past-year opioid use disorder (n=5,977*)
| Rx opioid use disorder (Rx OUD) and heroin
use disorder (HUD) Weighted % |
Rx OUD only | HUD only | Rx OUD+HUD | Rx OUD + HUD vs. Rx OUD only† | HUD only vs. Rx OUD only† | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Row, % | Row, % | Row, % | AOR | 95% CI | AOR | 95% CI | |
| Total | 81.93 | 9.75 | 8.32 | ||||
|
| |||||||
| Race/ethnicity | |||||||
| White | 82.55 | 7.81 | 9.64 | 1.00 | 1.00 | ||
| Black | 76.49 | 18.20 | 5.32 | 0.63 | 0.26–1.54 | 2.24 | 1.44–3.47 |
| Native-American | 93.69 | 4.75 | 1.57 | 0.15 | 0.03–0.72 | 0.54 | 0.15–2.02 |
| NH/PI/Asian-American | 96.45 | 0.40 | 3.15 | 0.47 | 0.10–2.15 | 0.06 | 0.01–0.26 |
| Mixed-race | 79.05 | 13.51 | 7.44 | 0.94 | 0.38–2.34 | 2.39 | 0.81–7.04 |
| Hispanic | 79.75 | 15.48 | 4.77 | 0.53 | 0.30–0.93 | 2.04 | 1.20–3.44 |
|
| |||||||
| Age in years | |||||||
| 12–17 | 94.00 | 3.14 | 2.85 | 1.00 | 1.00 | ||
| 18–25 | 81.03 | 9.25 | 9.72 | 2.62 | 1.67–4.11 | 2.85 | 1.77–4.60 |
| 26–34 | 79.86 | 11.15 | 8.98 | 2.00 | 1.17–3.44 | 2.73 | 1.52–4.90 |
| 35–49 | 80.26 | 10.30 | 9.44 | 2.97 | 1.67–5.27 | 2.59 | 1.55–4.32 |
| 50+ | 79.81 | 13.69 | 6.49 | 1.85 | 0.77–4.43 | 3.10 | 1.45–6.64 |
|
| |||||||
| Sex | |||||||
| Male | 78.50 | 10.79 | 10.70 | 1.00 | 1.00 | ||
| Female | 86.54 | 8.35 | 5.12 | 0.44 | 0.32–0.60 | 0.75 | 0.55–1.02 |
|
| |||||||
| Total annual family income | |||||||
| <$50,000 | 80.38 | 11.03 | 8.59 | 1.00 | 1.00 | ||
| $50,000–$74,999 | 86.76 | 6.85 | 6.40 | 0.80 | 0.46–1.39 | 0.81 | 0.52–1.25 |
| $75,000+ | 83.87 | 7.37 | 8.76 | 1.05 | 0.73–1.51 | 0.88 | 0.56–1.40 |
|
| |||||||
| Population density | |||||||
| Large metropolitan | 76.14 | 14.18 | 9.68 | 1.00 | 1.00 | ||
| Small metropolitan | 86.97 | 5.67 | 7.36 | 0.57 | 0.37–0.87 | 0.32 | 0.23–0.45 |
| Nonmetropolitan | 93.09 | 2.85 | 4.07 | 0.30 | 0.14–0.67 | 0.13 | 0.06–0.28 |
|
| |||||||
| Health insurance | |||||||
| None | 76.07 | 12.53 | 11.40 | 1.00 | 1.00 | ||
| Private | 86.85 | 6.16 | 6.99 | 0.67 | 0.47–0.95 | 0.57 | 0.40–0.81 |
| Public | 80.97 | 12.02 | 7.01 | 0.71 | 0.42–1.18 | 0.89 | 0.59–1.35 |
|
| |||||||
| Major depressive episode-past year | |||||||
| No | 81.42 | 10.74 | 7.84 | 1.00 | 1.00 | ||
| Yes | 83.17 | 7.31 | 9.53 | 1.04 | 0.69–1.57 | 0.62 | 0.44–0.87 |
|
| |||||||
| Nicotine dependence-current | |||||||
| No | 89.31 | 5.68 | 5.01 | 1.00 | 1.00 | ||
| Yes | 75.34 | 13.38 | 11.27 | 2.15 | 1.48–3.12 | 2.59 | 1.77–3.80 |
|
| |||||||
| Alcohol use disorder-past year | |||||||
| No | 80.86 | 11.13 | 8.01 | 1.00 | 1.00 | ||
| Yes | 83.46 | 7.77 | 8.78 | 0.85 | 0.58–1.26 | 0.57 | 0.41–0.81 |
|
| |||||||
| Other drug use disorder-past year** | |||||||
| No | 86.74 | 8.52 | 4.74 | 1.00 | 1.00 | ||
| Yes | 75.61 | 11.37 | 13.02 | 3.37 | 2.20–5.17 | 1.80 | 1.28–2.53 |
|
| |||||||
| Year | |||||||
| 2005 | 87.24 | 7.81 | 4.95 | 1.00 | 1.00 | ||
| 2006 | 84.00 | 12.02 | 3.99 | 0.87 | 0.32–2.38 | 1.32 | 0.64–2.70 |
| 2007 | 88.49 | 6.08 | 5.44 | 1.01 | 0.36–2.80 | 0.64 | 0.34–1.21 |
| 2008 | 84.50 | 10.21 | 5.29 | 0.98 | 0.39–2.48 | 1.10 | 0.59–2.03 |
| 2009 | 79.99 | 13.20 | 6.81 | 1.44 | 0.71–2.91 | 1.76 | 0.93–3.34 |
| 2010 | 82.23 | 8.46 | 9.31 | 1.88 | 0.92–3.83 | 0.98 | 0.51–1.90 |
| 2011 | 77.71 | 11.74 | 10.55 | 2.26 | 1.06–4.82 | 1.50 | 0.79–2.87 |
| 2012 | 79.20 | 9.36 | 11.44 | 2.38 | 1.19–4.76 | 1.01 | 0.56–1.84 |
| 2013 | 76.50 | 8.55 | 14.95 | 3.13 | 1.60–6.10 | 0.93 | 0.52–1.67 |
The sample was 5,977 (148 respondents with missing data on major depressive episode were excluded).
