Abstract
Context:
Knee overuse injuries are the most common musculoskeletal complaints in military trainees and are common in active-duty warfighters. Muscle strengthening is usually recommended; however, research is conflicting in this area, which makes it difficult to develop effective screening, prevention, and training interventions for warfighters.
Objective:
To determine if lower extremity muscular weakness contributes to knee overuse injuries and identify specific muscular involvement.
Data Sources:
We searched MEDLINE, PubMed, Web of Science, SPORTDiscus, CINAHL, and Military & Government Collection and reference lists of relevant articles published between January 1, 2000, and January 1, 2013.
Study Selection:
For inclusion, requirements were uninjured and injured groups; provision of the sample size, means, and standard deviations for all groups; identification of the specific muscles assessed; and clearly defined knee injury.
Data Extraction:
Sample size, sex, and muscle strength means and standard deviations.
Data Synthesis:
Twenty-five studies met these criteria. We used the Scottish Intercollegiate Guidelines Network algorithm to determine the appropriate tool for appraising article quality. Unweighted random-effects model meta-analyses were conducted. Separate meta-analyses were performed for the moderators of strength measurement scale (absolute or normalized muscle strength), muscle group, and sex. A weighted random-effects model with a Hedges g effect metric and 95% confidence intervals were used for comparison across studies.
Conclusions:
Our meta-analysis suggests that individuals with symptoms of a knee overuse injury have lower absolute and normalized hip muscle strength. Specifically, they had lower absolute hip external-rotator, knee-extensor, and knee-flexor strength, as well as lower normalized hip external-rotator, hip-extensor, and hip-abductor strength, compared with asymptomatic control participants. The findings suggest a possible link between lower hip and thigh strength and knee overuse injuries. Further research is needed to determine if weakness is a cause or a result of knee overuse injuries before screening and intervention can be developed for at-risk warfighters.
Key Words: hip strength, patellofemoral pain syndrome, iliotibial band syndrome, warfighters
Key Points
Knee overuse injuries are common in training, active-duty, and reserve military personnel.
Individuals with knee overuse injuries have lower absolute and normalized hip muscle strength compared with asymptomatic controls.
These findings suggest a possible link between lower extremity strength and knee overuse injuries.
Musculoskeletal injury is the primary problem facing the military today.1−3 Chronic knee overuse injuries are the most common overuse injury in military trainees, accounting for between 5.9% and 44% of injuries.4−7 They result in significant training time lost and medical expense.4,5,8−10 Knee overuse injuries are also a concern in both active-duty and reserve populations, and they affect the readiness of the force.7,11 Chronic knee pain limits activity, training time, and fitness. Diagnoses often include patellofemoral pain syndrome, iliotibial band syndrome, patellar tendinitis, and general anterior knee pain. In a study12 of 449 trainees involved in Naval Special Warfare training, iliotibial band syndrome and patellofemoral pain syndrome accounted for 10.9% and 9.4% of the reported injuries, respectively. These injuries are also common in the nonmilitary active population; patellofemoral pain syndrome accounts for 20% to 40% of the knee injuries treated in orthopaedic clinics,13−15 and iliotibial band syndrome occurs in 15% to 20% of runners seeking treatment for knee pain.16 These injuries are likely to be long term, tend to recur, and often result in the loss of a significant number of training days.
The military is working to develop both effective screening methods that will predict musculoskeletal injuries and interventions to prevent them. However, the causes of knee overuse injuries remain unclear and research is conflicting. A better understanding of the causes of these conditions is essential before we can develop effective screening, prevention, and treatment protocols to improve warfighter health and wellness while also reducing lost training time. These outcomes are essential in the current military environment, where efficient use of resources and training time while maintaining warfighter health are critical. Reported causes of knee overuse injuries in the military are large amounts of physical training, especially running, marching with weight (ie, ruck marching),6 jumping, walking long distances, kneeling, and prolonged standing on hard surfaces. In general, the amount of training and the inability of the individual warfighter to modify daily physical demands may result in training beyond the body's ability to adapt and recover. Research suggests that biomechanical dysfunction,17−20 muscular weakness,13,17−19 muscular tightness,18,19,21 and sedentary lifestyle all play roles in the development of these injuries.13 Prevention and treatment efforts have included tape,22 orthoses,23,24 prehabilitation exercise,25 and rehabilitation exercise,25,26 with mixed results. More recently, programs that involve hip and knee strengthening and stretching exercises have produced improvements in individuals with patellofemoral pain syndrome18,27,28 or iliotibial band syndrome.21,27
The effectiveness of intervention programs that include hip- or knee-strengthening exercises in reducing the symptoms of knee overuse injuries supports the suggestion that muscular weakness may be an injury risk factor.26 Weakness of the musculature of the hip and knee is believed to result in abnormal lower extremity movement mechanics during weight-bearing activities, thereby increasing the potential for development of knee overuse injuries.29−31 However, the literature9,17,31−33 is conflicting in regard to the specific muscle groups that may be linked to the development of knee overuse injuries. For example, several groups have shown that the hip abductors were weaker in persons with patellofemoral pain syndrome or iliotibial band syndrome compared with asymptomatic control participants,17,30,32,34 whereas others have demonstrated that the strength of the hip abductors31,33 was not different. Reports are also conflicting with regard to hip-extensor,17,30 hip external-rotator,30−32 and knee-extensor9,35 strength. Thus, the goal of our study was to determine if individuals with knee overuse injuries had less muscular strength at the hip and thigh compared with asymptomatic individuals. This knowledge can then be used to develop effective screening, prevention, training, and rehabilitation programs for warfighters.
