Abstract
Context:
Heat injury is a significant threat to military trainees. Different methods of heat mitigation are in use across military units. Mist fans are 1 of several methods used in the hot and humid climate of Fort Benning, Georgia.
Objectives:
To determine if (1) the mist fan or the cooling towel effectively lowered participant core temperature in the humid environment found at Fort Benning and (2) the mist fan or the cooling towel presented additional physiologic or safety benefits or detriments when used in this environment.
Design:
Randomized controlled clinical trial.
Setting:
Laboratory environmental chamber.
Patients or Other Participants:
Thirty-five physically active men aged 19 to 35 years.
Intervention(s):
(1) Mist fan, (2) commercial cooling towel, (3) passive-cooling (no intervention) control. All treatments lasted 20 minutes. Participants ran on a treadmill at 60% V̇o2max.
Main Outcome Measure(s):
Rectal core temperature, heart rate, thermal comfort, perceived temperature, perceived wetness, and blood pressure.
Results:
Average core temperature increased during 20 minutes of cooling (F1,28 = 64.76, P < .001, ηp2 = 0.70), regardless of group (F1,28 = 3.41, P = .08, ηp2 = 0.11) or condition (F1,28 < 1.0). Core temperature, heart rate, and blood pressure did not differ among the 3 conditions. Perceived temperature during 20 minutes of cooling decreased (F1,30 = 141.19, P < .001, ηp2 = 0.83) regardless of group or condition. Perceived temperature was lower with the mist-fan treatment than with the control treatment (F1,15 = 7.38, P = .02, ηp2 = 0.32). The mist-fan group perceived themselves to be cooler even at elevated core temperatures.
Conclusions:
The mist fan and cooling towel were both ineffective at lowering core temperature. Core temperature continued to increase after exercise in all groups. The mist fan produced feelings of coolness while the core temperature remained elevated, possibly increasing the risk of heat illness.
Key Words: military, heat illnesses, injury prevention, environmental conditions
Key Points
The mist fan was not effective in lowering core temperature in a hot and humid environment.
Core temperature continued to increase throughout the 20-minute cooling period in all conditions.
The commercial cooling towel did not lower core temperature or improve perceived coolness.
The mist fan created a feeling of coolness even at elevated core temperature, which may put a soldier or athlete at risk for heat injury while training in a hot and humid environment.
Heat-related injuries are a severe health threat during military training events1,2 as well as summer sport practice sessions.3−7 The effects of training in a hot environment can also strongly influence training and performance.3,8−13 Heat-related injury is a special threat from March through October at southern military training sites; it is also a threat in the north, where temperatures can suddenly increase before trainees have acclimatized. Soldiers in training coming from cooler climates without time to acclimate are also at elevated risk.7 Training events for tactical athletes are particularly problematic, as specialized training must be completed within limited timeframes, and clothing and equipment changes may not be options for safety reasons.4,14,15 Several heat-mitigation methods have been used to keep soldiers safe during outside training events.2,16 However, some methods currently in use have not been assessed to determine if they affect core temperature.
The Initial Entry Training Army site for infantry, armor, and cavalry soldiers, along with 2 basic training units and numerous career schools, is located at the Maneuver Center of Excellence, Fort Benning, Georgia. Fort Benning is known for its hot, humid climate that lasts 8 months of the year17; heat illness has been reported at this site every month of the year. Exertional heat illness is defined by the Army as a “spectrum of disorders (cramps, heat exhaustion, heat injury, heat stroke) resulting from total body heat stress. Primary heat casualties are forms of heat exhaustion, while more severe cases are heat stroke.”18 Heat-related injury is of particular concern in this environment because it is typically not possible to wait for a cooler day to conduct training. Heat-mitigation protocols (eg, uniform and equipment modifications) are in place, and mandatory heat-illness–prevention training occurs every spring.19 Additionally, intensive training events are conducted during the coolest hours of the day, with ruck marches often beginning at 2:00 am to avoid the heat. Every training unit monitors the heat index at each training location and practices heat emergency man-down and ice-sheeting drills daily.20 Heat emergency protocols include a quick evaluation to determine if a heat illness is involved, activating the emergency response process, moving the soldier to a cool location if possible, removing clothing, and applying ice sheeting with the feet elevated. If the soldier is conscious, he or she is allowed to sip cool water. If the soldier is unconscious, the airway and breathing are monitored. Ice sheeting involves wrapping the soldier with sheets from ice chests that are always kept with the unit. The ice sheet covers as much skin as possible (avoiding the face). If the sheet becomes warm, it is replaced with a new ice sheet, a process that continues until evacuation. One individual is assigned to stay with the soldier to monitor changes in status. The results of these efforts are clear: a low number of heat emergencies occur, even under the intense training conditions and given the high numbers of soldiers training.