Other drug included cannabis, tranquilizer, cocaine, stimulant, hallucinogen, sedative, or inhalant use disorder.
Each adjusted logistic regression included all variables listed in the first column. CI: confidence interval. AOR: adjusted odds ratio. Boldfaced: P<0.05.
Among persons with past-year OUD, 81.93% had Rx OUD only, 9.75% had HUD only, and 8.32% had Rx OUD+HUD. Adjusted logistic regression indicated that white race (vs. native-American, Hispanic), ages 18–49 (vs. ages 12–17), male sex (vs. female), large metropolitan areas (vs. small or non-metropolitan), no insurance (vs. private insurance), nicotine dependence, and other DUD were associated with increased odds of having Rx OUD+HUD vs. Rx OUD only. The proportion of persons with Rx OUD+HUD increased in 2011–2013 (vs. 2005). Blacks or Hispanics (vs. whites), adults (vs. adolescents), residents in large metropolitan areas, the uninsured (vs. privately insured), person with nicotine dependence or other DUD, and persons without MDE or AUD had elevated odds of having HUD only vs. Rx OUD only.
3.4. Substance use treatment and settings (Table 4, Fig. 1a–b)
Table 4.
Prevalence of treatment use among persons aged ≥12 years with past-year opioid use disorder: 2005–2013 NSDUH
| Race/ethnicity | Total | White | Black | Native-American | Native-Hawaiian/ Pacific-Islander/ Asian-American‡ |
Mixed-Race | Hispanic | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Past-year treatment service use, weighted % | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI |
| Alcohol/drug use related service use-past year,% | ||||||||||||||
| Persons with opioid abuse (n=1,654) | 12.96 | 10.30–16.17 | 14.61 | 10.97–19.21 | 14.49 | 6.85–28.06 | 22.74 | 8.42–48.51 | 5.39 | 1.44–18.19 | 9.53 | 3.28–24.66 | 8.54 | 4.93–14.40 |
| Persons with opioid dependence (n=4,471) | 30.54 | 27.95–33.26 | 30.21 | 27.59–32.96 | 31.89 | 22.94–42.42 | 29.66 | 15.26–49.67 | 4.50 | 1.41–13.42 | 35.87 | 21.32–53.58 | 34.33 | 25.55–44.35 |
| Persons with opioid abuse/dependence (n=6,125) | 26.19 | 24.00–28.51 | 26.98 | 24.68–29.40 | 26.48 | 19.64–34.67 | 28.15 | 17.15–42.58 | 4.91 | 2.09–11.12 | 30.46 | 18.31–46.13 | 24.21 | 18.63–30.84 |
|
| ||||||||||||||
| Drug use related service use-past year, % | ||||||||||||||
| Persons with opioid abuse (n=1,654) | 10.91 | 8.42–14.01 | 12.86 | 9.41–17.34 | 9.68 | 4.24–20.61 | 20.31 | 7.01–46.29 | 4.59 | 1.04–18.09 | 8.70 | 2.88–23.41 | 6.87 | 3.53–12.95 |
| Persons with opioid dependence (n=4,471) | 27.07 | 24.48–29.82 | 27.36 | 24.72–30.16 | 23.09 | 15.95–32.22 | 26.77 | 13.07–47.05 | 4.50 | 1.41–13.42 | 35.12 | 20.59–53.06 | 29.75 | 21.01–40.28 |
| Persons with opioid abuse/dependence (n=6,125) | 23.07 | 20.90–25.40 | 24.36 | 22.04–26.83 | 18.92 | 13.62–25.68 | 25.36 | 14.79–39.95 | 4.54 | 1.84–10.80 | 29.70 | 17.60–45.53 | 20.77 | 15.16–27.79 |
|
| ||||||||||||||
| Opioid use related service use-past year, % | ||||||||||||||
| Persons with opioid abuse (n=1,654) | 5.07 | 3.68–6.94 | 5.55 | 3.58–8.52 | 7.62 | 2.88–18.70 | 7.74 | 1.92–26.47 | 0 | …… | 3.81 | 1.13–12.11 | 3.18 | 1.42–6.98 |
