Abstract
Context:
Musculoskeletal injuries (MSIs) are among the most important challenges facing our military. They influence career success and directly affect military readiness. Several methods of screening initial entry training (IET) soldiers are being tested in an effort to predict which soldiers will sustain an MSI and to develop injury-prevention programs. The Army 1-1-1 Fitness Assessment was examined to determine if it could be used as a screening and MSI prediction mechanism in male IET soldiers.
Objective:
To determine if a relationship existed among the Army 1-1-1 Fitness Assessment results and MSI, MSI type, and program of instruction (POI) in male IET soldiers.
Design:
Retrospective cohort study.
Setting:
Fort Benning, Georgia.
Patients or Other Participants:
Male Army IET soldiers (N = 1788).
Main Outcome Measure(s):
The likelihood of sustaining acute and overuse MSI was modelled using separate logistic regression analyses. The POI, run time, push-ups and sit-ups (combined into a single score), and IET soldier age were tested as predictors in a series of linear models.
Results:
With POI controlled, slower run time, fewer push-ups and sit-ups, and older age were positively correlated with acute MSI; only slower run time was correlated with overuse MSI. For both MSI types, cavalry POIs had a higher risk of acute and overuse MSIs than did basic combat training, armor, or infantry POIs.
Conclusions:
The 1-1-1 Fitness Assessment predicted both the likelihood of MSI occurrence and type of MSI (acute or overuse). One-mile (1.6-km) run time predicted both overuse and acute MSIs, whereas the combined push-up and sit-up score predicted only acute MSIs. The MSIs varied by type of training (infantry, basic, armor, cavalry), which allowed the development of prediction equations by POI. We determined 1-1-1 Fitness Assessment cutoff scores for each event, thereby allowing the evaluation to be used as an MSI screening mechanism for IET soldiers.
Key Words: military, injury prevention, musculoskeletal injuries
Key Points
The Army Fitness Assessment is commonly conducted by Army training units and can be used to screen for those initial entry training soldiers most likely to be injured.
This assessment requires no additional specialized equipment, personnel, or time, unlike other screening methods now being tested.
The results allowed for specialized predictions of musculoskeletal injuries in basic combat, infantry, armor, and cavalry training programs of instruction.
Musculoskeletal injuries (MSIs) are the primary medical reason soldiers are unable to deploy and one of the most important factors affecting military readiness.1,2 Estimates suggest that 600 000 soldiers sustain an MSI each year, resulting in more than 2.2 million medical encounters.3,4 An estimated 68 000 soldiers per year are unable to deploy because of non–combat-related MSIs, creating an important readiness concern for our military.5 Physical training and recreational sports are the primary causes of these MSIs.6 The US Army currently takes a multipronged approach to address this problem and increase soldier health and wellness. These efforts include prevention, education, and a soldier-athlete approach to soldier training and medical care. The new Army Performance Triad program (focusing on sleep, nutrition, and exercise), recently launched by Army Medical Command, serves as the cornerstone of these efforts.7
The Army is focusing on both preventing the initial MSI and returning the soldier to fully functional status after MSI. Musculoskeletal injuries are a burden to soldiers in all military operational specialties as well as initial entry training (IET) soldiers. Research8–10 indicated that the best predictor of a future MSI is a previous MSI. Given that physical activity is such an important aspect of a military career, this suggests that MSIs first incurred during IET have a protracted effect on fitness and soldier readiness and may influence long-term career success. Between 19% and 44% of soldiers sustain some type of MSI during IET.6,11 Thus, preventing MSIs during IET likely reduces the occurrence of future MSIs, improves the health and wellness of the soldier, and possibly sets the soldier up for a more successful career. The large number of lost training hours and the additional cadre time needed to ensure that IET soldiers receive needed musculoskeletal care are also costly results of MSIs. Therefore, MSI prevention efforts improve the readiness of the force while decreasing overall medical expenditures and training costs.
Efforts to decrease the MSI rate in IET soldiers include revisions of the Army Physical Readiness Training Plan (exercise regimen),8 assessment of footwear,12–15 improved nutrition,4,7,16 changes in military equipment,14,17,18 increased sleep,7,19,20 and modification to the program of instruction (POI).21–23 Some of these prevention programs are still new, whereas others have shown positive effects on the IET soldier MSI rate.4,8,24
The Army today is focusing on the lower overall fitness levels of incoming recruits and how these affect MSI rates.25–28 Low fitness levels and higher MSI rates are known to be associated.4,24,29 The decreased level of fitness of the incoming recruit mimics the decreased fitness and increased obesity evident in our population as a whole. The challenge is to find a way to identify those recruits who are likely to become injured and develop a physical training program that improves fitness without resulting in MSI.
Developing an effective way to identify soldiers at risk is a vital MSI prevention tool. Multiple methods of screening are being assessed by the various military branches with the goal of identifying recruits or service members who are likely to become injured. Initial work has assessed the Functional Movement Screen, Landing Error Scoring System, and other screens in an effort to predict which individuals may become injured. An easy and effective screen is an important starting point for any effective injury-prevention program.30–32 However, screening programs often require additional equipment, specially trained examiners, and large amounts of time (Figure 1). This is especially problematic for our Reserve and National Guard units, as well as for other organizations that rely on tactical athletes (eg, firefighters, law enforcement, first responders) and may have limited resources. Effective screening is particularly difficult when large numbers of IET soldiers must be assessed upon arrival at the reception station. An ideal course of action would be to identify information already obtained from the IET soldier that could provide important data on MSI susceptibility.
Figure 1.
Army 1-1-1 Fitness Assessment. A, Push-up test. B, Sit-up test. C, 1-mile (1.6-km) run.