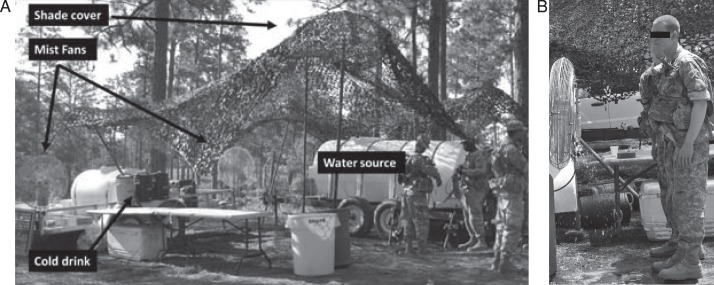
The cool zone is a site that is set up in the field to cool soldiers during training events at Fort Benning. The benefit of the cool zone in mitigating heat illness (or hyperthermia) is that it can be moved from place to place; training locations change daily and may occur anywhere across the 182 000 acres of the large Army post. The cool zone was designed as a preventive measure for all soldiers as opposed to an intervention for a soldier who has symptoms of heat illness. Once a soldier shows signs of a heat illness, the man-down ice-sheeting protocol is immediately initiated.21 The cool zone consists of a shaded area (trees or a canopy), mist fans, forearm cooling stations, and cool water or sports drinks. The exact setup varies by location and unit (Figure 1A and B). The mist fan requires fuel, a generator, and additional vehicles and time to implement. The mist fan cools by blowing a fine mist into the air. When the mist evaporates, it removes heat from the body (evaporative cooling). This method may be effective in dry climates. In the very humid environment at Fort Benning, the mist fans may not only fail to cool soldiers but also cause other problems. For example, the moisture from the mist fan may interfere with the evaporation of moisture and sweat, leaving the soldiers more wet and uncomfortable. Additionally, soldiers dislike the mist fans, complaining that they feel wet after using them. Wet uniforms often cause chafing during further maneuvers, frequently resulting in skin infections. Because research15 to date has called into question the effectiveness of mist fans, a Fort Benning unit asked us to investigate if the mist-fan aspect of the cool zone is an efficient heat-mitigation technique.
Figure 1.
A, Cooling zone setup. B, Mist fan.
METHODS
Experimental Design
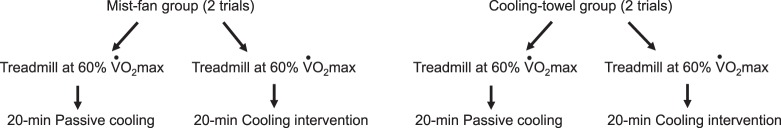
This study used a randomized, controlled, repeated-measures design. The independent variables for the mist-fan and cooling-towel interventions were condition (passive cooling or active cooling) and time. Session order and cooling method were determined by using a random number generator. For both the mist-fan and cooling-towel groups, passive cooling served as the control condition, and active cooling was the experimental intervention (Figure 2). The order of testing was randomly assigned to each participant. To ensure that the fitness levels of the active-cooling groups were not different, we measured V̇o2 performance. Dependent variables were rectal core temperature, heart rate, thermal comfort, perceived temperature, perceived wetness, and blood pressure.
Figure 2.
Experimental design.
Participants
Of the 36 men who began the study, 35 completed it (age range = 19 to 35 years, mist = 22.6 ± 3.19 years, cooling towel = 23.8 ± 4.23 years). One participant in the cooling-towel group was excluded because his core temperature elevated rapidly to the cutoff temperature after the exercise portion, forcing the termination of the trial. Participants completed the Physical Activity Readiness Questionnaire to ensure that there were no health contraindications to exercising in a hot and humid environment. The participants then read and signed the consent form approved by the institutional review board, which also approved the study. The primary investigator or a member of the research team was present to answer any questions.
Two interventions were tested: (1) mist fan (model VS-12; Schaefer Ventilation Equipment, St Cloud, MN) and (2) cooling towel (model Enduracool; Mission Athletecare, New York, NY). Each participant completed a passive-cooling condition (no cooling intervention), which served as the control condition. Anthropometric measures by group were height (mist fan = 1.78 ± 0.073 m, towel = 1.77 ± 0.059 m), weight (mist fan = 78.02 ± 12.09 kg, towel = 79.42 ± 10.52 kg), and V̇o2 (mist fan = 52.53 ± 6.82 mL O2·kg−1·min−1, towel = 51.78 ± 6.18 mL O2·kg−1·min−1).
Testing Protocol
Each participant performed a V̇o2max test to determine his fitness level 1 week before testing. One cooling condition (active or passive in random order) was completed on day 1. The remaining condition (active or passive) was completed a minimum of 7 days later to limit carryover effects. One participant completed the second condition in less than 7 days due to military deployment. He ran daily in the high humidity and temperature conditions consistent with those in our study, so we determined he was already acclimatized to the chamber conditions. Before inclusion, his results were assessed for any effect of the shorter washout period; no deviation was evident.
The V̇o2max Test
Participants completed a V̇o2max test to determine aerobic fitness. The V̇o2max tests were conducted on a treadmill (Woodway USA, Inc, Waukesha, WI) and analyzed via a metabolic measuring system (model TrueOne 2400; Parvo Medics Inc, East Sandy, UT). We averaged the highest values from the final stage of the graded exercise treadmill test to determine V̇o2max (mL O2·kg−1·min−1). The V̇o2max value and the submaximal recordings from the initial steady-state stages of the test (mL·kg−1·min−1) were used to calculate the treadmill speed that correlated with 60% of the individual's V̇o2max. The 60% level was chosen to increase the core temperature at a safe rate under the environmental conditions of this study. The speed that correlated with 60% intensity was used as the participant's running speed during the exercise portion of the cooling trials.