| Persons with opioid dependence (n=4,471) | 24.16 | 21.89–26.59 | 24.69 | 22.18–27.38 | 19.29 | 13.02–27.61 | 25.88 | 12.37–46.36 | 2.30 | 0.69–7.33 | 27.87 | 13.99–47.85 | 26.23 | 17.85–36.79 |
| Persons with opioid abuse/dependence (n=6,125) | 19.44 | 17.63–21.40 | 20.73 | 18.63–23.00 | 15.66 | 10.89–21.99 | 21.93 | 12.00–36.65 | 1.24 | 0.39–3.87 | 22.94 | 11.56–40.39 | 17.19 | 11.96–24.08 |
|
| ||||||||||||||
| Location of services received among past- year alcohol/drug use treatment users, % (n=1,487) | ||||||||||||||
| Self-help group | 59.42 | 55.10–63.59 | 57.10 | 52.64–61.45 | 70.28 | 57.55–80.50 | 83.78 | 63.01–94.00 | 79.10 | 39.99–95.56 | 73.36 | 49.94–88.37 | 60.00 | 42.80–75.05 |
| Rehabilitation, outpatient | 53.93 | 49.83–57.97 | 52.74 | 48.13–57.32 | 71.26 | 58.13–81.58 | 62.13 | 35.07–83.29 | 46.44 | 14.07–82.11 | 64.11 | 36.78–84.57 | 46.15 | 29.84–63.32 |
| Rehabilitation, inpatient | 45.23 | 41.06–49.47 | 45.73 | 40.74–50.81 | 55.07 | 40.83–68.52 | 52.86 | 26.48–77.73 | 46.47 | 14.20–81.98 | 13.13 | 5.33–28.87 | 38.75 | 25.22–54.26 |
| Hospital, inpatient | 40.12 | 35.94–44.46 | 39.02 | 34.50–43.74 | 46.05 | 31.59–61.20 | 50.78 | 24.49–76.64 | 20.22 | 4.45–57.95 | 55.00 | 27.58–79.68 | 39.65 | 24.95–56.49 |
| Mental health center, outpatient | 35.75 | 31.59–40.14 | 36.50 | 31.93–41.32 | 29.87 | 17.36–46.34 | 60.48 | 34.93–81.36 | 45.32 | 13.44–81.57 | 49.57 | 21.75–77.66 | 30.99 | 19.85–44.89 |
| Private doctor’s office | 30.14 | 25.52–35.19 | 31.21 | 26.43–36.44 | 20.30 | 10.59–35.38 | 16.77 | 4.89–44.10 | 60.49 | 22.47–89.00 | 26.24 | 8.09–58.96 | 32.07 | 18.63–49.34 |
| Emergency department | 27.40 | 23.39–31.81 | 25.76 | 21.48–30.56 | 36.09 | 20.75–54.92 | 31.05 | 8.61–68.29 | 30.58 | 6.22–74.55 | 54.58 | 26.75–79.82 | 26.42 | 13.54–45.16 |
| Prison/jail | 13.69 | 10.84–17.13 | 12.05 | 9.12–15.75 | 15.96 | 7.51–30.78 | 14.60 | 4.65–37.46 | 48.81 | 15.15–83.58 | 8.09 | 2.66–22.07 | 21.27 | 10.69–37.87 |
CI: confidence interval. Opioid use disorder included Rx opioid or heroin use disorder in the past year.
Estimates are preliminary due to sample size.
Boldfaced: The estimate in that group differed from the estimate among whites (P<0.05).
Figure 1.
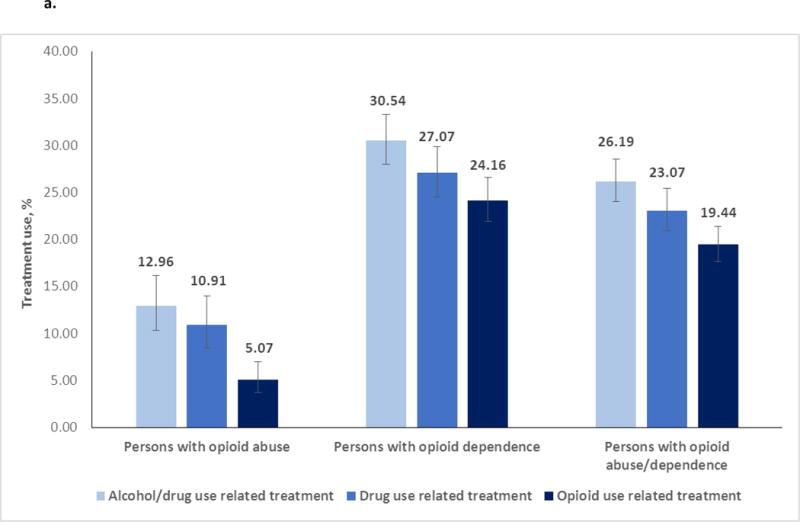
a. Prevalence of alcohol or drug use treatment use among persons aged ≥12 years with past-year opioid use disorder: 2005–2013 NSDUH (n=6,125)
b. Treatment settings among persons aged ≥12 years with past-year opioid use disorder that received alcohol or drug use treatment in the past year: 2005–2013 NSDUH (n=1,487)
Among persons with OUD, 26.19% used alcohol or drug use treatment, 23.07% used any drug use treatment, and 19.44% used opioid-specific treatment. Prevalence of treatment use was higher among persons with opioid dependence (alcohol/drug 30.54%, any drug 27.07%, opioid 24.16%) than persons with opioid abuse (alcohol/drug 12.96%, any drug 10.91%, opioid 5.07%). Naive-Hawaiians/Pacific-Islanders/Asian-Americans with OUD had the lowest prevalence of treatment use (alcohol/drug 4.91%, any drug 4.54%, opioid 1.24%).
