Abstract
Hypothesis
Changes in the weather influence symptom severity in Ménière’s disease (MD).
Background
MD is an unpredictable condition that significantly impacts on quality of life. It is suggested that fluctuations in the weather, especially atmospheric pressure may influence the symptoms of MD. However, to date, limited research has investigated the impact of the weather on MD.
Methods
In a longitudinal study, a mobile phone application collected data from 397 individuals (277 females and 120 males with an average age of 50 yr) from the UK reporting consultant-diagnosed MD. Daily symptoms (vertigo, aural fullness, tinnitus, hearing loss, and attack prevalence) and GPS locations were collected; these data were linked with Met Office weather data (including atmospheric pressure, humidity, temperature, visibility, and wind speed).
Results
Symptom severity and attack prevalence were reduced on days when atmospheric pressure was higher. When atmospheric pressure was below 1,013 hectopascals, the risk of an attack was 1.30 (95% confidence interval: 1.10, 1.54); when the humidity was above 90%, the risk of an attack was 1.26 (95% confidence interval 1.06, 1.49).
Conclusion
This study provides the strongest evidence to date that changes in atmospheric pressure and humidity are associated with symptom exacerbation in MD. Improving our understanding of the role of weather and other environmental triggers in Ménière’s may reduce the uncertainty associated with living with this condition, significantly contributing to improved quality of life.
Keywords: e-health, Longitudinal, Ménière’s, Weather
Ménière’s disease (MD) is an inner ear disorder that is chronic, progressive, and affects both the balance and hearing functions of the inner ear (1,2). The symptoms of MD include: hearing loss, vertigo, and tinnitus, often accompanied by aural fullness (1,3). Each symptom individually and in combination can detrimentally impact on mental health and wellbeing (4). MD has a prevalence of between 0.08 and 0.50% (2,5,6), with the highest prevalence noted in a population-based study in Finland (6). MD is estimated economic cost between £552.5 and £629.3 million per annum in the UK (7).
MD is experienced as a debilitating unpredictable disease; and is associated with high levels of psychosocial comorbidity and significantly reduced quality of life among diagnosed individuals (8). Currently, there is no known cure for MD, drug treatments are mainly targeted at symptom control, and surgical options are controversial with inconsistent results and few high-quality randomized trials into effectiveness (9). Therefore, significant emphasis is placed on self-management, with patients expected to identify and avoid individual triggers where possible. At present, evidence for the triggers of MD attacks and symptom spikes is limited, with at best anecdotal evidence suggesting atmospheric pressure, specific dietary components (e.g., salt, caffeine, aspartame, and alcohol) and stress as potential triggers (10). Recent qualitative research has identified a number of physiological, environmental, and psychological factors patients believe to be associated with either vertigo or aural fullness (10).
Atmospheric pressure is considered to be a possible trigger for spikes in MD symptoms and attacks (11), as has been observed with other diseases including headache (12) and migraine (13). Anecdotal evidence suggests that patients with MD are particularly sensitive to low frequency pressure changes, including weather fronts and windmills (14). However, further research is needed to understand if and how the weather may be associated with triggering attacks and exacerbating the individual symptoms of MD.
To investigate the role of weather on the symptoms of MD, we developed a mobile phone application, known as the “Ménière’s Monitor” (www.menieresmonitor.com), to allow people with MD to monitor their symptoms on a daily basis. In addition, with their permission, this application captures an individual’s GPS location data at the time when they use the app. Through collaborations with the Met Office, associations between reported MD symptoms and the weather were investigated. This study aimed to investigate if weather variables were associated with MD symptom severity and overall attack frequency.
Methods
Ménière’s Monitor App
This mobile phone application was designed by collaboration between researchers at the University of Exeter Medical School, patients with MD and Buzz Interactive (http://www.buzzinteractive.co.uk/). The app was designed to enable participants to monitor the main symptoms of MD on a daily basis. Individuals were recruited from a range of sources, including the Ménière’s Society (newsletter, website, and social media), Ménière’s online forums, and via word of mouth in ear, nose, and throat (ENT) clinics. When individuals signed up to the free app, they were asked a range of demographic questions and questions about their MD (Supplementary Table 1, http://links.lww.com/MAO/A480).
On a daily basis, participants were then asked to rate their vertigo, aural fullness, tinnitus, and hearing on a scale from 0 to 10. Participants were also able to record whether they considered themselves to have had an “attack” (defined as “incapacitated by their symptoms for a prolonged period”) or to have done anything unusual (defined as “an unusual event or stressful situation”) on that particular day.
The study programme was approved by the University of Exeter Medical School Human Research Ethics Committee (13/09/030). All participants provided informed consent for contributing to this study and gave permission for use of their anonymized data and GPS location information to link environmental data.
Participants
Data were collected over a year (February 1, 2014 to January 31, 2015) using the Ménière’s Monitor App. During this time, 1,532 adult participants (18 yr or older) were recruited with 688 (45%) from the UK and 844 (55%) from overseas. All participants considered themselves to have MD, but only those reporting ENT diagnosed MD were included in the detailed analysis. Weather data were available for 491 participants within the UK, with the majority diagnosed by an ENT consultant (n = 397). These 397 participants used the app a total of 9,048 times between them; the average number of uses was 66 (minimum 1, maximum 335).
Weather Data
For each participant diagnosed by a consultant and providing GPS data (n = 397), the closest Met Office (UK based global weather and climate forecaster) weather station was identified using QGIS software via the Distance Matrix function. The Met Office data were made available through the MRC NERC-funded Medical and Environmental Data Mash-up Infrastructure Project. Daily weather data from the closest weather station to the participants GPS location were recorded. For 38 (0.4%) data points, the closest weather station was missing data; the data were then collected from the next available station. The weather variables included wind speed (in knots), visibility (km), surface air pressure (atmospheric pressure at the station) and sea level air pressure (atmospheric pressure at the station adjusted for altitude) (hPa), air temperature (°C), and relative humidity (%). To account for the variation in distance from the app user and the weather station several categorical variables were investigated. Wind speed was categorized based on the Beaufort scale: calm or light air <3 knots; light breeze 3 to 10.6 knots; moderate/fresh breeze 10.6 to 21 knots; strong breeze 21 to 26.9 knots; high winds/gale >26 knots. Visibility was categorized as per the Met Office (15): very poor <1 km; poor 1 to 4 km; moderate 4 to 10 km; good 10 to 20 km; very good 20 to 40 km; excellent >40 km. A binary relative humidity variable was investigated comparing humidity above and below 90% (the median value in the data for U.K.). Air temperature, sea level and station pressure were analyzed using a continuous normalized variable. In addition a binary pressure variable for sea level pressure was generated based on the definition of standard pressure at sea level (1013.25 hectopascals [hPa] or millibars); comparisons were made between pressures above and below this value (16).