METHODS
Identification, Study Selection, and Data Extraction
The sections of this article have been written in accordance with The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).36 We searched MEDLINE, PubMed, Web of Science, SPORTDiscus, CINAHL, and Military & Government Collection from January 1, 2000, to January 1, 2013. The following terms were searched alone or in combination: patellofemoral pain syndrome, iliotibial band syndrome, anterior knee pain, hip, knee, abductor, adductor, internal rotators, external rotators, quadriceps, hamstrings, gluteus maximus, gluteus minimus, gluteus medius, tensor fasciae latae, and strength. The reference lists of articles were also searched for other relevant articles.
Inclusion criteria were determined before the start of the literature review. For inclusion, we required all studies to have an uninjured and an injured group, report means and standard deviations for the uninjured and injured groups, clearly identify the test muscles, and clearly define the knee injury. After screening the titles and abstracts, 2 reviewers (C.A., A.J.) evaluated the relevant full-text articles for final inclusion. The reviewers resolved disagreements concerning article eligibility by coming to consensus or by arbitration of a third reviewer (T.E.) if disagreement persisted. The reviewers extracted all relevant information from each eligible article: number of participants, sex, type of contraction (eccentric or concentric), type of testing (isometric or isokinetic), muscle group tested, hip-strength means and standard deviations, and normalizing equation.
Data Analysis
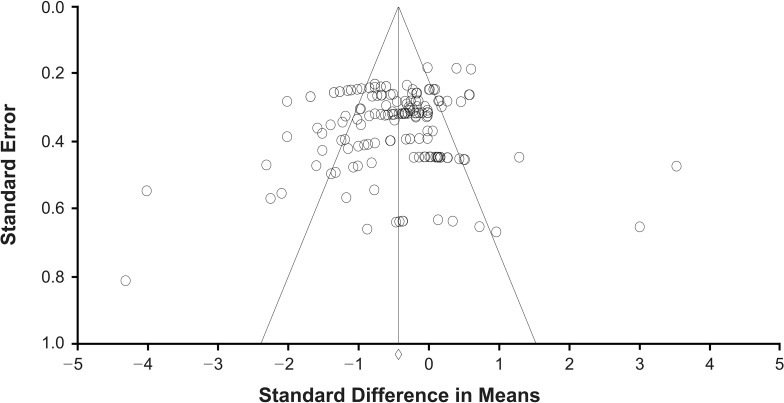
All extracted data were entered into a custom spreadsheet (Excel 2010; Microsoft Corporation, Redmond, WA) and transferred to Comprehensive Meta-Analysis (version 2; Biostat Inc, Englewood, NJ). Separate meta-analyses were performed for each of the predetermined moderators: strength measurement scale (absolute or normalized muscle strength), muscle group, and sex. Unweighted random-effects meta-analyses were conducted using the Hedges g effect metric. We also calculated 95% confidence intervals for each mean effect size to enable comparisons across studies as well as identification of null effects (ie, mean = 0). A funnel plot was checked for symmetry to determine if a publication bias was present (Figure 1). In addition, a fail-safe N was used to determine the number of negative data points needed to increase the P value for each meta-analysis to statistical insignificance (P > .05).
Figure 1.
Funnel plot of included studies.
RESULTS
Our search yielded 947 potential studies: 22 articles were retained and 3 more studies were identified through a hand search of reference lists. In total, 25 studies9,13,14,17,30−35,37–51 met the inclusion criteria and were included in the analyses (Figure 2). The characteristics of each study are described in Table 1. We used the Scottish Intercollegiate Guidelines Network (SIGN) grading system to evaluate the quality of evidence for each article.52 With the SIGN system, a level of evidence (1++, 1+, 1–, 2++, 2+, 2–, 3, or 4) is assigned to an article52; a grade of 1++ represents the highest level of evidence.52 The final grade was based on the SIGN criteria for recommendations, which range from A through D.52
Figure 2.
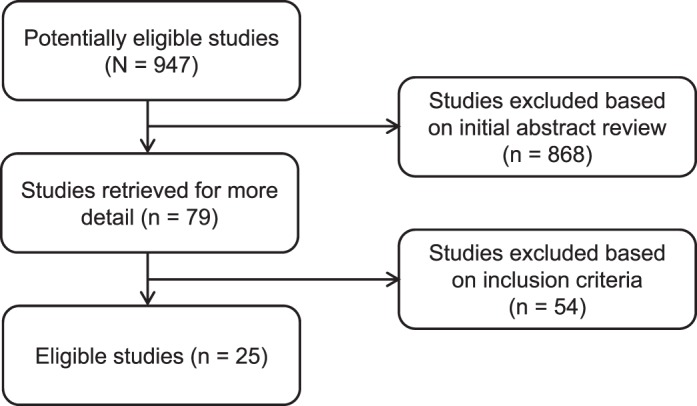
Outline of literature search and selection.
Table 1.
