Abstract
Objective:
Although tactical athletes (eg, military service members, law enforcement personnel, fire fighters) are exposed to several known risk factors, it remains unclear if they are at increased risk for osteoarthritis (OA). The purpose of this systematic review was to investigate the association between serving as a tactical athlete and the incidence and prevalence of OA.
Data Sources:
We completed a comprehensive systematic literature search in November 2014 using 12 bibliographic databases (eg, PubMed, Ovid, SportDiscus) supplemented with manual searches of reference lists.
Study Selection:
Studies were included if they met the following criteria: (1) an aim of the study was to investigate an association between tactical athletes and OA; (2) the outcome measure was radiographic OA, clinical OA, total joint replacement, self-reported diagnosis of OA, or placement on a waiting list for a total joint replacement; (3) the study design was a cohort study; and (4) the study was written in English.
Data Extraction:
One investigator extracted data from articles that met all inclusion criteria (eg, group descriptions, measures of disease burden, source of nonexposed controls).
Data Synthesis:
Twelve articles met the inclusion criteria and described retrospective cohort studies. Firefighters, active-duty military service members, and veteran military parachutists consistently had a higher incidence or prevalence of knee, hip, or any OA diagnosis (4 studies). Active-duty pilots and veteran military parachutists may have a higher prevalence of spine OA, but this was not statistically significant (2 studies). Occupational risk factors for OA among tactical athletes include rank and branch of military service. The risk of OA among individuals who completed mandatory national military service remains unclear (6 studies).
Conclusions:
The incidence of OA among tactical athletes appears to be significantly higher when compared with nonexposed controls. Further research is needed to specifically identify modifiable risk factors within this high-risk population to develop and implement effective risk-reduction strategies.
Key Words: epidemiology, military, fire fighters, police, law enforcement, first responders
Key Points
Active-duty military service members were significantly more likely to experience knee osteoarthritis (OA), hip OA, and any OA diagnosis, regardless of site, when compared with nonexposed controls.
The disparity between military service members and nonexposed controls appeared to exist regardless of age or sex and increased with advancing age.
Military rank and branch of military service appeared to be occupational risk factors associated with OA incidence.
Fire fighters were at increased risk for both knee and hip OA, with adjusted risk ratios of 2.93 and 2.52, respectively.
Osteoarthritis (OA) is a chronic degenerative disease that involve the articular cartilage, bone, and surrounding soft tissues in the affected joint. It is estimated that more than 27 million adults in the United States are affected by this debilitating condition.1 Known risk factors for OA include female sex, obesity, history of joint injury, and engaging in occupations that require a significant amount of repetitive bending, squatting, kneeling, and lifting.2–12 Although OA is typically thought to be a disease that affects individuals later in life, studies5,13 suggest that OA can affect individuals in their third and fourth decades of life, particularly in the presence of these known risk factors. As a result, some individuals may live more than half their lives with a chronic disease that limits their function and diminishes their quality of life. Specifically, OA has been associated with an increased risk for several other chronic health conditions and comorbidities (eg, obesity, cardiovascular disease, type 2 diabetes), and OA negatively affects activities of daily living and quality of life and can contribute to occupational disability.14
Tactical athlete is a term that has been used to describe individuals in service professions (eg, the military, fire fighters, law enforcement, first responders) that have significant physical fitness and physical performance requirements associated with their work. Tactical athletes are regularly exposed to many of the known risk factors for OA described earlier. Because of the physical training requirements and the nature of their work, tactical athletes are at increased risk for acute traumatic joint injury.15–19 Furthermore, the physical training and occupational demands placed upon most tactical athletes require a significant amount of repetitive bending, squatting, kneeling, and lifting. Finally, even though most tactical athletes are not obese, many are required to endure heavy equipment loads during training and the performance of their occupational tasks. This may produce joint damage due to excessive loading that is similar to that observed in obese individuals. Despite their being regularly exposed to several known risk factors for OA, based on the available evidence, it remains unclear if tactical athletes are at increased risk for OA.
The purpose of our study was to conduct a systematic review of the literature to investigate the association between working as a tactical athlete and the incidence and prevalence of OA. A secondary objective was to identify gaps in the existing literature with regard to OA risk among tactical athletes.
METHODS
Data Sources and Searches
A comprehensive literature search was conducted by 1 investigator (K.L.C.) between November 5 and 9, 2014. The 12 primary databases searched were (1) PubMed, (2) Ovid: MEDLINE, (3) Ovid: MEDLINE Daily Updates, (4) Ovid OLDMEDLINE, (5) Your Journals@Ovid, (6) Ovid: MEDLINE In-Process and Other Nonindexed Citations, (7) Ovid Healthstar, (8) Cochrane Database of Systematic Reviews, (9) American College of Physicians Journal Club, (10) Database of Abstracts of Reviews of Effects, (11) Global Health, and (12) SPORTDiscus. Studies were identified using predetermined search criteria: (osteoarthritis OR degenerative joint disease) AND (prevalence OR incidence OR epidemiology OR odds ratio) AND (military OR army OR navy OR naval OR air force OR special forces OR paratroopers OR servicemen OR servicewomen OR soldier OR officers OR occupation OR firefighters OR firemen OR first responders OR police OR detective OR law enforcement OR paramedics) AND (case control OR cross section* OR cohort OR surveillance system). The reference lists of full-text articles were also manually searched to identify potential additional articles not indexed by electronic databases. We also screened our personal libraries to ensure we had identified all relevant articles. Because all of the included articles were from journals listed on PubMed, only PubMed was monitored for updates through March 13, 2015. This systematic review had no external funding source.
Study Selection
We included studies if they met the following 4 criteria: (1) an aim of the study was to investigate an association between tactical athletes and OA (see search criteria noted earlier); (2) the outcome measure was radiographic OA, clinical OA, total joint replacement, self-reported diagnosis of OA, or placement on a waiting list for a total joint replacement; (3) the design was a cohort study; and (4) the study was written in English. A cohort study design was defined as a study that compared the incidence or prevalence of OA among groups of people according to whether they had a history of working as a tactical athlete or not (exposure). We also included articles that examined OA incidence or prevalence in tactical athletes without a control group if comparable reference values (eg, OA incidence or prevalence) for the general population were available in the literature. Articles were excluded if the authors reported incidence or prevalence of arthritis instead of specifically OA. If the primary reviewer (K.L.C.) was unsure if a study met the inclusion and exclusion criteria, the other 2 authors (J.B.D., S.J.S.) reviewed the article and reached a consensus.