Statistical Analysis
Validation of Self-reported Data
To validate cases represented by the self-reported data, we investigated known associations including:
-
1.
Age and hearing status, with hearing loss known to increase with age in the general population (17).
-
2.
Disease duration and hearing status, known to deteriorate rapidly in early stages of MD (18).
-
3.
Correlations between symptom severity, tinnitus, vertigo, and aural fullness (since all tend to peak at similar times, especially if an attack is reported (1)).
Associations between age and hearing, disease duration and hearing, attacks and symptom severity were noted in the expected directions (Supplementary Table 2, http://links.lww.com/MAO/A481). Hearing (baseline and app monitored) decreased with age and disease duration. Increases in symptom severity were predictive of attacks, especially vertigo.
Investigation of Weather Variables
To investigate the associations between the weather variables and symptom severity, fixed effort and random effect (RE) regressions were conducted using the xt suite of functions in STATA 13 (StataCorp, College Station, TX, U.S.A.). The Hausman test (19) was utilised, demonstrating that the null hypothesis should be accepted; therefore, only the results from RE models are reported here. RE linear regression models were used to estimate the change in each symptom per unit change in each weather variable. Models were adjusted for age, sex, disease duration, report of doing something unusual on same day, and ear(s) affected with MD (i.e., unilateral versus bilateral). Models were further adjusted for the other weather variables and seasonal effects.
The odds of an attack per unit increase in each weather variable were estimated using RE logistic regression models analysis in the panel data framework.
In weather variables where associations with MD symptom severity and/or attacks were noted, 1 day lag, lead and difference effects were investigated. Analysis was repeated using these three different variables to further explore the role of the weather in MD.
The xt suite of functions in STATA allow us to account for the unbalanced panel with individuals with more daily data available having a larger effect on the regression line and the estimated coefficients than those with more missing data. This means that individuals missing days at random do not bias the regression.
Sensitivity Analysis
Several sensitivity analyses were conducted where the analysis was repeated excluding participants reporting migraine (n = 69 [17%]), as migraine symptoms may have a relationship with the weather (20). Weather analyses were also repeated in the subset of participants who used the app for at least 30 days consecutively (n = 67) to eliminate any user who logged in to the app only once or twice and did not engage in regular data collection.
Results
The demographics for the 491 UK participants using the app over the 12-month period from February 2014 to January 2015 with valid weather data are summarised in Table 1. To limit bias in the results, we excluded all participants who were not diagnosed by an ENT consultant (n = 94 [19.0%]) from subsequent analyses.
Table 1.
Demographics of the 491 participants (including the 397 ENT diagnosed) using the Ménière’s monitor over the year from February 2014 with valid weather data
| All UK With GPS Data | ENT Diagnosed Only | |
|---|---|---|
| Number of participants | 491 | 397 |
| Sex (%) | ||
| Male | 140 (28.5) | 120 (30.2) |
| Female | 351 (71.5) | 277 (69.8) |
| Mean age, yr (SD) | 50.1 (11.3) | 50.0 (11.0) |
| Home location (%) | ||
| England | 438 (89.2) | 364 (91.7) |
| Scotland | 39 (7.9) | 24 (6.1) |
| Wales | 14 (2.9) | 9 (2.3) |
| Employment (%) | ||
| Employed/self-employed | 341 (69.5) | 267 (67.3) |
| Retired | 51 (10.4) | 40 (10.1) |
| Unemployed | 16 (3.3) | 15 (3.8) |
| Unable to work because of Ménière’s | 71 (14.5) | 65 (16.4) |
| Rather not say | 12 (2.4) | 10 (2.5) |
| MD demographics | ||
| Mean age at diagnosis, yr (SD) | 44.7 (11.8) | 44.3 (11.5) |
| Mean disease duration, yr (SD) | 5.4 (7.6) | 5.7 (7.8) |
| Diagnosed by (%) | ||
| ENT consultant | 397 (80.9) | |
| GP | 77 (15.7) | |
| Self | 17 (3.5) | |
| Ear affected (%) | ||
| Left | 136 (27.7) | 106 (26.7) |
| Right | 162 (33.0) | 147 (37.0) |
| Both | 193 (39.3) | 144 (36.3) |
| Suffer migraines (%) | 89 (18.1) | 69 (17.4) |
| Medication taken regularly (%) | 419 (85.3) | 340 (85.6) |
ENT indicates ear, nose, and throat; MD, Ménière’s disease.
The 397 ENT diagnosed users were predominantly female (70%), with a mean age of 50 years, and the majority were currently employed (67%) (Table 1). The mean age of their MD diagnosis was 44 ± 11 years, and on average participants had been diagnosed for 6 ± 8 years. Approximately two-thirds of users were defined as “unilateral” (i.e., MD in one ear; n = 253 [64%]) while the remainder were bilateral (both ears). Individuals were geographically spread across the UK (Supplementary Figure 1, http://links.lww.com/MAO/A482).