Study Demographics and Level of Evidence Continued on Next Page
| Authors (Year) |
Sample Population |
Pathologic Condition |
Muscle Group(s) |
Study Design |
Level of Evidence |
|
| Symptomatic |
Control |
|||||
| Chiu et al39 (2012) | 9; 5 Women, 4 men | 6 Able-bodied participants; 3 women, 3 men | PFPS | Knee extensors | CS | 2 (−) |
| Cowan et al40 (2009) | 10; 7 Women, 3 men | 27; 15 Women, 12 men | PFP | External rotators, hip abductors, and trunk side flexors | CS | 2 (−) |
| Krauss et al46 (2007) | 20 Females | 26 Females | Patellar tendinopathy | Knee flexors-to-knee extensors ratio, knee extensors, and knee flexors | CS | 2 (−) |
| Nakagawa et al48 (2012) | 40; 20 Women, 20 men | 40 Age-matched participants; 20 women, 20 men | PFPS | Hip external rotators and abductors | CS | 2 (−) |
| Bolgla et al38 (2008) | 18 Females | 18 Matched females | PFPS | Hip external rotators and abductors | CS | 2 (−) |
| Fredericson et al34 (2000) | 24 Club and collegiate runners; 14 women, 10 men | 30 Collegiate cross-country and track runners; 14 women, 16 men | Iliotibial band syndrome | Hip abductors | CS | 2 (−) |
| Witvrouw et al9 (2000) | 19 (11 Boys, 8 girls) of 138 physical education students | 119 (88 Boys, 31 girls) of 138 physical education students | Patellar tendinitis | Knee extensors and knee flexors | Cohort | 2 (−) |
| Ireland et al44 (2003) | 15 Women | 15 Age-matched women | PFP | Hip abductors and external rotators | CS | 2 (−) |
| Hazneci et al43 (2005) | 24 Men | 24 Healthy men | PFPS | Knee extensors and knee flexors | CS | 2 (−) |
| Duvigneaud et al35 (2008) | 26 of 62 Belgian Royal Military Academy women | 36 of 62 Belgian Royal Military Academy women | PFPS | Knee extensors, knee flexors, knee flexors-to-extensors ratio | CS | 2 (−) |
| Robinson and Nee50 (2007) | 10 Females | 10 Females | PFPS | Hip abductors, hip extensors, and hip external rotators | CS | 2 (−) |
| Boling et al17 (2009) | 20; 13 Women, 7 men | 20 Student, faculty, and staff; 13 women, 7 men | PFP | Hip extensors, external rotators, and abductors | CS | 2 (−) |
| Baldon et al37 (2009) | 10 Females | 10 Age-, height-, and body mass–matched females | PFPS | Hip abductors, adductors, external rotators, internal rotators, adductors-to-abductors ratio, and internal rotators-to-external rotators ratio | CS | 2 (−) |
| Grau et al33 (2008) | 10 Runners; 3 women, 7 men | 10 Runners; 3 women, 7 men | Iliotibial band syndrome | Hip abductors-to-adductors ratio, abductors, and adductors | CS | 2 (−) |
| Piva et al14 (2005) | 30; 17 Women, 13 men | 30 Age- and sex-matched participants; 17 women, 13 men | PFPS | Hip external rotators and abductors | CS | 2 (−) |
| Cichanowski et al32 (2007) | 13 Female collegiate athletes | 13 Age-, sex-, and sport-matched female collegiate athletes | PFP | Hip flexors, hip extensors, abductors, adductors, internal rotators, and external rotators | CS | 2 (−) |
| Olmo et al49 (2007) | 22 Male high school soccer players; involved leg | 22 Male high school soccer players; uninvolved leg | PFP | Knee flexors and knee extensors | CS | 2 (−) |
| Ferber et al20 (2010) | 15 Runners; 5 men, 10 women | 10 Runners; 4 men, 6 women | PFPS | Hip adductors | Cohort | 2 (−) |
| Finnoff et al42 (2011) | 5 High school runners; 3 female, 2 male | 93 High school runners; 41 female, 51 male | PFP | Hip abductors, hip adductors, hip flexors, hip extensors, internal rotators, external rotators, hip flexors-to-extensors ratio, abductors-to-adductors ratio, and external rotators-to-internal rotators ratio | Prospective cohort | 2 (−) |
| Kaya et al45 (2011) | 24 Women; involved leg | 24 Women; uninvolved leg | PFPS | Knee extensors | Case control | 2 (−) |
| Magalhães et al13 (2010) | 50 Sedentary women; 21 unilateral, 29 bilateral | 50 Sedentary women | PFPS | Hip flexors, hip extensors, abductors, adductors, internal rotators, and external rotators | CS | 2 (−) |
| Magalhães et al47 (2013) | 60 Women | 60 Women | PFP | Hip flexors-to-extensors ratio, adductors-to-abductors ratio, and internal rotators-to-external rotators ratio | CS | 2 (−) |
| Souza and Powers30 (2009) | 19 Women | 19 Women | PFP | Hip extensors, external rotators, and abductors | CS | 2 (−) |
| Thijs et al31 (2011) | 16 Novice female runners | 61 Novice female runners | PFP | Hip flexors, hip extensors, abductors, adductors, internal rotators, external rotators, hip flexors-to-extensors ratio, abductors-to-adductors ratio, and external rotators-to-internal rotators ratio | Cohort | 2 (−) |
| Willson and Davis51 (2009) | 20 Women | 20 Women | PFPS | Lateral trunk flexion, hip abductors, hip external rotators, knee flexors, and knee extensors | Case control | 2 (−) |
Abbreviations: CS, cross-sectional; PFP, patellofemoral pain; PFPS, patellofemoral pain syndrome.