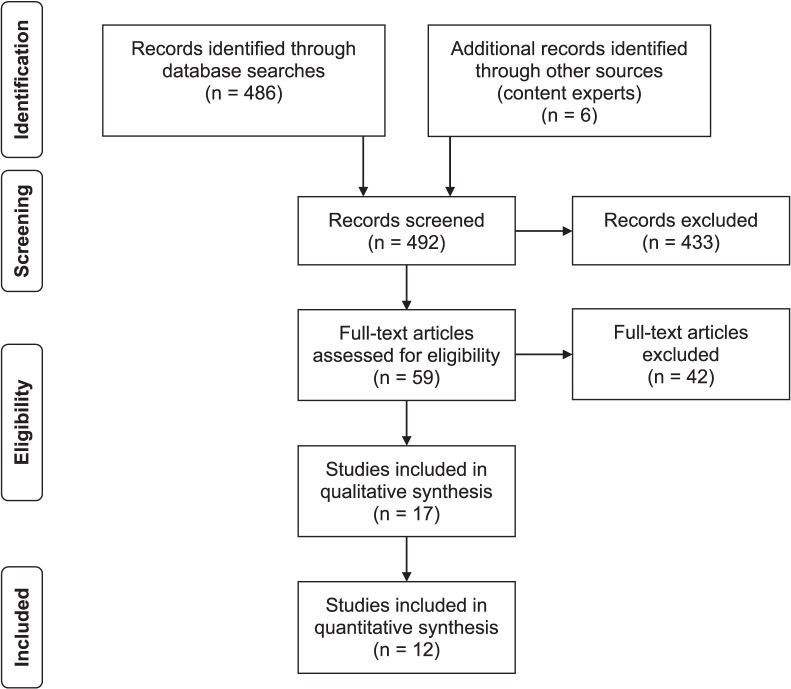
The Figure provides an overview of the selection of studies. Initially, we performed electronic and manual searches of reference lists. Articles clearly not meeting the inclusion or meeting the exclusion criteria were eliminated; if insufficient information was available in the abstract to assess inclusion and exclusion criteria, then we obtained the full-text article. After the initial screening process, full-text articles were retrieved and subsequently rescreened and independently assessed for meeting the inclusion and exclusion criteria by 2 authors (K.L.C., J.B.D.).
Figure.
Overview of the study identification, screening, and review process.
Data Extraction and Quality Assessment
The quality of the included studies was assessed by 2 raters (K.L.C., J.B.D.) using the Newcastle-Ottawa Scale (NOS). We chose this scale because of its ease of use and applicability for assessing cohort study designs.20 It assesses studies in 3 areas: selection (4 items), comparability (1 item), and outcome of cohort studies (3 items). The maximum score is 9 points, with higher scores indicating better quality.20 Coding rules and procedures were clarified as necessary between the 2 raters before their independent assessments. Specifically, comparability was scored based on a study's controlling for sex and age, and outcome was scored based on follow-up for 10 years or greater in 80% or more of the cohort. Authors (K.L.C., J.B.D.) independently rated each study in random order using the NOS instrument, and a third author (S.J.S.) provided consensus as needed. Consensus scores were determined using the following process. If the scores of authors 1 and 2 agreed, then that score was used as the consensus score. If the scores of authors 1 and 2 differed by 1 point (ie, 4 articles), the authors agreed on a consensus score through discussion. If the scores of authors 1 and 2 varied by 2 or more points or consensus could not be reached, author 3 scored the article, and all authors participated in discussion and reached a final consensus score. During this quality-assessment process, we excluded 1 article because of an inappropriate study design (ie, case control). This left 12 articles that had sufficient information and an appropriate study design to be included in the quantitative synthesis (Figure).
A data-extraction spreadsheet was generated and reviewed by 2 of the authors (K.L.C., J.B.D.). One author (K.L.C.) collected key information from each article: (1) publication data: first author, publication year, journal, country, study design, and quality-assessment score; (2) OA (outcome) details: definition of OA and time of follow up; (3) group descriptions: source of nonexposed cohort, source of exposed cohort, matching variables, sex, percentage lost to follow up, sample size, participant age; and (4) outcome measures. The outcome measures were studied joints; incidence or prevalence of OA; crude odds ratios, risk ratios, or rate ratios; adjusted odds ratios, risk ratios, or rate ratios; confounding variables; and associated 95% confidence intervals (CIs). A second author (J.B.D.) then compared the extracted data with the original articles to assess the accuracy of the extracted data.
Data Synthesis and Analysis
We extracted OA incidence or prevalence; risk, rate, or odds ratios; and 95% CIs. If only incidence or prevalence data were reported, then we calculated risk, rate, or odds ratios and 95% CIs (Table 1). All calculations were performed using STATA (version 10.1; Stata Corp, College Station, TX). Significant odds ratios were defined as 95% CIs that did not encompass 1.00. To assess the association between a history of being a tactical athlete and OA, we classified occupations into 1 of 3 categories: (1) significant association with OA, (2) unclear but possible association with OA, and (3) unclear but unlikely association with OA. Unclear but possible association with OA was defined as an odds ratio that was not statistically significant but was <0.70 or an odds ratio >1.50. Unclear but unlikely association with OA was defined as an odds ratio between 0.70 and 1.50. These cut points were based on odds ratios that correspond to a small standardized effect size (d = 0.20).33 These cut points are the same as those used by authors of another systematic review34 that evaluated the association between sport participation and knee OA.
Table 1.
