Abstract
Context:
Although inactivity, being overweight, smoking, and a history of injury are identified as risk factors for poor health and injury, few authors have examined their association on physical performance. Young adults may be more likely to adopt healthier lifestyles if they understand the effect of health behaviors on performance.
Objective:
To determine the association of being overweight, smoking, inactivity, and a history of injury with physical performance.
Design:
Cross-sectional study.
Setting:
Military population.
Patients or Other Participants:
Active-duty service members (N = 1466; 1380 men, 86 women; age = 24.7 ± 5.0 years; body mass index = 26.7 ± 3.4 kg/m2).
Main Outcome Measure(s):
Participants performed 8 measures (the triple-crossover hop for distance, the 6-m timed-hop test, the Functional Movement Screen, the Lower Quarter Y-Balance Test, the Upper Quarter Y-Balance Test, and the 3-event Army Physical Fitness Test) for evaluation of endurance, strength, muscular endurance, power, agility, balance, and motor control. Participants were categorized based on the number of health risk factors present. Using an analysis of covariance, we assessed the relationship between risk factors and physical performance with age and sex as covariates.
Results:
Compared with those who had no risk factors (27.9% of men, 34.9% of women), physical performance was worse in those who had 1, 2, or 3 to 4 risk factors present by 4.3%, 6.7%, and 10.3%, respectively. Decrements in performance for those with 3 to 4 risk factors ranged from 3.3% to 14.4%.
Conclusions:
An unhealthy lifestyle habit or a history of injury was negatively associated with physical performance. Physical performance decrements were associated with the number of risk factors present. Understanding how risk factors contribute to decreased physical performance may enable clinicians to improve compliance with injury-prevention programs in occupational settings in which a young and relatively healthy workforce may be more concerned about performance than health.
Key Words: functional movement, health, injury prediction, risk factors
Key Points
Physical performance was worse in those with health risk factors; performance was lowest in those with 3 to 4 health risk factors.
Risk factors can be responsible for a 10- to 47-point decrease in scores on the Army Physical Fitness Test.
Future researchers should determine if strategies focused on improving performance may be more effective in decreasing health risk factors in a relatively young and healthy population.
Substantial evidence exists that risk factors negatively affect health. Specifically, physical inactivity, being overweight, smoking, and a history of injury have been identified as having negative associations with health.1–4 Less clear is the association between these health risk factors and physical performance. Defining that association is of particular interest to organizations that value both health and physical performance. The US Army, in addition to funding health care for its members, must ensure optimal physical capability for mission readiness. If interventions that decrease risk factors for poor health are prioritized with a new focus on improving performance, this may speak to the soldier's goal of a high performance level with an overall result of improved force health. The health risk factors noted earlier (physical inactivity, being overweight, smoking, and a history of injury) are of specific interest given the substantial research on them and their effects on military readiness.5,6
In the military, the number of occupations requiring only light activity (predominantly sitting at a desk), the number of miles spent in a vehicle, and the number of hours spent in front of a computer or television continue to increase. Physical inactivity has been associated with a host of negative health effects and is positively associated with mortality.1 Strong evidence indicates that recruits with low levels of aerobic capacity, muscular endurance, and physical activity are at risk for musculoskeletal injuries from a physical training regimen during initial army training.5 Many believe that all active-duty army soldiers maintain an “active” lifestyle as part of their regular training and that they are therefore a fit population across the board. However, despite the mandatory physical training requirements associated with military service, a recent survey showed that only 63.1% of service members reported at least 150 minutes of moderate activity per week and only 42.6% reported at least 150 minutes of vigorous physical activity per week.6
Across the nation, as physical inactivity increases, the percentage of US individuals who are overweight or obese continues to rise.3 The medical costs associated with obesity totaled $147 billion in 2008, and obesity is a risk factor associated with the most common causes of death.1 A higher body mass index (BMI) has been identified as a risk factor for diabetes and cardiovascular disease (eg, heart disease and hypertension).7 In addition to having a negative association with health, higher BMI values have been associated with an increased risk for sustaining a musculoskeletal injury.8 In a large population-based study, the odds of sustaining an injury were 15% greater for those considered overweight, which increased incrementally up to 48% greater with each progressive class of obesity (I to III).8 In the military, a higher BMI is also associated with a higher prevalence of injury, illness, and cost of care compared with those of normal weight.9 Despite the military's mandated height and weight standards, a recent survey demonstrated 51.2% to be overweight and only 35.7% reported a healthy weight.6
Smoking is another risk factor that is negatively associated with health.2 Smoking also adversely affects functional outcomes independent of the nature or severity of musculoskeletal injury (relative risk = 1.34).10 Smoking is a documented risk factor for injury across a variety of populations and has a negative association with specific musculoskeletal conditions (eg, persistent low back pain,11 shoulder12 and lower extremity13 injuries). Specific to the military setting, recruits with a history of smoking 1 month before the start of basic training had higher rates of musculoskeletal injury than those who did not have such a history (odds ratio [OR] = 1.5), and the relationship was strongest for overuse injuries.14 Smoking has also been associated with time-loss injuries (1 or more days of limited duty) in both male and female soldiers during basic training and with premature discharge from military service.5,15 These studies did not address smokeless tobacco use.
A history of injury negatively influences future physical activity levels and overall health.16 Additionally, the most prominent risk factor identified in prospective injury risk studies in athletes has been a previous injury.4 For example, it is estimated that approximately 1 in 4 young active athletes who undergo anterior cruciate ligament reconstruction surgery will sustain a second knee injury.17 Previous injury increases the risk for future injury in military personnel.15 Specifically, trainees with a previous ankle sprain were more likely to sustain lower extremity overuse injuries.18 Furthermore, musculoskeletal complaints are a risk factor for early discharge from the military.9,15
Although there is limited research investigating the association of health risk factors with occupational or physical performance, Leyk et al19 studied 10- to 25-year olds and found that even a single risk factor (weight, smoking status, or physical activity level) associated with an unhealthy lifestyle could impair physical performance. Other researchers20 have suggested that risk-mitigation strategies may result in improved compliance if the strategy can also enhance performance. Based on the need to better understand the association between health risk factors and physical performance in a military setting, the primary purpose of our study was to determine if health risk factors (inactivity, increased body mass, smoking, and a history of injury) were associated with a broad range of physical performance measures, including aerobic endurance, strength, power, functional movement, balance, and core stability in a military population. A secondary purpose was to assess the independent associations of inactivity, increased body mass, smoking, and prior injury with physical performance. We hypothesized that the number of health risk factors would have an inverse relationship with physical performance measures in a military population.
