Summary
Background
In transitioning from the Millennium Development Goal to the Sustainable Development Goal era, it is imperative to comprehensively assess progress toward reducing maternal mortality to identify areas of success, remaining challenges, and frame policy discussions. We aimed to quantify maternal mortality throughout the world by underlying cause and age from 1990 to 2015.
Methods
We estimated maternal mortality at the global, regional, and national levels from 1990 to 2015 for ages 10–54 years by systematically compiling and processing all available data sources from 186 of 195 countries and territories, 11 of which were analysed at the subnational level. We quantified eight underlying causes of maternal death and four timing categories, improving estimation methods since GBD 2013 for adult all-cause mortality, HIV-related maternal mortality, and late maternal death. Secondary analyses then allowed systematic examination of drivers of trends, including the relation between maternal mortality and coverage of specific reproductive health-care services as well as assessment of observed versus expected maternal mortality as a function of Socio-demographic Index (SDI), a summary indicator derived from measures of income per capita, educational attainment, and fertility.
Findings
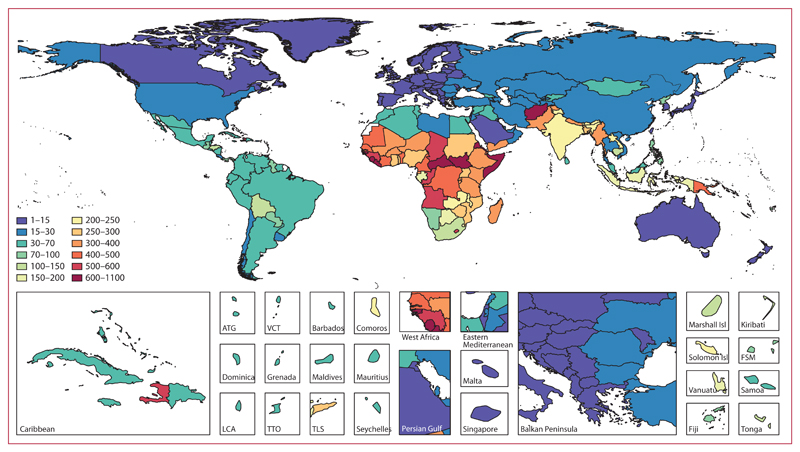
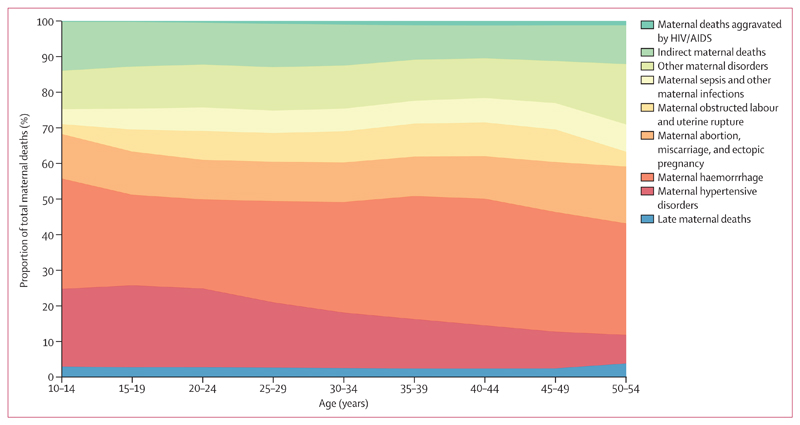
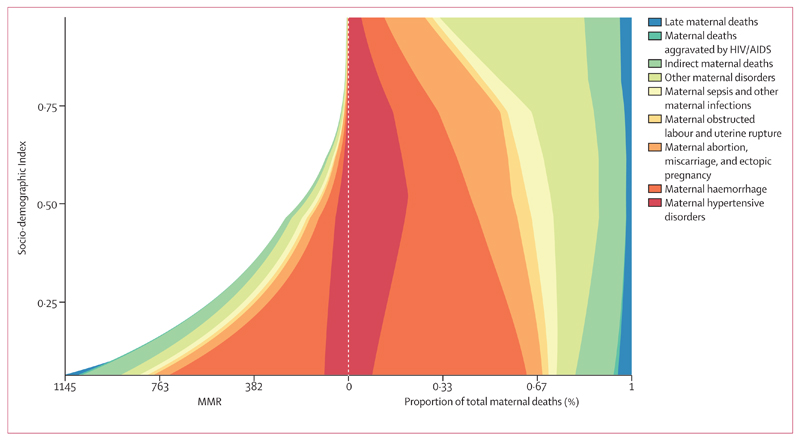
Only ten countries achieved MDG 5, but 122 of 195 countries have already met SDG 3.1. Geographical disparities widened between 1990 and 2015 and, in 2015, 24 countries still had a maternal mortality ratio greater than 400. The proportion of all maternal deaths occurring in the bottom two SDI quintiles, where haemorrhage is the dominant cause of maternal death, increased from roughly 68% in 1990 to more than 80% in 2015. The middle SDI quintile improved the most from 1990 to 2015, but also has the most complicated causal profile. Maternal mortality in the highest SDI quintile is mostly due to other direct maternal disorders, indirect maternal disorders, and abortion, ectopic pregnancy, and/or miscarriage. Historical patterns suggest achievement of SDG 3.1 will require 91% coverage of one antenatal care visit, 78% of four antenatal care visits, 81% of in-facility delivery, and 87% of skilled birth attendance.
Interpretation
Several challenges to improving reproductive health lie ahead in the SDG era. Countries should establish or renew systems for collection and timely dissemination of health data; expand coverage and improve quality of family planning services, including access to contraception and safe abortion to address high adolescent fertility; invest in improving health system capacity, including coverage of routine reproductive health care and of more advanced obstetric care—including EmOC; adapt health systems and data collection systems to monitor and reverse the increase in indirect, other direct, and late maternal deaths, especially in high SDI locations; and examine their own performance with respect to their SDI level, using that information to formulate strategies to improve performance and ensure optimum reproductive health of their population.
Funding
Bill & Melinda Gates Foundation.
Introduction
The global community adopted a set of 17 Sustainable Development Goals (SDGs) on Sept 25, 2015, to provide benchmark targets for global development between 2015 and 2030.1 These goals are intended to build on the momentum and enthusiasm generated by the Millennium Development Goals (MDGs),2 but also to reframe them within the context of a myriad of environmental and societal challenges inherent in achieving sustainable global development,3,4 The Global Strategy for Women’s, Children’s, and Adolescents’ Health 2016–2030 further aims to position the global discussion of maternal mortality within a continuum of programmes aimed at improving the health of women and children globally.5
As the MDG era has now come to a close and the SDG era is beginning, it is imperative to provide a comprehensive account of global, regional, and national progress toward MDG 5. Such information is of crucial importance to identify areas of success and remaining challenges, and to help to frame policy discussions as we continue to prioritise maternal and reproductive health for women in the SDG era.6 Whereas MDG 5 set a target reduction of 75% in the maternal mortality ratio (MMR; number of maternal deaths per 100 000 livebirths) between 1990 and 2015, SDG 3.1 sets a specific target for all countries to lower MMR to less than 70 by 2030. A secondary target of MDG 5, adopted in 2005, called for universal access to reproductive health care with named subtargets for contraceptive prevalence, adolescent pregnancy, antenatal care coverage, and family planning services,7 but notably not for other reproductive health services such as skilled birth attendance, in-facility delivery, or EmOC services. Because of the late addition of reproductive health access to the MDG agenda, related data collection systems have taken time to mature and this issue has not been tracked as closely as maternal mortality. SDG 3.7 has continued the calls for universal access to sexual and reproductive health services by 2030.
We have completed this study as part of the Global Burden of Disease (GBD) 2015, with the specific objective of ascertaining levels and trends in maternal mortality over the entire MDG period at the national, regional, and global levels. Relatedly, by also examining maternal mortality trends by age, cause, geography, and timing of death, we seek to better understand trends in maternal mortality epidemiology and thus generate insight into drivers of progress—or lack thereof—toward achievement of MDG 5 and help to frame discussions for monitoring of SDG 3.1 and 3.7. Multiple previous analyses, including several completed as part of the GBD collaboration have sought to provide the best possible information about levels and trends in maternal mortality.8–14 In dual recognition of both the importance and difficulty of accurately reporting on maternal mortality in many settings,15,16 each has incorporated increasingly large and geographically precise datasets and used more advanced statistical models. In their latest iteration,12 the WHO methods have also now adopted a single model for all countries and computed statistical uncertainty intervals. Important differences remain, however, between WHO and GBD maternal mortality estimates that at times paint divergent pictures of levels and trends in maternal mortality globally and in many countries. The main differences now stem from data selection, quality appraisal, data processing, and adult mortality estimation rather than the statistical maternal mortality models themselves.
In this GBD 2015 report, we present the underlying data for 519 distinct geographical units in 195 countries and territories, our methods for processing those data, the subsequent analytical approach, and findings on maternal mortality from 1990 to 2015. GBD 2010, published in 2012, presented results for 187 countries with a population greater than 50 000 in the year 2000.17 Collaborative teams completed subnational assessments for the UK, Mexico, and China for GBD 2013, expanding the number of geographies in the GBD analysis to 296.18–21 The value of subnational assessments to local decision makers22 has led to expansion of subnational analyses in GBD 2015 to also include Brazil, India, Japan, Kenya, Saudi Arabia, South Africa, Sweden, and the USA. We expect subnational analyses for other countries will be added in future GBD iterations. The expansion of the geographical units in the GBD will continue in a way that will sustain comparability over time for the period 1990 to present and across all geographical entities. We have not included constant rate-of-change forecasts in this Article because, as part of the broader effort to quantify the population disease burden, we are developing a set of rigorous statistical models to forecast each component of the GBD—including maternal mortality—and we expect to be able to explore much more robust forecasts in the near future.
As with all GBD revisions, the GBD 2015 study describes updated maternal mortality estimates for the entire time series from 1990 to 2015 based on newly identified data sources released or collected since GBD 2013. In response to published commentaries and unpublished seminars and communications on GBD methods, various methodological refinements have been implemented.23,24 In addition, a major effort toward data and code transparency has been part of the GBD 2015 cycle. And as with each GBD cycle, the full time series published here supersedes previous GBD studies. This analysis explores global, regional, national, and subnational progress and seeks to identify correlates that help to explain why some nations have seen great improvements in maternal health, while others have stagnated and others still have worsened. These include examination of associations in national maternal mortality levels and trends with coverage of reproductive health interventions and Socio-demographic Index (SDI).
Methods
Overview
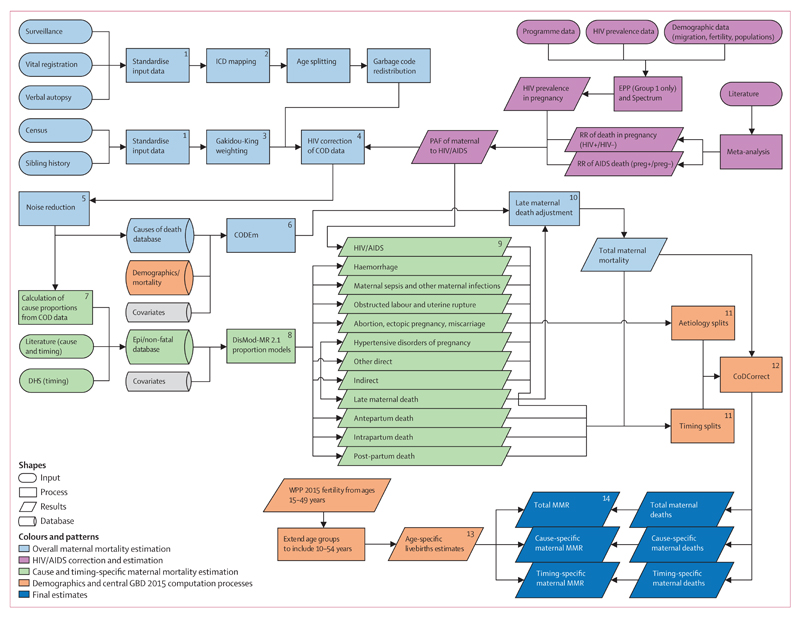
Maternal mortality is defined as a death that occurs to a woman as a direct result of obstetric complications or indirectly as a result of pregnancy-induced exacerbation of pre-existing medical conditions, but not as a result of incidental or accidental causes. To ensure internal consistency with all other causes of death, maternal mortality was also again analysed as a component of the overall GBD study. Many of the analytical components are therefore shared with other causes, including methods of data source identification and cataloguing, data preparation, modelling platforms, and processing of results. Here, we will focus on parts of the process that are unique, have been updated since GBD 2013, or are especially relevant to our analysis of maternal mortality. Figure 1 illustrates details of the analysis. General components are described in the appendix (pp 2–54), in other GBD 2015 Articles in The Lancet, and have also been published previously.10,20,25 This report follows the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) guidelines, which recommends documentation of data sources, methods, and analysis.26
Figure 1. Analytical flow chart for the estimation of maternal mortality for GBD 2015.
Ovals represent data inputs, square boxes represent analytical steps, cylinders represent databases, and parallelograms represent intermediate and final results. Numbers are steps of the prcoess. The flowchart is colour-coded by major estimation component: data preparation and overall maternal mortality in blue; cause-specific and timing-specific estimation in green; analysis and data specific to the role of HIV/AIDS in maternal mortality in pink; steps related to demographic and computational processes that ensure internal consistency in orange, and final estimates in dark blue. GBD=Global Burden of Disease. ICD=Internatinal Classification of Diseases. COD=causes of death. Epi=epidemiology. DHS=Demographic and Health Survey. CODEm=causes-of-death ensemble modelling. RR=relative risk. MMR=maternal mortality ratio. WPP=World Population Prospects. EPP=Estimation and Projection Package. RR=relative risk. Preg+=pregnant. Preg–=non-pregnant.
Maternal mortality estimation
Geographical units of analysis
Our analysis was completed separately for 519 unique locations in 195 countries and territories, including all 188 countries analysed in GBD 2013 as well as seven additional countries or territories—namely, American Samoa, Bermuda, Greenland, Guam, Northern Mariana Islands, Puerto Rico, and the Virgin Islands, where high-quality vital registration data were available. Of note, these territories were not included in the national totals for Denmark, the UK, or the USA, but were instead included in GBD 2013 regional totals. All 195 countries are hierarchically organised into 21 regions, each of which is nested in one of seven super regions. Based on a combination of data availability and collaborator interest, we disaggregated GBD 2015 analyses into subnational units for several countries, including 26 states and one district for Brazil, 34 provinces and municipalities for China, 31 states and union territory groupings for India that include 62 rural and urban units, 47 prefectures for Japan, 47 counties for Kenya, 32 states and districts for Mexico, 13 provinces for Saudi Arabia, nine provinces for South Africa, two regions for Sweden, 13 regions for the UK (Northern Ireland, Scotland, Wales, England, and nine subregions of England), and 51 states and districts for the USA. At the first subnational unit level, we have a total of 256 geographical units. In this Article, we present results for countries and territories, regions, super regions, SDI quintiles, and at the global level.
Data input and processing
The contents of the dataset used in our final model are shown in the appendix (p 667) and are compared with those used by the recent WHO analysis.12 A map showing the data coverage by location for all source types combined is shown in the appendix (p 57). We had 599 unique sources from data from 186 of 195 countries (95%), covering 12 052 site years, an increase of 71% from GBD 2013 when we had 7056 total site years of maternal mortality data. This compares to only 203 sources covering 2636 total site years in the WHO analysis. The nine countries without maternal mortality data included Andorra, Angola, Equatorial Guinea, the Federated States of Micronesia, Marshall Islands, Samoa, Solomon Islands, Somalia, and Vanuatu. Maternal mortality data were also available for additional subnational locations in Mexico, China, the UK, Japan, the USA, Kenya, South Africa, India, Sweden, and Brazil. All data were stored in a centralised structured query language causes-of-death database in three formats: number of deaths, cause-specific mortality rate per capita, and cause fraction (proportion of all deaths due to maternal causes).
Vital registration systems have been shown to underestimate maternal mortality, but the amount of underestimation varies by setting and can change over time.22–24 We therefore used a method that maximises the data-driven nature—and specificity—of our adjustments by systematically evaluating each underlying data source. We included all sources with population-level data for maternal mortality from each geography. We used a standardised process to identify, extract, and process all relevant data sources, including those from vital registration systems, verbal autopsy studies, maternal surveillance systems, national confidential enquiry reports, and sibling survival histories from health surveys and censuses (figure 1, step 1).
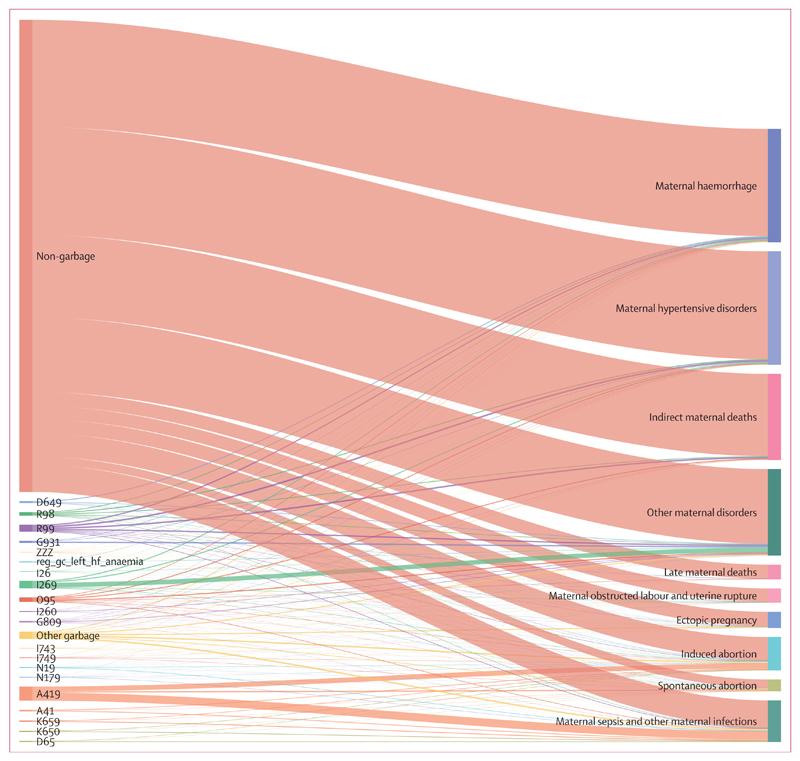
Standardised algorithms were implemented to adjust for age-specific, year-specific, and geography-specific patterns of incompleteness and underreporting for vital registration, as well as patterns of misclassification of deaths in vital registration and verbal autopsy sources (figure 1, step 2). These generalised algorithms were used across all GBD causes and thus were able to capture trends in quality changes in vital registration with respect to maternal mortality, even in locations where surveillance studies have not been completed.20 Each code in International Classification of Diseases (ICD)-coded vital registration datasets was uniquely assigned to a corresponding cause in the hierarchical GBD cause list. Codes used in tabular classification systems (eg, ICD-9 basic tabular list, verbal autopsy, maternal surveillance systems) were likewise uniquely matched with a GBD cause. A proportion of deaths assigned to causes that cannot be underlying causes of death (garbage coded) were reassigned to maternal causes based on statistical redistribution packages, as described in the appendix (pp 2–18). The net effect of data processing steps on vital registration across all locations and years combined was to increase maternal deaths by 168%. The net effect varied by geography and year even among those countries and territories with at least 10 years of data, ranging from less than 1% increase in Mongolia to a nine-fold increase in China. Final and raw vital registration data for each country and year are shown in the appendix (pp 519–652), including proportion of all deaths assigned to garbage codes, and comparisons with WHO vital registration adjustments.12 Figure 2 shows the results of garbage code redistribution for maternal mortality at the global level. Distinct cause groupings, many of which are garbage codes, are shown on the left and the relative thickness of lines shows the proportion of all deaths from those codes that were subsequently mapped to corresponding maternal causes on the right. Note that by definition the so-called non-garbage codes on the left map directly to maternal causes.
Figure 2. ICD-10 vital registration redistribution pattern from cause-specific and garbage codes to maternal-mortality specific GBD causes, global, all years combined.
The list of causes on the left are raw ICD-10 cause codes according to death certification data sources and those on the right are the final target aetiologies for maternal mortality. The height of each bar is proportional to the number of deaths in each category. The colours are for ease of visualisation. Redistribution categories: A41=other sepsis; A419=sepsis, unspecified organism; D649=anaemia, unspecified; D65=disseminated intravascular coagulation; G809=cerebral palsy, unspecified; G931=anoxic brain damage, not elsewhere classified; I26=pulmonary embolism; I269=pulmonary embolism without acute cor pulmonale; I743=embolism and thrombosis of arteries of the lower extremities; I749=embolism and thrombosis of unspecified artery; K650=generalised (acute) peritonitis; K659=peritonitis, unspecified; N179=acute kidney failure, unspecified; N19=unspecified kidney failure; O95=obstetric death of unspecified cause; R98=unattended death; R99=ill-defined and unknown cause of mortality; ZZZ=causes violating age/sex limitations); reg_gc_left_hf_anaemia=anaemia due to left heart failure; other garbage=all other garbage codes. ICD-10=International Classification of Diseases 10. GBD=Global Burden of Disease.
In view of their inconsistent use by vital registration systems, codes pertaining to HIV-related indirect maternal deaths were excluded at this stage in favour of a more comprehensive approach to estimate the effect of HIV on maternal death (see below for more details of HIV-related maternal mortality analysis). In addition to vital registration, we identified maternal mortality surveillance systems and published confidential enquiry studies identified via targeted web search and systematic review of national ministry of health websites. Confidential enquiries are specialised studies designed to investigate the number and circumstances of maternal deaths. Inclusion required a clear distinction identified between maternal and incidental deaths during pregnancy. As with vital registration systems, HIV-related indirect maternal deaths were excluded from surveillance datasets at this stage (see below for more details) but otherwise were unadjusted. Single-year sibling history and survey data derived from health surveys and censuses was processed as in GBD 2013, using Gakidou-King weights to adjust for survivor bias and only retaining data from older surveys when years of death overlapped (figure 1, step 3).27
Our general approach to quantify the role of HIV in maternal mortality is unchanged from GBD 2013 and again involved comprehensive estimation of the population attributable fraction of maternal mortality to HIV10 (figure 1, step 4). In view of the increased baseline mortality of those with advanced HIV, this approach has helped to distinguish between deaths in HIV-positive women that were caused by pregnancy and those for which the pregnancy was incidental to their death. A detailed description of the GBD 2013 approach and updates is in the appendix (pp 21–24). An updated systematic literature search completed on July 20, 2015, did not identify any new sources to inform either our meta-analysis of relative risk of pregnancy-related death for HIV-positive versus HIV-negative women or our analysis on the proportion of pregnancy-related deaths in HIV-positive women that are maternal (versus incidental). HIV prevalence in pregnancy, approximated as the ratio of livebirths in HIV-positive to HIV-negative women, was updated using our modified EPP-Spectrum model. We also made two important improvements to overall HIV mortality estimation, both of which affected our HIV-related maternal mortality estimates. First, to improve the internal consistency of estimates developed for countries with generalised HIV epidemics, we modified EPP-Spectrum to improve how it integrates ART-dependent HIV progression and mortality data from published cohort studies and combined these findings with results derived from statistical examination of how all-cause mortality relates to crude HIV death rate. Second, in recognition of the fact that HIV mortality rivals or exceeds that of high mortality events (referred to as so-called fatal discontinuities in GBD 2015) such as war and natural disaster in many locations—and that such discontinuities have major detrimental effects on statistical mortality models—all of our maternal mortality data were processed to ensure incidental HIV deaths were excluded before modelling. We processed sibling history and census data to exclude incidental HIV deaths using population attributable fractions calculated above for each geography, age group, and year. This method is analogous to the HIV-correction process used in GBD 2013 except that the correction was done on the data itself rather than the preliminary model results. To ensure consistency between all data sources, we also applied population attributable fractions to all vital registration, verbal autopsy, and surveillance data to add back the corresponding number of HIV-related indirect maternal deaths in each of those sources. Finally, to reduce error introduced by large stochastic fluctuations and upward bias introduced by data that have a value of zero, we processed all data of all specifications using Bayesian noise-reduction algorithms (see appendix [pp 2–18] for more details; figure 1, step 5). Zeros are problematic because the log of zero is undefined, so all zeroes would otherwise be ignored by log-based statistical mortality models.
Modelling overall maternal mortality
We again modelled overall maternal mortality using cause-of-death ensemble modelling (CODEm), which was developed for GBD 201028 and is described in detail in the appendix (figure 1, step 6). CODEm runs four separate models, including natural log of age-specific death rates and logit-transformed cause-fractions in each of linear and spatiotemporal Gaussian process regression formats. Using multiple holdout patterns and cross-validation testing, every combination of covariates was tested. Models where regression coefficients met requirements for direction and significance were then ranked on the basis of out-of-sample predictive validity performance through multiple iterations of cross-validation testing. We then generated a series of ensemble models with a range of weightings such that top-performing component models contributed the most to the final prediction. We ran two separate CODEm models, one for countries with extensive complete vital registration representation and another for all countries combined (see appendix pp 655–59 for a list of countries and territories with extensive complete vital registration included in separate CODEm model). The purpose was so that heterogeneous data from countries without extensive complete vital registration representation would not inflate the uncertainty interval (UI) for countries with extensive and complete cause-specific death data. Results from the former model were used for all geographies with extensive complete vital registration representation; results for all other geographies were from the latter model.
Predictive covariates were specified with respect to required directionality and significance level of regression coefficients (see appendix [p 661] for full details). Three hierarchical covariate levels reduce the combinatorial burden on CODEm. Covariates with strong or causal association were assigned to level 1; those that are ecologically related were assigned to level 2; and those where association is suspected but not proven at the population level were assigned to level 3. We largely used the same covariates as in GBD 2013, including age-standardised fertility rate, total fertility rate, years of education per capita, lag-distributed income (international $ per capita), neonatal mortality rate (per 1000 livebirths), HIV mortality in females of reproductive age, and the coverage proportion of one visit of antenatal care, four visits of antenatal care, skilled birth attendance, and in-facility delivery. Several new covariates were introduced in this analysis in recognition of their potential relation to maternal mortality, all of which were specified as level 3. Obesity prevalence was added to help to reflect the added complexity of care and heightened risk of maternal complications in those who are obese.29,30 Mortality death rate from fatal discontinuities, a covariate that aggregates the effects of war, famine, and natural disaster, was introduced to help to inform maternal mortality estimates in geographies where demographic shocks have led to interruption of vital statistics and where health systems are also hypothesised to have deteriorated.31,32 Hospital beds per 1000 population was added based on the hypothesis that it might be a proxy for the availability of basic EmOC.33 SDI, based on principal component analysis of fertility, maternal education (years per capita), and lag-distributed income (international $ per capita), was added as a covariate to all CODEm models in GBD 2015. The root-mean SE of the top-performing ensemble model was 0·318 for the CODEm model of countries with extensive complete vital registration model and 0·553 for the global model. In-sample and out-of-sample data coverage was 99·6% and 99·3%, respectively, for the CODEm model of countries with extensive complete vital registration, and 98·3% and 97·7%, respectively, for the global model. The relative contributions of each of the covariates and submodel performance for all component models in the top-performing CODEm ensemble are shown in the appendix (pp 662–75).
Modelling underlying cause and timing of maternal mortality
Our approach to quantify underlying cause and timing of maternal deaths was largely unchanged from GBD 2013, although in some cases we changed cause names to better reflect the ICD-9 and ICD-10 codes contained therein. ICD-9 and ICD-10 codes corresponding to each category are in the appendix (p 653). We examined six groups of direct obstetric causes, including maternal hypertensive disorders; maternal haemorrhage; maternal abortion, miscarriage, and ectopic pregnancy; maternal obstructed labour and uterine rupture; maternal sepsis and other maternal infections; and other maternal disorders. Two categories of indirect obstetric causes included maternal deaths aggravated by HIV/AIDS and indirect maternal disorders. Late maternal deaths occurring between 42 days and 1 year after the end of pregnancy were estimated as a separate cause (ICD-10 code, O96). Two differences can be noted between the GBD and ICD-maternal mortality modification classification systems, neither of which are new in this study, but nonetheless warrant mention in that they each reflect important clinical aspects of pregnancy complications. First, the GBD has grouped uterine rupture with obstructed labour rather than maternal haemorrhage, in recognition that most uterine rupture cases are secondary to inadequately addressed or prolonged obstruction of labour. Second is the combining of abortion, ectopic pregnancy, and miscarriage into one cause. Although there are important differences between them, we treated them similarly with the rationale that safe interventions can be similar during early pregnancy (eg, medication, potentially dilation, and evacuation), as can management of life-threating complications such as infection and bleeding, which require prompt evaluation, diagnosis, and often emergency surgical intervention. We also examined four distinct time windows of maternal death. In addition to late maternal deaths, we estimated deaths occurring during the antepartum period (before onset of labour), intrapartum and immediate post partum (onset of labour up to <24 h after delivery), and early and delayed post partum (24 h to 42 days after delivery). We analysed late maternal death as both a timing category and as a distinct cause because the underlying causes of late maternal deaths are not specified in most data sources.
Systematic literature reviews identified studies that examined underlying causes and timing of maternal deaths (figure 1, step 7). We extracted additional information from specialised studies such as confidential enquiries and maternal mortality review boards that were obtained from targeted web searches or from correspondence with GBD collaborators. We supplemented aetiology models with cause-specific data from the causes-of-death database. Of note, our criteria for including data from the causes-of-death database was modified from GBD 2013 to include all data from any source where specific subcauses were coded rather than limiting to only those sources where the complete complement of subcauses were included. This change had the effect of substantially increasing the size of our analytical dataset with respect to time and geography. Late maternal death data from the causes-of-death database were limited to those location years where at least 0·5% of all maternal deaths in raw vital registration data files were coded to late maternal deaths as this was the lowest proportion reported in any surveillance studies.34 Only 39 countries met these criteria with variable times in which they began coding late maternal deaths. Timing models were additionally supplemented with temporal information about pregnancy-related deaths from Demographic and Health Surveys maternal mortality modules. These data only reported on antepartum, intrapartum, and post-partum death. To maximise the volume and geographical distribution of data to inform causal attribution, we again modelled the proportion of deaths due to each cause and timing category using DisMod-MR 2.1.
The exception was HIV-related maternal mortality, for which the proportion was estimated using the population attributable fraction approach described above (figure 1, step 9). All data for cause and timing models for which late maternal death was excluded were statistically crosswalked within DisMod-MR 2.1 to the reference definition where late maternal death is included. Analytical details of DisMod-MR have been previously described.10 Further description, including details about updates contained in DisMod-MR 2.1 and statistical crosswalks, are also included in the appendix (pp 21–24). To correct for ascertainment bias inherent in the introduction of late maternal death partway through the MDG period, we corrected overall maternal mortality estimates for the systematic exclusion of late maternal death in those location years where it was not coded (figure 1, step 10). Selection criteria to identify those geographies and years to be corrected are described above. Geographies where coding of late maternal deaths was introduced partway through the time period were only corrected for the years before introduction. Age-specific, year-specific, and geography-specific proportions predicted by DisMod-MR 2.1 for underlying causes and timing were then applied to the overall maternal mortality model developed in CODEm (figure 1, step 11).
Ensuring consistency with all other causes of death
Another crucial strength of the GBD approach to maternal mortality is that all results are internally consistent with all other specific causes of death (figure 1, step 12). CoDCorrect is a process that uses a simple algorithm to scale all cause-specific deaths from all causes for each age group, sex, year, and location, and thereby ensures that the sum equals total all-cause mortality. For maternal mortality, it further scaled the sum of all cause-specific and timing-specific estimates to equal the total for all maternal mortality. Further details on CoDCorrect and its implementation are described in the appendix (p 48).
Age groups and fertility
Previous analyses have truncated evaluation of maternal mortality at 15 years to 49 years. Doing so ignores the non-trivial number of pregnancies and deaths occurring in those younger than 15 years and older than 50 years.35 Deaths in these age groups are routinely coded in our data sources, so for the first time, we have expanded the age range of our maternal mortality analysis to include all 5-year age groups from 10 years to 54 years in GBD 2015. To facilitate calculation of MMR in these age groups, our demographic analysis included expansion of UN Population Division estimates of age-specific livebirths to include 10–14 years and 50–54 years (figure 1, step 13). The appendix (pp 49–50, 684–701) provides more detail on fertility estimation in these age groups and a table of age-specific livebirths for all locations.