Among alcohol/drug use treatment users, common settings were self-help groups (59.42%), outpatient rehabilitation units (53.93%), inpatient rehabilitation units (45.23%), inpatient hospitals (40.12%), and outpatient mental health facilities (35.75%). A higher proportion of Native-Americans (83.78%) than whites (57.10%) used self-help groups. More blacks (71.26%) than whites (52.74%) used outpatient rehabilitation. Fewer mixed-race persons (13.13%) than whites (45.73%) used inpatient rehabilitation programs.
3.5. Adjusted odds ratio of substance use treatment (Table 5)
Table 5.
Adjusted analysis of past-year treatment service use among persons aged ≥12 years with past-year opioid use disorder: 2005–2013 NSDUH (n=5,977*)
| Treatment type | Alcohol/drug use treatment service use† | Drug use treatment service use† | Opioid use treatment service use† | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Adjusted odds ratio, AOR | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI |
| Race/ethnicity (vs. white) | ||||||
| Black | 0.73 | 0.47–1.14 | 0.50 | 0.31–0.80 | 0.47 | 0.29–0.77 |
| Native-American | 1.14 | 0.56–2.32 | 1.16 | 0.55–2.45 | 1.32 | 0.57–3.05 |
| Native-Hawaiian/Pacific-Islander/Asian-American | 0.23 | 0.08–0.64 | 0.22 | 0.08–0.67 | 0.09 | 0.03–0.31 |
| Mixed-race | 0.98 | 0.52–1.85 | 1.09 | 0.56–2.16 | 0.91 | 0.42–1.98 |
| Hispanic | 0.81 | 0.55–1.20 | 0.75 | 0.49–1.14 | 0.79 | 0.48–1.30 |
|
| ||||||
| Age in years (vs. 12–17) | ||||||
| 18–25 | 1.19 | 0.95–1.51 | 1.26 | 1.00–1.60 | 1.80 | 1.45–2.25 |
| 26–34 | 1.19 | 0.86–1.64 | 1.20 | 0.87–1.65 | 1.72 | 1.26–2.36 |
| 35–49 | 1.74 | 1.21–2.50 | 1.96 | 1.34–2.86 | 2.65 | 1.78–3.94 |
| 50+ | 1.33 | 0.70–2.50 | 1.27 | 0.63–2.56 | 2.34 | 1.19–4.60 |
|
| ||||||
| Sex (female vs. male) | 1.03 | 0.81–1.31 | 1.04 | 0.80–1.36 | 1.30 | 0.96–1.76 |
|
| ||||||
| Total annual family income (vs. <$50,000) | ||||||
| $50,000–$74,999 | 0.82 | 0.60–1.14 | 0.83 | 0.59–1.18 | 0.68 | 0.46–1.02 |
| $75,000+ | 1.11 | 0.81–1.53 | 1.16 | 0.85–1.57 | 1.10 | 0.79–1.54 |
|
| ||||||
| Population density (vs. large metropolitan) | ||||||
| Small metropolitan | 0.74 | 0.59–0.94 | 0.79 | 0.62–1.00 | 0.80 | 0.61–1.05 |
| Nonmetropolitan | 1.02 | 0.59–1.78 | 1.16 | 0.66–2.04 | 1.15 | 0.64–2.06 |
|
| ||||||
| Health insurance (vs. none) | ||||||
| Private | 1.31 | 0.97–1.75 | 1.23 | 0.93–1.64 | 1.29 | 0.95–1.76 |
| Public | 1.89 | 1.42–2.52 | 1.86 | 1.41–2.45 | 1.57 | 1.17–2.10 |
|
| ||||||
| Heroin use disorder (yes vs. no) | 5.12 | 4.12–6.37 | 5.20 | 4.10–6.59 | 6.23 | 4.78–8.12 |
|
| ||||||
| Major depressive episode – past year (yes vs. no) | 1.58 | 1.21–2.06 | 1.51 | 1.16–1.98 | 1.40 | 1.04–1.89 |
|
| ||||||
| Nicotine dependence – current (yes vs. no) | 1.96 | 1.54–2.49 | 1.80 | 1.40–2.31 | 1.78 | 1.32–2.39 |
|
| ||||||
| Alcohol use disorder – past year (yes vs. no) | 1.15 | 0.92–1.44 | 0.93 | 0.75–1.16 | 0.78 | 0.63–0.98 |
|
| ||||||
| Other drug use disorder-past year** (yes vs. no) | 2.00 | 1.54–2.61 | 2.17 | 1.70–2.79 | 1.84 | 1.39–2.45 |
|
| ||||||
| Year (vs. 2005) | ||||||
| 2006 | 1.45 | 0.91–2.31 | 1.55 | 0.93–2.56 | 1.25 | 0.74–2.12 |
| 2007 | 1.40 | 0.84–2.33 | 1.00 | 0.60–1.67 | 1.11 | 0.65–1.89 |
| 2008 | 1.03 | 0.66–1.62 | 0.99 | 0.63–1.56 | 1.02 | 0.62–1.69 |
| 2009 | 1.28 | 0.86–1.89 | 1.14 | 0.73–1.79 | 1.25 | 0.79–2.00 |
| 2010 | 1.29 | 0.83–2.00 | 1.04 | 0.66–1.62 | 0.88 | 0.55–1.42 |
| 2011 | 1.63 | 1.07–2.48 | 1.53 | 0.97–2.42 | 1.51 | 0.95–2.39 |
| 2012 | 1.59 | 1.10–2.32 | 1.56 | 1.06–2.30 | 1.67 | 1.11–2.50 |
| 2013 | 1.22 | 0.74–2.00 | 1.13 | 0.66–1.93 | 1.20 | 0.72–2.01 |
The sample was 5,977 (148 respondents with missing data on major depressive episode were excluded).