METHODS
The Military Power, Performance, and Prevention trial was a 1-year prospective cohort trial. The primary aim of the trial was to develop algorithms that predict injury in soldiers using baseline health, physical performance, and biopsychosocial factors. Participants completed a survey focused on their health and injury history and a series of physical performance measures. Our cross-sectional study targeted the data collected at baseline that was associated with health risk factors and physical performance.
Study Participants
Requirements for participation were being an active-duty soldier between 18 and 45 years of age, being able to speak and read English, and having no current physical limitations (ie, being able to participate in military training, physical training, and sport). Participants were excluded if they were on limited-duty status during the past 30 days as a result of physical limitations; were unable to perform routine physical training; had cardiac, pulmonary, balance, or visual impairments; or had a neurologic disorder. Participants were recruited from across the spectrum of military units (combat, combat service, and combat service support) and included both men and women. The institutional review board at Madigan Army Medical Center (Joint Base Lewis-McChord) granted ethical approval for this study. All soldiers provided written informed consent before their participation.
Health Risk Factors
Participants were categorized based on having either no risk factors or 1, 2, 3, or 4 of the risk factors (descriptions follow). Only 3 (0.2%) individuals in this study had 4 risk factors. Therefore, we considered participants with 3 or 4 risk factors as a single group.
Physical inactivity: Participants who endorsed a question stating they were inactive or physically inactive during the previous 1-year period were identified as physically inactive.19 Previous investigators5 have found soldiers' responses to this general question to predict future injury risk.
Body mass index: Participants' height and weight were measured to calculate BMI. Participants with a BMI ≥ 27.5 kg/m2 were identified as overweight. Although the traditional BMI overweight cutoff value for a general population is 25, the higher value is in agreement with previous research in trained individuals with higher muscle mass21 and is based on the Army screening table.22
Smoking: Participants who answered yes to “Do you smoke cigarettes regularly?” were identified as smokers.19 Questions related to other forms of tobacco use were not included.
Prior injury: Participants with a musculoskeletal injury in the past 5 years that resulted in medical care or limited physical activity for more than 7 days were considered to have a prior injury. Because of the average age of this population and the exclusion of those with long-term disability associated with prior injury, we considered injuries that occurred more than 5 years earlier to not be relevant.
Physical Performance Tests
In addition to the subjective self-report surveys examining individual lifestyle and history of injury, participants performed a series of physical performance and functional movement tests. Data were collected during a single session in which multiple tests were completed at a series of stations. Physical performance was measured on the triple-crossover hop for distance, the 6-m timed-hop test, the Functional Movement Screen, the Lower Quarter Y-Balance test (YBT-LQ), the Upper Quarter Y-Balance test (YBT-UQ), and the 3-event Army Physical Fitness Test (APFT). All physical performance measures except the APFT were obtained during a single visit in a counterbalanced manner. The APFT is a semiannual requirement for soldiers that is graded by their unit leadership. Performance data from the most recent APFT were included in the analysis.
The triple-crossover hop test for distance required the participants to consecutively hop and cross over a line (15.24-cm wide) on a single leg 3 times, and the distance hopped down the line was measured.23 The average distance (cm) of 3 trials was used. The researchers timed participants on the 6-m timed-hop test as they hopped 6 m on a single leg as fast as they could.23 The average time (seconds) of 3 trials was used. Performance did not differ by leg; therefore, the performance from the right leg was used.
The YBT-LQ is a test of dynamic balance that examines single-limb reach distance in 3 directions to assess an individual's performance and asymmetries.23 Reach distances were normalized to leg length to minimize the effect of anthropometric measures.23 Previous researchers23 have established the YBT-LQ as a reliable measure between raters and across days (intraclass correlation coefficient [ICC] values ranged from 0.85–1.00). In addition, reach asymmetries and low performance on the YBT-LQ have predicted noncontact injuries in athletes.
The YBT-UQ is a test of upper quarter and trunk function. It examines how far an individual can reach in 3 directions (medial, inferolateral, and superolateral) while maintaining a plank position with 1 hand and both feet in contact with the ground. Performance on the test examines asymmetry and overall reach performance normalized to arm length. Prior research23 suggested moderate correlations between YBT-UQ performance and traditional functional tests of the shoulder and core musculature. The ICC values for both intrarater and interrater reliability of the YBT-UQ have been reported as 0.80 to 0.99 and 1.00, respectively.23
The FMS rates the quality of fundamental movement patterns to identify an individual's limitations or asymmetries.23 It is an objective measure of 7 individual movement tasks (push up, in-line lunge, hurdle step, rotary stability, shoulder mobility, active straight-leg raise, and deep squat) that is scored on a 0 to 3 ordinal scale. The scores from the 7 movement patterns are summed for a composite score. Interrater reliability of the FMS composite score is excellent (ICC = 0.92).23
In addition to these measures, the Army uses the APFT to assess physical fitness.22 Three events are scored on a scale of 0 to 100 points: 2-mi (3.2-km) run time (seconds) and maximum number of sit-ups (repetitions) and push-ups (repetitions) completed in 2 minutes. Performance is translated into an APFT score based on age (years) and sex normative data. A passing score requires at least 60 points on each of the 3 events (180 total points). In addition to analyzing performance on each of the 3 events, we categorized fitness scores as not performing the APFT due to a physical profile (eg, an old injury that did not require military discharge), <180 points, 180 to 219 points, 220 to 269 points, 270 to 299 points, or 300 points. We collected the results of the most recent APFT.
Overall Performance Score
The overall performance score was calculated to assess and visually represent the association of the health risk factors across performance on all tests.19 The 5 physical performance tests and the 3 components of the APFT were used to calculate an overall performance score. Scores on each of the 8 tests were rank ordered and then translated into a point system (1–4) for each quartile based on sex. Those scoring in the top quartile received 4 points, and those in the lowest quartile received 1 point. Based on the 8 tests, the overall performance score ranged from 8 to 32 points. A score of 8 meant the individual was in the lowest quartile for all 8 tests, whereas a score of 32 indicated the individual was in the highest quartile for all 8 tests. This analysis provides a more global assessment of the influence of the health risk factors on performance across all 8 tests.