A potential screening tool is a modified version of the Army 1-1-1 Fitness Assessment that all soldiers must pass every 6 months.33 This fitness assessment is routinely completed within the first 72 hours of Army IET training. Originally a requirement of the Army standardized physical training field manual 21-20,34 it is now commonly used to place IET soldiers into fitness ability groups on the first or second day of IET.35 The IET soldier has 1 minute each to complete as many push-ups and sit-ups as possible, followed by a timed 1-mi (1.6-km) run. The equipment, experience, and training needed to complete the 1-1-1 Fitness Assessment are the same as for the required Army Physical Fitness Test, making it easy to complete with no additional resources. If the 1-1-1 results can be used to predict which IET soldiers are more likely to incur an MSI, then units may already have the information they need to address MSI prevention measures. The objective of our retrospective study was to review the 1-1-1 results of male IET soldiers from Army IET basic combat training (BCT) and infantry (IN), armor (AR), and cavalry (CAV) units to determine if a relationship was evident among 1-1-1 Fitness Assessment results and reported MSI, MSI type, and POI.
METHODS
All participants were IET soldiers who had completed BCT (9 weeks) or IN (14 weeks), AR (15 weeks), or CAV (16 weeks) 1-station unit training (OSUT). Before training, all IET soldiers complete a medical screening (that includes the age, height, and weight information included in this study) and their fitness for military training is determined. The 1-1-1 Fitness Assessment was completed in the receiving unit within 72 hours of arrival during 2013–2015. The push-up, sit-up, and run assessment was conducted according to Army Physical Fitness Test standards. The assessment was overseen and data recorded by the unit drill sergeants.
The 1-1-1 Assessment consists of a 1-minute push-up test, 1-minute sit-up test, and 1-mi (1.6-km) run test, performed in order, with approximately 10 minutes of rest between portions of the test. Each test is graded following specific standards, and each IET soldier is given a score based on age standards.33 Each trainee is provided a score card and enters his name, social security number, grade, age, and sex. The score card is then given to a scorekeeper who records the results of each section of the test. The testing process is supervised by commanding officers. Exercises were performed according to the following requirements (Figure 1).
Push-Up Test
-
1.
Begin in a forward leaning position.
-
2.
The body is positioned in a straight line from the ankles to the shoulders and must be maintained throughout the push-up.
-
3.
The feet are no more than 12 in (30.5 cm) apart.
-
4.
The participant is required to lower himself until his elbows are at least parallel to the ground and must extend his elbows fully to complete a repetition.
Sit-Up Test
-
1.
Participant begins with his back on the ground and knees bent at a 90° angle.
-
2.
Participant's feet are secured by another soldier.
-
3.
Participant must raise himself upward until the base of the neck is positioned superior to the vertical axis of the spine in the upright position.
-
4.
Participant lowers himself until the scapulae have made contact with the ground.
-
5.
The feet are no wider than 12 in (30.5 cm) apart.
-
6.
The hands are behind the head.
-
7.
The heels and feet must maintain contact with the ground.
For each correctly performed repetition in the push-up and sit-up tests, the scorekeeper states the number performed. Failure to maintain proper form as described results in the repetitions not being counted toward the participant's total.
Run Test
For the run test, each trainee was assigned a number to be worn during the test and was timed. The run test was administered by 2 cadre, designated as the supervisor and the scorekeeper. The test was timed by the supervisor on 2 stopwatches. Once the participant completed the test and crossed the finish line, the supervisor stated the time and the scorekeeper recorded it. The test was administered on a flat running track.
We obtained descriptions of MSI incidents from the Warrior Athletic Training (WAT) Program MSI tracking database and the Army's Armed Forces Health Longitudinal Technology Application (AHLTA) electronic medical records system from brigades of BCT and IN, AR, and CAV OSUT companies that had completed full training cycles. An MSI was defined as any reported musculoskeletal problem that required a trainee to miss training. Acute MSIs (eg, sprain, strain, dislocation, contusion, fracture) occurred from a traumatic event. Overuse MSIs resulted from repeated microtrauma (eg, tendinitis, stress fracture, plantar fasciitis). Musculoskeletal injuries were categorized by the body part (foot, ankle, shin/lower leg, knee, thigh, hip, pelvis, groin, hand, wrist, forearm, upper arm, shoulder, torso, lower back, midback, upper back, neck/cervical, head) reporting system used by the IET soldiers when presenting for morning sick call and type of MSI (acute, overuse). The 1-1-1 data were retrieved from either the records of the training companies or the training brigade database by company cadre. The MSI information was entered into a custom Excel database (version 2013; Microsoft Corp, Redmond, WA) by a WAT athletic trainer blinded to the purpose of the data collection. The 1-1-1 Fitness Assessment information was added to this database by a member of the research team.
Statistical Analysis
Acute MSIs and overuse MSIs were analyzed in separate logistic regression analyses using a step-up procedure to determine which of the assessed variables were most predictive of MSI. Initial differences in fitness (push-ups, sit-ups, and run times) and age were noted among POIs. These differences were confirmed by statistically significant 1-way analyses of variance with POI as a between-subjects factor. Thus, the first-stage models were used to test for differences in the probability of MSI among POIs. Next, while controlling for POI, we assessed variables that affected performance on the 3 parts of the 1-1-1 Assessment. Because push-up and sit-up performances were highly correlated (r = 0.51), these variables were summed into a single variable: FitSum. Similarly, run times (in seconds) were log transformed before being included in the model. This transformation was conducted for 2 reasons: (1) a priori, we did not think the relationship would be linear and (2) although normality is not strictly an assumption of logistic regression, nonnormal variables can distort parameter estimates.36 In the final stage of model building, we included the 2- and 3-way interactions of FitSum, ln (run time), and age. Model fit was assessed using the Wald test (α = .05) and the Akaike information criterion (AIC). The model that yielded a statistically significant Wald test and the smallest AIC was selected as the best model. Analyses were conducted using the R package (version 0.3.0.2; R Core Team, Vienna, Austria) and R Studio and the dplyr package (grammar of data manipulation).
