Abstract
Acute iron intoxication (FeI) in humans has not been adequately studied. The manifestation of FeI, defined as a serum iron concentration >300 μg/dL (55 μmol/L) within 12 hours of ingestion, include various symptoms appearing in progressive stages. Systemic toxicity is expected with an intake of 60 mg/kg. A 27-year-old female nurse presented with unintended acute intravenous iron intoxication (FeI) a week after self-injecting herself with 20 ampoules of IV iron (4,000 mg elemental iron, 60 mg/kg). She had stable vital signs and mild hepatic tenderness. Hepatic MRI (Ferriscan®) showed a moderate/severe liver iron content (LIC: 9 mg/g dry tissue). Her hemogram, electrolytes, hepatic and renal functions were normal. Based on the high dose of iron received and her elevated LIC, chelation therapy was advised. She accepted only oral therapy and was started on deferasirox at a dose of 30 mg/kg daily. This oral chelation proved to be effective in clearing her hepatic iron overload after six months (LIC: 2 mg/g dry tissue), without side effects. This case also proved the value of Ferriscan® in diagnosing the degree of hepatic FeI and monitoring therapy to achieve a safe level of LIC.
Keywords: Iron, acute iron intoxication, Ferriscan, liver iron content (LIC), oral iron chelation, deferasirox
Introduction
Poisoning from medications can happen for a variety of reasons, including intentional overdose, inadvertently taking an extra dose, dispensing or measuring errors, and exposure through breast milk. Iron poisoning is more commonly seen in children than in adults.1
Iron poisoning is primarily a clinical diagnosis. A combination of history, physical examination, and laboratory features can identify patients at risk for systemic toxicity.2–5 The purpose of the laboratory evaluation is to confirm the diagnosis of iron poisoning and to monitor for clinical effects. Measurement of serum iron concentration (SIC) is useful for establishing the diagnosis. A serum iron level of more than 350 μg/dl between 2 and 6 h post-ingestion is supposed to indicate a significant intoxication and levels more than 500 μg/dl suggest grave danger of acute liver failure.3,4
However, SIC cannot always be correlated with the severity or the clinical phase of iron intoxication because it measures free iron circulating in the blood and not the intracellular iron that causes systemic toxicity. The primary mechanism for iron-induced tissue damage is free radical production and lipid peroxidation.4
The generation of reactive oxygen species (ROS) secondary to iron intoxication is because, as a transition metal, iron is a key participant in both the Fenton and Haber–Weiss reactions, resulting in the creation of hydroxyl radicals. As physiologic defenses for the detoxification of ROS become overwhelmed, ROS causes a direct cellular damage such as lipid membrane destruction (via hydroxyl radical-initiated lipid peroxidation). The organ systems most affected include the gastrointestinal tract, liver, vessels, and occasionally pulmonary damage, renal damage and pancreatic necrosis.4–6
In 2005, a review of 70 patients with iron toxicity showed hepatotoxicity in 13 patients with severe toxicity (serum alanine transaminase >1,000 U/L) in nine patients. Ten of these patients (all <18 years) died with one of them requiring liver transplantation. 7–11
We report a young female adult with an acute unintended intravenous injection of iron that lead to iron intoxication (60 mg/kg of elemental iron). Because patient refused parenteral deferoxamine (DFO, Desferal ®) therapy, oral deferasirox (Exjade ®) was used as an iron chelator.
Deferasirox (Exjade®)is the first approved oral iron chelator in the USA. It is selective for iron (as Fe3+). It is a tridentate ligand that binds iron with high affinity in a 2:1 ratio. Its primary use is to reduce chronic iron overload in patients who are receiving long-term blood transfusions for conditions such as β-thalassemia.
It was approved by the United States Food and Drug Administration (FDA) in November 2005. According to FDA (May 2007), renal failure and cytopenias have been reported in patients receiving deferasirox oral suspension tablets. It is approved in the European Union by the European Medicines Agency (EMA) for children six years and older for chronic iron overload from repeated blood transfusions.12 FerriScan®, a non-invasive magnetic resonance imaging (MRI) method for measuring the degree of body iron burden through quantification of liver iron concentration (LIC), is used for quantifying and monitoring hepatic (tissue) iron overload.13
Case Report
A 27-year-old female nurse self-referred to hematology clinic for an unintended exposure of 20 ampoules of a preparation containing iron, given intravenously (IV), over a period of 20 days for iron deficiency anemia (Hb 9 g/dl, low hematocrit and low serum iron). Each ampoule contained 200 mg of elemental iron, (4,000 mg elemental iron, 60 mg/kg body weight).