Data Analysis
Descriptive statistics (means, standard deviations, percentages) were calculated for sex, height, weight, BMI, injury history, and for those defined as overweight, inactive, a smoker, or previously injured. For descriptive purposes, the number of risk factors present was compared based on both age range (18–20, 21–25, 26–30, and older than 31 years) and sex. Years of age was a continuous variable. Differences in means were calculated using an analysis of covariance (ANCOVA) with age and sex as covariates. The dependent measures consisted of the physical performance tests (2-mi run, 2-minute push-up, 2-minute sit-up, 6-m timed hop, triple-crossover hop, FMS, YBT-LQ, and YBT-UQ) and overall performance score. The independent variable was the number of risk factors (0, 1, 2, or 3–4). The Tukey honestly significant difference test was calculated for post hoc analyses. Dichotomous parameters were evaluated using χ2 or ORs (or both) with 95% confidence intervals (CIs). Independent t tests were conducted to assess the independent association of BMI, prior injury, inactivity, and smoking on individual physical performance tests and the overall performance score. A P value <.05 indicated significance. We used IBM SPSS (version 21.0; SPSS Inc, Chicago, IL) for all analyses. If data were missing, we removed the soldier's value from analysis of that outcome measure, but we did not remove the soldier from the overall analysis unless >5% of his or her data were missing.
RESULTS
Description of the Participants
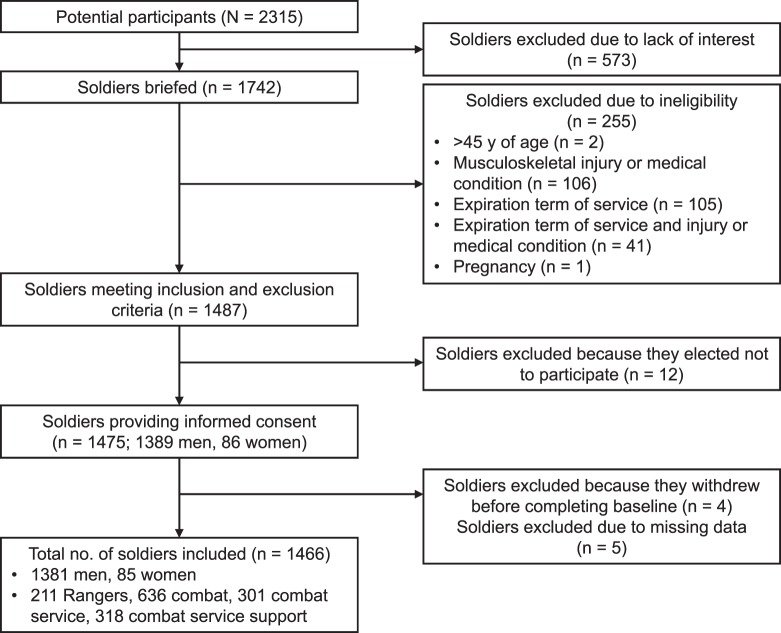
Participants consisted of 1466 active-duty service members (1380 men, 86 women; Table 1, Figure 1). Data for 5 soldiers were removed from the dataset due to the established standards for missing data. Overall, the proportion of physically inactive participants in the entire sample was low (6.3%, n = 93), but the highest percentage was in the 18–20-year-old group (12.9%, n = 36). The proportion of overweight participants (BMI ≥ 27.5 kg/m2) was higher in those older than 25 years of age (53.9%, n = 264) compared with those younger than 25 years of age (45.4%, n = 443). Smoking was consistent across all age groups, with the smallest proportion in the 31–45-year-old age group (22.8%, n = 44). The proportion of participants with a history of prior injury was higher in those over 25 years of age (42.2%, n = 207) compared with those less than 25 years of age (30.5%, n = 298). Most musculoskeletal injuries affected the lower extremity.
Table 1.
Descriptive Statistics and Proportions of Those Who Were Overweight, Inactive, Smokers, or Had a Previous Injury (N = 1466)a
| Age Group, y |
Participants |
Mean ± SD |
No. (%) |
|||||||
| Total, No. (%) |
Men, No. (%)b |
Women, No. (%) |
Height, cm |
Mass, kg |
Body Mass Index |
Overweight |
Inactivity |
Smoker |
Previous Injury |
|
| 18–20 | 279 (19.0) | 265 (95.0) | 14 (5.0) | 175.4 ± 6.6 | 79.4 ± 11.6 | 25.8 ± 3.2 | 127 (45.5) | 36 (12.9) | 79 (28.3) | 74 (26.5) |
| 21–25 | 697 (47.5) | 665 (95.4) | 32 (4.6) | 175.7 ± 7.4 | 82.0 ± 11.8 | 26.5 ± 3.2 | 316 (45.3) | 40 (5.7) | 206 (29.6) | 224 (32.1) |
| 26–30 | 297 (20.3) | 268 (90.2) | 29 (9.7) | 175.2 ± 7.6 | 83.5 ± 13.3 | 27.2 ± 3.5 | 155 (52.2) | 8 (2.7) | 78 (26.3) | 120 (40.4) |
| 31–45 | 193 (13.2) | 182 (94.3) | 11 (5.7) | 175.8 ± 7.2 | 86.6 ± 13.1 | 28.0 ± 3.5 | 109 (56.5) | 9 (4.7) | 44 (22.8) | 87 (45.1) |
Defining risk factors were body mass index ≥27.5, inactive or physically active <1 y, being a smoker, and previous injury. Percentages are rounded.
Figure 1.
Participant flow diagram.
The number of participants with no risk factors decreased with age (χ2 = 0.006): 18–20 years: 34.4% (n = 96); 21–25 years: 30.1% (n = 210); 26–30 years: 25.3% (n = 75); and 31–45 years: 18.1% (n = 35; Figure 2A). The majority of male (72.0%, n = 994) and female (65.1%, n = 56) participants had at least 1 risk factor. Only 3 of the 1466 participants (0.2%) had 4 risk factors. Therefore, for the purpose of our analysis, we considered those with 3 or 4 risk factors a single group (Figure 2B).
Figure 2.