Uncertainty analysis
We report 95% UIs for all estimates. UIs include uncertainty introduced by variable sample sizes, data adjustments for all-cause mortality sources, and cause-specific model specifications and estimation. In CODEm, after a model weighting scheme has been chosen, each model contributes a number of draws proportional to its weight such that 1000 draws are created. The mean of the draws is used as the final estimate for the CODEm process and 95% UI are created from the 0·025 and 0·975 quantiles of the draws. In DisMod-MR 2.1, uncertainty is calculated by sampling 1000 draws from the posterior distribution of each most-detailed geography, age group, and year. UIs for underlying causes and timing are propagated from the combination of CODEm and DisMod-MR 2.1 draws. We propagated uncertainty into all the final quantities of interest at all levels of geographic, temporal, and age-specific aggregations assuming no correlation between them.
Analysis of levels and trends
MMR, annualised rate of change, and reporting metrics
We report number of deaths and MMR; number of deaths per 100 000 livebirths) for ages 10–54 years inclusive. We calculated MMR for each 5-year age group separately using age-specific livebirths (figure 1, step 14). We calculated annualised rate of change (ARC) using the two-point continuously compounded rate-of-change formula36 in each geography separately for 1990–2000, 2000–15, 1990–2015, and all single years throughout the time period. ARC examination shows overall trends, highlights periods of acceleration (or deceleration) in improvement, and allows identification of those countries that probably achieved MDG 5.
Drivers of change in the MDG era, coverage target setting for SDGs
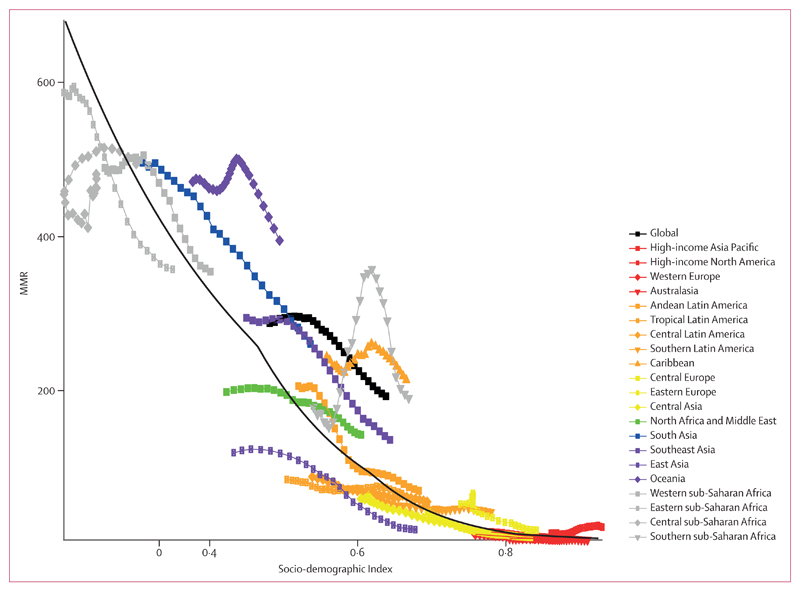
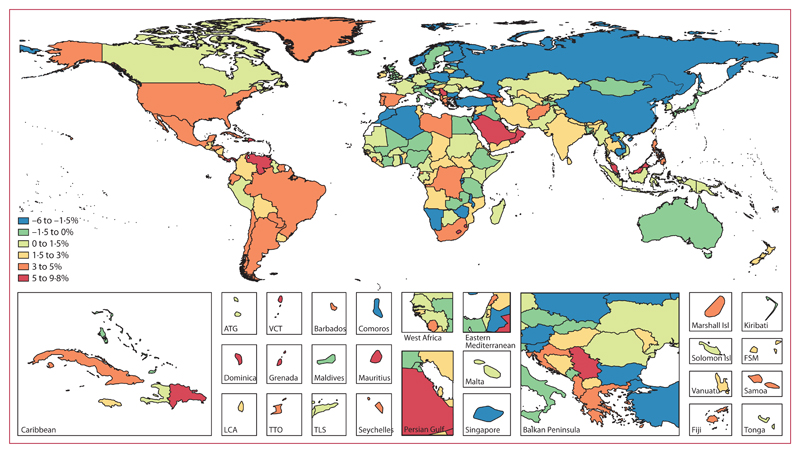
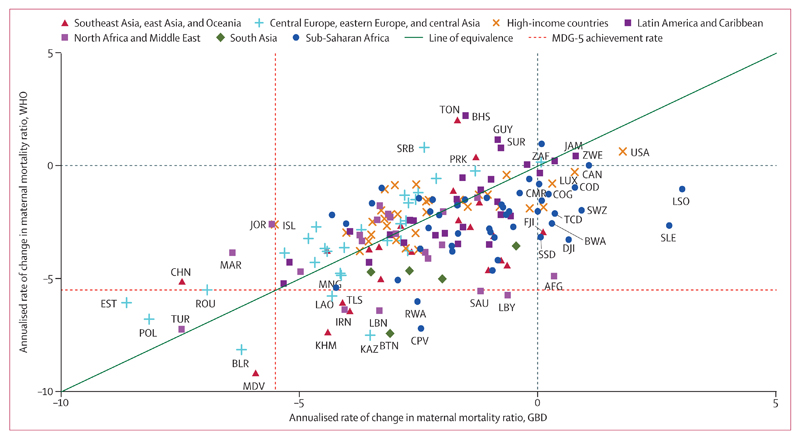
For GBD 2015, we completed two additional analyses to systematically describe drivers of levels and trends in maternal mortality. First, we examined the relation between MMR and SDI, a summary indicator derived from measures of income per capita, educational attainment, and fertility using the Human Development Index method.37 The SDI has an interpretable scale: zero represents the lowest income per capita, lowest educational attainment, and highest total fertility rate noted across all GBD geographies from 1980 to 2015 and one represents the highest income per capita, highest educational attainment, and lowest total fertility rate. We then used spline regression to calculate the average relation between MMR and SDI, thereby facilitating further evaluation of geographical and temporal MMR trends. Further details of SDI development and spline regressions are in the appendix (p 48). We then used the average relation between SDI and MMR to calculate observed minus expected (O–E) MMR ratio and O–E ARC (from 2000 to 2015), respectively, to show average patterns that can help to benchmark a country against other countries and provides insights into whether or not public action or other factors have been leading to narrowing—or growing—inequalities since the MDG declaration. Second, to capture how improvements in women’s access to the specific modes of reproductive health care might change the average relation observed between SDI and MMR, we also examined the relation between MMR and coverage of one visit of antenatal care, four antenatal care visits (a proxy for more comprehensive care), in-facility delivery, and skilled birth attendance by calculating the average coverage of each over different MMR ranges.
Role of the funding source
The funder of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The authors had access to the data in the study and had final responsibility for the decision to submit for publication.
Results
Global and country-specific maternal mortality
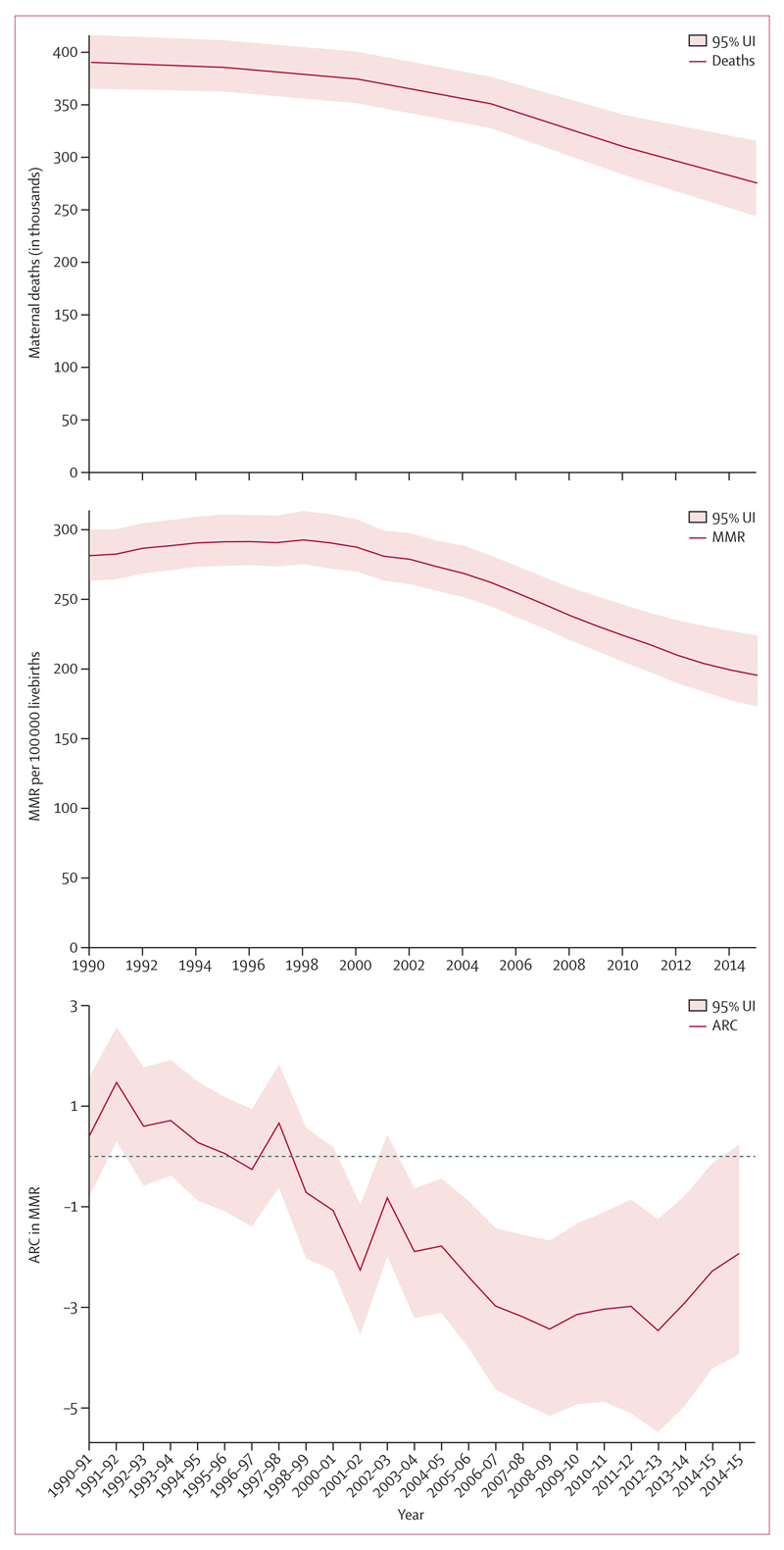
Global maternal deaths decreased slightly from 390 185 (95% UI 365 193–416 235) in 1990 to 374 321 (351 336–400 419) in 2000 before dropping to 275 288 (243 757–315 490) in 2015 (figure 3). The overall decrease from 1990 to 2015 in global maternal deaths was roughly 29% and the decrease in MMR was 30%. Table 1 shows results for all specific geographies in the GBD hierarchy. MMR followed a similar trend to overall maternal deaths; MMR was 282 (95% UI 264–300) in 1990, 288 (270–308) in 2000, and decreased to 196 (173–224) in 2015. Global ARC was –1·5% (95% UI –2·0 to –0·9) across the entire MDG period from 1990 to 2015. Global ARC was initially relatively flat at 0·2% (–0·5 to 0·9) from 1990 to 2000, but accelerated greatly after the Millennium Declaration to be –2·6% (–3·4 to –1·7) from 2000 to 2015. Looking at single-year ARC, we see the global acceleration began in the year 2001 and has continued accelerating until 2007–08, after which the rate of improvement has slowed.
Figure 3. Global results with 95% uncertainty interval (UI) for maternal deaths, maternal mortality ratio (MMR; number of deaths per 100 000 livebirths), and annualised rate of change (ARC) in MMR by year, 1990–2015.
Table 1.
Global, regional, and national or territory number of maternal deaths, maternal mortality ratio (MMR; number of deaths per 100 000 livebirths), and annualised rates of change in percent, 1990–2015
| Number of maternal deaths |
Maternal mortality ratio (per 100 000 livebirths) |
Annualised rate of change in maternal mortality ratio (%) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2000 | 2015 | 1990 | 2000 | 2015 | 1990–2000 | 2000–15 | 1990–2015 | |
| Global | 390 185 (365 193 to 416 235) |
374 321 (351 336 to 400 419) |
275 288 (243 757 to 315 490) |
281·5 (263·6 to 300·3) |
287·6 (270·1 to 307·6) |
195·7 (173·4 to 224·2) |
0·2 (–0·5 to 0·9) |
–2·6 (–3·4 to –1·7) |
–1·5 (–2·0 to –0·9) |
| High SDI | 3811 (3615 to 4012) |
2505 (2400 to 2608) |
2108 (1990 to 2235) |
25·4 (24·1 to 26·8) |
19·1 (18·3 to 19·8) |
15·0 (14·2 to 15·9) |
–2·9 (–3·5 to –2·3) |
–1·6 (–2·1 to –1·1) |
–2·1 (–2·4 to –1·8) |
| High-middle SDI | 25 802 (23 828 to 28 112) |
17 047 (15 867 to 18 944) |
10 245 (9113 to 11 423) |
86·9 (80·3 to 94·7) |
69·9 (65·1 to 77·7) |
41·9 (37·3 to 46·8) |
–2·2 (–2·9 to –1·3) |
–3·4 (–4·2 to –2·7) |
–2·9 (–3·4 to –2·5) |
| Middle SDI | 94 963 (87 723 to 103 991) |
69 038 (63 737 to 75 198) |
37 015 (32 496 to 42 666) |
226·2 (209·0 to 247·6) |
201·2 (185·8 to 219·1) |
101·7 (89·4 to 117·2) |
–1·2 (–1·9 to –0·4) |
–4·6 (–5·5 to –3·5) |
–3·2 (–3·8 to –2·6) |
| Low-middle SDI | 196 860 (178 400 to 216 483) |
197 781 (180 988 to 215 810) |
135 086 (114 335 to 166 218) |
496·7 (450·2 to 546·2) |
463·9 (424·5 to 505·7) |
298·2 (252·5 to 363·9) |
–0·7 (–1·8 to 0·4) |
–3·0 (–4·1 to –1·5) |
–2·1 (–2·8 to –1·1) |
| Low SDI | 68 497 (59 819 to 78 539) |
87 679 (77 726 to 98 833) |
90 639 (73 603 to 112 175) |
560·9 (489·9 to 642·8) |
562·9 (499·0 to 634·5) |
443·2 (360·3 to 546·6) |
0·1 (–1·4 to 1·3) |
–1·7 (–3·1 to –0·1) |
–1·0 (–1·8 to 0·0) |
| High income | 2321 (2233 to 2419) |
1848 (1782 to 1920) |
1989 (1877 to 2109) |
18·9 (18·2 to 19·7) |
15·8 (15·2 to 16·4) |
16·9 (16·0 to 17·9) |
–1·8 (–2·3 to –1·4) |
0·5 (0·0 to 0·9) |
–0·5 (–0·7 to –0·2) |
| High-income North America |
699 (668 to 734) |
727 (693 to 762) |
1091 (1016 to 1177) |
16·0 (15·3 to 16·8) |
16·7 (16·0 to 17·5) |
24·7 (23·0 to 26·7) |
0·5 (0·0 to 1·0) |
2·6 (2·0 to 3·2) |
1·8 (1·4 to 2·1) |
| Canada | 23 (20 to 27) |
26 (23 to 29) |
28 (24 to 34) |
6·0 (5·2 to 6·9) |
7·7 (6·8 to 8·8) |
7·3 (6·2 to 8·7) |
2·5 (0·8 to 4·3) |
–0·4 (–1·8 to 1·1) |
0·8 (–0·1 to 1·7) |
| Greenland | 1 (0 to 1) |
0 (0 to 1) |
0 (0 to 0) |
20·9 (15·5 to 29·0) |
21·2 (16·2 to 28·6) |
14·3 (10·4 to 20·9) |
0·1 (–3·0 to 3·3) |
–2·7 (–5·3 to –0·4) |
–1·5 (–3·3 to 0·1) |
| USA | 674 (644 to 711) |
700 (666 to 735) |
1063 (988 to 1 145) |
16·9 (16·2 to 17·8) |
17·5 (16·6 to 18·3) |
26·4 (24·6 to 28·4) |
0·3 (–0·2 to 0·8) |
2·7 (2·2 to 3·4) |
1·8 (1·4 to 2·1) |
| Australasia | 26 (23 to 30) |
25 (22 to 28) |
25 (21 to 29) |
8·4 (7·4 to 9·6) |
8·1 (7·1 to 9·1) |
6·6 (5·6 to 7·7) |
–0·5 (–1·9 to 1·0) |
–1·4 (–2·6 to –0·1) |
–1·0 (–1·8 to –0·2) |
| Australia | 19 (16 to 22) |
19 (16 to 22) |
18 (15 to 21) |
7·5 (6·4 to 8·7) |
7·6 (6·6 to 8·7) |
5·5 (4·6 to 6·6) |
0·1 (–1·8 to 2·0) |
–2·1 (–3·5 to –0·7) |
–1·2 (–2·1 to –0·2) |
| New Zealand | 7 (6 to 8) |
6 (5 to 7) |
7 (6 to 9) |
12·6 (10·7 to 14·6) |
10·2 (8·7 to 12·0) |
12·0 (10·0 to 14·3) |
–2·1 (–4·2 to 0·0) |
1·1 (–0·5 to 2·6) |
–0·2 (–1·2 to 0·8) |
| High-income Asia Pacific |
345 (319 to 371) |
192 (180 to 207) |
123 (112 to 135) |
17·2 (15·9 to 18·5) |
11·0 (10·3 to 11·8) |
8·0 (7·3 to 8·8) |
–4·5 (–5·4 to –3·6) |
–2·1 (–2·9 to –1·3) |
–3·0 (–3·5 to –2·6) |
| Brunei | 4 (3 to 5) |
3 (2 to 4) |
2 (2 to 3) |
48·2 (37·8 to 60·5) |
40·8 (33·7 to 48·6) |
33·5 (26·8 to 42·1) |
–1·6 (–4·4 to 0·9) |
–1·4 (–3·1 to 0·6) |
–1·5 (–2·9 to –0·1) |
| Japan | 164 (157 to 172) |
102 (97 to 108) |
66 (60 to 71) |
12·8 (12·3 to 13·5) |
8·8 (8·4 to 9·4) |
6·4 (5·8 to 6·9) |
–3·7 (–4·3 to –3·2) |
–2·1 (–2·9 to –1·6) |
–2·8 (–3·2 to –2·4) |
| Singapore | 5 (5 to 6) |
5 (5 to 6) |
2 (2 to 2) |
10·6 (9·3 to 12·1) |
11·5 (10·1 to 13·0) |
5·0 (4·3 to 5·8) |
0·9 (–0·9 to 2·4) |
–5·5* (–6·8 to –4·4) |
–3·0 (–3·9 to –2·2) |
| South Korea | 171 (148 to 195) |
82 (72 to 93) |
53 (44 to 62) |
25·5 (22·1 to 29·1) |
15·1 (13·3 to 17·2) |
11·6 (9·6 to 13·6) |
–5·3 (–7·0 to –3·7) |
–1·7 (–3·3 to –0·3) |
–3·2 (–4·1 to –2·3) |
| Western Europe | 617 (584 to 652) |
439 (417 to 461) |
315 (288 to 338) |
13·7 (13·0 to 14·5) |
10·2 (9·7 to 10·7) |
7·2 (6·6 to 7·7) |
–3·0 (–3·6 to –2·4) |
–2·4 (–3·0 to –1·8) |
–2·6 (–3·1 to –2·3) |
| Andorra | 0 (0 to 0) |
0 (0 to 0) |
0 (0 to 0) |
3·8 (1·9 to 5·5) |
2·5 (1·1 to 3·9) |
2·0 (1·1 to 3·0) |
–4·2 (–8·5 to –0·3) |
–1·6 (–4·4 to 3·3) |
–2·7 (–4·6 to 0·3) |
| Austria | 10 (9 to 12) |
6 (5 to 7) |
3 (3 to 4) |
11·6 (10·4 to 13·0) |
7·5 (6·7 to 8·3) |
4·2 (3·7 to 4·8) |
–4·4 (–5·8 to –3·0) |
–3·8 (–4·9 to –2·7) |
–4·0 (–4·8 to –3·3) |
| Belgium | 17 (15 to 19) |
12 (10 to 13) |
10 (8 to 11) |
14·1 (12·5 to 15·7) |
10·2 (9·1 to 11·4) |
7·4 (6·4 to 8·5) |
–3·2 (–4·7 to –1·9) |
–2·2 (–3·4 to –1·0) |
–2·6 (–3·4 to –1·9) |
| Cyprus | 2 (1 to 2) |
1 (1 to 2) |
0 (0 to 0) |
13·4 (10·1 to 17·4) |
12·0 (9·0 to 15·5) |
5·6 (4·1 to 7·2) |
–1·0 (–4·3 to 2·0) |
–5·2 (–7·8 to –2·3) |
–3·6 (–5·1 to –1·8) |
| Denmark | 6 (5 to 7) |
4 (3 to 4) |
3 (2 to 3) |
9·6 (8·3 to 11·0) |
5·8 (4·9 to 6·8) |
4·2 (3·5 to 5·1) |
–5·1 (–6·9 to –3·2) |
–2·0 (–3·6 to –0·6) |
–3·3 (–4·2 to –2·3) |
| Finland | 5 (4 to 6) |
4 (4 to 5) |
2 (2 to 3) |
7·9 (6·9 to 9·1) |
7·4 (6·5 to 8·6) |
3·8 (3·2 to 4·5) |
–0·6 (–2·3 to 1·3) |
–4·6 (–6·0 to –3·1) |
–3·0 (–3·8 to –2·1) |
| France | 126 (110 to 144) |
88 (76 to 99) |
61 (51 to 73) |
16·9 (14·7 to 19·3) |
11·7 (10·2 to 13·2) |
7·8 (6·5 to 9·3) |
–3·7 (–5·5 to –2·1) |
–2·7 (–4·3 to –1·2) |
–3·1 (–4·0 to –2·2) |
| Germany | 167 (151 to 187) |
85 (76 to 94) |
62 (54 to 70) |
20·2 (18·2 to 22·6) |
11·3 (10·2 to 12·6) |
9·0 (7·9 to 10·3) |
–5·8* (–7·1 to –4·5) |
–1·5 (–2·6 to –0·4) |
–3·2 (–3·9 to –2·6) |
| Greece | 10 (9 to 12) |
9 (7 to 10) |
9 (8 to 11) |
9·7 (8·5 to 11·0) |
8·2 (7·2 to 9·3) |
10·0 (8·4 to 11·5) |
–1·6 (–3·2 to 0·0) |
1·3 (0·1 to 2·5) |
0·1 (–0·7 to 0·9) |
| Iceland | 0 (0 to 0) |
0 (0 to 0) |
0 (0 to 0) |
2·9 (2·5 to 3·4) |
1·2 (1·1 to 1·4) |
0·7 (0·6 to 0·8) |
–8·6* (–10·5 to –6·9) |
–3·5 (–4·8 to –2·1) |
–5·5* (–6·3 to –4·6) |
| Ireland | 4 (3 to 4) |
3 (2 to 3) |
3 (2 to 4) |
7·0 (5·7 to 8·4) |
5·1 (4·3 to 6·1) |
4·7 (3·6 to 5·9) |
–3·2 (–5·6 to –0·7) |
–0·6 (–2·7 to 1·5) |
–1·6 (–2·9 to –0·3) |
| Israel | 11 (10 to 13) |
10 (9 to 11) |
10 (8 to 11) |
11·1 (9·7 to 12·6) |
7·8 (6·8 to 8·7) |
5·8 (4·9 to 6·8) |
–3·6 (–5·2 to –1·9) |
–1·9 (–3·3 to –0·7) |
–2·6 (–3·4 to –1·7) |
| Italy | 56 (50 to 63) |
37 (32 to 42) |
21 (18 to 24) |
10·1 (9·0 to 11·4) |
6·9 (6·0 to 7·8) |
4·2 (3·6 to 4·9) |
–3·8 (–5·4 to –2·3) |
–3·3 (–4·6 to –2·0) |
–3·5 (–4·3 to –2·7) |
| Luxembourg | 0 (0 to 1) |
0 (0 to 0) |
1 (1 to 1) |
10·2 (8·9 to 11·8) |
6·7 (5·8 to 7·7) |
11·0 (9·3 to 12·8) |
–4·2 (–6·0 to –2·5) |
3·3 (2·0 to 4·7) |
0·3 (–0·6 to 1·2) |
| Malta | 1 (1 to 1) |
0 (0 to 1) |
0 (0 to 0) |
10·5 (9·1 to 12·1) |
10·9 (9·5 to 12·5) |
5·9 (5·1 to 6·9) |
0·4 (–1·5 to 2·1) |
–4·1 (–5·5 to –2·8) |
–2·3 (–3·2 to –1·5) |
| Netherlands | 23 (20 to 26) |
26 (23 to 29) |
12 (10 to 14) |
12·0 (10·5 to 13·7) |
13·2 (11·7 to 14·9) |
6·7 (5·8 to 7·8) |
1·0 (–0·6 to 2·6) |
–4·5 (–5·8 to –3·3) |
–2·3 (–3·1 to –1·6) |
| Norway | 4 (3 to 5) |
3 (3 to 4) |
2 (2 to 3) |
6·7 (5·7 to 7·9) |
6·0 (5·1 to 7·0) |
3·8 (3·2 to 4·5) |
–1·2 (–3·2 to 0·9) |
–3·0 (–4·6 to –1·4) |
–2·3 (–3·3 to –1·4) |
| Portugal | 21 (19 to 24) |
15 (13 to 17) |
7 (6 to 9) |
18·8 (16·7 to 21·3) |
13·3 (11·8 to 14·9) |
9·0 (7·8 to 10·3) |
–3·5 (–5·0 to –2·0) |
–2·6 (–3·7 to –1·4) |
–2·9 (–3·7 to –2·2) |
| Spain | 50 (45 to 56) |
30 (27 to 34) |
23 (20 to 27) |
12·5 (11·1 to 13·9) |
7·5 (6·7 to 8·4) |
5·6 (4·8 to 6·4) |
–5·1 (–6·6 to –3·7) |
–1·9 (–3·2 to –0·8) |
–3·2 (–3·9 to –2·5) |
| Sweden | 12 (11 to 13) |
6 (6 to 7) |
5 (5 to 6) |
10·4 (9·6 to 11·4) |
6·8 (6·2 to 7·4) |
4·4 (3·9 to 4·9) |
–4·4 (–5·4 to –3·3) |
–2·9 (–3·9 to –2·0) |
–3·5 (–4·1 to –2·9) |
| Switzerland | 6 (5 to 7 |
6 (5 to 7) |
5 (4 to 6) |
7·1 (6·2 to 8·1) |
7·6 (6·6 to 8·7) |
5·8 (4·9 to 6·8) |
0·7 (–0·9 to 2·4) |
–1·8 (–3·1 to –0·4) |
–0·8 (–1·7 to 0·1) |
| UK | 85 (80 to 90) |
93 (87 to 99) |
75 (69 to 81) |
10·9 (10·3 to 11·6) |
13·4 (12·5 to 14·2) |
9·2 (8·5 to 10·0) |
2·1 (1·4 to 2·7) |
–2·5 (–3·1 to –1·8) |
–0·7 (–1·1 to –0·3) |
| England | 68 (64 to 73) |
75 (70 to 80) |
61 (56 to 67) |
10·5 (9·8 to 11·3) |
12·8 (11·9 to 13·7) |
8·8 (8·0 to 9·6) |
1·9 (1·2 to 2·7) |
–2·5 (–3·2 to –1·7) |
–0·7 (–1·2 to –0·3) |
| Northern Ireland |
3 (3 to 4) |
4 (3 to 4) |
3 (3 to 3) |
12·3 (10·8 to 14·1) |
16·0 (14·1 to 18·3) |
11·9 (10·2 to 13·9) |
2·7 (0·9 to 4·2) |
–1·9 (–3·2 to –0·7) |
–0·1 (–1·0 to 0·7) |
| Scotland | 9 (8 to 10) |
11 (9 to 12) |
7 (6 to 8) |
14·3 (12·5 to 16·2) |
19·4 (17·0 to 22·0) |
13·1 (11·3 to 15·2) |
3·0 (1·5 to 4·7) |
–2·6 (–3·9 to –1·3) |
–0·4 (–1·1 to 0·4) |
| Wales | 4 (3 to 4) |
4 (4 to 5) |
3 (3 to 4) |
10·0 (8·7 to 11·5) |
12·6 (11·1 to 14·2) |
9·3 (8·0 to 10·9) |
2·3 (0·4 to 3·9) |
–2·0 (–3·3 to –0·6) |
–0·3 (–1·1 to 0·5) |
| Southern Latin America |
635 (582 to 693) |
466 (426 to 509) |
435 (385 to 498) |
60·1 (55·2 to 65·6) |
45·3 (41·5 to 49·5) |
42·0 (37·2 to 48·0) |
–2·8 (–4·0 to –1·6) |
–0·5 (–1·5 to 0·6) |
–1·4 (–2·0 to –0·8) |
| Argentina | 463 (412 to 518) |
390 (351 to 431) |
377 (328 to 438) |
64·9 (57·7 to 72·5) |
54·2 (48·8 to 59·9) |
50·0 (43·6 to 58·1) |
–1·8 (–3·2 to –0·4) |
–0·6 (–1·7 to 0·7) |
–1·1 (–1·7 to –0·3) |
| Chile | 149 (133 to 164) |
60 (53 to 67) |
48 (41 to 56) |
52·1 (46·8 to 57·5) |
23·6 (21·0 to 26·5) |
20·5 (17·6 to 23·9) |
–7·9* (–9·3 to –6·4) |
–0·9 (–2·2 to 0·3) |
–3·7 (–4·5 to –3·0) |
| Uruguay | 23 (20 to 25) |
16 (14 to 18) |
10 (9 to 12) |
39·8 (35·0 to 44·5) |
29·8 (26·4 to 33·4) |
21·3 (18·3 to 24·8) |
–2·9 (–4·3 to –1·3) |
–2·2 (–3·5 to –1·0) |
–2·5 (–3·2 to –1·7) |
| Central Europe, eastern Europe, and central Asia | 3503 (3336 to 3675) |
2023 (1913 to 2142) |
1135 (1032 to 1239) |
52·4 (49·9 to 54·9) |
43·8 (41·4 to 46·4) |
20·3 (18·5 to 22·2) |
–1·8 (–2·4 to –1·1) |
–5·1 (–5·9 to –4·5) |
–3·8 (–4·2 to –3·4) |
| Eastern Europe | 1570 (1432 to 1705) |
934 (860 to 1 017) |
478 (425 to 539) |
52·9 (48·3 to 57·5) |
48·3 (44·5 to 52·5) |
18·9 (16·8 to 21·3) |
–0·9 (–2·0 to 0·2) |
–6·3* (–7·3 to –5·3) |
–4·1 (–4·7 to –3·5) |
| Belarus | 53 (46 to 61) |
36 (31 to 42) |
9 (7 to 11) |
37·5 (32·5 to 43·1) |
40·7 (35·0 to 47·2) |
7·9 (6·1 to 10·1) |
0·8 (–1·0 to 2·6) |
–10·9* (–12·9 to –9·0) |
–6·2* (–7·3 to –5·2) |
| Estonia | 8 (7 to 9) |
3 (3 to 3) |
1 (1 to 1) |
40·0 (35·1 to 45·4) |
23·4 (20·5 to 26·6) |
4·6 (3·8 to 5·6) |
–5·4 (–7·1 to –3·8) |
–10·8* (–12·5 to –9·3) |
–8·6* (–9·6 to –7·7) |
| Latvia | 17 (15 to 19) |
5 (4 to 6) |
3 (2 to 3) |
47·4 (41·6 to 53·7) |
26·2 (23·0 to 29·8) |
12·6 (10·6 to 14·8) |
–5·9* (–7·5 to –4·3) |
–4·9 (–6·3 to –3·5) |
–5·3 (–6·1 to –4·5) |
| Lithuania | 17 (15 to 20) |
5 (5 to 6) |
3 (3 to 3) |
32·0 (28·3 to 36·0) |
15·5 (13·5 to 17·6) |
10·0 (8·5 to 11·6) |
–7·2* (–8·8 to –5·6) |
–2·9 (–4·3 to –1·6) |
–4·7 (–5·4 to –3·9) |
| Moldova | 39 (34 to 43) |
15 (13 to 17) |
6 (5 to 7) |
48·0 (42·7 to 53·7) |
30·4 (26·6 to 34·6) |
14·4 (12·1 to 17·2) |
–4·5 (–6·1 to –2·9) |
–5·0 (–6·5 to –3·5) |
–4·8 (–5·7 to –4·0) |
| Russia | 1123 (1003 to 1247) |
655 (587 to 732) |
340 (292 to 398) |
56·1 (50·2 to 62·4) |
49·3 (44·2 to 55·1) |
18·7 (16·0 to 21·8) |
–1·3 (–2·8 to 0·1) |
–6·5* (–7·8 to –5·2) |
–4·4 (–5·1 to –3·7) |
| Ukraine | 313 (279 to 348) |
215 (192 to 241) |
116 (96 to 138) |
49·4 (44·0 to 54·9) |
53·3 (47·5 to 59·8) |
24·0 (19·9 to 28·5) |
0·7 (–0·7 to 2·3) |
–5·3 (–6·7 to –3·9) |
–2·9 (–3·8 to –2·0) |
| Central Europe | 738 (698 to 784) |
245 (230 to 262) |
111 (101 to 119) |
42·6 (40·3 to 45·2) |
20·4 (19·1 to 21·7) |
9·7 (8·8 to 10·4) |
–7·4* (–8·1 to –6·6) |
–5·0 (–5·7 to –4·3) |
–5·9* (–6·4 to –5·5) |
| Albania | 23 (19 to 28) |
8 (7 to 10) |
4 (3 to 5) |
29·3 (23·6 to 35·8) |
15·7 (12·8 to 19·0) |
9·6 (6·8 to 13·1) |
–6·2* (–8·9 to –3·7) |
–3·3 (–5·9 to –0·7) |
–4·5 (–5·9 to –3·0) |
| Bosnia and Herzegovina | 23 (19 to 29) |
10 (8 to 14) |
4 (3 to 6) |
36·4 (29·5 to 45·5) |
27·2 (20·4 to 36·1) |
13·2 (10·0 to 17·4) |
–2·9 (–5·9 to 0·1) |
–4·8 (–7·1 to –2·5) |
–4·1 (–5·4 to –2·7) |
| Bulgaria | 49 (44 to 54) |
35 (31 to 38) |
14 (12 to 16) |
46·4 (42·1 to 51·3) |
53·4 (48·0 to 59·0) |
21·1 (18·2 to 24·1) |
1·4 (0·1 to 2·6) |
–6·2* (–7·3 to –5·1) |
–3·2 (–3·8 to –2·5) |
| Croatia | 9 (8 to 10) |
6 (6 to 7) |
4 (3 to 4) |
16·1 (14·3 to 18·2) |
14·0 (12·5 to 15·8) |
9·5 (8·3 to 10·7) |
–1·4 (–2·9 to 0·0) |
–2·6 (–3·9 to –1·5) |
–2·1 (–2·9 to –1·4) |
| Czech Republic | 22 (20 to 25) |
9 (8 to 10) |
7 (6 to 8) |
17·5 (15·6 to 19·5) |
10·1 (9·0 to 11·2) |
6·2 (5·2 to 7·2) |
–5·5* (–7·0 to –4·1) |
–3·2 (–4·5 to –2·0) |
–4·1 (–5·0 to –3·4) |
| Hungary | 24 (21 to 27) |
11 (10 to 12) |