RESULTS
Descriptive Statistics
A total of 1788 male IET soldiers were included in this analysis (mean age = 20.48 ± 3.4 years). The 1-1-1 results are shown in Table 1. Height was 175.8 ± 7.5 cm and weight was 76.7 ± 11.8 kg. (Because of the retrospective nature of these data, height and weight data were complete for only 507 trainees, but these are considered representative of the larger sample.)
Table 1.
Army 1-1-1 Fitness Assessment Results by Program of Instruction (Mean ± SD)
| Program of Instruction |
Age, y |
Sit-Ups, No. |
Push-Ups, No. |
Run Time, s |
Run Time Natural Logarithm |
| Basic combat (n = 808) | 21.5 ± 3.9 | 29.3 ± 8.1 | 25.8 ± 12.2 | 491.6 ± 116.4 | 6.18 ± 0.19 |
| Infantry (n = 577) | 19.5 ± 2.3 | 33.3 ± 7.2 | 29.7 ± 12.1 | 441.4 ± 57.3 | 6.08 ± 0.13 |
| Armor (n = 111) | 20.5 ± 2.2 | 27.2 ± 9.0 | 22.4 ± 10.2 | 513.2 ± 69.1 | 6.23 ± 0.13 |
| Cavalry (n = 292) | 19.6 ± 2.6 | 30.2 ± 8.2 | 28.3 ± 11.8 | 472.2 ± 59.5 | 6.15 ± 0.12 |
| Overall (N = 1788) | 20.48 ± 3.27 | 30.6 ± 8.16 | 27.27 ± 12.17 | 473.5 ± 92.9 | 6.15 ± 0.17 |
With respect to overall MSIs, 503 trainees sustained 1 or more MSIs, whereas 1285 trainees had no documented MSI. For the specific MSI types, 308 trainees incurred acute MSIs, whereas 1480 trainees did not, and 222 sustained overuse MSIs, whereas 1566 did not. Note that these values do not sum perfectly as it was possible for trainees to sustain both acute and overuse injuries as separate events.
Descriptive statistics for mean fitness by POI are shown in Table 1. Differences were evident in age (F3,1748 = 55.7, P < .001), push-ups (F3,1748 = 18.9, P < .001), sit-ups (F3,1748 = 37.0, P < .001), and run time (F3,1748 = 52.9, P < .001). (To meet normality assumptions, the natural logarithm of run time was analyzed.) Post hoc t tests for these main effects are presented in Table 1. Critically, group differences in fitness suggest we need to control for POI when predicting MSI based on 1-1-1 performance.
The proportion of injured and uninjured IET soldiers in each POI is given in Table 2. Logistic regression predicting acute MSI as a function of POI revealed differences among the groups (χ23 = 15.74, P = .001; see step 2 of Table 3). Post hoc 2 × 2 contingency tables were constructed to compare the POIs. The CAV group had higher rates of MSIs than the BCT (P < .001) and IN (P < .001) groups. None of the other comparisons were significant.
Table 2.
Acute and Overuse Injuries by Program of Instruction
| Injuries |
Uninjured |
Injured |
Proportion Injured |
| Acute | |||
| Basic combat | 677 | 131 | 0.16 |
| Infantry | 493 | 84 | 0.15 |
| Armor | 92 | 19 | 0.17 |
| Cavalry | 218 | 74 | 0.25 |
| Overuse | |||
| Basic combat | 711 | 97 | 0.12 |
| Infantry | 519 | 58 | 0.10 |
| Armor | 97 | 14 | 0.13 |
| Cavalry | 239 | 53 | 0.18 |
Table 3.
Coefficients From the Best-Fitting Logistic Regression Model Predicting Acute Musculoskeletal Injurya
| Step |
Coefficients |
Estimate |
Standard Error |
Z Value |
P Value |
Δ Deviance |
Akaike Information Criterion |
| 1 | Intercept | −1.566 | 0.083 | −18.86 | <.001 | 1645.0 | |
| 2 | Point of instruction 1 | −0.007 | 0.273 | −0.02 | .97 | 15.74 | 1635.3 |
| Point of instruction 2 | 0.727 | 0.291 | 2.49 | .01 | |||
| Point of instruction 3 | −0.156 | 0.288 | 0.54 | .59 | |||
| 3 | ln (Run.c) | 1.172 | 0.398 | 2.94 | <.01 | 14.60 | 1622.7 |
| 4 | FitSum.c | −0.010 | 0.004 | −2.49 | .01 | 5.61 | 1619.0 |
| 5b | Age.c | 0.045 | 0.019 | 2.35 | .02 | 5.26 | 1615.8 |
Abbreviations: Age.c, centered mean of ages; Δ Deviance, change in deviance compared with the model in the previous step; FitSum.c, centered mean of the push-up and sit-up variables combined; ln (Run.c), centered mean of the natural logarithm of run time.
Points of instruction 1 through 3 are simple contrast codes for the different programs of instruction (the intercept is thus equivalent to the grand mean). Null deviance = 1643.0 with 1787 degrees of freedom. Adding the interactions of ln (Run.c), FitSum.c, and Age.c in step 6 (not shown) did not improve the fit of the model.
Denotes the best-fitting model according to Akaike information criterion and Δ Deviance (P < .05).
Similarly, logistic regression predicting overuse MSI as a function of POI revealed differences among the groups (χ23 = 11.16, P = .011; see step 2 of Table 4). We constructed post hoc 2 × 2 contingency tables to compare the POIs and found that the CAV group had a higher rate of MSI than the BCT (P = .013) and IN (P = .001) groups. None of the other comparisons were significant.
Table 4.