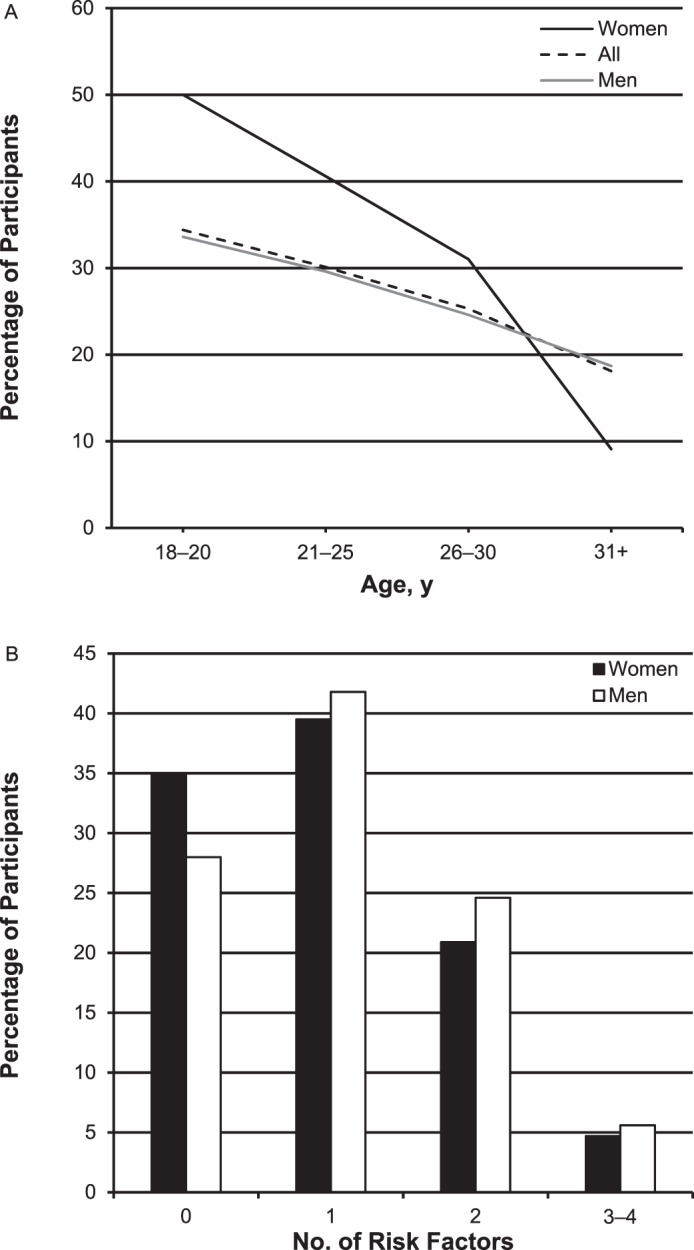
Proportion (%) of participants, A, without risk factors based on age group (n = 1466) and, B, with 0, 1, 2, and 3 to 4 risk factors based on sex (1380 men, 86 women). Risk factors were being overweight, physically inactive, or a smoker or having a previous injury.
Relationship Between Number of Risk Factors Present and Performance
Performance on all 3 components of the APFT decreased in direct association with the number of risk factors present (Table 2). The ANCOVA for the 2-mi run time was significantly different among groups (P < .001). Post hoc analyses for the 2-mi run time were statistically significant among all 3 risk groups (P ≤ .004) except for those with 2 versus 3 to 4 risk factors (P = .40). Compared with participants who had no risk factors (13.9 ± 1.6 minutes), participants who had 1 risk factor were on average 33.6 ± 7.0 seconds slower, those who had 2 risk factors were 58.7 ± 8.0 seconds slower, and those who had 3–4 risk factors were 83.0 ± 13.8 seconds slower. The ANCOVA for 2-minute sit-up performance differed among groups (P < .001). Post hoc analyses demonstrated that all groups were different from each other (P < .04) except for those with 1 versus 2 risk factors (P = .20). Compared with participants who had no risk factors (74.2 ± 0.6 sit-ups), participants who had 1 risk factor performed on average 2.9 ± 0.8 fewer sit-ups, those who had 2 risk factors performed 4.6 ± 0.9 fewer sit-ups, and those who had 3 to 4 risk factors performed 8.6 ± 1.5 fewer sit-ups. The ANCOVA for 2-minute push-up performance was significantly different between groups (P < .001). Post hoc analyses showed that all groups differed from each other (P < .003) except for those with 0 versus 1 or 1 versus 2 risk factors (P = .30). Compared with participants who had no risk factors (68.9 ± 0.6 push-ups), participants with 1 risk factor performed on average 1.7 ± 0.8 fewer push-ups, those who had 2 risk factors performed 3.3 ± 1.0 fewer push-ups, and those who had 3 to 4 risk factors performed 7.4 ± 1.6 fewer push-ups. Overall, those with 0 to 1 risk factor were more likely to have a higher score (270 points or greater) on the APFT (51.3%) than those with 2 to 4 risk factors (29.7%; OR = 2.49; 95% CI = 1.96, 3.17). Conversely, those with 2 to 4 risk factors were more likely to have a low score (less than 220 points) than those with 0 to 1 risk factor (14.8% versus 6.6%; OR: 2.48; 95% CI = 1.73, 3.57).
Table 2.
Analysis of Covariance for Performance Valuesa
| Measure |
Mean ± SD (95% Confidence Interval) |
Risk Factors (Mean ± Standard Error) |
|||
| 0 |
1 |
2 |
3–4 |
||
| 2-mi (3.2-km) Run, sb | 868.7 ± 121.0 (863.4, 875.0) | 836.1 ± 5.4 | 869.7 ± 4.4 | 894.8 ± 5.9 | 919.1 ± 12.6 |
| Sit-ups, repetitions per 2 minc | 71.4 ± 12.2 (70.8, 72.0) | 74.2 ± 0.6 | 71.3 ± 0.5 | 69.6 ± 0.6 | 65.6 ± 1.3 |
| Push-ups, repetitions per 2 minc,d | 67.0 ± 14.8 (66.2, 67.8) | 68.9 ± 0.6 | 67.2 ± 0.5 | 65.6 ± 0.7 | 61.5 ± 1.4 |
| Triple-crossover hop, cmb,d | 449.7 ± 87.9 (445.2, 454.3) | 463.4 ± 4.0 | 453.4 ± 3.3 | 433.8 ± 4.3 | 422.0 ± 9.0 |
| 6-m Timed hop, sb,c,e | 2.2 ± 0.5 (2.2, 2.3) | 2.10 ± 0.30 | 2.20 ± 0.02 | 2.30 ± 0.03 | 2.40 ± 0.05 |
| Functional Movement Screen, pointsb | 14.4 ± 2.7 (14.3, 14.5) | 15.2 ± 0.1 | 14.4 ± 0.1 | 13.7 ± 0.1 | 13.0 ± 0.3 |
| Lower Quarter Y-Balance Test, % limb lengthb,c,e | 96.9 ± 8.9 (96.4, 97.3) | 97.9 ± 0.4 | 97.0 ± 0.4 | 95.8 ± 0.5 | 94.8 ± 1.0 |
| Upper Quarter Y-Balance Test, % limb lengthb,d | 88.3 ± 9.7 (87.8, 88.8) | 89.9 ± 0.5 | 88.4 ± 0.4 | 86.7 ± 0.5 | 85.3 ± 1.1 |
| Overall performance score | 20.1 ± 5.6 (19.8, 20.4) | 22.0 ± 0.3 | 20.2 ± 0.2 | 18.6 ± 0.3 | 16.6 ± 0.6 |
All post hoc test results were different except where indicated.
