Abstract
Aim: To investigate whether body adiposity index (BAI; hip/height1.5–18), pediatric BAI (BAIp; hip/height0.8–38), and other hip/heightP ratios are useful in obese children.
Method: Ninety obese Japanese children, 55 boys and 35 girls, who visited our University Clinic, were enrolled. The age was 9.92 ± 2.6 (mean ± SD) years, and the percentage overweight (POW) was 51.6 ± 18.8%. We set the power value of the hip/heightP 0, 0.5, 0.8, 1, 1.5, and 2 and studied the association with overweight indices, biochemical data, and fat area measured by computed tomography. Waist, waist/height ratio, and waist/hip ratio were also evaluated.
Results: Hip/height and hip/height0.8 (BAIp) were more closely correlated with POW, body mass index percentile, and percentage body fat than hip/height1.5 (BAI). The correlation coefficient of hip/height with POW (r = 0.855) was the highest among the studied hip/heightP indices. The approximate line to predict POW was 411 × hip/height−207. The waist/height was also highly correlated with POW (r = 0.879). Hip and hip/height0.5 were more closely correlated with visceral fat area than hip/height, BAIp, and hip/height1.5. Hip and hip/height0.5 were significantly correlated with insulin. Only hip was also significantly associated with dyslipidemia. All hip/heightP indices were not significantly correlated with alanine aminotransferase (ALT). Waist was significantly correlated with serum lipids, ALT, and insulin.
Conclusion: Hip/height and BAIp are better markers for overweight (adiposity) in obese children than BAI. However, hip/height, BAIp, and BAI are not useful to predict metabolic complications. Waist appears to be the best index for obese children overall at this time.
Keywords: Body adiposity index, Overweight, Body fat, Visceral adipose tissue, Waist circumference
Introduction
The prevalence of obesity has rapidly increased since the last several decades in many countries. WHO stated that the worldwide prevalence of obesity increased to more than double between 1980 and 20141). Globally, the prevalence of childhood obesity is also still high, however, recent obesity trends in children and adolescents suggest a plateau in some countries2). Even so, childhood obesity is a major health problem because obese children are likely to remain obese as adults, and the obesity-related complications such as dyslipidemia, fatty liver, and insulin resistance are also likely to persist during adulthood. These complications lead to early atherosclerosis and diabetes mellitus. In addition, the treatment of severely obese children is not easy. To prevent obesity in middle age, early precautions and interventions are required during childhood. Therefore, it is important to find an indicator that can accurately predict the degree of both adiposity and metabolic complications in children.
In 2011, a new anthropometric indicator, body adiposity index (BAI), was proposed as a good marker for adiposity in Mexican–American and African–American adults3). BAI is calculated using the following equation: BAI=hip circumference (cm)/height (m)1.5–18. BAI was reported to be strongly correlated with body fat as measured by dual-energy X-ray absorptiometry (DEXA). However, some investigators had some questions about the usefulness of BAI in adults. For example, Schulze and Stefan described the effect of sexual dimorphism in body fatness on BAI4). In addition, it was reported that the association of cardiovascular risk factors, such as blood pressure, serum lipids, glucose, and adipocytokines, with BAI was weaker than that with waist-related indices, such as waist circumference, waist/hip ratio, waist/height ratio, and visceral adipose tissue level5–7). In obese adolescents, Thivel et al.8) reported that body mass index (BMI) was better than BAI for estimating adiposity. However, in children, it is not well known whether BAI is a useful marker. In 2013, BAI for pediatrics (BAIp): hip circumference (cm)/height (m)0.8–38 was also proposed to predict body fatness in 5–12-year-old children, and BAI was shown to overestimate the percentage of body fat measured using a bioimpedance method9). To the best of our knowledge, there are no reports in which the relationship between BAI or BAIp and obesity-related complications or abdominal adipose tissue area measured by computed tomography (CT) has been studied. Therefore, we studied hip-to-heightP ratio (hip/heightP) in obese children.
Aim
The aim of this study was to investigate which hip/heightP, including BAI and BAIp, is useful in children to predict not only adiposity but also obesity-related complications and whether the hip/heightP is better than waist-related indices.