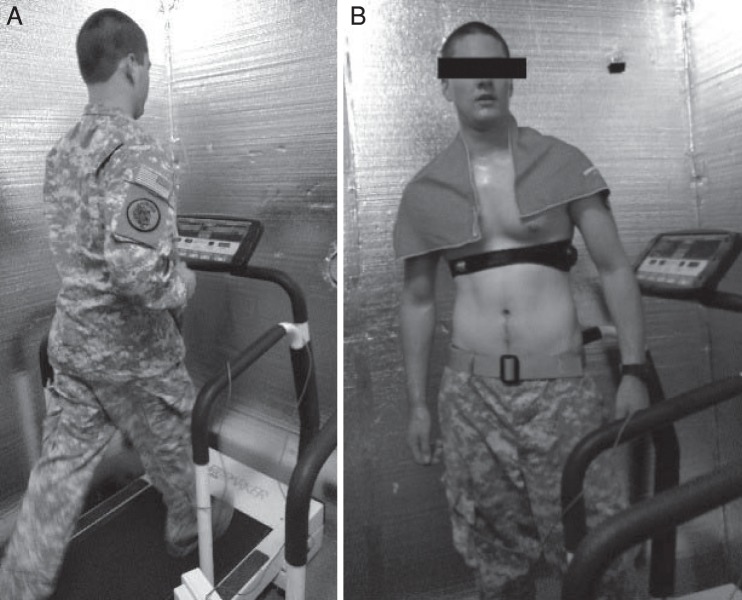
Experimental Trials
All trials were performed in the laboratory environmental chamber (mist-fan control trials: temperature = 32.05°C ± 0.50°C, relative humidity = 75.18% ± 2.7%; mist-fan treatment trials: temperature = 32.01°C ± 0.45°C, relative humidity = 75.31% ± 2.7%; towel control trials: temperature = 32.04°C ± 0.54°C, relative humidity = 75.15% ± 2.7%; towel treatment trials: temperature = 32.04°C ± 0.64°C, relative humidity = 75.91% ± 2.4%). Participants wore Army or Marine combat uniform (ACU) blouse, pants, T-shirt, and athletic shoes and socks (Figure 3A).
Figure 3.
A, Treadmill running in the environmental chamber. B, Cooling-towel intervention.
The trials were conducted the same way for both parts of this study (mist-fan group or cooling-towel group). Each trial consisted of exercise and a cooling portion. Upon each person's arrival, we measured his hydration status (via urine specific gravity) and baseline rectal core temperature (model 4000A; Yellow Springs Instruments Inc, Yellow Springs, OH). Each person was fitted with an activity monitor (model Bioharness 3; Zephyr Technology Corporation, Auckland, New Zealand) to assess heart rate. Baseline core temperature was measured before entry into the environmental chamber. Participants were then taken into the environmental chamber, and the exercise portion of the trial began. Each individual ran at 60% of his V̇o2max until core temperature was either 1.5°C above the baseline measurement or 39°C (the upper limit that participants were allowed to reach). After treadmill running was completed, participants were familiarized with the heat-perception scale, and cooling began immediately. All cooling phases (passive and active) were conducted in the thermal chamber. During the exercise phase, participants were given room-temperature water and allowed to drink ad libitum for their first trial. The amount of water ingested was recorded, and participants were required to drink the same amount during the exercise portion of the second trial. They did not drink during the cooling phases of this study.
Control Protocol.
Each participant underwent a control passive-cooling trial. Once the exercise protocol was completed, he removed the ACU blouse and T-shirt and stood for the 20-minute passive-cooling session in the chamber under the same environmental conditions as for the trial. We compared the passive-cooling data with those from the person's cooling-intervention session (mist fan or cooling towel) to test the efficacy of the cooling intervention.
Mist-Fan Protocol.
After the exercise portion of the trial, the participant removed his ACU blouse and T-shirt and stood approximately 2 ft (0.61 m) in front of the mist fan for 20 minutes of cooling. He alternated between facing toward and away from the fan in approximately 1-minute increments. In the field, the mist fan is used for only 1 to 5 minutes. We assessed cooling over 20 minutes to evaluate the effectiveness of 1 to 5 minutes of cooling and to determine if longer times resulted in more cooling.
Cooling-Towel Protocol.
After the exercise portion of the trial, the participant removed his ACU blouse and T-shirt and stood for the 20-minute cooling intervention in the environmental chamber. The towel was activated by snapping per the manufacturer's instructions and placed on the neck and shoulders of the individual (Figure 3B). After 10 minutes of cooling, the towel was removed, reactivated by snapping, and repositioned on the participant's neck and back.
Outcome Measures
Exercise Component.
During the exercise portion of the trial, rectal core temperature, heart rate, and ratings of perceived exertion (Borg scale) were collected every 5 minutes.
Cooling Component.
The measurements taken during the cooling phase are shown in Figure 4. During the cooling phase, heart rate and rectal core temperature were recorded every 2 minutes. Blood pressure was checked (model One Step Plus Memory; LifeSource, Chevy Chase, MD) every 5 minutes, and perceptual measures were recorded every 10 minutes. A Likert scale was used to evaluate measures of thermal comfort, perceived temperature, and perceived wetness. Thermal comfort rated how comfortable the person felt (range = neutral to extremely uncomfortable). Perceived temperature rated how hot the person felt (range = neutral to very hot). Perceived wetness rated how dry or wet the person felt (range = dry to very wet). All scales were measured from the left anchor term (neutral for perceived comfort and temperature and dry for perceived wetness) in centimeters. We compared values between the control and cooling sessions to determine the effect of the cooling method on perceptions.
Figure 4.
Timing of outcome measures during cooling phase of each trial.
Core temperature was measured via rectal probe. A member of the research team instructed each individual on how to properly insert the rectal probe to approximately 10 cm. The participant then went to the bathroom and inserted the probe himself. Next, the wire from the probe was secured to his clothing to minimize pulling or slipping during exercise.
Statistical Analysis
Missing Data.
With respect to core temperature data, 1 participant was missing data for the first time point of the cooling phase for both the control and experimental trials. Two participants were missing data for the 20-minute time point in the control condition, and 2 (separate) participants were missing data for the 20-minute time point in the experimental condition. Thus, 6 of 148 (approximately 4%) data points were missing for these primary outcome measures; similarly, these data points were missing for the survey and blood pressure measures. Data for all of these participants were removed from the analysis. Thus, the analyses involved 30 participants for core temperature and heart rate, 26 for blood pressure, and 32 for survey data. For the core temperature and heart rate analyses, we carried the last available data point forward to replace missing data. The results agreed with the data presented in the following sections, where missing data were omitted.