Post hoc test result was not different for 2 versus 3–4 risk factors (P > .05).
Post hoc test result was not different for 1 versus 2 risk factors (P > .05).
Post hoc test result was not different for 0 versus 1 risk factor (P > .05).
Post hoc test result was not different for 1 versus 3–4 risk factors (P > .05).
Performance decrements on the hop tests were also seen in accordance with the number of risk factors (Table 2). The ANCOVA for performance on the triple-crossover hop test was significantly different among groups (P < .001). Post hoc analyses demonstrated that all groups differed from each other (P < .006) except for those with 0 versus 1 risk factor and 2 versus 3 to 4 risk factors (P > .3). Compared with participants who had no risk factors (463.4 ± 4.0 cm), participants with 1 risk factor hopped 10.0 ± 5.2 cm less, those with 2 risk factors hopped 29.6 ± 5.9 cm less, and those with 3 to 4 risk factors hopped 41.4 ± 9.8 cm less. The ANCOVA for the 6-m timed-hop test was significantly different among groups (P < .001). Post hoc analyses showed that all group differences were statistically significant compared with those who had 0 risk factors (P < .005). No statistically significant differences were noted among all the other risk groups (P > .1). Although the performance decrements on this test were statistically significant, the actual differences among the groups were minimal and were not clinically significant. Compared with participants who had no risk factors (2.10 ± 0.30 seconds), participants with 1 risk factor were on average 0.10 ± 0.03 seconds slower, those who had 2 risk factors were 0.20 ± 0.03 seconds slower, and those who had 3 to 4 risk factors were 0.30 ± 0.06 seconds slower.
We also found performance decrements on the FMS, YBT-LQ, and YBT-UQ tests based on the number of risk factors present (Table 2). The ANCOVA for the FMS was significantly different among groups (P < .001). Post hoc analyses showed a significant difference among all groups (P < .001) except for those with 2 versus 3 to 4 risk factors (P = .18). Compared with the participants who had no risk factors (15.2 ± 0.1 points), participants with 1 risk factor scored on average 0.8 ± 0.2 points less, those with 2 risk factors scored 1.5 ± 0.2 points less, and those with 3 to 4 risk factors scored 2.2 ± 0.3 points less. The ANCOVA for the YBT-LQ was significantly different among groups (P < .001). Post hoc analyses indicated that those with 0 risk factors had further single-limb reach than those with 2 to 4 risk factors (P ≤ .006); limb reach was not significantly different for the other group comparisons (P > .18). Compared with the participants who had no risk factors (97.9 ± 0.4%), participants with 1 risk factor on average reached 0.9% ± 0.6% less, those who had 2 risk factors reached 2.1% ± 0.6% less, and those who had 3 to 4 risk factors reached 3.1% ± 1.1% less, demonstrating decreased dynamic balance as the number of risk factors increased. The ANCOVA for the YBT-UQ was significantly different among groups (P < .001). Post hoc analyses revealed statistically significant differences among all groups (P < .05) except for those with 0 and 1 risk factor and 2 and 3 to 4 risk factors (P > .07). Compared with the participants who had no risk factors (89.9% ± 0.5%), participants with 1 risk factor on average reached 1.5% ± 0.6% less, those who had 2 risk factors reached 3.2% ± 0.7% less, and those who had 3 to 4 risk factors reached 4.6% ± 1.2% less, demonstrating decreased upper quarter and trunk control as the number of risk factors increased.
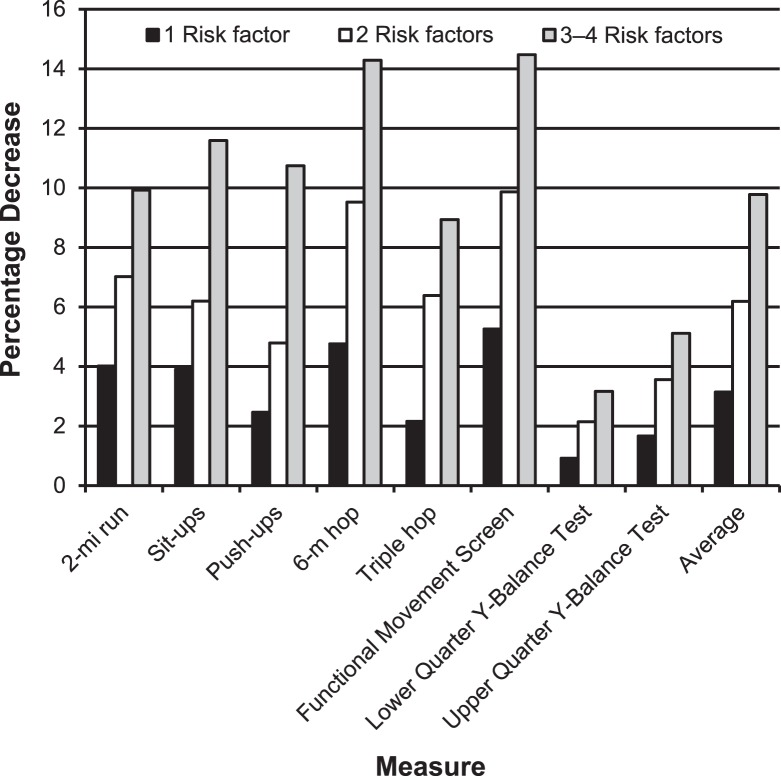
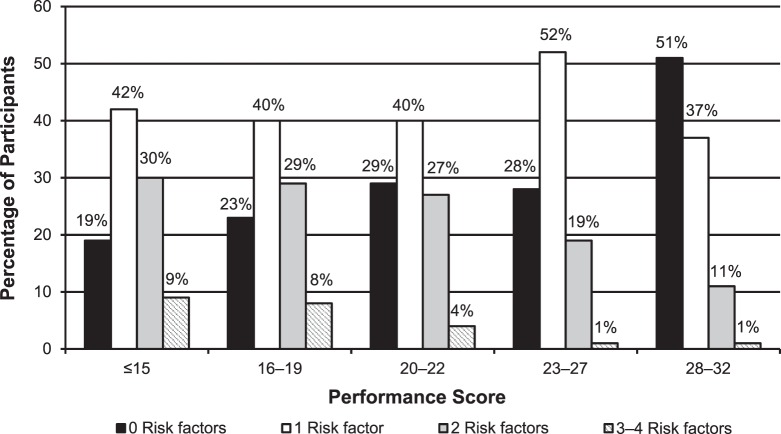
Overall, physical performance decreased as the number of risk factors increased. When decrements were compared with the group that had no risk factors, they averaged 4.3% for those with 1 risk factor, 6.7% for those with 2 risk factors, and 10.3% for those with 3 to 4 risk factors (Figure 3). The association between risk factors and overall performance score is demonstrated in Figure 4. Most individuals (51%) who scored highest on the overall performance score (28–32 points) had 0 risk factors. As performance scores decreased, the proportion of those with 0 risk factors also decreased. The reverse pattern was seen in those with 2 or 3 to 4 risk factors. Only 11% of those with 2 risk factors and 1% of those with 3 to 4 risk factors scored highest on the overall performance score. As performance scores decreased, the proportion of those with either 2 or 3 to 4 risk factors increased. As the number of risk factors increased, the proportion of individuals with higher overall performance scores decreased.