Incidence and Prevalence of Osteoarthritis Among 12 Retrospective Cohort Studies Extended on Next Page
| Tactical Athletes |
||||||||
| Study (Year) |
Sex(es) |
Age Range, y |
Type of Osteoarthritis |
Outcome |
Osteoarthritis |
No Osteoarthritis |
Total |
Incidence/ Prevalence |
| Firefighters | ||||||||
| Vingard et al21 (1991) | Male | 38–78 | Knee | Cumulative index | 8 | 1232 | 1240 | 0.65% |
| Male | 38–78 | Hip | Cumulative index | 11 | 1229 | 1240 | 0.89% | |
| Active-duty US military | ||||||||
| Cameron et al22 (2011) | Both | 20–24 | Any | Incidence rate | 12 859 | 4 549 717 | 4 562 576 | 2.82a |
| Both | 25–29 | Any | Incidence rate | 14 260 | 2 855 135 | 2 869 395 | 4.97a | |
| Both | 30–34 | Any | Incidence rate | 15 446 | 1 995 313 | 2 010 759 | 7.68a | |
| Both | 35–39 | Any | Incidence rate | 25 721 | 1 784 737 | 1 810 458 | 14.21a | |
| Both | ≥40 | Any | Incidence rate | 37 950 | 1 372 453 | 1 410 403 | 26.91a | |
| Scher et al23 (2009) | Male | 20–29 | Hip | Incidence rate | 713 | 5 425 162 | 5 425 875 | 13.14b |
| Male | 30–39 | Hip | Incidence rate | 1129 | 3 021 556 | 3 022 685 | 37.35b | |
| Male | 40–49 | Hip | Incidence rate | 1425 | 1 074 946 | 1 076 371 | 132.39b | |
| Male | 20–49 | Hip | Incidence rate | 3267 | 9 521 664 | 9 524 931 | 34.30b | |
| Female | 20–29 | Hip | Incidence rate | 302 | 1 015 238 | 1 015 540 | 29.73b | |
| Female | 30–39 | Hip | Incidence rate | 299 | 406 951 | 407 250 | 73.42b | |
| Female | 40–49 | Hip | Incidence rate | 296 | 151 358 | 151 654 | 195.18b | |
| Female | 20–49 | Hip | Incidence rate | 897 | 1 573 547 | 1 574 444 | 56.97b | |
| Veteran military parachutists | ||||||||
| Murray-Leslie et al24 (1977) | Male | 23–70 | Knee | Prevalence | 19 | 27 | 46 | 41.30% |
| Murray-Leslie et al25 (1977) | Male | 23–70 | Lumbar | Prevalence | 39 | 7 | 46 | 84.80% |
| Active-duty military pilots | ||||||||
| Aydog et al26 (2004) | Male | 31–35 | Cervical | Prevalence | 31 | 219 | 250 | 12.40% |
| Male | 31–35 | Lumbar | Prevalence | 18 | 232 | 250 | 7.20% | |
| Mandatory national military service | ||||||||
| Kujala et al27 (1994) | Male | 21–85 | Knee | Prevalence | 18 | 1385 | 1403 | 1.30% |
| Male | 21–85 | Hip | Prevalence | 20 | 1383 | 1403 | 1.40% | |
| Male | 21–85 | Ankle | Prevalence | 0 | 1403 | 1403 | 0.00% | |
| Kujala et al28 (1999) | Male | 47–71 | Hip | Prevalence | 13 | 166 | 179 | 7.30% |
| Male | 47–71 | Knee | Prevalence | 19 | 160 | 179 | 10.60% | |
| Kettunen et al29 (2006) | Male | 38–86 | Knee | Prevalence | 119 | 388 | 507 | 23.50% |
| Male | 38–86 | Hip | Prevalence | 80 | 400 | 480 | 16.67% | |
| Kettunen et al30 (2001) | Male | 47–99 | Hip | Prevalence | 81 | 400 | 481 | 16.80% |
| Male | 47–99 | Knee | Prevalence | 120 | 388 | 508 | 23.60% | |
| Sarna et al31 (1997) | Male | NA | Ankle, knee, and hip | Prevalence | 36 | 1676 | 1712 | 2.10% |
| Iosifidis et al32 (2015) | Male | 50–51 | Ankle, knee, and hip | Prevalence | 39 | 124 | 163 | 23.90% |
Abbreviation: NA, not able to calculate due to lack of observed cases.
Incidence rate per 1000 person-years.
Incidence rate per 100 000 person-years.
Table 1.
Extended From Previous Page
| Nonexposed Athletes |
Estimate |
Ratio (95% Confidence Interval) |
|||
| Osteoarthritis |
No Osteoarthritis |
Total |
Incidence/ Prevalence |
||
| 200 | 90 857 | 91 057 | 0.22% | Risk ratio | 2.93 (1.32, 5.46) |
| 320 | 90 737 | 91 057 | 0.35% | Risk ratio | 2.52 (1.38, 4.64) |
| 576 | 257 285 | 257 861 | 2.23a | Risk ratio | 1.26 (1.16, 1.37) |
| 833 | 264 586 | 265 419 | 3.14a | Risk ratio | 1.58 (1.48, 1.70) |
| 1336 | 288 908 | 290 244 | 4.60a | Risk ratio | 1.67 (1.58, 1.77) |
| 2319 | 325 155 | 327 474 | 7.08a | Risk ratio | 2.01 (1.92, 2.09) |
| 7486 | 596 057 | 603 543 | 12.40a | Risk ratio | 2.17 (2.12, 2.22) |
| 0 | 20 669 | 20 669 | 0b | Risk ratio | NA |
| 2 | 25 461 | 25 463 | 7.85b | Risk ratio | 4.76 (1.31, 39.31) |
| 4 | 19 039 | 19 043 | 21.01b | Risk ratio | 6.30 (2.46, 23.16) |
| 6 | 65 169 | 65 175 | 9.21b | Risk ratio | 3.72 (1.71, 10.16) |
| 0 | 21 888 | 21 888 | 0b | Risk ratio | NA |
| 1 | 24 948 | 24 949 | 4.01b | Risk ratio | 18.32 (3.26, 725.89) |
| 0 | 18 812 | 18 812 | 0b | Risk ratio | NA |
| 1 | 65 648 | 65 649 | 1.52b | Risk ratio | 37.40 (6.70, 1478.92) |
| 6 | 52 | 58 | 10.40% | Odds ratio | 6.10 (2.00, 20.56) |
| 120 | 34 | 154 | 77.90% | Odds ratio | 1.57 (0.62, 4.55) |
| 6 | 52 | 58 | 10.40% | Odds ratio | 6.10 (2.00, 20.56) |
| 120 | 34 | 154 | 77.90% | Odds ratio | 1.57 (0.62, 4.55) |
| 10 | 488 | 498 | 2.00% | Odds ratio | 0.63 (0.28, 1.55) |
| 10 | 488 | 498 | 2.00% | Odds ratio | 0.71 (0.31, 1.70) |
| 1 | 497 | 498 | 0.20% | Odds ratio | NA |
| 14 | 250 | 264 | 5.30% | Odds ratio | 1.40 (0.59, 3.30) |
| 45 | 219 | 264 | 17.00% | Odds ratio | 0.58 (0.31, 1.05) |
| 17 | 67 | 84 | 20.20% | Odds ratio | 1.21 (0.67, 2.28) |
| 9 | 69 | 78 | 11.53% | Odds ratio | 1.53 (0.72, 3.64) |
| 21 | 182 | 203 | 10.30% | Odds ratio | 1.76 (1.04, 3.08) |
| 49 | 163 | 212 | 23.10% | Odds ratio | 1.03 (0.69, 1.54) |
| 120 | 2561 | 2681 | 4.50% | Odds ratio | 0.46 (0.31, 0.67) |
| 2 | 9 | 11 | 18.20% | Odds ratio | 1.42 (0.28, 13.98) |
RESULTS
Study Characteristics
We identified a total of 492 potential articles using the electronic search and additional search strategies. After extensive screening (Figure), we extracted data from 12 articles (Table 2), all of which were classified as retrospective cohort studies. Quality-assessment (NOS) scores ranged from 3 to 7, with higher scores representing higher-quality studies (Table 2). Various OA outcomes were examined across studies (Table 1). One group examined the cumulative incidence of knee and hip OA in Swedish firefighters compared with the general population in low-exposure occupations.21 The remaining researchers either examined the incidence or prevalence of OA in active-duty or veteran military populations22–26 or examined the prevalence of OA in European countries where national military service is mandatory.27–32 Two studies examined OA incidence rates in active-duty military populations22,23 and compared them with published reference rates in the general population.3,35,36 No studies were identified that examined OA incidence or prevalence in other tactical athlete populations (eg, law enforcement, first responders). The heterogeneity among the studies regarding the type of OA and study outcome (ie, prevalence, incidence, cumulative incidence) prohibited us from conducting a meta-analysis as part of this review.