Methods
Subjects
Ninety obese Japanese children, 55 boys and 35 girls, who visited the Clinic for Obese Children at either Showa University or Showa University Koto Toyosu Hospital, were enrolled in the study (Table 1). According to the criteria for childhood obesity adopted by the Ministry of Education, Culture, Sports, Science and Technology in Japan, a child was considered to be obese when the percentage overweight (POW) exceeded 20%. POW = 20% means that one's body weight is 120% of standard body weight, which is defined as the mean body weight corresponding to the height for that age obtained from the national statistics for Japanese school children in 200010). The age of the subjects ranged from 5 to 17 (9.92 ± 2.6; mean ± SD) years. The mean POW, BMI-for-age percentile value (BMI percentile), and BMI-for-age Z-score (BMI-SD) were 51.6 ± 18.8 (%), 97.8 ± 2.5 (percentile), and 2.24 ± 0.54 (SD), respectively. They had no endocrine, metabolic, or kidney diseases.
Table 1. Characteristics of the obese boys and girls.
| All children (n = 90) |
Boys (n = 55) |
Girls (n = 35) |
Statistics*
(B vs. G) |
||
|---|---|---|---|---|---|
| Age (year) | 9.92 ± 2.6 | 10.5 ± 2.6 | 9.10 ± 2.5 | p < 0.05 | |
| Height (cm) | 139.6 ± 14.5 | 143.1 ± 13.6 | 134.1 ± 14.5 | p < 0.01 | |
| Weight (kg) | 53.3 ± 16.5 | 57.1 ± 16.4 | 47.3 ± 15.0 | p < 0.01 | |
| POW (%) | 51.6 ± 18.8 | 52.5 ± 20.0 | 50.2 ± 16.9 | ns | |
| BMI percentile | 97.8 ± 2.5 | 97.6 ± 2.6 | 98.2 ± 2.2 | ns | |
| BMI-SD | 2.24 ± 0.54 | 2.19 ± 0.54 | 2.35 ± 0.54 | ns | |
| PBF (%) | 35.6 ± 6.0 | 35.1 ± 5.8 | 36.5 ± 6.2 | ns | |
| Waist (cm) | 82.4 ± 11.1 | 85.4 ± 11.5 | 77.7 ± 8.8 | p < 0.01 | |
| Waist/height | 0.591 ± 0.054 | 0.597 ± 0.054 | 0.581 ± 0.051 | ns | |
| Waist/hip | 0.940 ± 0.061 | 0.955 ± 0.058 | 0.916 ± 0.058 | ns | |
| Hip (cm) | 87.7 ± 10.5 | 89.4 ± 10.0 | 85.1 ± 10.8 | ns | |
| Hip/height0.5 | 7.42 ± 0.59 | 7.46 ± 0.59 | 7.34 ± 0.59 | ns | |
| Hip/height | 0.629 ± 0.040 | 0.625 ± 0.041 | 0.634 ± 0.036 | ns | |
| Hip/height1.5 (×10−2) | 5.34 ± 0.45 | 5.24 ± 0.44 | 5.50 ± 0.42 | p < 0.01 | |
| Hip/height2 (×10−3) | 4.56 ± 0.59 | 4.41 ± 0.54 | 4.79 ± 0.59 | p < 0.01 | |
| BAI | 35.4 ± 4.5 | 34.4 ± 4.4 | 37.0 ± 4.3 | p < 0.01 | |
| BAIp | 29.1 ± 4.3 | 29.1 ± 4.5 | 29.2 ± 4.1 | ns | |
| (n = 65) | (n = 42) | (n = 23) | |||
| Total AT area (cm2) | 331.8 ± 104.9 | 346.0 ± 109.3 | 305.8 ± 93.1 | ns | |
| VAT area (cm2) | 71.4 ± 27.2 | 75.5 ± 26.8 | 64.0 ± 26.8 | ns | |
| SAT area (cm2) | 260.4 ± 87.2 | 270.6 ± 93.0 | 241.8 ± 73.8 | ns | |
Data are expressed as means ± SD. BMI; body mass index, POW; percentage overweight, PBF; percentage body fat, Waist; waist circumference at the level of umbilicus, Hip; hip circumference at the maximum level, BAI; body adiposity index (hip/height1.5–18), BAIp; BAI for pediatrics (hip/height0.8–38), AT; adipose tissue, VAT; visceral adipose tissue, SAT; subcutaneous adipose tissue,
using an unpaired t-test.