Tests of Statistical Assumptions.
We created Q-Q normal plots for each group at each time point and judged all the distributions to be approximately normal. A Shapiro-Wilk test confirmed no significant deviations from normality, except for core temperature in the cooling-towel group at time 0 of the control condition (W = 0.81, P < .01). Given that analysis of variance (ANOVA) is robust to violations of the normality assumption, we chose not to transform all cases of the dependent variable to adjust for this relatively minor violation of normality.
To test the effects of the different treatment conditions on core temperature and heart rate, we first conducted a group (mist fan versus cooling towel) × condition (passive-cooling control versus active-cooling experimental) × time (0 versus 20 minutes) mixed-factorial ANOVA with repeated measures on condition and time. Due to a significant 3-way interaction involving both core temperature and heart rate, we conducted follow-up condition × time ANOVAs separately for each group. For the analysis of blood pressure, we used a similar group × condition × time mixed-factorial ANOVA but with the additional repeated measure of cycle (diastolic versus systolic pressure). For analysis of the survey measures (thermal comfort, perceived temperature, and perceived wetness), a group × condition × time mixed-factorial ANOVA was conducted separately for each outcome.
RESULTS
Core Temperature
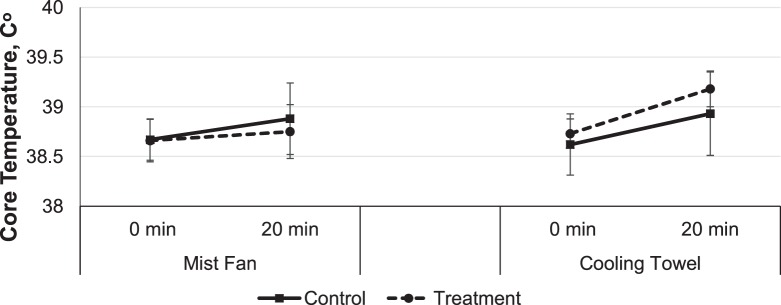
The significant 3-way interaction of group, condition, and time (F1,28 = 5.60, P = .03, ηp2 = 0.17; Figure 5) is important to understanding the significant increase in average core temperature across the 20 minutes of cooling (time 0 [38.67°C] to time 20 [38.94°C]; F1,28 = 64.76, P < .001, ηp2 = 0.70), regardless of group (F1,28 = 3.41, P = .08, ηp2 = 0.11) or condition (F1,28 < 1.0). When we explored this 3-way interaction with separate follow-up ANOVAs, evidence was insufficient to conclude that the increased temperature was attenuated by the treatment condition (ie, mist fan or cooling towel).
Figure 5.
Effect of experimental group, condition, and time on core temperature. Error bars are standard deviations for group at each time point.
In the mist-fan group, the main effect of time was significant: the average core temperature generally increased (Figure 5) from time 0 (38.67°C) to time 20 (38.82°C) during the cooling intervention (F1,15 = 9.52, P < .01, ηp2 = 0.39). Core temperature did not change over time between the mist-fan and control conditions (condition × time interaction: F1,15 = 2.52, P = .13, ηp2 = 0.14).
In the cooling-towel group, the effect of time was significant, such that the average core temperature generally increased from time 0 (38.67°C) to time 20 (39.06°C) during the cooling intervention (F1,13 = 73.98, P < .01, ηp2 = 0.85). Core temperature did not change over time between the cooling-towel and control conditions (condition × time interaction: F1,13 = 3.05, P = .10, ηp2 = 0.19). Thus, neither treatment condition (mist fan or cooling towel) was different from the passive-cooling control condition in decreasing core temperature.
Heart Rate
For heart rate, we noted a significant 3-way interaction of group, condition, and time (F1,28 = 11.99, P < .01, ηp2 = 0.30). To better understand this interaction, we calculated separate condition × time repeated-measures ANOVAs within each group. Heart rate did not differ between the groups (mist fan and towel: F1,28 < 1.0). However, cooling treatments decreased heart rate between the control (time 0 = 168.66 beats/min, time 20 = 130.38 beats/min) and treatment (time 0 = 168.17 beats/min, time 20 = 119.41 beats/min; F1,28 = 4.58, P = .04, ηp2 = 0.14) conditions (Figure 6). Time also affected heart rate: the longer participants cooled after exercise, the more heart rate decreased (time 0 versus time 20: F1,28 = 490.24, P < .001, ηp2 = 0.95).
Figure 6.
Effect of experimental group, condition, and time on heart rate. Error bars are standard deviations for group at each time point. a P < .001.
In the mist-fan group, we observed a significant condition × time interaction (F1,15 = 15.22, P < .001, ηp2 = 0.50). Heart rate decreased more in the mist-fan condition (time 0 = 169.56 beats/min, time 20 = 111.25 beats/min) than in the control condition (time 0 = 165.25 beats/min, time 20 = 133.19 beats/min).
Conversely, in the cooling-towel group, overall heart rate decreased over the 20 minutes of cooling (F1,13 = 262.18, P < .001, ηp2 = 0.95) but not between the treatment conditions, and no significant interaction was present. Thus, in the cooling-towel condition, the reduction in heart rate was not an effect of the treatment (cooling towel: time 0 = 166.79 beats/min, time 20 = 127.57 beats/min; control: time 0 = 172.07 beats/min, time 20 = 127.57 beats/min).