Coefficients from the Best-Fitting Logistic Regression Model Predicting Overuse Musculoskeletal Injurya
| Step |
Coefficients |
Estimate |
Standard Error |
Z Value |
P Value |
Δ Deviance |
Akaike Information Criterion |
| 1 | Intercept | −1.983 | 0.096 | −20.76 | <.001 | 0 | 1343.5 |
| 2 | Point of instruction 1 | 0.026 | 0.309 | 0.08 | .93 | 11.2 | 1338.3 |
| 2 | Point of instruction 2 | 0.683 | 0.330 | 2.07 | .04 | ||
| 2 | Point of instruction 3 | 0.152 | 0.329 | 0.46 | .64 | ||
| 3b | ln (Run.c) | 1.972 | 0.423 | 4.66 | <.001 | 26.4 | 1313.9 |
| 4 | FitSum.c | −0.006 | 0.004 | −1.44 | .15 | 1.9 | 1314.0 |
| 5 | Age.c | 0.028 | 0.022 | 1.29 | .20 | 1.3 | 1314.4 |
Abbreviations: Age.c, centered mean of ages; Δ Deviance, change in deviance compared with the model in the previous step; FitSum.c, centered mean of the push-up and sit-up variables combined; ln (Run.c), centered mean of the natural logarithm of run time.
Points of instruction 1 through 3 are simple contrast codes for the different programs of instruction (the intercept is thus equivalent to the grand mean). Null deviance = 1643.0 with 1787 degrees of freedom. Adding the interactions of ln (Run.c), FitSum.c, and Age.c in step 6 (not shown) did not improve the fit of the model.
Denotes the best-fitting model according to Akaike information criterion and Δ Deviance (P < .05).
Run times, FitSum, and age were significantly related to the odds of incurring an acute MSI. As shown in Table 3, run time (natural log) and age were positively associated with MSI, and FitSum (the sum of push-ups and sit-ups on the 1-1-1) was negatively associated with MSI. This model, containing contrast codes for POI and centered variables for 1-1-1 performance, was a statistically significant improvement over earlier models as measured by both the Wald test (χ21 = 5.26, P = .02) and the AIC (steps 1–4). A subsequent model that added the interactions of these factors did not improve the fit of the model. Given this lack of significant interactions, the main-effects model is presented.
For overuse MSIs, while controlling for the other variables in the model, only run times in the 1-1-1 were significantly related to the odds of being injured. As shown in Table 4, run time (natural log) was positively associated with MSI. This model (step 3), containing contrast codes for POI and the centered natural log of run times, was a significant improvement over earlier models as measured by the Wald test (χ21 = 26.39, P < .001) and the AIC. Adding FitSum, age, and the interactions for the 1-1-1 variables did not improve the fit of the model. The full model, including the nonsignificant factors of FitSum and age, is presented in Table 4.
To provide practitioners with a flexible method for making predictions about the likelihood of MSI, we present prediction equations for acute MSIs for each POI:
These prediction equations are statistically equivalent to the model in Table 3 with 2 key exceptions: (1) the POI contrasts have already been incorporated, so there is a unique intercept for each POI, and (2) the coefficients in Table 3 are based on mean-centered data to ease the interpretation of the regression, whereas the coefficients in the equations are based on raw data. Thus, to use the equations above, simply enter the run time (in seconds), the combined FitSum score (total number of push-ups + sit-ups), age (in years), and solve for the predicted logit,
 . As the logit (eg,
. As the logit (eg,
 ) is the natural log of the odds, exponentiate the results to obtain the odds of MSI,
) is the natural log of the odds, exponentiate the results to obtain the odds of MSI,
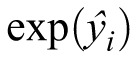 , or take
, or take
 to find the conditional probability of MSI. (We have made available an Excel spreadsheet that automatically performs these calculations [see the Supplemental Figure, available online at http://dx.doi.org/10.4085/1062-6050-51.9.09.S1.]).
to find the conditional probability of MSI. (We have made available an Excel spreadsheet that automatically performs these calculations [see the Supplemental Figure, available online at http://dx.doi.org/10.4085/1062-6050-51.9.09.S1.]).
To provide practitioners with a flexible method for making predictions about the likelihood of MSI, we present prediction equations for overuse MSIs for each POI:
Similar to the prediction equations for acute MSIs, the overuse equations have unique intercepts for each POI, and the run time, FitSum, and age predictors are in raw units (these predictions are otherwise statistically equivalent to the mean-centered equations in Table 4). To predict the risk of MSI for a specific IET soldier, enter the run time (in seconds), combined FitSum score (in total repetitions), and age (in years) and solve for the predicted logit,
 . As the logit is the natural log of the odds, exponentiate the results to obtain the odds of MSI,
. As the logit is the natural log of the odds, exponentiate the results to obtain the odds of MSI,
 , or take
, or take
 to find the conditional probability of MSI. (We have provided an Excel spreadsheet to conduct these calculations.)
to find the conditional probability of MSI. (We have provided an Excel spreadsheet to conduct these calculations.)
DISCUSSION
The goal of our retrospective study was to determine if the current 1-1-1 completed in most training units during the first 72 hours of training could predict which Army soldiers would sustain an MSI during IET. We also wanted to determine if the type of MSI sustained could be predicted and if this varied with the POI. Numerous screening methods are being investigated as ways to reduce the number of MSIs across the force.28–31 These often require specially trained individuals to conduct the screenings and analyze the results, specialized equipment, and extensive person-hours and time lost from training. If an assessment that is already being conducted could provide predictive MSI information without additional people, training, equipment, or time lost, we could begin to immediately use these data to develop MSI prevention programs.