9 (8 to 11) |
19·0 (16·7 to 21·7) |
11·4 (10·0 to 12·9) |
10·0 (8·6 to 11·7) |
–5·2 (–6·8 to –3·5) |
–0·8 (–2·1 to 0·4) |
–2·6 (–3·4 to –1·8) |
| Macedonia | 6 (5 to 7) |
4 (3 to 4) |
2 (2 to 2) |
16·8 (13·7 to 20·5) |
14·5 (12·5 to 16·8) |
8·3 (6·8 to 10·2) |
–1·5 (–3·7 to 0·7) |
–3·7 (–5·3 to –2·1) |
–2·8 (–4·0 to –1·6) |
| Montenegro | 1 (1 to 2) |
1 (1 to 2) |
0 (0 to 1) |
11·4 (8·5 to 14·9) |
14·1 (10·7 to 18·4) |
5·7 (4·1 to 8·0) |
2·0 (–1·1 to 5·2) |
–5·9* (–9·2 to –3·0) |
–2·8 (–4·6 to –0·8) |
| Poland | 194 (176 to 212) |
49 (44 to 54) |
17 (15 to 20) |
34·0 (30·8 to 37·2) |
13·2 (11·9 to 14·6) |
4·4 (3·9 to 5·1) |
–9·4* (–10·7 to –8·1) |
–7·3* (–8·4 to –6·2) |
–8·2* (–8·8 to –7·5) |
| Romania | 342 (311 to 377) |
88 (78 to 99) |
34 (28 to 40) |
107·5 (97·7 to 118·4) |
39·6 (35·2 to 44·4) |
18·9 (15·9 to 22·4) |
–10·0* (–11·4 to –8·6) |
–4·9 (–6·4 to –3·5) |
–6·9* (–7·8 to –6·2) |
| Serbia | 30 (22 to 44) |
15 (13 to 18) |
10 (8 to 12) |
21·0 (15·2 to 30·7) |
12·6 (10·8 to 14·9) |
11·0 (9·3 to 13·2) |
–4·7 (–9·1 to –1·6) |
–0·9 (–2·4 to 0·8) |
–2·4 (–4·3 to –1·0) |
| Slovakia | 13 (11 to 16) |
7 (6 to 8) |
4 (3 to 4) |
16·6 (13·8 to 19·6) |
13·2 (11·4 to 15·0) |
6·6 (5·5 to 7·8) |
–2·3 (–4·1 to –0·1) |
–4·6 (–6·0 to –3·2) |
–3·7 (–4·7 to –2·7) |
| Slovenia | 2 (2 to 3) |
2 (2 to 2) |
1 (1 to 1) |
10·5 (9·2 to 12·2) |
10·6 (9·3 to 12·1) |
5·6 (4·7 to 6·6) |
0·0 (–1·6 to 1·8) |
–4·2 (–5·6 to –2·9) |
–2·5 (–3·4 to –1·7) |
| Central Asia | 1195 (1111 to 1279) |
844 (785 to 921) |
547 (476 to 616) |
60·0 (55·8 to 64·2) |
57·0 (53·1 to 62·2) |
28·4 (24·8 to 32·0) |
–0·5 (–1·5 to 0·5) |
–4·6 (–5·7 to –3·7) |
–3·0 (–3·6 to –2·5) |
| Armenia | 37 (32 to 43) |
19 (16 to 22) |
9 (8 to 12) |
49·5 (42·4 to 57·6) |
45·7 (38·7 to 53·0) |
24·1 (19·2 to 29·7) |
–0·8 (–2·9 to 1·4) |
–4·3 (–6·0 to –2·5) |
–2·9 (–3·9 to –1·9) |
| Azerbaijan | 77 (66 to 90) |
67 (57 to 79) |
38 (29 to 49) |
39·1 (33·4 to 45·5) |
47·6 (40·3 to 55·7) |
19·8 (14·8 to 25·4) |
2·0 (–0·1 to 4·2) |
–5·9* (–8·2 to –3·8) |
–2·7 (–4·0 to –1·6) |
| Georgia | 38 (31 to 44) |
17 (15 to 21) |
23 (19 to 28) |
41·5 (34·4 to 48·5) |
30·7 (25·7 to 36·6) |
42·3 (34·6 to 51·7) |
–3·0 (–5·3 to –0·6) |
2·1 (0·3 to 3·9) |
0·1 (–0·9 to 1·1) |
| Kazakhstan | 243 (217 to 270) |
147 (131 to 164) |
100 (83 to 121) |
63·5 (56·7 to 70·5) |
61·4 (54·6 to 68·4) |
26·5 (22·1 to 32·0) |
–0·3 (–1·8 to 1·1) |
–5·6* (–7·0 to –4·1) |
–3·5 (–4·3 to –2·6) |
| Kyrgyzstan | 90 (77 to 104) |
69 (60 to 80) |
74 (60 to 88) |
66·2 (56·5 to 76·5) |
63·9 (55·1 to 73·7) |
47·8 (38·9 to 56·9) |
–0·4 (–2·3 to 1·6) |
–1·9 (–3·5 to –0·4) |
–1·3 (–2·3 to –0·4) |
| Mongolia | 119 (97 to 141) |
81 (69 to 96) |
40 (31 to 51) |
171·2 (140·5 to 202·4) |
175·4 (149·3 to 205·9) |
58·3 (45·0 to 73·2) |
0·3 (–2·0 to 2·4) |
–7·4* (–9·5 to –5·4) |
–4·3 (–5·4 to – 3·2) |
| Tajikistan | 151 (130 to 173) |
107 (92 to 126) |
66 (51 to 84) |
71·3 (61·5 to 81·6) |
56·5 (48·1 to 66·0) |
25·6 (19·8 to 32·6) |
–2·4 (–4·2 to –0·3) |
–5·3 (–7·0 to –3·6) |
–4·1 (–5·2 to –3·0) |
| Turkmenistan | 80 (70 to 92) |
74 (61 to 89) |
22 (18 to 27) |
61·6 (53·4 to 70·5) |
69·3 (56·8 to 83·1) |
19·4 (15·7 to 23·7) |
1·1 (–1·1 to 3·4) |
–8·5* (–10·1 to –6·8) |
–4·7 (–5·6 to –3·6) |
| Uzbekistan | 359 (311 to 415) |
262 (223 to 314) |
175 (134 to 219) |
51·6 (44·6 to 59·5) |
47·6 (40·6 to 57·0) |
26·2 (20·1 to 32·8) |
–0·9 (–2·8 to 1·3) |
–4·0 (–6·0 to –2·1) |
–2·7 (–3·8 to –1·6) |
| Latin America and Caribbean | 12 238 (11 695 to 12 878) |
9690 (9225 to 10 253) |
7214 (6605 to 8030) |
112·8 (107·8 to 118·7) |
89·7 (85·4 to 94·9) |
73·6 (67·4 to 81·9) |
–2·3 (–2·8 to –1·7) |
–1·3 (–1·9 to –0·6) |
–1·7 (–2·1 to –1·3) |
| Central Latin America | 4397 (4193 to 4625) |
3512 (3349 to 3668) |
2611 (2421 to 2803) |
89·0 (84·9 to 93·6) |
71·1 (67·8 to 74·2) |
55·9 (51·8 to 60·0) |
–2·2 (–2·7 to –1·8) |
–1·6 (–2·2 to –1·1) |
–1·9 (–2·2 to –1·5) |
| Colombia | 933 (806 to 1 086) |
703 (637 to 773) |
402 (344 to 459) |
103·0 (89·2 to 119·9) |
82·9 (75·2 to 91·2) |
53·8 (46·1 to 61·5) |
–2·1 (–3·7 to –0·6) |
–2·9 (–4·1 to –1·7) |
–2·6 (–3·3 to –1·8) |
| Costa Rica | 24 (21 to 27) |
27 (24 to 30) |
17 (14 to 20) |
29·6 (25·9 to 33·2) |
34·9 (30·9 to 39·4) |
24·3 (20·6 to 28·2) |
1·6 (0·2 to 3·2) |
–2·4 (–3·7 to –1·1) |
–0·8 (–1·6 to 0·0) |
| El Salvador | 228 (197 to 263) |
72 (61 to 86) |
40 (31 to 52) |
140·2 (121·4 to 161·9) |
51·8 (44·0 to 61·3) |
38·3 (29·2 to 49·3) |
–10·0* (–12·1 to –7·8) |
–2·1 (–4·1 to 0·1) |
–5·2 (–6·4 to –4·1) |
| Guatemala | 516 (454 to 587) |
433 (389 to 483) |
320 (228 to 417) |
146·2 (129·2 to 166·0) |
106·5 (95·5 to 118·5) |
73·2 (52·1 to 95·0) |
–3·1 (–4·8 to –1·7) |
–2·6 (–4·8 to –0·6) |
–2·8 (–4·2 to –1·6) |
| Honduras | 330 (281 to 381) |
238 (172 to 319) |
185 (119 to 274) |
175·4 (149·3 to 202·5) |
120·7 (87·5 to 161·7) |
109·6 (70·3 to 162·1) |
–3·8 (–6·9 to –0·7) |
–0·7 (–3·5 to 2·1) |
–2·0 (–3·7 to –0·3) |
| Mexico | 1804 (1709 to 1912) |
1518 (1428 to 1610) |
1131 (1057 to 1206) |
73·3 (69·5 to 77·7) |
61·1 (57·5 to 64·8) |
48·2 (45·1 to 51·4) |
–1·8 (–2·2 to –1·4) |
–1·6 (–2·2 to –1·0) |
–1·7 (–2·0 to –1·3) |
| Nicaragua | 130 (111 to 152) |
136 (117 to 160) |
83 (65 to 106) |
87·4 (74·5 to 102·3) |
101·0 (86·4 to 118·7) |
68·8 (53·7 to 87·3) |
1·4 (–0·7 to 3·7) |
–2·6 (–4·4 to –0·7) |
–1·0 (–2·2 to 0·1) |
| Panama | 44 (37 to 53) |
45 (39 to 53) |
52 (41 to 65) |
68·7 (56·7 to 82·3) |
64·2 (55·1 to 75·7) |
69·4 (54·8 to 86·2) |
–0·7 (–2·7 to 1·5) |
0·5 (–1·3 to 2·4) |
0·0 (–1·1 to 1·2) |
| Venezuela | 388 (348 to 426) |
339 (305 to 374) |
381 (298 to 467) |
67·2 (60·4 to 74·0) |
58·3 (52·5 to 64·4) |
63·5 (49·8 to 77·8) |
–1·4 (–2·8 to –0·1) |
0·6 (–1·2 to 2·2) |
–0·2 (–1·3 to 0·8) |
| Andean Latin America | 2504 (2250 to 2800) |
1450 (1319 to 1583) |
825 (674 to 985) |
206·7 (185·8 to 230·9) |
121·2 (110·2 to 132·2) |
68·8 (56·2 to 82·2) |
–5·3 (–6·7 to –4·1) |
–3·8 (–5·2 to –2·4) |
–4·4 (–5·4 to –3·6) |
| Bolivia | 941 (756 to 1 169) |
535 (448 to 628) |
366 (259 to 508) |
387·0 (311·1 to 480·7) |
207·5 (174·2 to 243·6) |
144·5 (102·4 to 200·8) |
–6·1* (–8·5 to –3·9) |
–2·4 (–5·0 to 0·0) |
–3·9 (–5·7 to –2·4) |
| Ecuador | 381 (332 to 432) |
231 (197 to 266) |
170 (136 to 212) |
123·7 (108·0 to 140·4) |
73·4 (62·8 to 84·7) |
51·3 (41·0 to 63·9) |
–5·3 (–7·0 to –3·2) |
–2·4 (–4·1 to –0·7) |
–3·5 (–4·6 to –2·4) |
| Peru | 1182 (997 to 1 406) |
685 (598 to 779) |
290 (218 to 363) |
179·0 (151·0 to 212·8) |
109·7 (95·8 to 124·6) |
47·1 (35·5 to 59·0) |
–4·9 (–6·9 to –2·8) |
–5·6* (–7·6 to –3·9) |
–5·3 (–6·6 to –4·2) |
| Caribbean | 2048 (1713 to 2590) |
1959 (1632 to 2468) |
1664 (1155 to 2430) |
234·4 (196·4 to 294·7) |
240·3 (200·9 to 301·2) |
219·7 (152·5 to 319·4) |
0·2 (–2·0 to 2·8) |
–0·8 (–3·0 to 1·9) |
–0·3 (–1·7 to 1·3) |
| Antigua and Barbuda | 1 (1 to 1) |
1 (1 to 1) |
1 (0 to 1) |
54·0 (45·7 to 64·6) |
50·7 (42·0 to 60·9) |
37·2 (31·1 to 45·0) |
–0·6 (–3·1 to 1·5) |
–2·1 (–3·7 to –0·4) |
–1·5 (–2·5 to –0·6) |
| The Bahamas | 5 (4 to 6) |
4 (3 to 5) |
3 (2 to 4) |
73·6 (58·9 to 90·5) |
74·6 (60·9 to 90·9) |
50·4 (37·2 to 63·8) |
0·2 (–2·6 to 2·9) |
–2·6 (–4·7 to –0·5) |
–1·5 (–2·9 to –0·2) |
| Barbados | 3 (3 to 4) |
1 (1 to 2) |
1 (1 to 2) |
83·8 (72·1 to 95·7) |
34·8 (29·2 to 41·0) |
38·9 (30·5 to 49·2) |
–8·8* (–10·9 to –6·6) |
0·7 (–1·3 to 2·7) |
–3·1 (–4·2 to –2·0) |
| Belize | 3 (3 to 4) |
5 (4 to 5) |
3 (2 to 3) |
47·7 (39·4 to 57·0) |
62·1 (51·7 to 74·5) |
32·2 (25·2 to 41·4) |
2·6 (0·3 to 5·0) |
–4·4 (–6·3 to –2·5) |
–1·6 (–2·7 to –0·4) |
| Bermuda | 0 (0 to 0) |
0 (0 to 0) |
0 (0 to 0) |
4·6 (3·9 to 5·5) |
3·0 (2·3 to 3·7) |
2·3 (1·8 to 2·9) |
–4·5 (–7·2 to –1·8) |
–1·7 (–3·8 to 0·6) |
–2·8 (–4·0 to –1·6) |
| Cuba | 91 (80 to 103) |
75 (67 to 85) |
48 (41 to 55) |
51·3 (45·5 to 58·1) |
51·5 (45·8 to 58·2) |
41·7 (35·8 to 48·3) |
0·0 (–1·5 to 1·7) |
–1·4 (–2·6 to –0·2) |
–0·9 (–1·6 to 0·0) |
| Dominica | 0 (0 to 0) |
0 (0 to 0) |
0 (0 to 1) |
22·5 (18·5 to 27·3) |
19·4 (15·8 to 23·7) |
38·6 (30·2 to 49·0) |
–1·5 (–4·2 to 1·0) |
4·6 (2·5 to 6·5) |
2·2 (0·9 to 3·3) |
| Dominican Republic | 196 (168 to 226) |
130 (114 to 149) |
116 (92 to 144) |
91·3 (78·4 to 105·6) |
60·3 (52·7 to 69·0) |
53·6 (42·8 to 66·8) |
–4·1 (–6·2 to –2·2) |
–0·8 (–2·5 to 1·0) |
–2·2 (–3·2 to –1·0) |
| Grenada | 1 (1 to 2) |
1 (1 to 1) |
1 (1 to 1) |
51·8 (42·5 to 61·9) |
30·1 (25·6 to 36·3) |
34·0 (26·9 to 42·7) |
–5·4 (–7·7 to –3·1) |
0·8 (–1·0 to 2·8) |
–1·7 (–3·0 to –0·5) |
| Guyana | 32 (27 to 37) |
30 (26 to 37) |
16 (12 to 21) |
132·6 (111·8 to 154·9) |
160·7 (134·9 to 194·2) |
108·7 (80·5 to 140·6) |
1·8 (–0·3 to 4·2) |
–2·6 (–4·7 to –0·6) |
–0·8 (–2·1 to 0·4) |
| Haiti | 1565 (1249 to 2062) |
1564 (1247 to 2048) |
1371 (880 to 2113) |
591·6 (472·5 to 776·8) |
587·9 (469·2 to 768·1) |
520·8 (334·5 to 802·1) |
–0·1 (–2·7 to 2·9) |
–1·0 (–3·6 to 2·1) |
–0·6 (–2·2 to 1·3) |
| Jamaica | 25 (20 to 32) |
37 (29 to 45) |
24 (18 to 32) |
41·1 (32·7 to 51·4) |
66·0 (52·9 to 81·4) |
50·3 (36·4 to 66·7) |
4·8 (1·8 to 7·6) |
–1·8 (–4·2 to 0·5) |
0·8 (–0·7 to 2·3) |
| Puerto Rico | 19 (16 to 21) |
14 (12 to 16) |
7 (5 to 8) |
29·6 (25·9 to 33·4) |
25·7 (22·8 to 28·9) |
15·1 (12·7 to 17·8) |
–1·4 (–3·0 to 0·3) |
–3·6 (–4·9 to –2·2) |
–2·7 (–3·6 to –1·8) |
| Saint Lucia | 2 (2 to 3) |
3 (2 to 3) |
2 (1 to 2) |
54·7 (46·7 to 64·2) |
84·2 (72·2 to 96·4) |
59·8 (47·7 to 73·9) |
4·3 (2·3 to 6·3) |
–2·3 (–4·0 to –0·5) |
0·3 (–0·7 to 1·5) |
| Saint Vincent and the Grenadines | 1 (1 to 2) |
1 (1 to 1) |
1 (1 to 1) |
54·9 (43·9 to 68·1) |
33·9 (29·2 to 39·7) |
40·5 (33·0 to 49·1) |
–4·8 (–7·5 to –2·0) |
1·2 (–0·6 to 2·8) |
–1·2 (–2·4 to –0·1) |
| Suriname | 7 (6 to 8) |
9 (8 to 11) |
5 (4 to 6) |
62·3 (50·8 to 74·9) |
86·4 (72·5 to 103·1) |
51·5 (39·4 to 66·2) |
3·3 (0·8 to 5·7) |
–3·5 (–5·3 to –1·5) |
–0·8 (–2·1 to 0·6) |
| Trinidad and Tobago | 19 (17 to 21) |
11 (10 to 13) |
9 (7 to 12) |
75·2 (66·5 to 84·6) |
60·8 (53·0 to 69·2) |
49·4 (38·8 to 62·1) |
–2·1 (–3·8 to –0·5) |
–1·4 (–3·2 to 0·5) |
–1·7 (–2·7 to –0·6) |
| Virgin Islands | 1 (1 to 1) |
0 (0 to 0) |
0 (0 to 0) |
30·0 (24·6 to 36·9) |
21·6 (18·0 to 25·8) |
10·9 (8·6 to 13·6) |
–3·3 (–5·8 to –0·9) |
–4·6 (–6·6 to –2·6) |
–4·1 (–5·3 to –2·8) |
| Tropical Latin America | 3290 (3097 to 3509) |
2769 (2613 to 2933) |
2113 (1918 to 2313) |
86·9 (81·8 to 92·7) |
72·5 (68·4 to 76·8) |
67·0 (60·8 to 73·2) |
–1·8 (–2·6 to –1·0) |
–0·5 (–1·2 to 0·1) |
–1·0 (–1·5 to –0·6) |
| Brazil | 3081 (2896 to 3299) |
2610 (2459 to 2778) |
1972 (1786 to 2165) |
84·5 (79·4 to 90·4) |
71·0 (66·9 to 75·5) |
65·4 (59·2 to 71·8) |
–1·7 (–2·5 to –0·9) |
–0·6 (–1·3 to 0·2) |
–1·0 (–1·5 to –0·5) |
| Paraguay | 209 (177 to 244) |
159 (136 to 186) |
141 (102 to 185) |
147·9 (124·9 to 172·1) |
110·6 (95·2 to 129·3) |
100·6 (72·8 to 131·7) |
–2·9 (–5·2 to –0·7) |
–0·7 (–3·1 to 1·5) |
–1·6 (–3·0 to –0·3) |
| Southeast Asia, east Asia, and Oceania | 67 636 (59 318 to 76 231) |
45 834 (39 712 to 53 353) |
20 424 (16 922 to 25 379) |
170·8 (149·8 to 192·4) |
161·1 (139·7 to 187·5) |
68·9 (57·1 to 85·5) |
–0·6 (–1·8 to 0·8) |
–5·7* (–7·1 to –4·1) |
–3·7 (–4·5 to –2·7) |
| East Asia | 30 419 (26 086 to 35 170) |
13 780 (12 296 to 15 438) |
3236 (2767 to 3714) |
112·8 (96·8 to 130·5) |
84·2 (75·1 to 94·3) |
18·8 (16·0 to 21·5) |
–3·0 (–4·5 to –1·2) |
–10·0* (–11·3 to –8·7) |
–7·2* (–8·0 to –6·4) |
| China | 29 922 (25 545 to 34 638) |
13 344 (11 932 to 14 962) |
2948 (2501 to 3426) |
114·2 (97·6 to 132·1) |
85·2 (76·2 to 95·6) |
17·7 (15·0 to 20·5) |
–3·0 (–4·5 to –1·1) |
–10·5* (–11·9 to –9·1) |
–7·5* (–8·3 to –6·6) |
| North Korea | 426 (240 to 725) |
390 (222 to 637) |
263 (155 to 409) |
101·3 (57·2 to 171·5) |
95·3 (54·3 to 155·1) |
73·0 (43·2 to 113·4) |
–0·5 (–7·0 to 5·1) |
–1·7 (–6·2 to 2·7) |
–1·3 (–4·1 to 1·6) |
| Taiwan | 71 (46 to 104) |
46 (32 to 64) |
25 (16 to 36) |
21·1 (13·7 to 30·7) |
15·1 (10·4 to 20·9) |
11·5 (7·5 to 16·8) |
–3·3 (–7·0 to 0·3) |
–1·8 (–5·4 to 1·8) |
–2·5 (–4·7 to 0·1) |
| Southeast Asia | 36 261 (30 495 to 43 464) |
30 895 (25 298 to 38 353) |
16 112 (12 578 to 21 203) |
292·2 (245·9 to 350·0) |
262·1 (214·6 to 325·1) |
133·4 (104·2 to 175·3) |
–1·1 (–2·7 to 0·6) |
–4·5 (–6·3 to –2·4) |
–3·1 (–4·3 to –1·9) |
| Cambodia | 1493 (1247 to 1779) |
1502 (1263 to 1799) |
485 (322 to 710) |
388·6 (324·8 to 462·8) |
440·2 (370·3 to 527·2) |
130·8 (86·9 to 191·3) |
1·2 (–0·7 to 3·3) |
–8·1* (–11·2 to –5·3) |
–4·4 (–6·2 to –2·8) |
| Indonesia | 18 715 (15 508 to 21 799) |
15 726 (13 450 to 18 578) |
8937 (6104 to 12 557) |
399·4 (331·1 to 464·8) |
345·3 (295·4 to 407·8) |
177·1 (121·0 to 248·6) |
–1·5 (–3·5 to 0·7) |
–4·6 (–7·2 to –1·9) |
–3·3 (–4·9 to –1·8) |
| Laos | 1193 (853 to 1 582) |
1002 (800 to 1 293) |
420 (296 to 574) |
652·7 (467·4 to 863·2) |
589·1 (470·8 to 759·9) |
234·4 (165·6 to 320·6) |
–1·0 (–3·5 to 1·8) |
–6·2* (–8·9 to –3·8) |
–4·1 (–5·8 to –2·4) |
| Malaysia | 450 (385 to 529) |
369 (325 to 421) |
313 (233 to 410) |
87·6 (74·9 to 102·9) |
70·2 (61·8 to 80·1) |
61·5 (45·8 to 80·0) |
–2·2 (–4·0 to –0·5) |
–0·9 (–3·0 to 1·2) |
–1·4 (–2·8 to –0·2) |
| Maldives | 17 (12 to 24) |
6 (5 to 7) |
3 (2 to 4) |
185·5 (136·3 to 263·4) |
93·4 (74·9 to 115·7) |
40·9 (27·7 to 56·7) |
–6·7* (–10·1 to –3·9) |
–5·5* (–8·4 to –2·9) |
–5·9* (–8·6 to –4·2) |
| Mauritius | 15 (13 to 17) |
8 (7 to 10) |
7 (6 to 8) |
67·3 (59·2 to 76·2) |
42·2 (37·3 to 47·9) |
49·6 (41·9 to 58·4) |
–4·7 (–6·3 to –3·1) |
1·1 (–0·3 to 2·5) |
–1·2 (–2·1 to –0·4) |
| Myanmar | 10 284 (5857 to 16 737) |
9503 (5027 to 16 391) |
3691 (1969 to 6476) |
909·3 (519·3 to 1478·1) |
820·8 (436·9 to 1415·5) |
391·2 (208·7 to 685·9) |
–1·1 (–5·4 to 3·2) |
–5·0 (–8·8 to –1·0) |
–3·5 (–5·9 to –0·6) |
| Philippines | 2208 (1906 to 2518) |
1636 (1499 to 1804) |
1637 (1319 to 1996) |
107·9 (93·2 to 123·1) |
70·7 (64·8 to 77·8) |
69·7 (56·2 to 85·0) |
–4·2 (–5·8 to –2·6) |
–0·1 (–1·7 to 1·3) |
–1·8 (–2·8 to –0·7) |
| Sri Lanka | 269 (223 to 324) |
222 (196 to 253) |
107 (70 to 155) |
75·2 (62·6 to 90·6) |
63·8 (56·4 to 72·7) |
33·1 (21·8 to 48·0) |
–1·6 (–3·7 to 0·3) |
–4·5 (–7·2 to –1·9) |
–3·3 (–5·1 to –1·6) |
| Seychelles | 1 (1 to 1) |
1 (0 to 1) |
1 (0 to 1) |
60·5 (46·6 to 75·8) |
38·7 (30·9 to 49·5) |
32·3 (24·5 to 43·1) |
–4·5 (–7·3 to –1·3) |
–1·2 (–3·6 to 1·1) |
–2·5 (–3·9 to –1·0) |
| Thailand | 438 (362 to 525) |
271 (207 to 344) |
143 (86 to 211) |
40·5 (33·5 to 48·6) |
29·9 (22·9 to 37·9) |
20·0 (12·1 to 29·6) |
–3·1 (–6·2 to –0·2) |
–2·7 (–5·8 to 0·2) |
–2·9 (–4·9 to –1·1) |
| Timor-Leste | 209 (141 to 277) |
152 (99 to 190) |
104 (64 to 144) |
641·3 (433·1 to 847·1) |
406·1 (264·7 to 505·3) |
236·3 (145·9 to 328·5) |
–4·5 (–9·0 to –0·3) |
–3·7 (–6·6 to –0·7) |
–3·9 (–6·3 to –2·0) |
| Vietnam | 916 (590 to 1 290) |
452 (311 to 630) |
247 (147 to 387) |
46·7 (30·2 to 65·8) |
32·1 (22·1 to 44·6) |
15·6 (9·4 to 24·4) |
–3·7 (–8·2 to 0·9) |
–4·9 (–8·9 to –1·0) |
–4·4 (–6·8 to –1·8) |
| Oceania | 957 (606 to 1449) |
1159 (685 to 1814) |
1076 (624 to 1784) |
460·6 (292·2 to 697·1) |
463·6 (274·2 to 722·5) |
386·8 (225·1 to 640·6) |
–0·1 (–3·3 to 3·8) |
–1·3 (–4·4 to 2·3) |
–0·8 (–3·0 to 1·8) |
| American Samoa | 1 (1 to 1) |
1 (1 to 1) |
1 (1 to 2) |
42·2 (30·5 to 57·9) |
59·9 (46·0 to 74·5) |
57·9 (41·0 to 79·5) |
3·5 (–0·3 to 7·1) |
–0·3 (–3·0 to 2·3) |
1·3 (–0·7 to 3·1) |
| Federated States of Micronesia | 4 (2 to 8) |
4 (2 to 7) |
2 (1 to 4) |
132·7 (64·0 to 232·8) |
118·1 (50·8 to 220·4) |
88·2 (45·4 to 167·4) |
–1·3 (–6·8 to 3·9) |
–2·0 (–6·1 to 2·8) |
–1·7 (–4·8 to 1·6) |
| Fiji | 20 (14 to 29) |
23 (18 to 29) |
17 (12 to 24) |
96·2 (65·8 to 133·9) |
114·9 (88·1 to 143·3) |
98·8 (67·4 to 135·7) |
1·9 (–2·2 to 6·0) |
–1·1 (–3·9 to 1·8) |
0·1 (–1·8 to 2·1) |
| Guam | 1 (1 to 1) |
1 (1 to 1) |
1 (1 to 2) |
21·4 (16·2 to 27·9) |
22·2 (16·9 to 28·4) |
43·0 (29·9 to 60·9) |
0·4 (–3·4 to 4·1) |
4·3 (1·3 to 7·2) |
2·8 (0·8 to 4·5) |
| Kiribati | 7 (5 to 9) |
4 (3 to 6) |
4 (3 to 6) |
250·5 (189·2 to 326·7) |
171·3 (128·5 to 220·4) |
131·2 (86·9 to 188·4) |
–3·8 (–7·0 to –0·5) |
–1·9 (–4·7 to 0·9) |
–2·7 (–4·4 to –0·6) |
| Marshall Islands | 2 (1 to 3) |
2 (1 to 3) |
2 (1 to 3) |
112·4 (80·1 to 156·0) |
126·6 (63·5 to 187·3) |
108·7 (70·0 to 165·8) |
1·2 (–3·1 to 4·9) |
–1·1 (–4·0 to 2·9) |
–0·2 (–2·1 to 2·0) |
| Northern Mariana Islands | 1 (1 to 1) |
1 (0 to 1) |
1 (1 to 1) |
78·9 (56·3 to 109·2) |
48·7 (37·2 to 62·6) |
59·5 (42·2 to 80·6) |
–4·7 (–8·3 to –1·2) |
1·3 (–1·5 to 3·9) |
–1·1 (–3·1 to 0·7) |
| Papua New Guinea | 787 (466 to 1241) |
972 (541 to 1558) |
933 (511 to 1607) |
538·1 (318·8 to 848·6) |
519·5 (290·2 to 832·7) |
434·6 (238·2 to 748·4) |
–0·5 (–4·2 to 3·7) |
–1·3 (–4·7 to 2·7) |
–0·9 (–3·4 to 1·8) |
| Samoa | 4 (2 to 5) |
3 (2 to 5) |
3 (2 to 4) |
65·0 (38·1 to 101·2) |
60·8 (30·1 to 96·0) |
55·2 (32·0 to 83·9) |
–0·6 (–6·9 to 3·6) |
–0·7 (–4·1 to 3·7) |
–0·6 (–3·1 to 1·9) |
| Solomon Islands | 33 (17 to 54) |
34 (17 to 59) |
35 (17 to 63) |
263·5 (134·3 to 434·0) |
232·9 (117·2 to 402·7) |
207·2 (102·0 to 369·1) |
–1·2 (–6·5 to 3·4) |
–0·8 (–4·7 to 3·7) |
–1·0 (–3·7 to 2·1) |
| Tonga | 6 (4 to 8) |
5 (4 to 6) |
3 (2 to 5) |
197·6 (135·8 to 278·9) |
187·2 (148·6 to 231·2) |
129·9 (84·1 to 192·4) |
–0·4 (–4·0 to 3·0) |
–2·6 (–5·5 to 0·5) |
–1·7 (–4·0 to 0·3) |
| Vanuatu | 11 (5 to 19) |
12 (5 to 22) |
12 (6 to 21) |
202·1 (102·6 to 350·5) |
202·0 (78·1 to 359·7) |
172·0 (92·0 to 309·6) |
–0·1 (–6·3 to 5·1) |
–1·2 (–5·0 to 4·3) |
–0·8 (–3·3 to 2·6) |
| North Africa and Middle East | 22 342 (19 092 to 26 906) |
20 772 (16 769 to 26 243) |
19 066 (14 475 to 25 599) |
197·8 (169·2 to 238·2) |
188·0 (151·8 to 236·6) |
142·3 (108·2 to 190·7) |
–0·5 (–2·3 to 1·1) |
–1·9 (–3·7 to –0·1) |
–1·3 (–2·4 to –0·3) |
| North Africa and Middle East | 22 342 (19 092 to 26 906) |
20 772 (16 769 to 26 243) |
19 066 (14 475 to 25 599) |
198·0 (169·3 to 238·4) |
188·1 (151·9 to 236·8) |
142·4 (108·3 to 190·9) |
–0·5 (–2·3 to 1·1) |
–1·9 (–3·7 to –0·1) |
–1·3 (–2·4 to –0·3) |
| Afghanistan | 4590 (2825 to 7111) |
7328 (4529 to 11 007) |
8525 (5010 to 13 221) |
732·3 (451·0 to 1130·9) |
753·3 (466·5 to 1130·7) |
788·9 (464·1 to 1219·2) |
0·4 (–4·8 to 5·0) |
0·3 (–3·6 to 3·8) |
0·3 (–2·1 to 2·7) |
| Algeria | 1275 (977 to 1 583) |