Referred symptoms at the admission included mild abdominal pain a week after the last injection. The clinical examination was not remarkable apart from mild hepatic tenderness. Serum iron concentration, ferritin, electrolytes, blood urea nitrogen (BUN), glucose, alanine and aspartate aminotransferases, albumin, prothrombin time (PT), arterial blood gasses and complete blood count with differential were urgently requested.
Markers of iron overload and hepatic MRI (Ferriscan ®) showed a severe iron overload (Table 1 and Figure 1). Serum iron and ferritin concentrations were 200 μmol/l and 1473 μg/l respectively. Therefore, she was advised to be treated with parenteral deferoxamine (DFO, Desferal ®). Her CBC serum electrolytes, liver and renal functions were all normal. The treatment with DFO was refused and a novel oral iron chelator, mainly used in patients with transfusion-dependent β-thalassemia, was recommended (deferasirox, Exjade ®) at the dose of 30 mg/kg daily. The duration of treatment was advised taking into consideration the patient’s clinical status, the serum iron concentration and the LIC levels. The mild symptoms previously reported by the patients disappeared after 4 weeks of treatment. The iron chelation therapy with deferasirox was stopped after 6 months. Despite LIC normalization, serum ferritin levels remained above the normal levels (1,000 μg/l; normal levels in females: 18–160 μg/L). A periodic 3 months’ reassessment of serum ferritin was advised.
Table 1.
Hemoglobin, liver enzymes and markers of iron overload before and after 6 months of therapy with deferasirox
| Before | After 6 months | |
|---|---|---|
| Hemoglobin | 12 g/dl | 12.5 g/dl |
| Serum iron | 200 μmol/l | 30 μmol/l |
| Serum ferritin | 1473 μg/l | 1000 μg/l |
| Total Iron Binding Capacity (TIBC) | 42 μmol/l | 44 μmol/l |
| Alanine transaminase (ALT) | 19 U/L | 17 U/L |
| Aspartate transaminase (AST) | 13 U/L | 11U/L |
| Serum albumin | 41g/L | 40.5 g/L |
| Prothrombin time (PT) | 11 seconds | 11.5 seconds |
| Liver iron concentration | 9 mg/g dry tissue | 2 mg/g dry tissue |
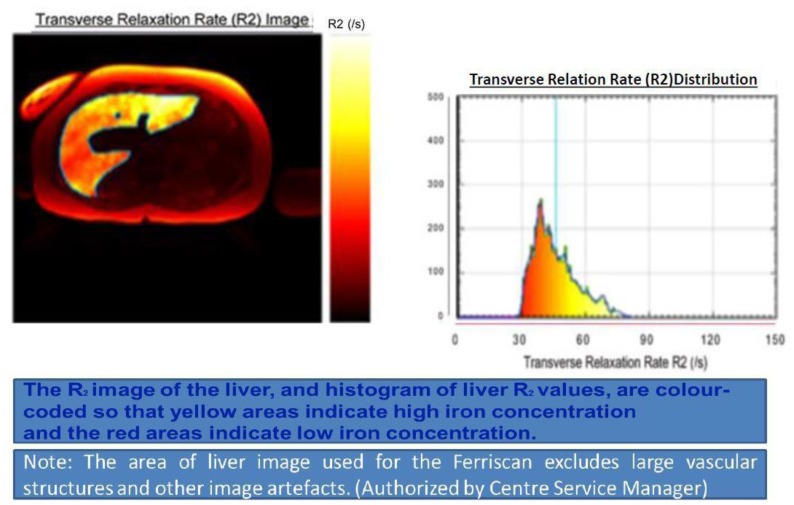
Figure 1.
Ferriscan in our patient at the first evaluation.