They were subjected to anthropometric measurements, and blood was drawn after an overnight fast. Serum total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), alanine aminotransferase (ALT), glucose, and insulin were measured at the clinical laboratories of both Showa University Hospital and Showa University Koto Toyosu Hospital. Low-density lipoprotein cholesterol (LDL-C) was calculated using the Friedewald equation (LDL-C=TC–HDL-C–TG/5). Non-HDL-C was calculated using the following equation: non-HDL-C=TC–HDL-C. Atherogenic index (AI) was calculated using the following equation: AI=(TC–HDL-C)/HDL-C.
This study protocol was approved by the Showa University Research Ethics Committee. Informed consent was obtained from the subjects' parents.
Anthropometric Measurements
Anthropometric measurements were performed, as previously described11, 12), by the medical staff at both the clinics. In brief, height was measured to the nearest 0.1 cm and body weight to the nearest 0.1 kg using a stadiometer. The waist circumference was measured at the level of the umbilicus (waist) and hip circumference was measured at the level of maximum extension of the buttocks (hip) to the nearest 0.1 cm. Skinfold thickness was measured to the nearest 0.1 cm using the skinfold caliper at triceps (halfway between the acromion and olecranon) and subscapular (1 cm below the inferior angle of the scapula).
POW, BMI percentile, and BMI-SD values were calculated from the Annual Report of School Health Statistics Research 2000 (Ministry of Education, Culture, Sports, Science and technology in Japan) using MS-EXCEL 2010 (Microsoft Co. Redmond, WA, USA.)10). The percentage body fat (PBF) based on the sum of triceps and subscapular skinfold thickness was obtained using Brozek's equation13), after body density was calculated using Nagamine's formula14).
Measurement of Abdominal Adipose Tissue Distribution
Total adipose tissue, visceral adipose tissue (VAT), and subcutaneous adipose tissue (SAT) area were measured by CT11). A single-slice CT scan of the abdomen was performed at the level of the umbilicus and analyzed for cross-sectional area of the adipose tissue. Adipose tissue area was measured in cm2 assuming a density of −40 to −140 Hounsfield Units for adipose tissue, as described by Tokunaga et al.15).
Hip/heightP Ratio
BAI is based on hip/height1.5 and BAIp is based on hip/height0.8. To investigate which hip/heightP formula was best fit for obese children, we studied the relation of hip/heightP with overweight indices, PBF, adipose tissue area, and obesity-related complications. We set the power value to 0, 0.5, 0.8, 1, 1.5, or 2 and calculated the correlation coefficients between the hip/heightP ratio and these obesity markers. Similarly, the waist-related indices (waist, waist/height, and waist/hip) were also studied.
Statistics
Data are presented as the means and SD. The statistical significance between means was estimated using an unpaired t-test for boys and girls. Differences were considered statistically significant at p < 0.05. Pearson's correlation coefficients were calculated by least-squares linear regression analysis. The statistical analyses were performed using SPSS version 11.0 (SPSS Inc., Chicago, IL, USA).
Results
Anthropometric Data and Fat Area Measured by CT in Obese Children
The anthropometric data and adipose tissue areas measured by CT for obese boys and girls in the study are summarized in Table 1. The mean age, height, body weight, and waist were higher in the obese boys than in the obese girls, whereas overweight indices (POW, BMI percentile, and BMI-SD), PBF, waist/height ratio, and waist/hip ratio were similar in both sexes.
Hip, hip/height0.5, and hip/height were similar in both sexes, whereas hip/height1.5 and hip/height2 were lower in the obese boys than in the obese girls. BAI was also lower in the boys than in the girls. BAIp was not significantly different between the boys and girls.