Figure 3.
Decrements (%) in physical performance of those with 1, 2, or 3 to 4 risk factors compared with those without any health risk factors. The physical performance tests included the 2-mi (3.2-km) run time, number of sit-ups and push-ups completed in 2 minutes, triple-crossover hop test for distance, 6-m timed-hop test, Functional Movement Screen, Lower and Upper Quarter Y-Balance Tests, and average performance decrement across all tests.
Figure 4.
Proportion of participants with 0, 1, 2, or 3 to 4 risk factors based on the overall performance score for the 8 physical performance tests. Overall, 51% of participants who scored 28 to 32 points had 0 risk factors. Participants with 2 to 4 risk factors were more likely to score <20 points. Scores on each of the 8 physical performance tests were rank ordered and then translated into a point system (1–4) based on quartile by sex. Those scoring in the highest quartile received 4 points; in the lowest, 1 point. Overall performance scores ranged from 8 to 32.
Relationship Between Specific Risk Factors and Performance
Using independent t tests, we found that those with BMI ≥ 27.5 kg/m2 performed poorer on all tests (P < .001) except for the 2-minute push-up test (P = .2). Those with a history of injury performed worse on the 2-mi run time, triple-crossover hop, 6-m timed hop, and FMS (P < .03). However, they performed similarly to the uninjured participants on the 2-minute sit-up and 2-minute push-up tests, YBT-LQ, and YBT-UQ (P > .5). Smokers performed worse on the 2-mi (3.2-km) run, 2-minute sit-up and 2-minute push-up tests, 6-m timed hop, FMS, and YBT-UQ (P ≤ .02). However, they performed similarly to nonsmokers on the triple-crossover hop and the YBT-LQ (P > .06). Those who reported being physically inactive the year before testing performed worse on the 2-mi run, 2-minute sit-up, and the 2-minute push-up tests, YBT-LQ, and YBT-UQ (P < .04). They performed similarly to the physically active participants on the triple-crossover hop, 6-m timed hop, and FMS (P > .3).
DISCUSSION
Numerous authors1–4 have linked the lack of exercise, being overweight or obese, smoking, and a history of injury with disease or to future injury (or both). However, limited evidence addresses the association of these risk factors with physical performance.19 Our primary finding was that having at least 1 health risk factor was associated with inferior performance on all physical testing; those possessing multiple health risk factors had even poorer physical performance. For all physical performance tests except the 6-m timed-hop test, the groups with 2 or 3 to 4 risk factors were beneath the lower bound of the 95% CI for the group mean. For the 6-m timed-hop test, only the group with 3 to 4 risk factors fell below the lower bound of the 95% CI. On average, physical performance decreased by 4.3%, 6.7%, and 10.3% when 1, 2, or 3 to 4 risk factors, respectively, were present. Performance decrements for those with 3 to 4 risk factors included 9.9% for the 2-mi run, 11.9% for the sit-ups, 10.3% for the push-ups, 8.8% for the triple-crossover hop, 14.3% for the 6-m timed hop, 14.4% for the FMS, 3.3% for the YBT-LQ, and 5.1% for the YBT-UQ. The decrements in the APFT measures (2-mi run, sit-ups, and push-ups) have clear negative consequences for soldiers in the Army, as performance on the 300-point APFT is associated with points toward professional promotion within the Army. Based on the published age and sex standards for the APFT, 22 individuals would score at least 10 to 16 points, 15 to 27 points, or 28 to 47 points lower based on having 1, 2, or 3 to 4 risk factors, respectively, compared with those who had no risk factors. Clinically, these findings are relevant because injury-prevention efforts, smoking-cessation programs, weight-control initiatives, and advocating additional physical activity to benefit individual health often have limited appeal to young adults. However, obvious performance decrements provide an opportunity to link health and injury risk-mitigation strategies with enhanced performance, which has been suggested to be a more effective way to encourage compliance with health-promotion and injury-prevention programs.20
Higher BMI values were associated with decreased performance on 7 of the 8 performance tests, whereas self-reported smoking, physical inactivity, and prior history of injury were associated with decreased performance on 6, 5, and 4 of the 8 tests, respectively. The negative association of smoking, BMI, physical inactivity, and past history of injury with current physical performance identified in this study highlights the potential need for a multifactorial and interdisciplinary approach to programs focused on human performance optimization and injury prevention in occupational settings. Current evidence on injury prevention suggests that a solution targeting modifiable risk factors that include physical performance deficits and appropriate return-to-duty criteria is effective in reducing injury risk.24,25 Our findings indicate that future researchers should also explore the influence of incorporating improvements in baseline physical activity levels, nutritional counseling, and smoking cessation to address occupation-related injury-prevention and human performance optimization programs.