Individuals with knee overuse injuries were found to have lower absolute and normalized strength compared with asymptomatic persons (Table 2). Using measurement scale (absolute or normalized strength) and muscle group as moderators, we observed that absolute hip external-rotator (P = .046), knee-extensor (P < .001), and knee-flexor (P = .039) strength was weaker in individuals with knee overuse injuries than in asymptomatic persons (Figure 3). Also, individuals with knee overuse injuries had less normalized hip-extensor (P < .001), normalized hip-flexor (P < .001), hip external-rotator (P < .001), hip internal-rotator (P = .001), hip-adduction (P < .001), and hip-abductor (P < .001) strength than asymptomatic persons (Figure 4). Based on these findings, we concluded that symptomatic individuals produced less strength than their healthy counterparts, regardless of the scale used. No findings were significant for any other analyses using these 2 moderators (Table 2). In addition, at the time of this analysis, data were insufficient to determine if individuals with knee overuse injuries had lower absolute strength for the hip-adductor, hip-extensor, hip-flexor, and hip internal-rotator muscle groups compared with asymptomatic persons.
Table 2.
Summary Effects for Overall and Each Moderated Analyses
| Strength |
Variable |
Hedges g |
95% Confidence Interval |
P Value |
| Overall | ||||
| Absolute | Not applicable | −0.197 | −0.301, −0.093 | <.001 |
| Normalized | Not applicable | −0.678 | −0.812, −0.544 | <.001 |
| Absolute | Hip external rotator | −0.287 | −0.568, −0.005 | .046 |
| Absolute | Hip abductor | 0.061 | −0.182, 0.304 | .62 |
| Absolute | Knee extensor | −0.412 | −0.636, −0.187 | <.001 |
| Absolute | Knee flexor | −0.192 | −0.376, −0.009 | .04 |
| Normalized | Hip extensor | −0.611 | −0.862, −0.361 | <.001 |
| Normalized | Hip flexor | −0.681 | −1.077, −0.285 | <.001 |
| Normalized | Hip external rotator | −0.671 | −0.911, −0.430 | <.001 |
| Normalized | Hip internal rotator | −0.379 | −0.608, −0.149 | .001 |
| Normalized | Hip abductor | −1.029 | −1.339, −0.718 | <.001 |
| Normalized | Hip adductor | −0.686 | −1.085, −0.288 | <.001 |
| Normalized | Knee extensor | −0.034 | −1.068, 1.001 | .95 |
| Normalized | Knee flexor | −0.262 | −0.611, 0.087 | .14 |
| Hip | External-internal rotator | −0.494 | −0.991, 0.003 | .052 |
| Hip | Internal-external rotator | −0.365 | −1.992, 1.261 | .66 |
| Hip | Flexor-extensor | 0.120 | −0.253, 0.493 | .53 |
| Hip | Abductor-adductor | 0.163 | −0.119, 0.446 | .26 |
| Hip | Adductor-abductor | 1.676 | −0.550, 3.903 | .14 |
| Absolute | Male | −0.719 | −1.106, −0.332 | <.001 |
| Normalized | Male | −1.256 | −1.908, −0.604 | <.001 |
| Absolute | Female | −0.340 | −0.517, −0.163 | <.001 |
| Normalized | Female | −0.776 | −0.941, −0.611 | <.001 |
Figure 3.
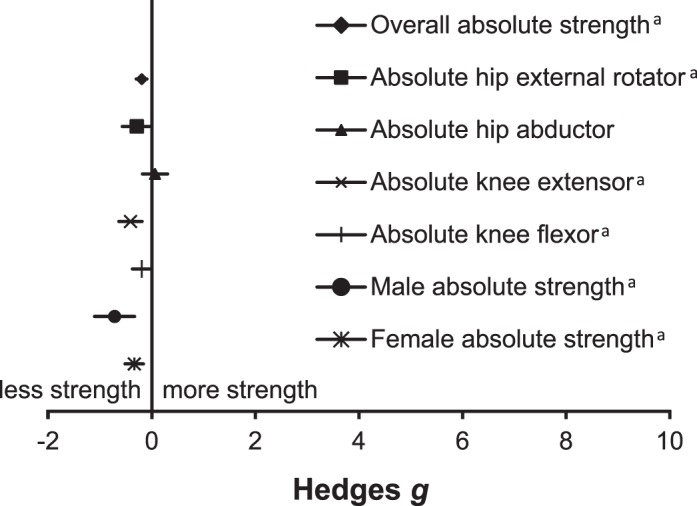
Forest plot of overall absolute strength and moderated analyses. a Indicates difference (P ≤ .05).
Figure 4.