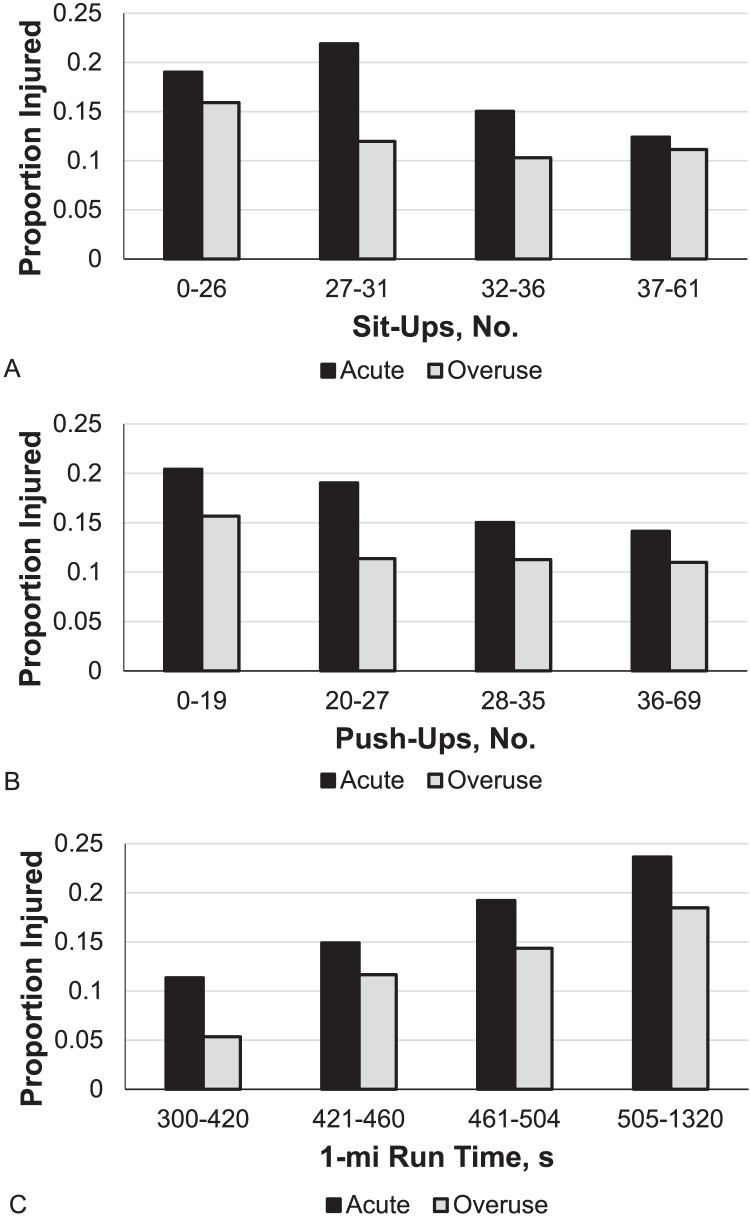
Our most important finding was that the 1-1-1 Assessment could predict if the IET soldier was likely to sustain an MSI. More importantly, it predicted if the IET soldier was more likely to sustain either an acute or overuse MSI when controlling for the age of the IET soldier and the POI. Specifically, 1-mi (1.6-km) run times were positively associated with overuse and acute MSIs. The FitSum score (combined push-up and sit-up scores) did not predict overuse MSIs but was negatively associated with acute MSIs. In other words, the higher the FitSum score, the less likely the IET soldier was to sustain an acute MSI. This relationship can be seen in Figure 2, which depicts the proportion of injured IET soldiers for each quartile of the 1-1-1. The poorest performing quartiles for each assessment (0–19 push-ups, 0–26 sit-ups, and run times >504 seconds) all had higher incidences of acute and overuse MSIs. The IET soldiers in a better-performing quartile were less likely to sustain an acute or overuse MSI (acute/overuse MSI specificity for push-ups was 0.74/0.74; sit-ups, 0.74/0.74; and run time, 0.77/0.76 with a minimum negative predictive value = 0.84). The IET soldiers in the lower-performing quartile were more likely to sustain an MSI, but the prediction was not as sensitive as in the higher quartile (ie, acute/overuse MSI sensitivity for push-ups was 0.32/0.34; sit-ups, 0.30/0.35; and run time, 0.34/0.37). With this understanding, we recommend that IET soldiers in the poorest-performing quartile of the 1-1-1 (fewer than 19 push-ups, fewer than 26 sit-ups, and slower than 8 minutes, 25 seconds on the 1-mi [1.6-km] run) then be further screened for the likelihood of MSI and to determine specific prevention interventions.
Figure 2.
The proportion of initial entry training soldiers who experienced either an acute (black bars) or overuse (gray bars) musculoskeletal injury by performance quartile on each part of the Army 1-1-1 Physical Assessment.
The 1-1-1 results are already used by the cadre to group IET soldiers into running-ability groups in an effort to improve fitness training and reduce MSIs. However, using the specific results of an assessment that is already being completed to determine those needing MSI prevention interventions could be a powerful tool in reducing MSI rates in the IET population. Although previous researchers28,37 associated a higher risk of MSI with a lower level of physical fitness, our data provide the first objective quantification of MSI risk for Army IET soldiers in both BCT and OSUT and specific to individual POIs.
We first assessed MSI, regardless of MSI type. We then considered acute and overuse MSIs independently to determine if the 1-1-1 could predict which type of MSI might be sustained. When the dependent variable in the regression model was simply MSI, regardless of type (acute versus overuse), the pattern of results was identical to the models for acute MSI in terms of the direction and statistical significance of the coefficients (however, the magnitudes of the individual coefficients were different). Acute MSIs were considered ankle sprains, muscle strains, contusions, fractures, and dislocations. For every 1-point increase in the FitSum score (eg, 1 additional push-up or sit-up), the odds of an acute MSI decreased by approximately 1%. This was an unexpected finding. Research38–40 suggested that those with greater hip-flexor, upper body, and core strength may be less likely to incur an acute MSI, which indicates that strength in the core and trunk areas affects leg swing,40 hip-flexor strength may affect knee function,38,39 and core strength can be the limiting factor in upper body strength movements.40 Higher FitSum–scoring individuals likely have had more movement experience, resulting in better neuromotor control and enabling them to better control their bodies during the challenging physical activity required during IET training.41 The 1-mi (1.6-km) run time was also a predictor of acute MSI: here we used a log transformation of the run time in seconds to present the run scores in a normal distribution. A 1-point increase in the natural log of run times (ie, slower run time, less cardiovascular fitness) resulted in an almost 300% increase in the odds of sustaining an acute MSI. For instance, the conditional probability of acute MSI for an AR IET soldier of average age with an average FitSum score and a 6-minute run time (natural logarithm [360] = 5.89) was 0.118 (approximately 12% chance of an acute MSI). Conversely, the conditional probability for an otherwise identical IET soldier with a 9-minute run time (natural logarithm [540] = 6.30) was 0.178 (approximately 18% chance of an acute MSI). This result was more expected, as poor cardiovascular fitness has been associated with increased MSIs in military populations.42–44 With fatigue, the IET soldier is more likely to stumble, fall, or sprain an ankle. This supports the idea that poor cardiovascular fitness is a serious contributor to the increased MSI rate in the military. We developed equations that allow for prediction of acute MSI by POI.