Other drug included illicit drugs other than opioid and heroin.
Each adjusted logistic regression included all variables listed in the first column. CI: confidence interval. AOR: adjusted odds ratio. Boldfaced: P<0.05.
Among persons with OUD, we conducted adjusted logistic regression to estimate correlates of alcohol/drug use treatment use, drug use treatment, and opioid-specific treatment use, respectively. Compared with whites, blacks had lower odds of using drug use and opioid-specific treatment; native-Hawaiians/Pacific-Islanders/Asian-Americans had lower odds of using treatment for alcohol/drug use and opioid-specific treatment. Other correlates of treatment use were generally similar for alcohol/drug use, any drug use, and opioid-specific treatment. Ages 12–17 (vs. ages 18+) and no insurance (vs. public insurance) were associated with lower odds of using opioid-specific treatment. Having HUD, MDE, nicotine dependence, or other DUD was associated with increased odds of using opioid-specific treatment. Finally, compared with treatment use in 2005, the odds of treatment use for alcohol, drug, or opioid use problems increased in 2012, which was consistent with descriptive results (Table S11).
4. DISCUSSION
In the United States, there has been a continuous 15–year upward trend in opioid overdose deaths (Rudd et al., 2016). Based on drug overdose death data between 1980 and 2011, Darakjy et al. (2014) estimated that drug overdose mortality rates would reach its peak in 2016–2017 and take about 18 years (by 2034) to return to the 1980 baseline level. These estimates demonstrate a need for active efforts to improve access to OUD treatment for all racial/ethnic groups. These findings from a large sample have implications for informing federal initiatives for expanding MAT to reduce opioid addiction. First, opioid overdose mortality data do not directly measure OUD-a common indicator for treatment. This study adds new estimates drawn from a large sample (n=503,101) to understand patterns of Rx OUD and HUD and identify treatment gaps for demographic groups. Additionally, there are mounting concerns about heroin use-related conditions, such as injection drug use and HIV/hepatitis virus infections (Conrad et al., 2015; Zibbell et al., 2015). This analysis adds unique information about the extent and some profiles of Rx OUD+HUD and HUD only. Persons with HUD represented 18% of persons with OUD (10% HUD only, 8% Rx OUD+HUD). Consistent with heroin-involved death data (Compton et al., 2016), we found that proportions of Rx OUD+HUD among persons with OUD tripled between 2005 (4.95%) and 2013 (14.95%). Our data further revealed that persons with Rx OUD+HUD tended to be white, male, aged 18–49, or uninsured, which is useful information for targeting demographic characteristics of opioid users to address overdose prevention. Because people with Rx OUD+HUD are likely to have severe comorbidities (Wu et al., 2011b), results suggest a rising demand for MAT to manage increased numbers of persons with complex Rx OUD+HUD. Given heroin’s elevated purity levels and rising use rates (DEA, 2015), in-depth research that can elucidate contextual and risk factors for initiating heroin use is needed to guide prevention strategies (Pollini et al., 2011). The high rate of injection drug use among heroin users and increased heroin use among whites and the uninsured (Rudd et al., 2016; SAMHSA, 2014) suggest urgency in identifying effective OUD care models to facilitate treatment entry and care coordination.
Another salient finding concerns low treatment use and severe patterns of OUD and comorbidity: 75% of persons with OUD had opioid dependence, 80% had another SUD, and 29% had MDE. On average, more whites than blacks or Hispanics had opioid dependence or another SUD. Whites represented 72% of persons with OUD. The burden of OUD has disproportionally affected whites, especially those with low-income or living in rural areas where MAT resources are especially limited (Hansen et al., 2011; Jones et al., 2015). Despite the high prevalence of comorbid SUD, just 26% of persons with OUD received ‘any’ alcohol/drug use treatment, and 19% used opioid-specific treatment. Thus, even in a subset of persons with ≥1 SUD that made the contact with SUD services, approximately one-fourth of treatment users might have their OUD unaddressed. Given its comorbidity, strategies for enhancing OUD treatment could improve detection of OUD among persons who already are in treatment for SUD or mental health conditions to facilitate treatment engagement. Additionally, as most people with OUD have not accessed OUD care, multifaceted interventions are required to change macro-environmental attitudes and knowledge towards OUD and treatment (e.g., misperceptions, stigma) in order to develop a more supportive culture and infrastructure to enable treatment-seeking for OUD (DeFlavio et al., 2015; Saloner and Karthikeyan, 2015; Volkow and McLellan, 2016).
The low rates of treatment reinforces the urgency of expanding insurance coverage by implementing the Affordable Care Act (ACA) and developing the infrastructure and workforce that can facilitate delivery of preventive and treatment services to address the opioid epidemic (Andrews et al., 2015). Unlike other medical illnesses, public funding provides crucial support for addiction treatment, while uninsurance or under-insurance are significant barriers to SUD care (Ali and Mutter, 2016). Further, treatment for OUD requires coverage for an extended period of treatment to facilitate recovery. We found that public insurance was an enabling correlate of treatment use, while private insurance did not differ from no insurance in predicting treatment use (Wu et al., 2003, 2011c). Unfortunately, most states have failed to use ACA resources adequately to help expand addiction treatment (Andrews et al., 2015). Uninsured adults are disproportionally affected by OUD. ACA has important implications for improving population health.