Blood Pressure
To analyze blood pressure, we added a within-subject factor of cycle (diastolic versus systolic) to the mixed-factorial ANOVA. Main effects were present for cycle (F1,24 = 505.72, P < .001, ηp2 = 0.96) and time (F1,24 = 15.30, P < .001, ηp2 = 0.39). A cycle × time interaction (F1,16 = 27.69, P < .001, ηp2 = 0.54) demonstrated that systolic blood pressure changed over time (time 0 = 137.61 mm Hg, time 20 = 120.69 mm Hg), whereas diastolic blood pressure did not change (time 0 = 77.94 mm Hg, time 20 = 77.16 mm Hg).
Neither group (F1,24 = 1.87, P = .19, ηp2 = 0.07) nor condition (F1,16 = 1.38, P = .25, ηp2 = 0.05) produced a main effect, and these factors did not interact, suggesting that although systolic blood pressure did tend to decrease over the cooling interval, the magnitude of the decrease did not depend on the method of cooling.
Survey Measures: Thermal Comfort, Perceived Temperature, and Perceived Wetness
Separate mixed-factorial ANOVAs were conducted for the 3 survey outcomes.
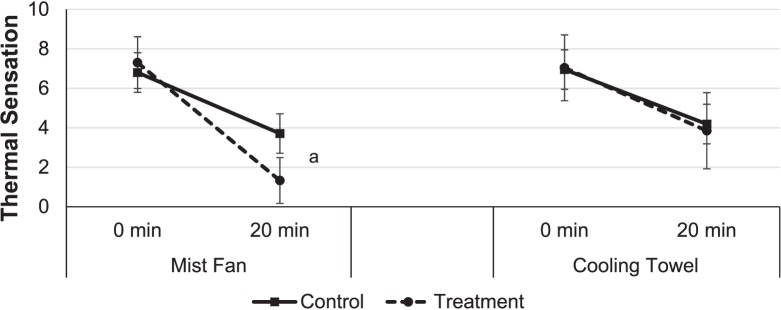
Thermal comfort decreased during the 20 minutes of cooling (F1,30 = 71.09, P < .001, ηp2 = 0.70). Furthermore, thermal comfort differed among groups (F1,30 = 4.75, P = .04, ηp2 = 0.14) and among the treatment and control conditions between the mist-fan and cooling-towel groups (3-way time × condition × group interaction: F1,30 = 16.61, P < .001, ηp2 = 0.34). This interaction was driven by the difference in thermal comfort over 20 minutes of cooling between the mist-fan treatment and the control treatment (condition × time interaction: F1,15 = 22.21, P < .001, ηp2 = 0.60). This interaction between treatment condition and time was not present in the towel group (F1,15 = 2.00, P = .18, ηp2 = 0.12). Thus, the mist-fan group rated themselves as more comfortable after the 20 minutes of cooling than in their control condition, whereas the cooling-towel group rated themselves the same as in their control condition.
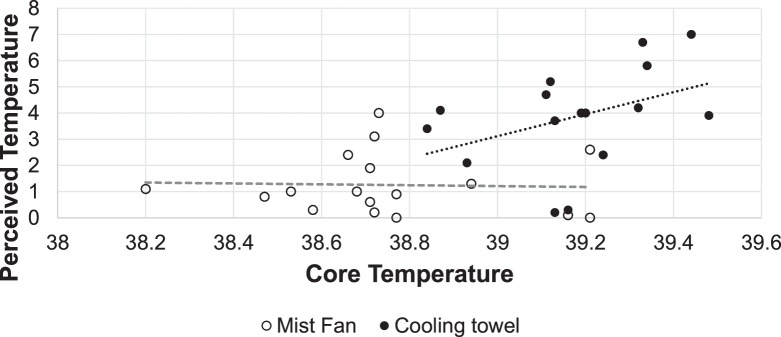
Perceived temperature decreased during the 20 minutes of cooling (F1,30 = 141.19, P < .001, ηp2 = 0.83), regardless of condition or treatment group. It also differed when the treatment condition was compared with the control condition during cooling (time × condition interaction: F1,30 = 8.59, P < .01, ηp2 = 0.22). Furthermore, a significant 3-way time × condition × group interaction indicated that the difference in perceived temperature across 20 minutes of cooling was determined by group (treatment or control) and treatment (mist fan or cooling towel: F1,30 = 4.70, P = .04, ηp2 = 0.14). This interaction, shown in Figures 7 and 8, was driven by the fact that, in the mist-fan group, perceived temperature decreased in comparison with the control treatment (F1,15 = 7.38, P = .02, ηp2 = 0.32). In the towel group, the treatment and control conditions did not differ (F1,15 < 1.0). Although their core temperature was elevated, the mist-fan group perceived themselves to be cooler.
Figure 7.
Effect of experimental group, condition, and time on thermal sensation. Error bars are standard deviations for group at each time point. a P < .001.
Figure 8.
Relationship between perceived and core temperature for the mist-fan and cooling-towel groups during cooling.
Perceived wetness differed between the active- and passive-cooling conditions (F1,30 = 18.72, P < .001, ηp2 = 0.38). It also differed between the treatment and control conditions as a function of group (group × condition interaction: F1,30 = 5.52, P = .03, ηp2 = 0.16). This interaction was driven by a larger mean difference between conditions in the mist-fan group (passive cooling [control] = 7.19, active cooling = 8.53) compared with the cooling-towel group (passive cooling [control] = 8.01, active cooling = 8.41). None of the other main effects or interactions were statistically significant.
DISCUSSION
The goals for this study were to determine if (1) the mist fan or the cooling towel effectively lowered participant core temperature in the humid environment of Fort Benning and (2) either the mist fan or the cooling towel presented additional physiologic or safety benefits or detriments when used in this environment.