Discussion
The 2014 Annual Report of the American Association of Poison Control Centers’ (AAPCC) National Poison Data System reported 4024 single exposures to iron or iron salts, with one major outcome and one death. Overall, 75% of cases were in children younger than 6 years.1
Iron is an essential element for normal cell metabolism, but in excess quantities iron is highly cytotoxic and even lethal. Children may show signs of toxicity with ingestions of 10–20 mg/kg of elemental iron. Ingestions between 20 and 60 mg/kg of elemental iron can develop mild to moderate clinical signs of iron intoxication, necessitating treatment or monitoring. Serious toxicity is likely with ingestions of more than 60 mg/kg and can result in serious poisoning or death.4–7
Manifestation of acute iron poisoning, defined as a serum iron concentration >300 μg/dL (55 μmol/L) within 12 hours of ingestion. Early signs, presenting within the first 6 hours, include abdominal pain, vomiting, diarrhoea and gastrointestinal bleeding. In the stage of stabilisation (12 hours post-ingestion), absorbed iron is rapidly cleared from the circulation by cellular uptake, and then affects mitochondrial function. Mitochondrial toxicity evokes signs of shock, acidosis, coagulopathy, hyper- or hypoglycaemia, and acute tubular necrosis. Once a critical amount of iron has reached the mitochondria, therapy has little effect and outcome is poor. Subsequently, within 48 hours acute liver failure predominates.7,8
Hepatotoxicity usually is observed at serum iron levels higher than 500 μg/dL and patients with serum iron levels higher than 1000 μg/dL may need intensive care.9 Two to 3 days post-ingestion, iron is absorbed by Kupffer cells and hepatocytes, exceeding the storage capacity of ferritin and causing oxidative damage. Pathologic changes include cloudy swelling, peri-portal hepatic necrosis, and elevated transaminase levels. This may result in hepatic failure. Intravenous iron leads to preferential involvement of the reticuloendothelial system of liver, spleen, bone marrow, and lymph nodes. After saturation, the iron accumulates in hepatocytes and in parenchymal cells of the pancreas, myocardium, and endocrine glands.10
Diagnosis of acute iron poisoning is based on clinical symptoms, elevated serum iron level and appearance of “vin rose” urine in deferoxamine test.11 For serum iron measurement, samples should be drawn at least 4 hours post-ingestion, to allow levels to reach steady state; however, levels drawn more than 6 hours after ingestion may underestimate toxicity because of ferritin binding and redistribution of iron.
Our patient came to our observation late (7 days after the last dose of iron). Acute intoxication manifestations did not occur probably due to the administration of iron doses over an extended period.11 However, it is possible that prompt iron chelation in our case had prevented the cumulative pathological effects of acute and subacute severe iron intoxication on the liver.
Liver iron concentration provides the best measure of total body iron stores and is a validated predictor of the risks a patient faces from the complications of iron toxicity. Currents methods for quantifying hepatic iron include biopsy, imaging, spectroscopy, and susceptometry. Biopsy is an invasive procedure that carries a significant risk of complications. In addition, biopsy specimens is subject to sampling error due to non-uniformity in the distribution of liver iron.14
Several imaging non-invasive techniques are available for measuring LIC. There are different validated MRI methods for quantitating the liver iron burden., the most widely relaxometry methods used include: the FerriScan® (T2/R2 based) and T2*/R2* based methods: the FerriScan® and T2 methods. The noninvasive FerriScan® is highly sensitive and specific for estimating LIC and is approved by the Food and Drug Administration for routine clinical use. However, it is usually not used to diagnose and monitor LIC in cases of acute iron intoxication.14–15
In our case, significantly increased LIC was documented despite moderately elevated serum iron and ferritin and normal TIBC. This indicates a weak reliability of biochemical parameters and the superiority of using this non-invasive method if the patient presents late during iron toxicity. In support of this finding, family studies on patients with idiopathic haemochromatosis suggested that the serum ferritin concentration was not a reliable index of hepatic iron overload and that a rise in serum ferritin levels occurred only when liver damage was present. An analysis of ferritin levels, estimated transfusion iron overload (TIL) in patients who received simple transfusions prior to the start of chelation therapy), and LIC (liver biopsy specimens) done on children enrolled in two trials for stroke prevention showed serum ferritin changes that were non-linear compared to TIL or LIC. Of note, serum ferritin rose rapidly with transfusion initially, then slowed after reaching 1,500–2,500 ng/ml, despite evidence of increasing iron load. Serum ferritin levels greater than 3,000 ng/ml were associated with both increased LIC and liver injury, as estimated by ALT levels. However, because of the non-linear association between serum ferritin level and LIC, authors recommended using more accurate methods for assessing iron levels in those with levels between 1,500 and 3,000 ng/ml.16–18
The goals of pharmacotherapy are to reduce iron levels, prevent complications, and reduce morbidity. DFO is used for chelation of iron in both acute and chronic toxicity. Approximately 8 mg of iron is bound by 100 mg of deferoxamine. DFO is a chelating agent that, in acute iron intoxication, binds with ferric iron (Fe3+) in the blood to form water-soluble ferrioxamine that is then excreted by the kidneys. Ferrioxamine gives urine the classical orange to reddish brown color. DFO must be administered early in the treatment of iron overdose because iron moves rapidly from the circulation into cells, where, in acute intoxication, it is not readily accessible for chelation.11,19
Patients who are symptomatic should receive DFO regardless of their iron level. Indications of potential serious toxicity include the following: ingestion of greater than 60 mg/kg of elemental iron; peak of serum iron concentration greater than 500 μg/dL (90 μmol/L); persistent serious symptoms such as vomiting, diarrhea, and/or altered mental status; presence of systemic symptoms, including subtle symptoms that can be seen in the latent phase of iron intoxication, such as tachycardia, hypotension, poor peripheral tissue perfusion, and/or tachypnea.18,20 In acute iron poisoning, intramuscular (IM) administration of deferoxamine is indicated for patients who are not in shock; intravenous (IV) administration should be reserved for patients in a state of cardiovascular collapse or shock. Nevertheless, there is a lack of knowledge about its optimal use.