Adolescents, the uninsured, blacks, and native-Hawaiians/Pacific-Islanders/Asian-Americans particularly underutilized opioid-specific treatment. Data from adolescents with OUD showed a very low rate of treatment use among blacks (<4%), and adolescents with OUD were unlikely to use treatment unless they were involved with the criminal justice system (Wu et al., 2011c). Adolescent-onset OUD suggested a high risk for severe OUD; as a result, comorbidity could have a lasting negative impact (Chambers et al., 2003; Wu et al., 2008, 2010). The low treatment use may be related to inadequate MAT data for adolescents. Clinical trials are needed to inform treatment options for adolescents with OUD (Fishman et al., 2010; Matson et al., 2014). Native-Hawaiians/Pacific-Islanders/Asian-Americans with OUD had the lowest prevalence of using alcohol/drug treatment (4.91%) or opioid-specific treatment (1.24%). Cultural-related stigma toward addiction and a lack of culturally congruent addiction providers are unique barriers to seeking treatment among Native-Hawaiians/Pacific-Islanders/Asian-Americans (Wu and Blazer, 2015). Finally, residents in rural areas have relatively high rates of opioid overdoses, but they face substantial barriers to OUD treatment (e.g., shortage of mental/behavioral health providers; CDC, 2012; Quest et al., 2012). We found that persons who lived in small or non-metropolitan areas were likely to have Rx OUD only, suggesting that expansions of office-based OUD treatment will be critical to improving OUD care (Stein et al., 2012).
This study has limitations. All results were based on self-reports. The cross-sectional data preclude causal interpretation. NSDUH excludes the homeless, military personnel on active duty, and residents of institutional group quarters. The survey does not collect the quality of addiction or opioid-specific care. Because treatment use is defined broadly to include any treatment service, the treatment gap is likely greater than these estimates. The results for native-Hawaiians/Pacific-Islanders/Asian-Americans with OUD are limited by a small sample size and should be considered preliminary. However, Native-Hawaiians/Pacific-Islanders/Asian-Americans are the fastest growing segments of the US population, and their addiction treatment needs are vastly under-recognized (Wu and Blazer, 2015). Their very low prevalence of opioid-specific treatment use (1.2%) merits research to identify effective strategies to combat opioid misuse/addiction. The NSDUH also has strengths. It is the primary source for estimating persons with OUD and treatment use, and it includes a large sample to identify underserved groups. For example, the NESARC–III (n=36,309) included a small number (n=330) of adults with past-year Rx OUD (Saha et al., 2016).
In conclusion, annual economic costs of nonmedical opioid use/Rx OUD were $53.4 billion in 2006 (Hansen et al., 2011); annual cost estimates for heroin use were $21.9 billion in 1996 (Mark et al., 2001). The low rate of OUD treatment use coupled with increases in heroin-involved deaths indicate escalating societal costs that can be intensified by untreated OUD. The huge economic burden of these largely untreated disorders highlights the importance of investment in education, research, prevention, and treatment for OUD. The ACA and federal opioid initiatives provide opportunities to transform the delivery of SUD care and curb the opioid overdose trajectories.
Supplementary Material
Highlights.
Of persons with opioid use disorder (OUD) nationally, 18% had heroin use disorder (HUD).
Persons with Rx OUD+HUD tended to be white, uninsured, or adults aged 18–49 years.
Of persons with OUD, 26% used any alcohol or drug use treatment in the past year.
Of persons with OUD, 19% used opioid-specific treatment.
Adolescents, the uninsured, blacks, those with Rx OUD only, had low odds of treatment use.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: The authors have no conflicts of interest to disclose.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Role of the funding source: This work was made possible by research support from the U.S. National Institutes of Health (R01MD007658, R01DA019623, and UG1DA040317; PI, Li-Tzy Wu). The sponsoring agency had no further role in the study design and analysis, the writing of the report, or the decision to submit the paper for publication. The opinions expressed in this paper are solely those of the authors.
Contributors: LT Wu secured funding, designed research questions and analysis, and wrote the drafts of the paper. H Zhu conducted data analyses under the supervision of LT Wu. All authors contributed to critical revisions and interpretations of the findings to result in the final manuscript.
References
- Ali MM, Mutter R. The CBHSQ Report: Patients Who Are Privately Insured Receive Limited Follow-up Services After Opioid-Related Hospitalizations. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; Rockville, MD: 2016. [PubMed] [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. fourth. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- Andrews C, Abraham A, Grogan CM, Pollack HA, Bersamira C, Humphreys K, Friedmann P. Despite resources from the ACA, most states do little to help addiction treatment programs implement health care reform. Health Aff (Millwood) 2015;34:828–835. doi: 10.1377/hlthaff.2014.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality (CBHSQ) Results from the 2015 National Survey on Drug Use and Health: detailed tables. 2016 http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf.