Table 2.
Descriptive Characteristics of the Included Studiesa
| Study (Year) |
Country |
Source |
Osteoarthritis |
Age Range, y |
Newcastle-Ottawa Scaleb |
||
| Nonexposed |
Exposed |
Outcome |
Definition |
||||
| Kujula et al27 (1994) | Finland | Elite track-and-field athletes | National military service | Knee, hip, or ankle | Physician diagnosedc | 21–85 | 6.0 |
| Cameron et al22 (2011) | United States | Canadian general population | Active-duty US military | Any osteoarthritis diagnosis | Physician diagnosedc | 17–62 | 7.0 |
| Scher et al23 (2009) | United States | Worcester County, MA, population | Active-duty US military | Hip | Physician diagnosedc | 17–62 | 7.0 |
| Vingard et al21 (1991) | Sweden | Swedish general population (low-exposure occupations) | Firefighters | Knee or hip | Physician diagnosedc | 38–78 | 5.0 |
| Aydog et al26 (2004) | Turkey | Office personnel | Military pilots | Cervical or lumbar | Radiographs | 31–35d | 4.0 |
| Iosifidis et al32 (2015) | Greece | Former elite track-and-field athletes | National military service | Knee, hip, or ankle | Radiographs | 50–51d | 6.0 |
| Kettunen et al30 (2001) | Finland | Former elite track-and-field athletes | National military service | Knee and hip | Self-reported diagnosis | 47–99 | 4.0 |
| Kettunen et al29 (2006) | Finland | Master track-and-field athletes | National military service | Knee and hip | Self-reported physician diagnosed | 38–86 | 5.0 |
| Sarna et al31 (1997) | Finland | Former elite athletes | National military service | Knee, hip, or ankle | Physician diagnosedc | NA | 5.0 |
| Murray-Leslie et al24 (1977) | United Kingdom | Sport parachutists | Veteran military parachutists | Knee and ankle | Radiographs | 23–70 | 3.0 |
| Murray-Leslie et al25 (1977) | United Kingdom | Sport parachutists | Veteran military parachutists | Cervical or lumbar | Radiographs | 23–70 | 3.0 |
| Kujula et al28 (1999) | Finland | Orienteering endurance athletes | National military service | Knee and hip | Self-reported physician diagnosed | 47–71 | 6.0 |
Abbreviation: NA, no data to extract.
All studies had a retrospective cohort design.
Scores range from 0 to 9, with a higher score indicating higher quality.
Based on International Classification of Diseases codes or a national hospital discharge registry.
Only range of average ages could be extracted.
Osteoarthritis in Firefighters, Active-Duty, and Veteran Populations
In the single study21 that examined OA incidence in firefighters, the results suggested that firefighters were at increased risk for both knee and hip OA, with adjusted risk ratios of 2.93 and 2.52, respectively (Table 1). Active-duty military service members appeared to be at significantly greater risk for any OA diagnosis22 and for hip OA,23 regardless of sex or age, in comparison with reference rates in the general population. Furthermore, the disparity between active-duty military service members and nonexposed controls increased with advancing age.22,23
Military rank and branch of military service also seem to be associated with the incidence rate of OA in active-duty military service members (Tables 3 and 4).22,23 After controlling for the influence of sex, age, branch of military service, and race, those in the junior enlisted ranks had the highest incidence rates for both any OA diagnosis and hip OA, followed by senior enlisted personnel and senior officers (Table 3). Service in the Army was also associated with the highest incidence rate of any OA diagnosis and of hip OA after controlling for sex, age, race, and military rank (Table 4). Veteran military parachutists appeared to be significantly more likely to experience knee OA than sport parachutists.24 Although the odds ratios for lumbar and cervical OA in active-duty military pilots26 and veteran parachutists25 suggested a higher prevalence compared with controls, the observed differences failed to reach statistical significance. Regardless of significance, the incidence or prevalence of OA among firefighters, active-duty military service members, and veterans appeared to be consistently higher than in controls.
Table 3.
Incidence Rate Ratios by Rank in Active-Duty US Military
| Study (Year) |
Sex(es) |
Age Range, y |
Type of Osteoarthritis |
Rank |
Unadjusted Incidence Rate |
Adjusted Rate Ratioa (95% Confidence Interval) |
| Cameron et al22 (2011)b | Both | 18–62 | Any | Junior enlisted | 3.57 | 1.67 (1.63, 1.72) |
| Senior enlisted | 11.61 | 1.49 (1.46, 1.53) | ||||
| Junior officers | 5.74 | 1.00 | ||||
| Senior officers | 17.45 | 1.12 (1.09, 1.15) | ||||
| Scher et al23 (2009)c | Both | 18–62 | Hip | Junior enlisted | 16.60 | 1.90 (1.63, 2.22) |
| Senior enlisted | 24.80 | 1.31 (1.16, 1.48) | ||||
| Junior officers | 46.40 | 1.00 | ||||
| Senior officers | 112.00 | 1.50 (1.31, 1.73) |
Adjusted for sex, age, branch of military service, and race.