Overuse MSIs are an even greater problem in this population.8,45 Overuse MSIs develop over time from repeated forces that produce microtrauma in muscle, tendons, bones, and joints. They become chronic MSIs and typically take much longer to resolve than acute MSIs (excluding surgical repairs or full fractures). Overuse MSIs include tendinitis and tenosynovitis, stress fractures and stress reactions, knee overuse syndromes (patellar tendinitis, patellofemoral syndrome, etc), plantar fasciitis, fascial dysfunction, and similar conditions. When we controlled for the other factors in the model, FitSum did not significantly predict overuse MSIs. For every 1-point increase in FitSum score, the odds of an overuse MSI decreased by 0.6%. However, for every 1-point increase in the natural logarithm (run time; ie, slower run time), there was a 700% increase in the odds of an overuse MSI. That is, for an IN IET soldier of average age, average FitSum, and 6-minute run time (natural logarithm [360] = 5.89), the conditional probability of an overuse MSI was 0.068 (approximately 7% chance of an MSI). For an otherwise identical IET soldier with a 9-minute run time (natural logarithm [540] = 6.30), the conditional probability was 0.133 (approximately 13% chance of an MSI). The relationship between cardiovascular fitness and overuse MSIs was expected.8,45 Overuse MSIs result from forces at a level or frequency to which the body cannot adapt. As the IET soldier fatigues, the biomechanics of running or movement are altered and stress on the structures may be increased, causing the breakdown of tissues to occur at a higher rate than tissue remodeling and resulting in MSI. Moreover, those who are less cardiovascularly fit are working closer to their maximum level of effort than their more-fit counterparts. The more-fit individuals can perform longer without exhaustion, fatigue slower, and recover more quickly. The less-fit individuals reach higher levels of exhaustion and experience slower or less complete physiologic recovery as the challenging and unaccustomed physical demands of the IET training environment compound daily.42,46 Eventually, the body cannot recover and MSI occurs.47 Equations were developed that allow for the prediction of overuse MSI by POI.
We studied 4 types of combat arms training occurring at the same physical location, which provided a unique opportunity to compare the 4 POIs for differences in entry fitness levels and MSI rates while controlling for reception unit policies and protocols, physical and training environment, command structure, and training policies. Cadre often rotate among units with fairly consistent training expectations, resources, and equipment; different units share training locations such as land navigation sites and ranges. Differences in MSI rates should then be due to differences in POI or fitness levels and other IET soldier characteristics (eg, mindset, motivation). Multiple companies (100–220 IET soldiers/company) were included in each POI group to control for the influence of the command climate. Basic combat training is for soldiers who will go on to be trained for many different types of Army occupations (eg, mechanic, translator, medic) and lasts 9 weeks. Infantry training includes all soldiers going into the infantry and lasts 14 weeks. The additional weeks consist of more ruck marches and range time and increased physical training. Armor training includes soldiers who will be manning tanks and lasts 15 weeks. Training includes time in, on, and around tanks and tank maintenance. Cavalry training includes all soldiers who will be cavalry scouts and involves working with and in Bradley fighting vehicles and other vehicles for 16 weeks in addition to extra ruck marches and land navigation, which are known to produce MSI. Both armor and cavalry trainees spend time on and around vehicles, which provides additional opportunity for MSIs, especially the acute types.
Among the possible limitations of our study was the fact that the training brigades at Fort Benning have had ongoing MSI prevention programs for up to 6 years, so MSI rates (especially those for chronic MSIs) may be lower than those reported elsewhere. The MSI data for this study were taken from the data collected daily by the WAT Program, which embeds 2 athletic trainers at the battalion level for each unit. Data on all MSIs and musculoskeletal problems are collected daily in a specialized Excel spreadsheet. This information is also entered into the AHLTA Army electronic medical records system. In most cases, IET soldiers are sent to the WAT program before being sent to the troop medical center (TMC). The WAT data collection includes information on all musculoskeletal concerns of all severities. If the program was not used in the battalion because of the time and effort involved, many of these problems would likely not be reported to the TMC until they became more severe. For this reason, the WAT data often include higher numbers of MSIs than data from AHLTA medical records systems at other locations. There may have been some variation in how health care providers entered the MSI identifiers, although they were trained as a group. The IET soldiers may have gone to the TMC or another provider instead of the WAT program and thereby not been included in this analysis. However, IET soldiers who go to the TMC are sent to WAT for follow-up in most cases.
Other limitations include the retrospective nature of this study. Cause and effect cannot be determined, and probabilities can only be calculated from available data. Some differences are likely in the physical training intensities of the different units that could have affected the analysis of the differences among POIs. Currently Fort Benning trains only male soldiers in these units, and these findings may be different for female IET soldiers.