Weather Data
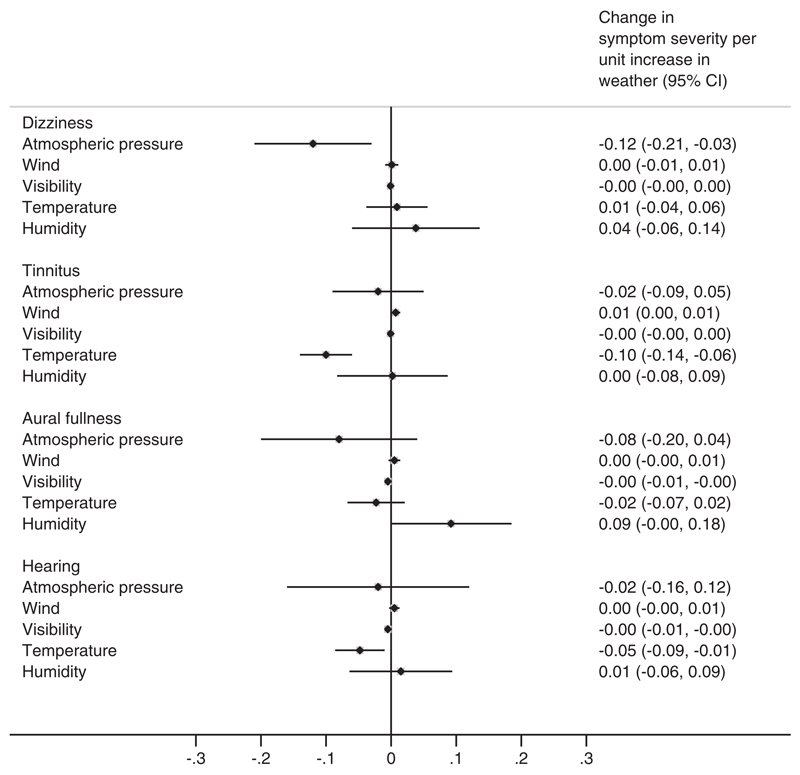
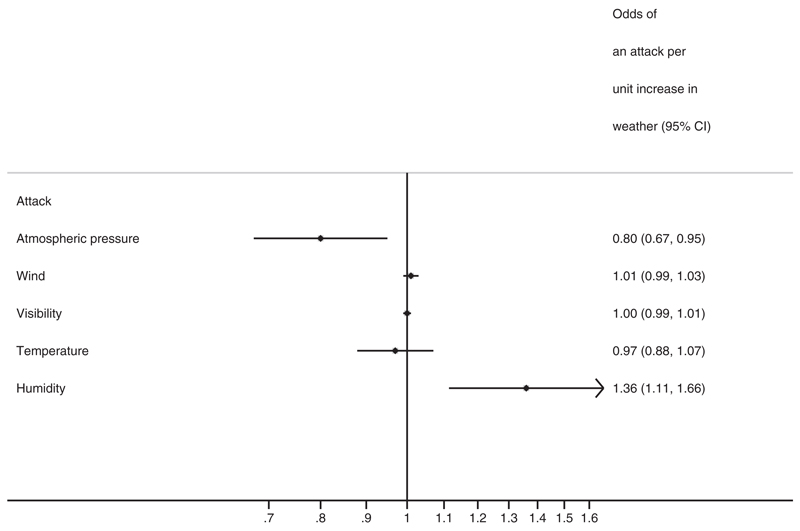
Lower mean sea level pressure or mean station air pressure was associated with higher levels of vertigo, tinnitus, and aural fullness (Table 2, Figure 1). No association was noted with changes in hearing level. Higher odds of reporting an attack were also noted at lower atmospheric pressures; when atmospheric pressure was below 1013.25 hPa, individuals were at greater odds of an attack (Table 2, Figure 2). This association suggested that when the atmospheric pressure was below 1013.25 hPa individuals were 23% more likely to have an attack. The associations with vertigo, aural fullness and attacks remained when other weather variables were considered in the model. Exclusion of individuals reporting migraine or unusual events did not alter these findings (Table 2). Furthermore, in the subset of participants reporting more than 30 consecutive days, low sea level pressure was associated with higher vertigo severity (0.13 [95% CI 0.04, 0.22]) and higher odds of an attack (OR: 1.49 [95% CI 1.18, 1.85]) remained (Table 2).
Table 2.
Associations between lower atmospheric pressure and the symptoms of MD
| Sea Level Air | High Versus Low | Station Air | ||||
|---|---|---|---|---|---|---|
| Pressure (hPa)a | p Value | Sea Level Pressure | p Value | Pressure (hPa)a | p Value | |
| Dizziness—regression coefficient (95% CI) representing change in dizziness severity per unit change in atmospheric pressure | ||||||
| Crude | 0.05 (0.01, 0.10) | 0.01 | 0.12 (0.04, 0.20) | 0.004 | 0.06 (0.01, 0.12) | 0.02 |
| Adjusted | 0.05 (0.01, 0.09) | 0.02 | 0.12 (0.03, 0.20) | 0.005 | 0.06 (0.01, 0.12) | 0.03 |
| Adjusted 2 | 0.05 (0.01, 0.10) | 0.03 | 0.12 (0.04, 0.21) | 0.005 | 0.06 (0.00, 0.12) | 0.04 |
| No migraine | 0.07 (0.02, 0.11) | 0.003 | 0.11 (0.03, 0.20) | 0.007 | 0.08 (0.03, 0.14) | 0.004 |
| No unusual events | 0.06 (0.02, 0.13) | 0.008 | 0.13 (0.04, 0.21) | 0.003 | 0.07 (0.01, 0.13) | 0.02 |
| More than a month | 0.08 (0.02, 0.14) | 0.007 | 0.15 (0.05, 0.24) | 0.002 | 0.11 (0.04, 0.18) | 0.005 |
| Tinnitus—regression coefficient (95%CI) representing change in tinnitus severity per unit change in atmospheric pressure | ||||||
| Crude | 0.06 (0.03, 0.10) | 0.001 | 0.09 (0.02, 0.16) | 0.02 | 0.07 (0.02, 0.12) | 0.005 |
| Adjusted | 0.06 (0.02, 0.10) | 0.001 | 0.09 (0.02, 0.16) | 0.02 | 0.07 (0.02, 0.12) | 0.004 |
| Adjusted 2 | 0.05 (0.01, 0.09) | 0.02 | 0.02 (−0.13, 0.09) | 0.74 | 0.05 (0.00, 0.10) | 0.06 |
| No migraine | 0.07 (0.03, 0.11) | 0.001 | 0.08 (0.01, 0.15) | 0.02 | 0.08 (0.03, 0.13) | 0.002 |
| No unusual events | 0.07 (0.03, 0.10) | 0.001 | 0.09 (0.01, 0.14) | 0.02 | 0.07 (0.02, 0.12) | 0.004 |
| More than a month | 0.04 (0.00, 0.08) | 0.05 | 0.03 (−0.04, 0.11) | 0.33 | 0.06 (0.01, 0.12) | 0.023 |
| Aural fullness—regression coefficient (95% CI) representing change in aural fullness severity per unit change in atmospheric pressure | ||||||
| Crude | 0.06 (0.02, 0.10) | 0.005 | 0.12 (0.04, 0.19) | 0.002 | 0.08 (0.02, 0.13) | 0.005 |
| Adjusted | 0.06 (0.02, 0.10) | 0.006 | 0.12 (0.04, 0.19) | 0.003 | 0.08 (0.02, 0.13) | 0.005 |
| Adjusted 2 | 0.05 (0.01, 0.10) | 0.019 | 0.08 (−0.04, 0.20) | 0.20 | 0.07 (0.01, 0.13) | 0.021 |
| No migraine | 0.06 (0.02, 0.11) | 0.003 | 0.12 (0.04, 0.20) | 0.002 | 0.08 (0.03, 0.14) | 0.003 |
| No unusual events | 0.07 (0.03, 0.11) | 0.001 | 0.13 (0.05, 0.21) | 0.001 | 0.09 (0.03, 0.14) | 0.002 |
| More than a month | 0.05 (−0.01, 0.10) | 0.08 | 0.08 (0.00, 0.17) | 0.06 | 0.07 (0.00, 0.14) | 0.05 |
| Hearing loss—regression coefficient (95% CI) representing change in hearing loss per unit change in atmospheric pressure | ||||||
| Crude | 0.03 (0.00, 0.07) | 0.09 | 0.05 (−0.01, 0.12) | 0.11 | 0.03 (−0.01, 0.08) | 0.14 |
| Adjusted | 0.03 (0.00, 0.07) | 0.08 | 0.05 (−0.01, 0.12) | 0.10 | 0.04 (−0.01, 0.08) | 0.11 |
| Adjusted 2 | 0.02 (−0.02, 0.05) | 0.39 | 0.02 (−0.08, 0.12) | 0.72 | 0.02 (−0.03, 0.070) | 0.40 |
| No migraine | 0.05 (0.02, 0.09) | 0.003 | 0.07 (0.00, 0.12) | 0.04 | 0.07 (0.02, 0.11) | 0.005 |
| No unusual events | 0.04 (0.00, 0.07) | 0.04 | 0.07 (0.00, 0.13) | 0.05 | 0.05 (0.00, 0.09) | 0.05 |
| More than a month | 0.07 (0.02, 0.12) | 0.003 | 0.08 (0.00, 0.16) | 0.04 | 0.09 (0.03, 0.15) | 0.003 |
| Odds ratio (95% CI) representing the odds of an attack per unit change in atmospheric pressure | ||||||