Incidence rate per 1000 person-years.
Incidence rate per 100 000 person-years.
Table 4.
Incidence Rate Ratios by Branch of Service in Active-Duty US Military
| Study (Year) |
Sex(es) |
Age Range, y |
Type of Osteoarthritis |
Service |
Unadjusted Incidence Rate |
Adjusted Rate Ratioa (95% Confidence Interval) |
| Cameron et al22 (2011)b | Both | 18–62 | Any | Army | 9.70 | 1.49 (1.47, 1.52) |
| Air Force | 8.06 | 1.08 (1.06, 1.10) | ||||
| Navy | 6.72 | 1.00 | ||||
| Marines | 4.71 | 1.07 (1.05, 1.10) | ||||
| Scher et al23 (2009)c | Both | 18–62 | Hip | Army | 43.30 | 1.90 (1.75, 2.07) |
| Marines | 37.00 | 1.85 (1.64, 2.09) | ||||
| Navy | 26.80 | 1.63 (1.49, 1.78) | ||||
| Air Force | 26.30 | 1.00 |
Adjusted for sex, age, military rank, and race.
Incidence rate per 1000 person-years.
Incidence rate per 100 000 person-years.
Mandatory National Military Service and OA
When we compared the prevalence of OA among those who had engaged in mandatory national military service with controls (elite-level male orienteering or track-and-field athletes), the results were inconclusive (Table 1). In 3 studies,27,28,31 the prevalence of OA was lower in those with mandatory national military service requirements than in controls; however, the prevalence of OA was significantly lower in only 1 of these studies.31 Conversely, investigators in 5 studies27–30,32 reported a higher prevalence of OA in those with mandatory national military service requirements compared with controls, but again, the prevalence of OA was significantly higher in only 1 of these studies.30 Authors of 2 studies37,28 found a higher prevalence for some OA outcomes and a lower prevalence for others.
DISCUSSION
Military service members and other tactical athletes likely share similar occupational exposures and risk factors for OA. These include an increased risk for joint injury; occupational and physical training demands that require frequent and repetitive kneeling, squatting, bending, and lifting; and wearing and carrying heavy equipment loads. Therefore, we hypothesized that tactical athletes would have a higher prevalence or incidence (or both) of OA when compared with nonexposed controls in the general population. The findings of our systematic review seem to support this hypothesis.
Osteoarthritis has consistently been a leading cause of disability discharge from the military for more than a decade, regardless of whether the estimates are from peacetime or periods of active combat.37,38 As a result, it is not surprising that the incidence and prevalence of OA among military service members and other tactical athletes in the current systematic review appeared to be higher than in nonexposed controls in the general population. This was particularly evident when we reviewed studies that specifically examined these OA outcomes in tactical athlete populations (Table 1).21–26 Active-duty military service members were significantly more likely to experience knee OA,24 hip OA,23 and any OA diagnosis regardless of site22 when compared with nonexposed controls. The disparity between military service members and nonexposed controls was present regardless of sex or age and increased with advancing age (Table 1). Though the prevalences of lumbar and cervical OA were 49% to 76% higher in specific military populations,24–26 the observed differences were not statistically significant. However, the magnitude of the observed odds ratios suggests an unclear but possible association with OA. Finally, based on the findings of a single study,21 the incidences of hip and knee OA appear to be 2.52 to 2.93 times higher, respectively, among firefighters than in nonexposed controls (Table 1). Despite the increased incidence and prevalence of OA observed among tactical-athlete populations, it remains unclear which specific risk factors or occupational exposures are contributing to the observed disparities between tactical athletes and nonexposed controls in the general population. Further study is needed to identify important modifiable and nonmodifiable risk factors for OA within this unique high-risk population in order to develop and implement effective primary and secondary risk-reduction strategies.
Military service members experience incidence rates for acute traumatic joint injuries that are an order of magnitude higher than rates observed in the general population,15–17,19,39 and acute traumatic joint injury has been identified as an important risk factor for OA.4,5,40,41 Although estimates are that posttraumatic OA accounts for 12% of all OA cases in the general population,42 the prevalence of posttraumatic OA in tactical athletes remains unclear and is probably much higher. Joint trauma in military populations has been associated with high rates of disability and medical discharge from service38,43–46 and likely contributes to the high rates of disability discharge associated with OA observed in this population.37,47,48 Limited data are available on acute traumatic joint injuries in other tactical athlete populations, but they are also probably at increased risk for these injuries. Based on the available data, it is unclear how many of the OA cases in our systematic review were associated with acute traumatic joint injury; however, given the observed disparities in the incidence and prevalence of OA and the high rates of joint trauma among tactical athletes, it is likely that posttraumatic OA is contributing to these differences.22 A possible association is also suggested by the highest rates of acute traumatic joint injury and OA, which are both seen within the junior enlisted ranks.15 As a result, in future studies, it is critical to accurately account for the number of OA cases among tactical athletes that may be related to a history of acute traumatic joint injury. Military service members offer a unique opportunity to study the progression of posttraumatic OA from the preinjury state due to the closed Military Health System and the available surveillance resources in this population.22,49 It is also critical to develop and implement primary prevention strategies to limit the effects of acute traumatic joint injuries in tactical-athlete populations. Emerging evidence suggests that injury-prevention programs targeting high-risk biomechanical movement patterns may be effective in the primary prevention of acute traumatic knee-joint injury,50,51 and these programs may be applicable to military training populations.52 Information on effective acute traumatic injury-prevention strategies for other joints is currently limited in the literature.