Abdominal adipose tissue areas were measured in 42 obese boys and 23 obese girls enrolled in the study. Total adipose tissue area, VAT area, and SAT area were not significantly different between sexes. The mean VAT area of obese children in this study was 71.4 ± 27.2 cm2, whereas the criterion16) of excess VAT accumulation in Japanese school-age children is 60 cm2.
The distribution between height and hip or waist and between age and hip/height or waist/height in the study subjects is shown in Fig. 1. The hip and waist were positively correlated with height, similarly in boys and girls (p < 0.001). The hip/height and waist/height were not significantly correlated with age except the girl's waist/height, which was negatively correlated with age (p < 0.05). Overall, the distribution of hip and waist in the enrolled obese boys and girls was similar; therefore, we combined both data and calculated correlation factors.
Fig. 1.
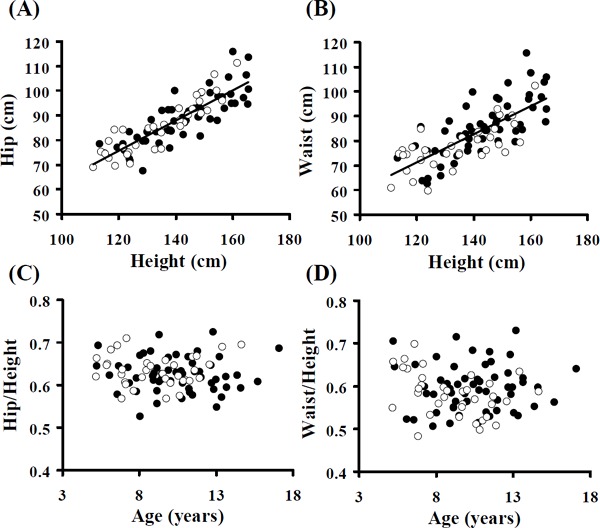
Distribution between height and hip circumference (A) or waist circumference (B) and between age and hip/height ratio (C) or waist/height ratio (D). Closed circles, Boys; Open circles, Girls. Pearson's correlation coefficients were r = 0.853 (Boys, 0.812; Girls, 0.899) in Fig (A) and r = 0.745 (Boys, 0.740; Girls, 0.700) in Fig (B), and all statistical differences were p < 0.001. Age and hip/height, Fig (C); r = 0.101 (Boys, 0.174; Girls, 0.067), and all correlations were not significant (ns). Age and waist/height, Fig (D); r = −0.073, ns (Boys, 0.034, ns; Girls, −0.375, p < 0.05).
Correlation between Hip/heightP Indices and Overweight Indices
Table 2 summarizes the relationships between hip/heightP indices and anthropometric indices in obese children. The correlation coefficients of BAIp or BAI were same as those of hip/height0.8 or hip/height1.5, respectively (Tables 2–4).
Table 2. Correlation between hip/heightP indices and overweight indices in obese children.
| POW (%) | BMI percentile | BMI-SD | PBF (%) | Waist (cm) | Waist/Height | Waist/Hip | |
|---|---|---|---|---|---|---|---|
|
Hip (cm) |
0.410§ |
0.235* |
0.021 |
0.481§ |
0.875§ |
0.303*** |
−0.025 |
| Hip/height0.5 | 0.641§ | 0.447§ | 0.282§ | 0.598§ | 0.825§ | 0.498§ | −0.017 |
| Hip/height0.8 (BAIp) | 0.809§ | 0.624§ | 0.544§ | 0.639§ | 0.650§ | 0.648§ | −0.003 |
| Hip/height | 0.855§ | 0.700§ | 0.704§ | 0.592§ | 0.420§ | 0.699§ | 0.011 |
| Hip/height1.5 (BAI) | 0.655§ | 0.613§ | 0.781§ | 0.305*** | −0.157 | 0.563§ | 0.035 |
| Hip/height2 | 0.455§ | 0.475§ | 0.700§ | 0.122 | −0.408§ | 0.411§ | 0.043 |
| Waist (cm) | 0.558§ | 0.260* | 0.142 | 0.511§ | 0.615§ | 0.459§ | |
| Waist/height | 0.879§ | 0.564§ | 0.686§ | 0.547§ | 0.699§ | ||
| Waist/hip | 0.397§ | 0.110 | 0.274** | 0.204 | |||
Table 4. Correlation between hip/heightP indices and obesity-related complications in obese children.