The results of Leyk et al19 in a group of adolescents and young adults (10–25-year olds) displayed several similarities with our results. Specifically, males had more risk factors than females, the percentage of those who were overweight increased with age, and the number of risk factors present increased with age. Although the population age ranges in the Leyk et al19 study were younger, the same trends with regard to risk factors and overweight status point to the concept that creating healthy habits and addressing health risk factors early in life may be helpful. Additionally, the participants in our study performed similar to high school and collegiate athletes, US Marines, and healthy active adults,23,26,27 but they performed slightly worse than elite soccer players.28
Some of our findings were different from those of Leyk et al.19 In our sample, the percentage of individuals with a history of inactivity decreased with age. This may be due to selection bias, as those who remain in the military are required to maintain the required physical fitness and weight standards.15 Similarly, the percentage of smokers decreased with age in our military population. This may be due to smokers discontinuing military service more frequently, as they tend to have other negative health-related risk behaviors that are not conducive to military service.29 This may also be due to either the Army's smoking-cessation program or a shift to smokeless tobacco. The lower prevalence of these 2 risk factors in older soldiers should be further explored.
Although this is a large cross-sectional study, a few limitations should be noted. Our sample had a greater proportion of men. This adequately represents the population studied, but sex comparisons may be limited given the small percentage of women. Further, as stated earlier, causation in either direction cannot be determined from this study. In addition, unidentified factors may be the underlying cause(s) of the relationship between health risk factors and performance (eg, psychosocial variables) that were not captured in our study. The data that were obtained via self-report survey are susceptible to reporting errors in activity levels, smoking frequency, and injury rates, as well as recall bias.30 However, we used the survey questions to allow comparison with Leyk et al.19 Additionally, these questions have demonstrated predictive validity for future injury risk in a military population and are commonly used in the military setting.5 Although underreporting of health risk factors is a potential limitation, the disclosure rates still resulted in significant associations between health risk factors and performance. Finally, the BMI cutoff value of 27.5 kg/m2 is higher than the typical cutoff value for being overweight (25.0 kg/m2).21 This higher rate was based on the enrollment of a relatively active population, and this cutoff value is aligned with current Army standards for determining weight status.21,22 Based on the exploratory nature of this study and the multiple comparisons in this study, there is a potential for type I error.
In summary, unhealthy lifestyles (inactivity, being overweight, and smoking) and a history of injury were associated with relatively lower levels of physical performance in military service members. The presence of a single risk factor was associated with decrements in physical performance; as the number of risk factors increased, performance decrements also increased. A better understanding of how negative lifestyle choices are associated with physical performance may motivate individuals to create and sustain changes in health. From an organizational perspective, understanding how health risk factors and prior injuries are associated with performance decrements may lead to greater incentives to prioritize interventions aimed at preventing injuries and improving the health of its workforce.
ACKNOWLEDGMENTS
This study was conducted in collaboration with physical therapy research and administrative assistants from US Army-Baylor University, US Army Medical Department Center and School, San Antonio, TX; the University of Evansville, Evansville, IN; Duke University, Durham, NC; and the University of Puget Sound, Tacoma, WA.
Additional research support was provided by Joint Base Lewis-McChord's Physical Therapy Clinic, Madigan Army Medical Center; 4-2 Infantry Division, First Corps: 2-12 Field Artillery Battalion, 1-38 Infantry Battalion, 2-23 Infantry Battalion, 4-9 Infantry Battalion; 75th Ranger Regiment; 42nd Military Police Brigade; 864th Combat Engineers; 160th SOAR; 2-2 Infantry Division, First Corps including First Battalion: 17th Infantry Regiment Second Battalion: First Infantry Regiment, Fourth Battalion: 23rd Infantry Regiment, Eighth Squadron: First Cavalry Regiment; and 593rd Sustainment Brigade including 593rd Special Troops Battalion, 57th Transportation Battalion, 80th Ordinance Battalion, 555th Engineer Brigade, and 62nd Medical Brigade.
We thank Ann-Maree Williams, PT, DPT, COMT, and Jennifer C. Prye, MEd, ATC, for their assistance with data collection, analysis, and manuscript preparation. We acknowledge the following staff for their administrative and technical support: Josh Miller; Julie Koepp; Nadine Shewell; Norman Gardner; Liz Reilly-Hess; Celestina Wildman; Miyoko D. Sasakura, MSPH; Gail Baudendistel, PT, CPA, MS, MAFM; Tom Kurtz, PT; and Jeff Wilson. Technology support included Bob Humphrey; Dalene Becka; Jack Brower; and Jaret Willard. Additional data logistical support was from Theresa Leatherwood; CPT Carrie Hoppes; SFC Sean Stephens; SFC Ryan Murphy; SSG Christopher Villarreal; CPO Ferdinand Ajel; Paul Gorman, ATC, PTA, CSCS; Luck Chanthabandith; Phil Borja; Matthew Buchanan; and Valeria DeAngelis.
This project was financially supported by the Army Medical Department Advanced Medical Technology Initiative, Telemedicine and Advanced Technology Research Center (TATRC), and the Defense Medical Research and Development Program, Military Operation Medicine Research Program from the US Army Medical Research and Materiel Command (MRMC), Fort Detrick, MD. The funding agencies were not involved in the study design, analysis, or dissemination of the findings of the study.
CONFLICTS OF INTEREST AND SOURCE OF FUNDING
This research trial was supported by the MRMC, Army Medical Department Advanced Medical Technology Initiative, TATRC, Military Operational Medicine Research Program, and Defense Medical Research and Development Program.
“Automated Musculoskeletal Injury Risk Identification Algorithms,” MRMC, TATRC, Army Medical Department Advanced Medical Technology Initiative, Fort Detrick, MD, Application Log Number: 1053.
“Military Specific Computerized Algorithms to Predict Musculoskeletal Injury,” Defense Medical Research and Development Program, Fort Detrick, MD; Application Log Number: D10_I_AR_J5_951.
Drs Kiesel and Plisky own equity in Move2Perform LLC and have developed the Move2Perform software that was used to collect data as part of this study. Dr Plisky developed the Y-Balance Test, which was also used in this study.