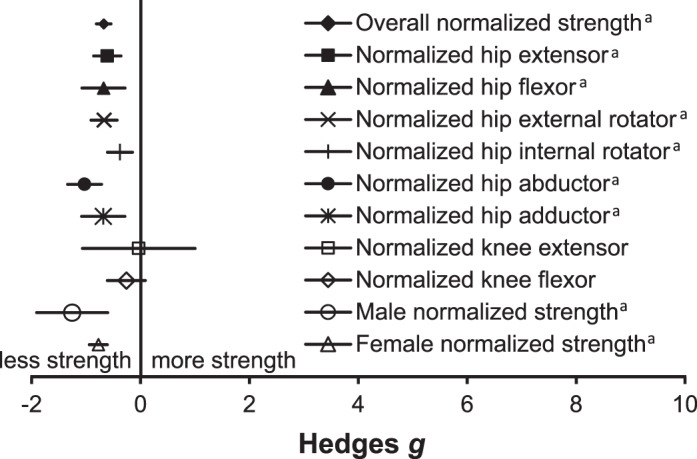
Forest plot of overall normalized strength and moderated analyses. a Indicates difference (P ≤ .05).
The muscle strength ratio of opposing muscle groups at the hip was also used as a moderator (Table 2). Individuals with knee overuse injuries did not have different hip external-internal rotator (P = .052), hip internal-external rotator (P = .660), hip flexor-extensor (P = .529), hip abductor-adductor (P = .257), or hip adductor-abductor (P = .140) strength ratios compared with asymptomatic control participants (Figure 5). Therefore, we concluded that persons with knee overuse injuries did not present with different hip-strength ratios between opposing muscle groups compared with asymptomatic persons.
Figure 5.
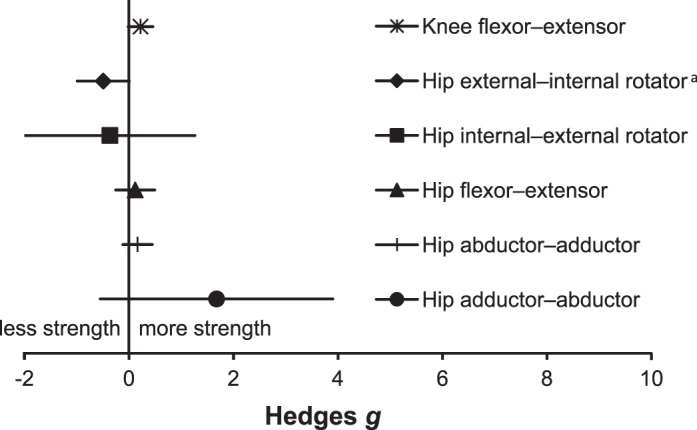
Forest plot of ratio strength. a Indicates difference (P ≤ .05).
Finally, using sex and measurement scale as moderators, we observed that males with knee overuse injures had less absolute muscular strength (P < .001) and normalized muscular strength (P < .001) than asymptomatic males (Table 2). Similarly, females with knee overuse injures produced less absolute muscular strength (P < .001) and normalized muscular strength (P < .001) compared with asymptomatic females (Table 2). Based on these findings, it appears that symptomatic individuals presented lower muscular-strength values than asymptomatic control participants, regardless of sex.
Publication bias was assessed using a funnel plot, which indicated that there was no publication bias (Figure 1). In addition, the fail-safe N analysis showed that for our 2 highest P values below .05, 5 negative effect sizes would be required to increase the P value for the meta-analysis to above .05. The fail-safe N calculated for the meta-analyses ranged between 0 and 7307, with an average fail-safe N of 750.77 negative effect sizes required to increase the P value for the meta-analysis to above .05.
DISCUSSION
Knee overuse injuries are common in training, active-duty, and reserve military personnel.1,2,6,7,10 To our knowledge, we are the first to summarize the strength-related studies in this area in an effort to support the development of effective screening, training, and preventive interventions for military trainees as well as active-duty, National Guard, and reserve personnel. Our main finding was that individuals with knee overuse injuries have lower hip and knee strength compared with asymptomatic control participants. Biomechanically, muscles are not only actuators and decelerators of motion but also stabilizers against motion, thus providing a protective mechanism for the more distal segments of an extremity.9,52 For example, in the lower extremities, the hip and knee muscles work together synergistically to control the various degrees of freedom of the hip joint.52,53 Failure of the hip and trunk musculature to control this motion may negatively influence distal segmental alignment9,52 upon foot contact. This could result in abnormal patellar motion through the trochlear groove and increase an individual's risk of developing patellofemoral pain syndrome.28,52
Muscle weakness was evident in people with different types of knee overuse injuries. Patellofemoral pain (ie, patellofemoral pain syndrome) was the most frequently reported knee overuse injury, affecting participants in 21 of the 25 studies in the literature (representing 130 of 167 data points). Only 4 other studies that met our inclusion criteria explored other types of knee overuse injuries: iliotibial band syndrome (2 studies identified) and patellar tendon injuries (tendinitis or tendinopathy; 2 studies identified). The separate analyses for iliotibial band syndrome and patellar tendon injuries produced similar results as those for patellofemoral pain syndrome.
Hip abductors (17 of 25 studies) and hip external rotators (15 of 25 studies) were the most commonly evaluated muscle groups. The hip abductors and external rotators aid in preventing excessive femoral adduction and internal rotation during weight-bearing activities. Researchers29,30,54 have theorized that increased femoral internal rotation during cyclical weight-bearing activities (eg, long-distance running) may predispose individuals to patellofemoral pain syndrome. This meta-analysis provided clear evidence that symptomatic individuals present with less normalized hip-abductor strength and less absolute and normalized external-rotator muscle strength than asymptomatic control participants. However, because the studies included in the meta-analysis mainly had cross-sectional designs, it is unclear whether strength deficits contribute to or are the result of these specific conditions. Investigators need to conduct more studies using longitudinal designs to help determine causality.