- Centers for Disease Control and Prevention (CDC) CDC grand rounds: prescription drug overdoses-a US epidemic. MMWR. 2012;61:10–13. [PubMed] [Google Scholar]
- Chambers RA, Taylor JR, Potenza MN. Developmental neurocircuitry of motivation in adolescence: a critical period of addiction vulnerability. Am J Psychiatry. 2003;160:1041–1052. doi: 10.1176/appi.ajp.160.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colby SL, Ortman JM. Projections of the Size and Composition of the US Population: 2014 to 2060. U.S. Census Bureau; Washington, DC: 2015. (Current Population Reports, P25-1143). https://www.census.gov/content/dam/Census/library/publications/2015/demo/p25-1143.pdf (accessed 02.10.2016. [Google Scholar]
- Compton WM, Jones CM, Baldwin GT. Relationship between nonmedical prescription-opioid use and heroin use. N Engl J Med. 2016;374:154–163. doi: 10.1056/NEJMra1508490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conrad C, Bradley HM, Broz D, Buddha S, Chapman EL, Galang RR, Hillman D, Hon J, Hoover KW, Patel MR, Perez A, Peters PJ, Pontones P, Roseberry JC, Sandoval M, Shields J, Walthall J, Waterhouse D, Weidle PJ, Wu H, Duwve JM, Centers for Disease Control and Prevention (CDC) Community outbreak of HIV infection linked to injection drug use of oxymorphone—Indiana, 2015. MMWR. 2015;64:443–444. [PMC free article] [PubMed] [Google Scholar]
- Darakjy S, Brady JE, DiMaggio CJ, Li GH. Applying Farr’s Law to project the drug overdose mortality epidemic in the United States. Inj Epidemiol. 2014;1:31. doi: 10.1186/s40621-014-0031-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dave D, Mukerjee S. Mental health parity legislation, cost-sharing and substance-abuse treatment admissions. Health Econ. 2011;20:161–183. doi: 10.1002/hec.1577. [DOI] [PubMed] [Google Scholar]
- DeFlavio JR, Rolin SA, Nordstrom BR, Kazal LA., Jr Analysis of barriers to adoption of buprenorphine maintenance therapy by family physicians. Rural Remote Health. 2015;15:3019. [PubMed] [Google Scholar]
- Drug Enforcement Administration (DEA) National Heroin Threat Assessment Summary. DEA web site; 2015. (DEA Intelligence Report). http://www.dea.gov/divisions/hq/2015/hq052215_National_Heroin_Threat_Assessment_Summary.pdf (assessed 06.07.16) [Google Scholar]
- Federal Register. Medication Assisted Treatment for Opioid Use Disorders. Federal Register web site; 2016. https://www.federalregister.gov/articles/2016/07/08/2016-16120/medication-assisted-treatment-for-opioid-use-disorders (assessed 06.07.16) [Google Scholar]
- Fleury MJ, Ngui AN, Bamvita JM, Grenier G, Caron J. Predictors of healthcare service utilization for mental health reasons. Int J Environ Res Public Health. 2014;11:10559–10586. doi: 10.3390/ijerph111010559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishman MJ, Winstanley EL, Curran E, Garrett S, Subramaniam G. Treatment of opioid dependence in adolescents and young adults with extended release naltrexone: preliminary case-series and feasibility. Addiction. 2010;105:1669–1676. doi: 10.1111/j.1360-0443.2010.03015.x. [DOI] [PubMed] [Google Scholar]
- Hansen RN, Oster G, Edelsberg J, Woody GE, Sullivan SD. Economic costs of nonmedical use of prescription opioids. Clin J Pain. 2011;27:194–202. doi: 10.1097/AJP.0b013e3181ff04ca. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Jones CM. The paradox of decreasing nonmedical opioid analgesic use and increasing abuse or dependence – an assessment of demographic and substance use trends, United States, 2003–2014. Addict Behav. 2016 doi: 10.1016/j.addbeh.2016.08.027. http://dx.doi.org/10.1016/j.addbeh.2016.08.027. [DOI] [PubMed]
- Jones CM, Logan J, Gladden RM, Bohm MK. Vital signs: demographic and substance use trends among heroin users – United States, 2002–2013. MMWR. 2015;64:719–725. [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Campopiano M, Baldwin G, McCance-Katz E. National and state treatment need and capacity for opioid agonist medication-assisted treatment. Am J Public Health. 2015;105:e55–e63. doi: 10.2105/AJPH.2015.302664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampman K, Jarvis M. American Society of Addiction Medicine (ASAM) National Practice Guideline for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9:358–367. doi: 10.1097/ADM.0000000000000166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13:60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Birnbaum H, Bromet E, Hwang I, Sampson N, Shahly V. Age differences in major depression: results from the National Comorbidity Survey Replication (NCS-R) Psychol Med. 2010;40:225–237. doi: 10.1017/S0033291709990213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lev R, Lee O, Petro S, Lucas J, Castillo EM, Wilke GM, Coyne CJ. Who is prescribing controlled medications to patients who die of prescription drug abuse? Am J Emerg Med. 2016;34:30–35. doi: 10.1016/j.ajem.2015.09.003. [DOI] [PubMed] [Google Scholar]
- Macrae J, Hyde P, Slavitt A. HHS launches multi-pronged effort to combat opioid abuse. U.S. Department of Health Human Services (USDHHS); 2015. web site http://www.hhs.gov/blog/2015/07/27/hhs-launches-multi-pronged-effort-combat-opioid-abuse.html (assessed 04.07.16) [Google Scholar]
- Mark TL, Woody GE, Juday T, Kleber HD. The economic costs of heroin addiction in the United States. Drug Alcohol Depend. 2001;61:195–206. doi: 10.1016/s0376-8716(00)00162-9. [DOI] [PubMed] [Google Scholar]