In addition to high rates of acute traumatic joint injury, tactical athletes also routinely engage in occupational and physical training activities that require frequent and repetitive bending, squatting, kneeling, and lifting. A substantial amount of evidence in the literature suggests that high-level occupation-related physical demands, particularly those that involve frequent and repetitive bending, squatting, kneeling, lifting, and climbing, may be associated with knee6,9,53–57 and hip56–59 OA. In the current systematic review, we observed that military rank and branch of military service were associated with the incidence of OA. Specifically, those serving in the Army and the junior enlisted ranks experienced the highest rates of OA after potentially important confounding variables, including sex and age, were controlled. These occupation-related factors may be surrogate measures for engaging in the high-risk occupational demands noted earlier; however, further research and analysis by specific Department of Defense occupational groups (eg, Military Occupational Specialty codes [MOS], Air Force Specialty Codes [AFSC], Navy Enlisted Classification system [NEC]) are warranted to determine which occupational codes are associated with the highest incidence of OA.22
Military service members are required to meet minimum height and weight standards, which limits the number of military personnel who are overweight and obese (a known risk factor for OA); however, a modern combat load can range from 52 lb (24 kg) to well over 100 lb (45 kg).60 Routinely carrying a load of this nature during extended military training or deployments may result in the same overloading of joints in tactical athletes that is typically seen in obese individuals in the general population. This excessive loading combined with repetitive physical activity (eg, marching, running) or joint injury (or both) may increase joint vulnerability and the risk of OA, even in young and physically fit tactical athletes.11 Excessive occupational loads are not limited to military personnel, as firefighters and law enforcement officers may also have to carry or bear heavy equipment in the execution of their duties. For firefighters, this equipment may include personal protective clothing, breathing equipment, hoses, ladders, and axes, which have been estimated to weigh between 45 lb (20 kg) and 75 lb (34 kg). For law enforcement officers, this may include personal protective equipment and clothing, shields, helmets, bulletproof vests, and other tactical gear. Further research is needed to better understand the association between exposure to these loads during the execution of occupational tasks and joint loading in relation to the initiation and progression of OA over time in tactical-athlete populations.
Although active-duty military service was consistently associated with OA, findings were inconsistent among the 5 studies that included individuals who participated in mandatory national military service in Finland or Greece. Each nation requires less than 1 year of active service.61 In a previous systematic review,34 individuals who participated in national military service were more likely to develop knee OA than were former athletes, including the reference groups selected for this systematic review (eg, former elite track-and-field athletes, former elite athletes, orienteering athletes). In our review, we failed to confirm that individuals with a history of mandatory national military service were at higher risk for OA. Unfortunately, the small number of studies and variations in the study designs, outcomes, ages, joint(s) of interest, and reference groups prevented us from pursuing a meta-analysis to further explore the association between mandatory national military service and OA. Future researchers should prospectively follow individuals in nations with various lengths of mandatory military service to determine its effect on OA. This is an interesting question because mandatory national military service may expose untrained individuals to episodes of overloading or increase their risk of injury, which could increase their risk of OA. Conversely, mandatory national military service may teach young adults the importance of a physically active and healthy lifestyle, which could reduce their risk for symptomatic OA, particularly if the required terms of service are of short duration. Finally, mandatory national military service may spread a relatively short-duration occupational exposure to OA over the entire population in comparison with an all-volunteer force, in which multiyear and career service commitments are common among a narrower portion of the national population.
Despite the findings of the current systematic review, notable gaps remain in our understanding of OA in tactical-athlete populations. Foremost, we were unable to find any data on the incidence or prevalence of OA in tactical athletes other than military service members and firefighters, and even the data in these populations are limited. No information seemed to be available on the incidence or prevalence of OA in law enforcement, first responder, or other tactical-athlete populations. Furthermore, outside the military, limited information exists on occupational disability due to OA in tactical athletes. As noted previously, the role of acute traumatic joint injury in the initiation and progression of OA in tactical-athlete populations is still poorly understood; however, examining the factors that contribute to the initiation and progression of posttraumatic OA in this population appears be warranted.22 Furthermore, OA studies in tactical athletes have primarily focused on the knee, hip, and spine, but few data are available on OA incidence or prevalence in other joints. This is an important gap, particularly when considering the high rates of joint injury to the ankle16 and shoulder18 observed in tactical-athlete populations. We know that acute traumatic joint injury—repetitive bending, squatting, kneeling, and lifting—and excessive joint loading are risk factors for OA and that tactical athletes are regularly exposed to these risk factors, but we still have a poor understanding of how these factors interact in relation to the initiation and progression of OA in tactical athletes.
Important limitations related to the interpretation of findings from this systematic review should be noted. None of the studies that we reviewed were conducted prospectively, and quality scores for all studies reviewed ranged from a low of 3 to a high of 7 on the 9-point NOS. High-quality prospective cohort studies are the best way to identify risk factors for OA within tactical-athlete populations. These studies are needed to better understand the modifiable and nonmodifiable risk factors for OA in tactical athletes so that effective prevention strategies can be developed and implemented. Despite this limitation, authors of some of the studies we reviewed were able to assess the incidence of OA as an outcome in comparison with a previous review in athletes from which only prevalence data were available.34 Tactical athletes may be more physically active than the general population, and this may influence OA risk for some activities, which could not be controlled in the current review.34 Finally, despite the observed differences in OA incidence and prevalence between tactical athletes and nonexposed controls from the general population, we still do not know which specific occupational factors or combination of factors are contributing to the observed disparity.
Even with these limitations in the literature, we consistently observed that specific subgroups of tactical athletes (eg, firefighters, active-duty military, veteran parachutists) were at elevated risk for various types of OA. However, important gaps still exist in our understanding of the risk factors that contribute to the increased OA risk among tactical athletes. Furthermore, data on the incidence and prevalence of OA in some tactical-athlete populations (eg, law enforcement, first responders) are not currently available. Research examining the risk of OA in these tactical-athlete populations is needed. The influence of mandatory national military service on the prevalence of OA also remains unclear. It is important to appreciate that tactical-athlete populations are at high risk for OA, which is a chronic disease that can impair physical function, lead to occupational disability and early retirement, and reduce quality of life. It is also critical to identify modifiable risk factors within this high-risk population in order to develop and implement effective risk-reduction strategies.