Our most important finding was no lowering of core temperature after 20 minutes of exposure to either the mist fan or the cooling towel. Moreover, after exercise ceased, core temperature continued to increase in all groups (mist fan, cooling towel, and passive-cooling control) for the full 20 minutes of cooling. Elevated core temperature after exercise has been demonstrated in previous research,22−24 although this effect is likely unknown in athletes and military members. Evaporative cooling accounts for 75% of cooling during exercise.25 The addition of water into the air by the mist fans reduces the capacity of the air to take on more water, thereby reducing evaporative cooling.25 Investigators23,24 have demonstrated a reduction in heat dissipation by evaporative mechanisms after exercise despite elevated core temperatures. This thermal inertia results in prolonged elevation of postexercise core temperature, even as long as 60 minutes later.24 These previous studies revealed that after exercise, core temperature did not decrease when metabolic heat production returned to pre-exercise levels. In our study, core temperature continued to increase in all conditions (mist fan, cooling towel, and control) throughout the 20-minute cooling period. This continued increase in core temperature is important for military members to recognize as they work to keep soldiers safe in hot training environments.
The mean temperature changes for the passive-cooling (control) conditions for the mist-fan and cooling-towel groups were not different: 38.65°C at time 0 and 38.94°C 20 minutes after exertion ceased. Core temperature increased from time 0 at the end of exertion to time 20 at the end of cooling in both the mist-fan–treatment (from 38.64°C to 38.74°C) and cooling-towel–treatment groups (from 38.72°C to 39.17°C). We chose to have the participants stand in front of the mist fan for longer than they typically did when using the mist fans at Fort Benning (20 minutes in our study versus 1−5 minutes at Fort Benning). This allowed us to determine if simply standing in front of the mist fan longer would affect core temperature. However, core temperature continued to increase in all conditions throughout the 20-minute cooling period.
Our results were contrary to those in a study26 that assessed the use of mist fans to lower core temperature after exercise but agreed with other studies15,27 that found little effect of mist fans. Authors15 who found a decrease in core temperature used an environmental chamber set at 62% relative humidity compared with the 75% in our study. We chose the higher humidity level to more closely resemble summer weather at Fort Benning. Yearly humidity ranges from 20% in the winter to as high as 100% in the summer, when it exceeds 93% on 3 of every 4 days.17 The Army received the most complaints about the mist fans during the summer weather, when the higher humidity interfered with evaporation of water. It may be that mist-fan interventions are more effective at lowering core temperature in drier environments.
Commercial cooling towels are not currently in use during training at Fort Benning but have become popular in sports and recreation. Soldiers have long placed ice towels over their heads and under their helmets to cool off in the heat. Commercial cooling towels are impregnated with a formulation including purified water, denatured alcohol, aloe vera, menthol, and other chemicals.28 They are activated by water and a snap of the towel, eliminating the need for ice, and can be reactivated when they become warm. They are marketed to “aid in lowering body temperature by helping to dissipate body heat.”28 It is important for all athletes to note that the towels used under these test conditions had no effect on core temperature. Previous work27,29−31 with ice towels has been completed, but to date, research on commercial cooling towels is lacking. In a single study,32 commercial cooling towels in the intensive care unit were more hygienic and easier for nurses to use. However, cooling efficacy was not assessed.32 More investigation into these new products needs to be completed to determine if they provide any cooling effect. Reliance on a cooling strategy that has no effect on core temperature could create a dangerous situation for individuals exposed to hot environments.
Our second important finding was that the mist-fan group rated their temperature as feeling cooler, even though their core temperature remained elevated to the same extent as the other groups (cooling-towel and passive-cooling conditions). Ratings of thermal comfort, perceived temperature, and perceived wetness were obtained with the goal of understanding how the participants felt after the interventions. These measures have been used by previous authors to assess how comfortable the person is,33,34 how hot the person feels,30 or how wet the person feels.35,36 Even at higher core temperatures, the mist-fan group felt that they were cooler after the intervention (Figures 7 and 8). This could lead to soldiers and athletes misjudging their level of recovery from the heat and returning to training with an elevated core temperature. This is a safety concern that may put individuals at a higher risk for heat illness.
Participants using the mist-fan intervention also had a greater feeling of wetness, as expected. Evaporation of sweat and water is a primary method of cooling the body.19,37 The mist fan blows cool to warm water on the soldiers. Evaporation of the water from the mist fan may be hampered by high humidity, especially on days with little breeze. Soldiers' uniforms become wet, hampering evaporation of sweat.19,37 Soldiers also comment that they see increases in chafing on days they use the mist fans. This can be painful, and skin can become infected (common in the training environment), resulting in the need for medical care. These problems are compounded when the units are in the field for several days in a row, making it difficult to find dry clothing or care for the skin. If the mist-fan intervention is not effective, then it is important to identify methods that cool soldiers more effectively; do not increase risk because the soldier feels cooler, even though the core temperature remains elevated; and do not increase the risk of skin infection.
Evaluation of heart rate and blood pressure allowed us to assess the cooling interventions' effects on physiologic reactions to exercise under hot and humid conditions.12,38,39 Compared with passive cooling, the mist fan decreased heart rate after 20 minutes of cooling. Compared with the control condition, the cooling towel did not affect heart rate. Systolic blood pressure decreased during the cooling period in all conditions (mist fan, cooling towel, control).
The cooling area setup used in the field also includes forearm cooling by immersion and cool water or sports drinks. These interventions have been studied elsewhere40,41 and have been shown to have important effects in avoiding heat illness. We looked only at the mist fan, as it is the aspect of the cooling protocol that creates the most problems, is highest in cost, and had not been studied under the environmental conditions at Fort Benning, Georgia, to our knowledge. The benefit of completing this study in the field as compared with a laboratory heat chamber was also assessed. After spending several days in the field with the unit to determine the feasibility of a field study, we decided that the laboratory approach would produce more reliable data, as it would allow us to control for energy expended and maintain consistent environmental conditions without interfering with required training.