| Crude | 1.11 (1.03, 1.20) | 0.010 | 1.23 (1.05, 1.45) | 0.010 | 1.14 (1.03, 1.27) | 0.014 |
| Adjusted | 1.10 (1.03, 1.20) | 0.012 | 1.23 (1.05, 1.45) | 0.011 | 1.15 (1.03, 1.27) | 0.010 |
| Adjusted 2 | 1.10 (1.01, 1.19) | 0.042 | 1.20 (1.01, 1.43) | 0.037 | 0.89 (1.01, 1.27) | 0.040 |
| No migraine | 1.11 (1.01, 1.22) | 0.027 | 1.27 (1.06, 1.52) | 0.008 | 1.15 (1.03, 1.30) | 0.014 |
| No unusual events | 1.12 (1.03, 1.22) | 0.006 | 1.30 (1.10, 1.54) | 0.002 | 1.15 (1.03, 1.28) | 0.010 |
| More than a month | 1.27 (1.10, 1.45) | 0.001 | 1.45 (1.14, 1.82) | 0.002 | 1.43 (1.19, 1.69) | <0.001 |
All models (except crude) adjusted for age, sex, disease duration, unusual and ear affected; “adjusted 2” includes additional adjustment for other weather variables, e.g., if atmospheric pressure investigated then adjusted for temperature, humidity, wind, etc.; “no migraine” excludes participants with migraine from analyses; “no unusual events” excludes unusual events as known to associate with symptoms; “more than a month” includes only users who used app for at least 30 consecutive days.
Bold font indicates p < 0.05.
The data presented represent a one SD reduction in sea level and station air pressure corresponding to a 12.0 and 16.2 hPa reduction.
MD indicates Ménière’s disease.
Fig. 1.
Dot plot representing change in symptom (vertigo, tinnitus, aural fullness and hearing loss) severity for a one SD change in the different weather variables. A negative change in the symptoms represents a reduction in symptom severity while a positive change represents an increase in symptoms severity. The zero line represents no change in symptoms per unit change in the weather; where this is crossed the associations are not statistically significant.
Fig. 2.
Dot plot representing change in odds of reporting an attack for a one SD change in the different weather variables. The reference line at one represents the null hypothesis that the weather variables do not influence an individual’s odds of an attack.
Relative humidity above 90% was associated with increased aural fullness and an increased odds of an individual reporting an attack (OR: 1.26 [95% CI 1.06, 1.49]; Table 3, Figure 2). There was some weak evidence of an interaction effect for low pressure and high humidity on the risk of an attack (P = 0.05). The risk of an attack on a low pressure high humidity day was 1.56-fold (95% CI 1.23, 1.96) greater than on low humidity high pressure days.
Table 3.
Associations between changes in wind categories, visibility, temperature, humidity and the symptoms of MD
| Wind (Beaufort Scale) | p | Visibility (km) | p | Temperature (°C) | p | Relative Humidity (%) | p | |
|---|---|---|---|---|---|---|---|---|
| Dizziness—regression coefficient (95% CI) representing change in dizziness severity per unit change in weather variable | ||||||||
| Crude | 0.003 (−0.005, 0.012) | 0.48 | −0.001 (−0.005, 0.003) | 0.57 | 0.008 (−0.036, 0.052) | 0.72 | 0.028 (−0.056, 0.112) | 0.52 |
| Adjusted | 0.003 (−0.006, 0.012) | 0.50 | −0.001 (−0.005, 0.003) | 0.53 | 0.007 (−0.037, 0.052) | 0.74 | 0.028 (−0.056, 0.113) | 0.51 |
| Adjusted 2 | 0.001 (−0.008, 0.011) | 0.78 | −0.001 (−0.005, 0.003) | 0.67 | 0.009 (−0.038, 0.056) | 0.71 | 0.038 (−0.061, 0.136) | 0.45 |
| No migraine | 0.001 (−0.007, 0.010) | 0.76 | −0.001 (−0.005, 0.003) | 0.49 | 0.022 (−0.023, 0.067) | 0.34 | 0.036 (−0.051, 0.123) | 0.42 |
| No unusual events | 0.004 (−0.005, 0.013) | 0.37 | −0.001 (−0.005, 0.003) | 0.78 | −0.000 (−0.046, 0.045) | 0.99 | 0.024 (−0.063, 0.111) | 0.59 |
| More than a month | 0.003 (−0.007, 0.013) | 0.56 | −0.001 (−0.005, 0.003) | 0.64 | 0.024 (−0.026, 0.073) | 0.35 | 0.041 (−0.058, 0.141) | 0.42 |
| Tinnitus—regression coefficient (95% CI) representing change in tinnitus severity per unit change in weather variable | ||||||||
| Crude | 0.008 (0.001, 0.016) | 0.033 | −0.001 (−0.004, 0.002) | 0.50 | −0.071 (−0.110, −0.033) | <0.001 | −0.006 (−0.080, 0.067) | 0.86 |
| Adjusted | 0.008 (0.001, 0.016) | 0.031 | −0.001 (−0.005, 0.002) | 0.49 | −0.073 (−0.111, −0.034) | <0.001 | −0.006 (−0.079, 0.067) | 0.87 |
| Adjusted 2 | 0.007 (−0.002, 0.015) | 0.11 | −0.001 (−0.005, 0.002) | 0.43 | −0.099 (−0.140, −0.058) | <0.001 | 0.002 (−0.082, 0.087) | 0.96 |
| No migraine | 0.007 (−0.001, 0.014) | 0.09 | −0.002 (−0.005, 0.001) | 0.23 | −0.071 (−0.109, −0.032) | <0.001 | −0.002 (−0.076, 0.073) | 0.96 |