REFERENCES
- 1. Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: part II. Arthritis Rheum. 2008; 58 1: 26– 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Richmond SA, Fukuchi RK, Ezzat A, Schneider K, Schneider G, Emery CA. . Are joint injury, sport activity, physical activity, obesity, or occupational activities predictors for osteoarthritis? A systematic review. J Orthop Sports Phys Ther. 2013; 43 8: 515– B19. [DOI] [PubMed] [Google Scholar]
- 3. Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM. . Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum. 1995; 38 8: 1134– 1141. [DOI] [PubMed] [Google Scholar]
- 4. Lohmander LS, Englund PM, Dahl LL, Roos EM. . The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007; 35 10: 1756– 1769. [DOI] [PubMed] [Google Scholar]
- 5. Lohmander LS, Ostenberg A, Englund M, Roos H. . High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004; 50 10: 3145– 3152. [DOI] [PubMed] [Google Scholar]
- 6. Seidler A, Bolm-Audorff U, Abolmaali N, Elsner G. . The role of cumulative physical work load in symptomatic knee osteoarthritis—a case-control study in Germany. J Occup Med Toxicol. 2008; 3: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Felson DT. . Obesity and vocational and avocational overload of the joint as risk factors for osteoarthritis. J Rheumatol Suppl. 2004; 70: 2– 5. [PubMed] [Google Scholar]
- 8. Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000; 133 8: 635– 646. [DOI] [PubMed] [Google Scholar]
- 9. Felson DT, Hannan MT, Naimark A, et al. Occupational physical demands, knee bending, and knee osteoarthritis: results from the Framingham Study. J Rheumatol. 1991; 18 10: 1587– 1592. [PubMed] [Google Scholar]
- 10. Felson DT, Zhang Y. . An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum. 1998; 41 8: 1343– 1355. [DOI] [PubMed] [Google Scholar]
- 11. Felson DT. . Risk factors for osteoarthritis: understanding joint vulnerability. Clin Orthop Relat Res. 2004; suppl 427: S16– S21. [DOI] [PubMed] [Google Scholar]
- 12. Issa SN, Sharma L. . Epidemiology of osteoarthritis: an update. Curr Rheumatol Rep. 2006; 8 1: 7– 15. [DOI] [PubMed] [Google Scholar]
- 13. Englund M, Lohmander LS. . Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004; 50 9: 2811– 2819. [DOI] [PubMed] [Google Scholar]
- 14. Vos T, Flaxman AD, Naghavi ML, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380 9859: 2163– 2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cameron KL, Owens BD. . The burden and management of sports-related musculoskeletal injuries and conditions within the US military. Clin Sports Med. 2014; 33 4: 573– 589. [DOI] [PubMed] [Google Scholar]
- 16. Cameron KL, Owens BD, DeBerardino TM. . Incidence of ankle sprains among active-duty members of the United States Armed Services from 1998 through 2006. J Athl Train. 2010; 45 1: 29– 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jones JC, Burks R, Owens BD, et al. Incidence and risk factors associated with meniscal injuries among active-duty US military service members. J Athl Train. 2012; 47 1: 67– 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Owens BD, Dawson L, Burks R, Cameron KL. . Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am. 2009; 91 4: 791– 796. [DOI] [PubMed] [Google Scholar]
- 19. Owens BD, Mountcastle SB, Dunn WR, DeBerardino TM, Taylor DC. . Incidence of anterior cruciate ligament injury among active duty U.S. military servicemen and servicewomen. Mil Med. 2007; 172 1: 90– 91. [DOI] [PubMed] [Google Scholar]
- 20. Hootman JM, Driban JB, Sitler MR, Harris KA, Cattano NM. . Reliability and validity of three quality rating instruments for systematic reviews of observational studies. Res Synth Methods. 2011; 2 2: 110– 118. [DOI] [PubMed] [Google Scholar]
- 21. Vingard E, Alfredsson L, Goldie I, Hogstedt C. . Occupation and osteoarthrosis of the hip and knee: a register-based cohort study. Int J Epidemiol. 1991; 20 4: 1025– 1031. [DOI] [PubMed] [Google Scholar]
- 22. Cameron KL, Hsiao MS, Owens BD, Burks R, Svoboda SJ. . Incidence of physician diagnosed osteoarthritis among active duty United States military service members. Arthritis Rheum. 2011; 63 10: 2974– 2982. [DOI] [PubMed] [Google Scholar]
- 23. Scher DL, Belmont PJ Jr, Mountcastle S, Owens BD. . The incidence of primary hip osteoarthritis in active duty US military service members. Arthritis Rheum. 2009; 61 4: 468– 475. [DOI] [PubMed] [Google Scholar]
- 24. Murray-Leslie CF, Lintott DJ, Wright V. . The knee and ankles in sport and veteran military parachutists. Ann Rheum Dis. 1977; 36 4: 327– 331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Murray-Leslie CF, Lintott DJ, Wright V. . The spine in sport and veteran military parachutists. Ann Rheum Dis. 1977; 36 4: 332– 342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Aydog ST, Turbedar E, Demirel AH, Tetik O, Akin A, Doral MN. . Cervical and lumbar spinal changes diagnosed in four-view radiographs of 732 military pilots. Aviat Space Environ Med. 2004; 75 2: 154– 157. [PubMed] [Google Scholar]
- 27. Kujala UM, Kaprio J, Sarna S. . Osteoarthritis of weight bearing joints of lower limbs in former elite male athletes. BMJ. 1994; 308 6923: 231– 234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kujala UM, Sarna S, Kaprio J, Koskenvuo M, Karjalainen J. . Heart attacks and lower-limb function in master endurance athletes. Med Sci Sports Exerc. 1999; 31 7: 1041– 1046. [DOI] [PubMed] [Google Scholar]
- 29. Kettunen JA, Kujala UM, Kaprio J, Sarna S. . Health of master track and field athletes: a 16-year follow-up study. Clin J Sport Med. 2006; 16 2: 142– 148. [DOI] [PubMed] [Google Scholar]
- 30. Kettunen JA, Kujala UM, Kaprio J, Koskenvuo M, Sarna S. . Lower-limb function among former elite male athletes. Am J Sports Med. 2001; 29 1: 2– 8. [DOI] [PubMed] [Google Scholar]
- 31. Sarna S, Kaprio J, Kujala UM, Koskenvuo M. . Health status of former elite athletes. The Finnish experience. Aging (Milano). 1997; 9 1–2: 35– 41. [DOI] [PubMed] [Google Scholar]
- 32. Iosifidis MI, Tsarouhas A, Fylaktou A. . Lower limb clinical and radiographic osteoarthritis in former elite male athletes. Knee Surg Sports Traumatol Arthrosc. 2015; 23 9: 2528– 2535. [DOI] [PubMed] [Google Scholar]
- 33. Chinn S. . A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000; 19 22: 3127– 3131. [DOI] [PubMed] [Google Scholar]