- Martins SS, Santaella-Tenorio J, Marshall BD, Maldonado A, Cerdá M. Racial/ethnic differences in trends in heroin use and heroin-related risk behaviors among nonmedical prescription opioid users. Drug Alcohol Depend. 2015;151:278–283. doi: 10.1016/j.drugalcdep.2015.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matson SC, Hobson G, Abdel-Rasoul M, Bonny AE. A retrospective study of retention of opioid-dependent adolescents and young adults in an outpatient buprenorphine/naloxone clinic. J Addict Med. 2014;8:176–182. doi: 10.1097/ADM.0000000000000035. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ. Prescription drug overdoses: a review. J Saf Res. 2012;43:283–289. doi: 10.1016/j.jsr.2012.08.009. [DOI] [PubMed] [Google Scholar]
- Pollini RA, Banta-Green CJ, Cuevas-Mota J, Metzner M, Teshale E, Garfein RS. Problematic use of prescription-type opioids prior to heroin use among young heroin injectors. Subst Abuse rehabil. 2011;2:173–180. doi: 10.2147/SAR.S24800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quest TL, Merrill JO, Roll J, Saxon AJ, Rosenblatt RA. Buprenorphine therapy for opioid addiction in rural Washington: the experience of the early adopters. J Opioid Manag. 2012;8:29–38. doi: 10.5055/jom.2012.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt RA, Andrilla CH, Catlin M, Larson EH. Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Ann Fam Med. 2015;13:23–26. doi: 10.1370/afm.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths – United States, 2000–2014. MMWR. 2016;64:1378–1382. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS, Grant BF. Nonmedical prescription opioid use and DSM-5 nonmedical prescription opioid use disorder in the United States. J Clin Psychiatry. 2016;77:772–780. doi: 10.4088/JCP.15m10386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saloner B, Karthikeyan S. Changes in substance abuse treatment use among individuals with opioid use disorders in the United States, 2004–2013. JAMA. 2015;314:1515–1517. doi: 10.1001/jama.2015.10345. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Waters A, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6:327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- Stein BD, Gordon AJ, Sorbero M, Dick AW, Schuster J, Farmer C. The impact of buprenorphine on treatment of opioid dependence in a Medicaid population: recent service utilization trends in the use of buprenorphine and methadone. Drug Alcohol Depend. 2012;123:72–78. doi: 10.1016/j.drugalcdep.2011.10.016. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2005 National Survey on Drug Use and Health: National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2006. (NSDUH Series H-30, DHHS Publication No. SMA 06-4194). [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2014. (NSDUH Series H-48, HHS Publication No. (SMA) 14-4863). [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- U.S. House of Representatives. Summary of the House-Senate Conference Report on S. 524 the Comprehensive Addiction and Recovery Act. U.S. House of Representatives web site; 2016. https://rules.house.gov/sites/republicans.rules.house.gov/files/114/PDF/114-CRS524-SxS.pdf (assessed 06.07.16) [Google Scholar]
- Volkow ND, Frieden TR, Hyde PS, Cha SS. Medication-assisted therapies–tackling the opioid-overdose epidemic. N Engl J Med. 2014;370:2063–2066. doi: 10.1056/NEJMp1402780. [DOI] [PubMed] [Google Scholar]
- Volkow ND, McLellan AT. Opioid abuse in chronic pain—misconceptions and mitigation strategies. N Engl J Med. 2016;374:1253–1263. doi: 10.1056/NEJMra1507771. [DOI] [PubMed] [Google Scholar]
- Wu LT, Ringwalt CL, Williams CE. Use of substance abuse treatment services by persons with mental health and substance use problems. Psychiatr Serv. 2003;54:363–369. doi: 10.1176/appi.ps.54.3.363. [DOI] [PubMed] [Google Scholar]
- Wu LT, Pilowsky DJ, Schlenger WE, Hasin D. Alcohol use disorders and the use of treatment services among college-age young adults. Psychiatr Serv. 2007;58:192–200. doi: 10.1176/appi.ps.58.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Ringwalt CL, Mannelli P, Patkar AA. Prescription pain reliever abuse and dependence among adolescents: a nationally representative study. J Am Acad Child Adolesc Psychiatry. 2008;47:1020–1029. doi: 10.1097/CHI.0b013e31817eed4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Blazer DG. Subtypes of nonmedical opioid users: results from the national epidemiologic survey on alcohol and related conditions. Drug Alcohol Depend. 2010;112:69–80. doi: 10.1016/j.drugalcdep.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Pan JJ, Blazer DG. Abuse and dependence on prescription opioids in adults: a mixture categorical and dimensional approach to diagnostic classification. Psychol Med. 2011a;41:653–664. doi: 10.1017/S0033291710000954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Woody GE, Yang C, Blazer DG. How do prescription opioid users differ from users of heroin or other drugs in psychopathology: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Addict Med. 2011b;5:28–35. doi: 10.1097/ADM.0b013e3181e0364e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG, Li TK, Woody GE. Treatment use and barriers among adolescents with prescription opioid use disorders. Addict Behav. 2011c;36:1233–1239. doi: 10.1016/j.addbeh.2011.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Blazer DG. Substance use disorders and co-morbidities among Asian Americans and Native Hawaiians/Pacific Islanders. Psychol Med. 2015;45:481–494. doi: 10.1017/S0033291714001330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell JE, Iqbal K, Patel RC, Suryaprasad A, Sanders KJ, Moore-Moravian L, Serrecchia J, Blankenship S, Ward JW, Holtzman D, Centers for Disease Control and Prevention (CDC) Increases in hepatitis C virus infection related to injection drug use among persons aged≤ 30 years-Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. MMWR. 2015;64:453–458. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