In addition to presenting with less normalized hip-abductor strength and less absolute and normalized external-rotator muscle strength than asymptomatic persons, those with knee overuse injuries also had normalized strength weakness of the hip extensors, hip flexors, hip internal rotators, and hip adductors. The same result was also observed with absolute sagittal-plane knee strength. This may point to a more global weakness in the lower extremity among those reporting knee overuse injuries; thus, future intervention programs should include appropriate functional activities that integrate multiple muscle groups across the activity.
We also assessed evidence of imbalances between opposing muscle groups by looking at strength ratios. We found only 7 groups that compared strength ratios between symptomatic and asymptomatic individuals. Of these studies, 5 evaluated hip abductor-adductor or adductor-abductor ratio strength; 3 of 7 studies also evaluated the hip flexor-extensor ratio, 2 of 7 assessed the knee flexor-extensor ratio, and 4 of 7 assessed the hip external-internal– or internal-external–rotator strength ratios. Our results indicated that strength ratios between any of these opposing muscle groups at the hip were not different in symptomatic individuals compared with control participants.
The results of our analyses suggested that both males and females with knee overuse injuries had less muscular strength than asymptomatic control participants. In 15 of 25 studies, separate strength data were provided for asymptomatic and systematic females. In 9 of 25 studies, strength data were available for asymptomatic individuals and symptomatic individuals (not separated by sex). Our literature search revealed a lack of published studies providing separate strength data for asymptomatic and symptomatic males. Only 4 studies meeting the inclusion criteria provided separate data for asymptomatic males and symptomatic males.
Overall, our results provide clear evidence that those with patellofemoral pain syndrome had less muscular strength than asymptomatic control participants (specifically at the hip and knee). The majority of the studies included in the meta-analysis involved cross-sectional designs; thus, we were unable to determine cause and effect (Table 1). As stated earlier, longitudinal studies are required to determine causality. Arguably, the muscular weakness observed at the knee in the symptomatic population may be a result of muscular inhibition. In a meta-analysis55 conducted in 2010, the investigators reported evidence supporting this relationship between the quadriceps musculature and anterior knee pain, in which muscular inhibition resulting from anterior knee pain reduced quadriceps activation by 78.6% on the involved side and 77.7% on the contralateral side.
In most of the included studies, the authors looked primarily at patellofemoral pain syndrome, with very few data points contributed by participants with iliotibial band syndrome or patellar tendinopathy. Another limitation was a lack of comparative data for males only. It remains unclear if males with knee overuse injuries have weak hip and thigh musculature compared with asymptomatic males. As per the SIGN criteria, the grade recommendation for the present study is a C, that is, a body of evidence including studies rated as 2+, directly applicable to the target population, and demonstrating overall consistency of results.
This meta-analysis suggests that individuals with symptoms of a knee overuse injury have lower hip muscular strength compared with control groups. The strength ratios of opposing muscle groups at the hip were not different in symptomatic persons compared with asymptomatic control persons. This knowledge may assist, along with research on other contributing factors, to develop effective screening, prevention, training, and rehabilitation protocols for military athletes.
REFERENCES
- 1. Allison KF, Keenan KA, Sell TC, et al. Musculoskeletal, biomechanical, and physiological gender differences in the US military. US Army Med Dep J. April−June 2015: 22−32. [PubMed] [Google Scholar]
- 2. Hauret KG, Jones BH, Bullock SH, Canham-Chervak M, Canada S. . Musculoskeletal injuries description of an under-recognized injury problem among military personnel. Am J Prev Med. 2010; 38 suppl 1: S61– S70. [DOI] [PubMed] [Google Scholar]
- 3. Heir T. . Musculoskeletal injuries in officer training: one-year follow-up. Mil Med. 1998; 163 4: 229– 233. [PubMed] [Google Scholar]
- 4. Taanila H, Suni J, Pihlajamaki H, et al. Musculoskeletal disorders in physically active conscripts: a one-year follow-up study in the Finnish Defence Forces. BMC Musculoskelet Disord. 2009; 10: 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kaufman KR, Brodine S, Shaffer R. . Military training-related injuries: surveillance, research, and prevention. Am J Prev Med. 2000; 18 suppl 3: S54– S63. [DOI] [PubMed] [Google Scholar]