756 (591 to 945) |
626 (466 to 809) |
153·2 (117·5 to 190·1) |
123·9 (96·9 to 154·8) |
66·9 (49·8 to 86·4) |
–2·2 (–5·1 to 0·7) |
–4·1 (–6·6 to –1·6) |
–3·3 (–4·8 to –1·8) |
| Bahrain | 8 (6 to 11) |
5 (4 to 7) |
5 (4 to 7) |
53·6 (39·9 to 73·5) |
35·6 (27·3 to 47·3) |
24·6 (18·3 to 35·4) |
–4·0 (–7·9 to –0·6) |
–2·5 (–5·1 to 0·4) |
–3·1 (–4·9 to –1·3) |
| Egypt | 2744 (2308 to 3176) |
1186 (976 to 1414) |
1052 (809 to 1340) |
146·7 (123·4 to 169·7) |
69·2 (57·0 to 82·5) |
42·3 (32·5 to 53·9) |
–7·5* (–9·7 to –5·5) |
–3·3 (–5·3 to –1·2) |
–5·0 (–6·1 to –3·7) |
| Iran | 1039 (704 to 1432) |
426 (337 to 539) |
281 (192 to 421) |
56·6 (38·5 to 78·0) |
34·5 (27·3 to 43·7) |
20·8 (14·2 to 31·1) |
–5·0 (–8·6 to –0·6) |
–3·5 (–6·4 to –0·2) |
–4·1 (–6·0 to –1·9) |
| Iraq | 969 (702 to 1300) |
950 (655 to 1311) |
729 (428 to 1199) |
146·0 (105·9 to 195·9) |
113·4 (78·3 to 156·4) |
58·6 (34·4 to 96·1) |
–2·5 (–6·7 to 1·4) |
–4·5 (–8·2 to –1·0) |
–3·7 (–6·0 to –1·3) |
| Jordan | 116 (89 to 149) |
121 (88 to 159) |
48 (36 to 63) |
97·9 (74·6 to 125·4) |
81·2 (58·7 to 106·2) |
24·2 (17·9 to 31·5) |
–1·9 (–5·1 to 1·1) |
–8·0* (–10·7 to –5·4) |
–5·6* (–7·2 to –4·1) |
| Kuwait | 4 (3 to 5) |
5 (4 to 6) |
4 (3 to 6) |
9·7 (8·1 to 11·8) |
11·9 (10·4 to 13·5) |
5·9 (4·4 to 7·5) |
2·1 (0·0 to 4·1) |
–4·8 (–6·8 to –2·8) |
–2·0 (–3·4 to –0·7) |
| Lebanon | 24 (15 to 38) |
17 (11 to 24) |
13 (8 to 21) |
35·6 (22·8 to 55·1) |
26·7 (18·0 to 39·0) |
15·3 (9·0 to 24·0) |
–2·9 (–7·6 to 1·6) |
–3·9 (–7·6 to 0·3) |
–3·3 (–6·2 to –0·7) |
| Libya | 34 (24 to 45) |
28 (20 to 37) |
30 (20 to 43) |
26·6 (19·1 to 36·0) |
23·9 (17·2 to 31·5) |
22·8 (15·6 to 32·9) |
–1·0 (–4·8 to 2·3) |
–0·3 (–3·5 to 2·8) |
–0·6 (–2·6 to 1·3) |
| Morocco | 2441 (1891 to 3201) |
1197 (894 to 1560) |
479 (299 to 756) |
332·7 (258·7 to 436·1) |
192·0 (143·4 to 249·6) |
68·5 (42·8 to 108·1) |
–5·4 (–8·8 to –2·4) |
–7·0* (–10·1 to –3·4) |
–6·4* (–8·6 to –4·3) |
| Palestine | 29 (19 to 43) |
17 (14 to 21) |
25 (17 to 35) |
29·3 (19·0 to 43·7) |
14·2 (11·3 to 17·8) |
16·2 (11·5 to 23·2) |
–7·1* (–11·2 to –3·1) |
0·8 (–1·9 to 3·9) |
–2·4 (–4·7 to 0·2) |
| Oman | 24 (14 to 38) |
12 (8 to 18) |
13 (9 to 18) |
34·1 (20·0 to 54·8) |
21·4 (14·8 to 31·7) |
15·5 (11·0 to 21·6) |
–4·5 (–8·7 to –0·3) |
–2·2 (–5·5 to 1·2) |
–3·1 (–5·6 to –0·7) |
| Qatar | 7 (4 to 10) |
7 (5 to 10) |
7 (4 to 9) |
64·0 (42·0 to 91·5) |
59·9 (41·4 to 84·2) |
25·5 (16·4 to 35·7) |
–0·6 (–4·6 to 3·6) |
–5·7* (–9·5 to –2·4) |
–3·7 (–6·0 to –1·6) |
| Saudi Arabia | 124 (93 to 162) |
101 (86 to 119) |
97 (82 to 115) |
21·3 (16·0 to 27·9) |
17·9 (15·2 to 21·0) |
15·7 (13·3 to 18·5) |
–1·6 (–4·0 to 0·6) |
–0·9 (–2·4 to 0·6) |
–1·2 (–2·5 to 0·1) |
| Sudan | 4131 (2736 to 5570) |
4653 (2790 to 6731) |
3941 (2098 to 5999) |
485·5 (321·7 to 654·4) |
414·4 (248·7 to 598·0) |
298·8 (159·2 to 454·7) |
–1·5 (–5·7 to 1·9) |
–2·3 (–5·5 to 1·0) |
–2·0 (–4·3 to 0·1) |
| Syria | 560 (421 to 719) |
365 (276 to 480) |
237 (181 to 309) |
125·7 (94·6 to 161·6) |
73·6 (55·6 to 96·7) |
54·1 (41·3 to 70·5) |
–5·3 (–8·1 to –2·6) |
–2·0 (–4·7 to 0·5) |
–3·4 (–5·0 to –1·8) |
| Tunisia | 183 (143 to 231) |
99 (74 to 126) |
82 (54 to 115) |
85·6 (66·9 to 108·0) |
59·2 (44·3 to 75·2) |
40·6 (26·6 to 56·9) |
–3·7 (–6·6 to –0·8) |
–2·6 (–5·5 to 0·2) |
–3·0 (–4·9 to –1·4) |
| Turkey | 1453 (1057 to 1985) |
659 (510 to 847) |
204 (162 to 255) |
103·3 (75·4 to 141·2) |
48·2 (37·4 to 61·8) |
15·8 (12·6 to 19·8) |
–7·6* (–10·9 to –4·4) |
–7·4* (–9·7 to –5·1) |
–7·5* (–9·1 to –5·9) |
| United Arab Emirates | 15 (9 to 23) |
12 (9 to 17) |
18 (11 to 28) |
31·8 (19·9 to 48·8) |
24·0 (17·0 to 32·4) |
18·0 (10·7 to 28·3) |
–2·6 (–7·3 to 2·0) |
–2·0 (–6·1 to 2·0) |
–2·3 (–5·3 to 0·4) |
| Yemen | 2559 (1342 to 3890) |
2810 (1509 to 4648) |
2631 (1402 to 5009) |
402·6 (211·8 to 611·4) |
399·6 (215·7 to 659·8) |
307·4 (164·5 to 583·8) |
–0·3 (–4·1 to 4·5) |
–1·9 (–5·5 to 2·1) |
–1·3 (–3·7 to 1·8) |
| South Asia | 174 943 (161 508 to 189 038) |
157 525 (145 824 to 170 598) |
92 416 (81 008 to 108 680) |
482·5 (445·5 to 521·3) |
429·2 (397·3 to 464·7) |
264·3 (231·8 to 310·3) |
–1·2 (–1·9 to –0·4) |
–3·3 (–4·1 to –2·2) |
–2·4 –2·9 to –1·8) |
| Bangladesh | 21 789 (18 195 to 25 380) |
16 597 (13 124 to 20 017) |
7663 (5584 to 10 226) |
581·7 (485·8 to 676·7) |
457·6 (362·0 to 551·3) |
244·5 (178·4 to 325·8) |
–2·4 (–4·6 to –0·3) |
–4·3 (–6·5 to –1·7) |
–3·5 (–4·8 to –2·1) |
| Bhutan | 96 (61 to 132) |
54 (36 to 76) |
31 (19 to 48) |
490·9 (312·6 to 673·8) |
346·7 (231·4 to 485·9) |
230·3 (138·0 to 354·0) |
–3·5 (–7·0 to 0·1) |
–2·8 (–6·0 to 0·5) |
–3·1 (–5·2 to –0·7) |
| India | 132 239 (120 991 to 144 659) |
116 206 (106 519 to 127 563) |
63 861 (55 155 to 77 388) |
482·1 (441·1 to 526·9) |
416·7 (382·1 to 457·3) |
247·6 (214·0 to 299·9) |
–1·4 (–2·3 to –0·6) |
–3·5 (–4·5 to –2·3) |
–2·7 (–3·3 to –1·9) |
| Nepal | 3846 (2663 to 4994) |
2630 (1 926 to 3 360) |
1856 (1170 to 2725) |
528·9 (366·2 to 686·0) |
345·8 (253·5 to 441·7) |
321·6 (203·1 to 472·0) |
–4·3 (–7·2 to –0·8) |
–0·5 (–3·3 to 2·0) |
–2·0 (–4·0 to 0·0) |
| Pakistan | 16 973 (13 060 to 21 189) |
22 038 (17 789 to 26 598) |
19 005 (14 012 to 24 369) |
391·5 (301·3 to 488·4) |
498·9 (404·1 to 601·7) |
348·6 (257·2 to 447·0) |
2·4 (–0·3 to 5·5) |
–2·4 (–4·7 to –0·3) |
–0·5 (–1·9 to 0·9) |
| Sub-Saharan Africa | 107 200 (91 543 to 125 722) |
136 629 (120 361 to 154 268) |
133 043 (106 996 to 168 218) |
495·2 (422·9 to 580·5) |
510·0 (449·6 to 575·7) |
374·9 (301·8 to 473·1) |
0·3 (–1·4 to 2·0) |
–2·1 (–3·6 to –0·4) |
–1·1 (–2·2 to 0·0) |
| Southern Sub-Saharan Africa | 2720 (2306 to 3138) |
3855 (3091 to 5155) |
3964 (2738 to 6233) |
170·4 (144·5 to 196·6) |
230·5 (184·9 to 307·8) |
211·3 (146·0 to 332·3) |
2·8 (0·6 to 6·0) |
–0·7 (–3·4 to 2·4) |
0·7 (–0·6 to 2·6) |
| Botswana | 74 (18 to 220) |
193 (35 to 815) |
118 (28 to 532) |
156·3 (38·6 to 458·5) |
406·0 (73·1 to 1709·9) |
211·9 (50·8 to 951·3) |
5·9 (–7·7 to 22·5) |
–3·2 (–16·9 to 10·0) |
0·3 (–6·1 to 8·2) |
| Lesotho | 113 (58 to 176) |
174 (109 to 289) |
301 (121 to 757) |
200·0 (102·4 to 310·3) |
299·6 (187·9 to 495·0) |
495·4 (199·4 to 1246·4) |
3·8 (−0·8 to 10·8) |
2·2 (−3·3 to 9·7) |
3·0 (−0·4 to 7·8) |
| Namibia | 102 (69 to 140) |
187 (108 to 280) |
74 (34 to 174) |
190·8 (128·1 to 260·8) |
316·0 (182·6 to 472·6) |
102·4 (47·1 to 240·8) |
5·0 (−1·3 to 10·7) |
−8·2* (−13·3 to −1·4) |
−3·3 (−5·1 to 1·0) |
| South Africa | 1558 (1318 to 1822) |
1611 (1307 to 1901) |
1754 (1396 to 2247) |
153·8 (130·1 to 179·8) |
151·5 (123·0 to 178·8) |
157·9 (125·7 to 202·1) |
−0·2 (−2·6 to 2·1) |
0·3 (−1·3 to 1·8) |
0·1 (−0·9 to 1·2) |
| Swaziland | 46 (24 to 78) |
48 (30 to 87) |
73 (22 to 216) |
124·7 (65·5 to 212·5) |
140·2 (86·8 to 253·9) |
194·2 (57·6 to 569·7) |
0·9 (−6·2 to 9·4) |
0·6 (−6·0 to 10·3) |
0·9 (−3·4 to 6·4) |
| Zimbabwe | 826 (612 to 1068) |
1641 (1131 to 2702) |
1 645 (742 to 3616) |
212·6 (157·6 to 274·5) |
400·4 (275·9 to 657·0) |
305·4 (137·8 to 668·5) |
5·8 (2·1 to 11·3) |
−2·3 (−8·4 to 4·1) |
1·1 (−1·8 to 4·7) |
| Western sub-Saharan Africa | 43 022 (32 030 to 56 910) |
56 537 (46 496 to 66 580) |
54 979 (40 856 to 81 866) |
482·9 (359·7 to 638·4) |
505·8 (416·2 to 595·5) |
362·9 (269·7 to 540·1) |
0·6 (−3·0 to 3·8) |
−2·5 (−4·4 to 0·5) |
−1·2 (−2·9 to 0·8) |
| Benin | 1223 (845 to 1682) |
1424 (917 to 1903) |
1667 (597 to 4004) |
523·8 (362·2 to 717·3) |
476·4 (307·2 to 635·6) |
429·7 (154·0 to 1025·8) |
−0·9 (−6·7 to 3·8) |
−1·3 (−8·2 to 5·2) |
−1·1 (−5·2 to 3·1) |
| Burkina Faso | 1639 (1206 to 2067) |
2320 (1526 to 3001) |
2523 (941 to 5007) |
391·5 (288·9 to 493·1) |
431·0 (284·0 to 557·4) |
351·8 (131·3 to 695·8) |
1·0 (−3·7 to 4·8) |
−1·5 (−7·9 to 4·1) |
−0·5 (−4·4 to 2·4) |
| Cameroon | 2421 (1793 to 2970) |
3659 (2321 to 4852) |
4 137 (1605 to 9156) |
448·5 (335·8 to 550·0) |
556·5 (353·2 to 736·3) |
488·5 (189·6 to 1076·6) |
2·2 (−2·3 to 5·8) |
−1·2 (−7·4 to 4·8) |
0·0 (−3·7 to 3·6) |
| Cape Verde | 13 (10 to 16) |
9 (6 to 14) |
6 (4 to 8) |
94·5 (74·7 to 116·8) |
72·1 (49·6 to 115·9) |
51·6 (38·7 to 72·1) |
−3·2 (−6·7 to 2·2) |
−2·0 (−6·0 to 1·3) |
−2·5 (−3·9 to −0·9) |
| Chad | 1451 (973 to 1917) |
2587 (1526 to 3442) |
3466 (1106 to 8614) |
477·1 (320·1 to 629·5) |
605·9 (357·4 to 805·4) |
549·9 (175·8 to 1363·7) |
2·4 (−3·2 to 7·4) |
−1·1 (−8·8 to 5·5) |
0·4 (−4·3 to 4·3) |
| Côte d’Ivoire | 2504 (1917 to 3074) |
4283 (2950 to 6081) |
4004 (1449 to 7867) |
477·5 (366·0 to 586·3) |
638·7 (441·1 to 904·7) |
477·6 (173·4 to 937·3) |
2·7 (−0·7 to 6·9) |
−2·2 (−8·8 to 3·1) |
−0·2 (−4·1 to 2·9) |
| The Gambia | 227 (71 to 487) |
257 (168 to 346) |
295 (153 to 539) |
526·0 (166·1 to 1129·6) |
459·6 (301·0 to 616·3) |
354·7 (184·6 to 647·2) |
−1·0 (−8·4 to 8·5) |
−2·1 (−6·7 to 3·1) |
−1·5 (−5·7 to 3·3) |
| Ghana | 2723 (1542 to 4447) |
3200 (2101 to 4410) |
2615 (1054 to 6187) |
476·2 (270·0 to 777·0) |
489·0 (323·4 to 671·9) |
296·0 (119·4 to 698·9) |
0·5 (−5·7 to 6·7) |
−4·2 (−10·2 to 2·6) |
−2·3 (−6·1 to 2·3) |
| Guinea | 2061 (1477 to 2571) |
2600 (1919 to 3 154) |
2779 (1120 to 4875) |
714·0 (512·3 to 890·1) |
690·1 (510·3 to 836·8) |
604·7 (244·2 to 1055·7) |
−0·3 (−3·9 to 3·2) |
−1·0 (−6·9 to 3·4) |
−0·8 (−4·2 to 1·8) |
| Guinea-Bissau | 244 (55 to 677) |
297 (63 to 857) |
403 (87 to 1492) |
508·6 (114·4 to 1393·1) |
552·7 (117·4 to 1588·7) |
595·4 (128·0 to 2190·7) |
0·4 (−11·1 to 11·4) |
0·2 (−9·8 to 9·2) |
0·0 (−6·4 to 7·3) |
| Liberia | 718 (396 to 1044) |
787 (500 to 1035) |
950 (417 to 1774) |
753·7 (416·3 to 1095·9) |
664·0 (423·2 to 873·1) |
607·6 (267·0 to 1122·2) |
−1·3 (−6·8 to 5·4) |
−0·9 (−6·3 to 4·5) |
−1·0 (−4·2 to 2·0) |
| Mali | 2476 (1975 to 2967) |
2792 (2061 to 3363) |
2 631 (1043 to 4600) |
593·6 (473·6 to 709·3) |
519·0 (383·2 to 624·9) |
347·3 (138·0 to 604·5) |
−1·3 (−4·5 to 1·6) |
−2·7 (−8·9 to 1·3) |
−2·1 (−5·9 to 0·3) |
| Mauritania | 643 (507 to 814) |
622 (319 to 806) |
575 (200 to 1110) |
778·8 (615·7 to 984·0) |
598·3 (307·0 to 775·0) |
428·2 (149·6 to 824·2) |
−2·4 (−8·6 to 0·7) |
−2·5 (−8·4 to 2·9) |
−2·5 (−6·5 to 0·5) |
| Niger | 1904 (1312 to 2619) |
2795 (1953 to 3731) |
3657 (1617 to 6310) |
434·2 (299·9 to 596·7) |
466·4 (326·0 to 622·4) |
372·0 (165·8 to 639·1) |
0·7 (−3·7 to 5·3) |
−1·5 (−7·1 to 2·8) |
−0·7 (−4·0 to 1·9) |
| Nigeria | 19 862 (9489 to 33 627) |
24 972 (16 262 to 33 862) |
20 321 (11 437 to 43 168) |
470·7 (225·4 to 796·4) |
472·0 (307·6 to 640·0) |
284·9 (160·4 to 604·6) |
0·5 (−6·9 to 7·9) |
−4·3 (−8·0 to 2·6) |
−2·3 (−5·7 to 2·5) |
| São Tomé and Príncipe | 10 (7 to 14) |
14 (11 to 19) |
10 (4 to 23) |
230·4 (157·1 to 317·5) |
268·5 (205·3 to 349·6) |
164·2 (65·0 to 367·5) |
1·6 (−2·4 to 6·0) |
−3·8 (−9·5 to 2·3) |
−1·7 (−5·4 to 2·0) |
| Senegal | 1532 (1097 to 1909) |
1919 (1301 to 2403) |
2577 (942 to 5912) |
467·5 (336·2 to 581·3) |
485·2 (329·4 to 606·7) |
454·3 (166·8 to 1035·3) |
0·4 (−4·4 to 4·7) |
−1·4 (−7·7 to 5·7) |
−0·7 (−4·4 to 3·4) |
| Sierra Leone | 655 (294 to 1270) |
1076 (775 to 1385) |
1 595 (737 to 2 820) |
369·6 (166·4 to 714·5) |
573·7 (413·8 to 738·8) |
695·7 (321·9 to 1229·1) |
5·2 (−3·2 to 12·4) |
1·2 (−4·4 to 5·7) |
2·8 (−1·3 to 6·3) |
| Togo | 713 (472 to 912) |
920 (542 to 1257) |
767 (321 to 1 454) |
443·3 (293·6 to 566·8) |
473·8 (279·5 to 643·3) |
298·9 (125·6 to 564·9) |
0·6 (−5·0 to 5·5) |
−3·3 (−9·4 to 2·1) |
−1·7 (−5·1 to 1·4) |
| Eastern sub-Saharan Africa | 49 401 (42 315 to 57 626) |
61 389 (52 635 to 71 472) |
50 443 (36 255 to 70 958) |
574·9 (493·0 to 670·4) |
582·0 (499·1 to 677·4) |
368·3 (265·6 to 517·0) |
0·1 (−1·6 to 1·7) |
−3·2 (−5·5 to -0·8) |
−1·9 (−3·2 to -0·4) |
| Burundi | 3110 (1408 to 5853) |
3032 (2062 to 4188) |
1915 (770 to 3 889) |
1119·1 (506·9 to 2103·0) |
1037·5 (706·6 to 1432·6) |
392·6 (158·4 to 789·8) |
−0·4 (−7·4 to 6·8) |
−7·1* (−12·9 to -0·5) |
−4·3 (−8·7 to 0·3) |
| Comoros | 103 (41 to 192) |
97 (72 to 126) |
56 (26 to 107) |
583·6 (232·2 to 1080·5) |
470·4 (352·1 to 611·3) |
213·3 (100·2 to 405·6) |
−1·8 (−8·3 to 7·2) |
−5·7* (−10·6 to -0·5) |
−4·0 (−7·9 to 0·0) |
| Djibouti | 86 (35 to 159) |
118 (43 to 283) |
107 (43 to 299) |
378·3 (154·4 to 698·7) |
523·8 (192·3 to 1247·0) |
486·2 (193·8 to 1353·5) |
2·8 (−9·8 to 15·3) |
−0·5 (−9·4 to 9·9) |
0·6 (−4·1 to 6·6) |
| Eritrea | 1073 (798 to 1452) |
848 (343 to 1608) |
1319 (345 to 3266) |
815·2 (606·2 to 1101·2) |
645·9 (262·8 to 1224·1) |
752·8 (197·4 to 1859·2) |
−3·1 (−10·8 to 4·3) |
0·5 (−6·5 to 7·0) |
−1·0 (−5·8 to 3·5) |
| Ethiopia | 18 283 (13 774 to 24 091) |
21 890 (16 330 to 28 474) |
13 017 (5497 to 28 519) |
796·7 (601·0 to 1049·6) |
752·4 (561·5 to 976·0) |
409·8 (173·2 to 892·0) |
−0·6 (−4·4 to 3·0) |
−4·6 (−10·1 to 1·3) |
−2·9 (−6·1 to 0·6) |
| Kenya | 3668 (2903 to 4614) |
6042 (4842 to 7574) |
5311 (4100 to 6758) |
371·4 (294·0 to 466·0) |
505·0 (404·9 to 632·9) |
338·0 (261·0 to 429·6) |
3·1 (0·9 to 5·3) |
−2·7 (−4·6 to -0·7) |
−0·4 (−1·6 to 0·8) |
| Madagascar | 1987 (1597 to 2359) |
2763 (1003 to 3733) |
2772 (929 to 6056) |
379·0 (304·8 to 449·9) |
426·5 (155·1 to 575·9) |
333·4 (112·3 to 727·4) |
1·4 (−7·7 to 4·6) |
−2·3 (−8·4 to 5·2) |
−0·9 (−4·9 to 2·7) |
| Malawi | 2268 (1659 to 2833) |
2939 (1952 to 4527) |
1462 (597 to 2932) |
508·4 (372·3 to 634·8) |
591·5 (392·9 to 908·9) |
219·7 (89·8 to 440·0) |
1·2 (−2·4 to 5·6) |
−6·8* (−12·5 to -1·7) |
−3·5 (−7·0 to -0·6) |
| Mozambique | 2187 (1469 to 2984) |
2837 (1622 to 3773) |
3 557 (1 274 to 8 671) |
347·6 (234·5 to 473·7) |
345·2 (199·4 to 458·2) |
327·2 (117·5 to 797·0) |
0·1 (−6·0 to 4·7) |
−1·0 (−8·0 to 6·2) |
−0·8 (−4·5 to 3·5) |
| Rwanda | 2142 (1578 to 2961) |
2411 (1861 to 3150) |
1353 (587 to 2878) |
666·9 (491·5 to 920·7) |
772·2 (596·1 to 1007·1) |
373·3 (161·9 to 791·7) |
1·4 (−2·2 to 5·1) |
−5·3 (−11·0 to 0·6) |
−2·5 (−6·2 to 1·0) |
| Somalia | 2509 (418 to 6 772) |
2899 (489 to 7449) |
3443 (661 to 10 512) |
830·5 (138·5 to 2193·9) |
811·0 (137·5 to 2077·9) |
731·1 (140·5 to 2218·6) |
−0·3 (−11·8 to 10·4) |
−0·8 (−8·6 to 8·8) |
−0·6 (−6·7 to 6·5) |
| South Sudan | 1565 (305 to 4258) |
1639 (318 to 4942) |
2868 (589 to 10 569) |
587·8 (114·7 to 1586·1) |
573·5 (111·5 to 1728·5) |
643·5 (132·4 to 2362·7) |
−0·5 (−11·2 to 10·9) |
0·4 (−9·0 to 10·8) |
0·1 (−6·9 to 7·3) |
| Tanzania | 6 139 (4654 to 7419) |
7139 (4932 to 9656) |
6974 (2670 to 17 367) |
544·3 (413·5 to 656·6) |
498·9 (345·0 to 673·7) |
337·8 (129·8 to 841·1) |
−1·0 (−4·8 to 3·0) |
−3·6 (−9·4 to 3·5) |
−2·5 (−5·8 to 1·6) |
| Uganda | 2923 (2051 to 3820) |
4714 (3426 to 6416) |
4664 (1746 to 10 115) |
337·4 (237·2 to 440·6) |
408·1 (297·0 to 554·5) |
280·1 (104·9 to 606·4) |
1·8 (−1·5 to 5·3) |
−2·9 (−9·4 to 3·0) |
−1·0 (−4·7 to 2·5) |
| Zambia | 1334 (1005 to 1682) |
1984 (1432 to 2809) |
1591 (654 to 3231) |
353·9 (267·1 to 446·1) |
424·3 (306·7 to 600·4) |
246·6 (101·7 to 499·3) |
1·7 (−1·6 to 5·6) |
−4·1 (−10·3 to 1·4) |
−1·8 (−5·2 to 1·6) |
| Central sub-Saharan Africa | 12 058 (7087 to 18 859) |
14 849 (9631 to 24 474) |
23 657 (12 760 to 41 319) |
474·1 (278·8 to 740·5) |
438·9 (284·8 to 721·4) |
497·4 (269·4 to 866·4) |
−0·7 (−5·5 to 4·1) |
0·8 (−3·6 to 4·7) |
0·1 (−2·5 to 2·9) |
| Angola | 4055 (783 to 10 270) |
5006 (897 to 14 417) |
5801 (1242 to 20 599) |
685·8 (133·2 to 1736·3) |
646·4 (115·8 to 1858·9) |
514·3 (110·7 to 1814·1) |
−1·0 (−12·2 to 10·3) |
−1·7 (−10·9 to 7·6) |
−1·8 (−7·5 to 5·6) |
| Central African Republic | 1083 (813 to 1 450) |
1496 (460 to 3 269) |
1763 (351 to 4693) |
893·5 (671·0 to 1195·7) |
1024·2 (314·9 to 2233·9) |
1074·3 (214·7 to 2856·6) |
0·2 (−9·7 to 9·3) |
−0·4 (−8·9 to 8·6) |
0·1 (−5·5 to 4·9) |
| Congo (Brazzaville) |
398 (233 to 650) |
769 (501 to 1118) |
808 (302 to 1707) |
436·0 (255·7 to 709·2) |
638·0 (416·0 to 926·3) |
484·3 (181·6 to 1021·1) |
3·9 (−1·7 to 9·7) |
−2·4 (−8·5 to 4·0) |
0·2 (−3·9 to 4·1) |
| Democratic Republic of the Congo | 6251 (2952 to 9699) |
7269 (5091 to 9430) |
15 067 (6764 to 26 513) |
370·7 (176·5 to 572·1) |
318·7 (223·6 to 413·1) |
468·4 (210·5 to 824·1) |
−1·5 (−7·4 to 5·7) |
2·4 (−3·0 to 6·9) |
0·8 (−2·5 to 4·5) |
| Equatorial Guinea | 161 (29 to 421) |
141 (26 to 439) |
120 (32 to 448) |
913·3 (166·0 to 2384·5) |
676·1 (125·9 to 2098·3) |
409·3 (108·2 to 1516·8) |
−3·6 (−15·9 to 7·3) |
−3·5 (−13·4 to 7·2) |
−4·2 (−9·6 to 3·9) |
| Gabon | 109 (80 to 149) |
167 (111 to 239) |
98 (43 to 197) |
309·2 (227·1 to 420·7) |
407·9 (274·5 to 584·7) |
191·4 (84·1 to 381·8) |
2·8 (−1·5 to 6·9) |
−5·5* (−11·2 to 0·6) |
−2·2 (−5·3 to 1·1) |
Data in parentheses are 95% UIs. *Shows locations that have met or exceeded the Milennium Development Goal 5 achievement rate of −5·5% during any time period.
Geographical differences in maternal mortality are readily apparent. In 1990, 60 countries had an MMR greater than 200, 40 countries had an MMR of greater than 400, and 15 greater than 600 (appendix pp 58–62). Only one country—Burundi—had an MMR greater than 1000. MMR was less than 70 in 93 countries at that time. A subset of 50 countries had an MMR of less than 30, and 28 countries were less than 15. By the year 2015, as shown in figure 4, 122 countries had an MMR of less than 70, and 49 countries had an MMR of less than 15, including Saudi Arabia, all countries in central Europe, and all high-income locations with the exception of the USA, Argentina, Brunei, Chile, and Uruguay. Several other countries in North Africa and Middle East along with the USA, Armenia, Azerbaijan, Bulgaria, Chile, China, Costa Rica, Kazakhstan, Puerto Rico, Romania, Russia, Tajikistan, Thailand, Turkmenistan, Ukraine, Uruguay, Uzbekistan, and Vietnam had an MMR between 15 and 30. Unfortunately, there were still 24 countries with an MMR of greater than 400, eight countries with greater than 600, and still one—Central African Republic—greater than 1000. Of those greater than 600, Sierra Leone, Afghanistan, and Central African Republic actually worsened, with ARC from 1990 to 2015 of 2·7% (–1·3 to 6·3), 0·34% (–2·1 to 2·7), and 0·08% (–5·5 to 4·9), respectively. Of those countries with an MMR higher than 400 in 1990, Burundi and Equatorial Guinea improved substantially by 2015 with total improvements of –4·3% (–8·7 to 0·3) and –4·2% (–9·6 to 3·9), respectively.