Other chelator therapies are still experimental. In 2005, the Food and Drug Administration approved deferasirox as an oral iron chelating agent for chronic iron overload due to blood transfusions in patients 2 year of age and older; it is also approved for treatment of chronic iron overload resulting from non–transfusion-dependent thalassemia. Efficacy of orally administered iron chelator deferiprone in acute iron poisoning is still under investigation.
Berkovitch M et al.19 reported that co-administration of 800 mg/kg deferiprone with LD50 dose of iron decreased morbidity and mortality caused by acute iron overdose. Histologically, there was a dose-dependent decrease in iron accumulation in the gastrointestinal tract. These findings in animals hold promise for its use in humans.
To determine the usefulness in management of acute iron ingestion, Griffith et al.20 studied the effect of orally administered deferasirox in 8 healthy human adults. Subjects ingested 5 mg/kg of elemental iron in the form of ferrous sulfate. One hour after iron ingestion, subjects were randomized to receive 20 mg/kg of deferasirox or placebo. Deferasirox significantly reduced serum iron levels when administered 1 hour after iron ingestion during the 12- and 24-hour periods after acute ingestion.
Uncommon serious side effects that may occur with deferasirox use include acute renal failure and hepatic injury. Measuring and monitoring serum creatinine and creatinine clearance and serum transaminases and bilirubin in all patients prior to initiating treatment, and at least monthly thereafter is recommended.
Conclusions
This case demonstrates the efficacy of oral iron chelation therapy in patients with mild to moderate clinical signs of iron intoxication with normal renal and hepatic functions and the usefulness of Ferriscan® to assess liver iron overload and to monitor the effect of chelation therapy. It appears that LIC of patients with acute iron intoxication can be accurately diagnosed and monitored by Ferriscan.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Mowry JB, Spyker DA, Brooks DE, McMillan N, Schauben JL. 2014 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd Annual Report. Clin Toxicol (Phila) 2015;53:962–1147. doi: 10.3109/15563650.2015.1102927. https://doi.org/10.3109/15563650.2015.1102927. [DOI] [PubMed] [Google Scholar]
- 2.Erickson TB, Thompson TM, Lu JJ. The approach to the patient with an unknown overdose. Emerg Med Clin North Am. 2007;25:249–81. doi: 10.1016/j.emc.2007.02.004. https://doi.org/10.1016/j.emc.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Velez L, Delaney K. Heavy metals. In: Marx J, Hockberger R, Walls R, editors. Emergency Medicine: Concepts and Clinical Practice. 5th edition. Mosby; St. Louis: 2006. p. 2418. [Google Scholar]
- 4.Tenenbein M. Toxicokinetics and toxicodynamics of iron poisoning. Toxicol Lett. 1998;28:102–3. doi: 10.1016/s0378-4274(98)00279-3. [DOI] [PubMed] [Google Scholar]
- 5.Mills KC, Curry SC. Acute iron poisoning. Emerg Med Clin North Am. 1994;12:397–413. [PubMed] [Google Scholar]
- 6.Link G, Saada A, Pinson A, Konijn AM, Hershko C. Mitochondrial respiratory enzymes are a major target of iron toxicity in rat heart cells. J Lab Clin Med. 1998;131:466–74. doi: 10.1016/s0022-2143(98)90148-2. https://doi.org/10.1016/S0022-2143(98)90148-2. [DOI] [PubMed] [Google Scholar]
- 7.Manoguerra AS, Erdman AR, Booze LL, Christianson G, Wax PM, Scharman EJ, Woolf AD, Chyka PA, Keyes DC, Olson KR, Caravati EM, Troutman WG. Iron ingestion: an evidenced-based consensus guideline for out-of-hospital management. Clin Toxicol. 2005;43:553–70. doi: 10.1081/clt-200068842. https://doi.org/10.1081/CLT-200068842. [DOI] [PubMed] [Google Scholar]
- 8.Lawrence DT, Bechtel L, Walsh JP, Holstege CD. The evaluation and management of acute poisoning emergencies. Minerva Med. 2007;98:543–68. [PubMed] [Google Scholar]