| No unusual events | 0.010 (0.002, 0.017) | 0.013 | −0.001 (−0.004, 0.003) | 0.73 | −0.081 (−0.120, −0.041) | <0.001 | −0.013 (−0.088, 0.063) | 0.74 |
| More than a month | 0.004 (−0.003, 0.012) | 0.27 | −0.001 (−0.004, 0.002) | 0.61 | −0.038 (−0.075, −0.001) | 0.042 | 0.027 (−0.046, 0.101) | 0.47 |
| Aural fullness—regression coefficient (95% CI) representing change in aural fullness per unit change in weather variable | ||||||||
| Crude | 0.004 (−0.004, 0.012) | 0.30 | −0.006 (−0.010, −0.002) | 0.001 | −0.013 (−0.055, 0.029) | 0.55 | 0.105 (0.025, 0.185) | 0.010 |
| Adjusted | 0.004 (−0.004, 0.012) | 0.31 | −0.006 (−0.010, −0.003) | 0.001 | −0.014 (−0.056, 0.028) | 0.52 | 0.106 (0.026, 0.187) | 0.009 |
| Adjusted 2 | 0.005 (−0.004, 0.014) | 0.29 | −0.005 (−0.009, −0.001) | 0.018 | −0.023 (−0.067, 0.021) | 0.31 | 0.092 (−0.001, 0.185) | 0.05 |
| No migraine | 0.002 (−0.006, 0.010) | 0.61 | −0.007 (−0.010, −0.003) | <0.001 | 0.000 (−0.043, 0.043) | 0.99 | 0.116 (0.034, 0.199) | 0.006 |
| No unusual events | 0.005 (−0.003, 0.013) | 0.23 | −0.006 (−0.009, −0.002) | 0.003 | −0.018 (−0.061, 0.025) | 0.41 | 0.106 (0.024, 0.189) | 0.011 |
| More than a month | 0.002 (−0.007, 0.010) | 0.63 | −0.006 (−0.010, −0.002) | 0.004 | 0.028 (−0.019, 0.075) | 0.24 | 0.102 (0.006, 0.198) | 0.032 |
| Hearing loss—regression coefficient (95% CI) representing change in hearing loss per unit change in weather variable | ||||||||
| Crude | 0.004 (−0.003, 0.011) | 0.22 | −0.006 (−0.009, −0.003) | <0.001 | −0.019 (−0.055, 0.017) | 0.29 | 0.034 (−0.034, 0.103) | 0.33 |
| Adjusted | 0.004 (−0.003, 0.011) | 0.21 | −0.006 (−0.009, −0.003) | <0.001 | −0.021 (−0.057, 0.015) | 0.27 | 0.034 (−0.035, 0.102) | 0.33 |
| Adjusted 2 | 0.005 (−0.003, 0.013) | 0.18 | −0.005 (−0.009, −0.002) | 0.002 | −0.048 (−0.086, −0.011) | 0.011 | 0.015 (−0.064, 0.094) | 0.71 |
| No migraine | 0.003 (−0.004, 0.010) | 0.44 | −0.006 (−0.009, −0.003) | <0.001 | −0.026 (−0.063, 0.010) | 0.16 | 0.035 (−0.035, 0.106) | 0.33 |
| No unusual events | 0.005 (−0.002, 0.012) | 0.18 | −0.005 (−0.009, −0.002) | 0.001 | −0.028 (−0.065, 0.009) | 0.14 | 0.036 (−0.035, 0.106) | 0.32 |
| More than a month | 0.006 (−0.002, 0.014) | 0.17 | −0.005 (−0.008, −0.001) | 0.010 | 0.015 (−0.026, 0.055) | 0.48 | 0.011 (−0.072, 0.094) | 0.80 |
| Odds ratio (95% CI) representing the odds of an attack per unit change in weather variable | ||||||||
| Crude | 1.01 (0.99, 1.03) | 0.38 | 1.00 (0.99, 1.01) | 0.65 | 1.00 (0.92, 1.10) | 0.95 | 1.24 (1.05, 1.47) | 0.011 |
| Adjusted | 1.01 (0.99, 1.03) | 0.43 | 1.00 (0.99, 1.01) | 0.61 | 0.99 (0.91, 1.09) | 0.85 | 1.26 (1.06, 1.49) | 0.007 |
| Adjusted 2 | 1.01 (0.99, 1.03) | 0.48 | 1.00 (0.99, 1.01) | 0.55 | 0.97 (0.88, 1.07) | 0.56 | 1.36 (1.12, 1.66) | 0.002 |
| No migraine | 1.01 (0.99, 1.03) | 0.56 | 1.00 (0.99, 1.01) | 0.91 | 0.98 (0.89, 1.08) | 0.63 | 1.23 (1.02, 1.48) | 0.026 |
| No unusual events | 1.01 (0.99, 1.03) | 0.38 | 1.00 (0.99, 1.01)) | 0.80 | 1.01 (0.92, 1.11) | 0.88 | 1.26 (1.06, 1.50) | 0.009 |
| More than a month | 0.99 (0.96, 1.02) | 0.51 | 1.00 (0.98, 1.01) | 0.40 | 1.01 (0.89, 1.14) | 0.89 | 1.40 (1.09, 1.80) | 0.009 |
All models except crude adjusted for age, sex, disease duration, unusual and ear affected; adjusted 2 includes additional adjustment for other weather variables; no migraine excludes participants with migraine from analyses; no unusual events excludes unusual events as known to associate with symptoms; more than a month represents users who used app for at least 30 consecutive days.
Bold font indicates p < 0.05.
Higher visibility was associated with improved hearing levels and lower levels of aural fullness; this association remained in fully adjusted models and when migraine or unusual events were excluded, and in the subset of participants using for at least 30 days (Table 3, Figure 1). Increased temperature was associated with lower levels of tinnitus in all models (Table 3, Figure 1), and with improved hearing only in fully adjusted models (including all other weather variables). Increased wind speed was associated with worse tinnitus, but not when all other weather variables were included in the model.
Generally, seasonality adjustment did not alter the findings, although the relationship between humidity and odds of attacks was no longer significant. Furthermore, an association was also noted between improved hearing status and higher atmospheric pressure in these models (Supplementary Table 3, http://links.lww.com/MAO/A483).