Figure 4. Maternal mortality ratio (MMR; number of deaths per 100 000 livebirths) for countries and territories, 2015.
The map is colour-coded according to the national MMR in the year 2015. Lowest MMR is shown in purple and highest in dark red. Inset images help to show smaller countries. ATG=Antigua. VCT=Saint Vincent and the Grenadines. Isl=Islands. FSM=Federated States of Micronesia. LCA=Saint Lucia. TTO=Trinidad and Tobago. TLS=Timor-Leste.
MDG 5 achievement
To achieve the primary objective of MDG 5, the ARC must have met or exceeded an average of –5·5% during the entire time period from 1990 to 2015. Based on this metric, a total of ten countries probably achieved MDG 5, including Iceland, Jordan, Maldives, Belarus, Morocco, Romania, China, Turkey, Poland, and Estonia. Several other countries achieved this rate of improvement at some point during the MDG period. From 2000 to 2015, 24 countries exceed ARC of –5·5%. Many countries, despite not achieving the ambitious MDG 5 target of a 75% reduction, actually have been experiencing steady declines in maternal mortality for quite some time. 148 of 195 countries and territories saw their peak MMR occur before the year 2000, with an additional 21 occurring by the year 2005. Maternal mortality increased in 26 countries between 1990 and 2015.
Relation between MMR, SDI, and reproductive health services
As shown in table 2, maternal mortality in the lowest SDI quintile improved the least, with ARC of only –0·97% (–1·8 to –0·001) from 1990 to 2015, and the low-middle SDI quintile was the next slowest with an ARC of –2·1% (–2·8 to –1·1). The proportion of all maternal deaths occurring in the bottom two SDI quintiles increased from roughly 68% in 1990 to more than 80% in 2015. The middle SDI quintile improved the fastest with ARC of –3·2% (–3·8 to –2·6) over the entire time period. Figure 5 shows global and regional-level MMR and SDI from 1990 to 2015. The black convex line represents the average relation between MMR and SDI over the time period and is the basis of expected MMR. Each coloured symbol represents a successive year from 1990 to 2015 for the global level and GBD regions. Globally, MMR in 2015 was more than double what would have been predicted solely by average SDI. This was following a period from 1990 to 2000 where global MMR improved more slowly than would have been expected based on SDI improvement and a period of faster-than-expected MMR improvement from 2000 to 2015. Based on the expected relation between MMR and SDI, reaching the SDG 3.1 achievement threshold of MMR 70 would require an SDI of 0·65, corresponding to an average income of roughly international $9442 per capita, 8·2 years of education, and total fertility rate of 2·5. Not all countries might be able to achieve that level of income, however, but education and fertility reduction efforts could still be compatible with reaching this SDI level. If all women were to complete a full 12 years of education and total fertility rate of 2·7, an SDI of 0·65 would on average be associated with income of $3214 per capita. If total fertility rate were to decrease further to the population replacement rate of to 2·0 and education were 12 years, this SDI level would only require an annual income of $2648 per capita.
Table 2. Average coverage of reproductive health services between including one visit of antenatal care (ANC), four ANC visits, in-facility delivery, and skilled birth attendance by MMR strata, all years from 1990 to 2015 combined.
| Antenatal care (1 visit) coverage | Antenatal care (4 visits) coverage | In-facility delivery | Skilled birth attendance | |
|---|---|---|---|---|
| 0 to 15 | 97·7% | 95·0% | 97·2% | 98·5% |
| 15 to 65 | 94·4% | 87·0% | 92·3% | 95·0% |
| 65 to 75 | 90·9% | 77·5% | 82·2% | 88·5% |
| 75 to 175 | 85·9% | 65·4% | 71·7% | 79·6% |
| 175 to 225 | 84·8% | 61·0% | 63·6% | 69·6% |
| 225 to 500 | 79·7% | 48·4% | 49·1% | 56·8% |
| 500 and above | 74·7% | 43·6% | 40·0% | 47·4% |
The coverage values for each aspect of reproductive care show the simple average of all observation for all location-years within the corresponding MMR range.
Figure 5. Co-evolution of maternal mortality ratio (MMR; number of livebirths per 100 000 livebirths) with SDI globally and for GBD regions, 1990–2015.
Coloured lines show global and region values for MMR. Each point in a line represents one year starting at 1990 and ending at 2015. In all regions, SDI has increased over time so progress in SDI is associated with points further to the right and later years for a given region. The black lines indicate expected trajectories for each geography expected on the basis of SDI alone. SDI=Socio-demographic Index.
MMR and SDI both improved between 1990 and 2015 in almost all regions, but MMR did not universally track with SDI over the entire time period in any single region. East Asia has had the lowest O–E MMR ratio since 2011, a period in which it has consistently been less than 0·4 of expected. Australasia has also had consistently lower MMR than would be predicted on the basis of SDI, with O–E MMR ratio ranging from 0·54 in 1990 to 0·71 in 2015. In addition to east Asia and Australasia, several other regions have consistently had lower MMR than would have been expected by SDI, including central Asia, central Europe, eastern sub-Saharan Africa, Western Europe, and high-income Asia Pacific. Southern Latin America and north Africa and the Middle East both had lower than expected MMR in 1990 when both had O–E MMR ratios of less than 0·7, but improvement has not kept pace with SDI gains in either region: by 2015, O–E MMR ratios were 2·23 and 1·41, respectively. Central sub-Saharan Africa has been an exception in several ways. In addition to having the highest MMR of any region in 2015, MMR worsened from 1990 to 2015. Despite maternal mortality being high in central sub-Saharan Africa, it was still lower than would have been expected until 2014 because SDI is still so low in that region and has improved only slowly.
O–E MMR ratio has consistently been 1·25 or more in a larger number of regions, including the Caribbean, eastern Europe, high-income North America, Oceania, south Asia, southeast Asia, and southern sub-Saharan Africa. Andean Latin America had periods of rapid improvement in MMR during the early 2000s that exceeded that expected based on SDI. Unfortunately, MMR reductions there have slowed substantially since then, to the point where O–E MMR ratio was 1·41 in 2015. Improvements in eastern Europe have been faster than SDI after the year 2000, but MMR improvement in the remaining regions has continued to be slower than expected on the basis of SDI. Southern sub-Saharan Africa and the Caribbean had the highest O–E MMR ratios of any regions at 3·57 and 3·71, respectively, in 2015, but both have had recent periods of MMR improvement that were much more rapid than expected on the basis of SDI. These trend reversals began in 2006 and 2007, respectively. South Asia and southeast Asia are unique in that although both have made major gains in terms of SDI and MMR, the difference between observed and expected MMR based on SDI remained the same.
Even within regions, the degree to which MMR diverged on the basis of SDI varied. For each country, we calculated observed ARC minus expected ARC (O–E ARC) on the basis of SDI change from 2000 to 2015 (figure 6). In 60 countries, the O–E ARC was faster than would have been expected based on SDI alone, and 25 of these had ARC at least 1·5% faster than expected. Within south Asia, Bangladesh has improved faster than expected, whereas Nepal, Bhutan, and India all had slower MMR reductions. Of the countries in southeast Asia, Cambodia and Laos have improved much faster than expected, whereas Thailand, Philippines, and Malaysia have not. In sub-Saharan Africa, Namibia, Malawi, and Burundi were all more than 1·5% faster than expected, but ARC in most of the countries of eastern and western sub-Saharan Africa exceeded SDI-based expectations. By contrast, only Gabon in central sub-Saharan Africa reduced MMR as rapidly as expected, with the Democratic Republic of the Congo and Equatorial Guinea both more than 3% slower. 93 countries had an O–E ARC of 1·5% or more, and there were 17 countries where O–E ARC was greater than 5%.
Figure 6. Difference between observed annualised rate of change (ARC) in maternal mortality ratio (MMR; number of deaths per 100 000 livebirths) and expected ARC on the basis of Socio-demographic Index (SDI) alone from 2000 to 2015 for countries and territories.
The map displays the difference between the observed average annual rate of change in MMR and the average annual rate of change that would have been expected based on the change in each country and territory’s SDI from 2000 to 2015. Values below zero indicate faster than expected progress while those above zero indicate MMR has improved more slowly than expected. ATG=Antigua. VCT=Saint Vincent and the Grenadines. Isl=Islands. FSM=Federated States of Micronesia. LCA=Saint Lucia. TTO=Trinidad and Tobago. TLS=Timor-Leste.
To begin exploring the hypothesis that MMR improvements are related to coverage of specific modes of reproductive health care, we examined the relation between MMR and coverage of one visit of antenatal care, four antenatal care visits, in-facility delivery, and skilled birth attendance over the period from 1990 to 2015 (table 2). We found that, on average, countries with an MMR of less than 15 had 98% coverage of one antenatal care visit, 95% of four antenatal care visits, 97% of in-facility delivery, and 99% of skilled birth attendance. Those with an MMR of 70—the SDG 3.1 target for all countries—have roughly 91% coverage of one antenatal care visit, 78% of four antenatal care visits, 81% of in-facility delivery, and 87% of skilled birth attendance. This is by contrast with those countries with an MMR around 200 where there is an average of 84% coverage of one antenatal care visit, 61% of four antenatal care visits, 63% of in-facility delivery, and 70% of skilled birth attendance, and those locations with an MMR higher than 500 where coverage of all services was low, including just 76% coverage of one antenatal care visit, 45% of four antenatal care visits, 41% of in-facility delivery, and 48% of skilled birth attendance. Comparable datasets were not available to examine the relation between MMR and coverage of either EmOC, distance to obstetric care, post natal care coverage, or family planning services such as modern contraception and access to safe abortion services.
Age pattern of maternal mortality and fertility
The risk of maternal mortality increases greatly with age but decreased greatly in almost all age groups from 1990 to 2015 (appendix pp 63–295). Globally in 2015, MMR in 10–14 year olds girls was 278 (95% UI 229–339). MMR then decreased and was lowest in women from 15–29 years old before increasing substantially to 1832 (95% UI 1284–2746) in 50–54 year olds (not shown on graph). Although the largest number of births still occur among women between the ages of 20 years and 29 years (55% of total), adolescent fertility has decreased in and a net shift in births to older women has been noted (appendix pp 684–701). In 1990, 23·3 million (17% of total) livebirths occurred in those women aged younger than 20 years, and 0·58 million (0·42% of the total) were to girls aged 10–14 years. In 2015, 19·4 million (14% of total) births were in those aged 10–19 years, but there were still 0·48 million (0·34% of total) to girls younger than 15 years. By contrast, the absolute number of annual births to women aged 35 years and older increased from 16·1 million (12% of total) in 1990 to 18 million (13% of total) in 2015. ARC in MMR among 10–19 year olds from 2000 to 2015 was –2·3 (95% UI –3·3 to –1·2), which was slower than the global ARC in MMR for all ages combined.
Cause pattern of maternal mortality
Although the risk of death from all causes increases with age, most deaths still occur in younger women and the absolute numbers of deaths from all causes except HIV are higher in younger age groups (see appendix pp 296–98 for number of deaths in 1990, 2000, and 2015). Direct obstetric causes accounted for about 86% of all maternal deaths globally in 2015, led by maternal haemorrhage, maternal hypertensive disorders, and other maternal disorders. This number is down only slightly from 1990 when direct complications accounted for 87% of all maternal deaths. Other maternal disorders decreased with the most of all causes between 1990 and 2015, from 74 299 (95% UI 61 159–89 653) deaths in 1990, down to 32 734 (26 256–40 507) deaths in 2015. Maternal abortion, miscarriage, and ectopic pregnancy, and maternal sepsis and other maternal infections were the causes with the next largest declines between 1990 and 2015. Indirect maternal disorders increased in importance from 1990 when they caused 42 246 (95% UI 32 355–54 032) deaths (about 11% of total) to 2015 when they caused 33 108 (25 463–43 344) (about 12% of total). HIV-related maternal deaths were responsible for a portion of the increase in indirect maternal deaths, rising from 754 (95% UI 433–1095) globally in 1990, peaking in the year 2000, and coming down to 2322 (1394–3337) in 2015; this was 0·84% of overall maternal mortality in 2015. 2181 (95% UI 1306–3174) of HIV-related maternal deaths were in sub-Saharan Africa in 2015, roughly 1·6% of the total there. Overall, the contribution of HIV to overall maternal death was quite small, but a large number of women with HIV/AIDS are dying incidentally while pregnant or after delivering. If we include incidental HIV deaths during pregnancy from our population attributable fraction analysis, 20 180 (95% UI 12 120–29 005) HIV-positive women died while pregnant or post partum in 2015 (appendix pp 720–37 shows cause-specific maternal deaths for all GBD locations).
Changing cause pattern by age
The age pattern for underlying maternal mortality causes in 2015 (figure 7) shows that in the youngest age groups, maternal haemorrhage and maternal hypertensive disorders are the dominant causes, together accounting for more than 50% of all maternal deaths. Although the comparative risk associated with maternal hypertensive disorders decreases with age, haemorrhage actually peaked in importance in the 35–39 year olds. The contribution of most other causes of maternal death also increased with age, especially other direct maternal disorders and the combined category of abortion, ectopic pregnancy, and miscarriage. Late maternal deaths decreased steadily in importance from 1990, when 8460 (95% UI 5792–11 935) late maternal deaths occurred, to 2015, when 6711 (4335–9996) occurred, and still was the time period with the smallest absolute number of deaths (see appendix pp 738–69 for timing deaths). The antepartum and post-partum periods were the periods with the largest numbers of deaths in 2015 at 101 774 (95% UI 88 185–117 570) and 85 686 (72 956–101 862), respectively. The age pattern showed that the proportion of post-partum deaths peaked in the youngest age groups, whereas intrapartum and antepartum deaths were more important in those older than 35 years (appendix pp 299–302). If we look at the change in underlying causal patterns as predicted by SDI (figure 8), we see that in the lowest SDI geographies, maternal mortality is dominated by maternal haemorrhage. In high-SDI geographies, by contrast, the causal pattern changes substantially to one where other direct maternal disorders, indirect maternal disorders and abortion, ectopic pregnancy, and miscarriage are the most important causes of maternal death. In middle-SDI geographies, the epidemiological profile is even more complicated, with a particularly high proportion of maternal deaths being due to maternal hypertensive disorders.
Figure 7. Global proportion of total maternal deaths by underlying cause and age, 2015.
The stacked area graph shows the proportion of total maternal deaths due to each cause globally in 2015 as a function of female age group.
Figure 8. Expected relationship between cause-specific maternal mortality ratio (MMR; number of livebirths per 100 000 livebirths) and SDI (left) and proportion of maternal deaths due to each underlying cause and SDI (right).
These stacked curves represent the average relation between SDI and each cause of maternal mortality observed across all geographies over the time period 1990–2015. In each figure, the y axis goes from lowest SDI up to highest SDI. To the left of the midline are maternal mortality ratios (MMR; number of deaths per 100 000 livebirths), and the right-hand side shows the proportion of the total in order to highlight the different cause pattern in high SDI locations. SDI=Socio-demographic index.
Discussion
In summary, the overall change from 1990 to 2015 in global maternal deaths was roughly –29% and in MMR was –30%, both of which were well short of the MDG 5 goal of –75%. Global maternal deaths were largely unchanged from 1990 to 2000, decreasing only slightly from 390 185 (95% UI 365 193–416 235) in 1990 to 374 321 (351 336–400 419) in 2000. Progress in MMR during the 1990s was also virtually undetectable when global ARC was only 0·21% (–0·46 to 0·87). This was 4·1% slower than would have been expected on the basis of SDI alone. After the Millennium Declaration, maternal mortality improvements accelerated. In 2015, there were 275 288 (95% UI 243 757–315 490) maternal deaths, and average global ARC in MMR from 2000 to 2015 was –2·6% (–3·4 to –1·7), although even with acceleration progress was 1·8% slower than would have been expected on the basis of SDI improvements alone.
Only ten countries achieved MDG 5 based on this analysis: Iceland, Jordan, Maldives, Belarus, Morocco, Romania, China, Turkey, Poland, and Estonia. Although overall progress has been slow during the MDG era, recent accelerations mean there are an additional 24 countries where ARC has met or exceeded the MDG 5 achievement rate between 2000 and 2015. There was significant variability in MMR throughout the world in 2015, ranging from a low of 0·8 (95% UI 0·6–0·9) in Iceland to a high of 1074 (215–2857) in Central African Republic. 122 of 195 countries had MMR in 2015 that is already less than the SDG 3·1 goal of 70.
Impediments to MMR reduction are multifaceted and variable; many are also well-conceptualised through the lens of our SDI analysis. First, slow improvement in the two lowest SDI quintiles is one of the primary reasons that maternal mortality reduction has been slower than expected at the global level. In 1990, these two quintiles collectively accounted for 68% of maternal mortality, but by 2015, increased to more than 80% of the global total. Part of the reason is that high adolescent fertility rates in these locations, coupled with comparatively slow improvement in adolescent MMR, led to concentration of maternal mortality burden in young women and girls and higher total fertility in these populations. Second, some middle SDI locations might be experiencing a period of inertia where progress is stalling because health systems have not evolved to meet the challenge of identifying and managing high-risk pregnancies and efficiently responding to rapid clinical deterioration. Middle SDI geographies have historically had a higher proportion of cases due to conditions such as hypertensive disorders of pregnancy and other direct maternal disorders (eg, cardiomyopathy and embolism). Maternal haemorrhage also evolves with increasing SDI because, as increased in-facility delivery and skilled birth attendance lead to near universal active management of the third stage of labour, an increasing proportion of remaining haemorrhage cases—especially those that result in death—will be due to intractable uterine atony or placental disorders, both of which require high levels of performance and responsiveness from horizontally integrated health systems.38 This treatise is supported by the observation that many of the countries or regions that improved more rapidly than would have been expected after 2000 were also the biggest recipients of Development Assistance for Health,39 funds that are often directed toward strengthening health systems, while many of those that have improved more slowly than expected have suffered from epidemics, natural disasters, and armed conflicts that impair the function of health systems and the willingness or ability of women to seek care. Third, within any given region, heterogeneous or slower-than-expected MMR improvements might be related to uneven ramp-up of coverage for specific method of reproductive health care— antenatal care, in-facility delivery, skilled birth attendance, family planning services, EmOC, and post natal care—that are all known to decrease the risk of bad pregnancy outcomes.40,41 Indeed, increasing use of reproductive health services was one of the driving factors behind establishment of the Janani Suraksha Yojana conditional cash transfer programme in India. Janani Suraksha Yojana has been successful at increasing reproductive health-care services, but even despite its popularity this programme has not been as effective at reaching poor rural women, the sociodemographic group that is already at highest risk of adverse pregnancy outcomes.42 In addition to the Janani Suraksha Yojana programme in India, other countries such as Nepal, Mexico, El Salvador, Honduras, Guatemala, Uruguay, and Brazil have also had success in encouraging use of reproductive care services,43,44 so this might be a viable option for countries seeking to increase women’s use of reproductive health-care services. Fourth, the highest SDI geographies are likely also experiencing a confluence of factors leading to higher-risk pregnancies and subsequently higher than expected MMR—namely, delay of fertility to older ages and a corresponding increase in the proportion of pregnant women with non-communicable diseases (NCDs). Other direct maternal disorders are the dominant cause of maternal death in high SDI locations, driven by cardiomyopathy and obstetric embolism, both of which are of higher risk in older women and those with preexisting conditions such as hypertension, obesity, and diabetes.45,46 If the trend of increasing NCDs continues and, barring any breakthrough in preventing such complications, we could reasonably expect to see MMR increases begin to emerge in other regions besides those in the highest SDI.
Because of the importance of reproductive care coverage in overall reproductive health, and to help to guide specific coverage targets for achieving SDG 3.1 and 3.7, comparable metrics and monitoring on coverage of all of these reproductive health services should be integrated into regular progress reports at the global, regional, national, and subnational levels, including the development of comprehensive strategies to reach those targets. Our analysis found that an MMR of 70 is expected with an SDI level of 0·65, which corresponds to an average income of international $2648 per capita, a total fertility rate of 2·0, and completing 12 years of education, so even lower income countries might have a path to SDG 3.1 attainment. An MMR of 70 is also associated with about 91% coverage of one antenatal care visit, 78% of four antenatal care visits, 81% of in-facility delivery, and 87% of skilled birth attendance. Higher MMR locations have historically had much lower coverage of these services, particularly in-facility delivery and skilled birth attendance, and increasing access to them will require sustained focus.
Quality of care must also be a focus as coverage of family planning services, antenatal care, in-facility delivery, skilled birth attendance, EmOC, and postnatal care increase, because the existence of these programmes by themselves is not sufficient to ensure that women are receiving the care they need during pregnancy and the post-partum period.47 Care should be integrated and not be focused on single vertical interventions.48 Family planning services should be longitudinal and include provision of comprehensive sex education, multiple methods of modern contraception, and access to safe abortion.49 High-quality antenatal care should reflect appropriate use of services, good communication between patient and provider, and reliable screening and treatment for infectious diseases (eg, sexually transmitted infections), chronic conditions (eg, blood disorders, obesity, substance abuse, renal dysfunction, rheumatic, or other heart disease) and pregnancy abnormalities (eg, anaemia, nutritional deficiencies, blood pressure, glucose, urine protein, fetal growth anomalies).50,51 In-facility delivery and skilled birth attendance services must be adequately staffed to meet demand and, because not all major complications of pregnancy are avoidable or easily predictable, women need to have ready access to well-functioning basic and comprehensive EmOC services. These services must be appropriately distributed to meet demand52 and be staffed by sufficient numbers of trained midwives, nurses, and anaesthesia and obstetrical providers to meet demand, including on nights and weekends. Health professionals in EmOC facilities also need to have appropriate equipment including medications, access to blood transfusion materials, and intensive care services to help to prevent complications from leading to death.53,54 Post natal care should focus on detection and treatment of those conditions known to be more common in the post-partum and late maternal period, including cardiomyopathy, pulmonary embolism, and renal complications.55,56 In countries with generalised HIV epidemics, AIDS-related deaths have also been observed to commonly occur 42 days or more after pregnancy ends, and care efforts for HIV-positive mothers should focus on ensuring uninterrupted antiretroviral treatment.57,58
Late maternal death statistics need to be improved. Maternal mortality surveillance studies such as confidential enquiry have showed that late maternal death is non-trivial in even low-resource settings34,59 and can account for up to 40% of maternal deaths in high-income settings.60 A contemporary linkage study in Mexico found that 18% of maternal deaths are missed when the definition is truncated at 42 days’ post partum.61 As immediate mortality continues to decrease as a result of improved antenatal, obstetric, and post-partum care, it is therefore increasingly likely that the proportion of late maternal deaths will continue to increase. Despite knowledge of its importance, only a few countries using ICD-10 reliably code late maternal deaths. This is especially egregious because many of the same countries who have completed multiple confidential enquiries also have not recorded a single late maternal death in their official statistics. Denmark, Ireland, Finland, and the UK all fall into this category. Australia, France, and South Africa likewise completed multiple confidential enquiries and have recorded a total of eight maternal deaths combined in the entirety of their official statistics. This is the exact inverse of the USA where no nationally comprehensive confidential enquiries have been completed (although some states have established maternal mortality review boards). The USA has high MMR for a high-SDI country—and is one of the few where it is increasing—but following the lead of Mexico and much of Latin America, it is also one of the only countries that has proactively improved its civil registration system with addition of a pregnancy checkbox on the standard death certificate,62 so it is possible that at least a portion of the increase is related to enhanced case ascertainment.62 The USA should learn from the experiences of other countries and consider implementing regular, comprehensive confidential enquiries into drivers of maternal mortality. Other countries and subnational locations should follow the lead of the countries of the Americas by adding pregnancy checkboxes to their official death certificates and also ensuring that cooperation between their national statistics office and confidential enquiries committees maximises data quality.
WHO also recently published a set of maternal mortality estimates for 1990 to 201563,64 as part of its collaboration with the UN Maternal Mortality Estimation Inter-Agency Group (MMEIG). MMEIG 2015 global results again show a steep decline in maternal mortality from 1995 to 2005, and some deceleration in the period 2005–15 when maternal and newborn health Development Assistance for Health increased rapidly. GBD 2015 shows relatively little progress in the 1990s, but acceleration in MMR declines particularly after 2005. We have previously discussed some of the important differences between the analytical approaches used by GBD and MMEIG.65 These included differences in dataset content, data processing methods, all-cause mortality, model specification, quantification of uncertainty, the use of CoDCorrect to ensure consistency between all specific causes of death, and the fact that MMEIG 2013 combined three separate estimation methods for different categories of countries, whereas GBD uses one approach for all countries.
MMEIG has made some important modifications to their analysis since 2013—most notably implementation of a Bayesian approach that combines all countries into a single model to estimate maternal mortality cause fractions (the proportion of all deaths in the population that are due to maternal causes). These changes are especially apparent in estimates for a number of countries, including Bosnia and Herzegovina, Cyprus, Estonia, Finland, Georgia, Kiribati, Latvia, Malaysia, Mongolia, Romania, Russia, South Korea, and Sri Lanka. Figures comparing MMEIG 2015 and GBD 2015 data inputs and results for each country are contained in the appendix. The correlation in MMR between MMEIG 2015 and GBD 2015 estimates is now 0·85 over the entire time period from 1990 to 2015; this compares to a correlation in MMR between GBD 2013 and MMEIG 2013 of 0·77. If we limit the comparison to 2005 to 2015, correlation in MMR increases to 0·89.
Figure 9 compares the country-specific trends from 1990 to 2015 between the two analyses. Whereas GBD 2015 identified only ten countries as likely having achieved MDG 5, MMEIG 2015 found a total of 18 achieved the MDG 5 target. Because both groups use the same set of livebirths estimates from the UN Population Division, with the exception that GBD 2015 estimated maternal mortality for the entire age range from 10–54 years, differences in fertility are unlikely to be a major driver of differences between the two results. Drivers of differences can thus be best summarised as being due to differences in maternal cause fraction estimates or differences in all-cause mortality numbers as shown in the appendix (pp 499–518).
Figure 9. Comparison of annualised rate of change (ARC) in maternal mortality ratio (MMR; number of deaths per 100 000 livebirths) from GBD 2015 and MMEIG 2015 for all countries included in both analyses, 1990–2015.
This scatterplot shows the net difference in average annualised rate of change (ARC) in maternal mortality ratio (MMR; number of deaths per 100 000 livebirths) estimates between GBD 2015 and MMEIG 2015 over the entire time period from 1990 to 2015. MMEIG 2015 average ARC results are shown on the y-axis and GBD 2015 average ARC are shown on the x-axis. Points are colour-coded according to GBD super region. All countries under the horizontal dotted line were estimated by MMEIG to have achieved Millennium Development Goal (MDG) 5. Those to the left of the dotted line were estimated to have achieved MDG 5 by GBD 2015. UN Maternal Mortality Estimation Inter-agency Group. AFG=Afghanistan. BHS=The Bahamas. BLR=Belarus. BTN=Bhutan. BWA=Botswana. CAN=Canada. CHN=China. CMR=Cameroon. COD=Democratic Republic of the Congo. COG=Congo (Brazzaville). CPV=Cape Verde. DJI=Djibouti. EST=Estonia. FJI=Fiji. GUY=Guyana. IRN=Iran. ISL=Iceland. JAM=Jamaica. JOR=Jordan. KAZ=Kazakhstan. KHM=Cambodia. LAO=Laos. LBN=Lebanon. LBY=Libya. LSO=Lesotho. LUX=Luxembourg. MAR=Morocco. MDV=Maldives. MNG=Mongolia. POL=Poland. PRK=North Korea. ROU=Romania. RWA=Rwanda. SAU=Saudi Arabia. SLE=Sierra Leone. SRB=Serbia. SSD=South Sudan. SUR=Suriname. SWZ=Swaziland. TCD=Chad. TUR=Turkey. TLS=Timor-Leste. TON=Tonga. ZAF=South Africa. ZWE=Zimbabwe.
Global MMR estimates in 1990 were much higher in the MMEIG 2015 analysis, driven largely by higher estimates of maternal cause fraction in sub-Saharan Africa, south Asia, central Asia, central Latin America, and north Africa and the Middle East. 2015 MMEIG all-cause mortality estimates for 1990 were also higher in many of these same regions as well as in tropical and Andean Latin America, all of which led to higher MMR estimates than those produced by GBD 2015. Of note, GBD 2015 maternal cause fraction estimates were higher in most high-income regions, central Europe, and Oceania. By contrast, our decomposition of the drivers of differences in 2015 estimates show that differences in maternal cause fraction and all-cause mortality estimates narrowed in south Asia, central Asia, and much of sub-Saharan Africa, which has on aggregate led to broad agreement in global MMR figures for 2015. GBD 2015 estimates of maternal cause fraction estimates remain notably higher in high-income North America, western Europe, and Oceania, although it is likely that much of this is driven by MMEIG 2015 exclusion of late maternal mortality.
The total number of sources used by MMEIG 2015 was 203 and by GBD 2015 was 599 (appendix pp 677–83 shows all country-specific sources by type used in each analysis). For a number of populous countries—including China, Ethiopia, Indonesia, and India—differences in maternal cause fraction estimates are largely driven by dataset content. MMEIG 2015 did not include data from Medical Certification of Cause of Death66 or the Survey of Causes of Death67 from India, several years of census and verbal autopsy data from Indonesia and Ethiopia, and maternal mortality surveillance data from China. MMEIG 2015 similarly did not include vital registration data from Iran and the Dominican Republic or sibling history from Jordan, all of which led to very different estimates of levels and trends of maternal mortality in those countries. In total, 396 sources were excluded by MMEIG 2015. In many cases the MMEIG 2015 documentation does not describe reasons for not including these data. In future iterations of both the GBD and MMEIG estimation, the groups should both work more closely to ensure relevant data sources are included in both analyses.
Differences in processing methods of sibling history data are important, especially for countries in sub-Saharan Africa. The nine countries without maternal mortality data in the GBD 2015 analysis were Andorra, Angola, Equatorial Guinea, the Federated States of Micronesia, Marshall Islands, Samoa, Solomon Islands, Somalia, and Vanuatu. MMEIG 2015 had no data for 23 GBD 2015 countries or territories, including Angola, Djibouti, Federated States of Micronesia, Guinea Bissau, North Korea, Palestine, Papua New Guinea, Samoa, Solomon Islands, Somalia, Tonga, and Vanuatu. They did not generate estimates for American Samoa, Andorra, nd Barbuda, Bermuda, Dominica, Greenland, Guam, Marshall Islands, Seychelles, Taiwan, and the Virgin Islands.
GBD 2015 used single-year sibling history survival data from each source, applied Gakidou-King weights to adjust for survivor bias, corrected for incidental HIV deaths using country-year-age-specific information about the population attributable fraction of HIV to maternal death, and used Bayesian noise-reduction algorithms to help to reduce stochastic variability in data. On aggregate, this approach maximises capture of underlying information about levels and trends of pregnancy-related mortality in health surveys. MMEIG 2015 combined all data from each survey and assigned them to the midpoint year of the recall period. They then uniformly applied a correction factor to reduce every datum by 10% or 15%, depending on the geography. The resulting MMEIG dataset is fairly sparse in some locations, and estimates are driven by regression coefficients. Examples can be seen in Democratic Republic of the Congo, Ethiopia, Ghana, and Saudi Arabia (see appendix pp 303–498). We would encourage MMEIG to consider using single-year sibling history data in their future analyses, because this difference in data processing might be driving divergence in trends from the early part of the MDG period, especially in sub-Saharan Africa.
Another important dataset difference is in the method used for processing and adjustment of vital registration data. GBD uses a standardised approach for all causes of death, empirically analysing every location’s single-year vital registration quality to guide dynamic adjustments to raw data (appendix pp 519–652). In past studies, MMEIG applied a default correction factor of 1·5 to all vital registration data. That method was modified in two ways in 2015. First, correction factors for vital registration were adjusted to match the deaths in published surveillance studies for those countries that had completed them. Second, MMEIG 2015 reclassified selected recent years of vital registration data as special studies. These reclassified years were not subjected to the 1·5 correction factor, but earlier years were. This reclassification resulted in estimates showing faster declines in the MMR than are supported by raw data. These eight countries where the MMEIG results are affected by the selective vital registration reclassification are Brazil, Costa Rica, Cuba, Ecuador, Guatemala, Kazakhstan, Mexico, and Uruguay. The criteria used for reclassification of vital registration as special studies are not clearly documented, and it is unclear if these criteria have been objectively applied to all country-years of vital registration.