- 9.Robertson A, Tenenbein M. Hepatotoxicity in acute iron poisoning. Hum Exp Toxicol. 2005;24:559–62. doi: 10.1191/0960327105ht564oa. https://doi.org/10.1191/0960327105ht564oa. [DOI] [PubMed] [Google Scholar]
- 10.Siegelman ES, Mitchell DG, Semelka RC. Abdominal iron deposition: metabolism, MR findings, and clinical importance. Radiology. 1996;199:13–22. doi: 10.1148/radiology.199.1.8633135. https://doi.org/10.1148/radiology.199.1.8633135. [DOI] [PubMed] [Google Scholar]
- 11.Baranwal AK, Singhi SC. Acute iron poisoning: management guidelines. Indian Pediatr. 2003;40:534–40. [PubMed] [Google Scholar]
- 12.Kontoghiorghe CN, Kontoghiorghes GJ. Efficacy and safety of iron-chelation therapy with deferoxamine, deferiprone, and deferasirox for the treatment of iron-loaded patients with non-transfusion-dependent thalassemia syndromes. Drug Des Devel Ther. 2016;10:465–81. doi: 10.2147/DDDT.S79458. https://doi.org/10.2147/DDDT.S79458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sirlin CB, Reeder SB. Magnetic Resonance Imaging Quantification of Liver Iron. Magn Reson Imaging Clin N Am. 2010;18:359–81. doi: 10.1016/j.mric.2010.08.014. https://doi.org/10.1016/j.mric.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.St Pierre TG, El-Beshlawy A, Elalfy M, Al Jefri A, Al Zir K, Daar S, Habr D, Kriemler-Krahn U, Taher A. Multicenter validation of spin-density projection-assisted R2-MRI for the noninvasive measurement of liver iron concentration. Magn Reson Med. 2014;71:2215–2223. doi: 10.1002/mrm.24854. https://doi.org/10.1002/mrm.24854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garbowski MW, Carpenter JP, Smith G, Roughton M, Alam MH, He T, Pennell DJ, Porter JB. Biopsy-based calibration of T2* magnetic resonance for estimation of liver iron concentration and comparison with R2 Ferriscan. J Cardiovasc Magn Reson. 2014 Jun 10;16:40. doi: 10.1186/1532-429X-16-40. https://doi.org/10.1186/1532-429X-16-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feller ER, Pont A, Wands JR, Carter EA, Foster G, Kourides IA, Isselbacher KJ. Familial hemochromatosis. Physiologic studies in the precirrhotic stage of the disease. N Engl J Med. 1977;296:1422–6. doi: 10.1056/NEJM197706232962501. https://doi.org/10.1056/NEJM197706232962501. [DOI] [PubMed] [Google Scholar]
- 17.Adamkiewicz TV1, Abboud MR, Paley C, Olivieri N, Kirby-Allen M, Vichinsky E, Casella JF, Alvarez OA, Barredo JC, Lee MT, Iyer RV, Kutlar A, McKie KM, McKie V, Odo N, Gee B, Kwiatkowski JL, Woods GM, Coates T, Wang W, Adams RJ. Serum ferritin level changes in children with sickle cell disease on chronic blood transfusion are nonlinear and are associated with iron load and liver injury. Blood. 2009;114:4632–8. doi: 10.1182/blood-2009-02-203323. https://doi.org/10.1182/blood-2009-02-203323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tenenbein M. Benefits of parenteral deferoxamine for acute iron poisoning. J Toxicol Clin Toxicol. 1996;34:485–489. doi: 10.3109/15563659609028005. https://doi.org/10.3109/15563659609028005. [DOI] [PubMed] [Google Scholar]
- 19.Berkovitch M, Livne A, Lushkov G, Segal M, Talmor C, Bentur Y, Klein J, Koren G. The efficacy of oral deferiprone in acute iron poisoning. Am J Emerg Med. 2000;18:36–40. doi: 10.1016/s0735-6757(00)90045-7. https://doi.org/10.1016/S0735-6757(00)90045-7. [DOI] [PubMed] [Google Scholar]
- 20.Griffith EA, Fallgatter KC, Tantama SS, Tanen DA, Matteucci MJ. Effect of deferasirox on iron absorption in a randomized, placebo-controlled, crossover study in a human model of acute supratherapeutic iron ingestion. Ann Emerg Med. 2011;58:69–73. doi: 10.1016/j.annemergmed.2010.11.020. https://doi.org/10.1016/j.annemergmed.2010.11.020. [DOI] [PubMed] [Google Scholar]