- 6. Almeida SA, Williams KM, Shaffer RA, Brodine SK. . Epidemiological patterns of musculoskeletal injuries and physical training. Med Sci Sports Exerc. 1999; 31 8: 1176– 1182. [DOI] [PubMed] [Google Scholar]
- 7. Jones BH, Cowan DN, Tomlinson JP, Robinson JR, Polly DW, Frykman PN. . Epidemiology of injuries associated with physical training among young men in the army. Med Sci Sports Exerc. 1993; 25 2: 197– 203. [PubMed] [Google Scholar]
- 8. Brushøj C, Larsen K, Albrecht-Beste E, Nielsen MB, Løye F, Hölmich P. . Prevention of overuse injuries by a concurrent exercise program in subjects exposed to an increase in training load: a randomized controlled trial of 1020 army recruits. Am J Sports Med. 2008; 36 4: 663– 670. [DOI] [PubMed] [Google Scholar]
- 9. Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. . Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med. 2000; 28 4: 480– 489. [DOI] [PubMed] [Google Scholar]
- 10. Heir T, Glomsaker P. . Epidemiology of musculoskeletal injuries among Norwegian conscripts undergoing basic military training. Scand J Med Sci Sports. 1996; 6 3: 186– 191. [DOI] [PubMed] [Google Scholar]
- 11. Knapik JJ, Jones SB, Darakjy S, et al. Injury rates and injury risk factors among U.S. Army wheel vehicle mechanics. Mil Med. 2007; 172 9: 988– 996. [DOI] [PubMed] [Google Scholar]
- 12. Kaufman KR, Brodine SK, Shaffer RA, Johnson CW, Cullison TR. . The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med. 1999; 27 5: 585– 593. [DOI] [PubMed] [Google Scholar]
- 13. Magalhães E, Fukuda TY, Sacramento SN, Forgas A, Cohen M, Abdalla RJ. . A comparison of hip strength between sedentary females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2010; 40 10: 641– 647. [DOI] [PubMed] [Google Scholar]
- 14. Piva SR, Goodnite EA, Childs JD. . Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2005; 35 12: 793– 801. [DOI] [PubMed] [Google Scholar]
- 15. Chesworth BM, Culham E, Tata GE, Peat M. . Validation of outcome measures in patients with patellofemoral syndrome. J Orthop Sports Phys Ther. 1989; 10 8: 302– 308. [DOI] [PubMed] [Google Scholar]
- 16. Schreiber R, Louw Q. . The effect of gluteus medius training on hip kinematics in a runner with iliotibial band syndrome. S Afr J Physiother. 2011; 67 2: 23– 28. [Google Scholar]
- 17. Boling MC, Padua DA, Creighton Alexander R. Concentric and eccentric torque of the hip musculature in individuals with and without patellofemoral pain. J Athl Train. 2009; 44 1: 7– 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Meira EP, Brumitt J. . Influence of the hip on patients with patellofemoral pain syndrome: a systematic review. Sports Health. 2011; 3 5: 455– 465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Thomeé R, Augustsson J, Karlsson J. . Patellofemoral pain syndrome: a review of current issues. Sports Med. 1999; 28 4: 245– 262. [DOI] [PubMed] [Google Scholar]
- 20. Ferber R, Noehren B, Hamill J, Davis IS. . Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J Orthop Sports Phys Ther. 2010; 40 2: 52– 58. [DOI] [PubMed] [Google Scholar]
- 21. Baker RL, Souza RB, Fredericson M. . Iliotibial band syndrome: soft tissue and biomechanical factors in evaluation and treatment. PM R. 2011; 3 6: 550– 561. [DOI] [PubMed] [Google Scholar]
- 22. Post WR. . Patellofemoral pain: results of nonoperative treatment. Clin Orthop Relat Res. 2005; 436: 55– 59. [PubMed] [Google Scholar]
- 23. Collins N, Crossley K, Beller E, Darnell R, McPoil T, Vicenzino B. . Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: randomised clinical trial. Br J Sports Med. 2009; 43 3: 169– 171. [DOI] [PubMed] [Google Scholar]
- 24. Vicenzino B, Collins N, Crossley K, Beller E, Darnell R, McPoil T. . Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: a randomised clinical trial. BMC Musculoskelet Disord. 2008; 9: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Waryasz GR, McDermott AY. . Patellofemoral pain syndrome (PFPS): a systematic review of anatomy and potential risk factors. Dyn Med. 2008; 7: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Avraham F, Aviv S, Ya'akobi P, et al. The efficacy of treatment of different intervention programs for patellofemoral pain syndrome—a single blinded randomized clinical trial. Pilot study. ScientificWorldJournal. 2007; 7: 1256– 1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Reiman MP, Bolgla LA, Lorenz D. . Hip function's influence on knee dysfunction: a proximal link to a distal problem. J Sport Rehabil. 2009; 18 1: 33– 46. [DOI] [PubMed] [Google Scholar]
- 28. Tyler TF, Nicholas SJ, Mullaney MJ, McHugh MP. . The role of hip muscle function in the treatment of patellofernoral pain syndrome. Am J Sports Med. 2006; 34 4: 630– 636. [DOI] [PubMed] [Google Scholar]
- 29. Powers CM. . The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010; 40 2: 42– 51. [DOI] [PubMed] [Google Scholar]
- 30. Souza RB, Powers CM. . Predictors of hip internal rotation during running: an evaluation of hip strength and femoral structure in women with and without patellofemoral pain. Am J Sports Med. 2009; 37 3: 579– 587. [DOI] [PubMed] [Google Scholar]