CONCLUSIONS
The 1-1-1 Assessment currently conducted by most training units can predict the likelihood of acute and overuse MSIs in IET soldiers. Controlling for POI, 1-mi (1.6-km) run times predicted both overuse and acute MSIs, whereas push-up and sit-up scores predicted only acute MSIs. These results suggest that the 1-1-1 could be a quick and easy initial screen for all IET soldiers. At the IET soldiers' present levels of fitness, the 1-1-1 test would place approximately 25% into a low-fitness group. Low-fitness IET soldiers could then be put into a fitness-improvement unit until they were deemed physically ready to complete IET training.46,47 This is not a new idea, and different methods to pretrain recruits are being tested. If available resources cannot provide a remedial fitness program for this large a group, then additional screening could be completed on only the lower 25%, whose 1-1-1 performance indicates a higher probability of MSI. Screening only the lower 25% would make a more thorough additional screening plausible. Several more-involved screenings are currently being investigated for use in this population (eg, Functional Movement Screen, Landing Error Scoring System, Y-Balance test). These may provide more detailed analysis and direct MSI reduction interventions (above and beyond fitness improvement) at the IET soldiers most likely to become injured. This combination could save extensive time and money by avoiding screening of all the IET soldiers, and resources could then be concentrated to serve those most in need of intervention.
Supplementary Material
SUPPLEMENTAL MATERIAL
Supplemental Figure. Spreadsheet to determine the conditional probability of musculoskeletal injury.
Found at DOI: http://dx.doi.org/10.4085/1062-6050-51.9.09.S1
REFERENCES
- 1. Ruscio BA, Jones BH, Bullock SH, et al. A process to identify military injury prevention priorities based on injury type and limited duty days. Am J Prev Med. 2010; 38 suppl 1: S19– S33. [DOI] [PubMed] [Google Scholar]
- 2. Hauret KG, Jones BH, Bullock SH, Canham-Chervak M, Canada S. . Musculoskeletal injuries description of an under-recognized injury problem among military personnel. Am J Prev Med. 2010; 38 suppl 1: S61– S70. [DOI] [PubMed] [Google Scholar]
- 3. Army Medical Surveillance Activity. Absolute and relative morbidity burdens attributable to various illnesses and injuries, U.S. Armed Forces, 2012. MSMR. 2013; 20 4: 5– 10. [PubMed] [Google Scholar]
- 4. Nindl BC, Williams TJ, Deuster PA, Butler NL, Jones BH. . Strategies for optimizing military physical readiness and preventing musculoskeletal injuries in the 21st century. US Army Med Dep J. Oct-Dec 2013: 5– 23. [PubMed] [Google Scholar]
- 5. Sample D. . Army wants more soldiers back on deployable status. US Army Web site. https://www.army.mil/article/67037/Army_wants_more_Soldiers_back_on_deployable_status. Accessed July 13, 2016. [Google Scholar]
- 6. Prevention and Control of Musculoskeletal Injuries Associated With Physical Training. Washington, DC: Department of the Army, US Department of Defense; 2011. Technical bulletin Med-592. [Google Scholar]
- 7. The performance triad. Army Medicine Web site. http://armymedicine.mil/Pages/performance-triad.aspx. Accessed July 15, 2015. [Google Scholar]
- 8. Knapik JJ, Hauret KG, Arnold S, et al. Injury and fitness outcomes during implementation of physical readiness training. Int J Sports Med. 2003; 24 5: 372– 381. [DOI] [PubMed] [Google Scholar]
- 9. Jones BH, Hansen BC. . An armed forces epidemiological board evaluation of injuries in the military. Am J Prev Med. 2000; 18 suppl 3: 14– 25. [DOI] [PubMed] [Google Scholar]
- 10. Fulton J, Wright K, Kelly M, et al. Injury risk is altered by previous injury: a systematic review of the literature and presentation of causative neuromuscular factors. Int J Sports Phys Ther. 2014; 9 5: 583– 595. [PMC free article] [PubMed] [Google Scholar]
- 11. Sefton FM. . WAT Program Year End Command Contract Report. Ft Benning, GA: Auburn University; 2014. [Google Scholar]
- 12. Jones BH, Knapik JJ, Daniels WL, Toner MM. . The energy cost of women walking and running in shoes and boots. Ergonomics. 1986; 29 3: 439– 443. [DOI] [PubMed] [Google Scholar]
- 13. Kaufman KR, Brodine SK, Shaffer RA, Johnson CW, Cullison TR. . The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999; 27 5: 585– 593. [DOI] [PubMed] [Google Scholar]
- 14. Knapik JJ. . Injuries and injury prevention during foot marching. J Spec Oper Med. 2014; 14 4: 131– 135. [DOI] [PubMed] [Google Scholar]
- 15. Knapik JJ. . Prevention of foot blisters. J Spec Oper Med. 2014; 14 2: 95– 97. [DOI] [PubMed] [Google Scholar]
- 16. Teyhen D, Bergeron MF, Deuster P, et al. Consortium for health and military performance and American College of Sports Medicine Summit: utility of functional movement assessment in identifying musculoskeletal injury risk. Curr Sports Med Rep. 2014; 13 1: 52– 63. [DOI] [PubMed] [Google Scholar]
- 17. Knapik JJ, Steelman R, Hoedebecke K, et al. Risk factors for closed-head injuries during military airborne operations. Aviat Space Environ Med. 2014; 85 2: 105– 111. [DOI] [PubMed] [Google Scholar]
- 18. Knapik JJ, Steelman R, Hoedebecke K, et al. Injury incidence with T-10 and T-11 parachutes in military airborne operations. Aviat Space Environ Med. 2014; 85 12: 1159– 1169. [DOI] [PubMed] [Google Scholar]
- 19. O'Hara R, Henry A, Serres J, Russell D, Locke R. . Operational stressors on physical performance in special operators and countermeasures to improve performance: a review of the literature. J Spec Oper Med. 2014; 14 1: 67– 78. [DOI] [PubMed] [Google Scholar]