MMEIG implemented a Bayesian approach to estimate maternal mortality for the first time in their 2015 estimates, which substantially improved their model fit in countries with long time series of data. However, the base MMEIG model still relied on a simple linear mixed-effects model with only three covariates—gross domestic product, general fertility rate, and skilled birth attendance—and country random effects. By contrast, the GBD 2015 used four families of statistical models and used 15 different covariates to develop ensemble models that were chosen based on a robust out-of-sample validity testing. MMEIG models were developed for the aggregate age range of 15–49 years, while the GBD 2015 estimates were generated separately for nine different 5-year age bands ranging from 10–54 years. The latter approach has the noted advantage of being able to automatically adjust for compositional bias if the age structure of the sample population is different from the general population. This approach also facilitates insight into potentially divergent age trends in maternal mortality within individual populations, matching them with corresponding shifts in age-specific fertility. Such an approach is crucial to singling out—for example—the contribution of adolescent fertility to overall maternal mortality levels and trends in maternal mortality. We therefore believe age-specific maternal mortality estimates, covering the entire reproductive age range, should be standard practice.
While recognising the potential caveats of adult mortality rates estimated using sibling survival, we made important improvements in GBD 2015 in accounting for selection bias and recall bias. We incorporated the uncertainty around adult mortality rate into our all-cause mortality estimation process for countries affected by HIV/AIDS in the sub-Saharan Africa regions. We did this by using single-year data for adult mortality rate from sibling survival modules—instead of pooled data for 5-year periods—and the crude death rate due to HIV/AIDS into the space-time Gaussian process regression that generates adult mortality rate estimates. This approach helped to reconcile between all-cause mortality estimates based on demographic sources and the HIV-specific mortality estimates using EPP-Spectrum, thus allowing us to better capture levels and trends of mortality in adult women, especially in western and central sub-Saharan Africa. By contrast, mortality estimates from World Population Prospects 2015 do not incorporate all available data, do not explicitly reconcile HIV-related and background mortality estimates, and for many countries are largely based on a tabular model life table system derived from that age pattern of mortality from countries in the 1950s and 1960s and a single entry parameter, the under-5 mortality rate. Such a system is likely to misrepresent the changing relation between mortality in child age groups and adult age groups68 and, as we see from World Population Prospects 2015, all-cause mortality estimates in the 1990s, might overestimate mortality in western and central sub-Saharan Africa.69
The GBD approach to quantification of uncertainty assumes that uncertainty is uncorrelated in all locations. MMEIG has in the past assumed uncertainty is 50% correlated and 50% uncorrelated. This approach has led to very large uncertainty intervals in many countries and at the global level in past reports. MMEIG 2015 has implemented a more rigorous statistical approach to estimate uncertainty but has chosen the non-standard step of reporting only 80% UIs, despite the general global health practice of reporting 95% UIs. The rationale provided for this decision was that 95% UIs cannot be reliably interpreted, although why 80% intervals are more interpretable is unclear. In the interests of transparency and comparability to other analyses such as the GBD, we hope that in future estimates MMEIG will provide 95% UIs along with other narrower intervals.
This analysis, like many before it, has a number of limitations. First, despite continued increase in the size and breadth of our data sources, we still have no data for maternal mortality from several countries and territories. In several other locations, especially low-SDI regions, we continue to rely on data reporting aggregate pregnancy-related deaths from surveys and censuses. Unlike verbal autopsy and vital registration sources, survey and census data sources do not differentiate between maternal and non-maternal (incidental) deaths during pregnancy. The degree to which underreporting due to survival and recall bias offsets overreporting due to inclusion of incidental deaths is unclear and is further reason to advocate for improved data collection efforts. Second, although we report results on the entire period from 1990 to 2015, because of large lag times in release of data we have not been able to include any data from 2015 and data from only 13 countries from 2014. Final 2015 results are thus based on recent historical data and model results. Third, our CODEm models have limited ability to capture non-stochastic rapid increases and decreases that might occur as a result of epidemics such as Ebola virus and H1N1 influenza,70,71 armed conflicts,72 or other events. Fourth, this report has examined nine specific causal categories of maternal death, but this classification system is certainly not exhaustive. We have not evaluated the contributions of some important chronic conditions known to increase risk to pregnant women such as obesity, diabetes, heart disease, haemoglobinopathies, such as sickle cell disease, chronic kidney disease, and chronic hypertension, or specific risk factors that might contribute to mortality. Our evaluation of ectopic pregnancy, abortion, and miscarriage together limits the ability to specifically quantify the burden of unsafe abortion. We likewise have not disaggregated the other direct obstetric complications category to quantify the relative importance of anaesthesia complications, cardiomyopathy, and pulmonary embolism, all of which are known to be important contributors to maternal mortality in many settings. Continuing to improve on the specificity of our analysis of the underlying cause of maternal death will be expected to improve the clinical use of GBD estimates. Fifth, while the GBD approach has the ability to provide excellent detail on geographic and temporal trends in maternal mortality, it has limited ability to explore subpopulations that are not geographically based, including indigenous populations or other high-risk groups who might have higher MMR due to cultural, religious, or other differences.
In conclusion, a shift from a relative target of percent reduction in MDGs to an absolute threshold target of an MMR of 70 in the SDGs has important ramifications. It will emphasise countries with high maternal mortality rates over those that have already achieved the goal. Such emphasis might be beneficial in that it should help to focus additional international attention and resources on those countries who have the farthest distance to go. On the other hand, pre-emptive so-called achievement of SDG 3·1 has the potential to sap political and financial investment in reproductive health in countries that still have major numbers of preventable maternal deaths, especially when continued progress is likely to depend largely on improvements in overall health systems performance.73–77 One approach to mitigate this risk would be to promote SDG 3.1 not only as a threshold goal for nations on aggregate, but also as a target for all subpopulations within each. This approach will require all stakeholders to make disaggregated data and information about women’s, children’s, and adolescents’ health publicly available.5 Furthermore, as the global community pursues SDG 3.1, monitoring and reporting on all aspects of reproductive health care as outlined in SDG 3.7 will be important.5 Achievement of this will require the international community to pay heed to the intricately related issues of immigration, armed conflicts, epidemics and pandemics, environment, economic instability, and gender equality, all of which can have substantial effects on the availability and quality of reproductive health services and women’s willingness to seek them.
Global progress in reducing maternal mortality has been accelerating in the past 15 years, but there is still major work left to do. More than 250 000 women died during or following pregnancy in 2015, most of which were preventable deaths. Every woman that died left children, widowers, family, and their communities behind. The quantitative effect of MDG 5 is difficult to measure, but it is even harder to dispute the notion that it has united the international community in striving to decrease maternal mortality. With the ratification of SDG 3.1 and SDG 3.7, relevant stakeholders need to make informed decisions about how to prioritise actions needed to bring about continued progress, and they can only do that with better data. As we continue on the path toward 2030, necessary and urgent steps will include rapid improvement in cause of death data collection systems and data dissemination coupled with more effective and widespread action and policies to promote education of girls and women, provide them with comprehensive family planning services, and ensure that each and every woman has access to the types of reproductive care they need to survive—and thrive.
Supplementary Material
Research in context.
Evidence before this study
Published in 2012, GBD 2010 presented results for 187 countries with a population greater than 50 000 in the year 2000. Collaborative teams completed subnational assessments for the UK, Mexico, and China for GBD 2013, expanding the number of geographies in the GBD analysis to 296. The value of subnational assessments to local decision makers has led to expansion of subnational analyses in GBD 2015 to also include Brazil, India, Japan, Kenya, Saudi Arabia, South Africa, Sweden, and the USA. Several previous analyses, including several completed as part of the Global Burden of Diseases, Injuries, and Risk Factors (GBD) Collaboration, have sought to provide the best possible information about levels and trends in maternal mortality. In dual recognition of both the importance and difficulty of accurately reporting on maternal mortality in many settings, each has incorporated increasingly large and geographically precise datasets and used more advanced statistical models. In their latest iteration, the WHO methods have also now adopted a single model for all countries and computed statistical uncertainty intervals. Important differences remain, however, that at times paint divergent pictures of levels and trends in maternal mortality globally and in many countries.
Added value of this study
The GBD 2015 assessment of maternal mortality provides new and more robust evidence on the levels and trends in maternal mortality in 195 countries and territories throughout the world as the MDG era has ended and the SDG era is beginning. It incorporates subnational data from an expanded group of countries that now includes Brazil, China, India, Japan, Kenya, Mexico, Saudi Arabia, South Africa, Sweden, the UK, and the USA. This study complies with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) recommendations. Further, this analysis extends the concept of sociodemographic status by introducing a new sociodemographic index for a more robust positioning of countries and territories on the development continuum.
Implications of all the available evidence
This study provides the most comprehensive assessment to date of patterns and levels of maternal mortality worldwide, expanding on previous analyses by including the full reproductive age range of 10–54 years, more comprehensively evaluating the interplay between maternal mortality, HIV/AIDS, and all-cause mortality, and reporting on how the coverage of reproductive health services relates to risk of maternal mortality. This study further investigates the main determinants of epidemiological patterns and trends across geographies and over time by comparing the observed maternal mortality, including eight underlying aetiologies of maternal mortality, with patterns expected on the basis of SDI. The GBD 2015 study entails a complete reanalysis of levels and trends from 1990 to 2015; the time series published here therefore supersedes the results of the GBD 2013 study. The expansion of geographic units, from 296 in GBD 2013 to 519 for GBD 2015, is envisaged to continue so as to sustain comparability over time and across all geographies.
Acknowledgments
We would like to thank the countless individuals who have contributed to the Global Burden of Disease Study 2015 in various capacities. Data for this research was provided by MEASURE Evaluation, funded by the United States Agency for International Development (USAID). Collection of these data was made possible by the US Agency for International Development (USAID) under the terms of cooperative agreement GPO-A-00-08-000_D3-00. Views expressed do not necessarily reflect those of USAID, the US Government, or MEASURE Evaluation. The following individuals would like to acknowledge various forms of institutional support: Panniyammakal Jeemon is supported by a clinical and public health intermediate fellowship from the Wellcome Trust-DBT India Alliance (2015-2020). Boris Bikbov, Monica Cortinovis, Giuseppe Remuzzi, and Norberto Perico would like to acknowledge that their contribution to this paper has been on behalf of the International Society of Nephrology (ISN) as a follow-up of the activities of the GBD 2010 Genitourinary Diseases Expert Group. Shifalika Goenka is partially supported through a Wellcome Trust Grant (No: 096735/A/11/Z) and The Bernard Lown Scholars in Cardiovascular Health Program, Harvard School of Public Health. Hjalte H Andersen would like to acknowledge funding received from the EliteForsk 2016 travel grant of the Danish Ministry of Higher Education and Science. Amador Goodridge would like to acknowledge funding for me from Sistema Nacional de Investigadores de Panamá-SNI. José das Neves was supported in his contribution to this work by a Fellowship from Fundação para a Ciência e a Tecnologia, Portugal (SFRH/BPD/92934/2013). Beatriz Paulina Ayala Quintanilla would like to acknowledge the Institutional support of PRONABEC (National Program of Scholarship and Educational Loan), provided by the Peruvian Government, while studying for her doctoral course at the Judith Lumley Centre of La Trobe University funded by PRONABEC. Ulrich O Mueller gratefully acknowledges funding by the German National Cohort Consortium (O1ER1511D). Andrea Werdecker gratefully acknowledges funding by the German National Cohort BMBF grant No OIER 1301/22. Charles D A Wolfe would like to acknowledge the following: National Institute for Health Research (NIHR) Program Grant (RP-PG-0407-10184), and the National Institute for Health Research Biomedical Research Centre at Guy’s and St Thomas’ National Health Service (NHS) Foundation Trust and King’s College London. No individuals acknowledged received additional compensation for their efforts.
GBD 2015 Maternal Mortality Collaborators
Nicholas J Kassebaum†, Ryan M Barber, Zulfiqar A Bhutta, Lalit Dandona, Peter W Gething, Simon I Hay, Yohannes Kinfu, Heidi J Larson, Xiaofeng Liang, Stephen S Lim, Alan D Lopez, Rafael Lozano, George A Mensah, Ali H Mokdad, Mohsen Naghavi, Christine Pinho, Joshua A Salomon, Caitlyn Steiner, Theo Vos, Haidong Wang, Amanuel Alemu Abajobir*, Kalkidan Hassen Abate*, Kaja M Abbas*, Foad Abd-Allah*, Mahmud A Abdallat*, Abdishakur M Abdulle*, Semaw Ferede Abera*, Victor Aboyans*, Ibrahim Abubakar*, Niveen M E Abu-Rmeileh*, Tom Achoki*, Akindele Olupelumi Adebiyi*, Isaac Akinkunmi Adedeji*, Ademola Lukman Adelekan*, Arsène Kouablan Adou*, Kossivi Agbelenko Afanvi*, Arnav Agarwal*, Aliasghar Ahmad Kiadaliri*, Oluremi N Ajala*, Tomi F Akinyemiju*, Nadia Akseer*, Ziyad Al-Aly*, Khurshid Alam*, Noore K M Alam*, Deena Alasfoor*, Saleh Fahed Aldhahri*, Robert William Aldridge*, Samia Alhabib*, Raghib Ali*, Ala’a Alkerwi*, François Alla*, Rajaa Al-Raddadi*, Ubai Alsharif*, Elena Alvarez Martin*, Nelson Alvis-Guzman*, Azmeraw T Amare*, Alemayehu Amberbir*, Adeladza Kofi Amegah*, Walid Ammar*, Stephen Marc Amrock*, Hjalte H Andersen*, Gregory M Anderson*, Rose Mayerline Antoine*, Carl Abelardo T Antonio*, Atsede Fantahun Aregay*, Johan Ärnlöv*, Megha Arora*, Valentina S Arsic Arsenijevic*, Al Artaman*, Hamid Asayesh*, Suleman Atique*, Euripide Frinel G Arthur Avokpaho*, Ashish Awasthi*, Beatriz Paulina Ayala Quintanilla*, Peter Azzopardi*, Umar Bacha*, Alaa Badawi*, Maria C Bahit*, Kalpana Balakrishnan*, Amitava Banerjee*, Aleksandra Barac*, Suzanne L Barker-Collo*, Till Bärnighausen*, Sanjay Basu*, Tigist Assefa Bayou*, Yibeltal Tebekaw Bayou*, Shahrzad Bazargan-Hejazi*, Justin Beardsley*, NeerajHaidong Wang,Bedi*, Tolesa Bekele*, Michelle L Bell*, Derrick A Bennett*, Isabela M Bensenor*, Adugnaw Berhane*, Eduardo Bernabé*, Balem Demtsu Betsu*, Addisu Shunu Beyene*, Sibhatu Biadgilign*, Boris Bikbov*, Aref A Bin Abdulhak*, Brian J Biroscak*, Stan Biryukov*, Donal Bisanzio*, Espen Bjertness*, Jed D Blore*, Michael Brainin*, Alexandra Brazinova*, Nicholas J K Breitborde*, Traolach S Brugha*, Zahid A Butt*, Ismael Ricardo Campos-Nonato*, Julio Cesar Campuzano*, Rosario Cárdenas*, Juan Jesus Carrero*, Austin Carter*, Daniel C Casey*, Carlos A Castañeda-Orjuela*, Ruben Estanislao Castro*, Ferrán Catalá-López*, Fiorella Cavalleri*, Hsing-Yi Chang*, Jung-Chen Chang*, Laxmikant Chavan*, Chioma Ezinne Chibueze*, Vesper Hichilombwe Chisumpa*, Jee-Young Jasmine Choi*, Rajiv Chowdhury*, Devasahayam Jesudas Christopher*, Liliana G Ciobanu*, Massimo Cirillo*, Matthew M Coates*, Megan Coggeshall*, Valentina Colistro*, Samantha M Colquhoun*, Cyrus Cooper*, Leslie Trumbull Cooper*, Monica Cortinovis*, Tukur Dahiru*, Albertino Damasceno*, Hadi Danawi*, Rakhi Dandona*, José das Neves*, Diego De Leo*, Robert P Dellavalle*, Kebede Deribe*, Amare Deribew*, Don C Des Jarlais*, Samath D Dharmaratne*, Daniel J Dicker*, Eric L Ding*, Edem Dossou*, Manisha Dubey*, Beth E Ebel*, Christian Lycke Ellingsen*, Iqbal Elyazar*, Aman Yesuf Endries*, Sergey Petrovich Ermakov*, Babak Eshrati*, Alireza Esteghamati*, Emerito Jose Aquino Faraon*, Talha A Farid*, Carla Sofia e Sa Farinha*, André Faro*, Maryam S Farvid*, Farshad Farzadfar*, Seyed-Mohammad Fereshtehnejad*, Joao C Fernandes*, Florian Fischer*, Joseph R A Fitchett*, Tom Fleming*, Nataliya Foigt*, Elisabeth Barboza Franca*, Richard C Franklin*, Maya S Fraser*, Joseph Friedman*, Nancy Fullman*, Thomas Fürst*, Neal D Futran*, Ketevan Gambashidze*, Amiran Gamkrelidze*, Teshome Gebre*, Tsegaye Tewelde Gebrehiwot*, Amanuel Tesfay Gebremedhin*, Mengistu Gebremedhin*, Alemseged Aregay Gebru*, Johanna M Geleijnse*, Katherine B Gibney*, Ababi Zergaw Giref*, Maurice Giroud*, Melkamu Dedefo Gishu*, Elizabeth Glaser*, Shifalika Goenka*, Hector Gomez-Dantes*, Philimon Gona*, Amador Goodridge*, Sameer Vali Gopalani*, Atsushi Goto*, Nicholas Graetz*, Harish Chander Gugnani*, Yuming Guo*, Rahul Gupta*, Rajeev Gupta*, Vipin Gupta*, Nima Hafezi-Nejad*, Alemayehu Desalegne Hailu*, Gessessew Bugssa Hailu*, Randah Ribhi Hamadeh*, Samer Hamidi*, Jamie Hancock*, Alexis J Handal*, Graeme J Hankey*, Hilda L Harb*, Sivadasanpillai Harikrishnan*, Kimani M Harun*, Rasmus Havmoeller*, Hans W Hoek*, Masako Horino*, Nobuyuki Horita*, H Dean Hosgood*, Damian G Hoy*, Aung Soe Htet*, Guoqing Hu*, Hsiang Huang*, John J Huang*, Inge Huybrechts*, Chantal Huynh*, Marissa Iannarone*, Kim Moesgaard Iburg*, Bulat T Idrisov*, Veena J Iyer*, Kathryn H Jacobsen*, Nader Jahanmehr*, Mihajlo B Jakovljevic*, Mehdi Javanbakht*, Achala Upendra Jayatilleke*, Sun Ha Jee*, Panniyammakal Jeemon*, Vivekanand Jha*, Guohong Jiang*, Ying Jiang*, Tariku Jibat*, Jost B Jonas*, Zubair Kabir*, Ritul Kamal*, Haidong Kan*, André Karch*, Dimitris Karletsos*, Amir Kasaeian*, Anil Kaul*, Norito Kawakami*, Jeanne Françoise Kayibanda*, Konstantin Kazanjan*, Dhruv S Kazi*, Peter Njenga Keiyoro*, Laura Kemmer*, Andrew Haddon Kemp*, Andre Pascal Kengne*, Andre Keren*, Maia Kereselidze*, Chandrasekharan Nair Kesavachandran*, Yousef Saleh Khader*, Abdur Rahman Khan*, Ejaz Ahmad Khan*, Young-Ho Khang*, Irma Khonelidze*, Ardeshir Khosravi*, Jagdish Khubchandani*, Yun Jin Kim*, Miia Kivipelto*, Luke D Knibbs*, Yoshihiro Kokubo*, Soewarta Kosen*, Parvaiz A Koul*, Ai Koyanagi*, Sanjay Krishnaswami*, Barthelemy Kuate Defo*, Burcu Kucuk Bicer*, Andreas A Kudom*, Xie Rachel Kulikoff*, Chanda Kulkarni*, G Anil Kumar*, Michael J Kutz*, Dharmesh Kumar Lal*, Ratilal Lalloo*, Hilton Lam*, Hector Lamadrid-Figueroa*, Qing Lan*, Anders Larsson*, Dennis Odai Laryea*, James Leigh*, Ricky Leung*, Yichong Li*, Yongmei Li*, Steven E Lipshultz*, Patrick Y Liu*, Shiwei Liu*, Yang Liu*, Belinda K Lloyd*, Paulo A Lotufo*, Raimundas Lunevicius*, Stefan Ma*, Hassan Magdy Abd El Razek*, Mohammed Magdy Abd El Razek*, Marek Majdan*, Azeem Majeed*, Reza Malekzadeh*, Chabila C Mapoma*, Wagner Marcenes*, David Joel Margolis*, Neal Marquez*, Felix Masiye*, Melvin Barrientos Marzan*, Amanda J Mason-Jones*, Tasara T Mazorodze*, Peter A Meaney*, Alem Mehari*, Man Mohan Mehndiratta*, Fabiola Mejia-Rodriguez*, Alemayehu B Mekonnen*, Yohannes Adama Melaku*, Ziad A Memish*, Walter Mendoza*, Atte Meretoja*, Tuomo J Meretoja*, Francis Apolinary Mhimbira*, Ted R Miller*, Edward J Mills*, Mojde Mirarefin*, Awoke Misganaw*, Norlinah Mohamed Ibrahim*, Karzan Abdulmuhsin Mohammad*, Alireza Mohammadi*, Shafiu Mohammed*, Glen Liddell D Mola*, Lorenzo Monasta*, Jonathan de la Cruz Monis*, Julio Cesar Montañez Hernandez*, Pablo Montero*, Marcella Montico*, Meghan D Mooney*, Ami R Moore*, Maziar Moradi-Lakeh*, Lidia Morawska*, Rintaro Mori*, Ulrich O Mueller*, Gudlavalleti Venkata Satyanarayana Murthy*, Srinivas Murthy*, Jean B Nachega*, Aliya Naheed*, Luigi Naldi*, Devina Nand*, Vinay Nangia*, Denis Nash*, Subas Neupane*, John N Newton*, Marie Ng*, Frida Namnyak Ngalesoni*, Peter Nguhiu*, Grant Nguyen*, Quyen Le Nguyen*, Muhammad Imran Nisar*, Marika Nomura*, Ole F Norheim*, Rosana E Norman*, Luke Nyakarahuka*, Carla Makhlouf Obermeyer*, Felix Akpojene Ogbo*, In-Hwan Oh*, Foluke Adetola Ojelabi*, Pedro R Olivares*, Bolajoko Olubukunola Olusanya*, Jacob Olusegun Olusanya*, John Nelson Opio*, Eyal Oren*, Erika Ota*, Abayomi Samuel Oyekale*, Mahesh PA*, Amanda Pain*, Nikolaos Papantoniou*, Eun-Kee Park*, Hye-Youn Park*, Angel J Paternina Caicedo*, Scott B Patten*, Vinod K Paul*, David M Pereira*, Norberto Perico*, Konrad Pesudovs*, Max Petzold*, Michael Robert Phillips*, Julian David Pillay*, Farhad Pishgar*, Suzanne Polinder*, Daniel Pope*, Farshad Pourmalek*, Mostafa Qorbani*, Anwar Rafay*, Kazem Rahimi*, Vafa Rahimi-Movaghar*, Mahfuzar Rahman*, Mohammad Hifz Ur Rahman*, Sajjad Ur Rahman*, Rajesh Kumar Rai*, Usha Ram*, Chhabi Lal Ranabhat*, Thara Rangaswamy*, Paturi Vishnupriya Rao*, Amany H Refaat*, Giuseppe Remuzzi*, Serge Resnikoff*, David Rojas-Rueda*, Luca Ronfani*, Gholamreza Roshandel*, Ambuj Roy*, George Mugambage Ruhago*, Rajesh Sagar*, Muhammad Muhammad Saleh*, Juan R Sanabria*, Maria Dolores Sanchez-Niño*, Itamar S Santos*, Joao Vascos Santos*, Rodrigo Sarmiento-Suarez*, Benn Sartorius*, Maheswar Satpathy*, Miloje Savic*, Monika Sawhney*, Mete I Saylan*, Ione J C Schneider*, David C Schwebel*, Soraya Seedat*, Sadaf G Sepanlou*, Edson E Servan-Mori*, Tesfaye Setegn*, Katya A Shackelford*, Masood Ali Shaikh*, Marina Shakh-Nazarova*, Rajesh Sharma*, Jun She*, Sara Sheikhbahaei*, Jiabin Shen*, Kenji Shibuya*, Min-Jeong Shin*, Rahman Shiri*, Kawkab Shishani*, Ivy Shiue*, Inga Dora Sigfusdottir*, Naris Silpakit*, Diego Augusto Santos Silva*, Dayane Gabriele Alves Silveira*, Jonathan I Silverberg*, Edgar P Simard*, Shireen Sindi*, Abhishek Singh*, Jasvinder A Singh*, Om Prakash Singh*, Prashant Kumar Singh*, Virendra Singh*, Vegard Skirbekk*, Amber Sligar*, Karen Sliwa*, Jessica M Smith*, Samir Soneji*, Reed J D Sorensen*, Joan B Soriano*, Sergey Soshnikov*, Luciano A Sposato*, Chandrashekhar T Sreeramareddy*, Vasiliki Stathopoulou*, Konstantinos Stroumpoulis*, Lela Sturua*, Bruno F Sunguya*, Soumya Swaminathan*, Bryan L Sykes*, Cassandra E I Szoeke*, Rafael Tabarés-Seisdedos*, Karen M Tabb*, Roberto Tchio Talongwa*, Mohammad Tavakkoli*, Bineyam Taye*, Bemnet Amare Tedla*, Worku Mekonnen Tefera*, Tesfaye Tekle*, Girma Temam Shifa*, Abdullah Sulieman Terkawi*, Fisaha Haile Tesfay*, Gizachew Assefa Tessema*, Alan J Thomson*, Andrew L Thorne-Lyman*, Ruoyan Tobe-Gai*, Roman Topor-Madry*, Jeffrey Allen Towbin*, Bach Xuan Tran*, Zacharie Tsala Dimbuene*, Abera Kenay Tura*, Stefanos Tyrovolas*, Kingsley N Ukwaja*, Olalekan A Uthman*, Tommi Vasankari*, Narayanaswamy Venketasubramanian*, Francesco S Violante*, Sergey K Vladimirov*, Vasiliy Victorovich Vlassov*, Stein Emil Vollset*, Joseph A Wagner*, Linhong Wang*, Scott Weichenthal*, Elisabete Weiderpass*, Robert G Weintraub*, Andrea Werdecker*, Ronny Westerman*, Tissa Wijeratne*, James D Wilkinson*, Charles Shey Wiysonge*, Solomon Meseret Woldeyohannes*, Charles D A Wolfe*, Timothy Wolock*, Sungho Won*, Mamo Wubshet*, Qingyang Xiao*, Gelin Xu*, Ajit Kumar Yadav*, Bereket Yakob*, Ayalnesh Zemene Yalew*, Yuichiro Yano*, Henock Gebremedhin Yebyo*, Paul Yip*, Naohiro Yonemoto*, Seok-Jun Yoon*, Mustafa Z Younis*, Chuanhua Yu*, Shicheng Yu*, Zoubida Zaidi*, Maysaa El Sayed Zaki*, Hajo Zeeb*, Yi Zhao*, Yong Zhao*, Maigeng Zhou*, Sanjay Zodpey*, Liesl Joanna Zuhlke*, Christopher J L Murray
*Authors listed alphabetically. †Corresponding author.