| TC (mg/dl) |
TG (mg/dl) |
HDL-C (mg/dl) |
LDL-C (mg/dl) |
non HDL-C (mg/dl) |
AI | ALT (U/L) |
Insulin (µU/L) |
|
|---|---|---|---|---|---|---|---|---|
| Hip (cm) | −0.038 | 0.214* | −0.214* | −0.033 | 0.048 | 0.115 | 0.139 | 0.526§ |
| Hip/height0.5 | −0.019 | 0.170 | −0.201 | 0.002 | 0.063 | 0.144 | 0.120 | 0.452§ |
| Hip/height0.8 (BAIp) | 0.003 | 0.095 | −0.155 | 0.037 | 0.067 | 0.153 | 0.080 | 0.302 |
| Hip/height | 0.020 | 0.017 | −0.097 | 0.060 | 0.060 | 0.141 | 0.035 | 0.137 |
| Hip/height1.5 (BAI) | 0.043 | −0.138 | 0.049 | 0.082 | 0.024 | 0.067 | −0.063 | −0.222* |
| Hip/height2 | 0.044 | −0.192 | 0.113 | 0.076 | −0.001 | 0.018 | −0.102 | −0.359§ |
| Waist (cm) | −0.064 | 0.221* | −0.317*** | −0.018 | 0.063 | 0.214* | 0.210* | 0513§ |
| Waist/height | −0.036 | 0.070 | −0.273** | 0.054 | 0.074 | 0.283** | 0.163 | 0.161 |
| Waist/hip | −0.065 | 0.084 | −0.289** | 0.023 | 0.050 | 0.261* | 0.189 | 0.093 |
All hip/heightP indices were significantly correlated with overweight indices. Particularly hip/height0.8 (BAIp), hip/height, and hip/height1.5 (BAI) were highly correlated among hip/heightP. Hip/height and hip/height0.8 were more closely correlated with POW and BMI percentile value than hip/height1.5 However, hip/height1.5 was more closely correlated with BMI-SD value (r = 0.781) than hip/height and hip/height0.8. Hip/height0.8 was more closely correlated with PBF (r = 0.639) than hip/height and hip/height1.5. The correlation coefficients of these three hip/heightP (P = 0.8, 1, and 1.5) with overweight indices were higher than those of waist and waist/hip. In addition, waist/height was most closely correlated with overweight indices among the waist-related indices studied. Hip was of course highly correlated with waist. Hip/height was highly correlated with waist/height.
The correlation between hip/height and POW was very high (r = 0.855, p < 0.001). Fig. 2 shows the scatter graph. The approximate line for prediction of POW was as follows: POW = 411 × hip/height − 207. If one's hip/height is 0.626, POW is expected to be 50.3%, which is equal to 150.3% of the standard weight. The waist/height was also highly correlated with POW (r = 0.879, p < 0.001). The approximate line to predict POW was POW = 308 × waist/height − 131. If one's waist/height is 0.588, POW is estimated to be 50.1%.
Fig. 2.