Lower mean sea level pressure for the day before symptom recording was associated with higher levels of tinnitus, hearing loss, aural fullness (Table 4). Decreases in sea level pressure between day 1 and day 2 were associated with higher odds of an attack (OR: 1.23 [95% CI: 1.05, 1.45]; Table 4). Relative humidity above 90% the day before was also associated with an increased risk of attack (OR: 1.26 [95% CI: 1.11, 1.57]; Table 4). Lower sea level pressure was associated with higher tinnitus and aural fullness and increased risk of an attack when considering the pressure for the day after symptom recording.
Table 4.
Lead (T+1), lag (T−1), and difference (D) effects of change in the weather variables on the symptoms of MD
| Model | Dizziness | p | Tinnitus | p | Aural Fullness | p | Hearing Loss | p | Attack | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sea level pressure (hPa) | T+1 | 0.04 (−0.02, 0.09) | 0.18 | 0.06 (0.02, 0.12) | 0.008 | 0.05 (0.00, 0.11) | 0.033 | 0.04 (0.00, 0.08) | 0.08 | 1.25 (1.12, 1.38) | <0.001 |
| T−1 | 0.05 (−0.01, 0.10) | 0.08 | 0.08 (0.03, 0.13) | 0.001 | 0.07 (0.02, 0.12) | 0.004 | 0.08 (0.04, 0.12) | <0.001 | 1.04 (0.95, 1.19) | 0.26 | |
| D | 0.03 (−0.04, 0.10) | 0.44 | −0.02 (−0.08, 0.05) | 0.60 | 0.04 (−0.03, 0.11) | 0.23 | −0.032 (−0.09, 0.03) | 0.29 | 1.24 (1.06, 1.46) | 0.009 | |
| Visibility (km) | T+1 | −0.00 (−0.01, 0.00) | 0.48 | 0.00 (−0.01, 0.01) | 0.99 | −0.00 (−0.01, 0.00) | 0.37 | −0.01 (−0.01, −0.00) | 0.006 | 1.00 (0.99, 1.01) | 0.55 |
| T − 1 | −0.00 (−0.01, 0.00) | 0.59 | 0.00 (−0.01, 0.01) | 0.92 | −0.01 (−0.01, −0.00) | 0.026 | −0.01 (−0.01, −0.00) | 0.013 | 1.00 (0.99, 1.01) | 0.59 | |
| D | 0.001 (−0.003, 0.004) | 0.76 | 0.00 (−0.01, 0.00) | 0.62 | −0.00 (−0.01, 0.00) | 0.75 | −0.00 (−0.003, 0.003) | 0.80 | 1.00 (0.99, 1.01) | 0.90 | |
| Temperature (°C) | T+1 | −0.02 (−0.07, 0.04) | 0.51 | −0.08 (−0.12, −0.03) | 0.001 | −0.05 (−0.10, 0.00) | 0.07 | −0.07 (−0.12, −0.03) | 0.001 | 0.90 (0.80, 1.00) | 0.06 |
| T−1 | −0.02 (−0.07, 0.03) | 0.43 | −0.09 (−0.13, −0.04) | <0.001 | −0.04 (−0.09, 0.01) | 0.13 | −0.04 (−0.08, 0.01) | 0.10 | 0.83 (0.74, 0.94) | 0.003 | |
| D | 0.06 (−0.01, 0.13) | 0.08 | 0.02 (−0.04, 0.07) | 0.61 | 0.07 (0.01, 0.13) | 0.032 | 0.01 (−0.04, 0.07) | 0.61 | 1.27 (1.09, 1.48) | 0.002 | |
| Relative humidity (%) | T+1 | 0.03 (−0.07, 0.13) | 0.51 | −0.05 (−0.14, 0.04) | 0.26 | 0.07 (−0.03, 0.16) | 0.17 | 0.03 (−0.06, 0.11) | 0.52 | 1.26 (1.11, 1.57) | 0.035 |
| T−1 | 0.03 (−0.07, 0.13) | 0.51 | 0.02 (−0.06, 0.11) | 0.63 | 0.11 (0.01, 0.20) | 0.025 | 0.04 (−0.04, 0.12) | 0.36 | 1.12 (0.96, 1.50) | 0.11 | |
| D | −0.03 (−0.11, 0.05) | 0.45 | −0.03 (−0.09, 0.04) | 0.43 | −0.01 (−0.09, 0.06) | 0.74 | −0.03 (−0.09, 0.04) | 0.45 | 0.97 (0.81, 1.16) | 0.76 |
Adjusted for age, sex, disease duration, unusual event, and ear affected. Lead effects look at the association between weather the next day (t=+1) and symptoms for the current day (t=0). Lag effects look at the association between the weather the previous day (t=−1) and symptoms for the current day (t=0). Difference effects look at the daily change in the weather, i.e., if atmospheric pressure was 1,000 hPa on day 1 and 1,030 on day 2 the difference would be 30.
Bold font indicates p < 0.05.
The visibility on the day before or after data collection was associated with improved hearing, while temperature on the days either side of data collection remained associated with tinnitus (Table 4).
Discussion
This study has used a novel approach to investigate the role of the weather on the severity of the key symptoms of MD (i.e., vertigo, tinnitus, hearing loss, and aural fullness). The mobile phone application data, in conjunction with weather data from the Met Office, have enabled us to make several advances in the understanding of this disease.
Weather Changes, Especially Atmospheric Pressure and Humidity, Are Associated With Changes in Symptom Severity
First, we provide the strongest evidence to date that changes in atmospheric pressure are associated with disease activity in MD. Lower daily atmospheric pressure was associated with higher levels of vertigo, tinnitus and aural fullness, and higher odds of an individual reporting an attack. These associations remained when models were adjusted for all the measured weather variables and seasonality. Low atmospheric pressure on the day before or the day after symptom recording was also associated with symptom exacerbation and an increased risk of an attack. This significantly builds on the evidence base for the role of atmospheric pressure in MD, which was previously based on anecdotal reports. One recent Brazilian study suggested an inverse relationship between atmospheric pressure and presentation at an emergency room with vertigo (not MD specific), supporting the role of weather as a trigger for this symptom (21).
High humidity was positively associated with aural fullness, hearing loss and increased odds of an attack when the other weather variables (added independently or as interactions) were accounted for. Temperature was inversely associated with tinnitus nuisance and visibility was inversely associated with the severity of hearing loss and aural fullness. No consistent associations were noted between wind speed and the symptoms of MD.