Limitations of our study include the fact that the most effective method of using cooling towels has not been researched. We conducted several pilot trials using an infrared thermography camera to assess changes in superficial skin temperature resulting from different methods. Draping the towel over the neck and shoulders was the most effective method tried during these trials. More research is recommended to determine the positive or negative effects of different commercial cooling towels used as heat-mitigation measures. We also decided against having participants wear boots and helmets. During heat-alert conditions, head gear is removed to improve cooling. Participants were not accustomed to wearing Army boots, and we felt this might interfere with treadmill walking or put them at risk for blisters. All participants wore the standard-issue ACU to ensure applicability of the results to the study population.
CONCLUSIONS
This study showed no beneficial effect of the mist fan or a commercial cooling towel in lowering core temperature in the hot and humid training environment representative of training conditions at Fort Benning, Georgia. In hot, humid environments, misters add water to the air, diminishing the body's ability to cool through evaporation. Additionally, core temperature continued to rise throughout the 20 minutes after exercise. Importantly, we also observed that the mist fan enabled the soldiers to feel cooler, even though core temperature remained elevated. This could result in soldiers returning to physical activity before they have properly recovered from the heat exposure, thereby increasing the risk of heat illness.
ACKNOWLEDGMENTS
We thank the Warrior Athletic Training Program athletic trainers and the Fort Benning cadre for their help on this project.
REFERENCES
- 1. Carter R, Cheuvront SN, Williams JO, et al. . Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med Sci Sports Exerc. 2005; 37 8: 1338– 1344. [DOI] [PubMed] [Google Scholar]
- 2. Dickinson JG. . Heat illness in the services. J R Army Med Corps. 1994; 140 1: 7– 12. [DOI] [PubMed] [Google Scholar]
- 3. Coris E, Ramirez A, Van Durme D. . Heat illness in athletes: the dangerous combination of heat, humidity and exercise. Sports Med. 2004; 34 1: 9– 16. [DOI] [PubMed] [Google Scholar]
- 4. Taylor NA. . Challenges to temperature regulation when working in hot environments. Ind Health. 2006; 44 3: 331– 344. [DOI] [PubMed] [Google Scholar]
- 5. Casa DJ, Armstrong LE, Ganio MS, Yeargin SW. . Exertional heat stroke in competitive athletes. Curr Sports Med Rep. 2005; 4 6: 309– 317. [DOI] [PubMed] [Google Scholar]
- 6. Casa DJ, Armstrong LE, Kenny GP, O'Connor FG, Huggins RA. . Exertional heat stroke: new concepts regarding cause and care. Curr Sports Med Rep. 2012; 11 3: 115– 123. [DOI] [PubMed] [Google Scholar]
- 7. Casa DJ, DeMartini JK, Bergeron MF, et al. . National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2015; 50 9: 986– 1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ely MR, Cheuvront SN, Roberts WO, Montain SJ. . Impact of weather on marathon-running performance. Med Sci Sports Exerc. 2007; 39 3: 487– 493. [DOI] [PubMed] [Google Scholar]
- 9. González-Alonso J, Teller C, Andersen SL, Jensen FB, Hyldig T, Nielsen B. . Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol (1985). 1999; 86 3: 1032– 1039. [DOI] [PubMed] [Google Scholar]
- 10. House J. . Extremity cooling as a method for reducing heat strain. J Def Sci. 1998; 3 1: 108– 114. [Google Scholar]
- 11. Maughan RJ, Shirreffs SM, Ozgünen KT, et al. . Living, training and playing in the heat: challenges to the football player and strategies for coping with environmental extremes. Scand J Med Sci Sports. 2010; 20 suppl 3: 117– 124. [DOI] [PubMed] [Google Scholar]
- 12. Cheuvront SN, Kenefick RW, Montain SJ, Sawka MN. . Mechanisms of aerobic performance impairment with heat stress and dehydration. J Appl Physiol (1985). 2010; 109 6: 1989– 1995. [DOI] [PubMed] [Google Scholar]
- 13. Houmard JA, Costill DL, Davis JA, Mitchell JB, Pascoe DD, Robergs RA. . The influence of exercise intensity on heat acclimation in trained subjects. Med Sci Sports Exerc. 1990; 22 5: 615– 620. [DOI] [PubMed] [Google Scholar]
- 14. McEntire SJ, Suyama J, Hostler D. . Mitigation and prevention of exertional heat stress in firefighters: a review of cooling strategies for structural firefighting and hazardous materials responders. Prehosp Emerg Care. 2013; 17 2: 241– 260. [DOI] [PubMed] [Google Scholar]
- 15. Selkirk GA, McLellan TM, Wong J. . Active versus passive cooling during work in warm environments while wearing firefighting protective clothing. J Occup Environ Hyg. 2004; 1 8: 521– 531. [DOI] [PubMed] [Google Scholar]
- 16. DeGroot DW, Gallimoreb RP, Thompson SM, Keneficka RW. . Extremity cooling for heat stress mitigation in military and occupational settings. J Therm Biol. 2013; 38 6: 305– 310. [Google Scholar]
- 17. Average weather for Fort Benning, Georgia, USA. WeatherSpark Web site. https://weatherspark.com/averages/30776/Fort-Benning-Georgia-United-States. Accessed July 13, 2016. [Google Scholar]