- 20. Wright JE, Vogel JA, Sampson JB, Knapik JJ, Patton JF, Daniels WL. . Effects of travel across time zones (jet-lag) on exercise capacity and performance. Aviat Space Environ Med. 1983; 54 2: 132– 137. [PubMed] [Google Scholar]
- 21. Knapik JJ, Bullock SH, Canada S, et al. Influence of an injury reduction program on injury and fitness outcomes among soldiers. Inj Prev. 2004; 10 1: 37– 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Knapik J, Harman E, Reynolds K. . Load carriage using packs: a review of physiological, biomechanical and medical aspects. Appl Ergon. 1996; 27 3: 207– 216. [DOI] [PubMed] [Google Scholar]
- 23. Huang GD, Feuerstein M. . Identifying work organization targets for a work-related musculoskeletal symptom prevention program. J Occup Rehabil. 2004; 14 1: 13– 30. [DOI] [PubMed] [Google Scholar]
- 24. Molloy JM, Feltwell DN, Scott SJ, Niebuhr DW. . Physical training injuries and interventions for military recruits. Mil Med. 2012; 177 5: 553– 558. [DOI] [PubMed] [Google Scholar]
- 25. Niebuhr DW, Scott CT, Powers TE, et al. Assessment of recruit motivation and strength study: preaccession physical fitness assessment predicts early attrition. Mil Med. 2008; 173 6: 555– 562. [DOI] [PubMed] [Google Scholar]
- 26. Deuster PA, O'Connor FG, Henry KA, et al. Human performance optimization: an evolving charge to the Department of Defense. Mil Med. 2007; 172 11: 1133– 1137. [DOI] [PubMed] [Google Scholar]
- 27. Knapik JJ. . The importance of physical fitness for injury prevention: part 2. J Spec Oper Med. 2015; 15 2: 112– 115. [DOI] [PubMed] [Google Scholar]
- 28. Knapik JJ. . The importance of physical fitness for injury prevention: part 1. J Spec Oper Med. 2015; 15 1: 123– 127. [PubMed] [Google Scholar]
- 29. Taanila H, Hemminki AJ, Suni JH, Pihlajamaki H, Parkkari J. . Low physical fitness is a strong predictor of health problems among young men: a follow-up study of 1411 male conscripts. BMC Public Health. 2011; 11: 590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Knapik JJ, Cosio-Lima LM, Reynolds KL, Shumway RS. . Efficacy of functional movement screening for predicting injuries in coast guard cadets. J Strength Cond Res. 2015; 29 5: 1157– 1162. [DOI] [PubMed] [Google Scholar]
- 31. O'Connor FG, Deuster PA, Davis J, Pappas CG, Knapik JJ. . Functional movement screening: predicting injuries in officer candidates. Med Sci Sports Exerc. 2011; 43 12: 2224– 2230. [DOI] [PubMed] [Google Scholar]
- 32. Teyhen DS, Shaffer SW, Umlauf JA, et al. Automation to improve efficiency of field expedient injury prediction screening. J Strength Cond Res. 2012; 26 suppl 2: S61– S72. [DOI] [PubMed] [Google Scholar]
- 33. FM 21-20: Physical Fitness Training. Washington, DC: Department of the Army, US Department of Defense; 1998. [Google Scholar]
- 34. US Army Training and Doctrine Command. TRADOC Standardized Physical Training Guide. Fort Eustis, VA: US Army Training and Doctrine Command; 2003. [Google Scholar]
- 35. FM 7-22 Army Physical Readiness Training. Washington, DC: Department of the Army; 2012. [Google Scholar]
- 36. Osbourne J. . Best Practices in Logistic Regression. Thousand Oaks, CA: SAGE Publications Inc; 2015. [Google Scholar]
- 37. Lisman P, O'Connor FG, Deuster PA, Knapik JJ. . Functional movement screen and aerobic fitness predict injuries in military training. Med Sci Sports Exerc. 2013; 45 4: 636– 643. [DOI] [PubMed] [Google Scholar]
- 38. Nadler SF, Malanga GA, DePrince M, Stitik TP, Feinberg JH. . The relationship between lower extremity injury, low back pain, and hip muscle strength in male and female collegiate athletes. Clin J Sport Med. 2000; 10 2: 89– 97. [DOI] [PubMed] [Google Scholar]
- 39. Nadler SF, Malanga GA, Bartoli LA, Feinberg JH, Prybicien M, Deprince M. . Hip muscle imbalance and low back pain in athletes: influence of core strengthening. Med Sci Sports Exerc. 2002; 34 1: 9– 16. [DOI] [PubMed] [Google Scholar]
- 40. McGill S. . Core training: evidence translating to better performance and injury prevention. Strength Cond J. 2010; 32 3: 33– 46. [Google Scholar]
- 41. Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. . Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005; 330 7489: 449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bell NS, Mangione TW, Hemenway D, Amoroso PJ, Jones BH. . High injury rates among female army trainees: a function of gender? Am J Prev Med. 2000; 18 suppl 3: 141– 146. [DOI] [PubMed] [Google Scholar]
- 43. Grier TL, Morrison S, Knapik JJ, Canham-Chervak M, Jones BH. . Risk factors for injuries in the U.S. Army Ordnance School. Mil Med. 2011; 176 11: 1292– 1299. [DOI] [PubMed] [Google Scholar]
- 44. Knapik JJ, Sharp MA, Canham-Chervak M, Hauret K, Patton JF, Jones BH. . Risk factors for training-related injuries among men and women in basic combat training. Med Sci Sports Exerc. 2001; 33 6: 946– 954. [DOI] [PubMed] [Google Scholar]
- 45. Popovich RM, Gardner JW, Potter R, Knapik JJ, Jones BH. . Effect of rest from running on overuse injuries in army basic training. Am J Prev Med. 2000; 18 suppl 3: 147– 155. [DOI] [PubMed] [Google Scholar]
- 46. Knapik JJ, Canham-Chervak M, Hoedebecke E, et al. The fitness training unit in U.S. Army basic combat training: physical fitness, training outcomes, and injuries. Mil Med. 2001; 166 4: 356– 361. [DOI] [PubMed] [Google Scholar]
- 47. Knapik JJ, Darakjy S, Hauret KG, et al. Increasing the physical fitness of low-fit recruits before basic combat training: an evaluation of fitness, injuries, and training outcomes. Mil Med. 2006; 171 1: 45– 54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.