REFERENCES
- 1. Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. . Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010; 85 12: 1138– 1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Godtfredsen NS, Prescott E. . Benefits of smoking cessation with focus on cardiovascular and respiratory comorbidities. Clin Respir J. 2011; 5 4: 187– 194. [DOI] [PubMed] [Google Scholar]
- 3. Obesity: Preventing and Managing the Global Epidemic. Geneva, Switzerland: World Health Organization; 2000. [PubMed] [Google Scholar]
- 4. Tyler TF, McHugh MP, Mirabella MR, Mullaney MJ, Nicholas SJ. . Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006; 34 3: 471– 475. [DOI] [PubMed] [Google Scholar]
- 5. Knapik JJ, Sharp MA, Canham-Chervak M, Hauret K, Patton JF, Jones BH. . Risk factors for training-related injuries among men and women in basic combat training. Med Sci Sports Exerc. 2001; 33 6: 946– 954. [DOI] [PubMed] [Google Scholar]
- 6. Barlas F, Higgins W, Pflieger J, Diecker K. . 2011: Health Related Behaviors Survey of Active Duty Military Personnel. Fairfax, VA: Defense Health Headquarters; 2013: 1– 22. [Google Scholar]
- 7. Tirosh A, Shai I, Afek A, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med. 2011; 364 14: 1315– 1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Finkelstein EA, Chen H, Prabhu M, Trogdon JG, Corso PS. . The relationship between obesity and injuries among US adults. Am J Health Promot. 2007; 21 5: 460– 468. [DOI] [PubMed] [Google Scholar]
- 9. Knapik JJ, Canham-Chervak M, Hauret K, Hoedebecke E, Laurin MJ, Cuthie J. . Discharges during US Army basic training: injury rates and risk factors. Mil Med. 2001; 166 7: 641– 647. [PubMed] [Google Scholar]
- 10. Langley J, Davie G, Wilson S, et al. Difficulties in functioning 1 year after injury: the role of preinjury sociodemographic and health characteristics, healthcare and injury-related factors. Arch Phys Med Rehabil. 2013; 94 7: 1277– 1286. [DOI] [PubMed] [Google Scholar]
- 11. Behrend C, Prasarn M, Coyne E, Horodyski M, Wright J, Rechtine GR. . Smoking cessation related to improved patient-reported pain scores following spinal care. J Bone Joint Surg Am. 2012; 94 23: 2161– 2166. [DOI] [PubMed] [Google Scholar]
- 12. Rechardt M, Shiri R, Karppinen J, Jula A, Heliovaara M, Viikari-Juntura E. . Lifestyle and metabolic factors in relation to shoulder pain and rotator cuff tendinitis: a population-based study. BMC Musculoskelet Disord. 2010; 11: 165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Van Middelkoop M, Kolkman J, Van Ochten J, Bierma-Zeinstra SM, Koes BW. . Risk factors for lower extremity injuries among male marathon runners. Scand J Med Sci Sports. 2008; 18 6: 691– 697. [DOI] [PubMed] [Google Scholar]
- 14. Altarac M, Gardner JW, Popovich RM, Potter R, Knapik JJ, Jones BH. . Cigarette smoking and exercise-related injuries among young men and women. Am J Prev Med. 2000; 18 suppl 3: 96– 102. [DOI] [PubMed] [Google Scholar]
- 15. Larsson H, Broman L, Harms-Ringdahl K. . Individual risk factors associated with premature discharge from military service. Mil Med. 2009; 174 1: 9– 20. [DOI] [PubMed] [Google Scholar]
- 16. Hootman JM, Macera CA, Ainsworth BE, Addy CL, Martin M, Blair SN. . Epidemiology of musculoskeletal injuries among sedentary and physically active adults. Med Sci Sports Exerc. 2002; 34 5: 838– 844. [DOI] [PubMed] [Google Scholar]
- 17. Hewett TE, Di Stasi SL, Myer GD. . Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013; 41 1: 216– 224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Waterman BR, Belmont PJ Jr, Cameron KL, Deberardino TM, Owens BD. . Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010; 38 4: 797– 803. [DOI] [PubMed] [Google Scholar]
- 19. Leyk D, Ruther T, Witzki A, et al. Physical fitness, weight, smoking, and exercise patterns in young adults. Dtsch Arztebl Int. 2012; 109 44: 737– 745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hrysomallis C. . Injury incidence, risk factors and prevention in Australian rules football. Sports Med. 2013; 43 5: 339– 354. [DOI] [PubMed] [Google Scholar]
- 21. Ode J, Pivarnik J, Reeves M. . Body mass index as a predictor of percent fat in college athletes and nonathletes. Med Sci Sports Exer. 2007; 39 3: 403– 409. [DOI] [PubMed] [Google Scholar]
- 22. Army Regulation FM 21-20: Physical Fitness Training. US Army; 2004. [Google Scholar]
- 23. Teyhen DS, Riebel MA, McArthur DR, et al. Normative data and the influence of age and gender on power, balance, flexibility, and functional movement in healthy service members. Mil Med. 2014; 179 4: 413– 420. [DOI] [PubMed] [Google Scholar]
- 24. Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. . Prevention of injuries among male soccer players: a prospective, randomized intervention study targeting players with previous injuries or reduced function. Am J Sports Med. 2008; 36 6: 1052– 1060. [DOI] [PubMed] [Google Scholar]
- 25. Grooms DR, Palmer T, Onate JA, Myer G, Grindstaff T. . Comprehensive soccer-specific warm-up and lower extremity injury in collegiate male soccer players. J Athl Train. 2013; 48 6: 782– 789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O'Connor FG, Deuster PA, Davis J, Pappas CG, Knapik JJ. . Functional movement screening: predicting injuries in officer candidates. Med Sci Sports Exerc. 2011; 43 12: 2224– 2230. [DOI] [PubMed] [Google Scholar]
- 27. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. . Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006; 36 12: 911– 919. [DOI] [PubMed] [Google Scholar]
- 28. Rahnama N, Lees A, Bambaecichi E. . Comparison of muscle strength and flexibility between the preferred and non-preferred leg in English soccer players. Ergonomics. 2005; 48 11–14: 1568– 1575. [DOI] [PubMed] [Google Scholar]
- 29. Lynch JP, Hanson K, Kao TC. . Health-related behaviors in young military smokers. Mil Med. 2004; 169 3: 230– 235. [DOI] [PubMed] [Google Scholar]
- 30. Coughlin SS. . Recall bias in epidemiologic studies. J Clin Epidemiol. 1990; 43 1: 87– 91. [DOI] [PubMed] [Google Scholar]