These results significantly extend the evidence base on the role of weather in MD. Previous work has suggested atmospheric pressure may have a role in the onset of the first vertigo attack (22) and anecdotally it is reported to cause symptom spikes (14). The Japanese study showed that 36 individuals of 67 MD patients (54%) had their first attack on the day when a cold front passed by or on the next day (22). This fits with our findings, as fronts are a boundary between air masses that lead to low pressure systems as the atmosphere attempts to even out the temperature contrast. Hence the attacks noted in Japan occurred around a time when the pressure was low or changing. However previous studies have predominantly used questionnaire data in very small numbers of individuals. In our research, daily Met Office weather data for specific postcode districts (~3,000 unique districts in the UK) were linked to individuals’ symptoms for that specific day in 397 UK-based individuals with selfreported MD diagnosed by an ENT consultant. We were also able to consider lag, lead and difference effects. This is therefore the most comprehensive analysis of the effects of weather on MD. Furthermore, this study also demonstrated for the first time that humidity may be important in attacks, aural fullness and hearing level, and was observed to weakly interact with atmospheric pressure to further exacerbate the odds of an attack.
Previous studies have demonstrated relationships between low atmospheric pressure and pain in migraine, rheumatic disease and osteoarthritis (13,23,24). Associations have also been noted between cardiovascular events and low atmospheric pressure (25,26). However, in general, the actual mechanisms linking changes in atmospheric pressure and health are poorly understood.
Rat model experiments suggest that there is an atmospheric pressure sensor in the vestibular system of the inner ear (27). This may help to explain the relationship between atmospheric pressure and MD, where individuals have a compromised vestibular system. Furthermore, if MD is due to endolymphatic hydrops (28,29), then changes in atmospheric pressure may well, in turn, influence endolymphatic pressure via the middle ear.
Humidity was also independently associated with tinnitus, hearing loss, and increased odds of attacks. More humid air is less dense and absorbs more sound (30), possibly explaining the reduction in hearing on more humid days. Anecdotal evidence indicates a relationship between tinnitus and humidity, but no studies to date have investigated the relationship between humidity and tinnitus severity. More research is needed to investigate potential aetiological mechanisms linking humidity with the symptoms of MD. There was also evidence of an additive effect of humidity and atmospheric pressure on the odds of an attack, with high humidity low pressure days increasing the odds of an attack by approximately 50% when compared with low humidity, high pressure days.
Strengths and Limitations
This is the first time that the symptoms of MD have been monitored on a regular basis in a large number of individuals and linked with weather data from the Met Office, enabling a thorough investigation of the role of the weather in MD severity. Participants were not informed that the researchers were monitoring weather to limit biased reporting, and the use of panel data analysis enables control of individual heterogeneity.
We do, however, acknowledge some limitations. Firstly, the diagnoses of MD were self-reported, and MD diagnosis can be difficult and variable as there is no specific test for the condition. However, only individuals reporting diagnosis by an ENT consultant were included and several expected associations were observed, including age and hearing status and disease duration and vertigo and hearing status. Future work will extend the app to attempt to identify those individuals with vestibular migraine and attempt to link the app with health records. Second, the data from the panel used were unbalanced (i.e. people had missed reporting days); however, a sensitivity analysis to include only participants who had used the app for at least 30 days in a row did not alter our findings. The closest weather station to the location of the individual was used, however there might be subtle differences in pressure and other weather parameters within as little as a 2 mile radius in hilly and mountainous regions. The cohort also had a high prevalence of migraine, which is known to be influenced by the weather; however, our results remained unaltered when we only included individuals without migraine. We were unable to account for other changes in pressure that an individual might have experienced during any one day (e.g., driving up mountains), although we anticipate that the majority of participants will not undergo significant altitude changes in 24 hours. Individuals tended to log their symptoms at the end of the day at home, so the weather data may not completely represent exposure for that day. However, it is likely that users work within a 50 mile radius of home and therefore the weather data for the GPS location recorded should approximate to actual exposure. Future study designs may involve a predictive model based on air pressure changes and comparison to collected episode data from MD patients. No controls (i.e., individuals without MD) were monitored in this study; however, the study was focused on the MD population. Finally, this study may be subject to participation and reporting biases, the use of an App may limit our users to younger individuals with MD and participants may be more likely to monitor their condition when it is particularly active.
Conclusions
This study suggested that lower atmospheric pressure was associated with higher odds of an attacks and higher levels of vertigo, tinnitus, and aural fullness in individuals suffering MD. High humidity also increased the odds of experiencing an attack. Monitoring weather by those who suffer MD may remove some of the uncertainty of when attacks may occur, which is known to significantly contribute to the lowered quality of life among patients. These findings, pending further validation, could result in the Met Office providing a health forecast for MD sufferers in the UK. For example when extreme lows are forecast (e.g., incoming storm fronts) individuals with MD (or a sub-group of sufferers) could be warned and potentially modify their plans and/or treatments for that day.
Supplementary Material
Supplemental digital content is available in the text.
Acknowledgments
The authors thank the study participants for involvement and the team at Buzz Interactive for designing the mobile app.
The European Centre for Environment and Human Health (part of the University of Exeter Medical School) is partly financed by the European Regional Development Fund Programme 2007 to 2013 and European Social Fund Convergence Programme for Cornwall and the Isles of Scilly (Dr. J.T. and Dr. N.O.). Dr. J.T. is supported by the Diabetes Research and Wellness Foundation. This research is part of the MEDMI Project (Medical and Environmental Data Mashup Infrastructure) MR/K019341/1, which is funded in part by the UK Medical Research Council (MRC) and the U.K. Natural Environment Research Council (NERC) (Dr. W.S.). The UK Meniere’s Society assisted in patient recruitment. The funders had no role in the design, analysis, or interpretation of the data presented. The researchers are independent of the funders.
Footnotes
W.S. contributed to the statistical analysis plan, analyzed the data, and contributed to drafting the manuscript. C.S. provided the Met Office data that was used in this manuscript, provided expertise in data linkage, assisted in interpretation of the data, and revised the draft manuscript. D.J.W., N.R., and G.B. provided clinical expertise and assisted in the design of the Ménière’s monitor, interpretation of annual results and revised the draft manuscript. N.J.O. wrote the statistical analysis plan, monitored data collection for the whole year, and revised the draft paper. J.T. designed the Ménière’s monitor, oversaw data collection for the year, wrote the statistical analysis plan, cleaned and analyzed components of the data, and drafted and revised the article.
The authors disclose no conflicts of interest.