- 18. Heat illness prevention and sun safety: heat illness prevention. Army Public Health Center Web site. https://phc.amedd.army.mil/topics/discond/hipss/pages/heatinjuryprevention.aspx. Accessed July 13, 2016. [Google Scholar]
- 19. Pascoe DD, Shanley LA, Smith EW. . Clothing and exercise. I: biophysics of heat transfer between the individual, clothing and environment. Sports Med. 1994; 18 1: 38– 54. [DOI] [PubMed] [Google Scholar]
- 20. US Army Training and Doctrine Command. TRADOC Regulation 350-6: Enlisted Initial Entry Training Policies and Administration. Fort Eustis, VA: US Army Training and Doctrine Command; 2015. [Google Scholar]
- 21. US Army Training and Doctrine Command. TRADOC Regulation 350-29: Prevention of Heat and Cold Casualties. Fort Eustis, VA: US Army Training and Doctrine Command; 2010. [Google Scholar]
- 22. Journeay WS, Carter R III, Kenny GP. . Thermoregulatory control following dynamic exercise. Aviat Space Environ Med. 2006; 77 11: 1174– 1182. [PubMed] [Google Scholar]
- 23. Kenny GP, Reardon FD, Thoden JS, Giesbrecht GG. . Changes in exercise and post-exercise core temperature under different clothing conditions. Int J Biometeorol. 1999; 43 1: 8– 13. [DOI] [PubMed] [Google Scholar]
- 24. Kenny GP, Webb P, Ducharme MB, Reardon FD, Jay O. . Calorimetric measurement of postexercise net heat loss and residual body heat storage. Med Sci Sports Exerc. 2008; 40 9: 1629– 1636. [DOI] [PubMed] [Google Scholar]
- 25. Plowman SA, Smith DL. . Exercise Physiology for Health, Fitness, and Performance. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 26. Sinclair WH, Rudzki SJ, Leicht AS, Fogarty AL, Winter SK, Patterson MJ. . Efficacy of field treatments to reduce body core temperature in hyperthermic subjects. Med Sci Sports Exerc. 2009; 41 11: 1984– 1990. [DOI] [PubMed] [Google Scholar]
- 27. DeMartini JK, Ranalli GF, Casa DJ, et al. . Comparison of body cooling methods on physiological and perceptual measures of mildly hyperthermic athletes. J Strength Cond Res. 2011; 25 8: 2065– 2074. [DOI] [PubMed] [Google Scholar]
- 28. Wimer AH, . inventor. Cooling towel. US patent 0140-6736. July 25, 2015. [Google Scholar]
- 29. Ross ML, Garvican LA, Jeacocke NA, et al. . Novel precooling strategy enhances time trial cycling in the heat. Med Sci Sports Exerc. 2011; 43 1: 123– 133. [DOI] [PubMed] [Google Scholar]
- 30. Schulze E, Daanen HA, Levels K, et al. . Effect of thermal state and thermal comfort on cycling performance in the heat. Int J Sports Physiol Perform. 2015; 10 5: 655– 663. [DOI] [PubMed] [Google Scholar]
- 31. Verducci FM. . Interval cryotherapy decreases fatigue during repeated weight lifting. J Athl Train. 2000; 35 4: 422– 426. [PMC free article] [PubMed] [Google Scholar]
- 32. Vaga A, Busch M, Karlsen TE, Nilsen OB, Soreide E. . A pilot study of key nursing aspects with different cooling methods and devices in the ICU. Resuscitation. 2008; 76 1: 25– 30. [DOI] [PubMed] [Google Scholar]
- 33. Park H, Branson D, Petrova A, et al. . Impact of ballistic body armour and load carriage on walking patterns and perceived comfort. Ergonomics. 2013; 56 7: 1167– 1179. [DOI] [PubMed] [Google Scholar]
- 34. Sakellaris IA, Saraga DE, Mandin C, et al. . Perceived indoor environment and occupants' comfort in European “modern” office buildings: the OFFICAIR study. Int J Environ Res Public Health. 2016; 13(5). doi: 10.3390/ijerph13050444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Li Y. . Perceptions of temperature, moisture and comfort in clothing during environmental transients. Ergonomics. 2005; 48 3: 234– 248. [DOI] [PubMed] [Google Scholar]
- 36. Lee KA. . Design Implementation, Fabric Analysis, and Physiological and Subjective Testing of a Sportswear Garment Prototype [dissertation]. AL: Auburn University; 2014. [Google Scholar]
- 37. Pascoe DD, Bellingar TA, McCluskey BS. . Clothing and exercise. II. Influence of clothing during exercise/work in environmental extremes. Sports Med. 1994; 18 2: 94– 108. [DOI] [PubMed] [Google Scholar]
- 38. Sawka MN, Leon LR, Montain SJ, Sonna LA. . Integrated physiological mechanisms of exercise performance, adaptation, and maladaptation to heat stress. Compr Physiol. 2011; 1 4: 1883– 1928. [DOI] [PubMed] [Google Scholar]
- 39. Barberio MD, Elmer DJ, Laird RH, Lee KA, Gladden B, Pascoe DD. Systemic LPS. and inflammatory response during consecutive days of exercise in heat. Int J Sports Med. 2015; 36 3: 262– 270. [DOI] [PubMed] [Google Scholar]
- 40. Colburn D, Suyama J, Reis SE, et al. . A comparison of cooling techniques in firefighters after a live burn evolution. Prehosp Emerg Care. 2011; 15 2: 226– 232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hostler D, Reis SE, Bednez JC, Kerin S, Suyama J. . Comparison of active cooling devices with passive cooling for rehabilitation of firefighters performing exercise in thermal protective clothing: a report from the Fireground Rehab Evaluation (FIRE) trial. Prehosp Emerg Care. 2010; 14 3: 300– 309. [DOI] [PMC free article] [PubMed] [Google Scholar]