Affiliations
Institute for Health Metrics and Evaluation (N J Kassebaum MD, R M Barber BS, Prof L Dandona MD, Prof S I Hay DSc, H J Larson PhD, Prof S S Lim PhD, Prof A D Lopez PhD, Prof A H Mokdad PhD, Prof M Naghavi PhD, C Pinho BA, C Steiner MPH, Prof T Vos PhD, H Wang PhD, T Achoki MD, G M Anderson MS EE, M Arora BSA, S Biryukov BS, J D Blore PhD, A Carter BS, D C Casey BA, M M Coates MPH, M Coggeshall BA, D J Dicker BS, E Dossou BS, T Fleming BS, M S Fraser BA, J Friedman BA, N Fullman MPH, N Graetz MPH, J Hancock MLS, C Huynh BA, M Iannarone MSc, L Kemmer PhD, X R Kulikoff BA, M J Kutz BS, P Y Liu BA, N Marquez BS, A Misganaw PhD, M D Mooney BS, M Moradi-Lakeh MD, M Ng PhD, G Nguyen MPH, A Pain MPH, K A Shackelford BA, N Silpakit BS, A Sligar MPH, J M Smith BA, R J D Sorensen MPH, Prof S E Vollset PhD, J A Wagner BS, T Wolock BA, Y Zhao MS, Prof M Zhou PhD, Prof C J L Murray DPhil), Harborview Injury Prevention and Research Center (B E Ebel MD), University of Washington, Seattle, WA, USA (N D Futran MD, K M Harun MPH); Centre of Excellence in Women and Child Health (Prof Z A Bhutta PhD), Aga Khan University, Karachi, Pakistan (M I Nisar MSc); Centre for Global Child Health, The Hospital for Sick Children, Toronto, ON, Canada (N Akseer MSc, Prof Z A Bhutta PhD); Centre for Control of Chronic Conditions (P Jeemon PhD), Public Health Foundation of India, New Delhi, India (Prof L Dandona MD, R Dandona PhD, S Goenka PhD, G A Kumar PhD); Department of Zoology (P W Gething PhD), Nuffield Department of Medicine (D Bisanzio PhD, A Deribew PhD), NIHR Musculoskeletal Biomedical Research Centre (Prof C Cooper FMedSci); University of Oxford, Oxford, UK (R Ali FRCP, D A Bennett PhD, Prof V Jha DM, K Rahimi DM); Centre for Research & Action in Public Health, Faculty of Health, University of Canberra, Canberra, ACT, Australia (Y Kinfu PhD); Department of Infectious Disease Epidemiology (H J Larson PhD), London School of Hygiene & Tropical Medicine, London, UK (Prof G V S Murthy MD); National Center for Chronic and Noncommunicable Disease Control and Prevention (Y Li MPH, S Liu PhD, Prof L Wang MD, Prof M Zhou PhD), Chinese Center for Disease Control and Prevention, Beijing, China (Prof X Liang MD, Prof S Yu PhD); Melbourne School of Population and Global Health (Prof A D Lopez PhD), Department of Paediatrics (P Azzopardi MEpi), The Peter Doherty Institute for Infection and Immunity (K B Gibney FRACP), Department of Medicine (A Meretoja PhD), Institute of Health and Ageing (Prof C E I Szoeke PhD), Murdoch Childrens Research Institute (P Azzopardi MEpi, K Alam PhD, S M Colquhoun PhD, R G Weintraub MBBS), The University of Melbourne, Melbourne, VIC, Australia (K Alam PhD, S M Colquhoun PhD, Prof T Wijeratne MD); National Institute of Public Health, Cuernavaca, Mexico (Prof R Lozano PhD, I R Campos-Nonato PhD, J C Campuzano PhD, H Gomez-Dantes MC, H Lamadrid-Figueroa DSc, F Mejia-Rodriguez MD, J C Montañez Hernandez MSc, P Montero MS); Center for Translation Research and Implementation Science, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, MD, USA (G A Mensah MD); Department of Global Health and Population (Prof J A Salomon PhD), Department of Nutrition, (A L Thorne-Lyman ScD), Harvard T H Chan School of Public Health (O N Ajala MD, Prof T Bärnighausen MD, I R Campos-Nonato PhD, E L Ding ScD, M S Farvid PhD), Harvard University, Boston, MA, USA (J R A Fitchett MD); School of Public Health (A A Abajobir MPH, L D Knibbs PhD), School of Dentistry (Prof R Lalloo PhD), University of Queensland, Brisbane, QLD, Australia (N K M Alam MPH, Y Guo PhD); Jimma University, Jimma, Ethiopia (K H Abate MS, T T Gebrehiwot MPH, A T Gebremedhin MPH); Virginia Tech, Blacksburg, VA, USA (Prof K M Abbas PhD); Department of Neurology, Cairo University, Cairo, Egypt (Prof F Abd-Allah MD); Royal Jordanian Medical Services, Amman, Jordan (M A Abdallat MPH); New York University Abu Dhabi, Abu Dhabi, United Arab Emirates (A M Abdulle PhD); School of Public Health, College of Health Sciences (S F Abera MSc), School of Public Health (Y A Melaku MPH), College of Health Sciences (F H Tesfay MPH), Mekelle University, Mekelle, Ethiopia (A F Aregay MS, T A Bayou BS, B D Betsu MPH, M Gebremedhin BA, A A Gebru MPH, G B Hailu MSc, T Tekle MPH, A Z Yalew MS, H G Yebyo MS); Kilte Awlaelo-Health and Demographic Surveillance Site, Mekelle, Ethiopia (S F Abera MSc); Food Security and Institute for Biological Chemistry and Nutrition, University of Hohenheim, Stuttgart, Germany (S F Abera MSc); Dupuytren University Hospital, Limoges, France (Prof V Aboyans PhD); Institute for Global Health (Prof I Abubakar PhD), Centre for Public Health Data Science, Institute of Health Informatics (R W Aldridge PhD), Farr Institute of Health Informatics Research (A Banerjee DPhil), University College London, London, UK; Institute of Community and Public Health, Birzeit University, Ramallah, Palestine (N M AbuRmeileh PhD); College of Medicine (A O Adebiyi MD), University of Ibadan, Ibadan, Nigeria (A L Adelekan MPH, F A Ojelabi MPH); University College Hospital, Ibadan, Nigeria (A O Adebiyi MD); Olabisi Onabanjo University, Ago-Iwoye, Nigeria (I A Adedeji MS); Public Health Promotion Alliance, Osogbo, Nigeria (A L Adelekan MPH); Association Ivoirienne pour le Bien-Être Familial, Abidjan, Côte d’Ivoire (A K Adou MD); Direction du District Sanitaire de Haho, Notse, Togo (K A Afanvi MD); Faculte des Sciences de Sante, Universite de Lome, Lome, Togo (K A Afanvi MD); Dalla Lana School of Public Health (N Akseer MSc), Department of Nutritional Sciences, Faculty of Medicine (A Badawi PhD), University of Toronto, Toronto, ON, Canada (A Agarwal BHSc); McMaster University, Hamilton, ON, Canada (A Agarwal BHSc); Department of Clinical Sciences Lund, Orthopedics, Clinical Epidemiology Unit, Lund University, Lund, Sweden (A Ahmad Kiadaliri PhD); Health Services Management Research Center, Institute for Futures Studies in Health, Kerman University of Medical Sciences, Kerman, Iran (A Ahmad Kiadaliri PhD); University of Pittsburgh Medical Center, McKeesport, PA, USA (O N Ajala MD); Department of Epidemiology (T F Akinyemiju PhD), University of Alabama at Birmingham, Birmingham, AL, USA (D C Schwebel PhD, J A Singh MD); Washington University in Saint Louis, St Louis, MO, USA (Z Al-Aly MD); University of Sydney, Sydney, NSW, Australia (K Alam PhD, Prof A H Kemp PhD, J Leigh PhD, A B Mekonnen MS); Queensland Health, Herston, QLD, Australia (N K M Alam MPH); Ministry of Health, Al Khuwair, Oman (D Alasfoor MSc); King Saud University, Riyadh, Saudi Arabia (S F Aldhahri MD); Department of Anesthesiology (A S Terkawi MD), King Fahad Medical City, Riyadh, Saudi Arabia (S F Aldhahri MD); King Abdullah Bin Abdulaziz University Hospital, Riyadh, Saudi Arabia (S Alhabib PhD); Luxembourg Institute of Health (LIH), Strassen, Luxembourg (A Alkerwi PhD); School of Public Health, University of Lorraine, Nancy, France (Prof F Alla PhD); Ministry of Health, Jeddah, Saudi Arabia (R Al-Raddadi PhD); Charité Universitätsmedizin, Berlin, Germany (U Alsharif MPH); Spanish Observatory on Drugs, Government Delegation for the National Plan on Drugs, Ministry of Health, Social Policy and Equality, Madrid, Spain (E Alvarez Martin PhD); Universidad de Cartagena, Cartagena de Indias, Colombia (Prof N Alvis-Guzman PhD); School of Medicine (A T Amare MPH, Y A Melaku MPH), University of Adelaide, Adelaide, SA, Australia (L G Ciobanu MS, G A Tessema MPH); College of Medicine and Health Sciences (A T Amare MPH), Bahir Dar University, Bahir Dar, Ethiopia (T Setegn MPH); Dignitas International, Zomba, Malawi (A Amberbir PhD); University of Cape Coast, Cape Coast, Ghana (A K Amegah PhD, A A Kudom PhD); Ministry of Public Health, Beirut, Lebanon (W Ammar PhD, H L Harb MPH); Oregon Health & Science University, Portland, OR, USA (S M Amrock MD); Center of Sensory-Motor Interaction, Department of Health Science and Technology, Faculty of Medicine, Aalborg University, Aalborg, Denmark (H H Andersen MS); Rose Foundation of Haiti, Port-au-Prince, Haiti (R M Antoine MD); Department of Health Policy and Administration, College of Public Health (C A T Antonio MD), College of Public Health (E J A Faraon MD), University of the Philippines Manila, Manila, Philippines; Department of Medical Sciences, Uppsala University, Uppsala, Sweden (Prof J Ärnlöv PhD, Prof A Larsson PhD); Dalarna University, Falun, Sweden (Prof J Ärnlöv PhD); School of Medicine, Institute of Microbiology and Immunology (Prof V S Arsic Arsenijevic PhD), Faculty of Medicine (A Barac PhD), University of Belgrade, Belgrade, Serbia; University Children’s Hospital, Belgrade, Serbia (Prof V S Arsic Arsenijevic PhD); University of Manitoba, Winnipeg, MB, Canada (A Artaman PhD); Department of Medical Emergency, School of Paramedic, Qom University of Medical Sciences, Qom, Iran (H Asayesh PhD); Graduate Institute of Biomedical Informatics, Taipei Medical University, Taipei, Taiwan (S Atique MS); Institut de Recherche Clinique du Bénin, Cotonou, Benin (E F G A Avokpaho MPH); Laboratoire d’Etudes et de Recherche-Action en Santé (LERAS Afrique), Parakou, Benin (E F G A Avokpaho MPH); Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, India (A Awasthi MSc); The Judith Lumley Centre for Mother, Infant and Family Health Research, La Trobe University, Melbourne, VIC, Australia (B P Ayala Quintanilla PhD); Peruvian National Institute of Health, Lima, Peru (B P Ayala Quintanilla PhD); Wardliparingga Aboriginal Research Unit, South Australian Health and Medical Research Institute, Adelaide, SA, Australia (P Azzopardi MEpi); School of Health Sciences, University of Management and Technology, Lahore, Pakistan (U Bacha PhD); Public Health Agency of Canada, Toronto, ON, Canada (A Badawi PhD); INECO Neurociencias, Rosario, Argentina (M C Bahit MD); Sri Ramachandra University, Chennai, India (K Balakrishnan PhD); School of Psychology, University of Auckland, Auckland, New Zealand (S L Barker-Collo PhD); Africa Health Research Institute, Mtubatuba, South Africa (Prof T Bärnighausen MD); Institute of Public Health, Heidelberg University, Heidelberg, Germany (Prof T Bärnighausen MD, S Mohammed PhD); Stanford University, Stanford, CA, USA (S Basu PhD); Jhpiego-Ethiopia, Addis Ababa, Ethiopia (Y T Bayou PhD); Charles R Drew University of Medicine and Science, Los Angeles, CA, USA (Prof S Bazargan-Hejazi PhD); David Geffen School of Medicine, University of California, Los Angeles, Los Angeles, CA, USA (Prof S Bazargan-Hejazi PhD); Kermanshah University of Medical Science, Kermanshah, Iran (Prof S Bazargan-Hejazi PhD); Oxford University, Ho Chi Minh City, Vietnam (J Beardsley MBChB); College of Public Health and Tropical Medicine, Jazan, Saudi Arabia (N Bedi MD); Madawalabu University, Bale Goba, Ethiopia (T Bekele MPH); Yale University, New Haven, CT, USA (Prof M L Bell PhD, Prof B J Biroscak PhD, J J Huang MD); Internal Medicine Department (Prof I S Santos PhD), University of São Paulo, São Paulo, Brazil (I M Bensenor PhD, Prof P A Lotufo DrPH); Debre Berhane University, Debre Berhan, Ethiopia (A Berhane MPH); Division of Health and Social Care Research (Prof C D Wolfe MD), King’s College London, London, UK (E Bernabé PhD); Haramaya University, Harar, Ethiopia (A S Beyene MPH); Independent Public Health Consultants, Addis Ababa, Ethiopia (S Biadgilign MPH); Department of Nephrology Issues of Transplanted Kidney, Academician V I Shumakov Federal Research Center of Transplantology and Artificial Organs, Moscow, Russia (B Bikbov MD); University of Iowa Hospitals and Clinics, Iowa City, IA, USA (A A Bin Abdulhak MD); University of South Florida, Tampa, FL, USA (Prof B J Biroscak PhD); Department of Community Medicine (Prof E Bjertness PhD), University of Oslo, Oslo, Norway (A S Htet MPhil); Danube-University Krems, Krems, Austria (Prof M Brainin PhD); Faculty of Health Sciences and Social Work, Department of Public Health, Trnava University, Trnava, Slovakia (A Brazinova PhD, M Majdan PhD); International Neurotrauma Research Organization, Vienna, Austria (A Brazinova PhD); College of Medicine (J Shen PhD), Ohio State University, Columbus, OH, USA (Prof N J K Breitborde PhD); University of Leicester, Leicester, UK (Prof T S Brugha MD); Al Shifa Trust Eye Hospital, Rawalpindi, Pakistan (Z A Butt PhD); Metropolitan Autonomous University, Mexico City, Mexico (R Cárdenas ScD); Department of Neurobiology, Care Sciences and Society (NVS) (S Fereshtehnejad MD), Aging Research Center (Prof M Kivipelto PhD), Department of Medical Epidemiology and Biostatistics (E Weiderpass PhD), Karolinska Institutet, Stockholm, Sweden (R Havmoeller PhD, S Sindi PhD); Colombian National Health Observatory, Instituto Nacional de Salud, Bogotá, Colombia (C A Castañeda-Orjuela MSc); Epidemiology and Public Health Evaluation Group, Public Health Department, Universidad Nacional de Colombia, Bogotá, Colombia (C A CastañedaOrjuela MSc); Universidad Diego Portales, Santiago, Chile (R E Castro PhD); Department of Medicine, University of Valencia/INCLIVA Health Research Institute and CIBERSAM, Valencia, Spain (F Catalá-López PhD); Clinical Epidemiology Program, Ottawa Hospital Research Institute, Ottawa, ON, Canada (F Catalá-López PhD); Faculty of Medicine (F Cavalleri BS), University of the Republic, Montevideo, Uruguay (V Colistro MSc); National Health Research Institutes, Zhunan Town, Taiwan (Prof H Chang DrPH); National Yang-Ming University, Taipei, Taiwan (Prof H Chang DrPH); School of Nursing, College of Medicine, National Taiwan University, Taipei, Taiwan (Prof J Chang PhD); World Health Organization, New Delhi, India (L Chavan MD); National Center for Child Health and Development, Setagaya, Japan (C E Chibueze PhD); University of Zambia, Lusaka, Zambia (V H Chisumpa MPhil, C C Mapoma PhD, F Masiye PhD); University of Witwatersrand, Johannesburg, South Africa (V H Chisumpa MPhil); Seoul National University Medical Library, Seoul, South Korea (J J Choi PhD); Department of Public Health and Primary Care, University of Cambridge, Cambridge, UK (R Chowdhury PhD); Christian Medical College, Vellore, India (Prof D J Christopher MD); University of Salerno, Baronissi, Italy (Prof M Cirillo MD); Ministerio de Salud Pública, Montevideo, Uruguay (V Colistro MSc); MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton, UK (Prof C Cooper FMedSci); NIHR Biomedical Research Centre, University of Southampton and University Hospital Southampton NHS Foundation Trust, Southampton, UK (Prof C Cooper FMedSci); Mayo Clinic, Jacksonville, FL, USA (L T Cooper MD); IRCCS - Istituto di Ricerche Farmacologiche Mario Negri, Milan, Italy (M Cortinovis Biotech D); Ahmadu Bello University Zaria, Zaria, Nigeria (T Dahiru MA); Faculty of Medicine, Eduardo Mondlane University, Maputo, Mozambique (Prof A Damasceno PhD); Walden University, Minneapolis, MN, USA (H Danawi PhD, Prof A H Refaat PhD); i3S - Instituto de Investigação e Inovação em Saúde and INEB - Instituto de Engenharia Biomédica (J das Neves PhD), Faculty of Medicine (J V Santos BHlthSc), University of Porto, Porto, Portugal; Griffith University, Brisbane, QLD, Australia (Prof D De Leo DSc); University of Colorado School of Medicine and the Colorado School of Public Health, Aurora, CO, USA (R P Dellavalle MD); Brighton and Sussex Medical School, Brighton, UK (K Deribe MPH); School of Public Health (K Deribe MPH, A D Hailu MPH), College of Health Sciences, School of Public Health (W Tefera MPH), Addis Ababa University, Addis Ababa, Ethiopia (A Z Giref PhD, T Jibat MS, G Temam Shifa MPH); KEMRI-Wellcome Trust Research Programme, Kilifi, Kenya (A Deribew PhD); Mount Sinai Beth Israel, New York, NY, USA (Prof D C Des Jarlais PhD); Icahn School of Medicine at Mount Sinai, New York City, NY, USA (Prof D C Des Jarlais PhD); Department of Community Medicine, Faculty of Medicine, University of Peradeniya, Peradeniya, Sri Lanka (S D Dharmaratne MD); International Institute for Population Sciences, Mumbai, India (M Dubey MPhil, M H U Rahman MPhil, Prof U Ram PhD, A Singh PhD, A K Yadav MPhil); Centre for Disease Burden (Prof S E Vollset DrPH), Norwegian Institute of Public Health, Oslo, Norway (C L Ellingsen MD, M Savic PhD, Prof V Skirbekk PhD); Eijkman-Oxford Clinical Research Unit, Jakarta, Indonesia (I Elyazar PhD); The Institute of Social and Economic Studies of Population, Russian Academy of Sciences, Moscow, Russia (Prof S P Ermakov DSc); Federal Research Institute for Health Organization and Informatics, Ministry of Health of the Russian Federation, Moscow, Russia (Prof S P Ermakov DSc, S Soshnikov PhD); Ministry of Health and Medical Education, Tehran, Iran (B Eshrati PhD); Arak University of Medical Sciences, Arak, Iran (B Eshrati PhD); Non-Communicable Diseases Research Center (F Farzadfar MD, A Kasaeian PhD, F Pishgar MD), Endocrinology and Metabolism Population Sciences Institute (Prof A Esteghamati MD, N Hafezi-Nejad MD, S Sheikhbahaei MD), Hematology-Oncology and Stem Cell Transplantation Research Center (A Kasaeian PhD), Non-Communicable Diseases Research Center (A Khosravi PhD), Digestive Diseases Research Institute (Prof R Malekzadeh MD, G Roshandel PhD, S G Sepanlou PhD), Uro-Oncology Research Center (F Pishgar MD), Sina Trauma and Surgery Research Center (Prof V Rahimi-Movaghar MD), Tehran University of Medical Sciences, Tehran, Iran; Department of Health, Manila, Philippines (E J A Faraon MD); University of Louisville, Louisville, KY, USA (T A Farid MD, A R Khan MD); DGS Directorate General of Health, Lisboa, Portugal (C S E S Farinha MSc); Universidade Aberta, Lisboa, Portugal (C S E S Farinha MSc); Federal University of Sergipe, Aracaju, Brazil (Prof A Faro PhD); Harvard/MGH Center on Genomics, Vulnerable Populations, and Health Disparities, Mongan Institute for Health Policy, Massachusetts General Hospital, Boston, MA, USA (M S Farvid PhD); Centre for Experimental Medicine & Rheumatology, William Harvey Research Institute, Barts and The London School of Medicine & Dentistry, Queen Mary University of London, London, UK (J C Fernandes PhD), Bielefeld University, Bielefeld, Germany (F Fischer MPH); Institute of Gerontology, Academy of Medical Science, Kyiv, Ukraine (N Foigt PhD); Federal University of Minas Gerais, Belo Horizonte, Brazil (E B Franca PhD); James Cook University, Townsville, QLD, Australia (R C Franklin PhD); Department of Infectious Disease Epidemiology (T Fürst PhD), Imperial College London, London, UK (Prof A Majeed MD); Department of Epidemiology and Public Health, Swiss Tropical and Public Health Institute, Basel, Switzerland (T Fürst PhD); University of Basel, Basel, Switzerland (T Fürst PhD); National Center for Disease Control and Public Health, Tbilisi, Georgia (K Gambashidze MS, K Kazanjan MS, M Kereselidze PhD, I Khonelidze MPA, M Shakh-Nazarova MS, L Sturua PhD); National Center for Disease Control & Public Health, Tbilisi, Georgia (A Gamkrelidze PhD); The Task Force for Global Health, Decatur, GA, USA (T Gebre PhD); Ludwig Maximilians University, Munich, Germany (A T Gebremedhin MPH); Kilte Awlaelo Health and Demographic Surveillance System, Mekelle, Ethiopia (A A Gebru MPH, G B Hailu MSc); Division of Human Nutrition (J M Geleijnse PhD), Wageningen University, Wageningen, Netherlands (T Jibat MS); The Royal Melbourne Hospital, Melbourne, VIC, Australia (K B Gibney FRACP); University Hospital of Dijon, Dijon, France (Prof M Giroud MD); Haramaya University, Dire Dawa, Ethiopia (M D Gishu MS, A K Tura MPH); Kersa Health and Demographic Surveillance System, Harar, Ethiopia (M D Gishu MS); Heller School for Social Policy and Management, Brandeis University, Waltham, MA, USA (E Glaser MS); University of Massachusetts Boston, Boston, MA, USA (Prof P Gona PhD); Instituto de Investigaciones Cientificas y Servicios de Alta Tecnologia - INDICASAT-AIP, Cuidad del Saber, Panama (A Goodridge PhD); Department of Health and Social Affairs, Government of the Federated States of Micronesia, Palikir, Federated States of Micronesia (S V Gopalani MPH); Division of Epidemiology, Center for Public Health Sciences, National Cancer Center, Tokyo, Japan (A Goto PhD); Departments of Microbiology and Epidemiology & Biostatistics, Saint James School of Medicine, The Quarter, Anguilla (Prof H C Gugnani PhD); West Virginia Bureau for Public Health, Charleston, WV, USA (R Gupta MD); Eternal Heart Care Centre and Research Institute, Jaipur, India (R Gupta PhD); Department of Anthropology, University of Delhi, Delhi, India (V Gupta PhD); Department of Global Public Health and Primary Care (Prof S E Vollset DrPH), University of Bergen, Bergen, Norway (A D Hailu MPH, Prof O F Norheim PhD); Arabian Gulf University, Manama, Bahrain (Prof R R Hamadeh DPhil); Hamdan Bin Mohammed Smart University, Dubai, United Arab Emirates (S Hamidi PhD); University of New Mexico, Albuquerque, NM, USA (A J Handal PhD); School of Medicine and Pharmacology, University of Western Australia, Perth, WA, Australia (Prof G J Hankey MD); Harry Perkins Institute of Medical Research, Nedlands, WA, Australia (Prof G J Hankey MD); Western Australian Neuroscience Research Institute, Nedlands, WA, Australia (Prof G J Hankey MD); Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, India (S Harikrishnan DM); Kenyatta University, Nairobi, Kenya (K M Harun MPH); Department of Psychiatry, University Medical Center Groningen (Prof H W Hoek MD), University of Groningen, Groningen, Netherlands (A K Tura MPH); Department of Epidemiology, Mailman School of Public Health (Prof H W Hoek MD), Columbia University, New York, NY, USA (Prof V Skirbekk PhD); Nevada Division of Behavior and Public Health, Carson City, NV, USA (M Horino MPH); Fielding School of Public Health, University of California Los Angeles, Los Angeles, CA, USA (M Horino MPH); Yokohama City University School of Medicine, Yokohama, Japan (N Horita MD); Albert Einstein College of Medicine, Bronx, NY, USA (Prof H D Hosgood PhD); Public Health Division, Secretariat of the Pacific Community, Noumea, New Caledonia (D G Hoy PhD); International Relations Division, Ministry of Health, Nay Pyi Taw, Myanmar (A S Htet MPhil); Department of Epidemiology and Health Statistics, School of Public Health, Central South University, Changsha, China (G Hu PhD); Cambridge Health Alliance, Cambridge, MA, USA (H Huang MD); International Agency for Research on Cancer (IARC), Lyon, France (I Huybrechts PhD); Ghent University, Ghent, Belgium (I Huybrechts PhD); Aarhus University, Aarhus, Denmark (K M Iburg PhD); Bashkir State Medical University, Ufa, Russia (B T Idrisov MD); Boston Medical Center, Boston University, Boston, MA, USA (B T Idrisov MD); Indian Institute of Public Health Gandhinagar, Ahmedabad, India (V J Iyer MPH); Department of Global and Community Health, George Mason University, Fairfax, VA, USA (K H Jacobsen PhD); School of Public Health, Shahid Beheshti University of Medical Sciences, Tehran, Iran (N Jahanmehr PhD); Faculty of Medical Sciences, University of Kragujevac, Kragujevac, Serbia (Prof M B Jakovljevic PhD); University of Aberdeen, Aberdeen, UK (M Javanbakht PhD); Postgraduate Institute of Medicine, Colombo, Sri Lanka (A U Jayatilleke PhD); Institute of Violence and Injury Prevention, Colombo, Sri Lanka (A U Jayatilleke PhD); Graduate School of Public Health (Prof S H Jee PhD), Yonsei University, Seoul, South Korea; Centre for Chronic Disease Control, New Delhi, India (P Jeemon PhD); Centre for Control of Chronic Conditions (P Jeemon PhD), Public Health Foundation of India, Gurgaon, India (D K Lal MD, Prof S Zodpey PhD); Postgraduate Institute of Medical Education and Research, Chandigarh, India (Prof V Jha DM); Tianjin Centers for Disease Control and Prevention, Tianjin, China (G Jiang MD); Department of Health Development, Institute of Industrial Ecological Sciences, Department of Environmental Epidemiology, University of Occupational and Environmental Health, Kitakyushu, Japan (Y Jiang PhD); Department of Ophthalmology, Medical Faculty Mannheim, Ruprecht-Karls-University Heidelberg, Mannheim, Germany (Prof J B Jonas MD); University College Cork, Cork, Ireland (Z Kabir PhD); CSIR - Indian Institute of Toxicology Research, Lucknow, India (R Kamal MSc, C N Kesavachandran PhD); Department of Pulmonary Medicine, Zhongshan Hospital (J She MD), Fudan University, Shanghai, China (H Kan MD); Epidemiological and Statistical Methods Research Group, Helmholtz Centre for Infection Research, Braunschweig, Germany (A Karch MD); Hannover-Braunschweig Site, German Center for Infection Research, Braunschweig, Germany (A Karch MD); Center for Research in Health and Economics, Universitat Pompeu Fabra, Barcelona, Spain (D Karletsos MS); Oklahoma State University, Tulsa, OK, USA (A Kaul MD); School of Public Health (Prof N Kawakami MD), University of Tokyo, Tokyo, Japan (K Shibuya MD); Institut de recherche de l’hôpital de Monttfort, Ottawa, ON, Canada (J F Kayibanda PhD); University of California San Francisco, San Francisco, CA, USA (D S Kazi MD); Institute of Tropical and Infectious Diseases, Nairobi, Kenya (P N Keiyoro PhD); School of Continuing and Distance Education, Nairobi, Kenya (P N Keiyoro PhD); Swansea University, Swansea, UK (Prof A H Kemp PhD); South African Medical Research Council, Cape Town, South Africa (A P Kengne PhD, Prof C S Wiysonge PhD); Faculty of Health Sciences, Hatter Institute for Cardiovascular Research in Africa (Prof K Sliwa PhD), University of Cape Town, Cape Town, South Africa (A P Kengne PhD); Assuta Hospitals, Assuta Hashalom, Tel Aviv, Israel (Prof A Keren MD); Jordan University of Science and Technology, Irbid, Jordan (Prof Y S Khader ScD); Health Services Academy, Islamabad, Pakistan (E A Khan MPH); College of Medicine (Prof Y H Khang MD), Graduate School of Public Health (Prof S Won PhD), Seoul National University, Seoul, South Korea; Iranian Ministry of Health and Medical Education, Tehran, Iran (A Khosravi PhD); Ball State University, Muncie, IN, USA (J Khubchandani PhD); Southern University College, Skudai, Malaysia (Y J Kim PhD); Department of Preventive Cardiology, National Cerebral and Cardiovascular Center, Suita, Japan (Y Kokubo PhD); Center for Community Empowerment, Health Policy and Humanities, NIHRD, Jakarta, Indonesia (S Kosen MD); Sher-i-Kashmir Institute of Medical Sciences, Srinagar, India (Prof P A Koul MD); Research and Development Unit, Parc Sanitari Sant Joan de Deu (CIBERSAM), Barcelona, Spain (A Koyanagi MD); Oregon Health and Science University, Portland, OR, USA (S Krishnaswami MD); Department of Demography and Public Health Research Institute (Prof B Kuate Defo PhD), Department of Social and Preventive Medicine, School of Public Health (Prof B Kuate Defo PhD), University of Montreal, Montreal, QC, Canada; Institute of Public Health, Hacettepe University, Ankara, Turkey (B Kucuk Bicer PhD); Institute of Health Policy and Development Studies, National Institutes of Health, Manila, Philippines (Prof H Lam PhD); National Cancer Institute, Rockville, MD, USA (Q Lan PhD); Komfo Anokye Teaching Hospital, Kumasi, Ghana (D O Laryea MD); State University of New York, Albany, Rensselaer, NY, USA (R Leung PhD); San Francisco VA Medical Center, San Francisco, CA, USA (Y Li PhD); School of Medicine, Wayne State University, Detroit, MI, USA (Prof S E Lipshultz MD, Prof J D Wilkinson MD); Children’s Hospital of Michigan, Detroit, MI, USA (Prof S E Lipshultz MD); Rollins School of Public Health (E P Simard PhD), Emory University, Atlanta, GA, USA (Prof Y Liu PhD, Prof M R Phillips MD, Q Xiao MPH); Eastern Health Clinical School, Monash University, Fitzroy, VIC, Australia (B K Lloyd PhD); Turning Point, Eastern Health, Melbourne, VIC, Australia (B K Lloyd PhD); Aintree University Hospital National Health Service Foundation Trust, Liverpool, UK (Prof R Lunevicius PhD); School of Medicine (Prof R Lunevicius PhD), University of Liverpool, Liverpool, UK (D Pope PhD); Ministry of Health Singapore, Singapore, Singapore (S Ma PhD); Saw Swee Hock School of Public Health, National University of Singapore, Singapore, Singapore (S Ma PhD); Mansoura Faculty of Medicine, Mansoura, Egypt (H Magdy Abd El Razek MBBCH); Aswan University Hospital, Aswan Faculty of Medicine, Aswan, Egypt (M Magdy Abd El Razek MBBCh); Division of Population and Patient Health, King’s College London Dental Institute, London, UK (Prof W Marcenes PhD); Perelman School of Medicine (P A Meaney MD), University of Pennsylvania, Philadelphia, PA, USA (D J Margolis PhD); University of the East Ramon Magsaysay Memorial Medical Center, Quezon City, Philippines (M B Marzan MSc); Department of Health Sciences, University of York, York, UK (A J Mason-Jones PhD); Automotive Industry Development Centre Eastern Cape, Port Elizabeth, South Africa (T T Mazorodze MA); Children’s Hospital of Philadelphia, Philadelphia, PA, USA (P A Meaney MD); College of Medicine, Howard University, Washington, DC, USA (A Mehari MD); Janakpuri Superspecialty Hospital, New Delhi, India (Prof M M Mehndiratta DM); Department of Epidemiology and Biostatistics, Institute of Public Health (S M Woldeyohannes MPH), University of Gondar, Gondar, Ethiopia (A B Mekonnen MS, B A Tedla BS, G A Tessema MPH); Saudi Ministry of Health, Riyadh, Saudi Arabia (Prof Z A Memish MD); College of Medicine, Alfaisal University, Riyadh, Saudi Arabia (Prof Z A Memish MD); United Nations Population Fund, Lima, Peru (W Mendoza MD); Department of Neurology, Helsinki University Hospital, Helsinki, Finland (A Meretoja PhD); Helsinki University Hospital, Comprehensive Cancer Center, Breast Surgery Unit, Helsinki, Finland (T J Meretoja PhD); University of Helsinki, Helsinki, Finland (T J Meretoja PhD); Ifakara Health Institute, Bagamoyo, Tanzania (F A Mhimbira MS); Pacific Institute for Research & Evaluation, Calverton, MD, USA (T R Miller PhD); Centre for Population Health, Curtin University, Perth, WA, Australia (T R Miller PhD); University of Ottawa, Ottawa, ON, Canada (E J Mills PhD); Department of Medicine, Universiti Kebangsaan Malaysia Medical Center, Bandar Tun Razak, Malaysia (Prof N Mohamed Ibrahim MRCP); University of Salahaddin, Erbil, Iraq (K A Mohammad PhD); Neuroscience Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran (A Mohammadi PhD); Health Systems and Policy Research Unit, Ahmadu Bello University, Zaria, Nigeria (S Mohammed PhD); University of Papua New Guinea, Boroko, Papua New Guinea (G L D Mola DPH FRANCOG); Institute for Maternal and Child Health, IRCCS “Burlo Garofolo”, Trieste, Italy (L Monasta DSc, M Montico Msc, L Ronfani PhD); Bureau of International Health Cooperation, Manila City, Philippines (J D Monis MSc); University of North Texas, Denton, TX, USA (Prof A R Moore PhD); Department of Community Medicine, Gastrointestinal and Liver Disease Research Center, Iran University of Medical Sciences, Tehran, Iran (M MoradiLakeh MD); International Laboratory for Air Quality and Health (L Morawska PhD), Institute of Health and Biomedical Innovation (R E Norman PhD), Queensland University of Technology, Brisbane, QLD, Australia; National Center for Child Health and Development, Setagaya, Japan (R Mori PhD); Competence Center Mortality-Follow-Up of the German National Cohort (A Werdecker PhD), Federal Institute for Population Research, Wiesbaden, Germany (Prof U O Mueller PhD, R Westerman PhD); Indian Institute of Public Health (Prof G V S Murthy MD), Public Health Foundation of India, Gurgaon, India (D K Lal MD, Prof S Zodpey PhD); University of British Columbia, Vancouver, BC, Canada (S Murthy MD, F Pourmalek PhD); Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA, USA (Prof J B Nachega PhD); Public Health Dynamics Laboratory (A J Paternina Caicedo MD), University of Pittsburgh, Pittsburgh, PA, USA; Stellenbosch University, Cape Town, South Africa (Prof J B Nachega PhD, Prof S Seedat PhD, Prof C S Wiysonge PhD); Bloomberg School of Public Health (Prof J B Nachega PhD), Johns Hopkins University, Baltimore, MD, USA (B X Tran PhD); International Centre for Diarrhoeal Disease Research (icddr,b), Bangladesh, Dhaka, Bangladesh (A Naheed PhD); Azienda Ospedaliera Papa Giovanni XXIII, Bergamo, Italy (Prof L Naldi MD, Prof G Remuzzi MD); Ministry of Health, Suva, Fiji (D Nand MPH); Suraj Eye Institute, Nagpur, India (Prof V Nangia MD); School of Public Health, City University of New York, New York, NY, USA (D Nash PhD); School of Health Sciences, University of Tampere, Tampere, Finland (S Neupane PhD); Public Health England, London, UK (Prof J N Newton FRCP); Ministry of Health and Social Welfare, Dar es Salaam, Tanzania (F N Ngalesoni MSc); KEMRI - Wellcome Trust Research Program, Nairobi, Kenya (P Nguhiu BPharm); Institute for Global Health Innovations, Duy Tan University, Da Nang, Vietnam (Q L Nguyen MD); National Institute of Public Health, Japan, Saitama, Japan (M Nomura PhD); Makerere University, Kampala, Uganda (L Nyakarahuka MPH); Center for Research on Population and Health, Faculty of Health Sciences, American University of Beirut, Beirut, Lebanon (Prof C M Obermeyer DSc); University of Western Sydney, Sydney, NSW, Australia (F A Ogbo MPH); Department of Preventive Medicine, School of Medicine, Kyung Hee University, Seoul, South Korea (Prof I Oh PhD); Universidad Autonoma de Chile, Talca, Chile (Prof P R Olivares PhD); Center for Healthy Start Initiative, Lagos, Nigeria (B O Olusanya PhD, J O Olusanya MBA); Lira District Local Government, Lira Municipal Council, Uganda (J N Opio MPH); University of Arizona, Tucson, AZ, USA (Prof E Oren PhD); St Luke’s International University, Tokyo, Japan (E Ota PhD); North-West University, Mafikeng, South Africa (Prof A S Oyekale PhD); JSS Medical College, JSS University, Mysore, India (Prof Mahesh PA DNB); Department of Obstetrics & Gynecology (Prof N Papantoniou PhD), Attikon University Hospital, Athens, Greece (V Stathopoulou PhD); Department of Medical Humanities and Social Medicine, College of Medicine, Kosin University, Busan, South Korea (E Park PhD); California Air Resources Board, Sacramento, CA, USA (H Park PhD); Universidad de Cartagena, Cartagena, Colombia (A J Paternina Caicedo MD); Department of Community Health Sciences, University of Calgary, Calgary, AB, Canada (Prof S B Patten PhD); All India Institute of Medical Sciences, New Delhi, India (V K Paul MD, A Roy DM, R Sagar MD, M Satpathy PhD); REQUIMTE/LAQV, Laboratório de Farmacognosia, Departamento de Química, Faculdade de Farmácia, Universidade do Porto, Porto, Portugal (Prof D M Pereira PhD); IRCCS - Istituto di Ricerche Farmacologiche Mario Negri, Bergamo, Italy (N Perico MD, Prof G Remuzzi MD); Flinders University, Adelaide, SA, Australia (Prof K Pesudovs PhD, F H Tesfay MPH); Health Metrics Unit, Gothenburg, Sweden (Prof M Petzold PhD); University of the Witwatersrand, Johannesburg, South Africa (Prof M Petzold PhD); Shanghai Jiao Tong University School of Medicine, Shanghai, China (Prof M R Phillips MD); Durban University of Technology, Durban, South Africa (J D Pillay PhD); Department of Public Health, Erasmus MC, University Medical Center Rotterdam, Rotterdam, Netherlands (S Polinder PhD); Department of Community Medicine, School of Medicine, Alborz University of Medical Sciences, Karaj, Iran (M Qorbani PhD); Contech School of Public Health, Lahore, Pakistan (A Rafay MS); Research and Evaluation Division, BRAC, Dhaka, Bangladesh (M Rahman PhD); Hamad Medical Corporation, Doha, Qatar (S U Rahman FCPS); Society for Health and Demographic Surveillance, Suri, India (R K Rai MPH); Wonju College of Medicine (C L Ranabhat PhD), Institute for Poverty Alleviation and International Development (C L Ranabhat PhD), Yonsei University, Wonju, South Korea; Schizophrenia Research Foundation, Chennai, India (T Rangaswamy FRCPsych); Diabetes Research Society, Hyderabad, India (Prof P V Rao MD); Diabetes Research Center, Hyderabad, India (Prof P V Rao MD); Suez Canal University, Ismailia, Egypt (Prof A H Refaat PhD); Department of Biomedical and Clinical Sciences L Sacco, University of Milan, Milan, Italy (Prof G Remuzzi MD); Brien Holden Vision Institute, University of New South Wales, Sydney, NSW, Australia (Prof S Resnikoff MD); ISGlobal, Instituto de Salud Global de Barcelona, Barcelona, Spain (D Rojas-Rueda PhD); Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran (G Roshandel PhD); Muhimbili University of Health and Allied Sciences, Dar es Salaam, Tanzania (G M Ruhago PhD, B F Sunguya MSc); Development Research and Projects Center, Abuja, Nigeria (M M Saleh MPH); Marshall University J Edwards School of Medicine, Huntington, WV, USA (J R Sanabria MD); Case Western Reserve University, Cleveland, OH, USA (J R Sanabria MD); IIS-Fundacion Jimenez Diaz, Madrid, Spain (M D Sanchez-Niño PhD); Universidad Ciencias Aplicadas y Ambientales, Bogotá, Colombia (R Sarmiento-Suarez MPH); University of KwaZulu-Natal, Durban, South Africa (Prof B Sartorius PhD); Marshall University, Huntington, WV, USA (M Sawhney PhD); Novartis Turkey, Istanbul, Turkey (M I Saylan PhD); Federal University of Santa Catarina, Florianópolis, Brazil (I J C Schneider PhD, D A S Silva PhD); National Institute of Public Health, Morelos, Mexico (Prof E E Servan-Mori MSc); Independent Consultant, Karachi, Pakistan (M A Shaikh MD); Indian Institute of Technology Ropar, Roopnagar, India (R Sharma MA); Research Institute at Nationwide Children’s Hospital, Columbus, OH, USA (J Shen PhD); Department of Public Health Science, Graduate School (Prof M Shin PhD), Department of Preventive Medicine, College of Medicine (S Yoon PhD), Korea University, Seoul, South Korea; Finnish Institute of Occupational Health, Helsinki, Finland (R Shiri PhD); Washington State University, Spokane, WA, USA (K Shishani PhD); Faculty of Health and Life Sciences, Northumbria University, Newcastle upon Tyne, UK (I Shiue PhD); Alzheimer Scotland Dementia Research Centre, University of Edinburgh, Edinburgh, UK (I Shiue PhD); Reykjavik University, Reykjavik, Iceland (I D Sigfusdottir PhD); Brasília University, Brasília, Brazil (D G A Silveira MD); Feinberg School of Medicine (J I Silverberg MD), Department of Preventive Medicine (Y Yano MD), Northwestern University, Chicago, IL, USA; Department of Medicine, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India (O P Singh PhD); Institute for Human Development, New Delhi, India (P K Singh PhD); Asthma Bhawan, Jaipur, India (V Singh MD); Dartmouth College, Lebanon, NH, USA (S Soneji PhD); Instituto de Investigación Hospital Universitario de la Princesa, Universidad Autónoma de Madrid, Cátedra UAM-Linde, Palma de Mallorca, Spain (Prof J B Soriano PhD); Department of Clinical Neurological Sciences, Western University, London, ON, Canada (L A Sposato MD); Department of Community Medicine, International Medical University, Kuala Lumpur, Malaysia (C T Sreeramareddy MD); Alexandra General Hospital of Athens, Athens, Greece (K Stroumpoulis PhD); Centre Hospitalier Public du Cotentin, Cherbourg, France (K Stroumpoulis PhD); Indian Council of Medical Research, New Delhi, India (S Swaminathan MD); Departments of Criminology, Law & Society, Sociology, and Public Health, University of California, Irvine, Irvine, CA, USA (Prof B L Sykes PhD); Department of Medicine, University of Valencia/CIBERSAM, Valencia, Spain (Prof R Tabarés-Seisdedos PhD); School of Social Work, University of Illinois at Urbana-Champaign, Champaign, IL, USA (K M Tabb PhD); Ministry of Health, MINSANTE, Yaounde, Cameroon (R T Talongwa MHE); Westchester Medical Center, Valhalla, NY, USA (M Tavakkoli MD); Department of Biology, Colgate University, Hamilton, NY, USA (B Taye PhD); James Cook University, Cairns, QLD, Australia (B A Tedla BS); Arba Minch University, Arba Minch, Ethiopia (A Y Endries MPH, G Temam Shifa MPH); Department of Anesthesiology, University of Virginia, Charlottesville, VA, USA (A S Terkawi MD); Outcomes Research Consortium, Cleveland Clinic, Cleveland, OH, USA (A S Terkawi MD); Adaptive Knowledge Management, Victoria, BC, Canada (A J Thomson PhD); WorldFish, Penang, Malaysia (A L Thorne-Lyman ScD); National Center for Child Health and Development, Tokyo, Japan (R Tobe-Gai PhD); Faculty of Health Sciences, Jagiellonian University, Kraków, Poland (R Topor-Madry PhD); Faculty of Health Sciences, Wroclaw Medical University, Wroclaw, Poland (R Topor-Madry PhD); Le Bonheur Children’s Hospital, Memphis, TN, USA (Prof J A Towbin MD); University of Tennessee Health Science Center, Memphis, TN, USA (Prof J A Towbin MD); St Jude Children’s Research Hospital, Memphis, TN, USA (Prof J A Towbin MD); Hanoi Medical University, Hanoi, Vietnam (B X Tran PhD); Department of Population Sciences and Development, Faculty of Economics and Management, University of Kinshasa, Kinshasa, Democratic Republic of the Congo (Z Tsala Dimbuene PhD); Parc Sanitari Sant Joan de Déu, Fundació Sant Joan de Déu, Universitat de Barcelona, CIBERSAM, Barcelona, Spain (S Tyrovolas PhD); Department of Internal Medicine, Federal Teaching Hospital, Abakaliki, Nigeria (K N Ukwaja MD); Warwick Medical School, University of Warwick, Coventry, UK (O A Uthman PhD); UKK Institute for Health Promotion Research, Tampere, Finland (Prof T Vasankari PhD); Raffles Neuroscience Centre, Raffles Hospital, Singapore, Singapore (N Venketasubramanian FRCP); University of Bologna, Bologna, Italy (Prof F S Violante MD); Federal Research Institute for Health Organization and Informatics, Moscow, Russia (S K Vladimirov PhD); National Research University Higher School of Economics, Moscow, Russia (Prof V V Vlassov MD); McGill University, Montreal, QC, Canada (S Weichenthal PhD); Department of Research, Cancer Registry of Norway, Institute of Population-Based Cancer Research, Oslo, Norway (E Weiderpass PhD); Department of Community Medicine, Faculty of Health Sciences, University of Tromsø, The Arctic University of Norway, Tromsø, Norway (E Weiderpass PhD); Genetic Epidemiology Group, Folkhälsan Research Center, Helsinki, Finland (E Weiderpass PhD); Royal Children’s Hospital, Melbourne, VIC, Australia (R G Weintraub MBBS); German National Cohort Consortium, Heidelberg, Germany (R Westerman PhD); Western Health, Footscray, VIC, Australia (Prof T Wijeratne MD); Children’s Hospital of Michigan, Detroit, MI, USA (Prof J D Wilkinson MD); National Institute for Health Research Comprehensive Biomedical Research Centre, Guy’s & St Thomas’ NHS Foundation Trust and King’s College London, London, UK (Prof C D Wolfe MD); St Paul’s Hospital, Millennium Medical College, Addis Ababa, Ethiopia (M Wubshet PhD); Department of Neurology, Jinling Hospital, Nanjing University School of Medicine, Nanjing, China (Prof G Xu PhD); Discipline of Public Health Medicine, School of Nursing and Public Health, University of KwaZulu Natal, Durban, South Africa (B Yakob PhD); University of Zurich, Zurich, Switzerland (H G Yebyo MS); Social Work and Social Administration Department and The Hong Kong Jockey Club Centre for Suicide Research and Prevention, University of Hong Kong, Hong Kong, China (Prof P Yip PhD); Department of Biostatistics, University of Hong Kong, Hong Kong, China; Department of Biostatistics, School of Public Health, Kyoto University, Kyoto, Japan (N Yonemoto MPH); Jackson State University, Jackson, MS, USA (Prof M Z Younis DrPH); Department of Epidemiology and Biostatistics, School of Public Health (Prof C Yu PhD), Global Health Institute (Prof C Yu PhD), Wuhan University, Wuhan, China; University Hospital, Setif, Algeria (Prof Z Zaidi PhD); Faculty of Medicine, Mansoura University, Mansoura, Egypt (Prof M E Zaki PhD); Leibniz Institute for Prevention Research and Epidemiology, Bremen, Germany (Prof H Zeeb PhD); Chongqing Medical University, Chongqing, China (Prof Y Zhao MSc); and Red Cross War Memorial Children’s Hospital, Cape Town, South Africa (L J Zuhlke PhD).
Footnotes
Contributors
Nicholas J Kassebaum, Caitlyn Steiner, Christopher J L Murray, Alan D Lopez, and Rafael Lozano prepared the first draft. Christopher J L Murray and Alan D Lopez conceived the study and provided overall guidance. All other authors provided data, developed models, reviewed results, initiated modeling infrastructure, and/or reviewed and contributed to the report.
Declaration of interests
Itamar S Santos reports grants from FAPESP (Brazilian public agency), outside the submitted work. Carl Abelardo T Antonio reports grants, personal fees and non-financial support from Johnson & Johnson (Philippines), Inc, outside the submitted work. Cyrus Cooper reports other from Alliance for Better Bone Health, other from Amgen, other from Eli Lilly, other from GSK, other from Medtronic, other from Merck, other from Novartis, other from Pfizer, other from Roche, other from Servier, outside the submitted work. Walter Mendoza is currently employed by the Peru Country Office of the United Nations Population Fund, an institution which does not necessarily endorse this study. Katherine B Gibney received the NHMRC Gustav Nossal Postgraduate Scholarship sponsored by CSL in 2012, an award peer reviewed through the standard NHMRC peer review process; CSL does not play any part in the selection of the awardee. Manisha Dubey has received financial support from University Grants Commission, New Delhi, India for pursuing a PhD. Shireen Sindi has received postdoctoral funding from the Fonds de la recherche en santé du Québec (FRSQ), including its renewal. Ashish Awasthi has received financial support from Indian Council of Medical Research, New Delhi, India for pursuing a PhD. Jasvinder A Singh has received research grants from Takeda and Savient and consultant fees from Savient, Takeda, Regeneron, Merz, Iroko, Bioiberica, Crealta and Allergan pharmaceuticals, WebMD, UBM LLC and the American College of Rheumatology; he serves as the principal investigator for an investigator-initiated study funded by Horizon pharmaceuticals through a grant to DINORA, Inc, a 501 (c)(3) entity; is a member of the executive of OMERACT, an organization that develops outcome measures in rheumatology and receives arms-length funding from 36 companies; a member of the American College of Rheumatology’s (ACR) Annual Meeting Planning Committee (AMPC); Chair of the ACR Meet-the-Professor, Workshop and Study Group Subcommittee; and a member of the Veterans Affairs Rheumatology Field Advisory Committee. Rafael Tabarés-Seisdedos and Ferrán Catalá-López are supported in part by grant PROMETEOII/2015/021 from Generalitat Valenciana, and Rafael Tabarés-Seisdedos is supported by the national grant PI14/00894 from ISCIII-FEDER. Ai Koyanagi’s work is supported by the Miguel Servet contract financed by the CP13/00150 and PI15/00862 projects, integrated into the National R + D + I and funded by the ISCIII - General Branch Evaluation and Promotion of Health Research - and the European Regional Development Fund (ERDF-FEDER). Donal Bisanzio is supported by Bill and Melinda Gates Foundation (#OPP1068048). Kebede Deribe is supported by a Wellcome Trust Fellowship in Public Health and Tropical Medicine (grant number 099876). Thomas Fürst has received financial support from the Swiss National Science Foundation (SNSF; project no. P300P3-154634). Jost B Jonas reports personal fees from Consultant for Mundipharma Co (Cambridge, UK); other from patent application with University of Heidelberg (Heidelberg, Germany) (Title: Agents for use in the therapeutic or prophylactic treatment of myopia or hyperopia; Europäische Patentanmeldung 15 000 771.4), and other from patent holder with Biocompatibles UK Ltd. (Franham, Surrey, UK) (Title: Treatment of eye diseases using encapsulated cells encoding and secreting neuroprotective factor and / or anti-angiogenic factor; Patent number: 20120263794), outside the submitted work. Rodrigo Sarmiento-Suarez has received institutional support from Universidad de Ciencias Aplicadas y Ambientales, UDCA, Bogotá Colombia. Stefanos Tyrovolas’s work is supported by the Foundation for Education and European Culture (IPEP), the Sara Borrell postdoctoral programme (reference no. CD15/00019 from the Instituto de Salud Carlos III (ISCIII - Spain) and the Fondos Europeo de Desarrollo Regional (FEDER). Beatriz Paulina Ayala Quintanilla would like to acknowledge the Institutional support of PRONABEC (National Program of Scholarship and Educational Loan), provided by the Peruvian Government, while studying for her doctoral course at the Judith Lumley Centre of La Trobe University funded by PRONABEC. Miia Kivipelto receives research support from the Academy of Finland, the Swedish Research Council, Alzheimerfonden, Alzheimer’s Research & Prevention Foundation, Center for Innovative Medicine (CIMED) at Karolinska Institutet South Campus, AXA Research Fund and the Sheika Salama Bint Hamdan Alnahyan Foundation. Juan Jesus Carrero would like to acknowledge the following source of funding: The Swedish Heart and Lung Foundation (grant number 20150497). Charles D A Wolfe’s research was funded/supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. The other authors declare no competing interests.
References
- 1.United Nations. Sustainable Development Knowledge Platform; [accessed March 22, 2016]. Transforming our world: the 2030 Agenda for Sustainable Development. https://sustainabledevelopment.un.org/post2015/transformingourworld. [Google Scholar]
- 2.Sachs JD. From Millennium Development Goals to Sustainable Development Goals. Lancet. 2012;379:2206–11. doi: 10.1016/S0140-6736(12)60685-0. [DOI] [PubMed] [Google Scholar]
- 3.Griggs D, Stafford-Smith M, Gaffney O, et al. Policy: sustainable development goals for people and planet. Nature. 2013;495:305–07. doi: 10.1038/495305a. [DOI] [PubMed] [Google Scholar]
- 4.Griggs D, Stafford Smith M, Rockström J, et al. An integrated framework for sustainable development goals. Ecol Soc. 2014;19:49. [Google Scholar]
- 5.WHO. Global Strategy for Women’s, Children’s and Adolescents’ Health, 2016–2030. [accessed April 26, 2016]; http://www.who.int/life-course/partners/global-strategy/global-strategy-2016-2030/en/
- 6.Langer A, Horton R, Chalamilla G. A manifesto for maternal health post-2015. Lancet. 2013;381:601–02. doi: 10.1016/S0140-6736(13)60259-7. [DOI] [PubMed] [Google Scholar]
- 7.Yamin AE, Boulanger VM. Embedding sexual and reproductive health and rights in a transformational development framework: lessons learned from the MDG targets and indicators. Reprod Health Matters. 2013;21:74–85. doi: 10.1016/S0968-8080(13)42727-1. [DOI] [PubMed] [Google Scholar]
- 8.Hogan MC, Foreman KJ, Naghavi M, et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2010;375:1609–23. doi: 10.1016/S0140-6736(10)60518-1. [DOI] [PubMed] [Google Scholar]
- 9.Lozano R, Wang H, Foreman KJ, et al. Progress towards Millennium Development Goals 4 and 5 on maternal and child mortality: an updated systematic analysis. Lancet. 2011;378:1139–65. doi: 10.1016/S0140-6736(11)61337-8. [DOI] [PubMed] [Google Scholar]
- 10.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:980–1004. doi: 10.1016/S0140-6736(14)60696-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO. Trends in Maternal Mortality: 1990 to 2013. [accessed March 22, 2016]; http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2013/en/
- 12.WHO. Trends in maternal mortality: 1990 to 2015. [accessed March 22, 2016]; http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/
- 13.WHO. Trends in maternal mortality: 1990 to 2010. [accessed March 22, 2016]; http://www.who.int/reproductivehealth/publications/monitoring/9789241503631/en/
- 14.WHO. Trends in maternal mortality: 1990 to 2008. [accessed March 22, 2016]; http://www.who.int/reproductivehealth/publications/monitoring/9789241500265/en/
- 15.Attaran A. An immeasurable crisis? a criticism of the millennium development goals and why they cannot be measured. PLoS Med. 2005;2:e318. doi: 10.1371/journal.pmed.0020318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horton R. Maternal mortality: surprise, hope, and urgent action. Lancet. 2010;375:1581–82. doi: 10.1016/S0140-6736(10)60547-8. [DOI] [PubMed] [Google Scholar]
- 17.Wang H, Dwyer-Lindgren L, Lofgren KT, et al. Age-specific and sex-specific mortality in 187 countries, 1970–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2071–94. doi: 10.1016/S0140-6736(12)61719-X. [DOI] [PubMed] [Google Scholar]
- 18.Newton JN, Briggs ADM, Murray CJL, et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2257–74. doi: 10.1016/S0140-6736(15)00195-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–72. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
- 20.GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age–sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gómez-Dantés H, Fullman N, Lamadrid-Figueroa H, et al. Dissonant health transition in the states of Mexico, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2016 doi: 10.1016/S0140-6736(16)31773-1. published online Oct 5. [DOI] [PubMed] [Google Scholar]
- 22.Public Health England. From evidence into action: opportunities to protect and improve the nation’s health. London, UK: Public Health England; 2014. [Google Scholar]
- 23.Bhalla K, Harrison JE. GBD-2010 overestimates deaths from road injuries in OECD countries: new methods perform poorly. Int J Epidemiol. 2015;44:1648–56. doi: 10.1093/ije/dyv019. [DOI] [PubMed] [Google Scholar]
- 24.Rudan I, Chan KY. Global health metrics needs collaboration and competition. Lancet. 2015;385:92–4. doi: 10.1016/S0140-6736(14)62006-7. [DOI] [PubMed] [Google Scholar]
- 25.Global Burden of Disease Study 2013 Collaborators. Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015 doi: 10.1016/S0140-6736(15)60692-4. published online June 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The GATHER Working Group. Guidelines for Accurate and Transparent Health Estimates Reporting: The GATHER statement. Lancet. 2016 doi: 10.1016/S0140-6736(16)30388-9. published online June 28. [DOI] [PubMed] [Google Scholar]
- 27.Gakidou E, King G. Death by survey: estimating adult mortality without selection bias from sibling survival data. Demography. 2006;43:569–85. doi: 10.1353/dem.2006.0024. [DOI] [PubMed] [Google Scholar]
- 28.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baeten JM, Bukusi EA, Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am J Public Health. 2001;91:436–40. doi: 10.2105/ajph.91.3.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sebire NJ, Jolly M, Harris JP, et al. Maternal obesity and pregnancy outcome: a study of 287 213 pregnancies in London. Int J Obes Relat Metab Disord. 2001;25:1175. doi: 10.1038/sj.ijo.0801670. [DOI] [PubMed] [Google Scholar]
- 31.Price JI, Bohara AK. Maternal health care amid political unrest: the effect of armed conflict on antenatal care utilization in Nepal. Health Policy Plan. 2013;28:309–19. doi: 10.1093/heapol/czs062. [DOI] [PubMed] [Google Scholar]
- 32.Chi PC, Bulage P, Urdal H, Sundby J. A qualitative study exploring the determinants of maternal health service uptake in post-conflict Burundi and Northern Uganda. BMC Pregnancy Childbirth. 2015;15:18. doi: 10.1186/s12884-015-0449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mony PK, Krishnamurthy J, Thomas A, et al. Availability and distribution of emergency obstetric care services in Karnataka State, South India: access and equity considerations. PLoS One. 2013;8:e64126. doi: 10.1371/journal.pone.0064126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abouchadi S, Belghiti Alaoui A, Meski FZ, De Brouwere V. Implementing a maternal mortality surveillance system in Morocco—challenges and opportunities. Trop Med Int Health. 2013;18:357–65. doi: 10.1111/tmi.12053. [DOI] [PubMed] [Google Scholar]
- 35.National Center for Health Statistics. Birth Data. [accessed March 27, 2016]; http://www.cdc.gov/nchs/births.htm.
- 36.Ruppert D, Matteson DS. Statistics and Data Analysis for Financial Engineering. New York, NY: Springer New York; 2015. Return calculations; pp. 1–35. Chapter 1. [Google Scholar]
- 37.United Nations Development Programme. Human development report 2015. [S.l.] United Nations; 2016. [Google Scholar]
- 38.Padmanaban P, Raman PS, Mavalankar DV. Innovations and challenges in reducing maternal mortality in Tamil Nadu, India. J Health Popul Nutr. 2009;27:202–19. doi: 10.3329/jhpn.v27i2.3364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dieleman J, Murray CML, Haakenstad A. Financing Global Health 2014: Shifts in Funding as the MDG Era Closes. [accessed July 1, 2015]; http://www.healthdata.org/policy-report/financing-global-health-2014-shifts-funding-mdg-era-closes.
- 40.Mavalankar DV, Vora KS, Ramani KV, Raman P, Sharma B, Upadhyaya M. Maternal health in Gujarat, India: a case study. J Health Popul Nutr. 2009;27:235–48. doi: 10.3329/jhpn.v27i2.3366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Randive B, San Sebastian M, De Costa A, Lindholm L. Inequalities in institutional delivery uptake and maternal mortality reduction in the context of cash incentive program, Janani Suraksha Yojana: results from nine states in India. Soc Sci Med. 2014;123:1–6. doi: 10.1016/j.socscimed.2014.10.042. [DOI] [PubMed] [Google Scholar]
- 42.Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. Lancet. 2010;375:2009–23. doi: 10.1016/S0140-6736(10)60744-1. [DOI] [PubMed] [Google Scholar]
- 43.Barber SL, Gertler PJ. Empowering women to obtain high quality care: evidence from an evaluation of Mexico’s conditional cash transfer programme. Health Policy Plan. 2009;24:18–25. doi: 10.1093/heapol/czn039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Glassman A, Duran D, Fleisher L, et al. Impact of conditional cash transfers on maternal and newborn health. J Health Popul Nutr. 2013;31:S48–66. [PubMed] [Google Scholar]
- 45.Givertz MM. Peripartum Cardiomyopathy. Circulation. 2013;127:e622–26. doi: 10.1161/CIRCULATIONAHA.113.001851. [DOI] [PubMed] [Google Scholar]
- 46.Tepper NK, Boulet SL, Whiteman MK, et al. Postpartum venous thromboembolism: incidence and risk factors. Obstet Gynecol. 2014;123:987–96. doi: 10.1097/AOG.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 47.Rowe AK, de Savigny D, Lanata CF, Victora CG. How can we achieve and maintain high-quality performance of health workers in low-resource settings? Lancet. 2005;366:1026–35. doi: 10.1016/S0140-6736(05)67028-6. [DOI] [PubMed] [Google Scholar]
- 48.Campbell OM, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet. 2006;368:1284–99. doi: 10.1016/S0140-6736(06)69381-1. [DOI] [PubMed] [Google Scholar]
- 49.Ahmed S, Li Q, Liu L, Tsui AO. Maternal deaths averted by contraceptive use: an analysis of 172 countries. Lancet. 2012;380:111–25. doi: 10.1016/S0140-6736(12)60478-4. [DOI] [PubMed] [Google Scholar]
- 50.Bollini P, Quack-Lötscher K. Guidelines-based indicators to measure quality of antenatal care. J Eval Clin Pract. 2013;19:1060–66. doi: 10.1111/jep.12027. [DOI] [PubMed] [Google Scholar]
- 51.Bhutta ZA, Ahmed T, Black RE, et al. What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371:417–40. doi: 10.1016/S0140-6736(07)61693-6. [DOI] [PubMed] [Google Scholar]
- 52.Olsen ØE, Ndeki S, Norheim OF. Human resources for emergency obstetric care in northern Tanzania: distribution of quantity or quality? Hum Resour Health. 2005;3:5. doi: 10.1186/1478-4491-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dogba M, Fournier P. Human resources and the quality of emergency obstetric care in developing countries: a systematic review of the literature. Hum Resour Health. 2009;7:7. doi: 10.1186/1478-4491-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hofmeyr GJ, Haws RA, Bergström S, et al. Obstetric care in low-resource settings: what, who, and how to overcome challenges to scale up? Int J Gynaecol Obstet. 2009;107:S21–44. doi: 10.1016/j.ijgo.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 55.Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125:5–12. doi: 10.1097/AOG.0000000000000564. [DOI] [PubMed] [Google Scholar]
- 56.Sliwa K, Mayosi BM. Recent advances in the epidemiology, pathogenesis and prognosis of acute heart failure and cardiomyopathy in Africa. Heart. 2013;99:1317–22. doi: 10.1136/heartjnl-2013-303592. [DOI] [PubMed] [Google Scholar]
- 57.Ryder RW, Nsuami M, Nsa W, et al. Mortality in HIV-1-seropositive women, their spouses and their newly born children during 36 months of follow-up in Kinshasa, Zaïre. AIDS Lond Engl. 1994;8:667–72. doi: 10.1097/00002030-199405000-00014. [DOI] [PubMed] [Google Scholar]
- 58.Zvandasara P, Hargrove JW, Ntozini R, et al. Mortality and morbidity among postpartum HIV-positive and HIV-negative women in Zimbabwe: risk factors, causes, and impact of single-dose postpartum vitamin A supplementation. J Acquir Immune Defic Syndr 1999. 2006;43:107–16. doi: 10.1097/01.qai.0000229015.77569.c7. [DOI] [PubMed] [Google Scholar]
- 59.Høj L, da Silva D, Hedegaard K, Sandström A, Aaby P. Maternal mortality: only 42 days? BJOG. 2003;110:995–1000. doi: 10.1016/s1470-0328(03)03907-7. [DOI] [PubMed] [Google Scholar]
- 60.Andersen BR, Westergaard HB, Bødker B, Weber T, Møller M, Sørensen JL. Maternal mortality in Denmark, 1985–1994. Eur J Obstet Gynecol Reprod Biol. 2009;142:124–28. doi: 10.1016/j.ejogrb.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 61.Lamadrid-Figueroa H, Montoya A, Fritz J, Olvera M, Torres LM, Lozano R. Towards an inclusive and evidence-based definition of the maternal mortality ratio: an analysis of the distribution of time after delivery of maternal deaths in Mexico, 2010–2013. PLoS One. 2016;11:e0157495. doi: 10.1371/journal.pone.0157495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Horon IL, Cheng D. Effectiveness of pregnancy check boxes on death certificates in identifying pregnancy-associated mortality. Public Health Rep. 2011;126:195–200. doi: 10.1177/003335491112600210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387:462–74. doi: 10.1016/S0140-6736(15)00838-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Alkema L, Zhang S, Chou D, et al. A Bayesian approach to the global estimation of maternal mortality. [accessed June 16, 2016];ArXiv151103330 Stat. 2015 published online Nov 10. http://arxiv.org/abs/1511.03330. [Google Scholar]
- 65.Kassebaum NJ, Lopez AD, Murray CJL, Lozano R. A comparison of maternal mortality estimates from GBD 2013 and WHO. Lancet. 2014;384:2209–10. doi: 10.1016/S0140-6736(14)62421-1. [DOI] [PubMed] [Google Scholar]
- 66.Government of India Ministry of Home Affairs. Census of India: Medical Certification of Cause of Death. [accessed April 3, 2016]; http://www.censusindia.gov.in/2011-common/mccd.html.
- 67.Registrar General of India. India Survey of Causes of Death. New Delhi: Government of India; 1998. 1972, 1979–1986, 1988–1989. [Google Scholar]
- 68.Kassebaum NJ, Wang H, Lopez AD, Murray CJL, Lozano R. Maternal mortality estimates–authors’ reply. Lancet. 2014;3844:2211–12. doi: 10.1016/S0140-6736(14)62425-9. [DOI] [PubMed] [Google Scholar]
- 69.Masquelier B. Adult mortality from sibling survival data: A reappraisal of selection biases. Demography. 2013;50:207–28. doi: 10.1007/s13524-012-0149-1. [DOI] [PubMed] [Google Scholar]
- 70.Rojas-Suarez J, Paternina-Caicedo A, Cuevas L, et al. Maternal mortality due to pandemic influenza A H1N1 2009 virus in Colombia. J Perinat Med. 2014;42:19–26. doi: 10.1515/jpm-2013-0140. [DOI] [PubMed] [Google Scholar]
- 71.Dede FS, Celen S, Bilgin S, et al. Maternal deaths associated with H1N1 influenza virus infection in Turkey: a whole-of-population report. BJOG. 2011;118:1216–22. doi: 10.1111/j.1471-0528.2011.03002.x. [DOI] [PubMed] [Google Scholar]
- 72.Fatusic Z, Kurjak A, Grgic G, Tulumovic A. The influence of the war on perinatal and maternal mortality in Bosnia and Herzegovina. J Matern Fetal Neonatal Med. 2005;18:259–63. doi: 10.1080/147670500198501. [DOI] [PubMed] [Google Scholar]
- 73.Witter S, Adjei S, Armar-Klemesu M, Graham W. Providing free maternal health care: ten lessons from an evaluation of the national delivery exemption policy in Ghana. Glob Health Action. 2009;2 doi: 10.3402/gha.v2i0.1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. 2007;370:1358–69. doi: 10.1016/S0140-6736(07)61578-5. [DOI] [PubMed] [Google Scholar]
- 75.Fournier P, Dumont A, Tourigny C, Dunkley G, Dramé S. Improved access to comprehensive emergency obstetric care and its effect on institutional maternal mortality in rural Mali. Bull World Health Organ. 2009;87:30–38. doi: 10.2471/BLT.07.047076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Srofenyoh E, Ivester T, Engmann C, Olufolabi A, Bookman L, Owen M. Advancing obstetric and neonatal care in a regional hospital in Ghana via continuous quality improvement. Int J Gynaecol Obstet. 2012;116:17–21. doi: 10.1016/j.ijgo.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 77.Islam MT, Haque YA, Waxman R, Bhuiyan AB. Implementation of emergency obstetric care training in Bangladesh: lessons learned. Reprod Health Matters. 2006;14:61–72. doi: 10.1016/S0968-8080(06)27229-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.