References
- 1.Sajjadi H, Paparella MM. Meniere’s disease. Lancet. 2008;372:406–14. doi: 10.1016/S0140-6736(08)61161-7. [DOI] [PubMed] [Google Scholar]
- 2.Nakashima T, Pyykko I, Arroll MA, et al. Meniere’s disease. Nat Rev Dis Primers. 2016;2:16028. doi: 10.1038/nrdp.2016.28. [DOI] [PubMed] [Google Scholar]
- 3.Tyrrell J, Whinney DJ, Fleming LE, et al. Prevalence, associated factors and comorbid conditions for Méniére’s disease. Ear Hear. 2014;35:e162–9. doi: 10.1097/AUD.0000000000000041. [DOI] [PubMed] [Google Scholar]
- 4.Yardley L, Dibb B, Osborne G. Factors associated with quality of life in Meniere’s disease. Clin Otolaryngol Allied Sci. 2003;28:436–41. doi: 10.1046/j.1365-2273.2003.00740.x. [DOI] [PubMed] [Google Scholar]
- 5.Simo H, Yang S, Qu W, et al. Meniere’s disease: Importance of socioeconomic and environmental factors. Am J Otolaryngol. 2015;36:393–8. doi: 10.1016/j.amjoto.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 6.Havia M, Kentala E, Pyykko I. Prevalence of Meniere’s disease in general population of Southern Finland. Otolaryngol Head Neck Surg. 2005;133:762–8. doi: 10.1016/j.otohns.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 7.Tyrrell J, Whinney DJ, Taylor T. The cost of Méniére’s disease: A novel multi-source approach. Ear Hear. 2016;37:e202–9. doi: 10.1097/AUD.0000000000000264. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JP, Harris JP. Impact of Meniere’s disease on quality of life. Otol Neurotol. 2001;22:888–94. doi: 10.1097/00129492-200111000-00030. [DOI] [PubMed] [Google Scholar]
- 9.Pullens B, Verschuur HP, van Benthem PP. Surgery for Meniere’s disease. Cochrane Database Syst Rev. 2013;2 doi: 10.1002/14651858.CD005395.pub3. CD005395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirby SE, Yardley L. Physical and psychological triggers for attacks in Meniere’s disease: The patient perspective. Psychother Psychosom. 2012;81:396–8. doi: 10.1159/000337114. [DOI] [PubMed] [Google Scholar]
- 11.Herbert I, Nolte E, Eichhorn T. Weather status and incidence of idiopathic facial nerve paralyses, vestibular disorders, Meniere’s attacks and sudden deafness. Laryngol Rhinol Otol (Stuttg) 1987;66:249–50. [PubMed] [Google Scholar]
- 12.Ozeki K, Noda T, Nakamura M, et al. Weather and headache onset: A large-scale study of headache medicine purchases. Int J Biometeorol. 2015;59:447–51. doi: 10.1007/s00484-014-0859-8. [DOI] [PubMed] [Google Scholar]
- 13.Kimoto K, Aiba S, Takashima R, et al. Influence of barometric pressure in patients with migraine headache. Intern Med. 2011;50:1923–8. doi: 10.2169/internalmedicine.50.5640. [DOI] [PubMed] [Google Scholar]
- 14.Salt AN, Plontke SK. Endolymphatic hydrops: Pathophysiology and experimental models. Otolaryngol Clin North Am. 2010;43:971–83. doi: 10.1016/j.otc.2010.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Met office. [Accessed April 2015];2015 Available at: http://www.metoffice.gov.uk/guide/weather/symbols - visibility.
- 16.Bureau International des Poids et Mesures (BIPM) [Accessed September 15, 2015];2015 Available at: http://www.bipm.org/utils/common/pdf/CGPM/CGPM10.pdf.
- 17.Patterson RD, Nimmo-Smith I, Weber DL, et al. The deterioration of hearing with age: Frequency selectivity, the critical ratio, the audiogram, and speech threshold. J Acoust Soc Am. 1982;72:1788–803. doi: 10.1121/1.388652. [DOI] [PubMed] [Google Scholar]
- 18.Stahle J. Advanced Meniere’s disease. A study of 356 severely disabled patients. Acta Otolaryngol. 1976;81:113–9. doi: 10.3109/00016487609107484. [DOI] [PubMed] [Google Scholar]
- 19.Hausman JA. Specification tests in econometrics. Econometrica. 1978;46:1251–71. [Google Scholar]
- 20.Zebenholzer K, Rudel E, Frantal S, et al. Migraine and weather: A prospective diary-based analysis. Cephalalgia. 2011;31:391–400. doi: 10.1177/0333102410385580. [DOI] [PubMed] [Google Scholar]
- 21.Pereira AB, Almeida LAF, Pereira NG, et al. Seasonality of dizziness and vertigo in a tropical region. Chronobiol Int. 2015;0:1–6. doi: 10.3109/07420528.2015.1014094. [DOI] [PubMed] [Google Scholar]
- 22.Mizukoshi K, Watanabe Y, Shojaku H, et al. Influence of a cold front upon the onset of Meniere’s disease in Toyama, Japan. Acta Otolaryngol Suppl. 1995;520(Pt 2):412–4. doi: 10.3109/00016489509125285. [DOI] [PubMed] [Google Scholar]
- 23.Gorin AA, Smyth JM, Weisberg JN, et al. Rheumatoid arthritis patients show weather sensitivity in daily life, but the relationship is not clinically significant. Pain. 1999;81:173–7. doi: 10.1016/s0304-3959(99)00010-x. [DOI] [PubMed] [Google Scholar]
- 24.Guedj D, Weinberger A. Effect of weather conditions on rheumatic patients. Ann Rheum Dis. 1990;49:158–9. doi: 10.1136/ard.49.3.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Danet S, Richard F, Montaye M, et al. Unhealthy effects of atmospheric temperature and pressure on the occurrence of myocardial infarction and coronary deaths. A 10-year survey: The Lille-World Health Organization MONICA project (Monitoring trends and determinants in cardiovascular disease) Circulation. 1999;100:E1–7. doi: 10.1161/01.cir.100.1.e1. [DOI] [PubMed] [Google Scholar]
- 26.Schwartz BG, Qualls C, Kloner RA, et al. Relation of total and cardiovascular death rates to climate system, temperature, barometric pressure, and respiratory infection. Am J Cardiol. 2015;116:1290–7. doi: 10.1016/j.amjcard.2015.07.050. [DOI] [PubMed] [Google Scholar]
- 27.Sato J. Weather change and pain: A behavioral animal study of the influences of simulated meteorological changes on chronic pain. Int J Biometeorol. 2003;47:55–61. doi: 10.1007/s00484-002-0156-9. [DOI] [PubMed] [Google Scholar]
- 28.Merchant SN, Adams JC, Nadol JB., Jr Pathophysiology of Meniere’s syndrome: Are symptoms caused by endolymphatic hydrops? Otol Neurotol. 2005;26:74–81. doi: 10.1097/00129492-200501000-00013. [DOI] [PubMed] [Google Scholar]
- 29.Pyykko I, Nakashima T, Yoshida T, et al. Meniere’s disease: A reappraisal supported by a variable latency of symptoms and the MRI visualisation of endolymphatic hydrops. BMJ Open. 2013;3:e001555. doi: 10.1136/bmjopen-2012-001555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bohn DA. Environmental effects on the speed of sound. J Audio Eng Soc. 1988;36:223–31. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.