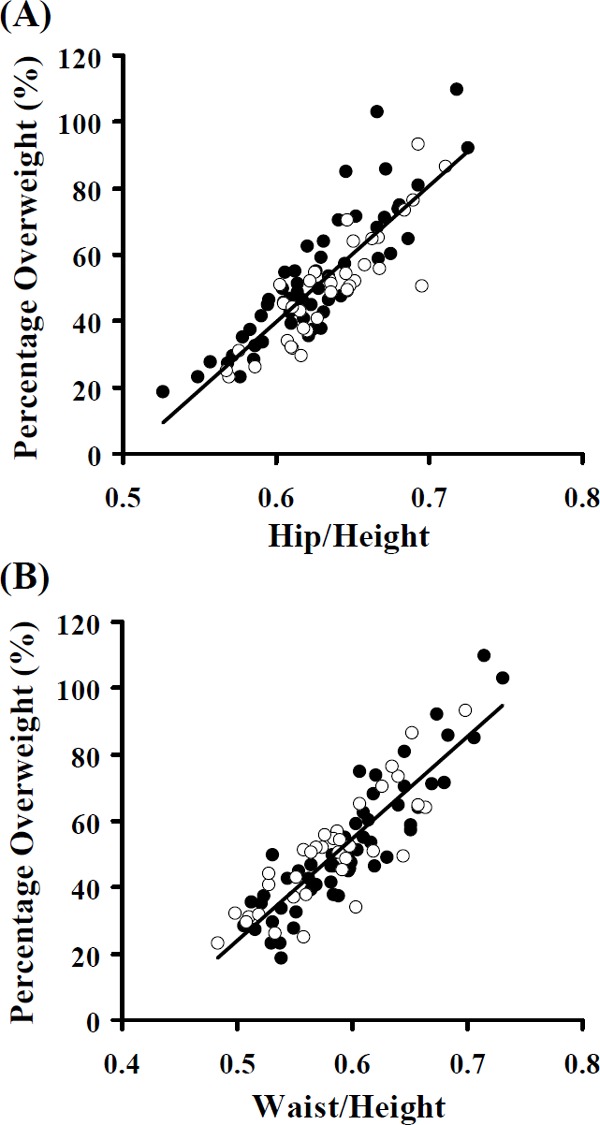
Correlation between percentage overweight and hip/height (A) or waist/height (B). Closed circles, Boys; Open circles, Girls. Pearson's correlation coefficients were r = 0.855 (Boys, 0.870; Girls, 0.870) and r = 0.879 (Boys, 0.898; Girls, 0.850), respectively, and all were significant, p < 0.001.
Correlation between Hip/heightP Indices and Adipose Tissue Area by CT
Hip and hip/height0.5 were more closely correlated with total adipose tissue, VAT, and SAT area than hip/height0.8 (BAIp) and hip/height (Table 3). Hip/height1.5 (BAI) was not significantly correlated with adipose tissue area. Hip was the best index to predict VAT accumulation (r = 0.569, p < 0.001).
Table 3. Correlation between hip/heightP and adipose tissue (AT) area measured by CT.
| Total AT area (cm2) | VAT area (cm2) | SAT area (cm2) | |
|---|---|---|---|
|
Hip (cm) |
0.846§ |
0.569§ |
0.840§ |
| Hip/height0.5 | 0.828§ | 0.503§ | 0.839§ |
| Hip/height0.8 (BAIp) | 0,725§ | 0.380* | 0.754§ |
| Hip/height | 0.568§ | 0.236 | 0.609§ |
| Hip/height1.5 (BAI) | 0.031 | −0.161 | 0.088 |
| Hip/height2 | −0.269* | −0.347*** | −0.216 |
| Waist (cm) | 0.937§ | 0.675§ | 0.916§ |
| Waist/height | 0.661§ | 0.416§ | 0.666§ |
| Waist/hip | 0.328** | 0.337** | 0.290* |
On the other hand, all three waist-related indices were significantly correlated with abdominal adipose tissue areas. In the study, waist was most strongly correlated with VAT (r = 0.675, p < 0.001) (Table 3).
Correlation between Hip/heightP Indices and Biochemical Data
The median values of TC, TG, and LDL-C in the obese children (177, 75, and 104 mg/dL, respectively) were higher than those in Japanese standard values17) (170, 60, and 95 mg/dL, respectively), and the median value of HDL-C (52 mg/dL) was lower than the standard value (60 mg/dL)17). The mean value of ALT was 56.0 ± 62.2 U/L (mean ± SD), and the mean value of insulin was 17.2 ± 10.9 µU/L. In Japan, we considered that the value > 25 U/L and 15 µU/L is high, respectively16). Therefore, many children in the study already had dyslipidemia, fatty liver, and insulin resistance. However, fasting plasma glucose levels were within normal limits (data not shown).