- 31. Thijs Y, Pattyn E, Van Tiggelen D, Rombaut L, Witvrouw E. . Is hip muscle weakness a predisposing factor for patellofemoral pain in female novice runners? A prospective study. Am J Sports Med. 2011; 39 9: 1877– 1882. [DOI] [PubMed] [Google Scholar]
- 32. Cichanowski HR, Schmitt JS, Johnson RJ, Niemuth PE. . Hip strength in collegiate female athletes with patellofemoral pain. Med Sci Sports Exerc. 2007; 39 8: 1227– 1232. [DOI] [PubMed] [Google Scholar]
- 33. Grau S, Krauss I, Maiwald C, Best R, Horstmann T. . Hip abductor weakness is not the cause for iliotibial band syndrome. Int J Sports Med. 2008; 29 7: 579– 583. [DOI] [PubMed] [Google Scholar]
- 34. Fredericson M, Cookingham CL, Chaudhari AM, Dowdell BC, Oestreicher N, Sahrmann SA. . Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med. 2000; 10 3: 169– 175. [DOI] [PubMed] [Google Scholar]
- 35. Duvigneaud N, Bernard E, Stevens V, Witvrouw E, Van Tiggelen D. . Isokinetic assessment of patellofemoral pain syndrome: a prospective study in female recruits. Isokinet Exerc Sci. 2008; 16 4: 213– 219. [Google Scholar]
- 36. Moher D, Liberati A, Tetzlaff J, Altman DG. . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009; 62 10: 1006– 1012. [DOI] [PubMed] [Google Scholar]
- 37. Baldon Rde M, Nakagawa TH, Muniz TB, Amorim CF, Maciel CD, Serrao FV. Eccentric hip muscle function in females with and without patellofemoral pain syndrome. J Athl Train. 2009; 44 5: 490– 496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Bolgla L, Malone T, Umberger B, Uhl T. . Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008; 38 1: 12– 18. [DOI] [PubMed] [Google Scholar]
- 39. Chiu JK, Wong YM, Yung PS, Ng GY. . The effects of quadriceps strengthening on pain, function, and patellofemoral joint contact area in persons with patellofemoral pain. Am J Phys Med Rehabil. 2012; 91 2: 98– 106. [DOI] [PubMed] [Google Scholar]
- 40. Cowan SM, Crossley KM, Bennell KL. . Altered hip and trunk muscle function in individuals with patellofemoral pain. Br J Sports Med. 2009; 43 8: 584– 588. [DOI] [PubMed] [Google Scholar]
- 41. Ferber R, Kendall KD, Farr L. . Changes in knee biomechanics after a hip-abductor strengthening protocol for runners with patellofemoral pain syndrome. J Athl Train. 2011; 46 2: 142– 149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Finnoff JT, Hall MM, Kyle K, Krause DA, Lai J, Smith J. . Hip strength and knee pain in high school runners: a prospective study. PM R. 2011; 3 9: 792– 801. [DOI] [PubMed] [Google Scholar]
- 43. Hazneci B, Yildiz Y, Sekir U, Aydin T, Kalyon TA. . Efficacy of isokinetic exercise on joint position sense and muscle strength in patellofemoral pain syndrome. Am J Phys Med Rehabil. 2005; 84 7: 521– 527. [DOI] [PubMed] [Google Scholar]
- 44. Ireland M, Willson J, Ballantyne B, Davis I. . Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003; 33 11: 671– 676. [DOI] [PubMed] [Google Scholar]
- 45. Kaya D, Citaker S, Kerimoglu U, et al. Women with patellofemoral pain syndrome have quadriceps femoris volume and strength deficiency. Knee Surg Sports Traumatol Arthrosc. 2011; 19 2: 242– 247. [DOI] [PubMed] [Google Scholar]
- 46. Krauss I, Grau S, Rombach S, et al. Association of strength with patellar tendinopathy in female runners. Isokinet Exerc Sci. 2007; 15 3: 217– 223. [Google Scholar]
- 47. Magalhães E, Silva AP, Sacramento SN, Martin RL, Fukuda TY. . Isometric strength ratios of the hip musculature in females with patellofemoral pain: a comparison to pain-free controls. J Strength Cond Res. 2013; 27 8: 2165– 2170. [DOI] [PubMed] [Google Scholar]
- 48. Nakagawa T, Moriya É, Maciel C, Serrão F. . Trunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2012; 42 6: 491– 501. [DOI] [PubMed] [Google Scholar]
- 49. Olmo J, Aguado J, Cortés L, Espiniella A, Morate F. . Quadriceps strength loss at flexed knee angles in active high-level soccer players with patellofemoral pain. Isokinet Exerc Sci. 2007; 15 4: 303– 307. [Google Scholar]
- 50. Robinson RL, Nee RJ. . Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007; 37 5: 232– 238. [DOI] [PubMed] [Google Scholar]
- 51. Willson JD, Davis IS. . Lower extremity strength and mechanics during jumping in women with patellofemoral pain. J Sport Rehabil. 2009; 18 1: 76– 90. [DOI] [PubMed] [Google Scholar]
- 52. SIGN grading system 1999–2012. Scottish Intercollegiate Guidelines Network Web site. http://www.sign.ac.uk/guidelines/fulltext/50/annexoldb.html. Accessed December 11, 2012. [Google Scholar]
- 53. Claiborne TL, Armstrong CW, Gandhi V, Pincivero DM. . Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006; 22 1: 41– 50. [DOI] [PubMed] [Google Scholar]
- 54. Kollock RO, Onate JA, Van Lunen B. . Assessing muscular strength at the hip joint. Athl Ther Today. 2008; 13 2: 18– 24. [Google Scholar]
- 55. Niemuth PE, Johnson RJ, Myers MJ, Thieman TJ. . Hip muscle weakness and overuse injuries in recreational runners. Clin J Sport Med. 2005; 15 1: 14– 21. [DOI] [PubMed] [Google Scholar]