- 34. Driban JB, Hootman JM, Sitler MR, Harris K, Cattano NM. . Is participation in certain sports associated with knee osteoarthritis? A systematic review. J Athl Train. 2016. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kopec JA, Rahman MM, Berthelot JM, et al. Descriptive epidemiology of osteoarthritis in British Columbia, Canada. J Rheumatol. 2007; 34 2: 386– 393. [PubMed] [Google Scholar]
- 36. Kopec JA, Rahman MM, Sayre EC, et al. Trends in physician-diagnosed osteoarthritis incidence in an administrative database in British Columbia, Canada, 1996–1997 through 2003–2004. Arthritis Rheum. 2008; 59 7: 929– 934. [DOI] [PubMed] [Google Scholar]
- 37. Patzkowski JC, Rivera JC, Ficke JR, Wenke JC. . The changing face of disability in the US Army: the Operation Enduring Freedom and Operation Iraqi Freedom effect. J Am Acad Orthop Surg. 2012; 20 suppl 1: S23– S30. [DOI] [PubMed] [Google Scholar]
- 38. Amoroso PJ, Canham ML. . Chapter 4. Disabilities related to the musculoskeletal system: Physical Evaluation Board data. Mil Med. 1999; 164 suppl 8: 1– 73. [PubMed] [Google Scholar]
- 39. Hsiao M, Owens BD, Burks R, Sturdivant RX, Cameron KL. . Incidence of acute traumatic patellar dislocation among active-duty United States military service members. Am J Sports Med. 2010; 38 10: 1997– 2004. [DOI] [PubMed] [Google Scholar]
- 40. Roos H, Adalberth T, Dahlberg L, Lohmander LS. . Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthritis Cartilage. 1995; 3 4: 261– 267. [DOI] [PubMed] [Google Scholar]
- 41. Wilder FV, Hall BJ, Barrett JP Jr, Lemrow NB. . History of acute knee injury and osteoarthritis of the knee: a prospective epidemiological assessment. The Clearwater Osteoarthritis Study. Osteoarthritis Cartilage. 2002; 10 8: 611– 616. [DOI] [PubMed] [Google Scholar]
- 42. Brown TD, Johnston RC, Saltzman CL, Marsh JL, Buckwalter JA. . Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006; 20 10: 739– 744. [DOI] [PubMed] [Google Scholar]
- 43. Songer TJ, LaPorte RE. . Disabilities due to injury in the military. Am J Prev Med. 2000; 18 suppl 3: 33– 40. [DOI] [PubMed] [Google Scholar]
- 44. Dunn WR, Lincoln AE, Hinton RY, Smith GS, Amoroso PJ. . Occupational disability after hospitalization for the treatment of an injury of the anterior cruciate ligament. J Bone Joint Surg Am. 2003; 85 9: 1656– 1666. [DOI] [PubMed] [Google Scholar]
- 45. Sulsky SI, Mundt KA, Bigelow C, Amoroso PJ. . Case-control study of discharge from the US Army for disabling occupational knee injury: the role of gender, race/ethnicity, and age. Am J Prev Med. 2000; 18 suppl 3: 103– 111. [DOI] [PubMed] [Google Scholar]
- 46. Sulsky SI, Mundt KA, Bigelow C, Amoroso PJ. . Risk factors for occupational knee related disability among enlisted women in the US Army. Occup Environ Med. 2002; 59 9: 601– 607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cross JD, Ficke JR, Hsu JR, Masini BD, Wenke JC. . Battlefield orthopaedic injuries cause the majority of long-term disabilities. J Am Acad Orthop Surg. 2011; 19 suppl 1: S1– S7. [DOI] [PubMed] [Google Scholar]
- 48. Rivera JC, Wenke JC, Buckwalter JA, Ficke JR, Johnson AE. . Posttraumatic osteoarthritis caused by battlefield injuries: the primary source of disability in warriors. J Am Acad Orthop Surg. 2012; 20 suppl 1: S64– S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rubertone MV, Brundage JF. . The Defense Medical Surveillance System and the Department of Defense serum repository: glimpses of the future of public health surveillance. Am J Public Health. 2002; 92 12: 1900– 1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sugimoto D, Myer GD, Foss KD, Hewett TE. . Specific exercise effects of preventive neuromuscular training intervention on anterior cruciate ligament injury risk reduction in young females: meta-analysis and subgroup analysis. Br J Sports Med. 2014; 49 5: 282– 289. [DOI] [PubMed] [Google Scholar]
- 51. Pappas E, Nightingale EJ, Simic M, Ford KR, Hewett TE, Myer GD. . Do exercises used in injury prevention programmes modify cutting task biomechanics? A systematic review with meta-analysis. Br J Sports Med. 2015; 49 10: 673– 680. [DOI] [PubMed] [Google Scholar]
- 52. Carow S, Haniuk E, Cameron K, et al. Risk of lower extremity injury in a military cadet population after a supervised injury-prevention program. J Athl Train. 2016. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Coggon D, Croft P, Kellingray S, Barrett D, McLaren M, Cooper C. . Occupational physical activities and osteoarthritis of the knee. Arthritis Rheum. 2000; 43 7: 1443– 1449. [DOI] [PubMed] [Google Scholar]
- 54. Jensen LK, Mikkelsen S, Loft IP, Eenberg W, Bergmann I, Logager V. . Radiographic knee osteoarthritis in floorlayers and carpenters. Scand J Work Environ Health. 2000; 26 3: 257– 262. [DOI] [PubMed] [Google Scholar]
- 55. Sandmark H, Hogstedt C, Vingard E. . Primary osteoarthrosis of the knee in men and women as a result of lifelong physical load from work. Scand J Work Environ Health. 2000; 26 1: 20– 25. [DOI] [PubMed] [Google Scholar]
- 56. Lau EC, Cooper C, Lam D, Chan VN, Tsang KK, Sham A. . Factors associated with osteoarthritis of the hip and knee in Hong Kong Chinese: obesity, joint injury, and occupational activities. Am J Epidemiol. 2000; 152 9: 855– 862. [DOI] [PubMed] [Google Scholar]
- 57. Allen KD, Chen JC, Callahan LF, et al. Associations of occupational tasks with knee and hip osteoarthritis: the Johnston County Osteoarthritis Project. J Rheumatol. 2010; 37 4: 842– 850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Coggon D, Kellingray S, Inskip H, Croft P, Campbell L, Cooper C. . Osteoarthritis of the hip and occupational lifting. Am J Epidemiol. 1998; 147 6: 523– 528. [DOI] [PubMed] [Google Scholar]
- 59. Yoshimura N, Sasaki S, Iwasaki K, et al. Occupational lifting is associated with hip osteoarthritis: a Japanese case-control study. J Rheumatol. 2000; 27 2: 434– 440. [PubMed] [Google Scholar]
- 60. US Army Center for Army Lessons Learned. Task Force Devil Combined Arms Assessment Team (DevilCAAT). The Modern Warrior's Combat Load: Dismounted Operations in Afghanistan. Arlington, VA: Department of Defense; 2003: 1– 115. [Google Scholar]
- 61. Central Intelligence Agency. The World Factbook2014–2015. Washington, DC: Central Intelligence Agency; 2014. [Google Scholar]