Only hip was significantly correlated with TG and HDL-C (Table 4). Other hip/heightP indices were not significantly correlated with serum lipids, including non-HDL-C and AI. Hip/heightP indices were not correlated with ALT either. Hip and hip/height0.5 were significantly correlated with insulin; however, hip/height1.5 and hip/height2 were inversely correlated strangely.
Waist was significantly correlated with TG, HDL-C, AI, ALT, and insulin. Waist/height and waist/hip were significantly correlated with only HDL-C and AI (Table 4).
Discussion
Almost all hip/heightP indices studied in this study were significantly correlated with overweight indices (POW, BMI-percentile, and BMI-SD) and PBF. On judging these correlation factors, hip/height appears to be the best index among them. The correlation coefficients of hip/height with overweight indices were also higher than those of waist-related indices (waist, waist/height, and waist/hip), except the correlation of waist/height with POW.
The associations between hip/height and POW and between waist/height and POW were very strong. If one's hip/height is > 0.63 or waist/height is > 0.59, he or she is considered to be severely obesity, POW > 50%10). It is well known that BMI itself cannot be used for defining childhood obesity10). In Japan, we use the POW method, but not the BMI-for-age method, for the evaluation of childhood obesity. We believe that POW is more accurate for the evaluation of overweight than BMI-percentile value and BMI-SD score10).
The correlation between hip/height or hip/height0.8 (BAIp) and overweight indices was higher than that of hip/height1.5 (BAI). In addition, BAIp was more correlated with PBF than hip/height or BAI. Some groups8, 18–20) have also reported that BMI (SD) is rather a better tool than BAI for estimating body fat in pediatric field. El Aarbaoui et al.9) have proposed that BAIp is better than BAI. However, Thivel et al.8) reported in 2015 that BAIp did not provide better estimate of adiposity than BMI in obese 12–16-year-old adolescents. We could not investigate the body fat levels by DEXA in this study. DEXA is now considered to be the gold standard method for the estimation of body adiposity. However, the body fat percentage measured by DEXA has been reported to be influenced by the bone mineral density and also by height in children21). In general, the overweight indices, such as POW, must be significantly associated with body fat volume because muscle volumes do not increase so fast in normal children. As mentioned above, hip/height appears to be a more useful marker of overweight than BAIp, based on the correlation factors. Furthermore, the formula of hip/height is simpler than BAIp. In this study, we also found that waist/height is a very good indicator for predicting overweight. Hip/height and waist/height are interesting because they do not require body–weight data.
Hip and hip/height0.5 were more closely correlated with total adipose tissue, VAT, and SAT area than any other hip/heightP indices, including BAIp. Hip was the best index to predict VAT accumulation among hip/heightP, whereas waist was more closely correlated than hip. To the best of our knowledge, this is the first report studying the association between hip/heightP indices with abdominal adipose tissue area measured by CT.
The correlations between hip/heightP indices and complications were weak. Only hip was significantly correlated with TG, HDL-C, and insulin. On the other hand, waist was significantly correlated with TG, HDL-C, AI, ALT, and insulin. Only hip was significantly correlated with VAT; therefore, hip was correlated with complications as well as waist. These results suggest that hip/height, BAIp, and BAI are not useful markers for metabolic complications because they are not associated with VAT area.
VAT accumulation in obesity relates not only to the development of complication risks but also directly relates to the development of obesity-related complications22). In Japan, metabolic syndrome has been designated to be a multiple risk factor clustering syndrome, which is caused by VAT accumulation22). Therefore, abdominal obesity is necessary as an essential factor required in the diagnosis with waist circumference at the level of umbilicus as a first screening tool. In children, excessive accumulation of VAT is a major health problem as well as in adults. Our previous studies showed that VAT area by CT at the umbilical level is the best predictor for liver dysfunction, dyslipidemia, and insulin resistance11, 16). The correlation of VAT area and waist is very high10, 11, 16). Therefore, waist, at the umbilical level, is a more useful surrogate marker for complications than POW or BMI percentile11, 16). The critical value for VAT area and waist are approximately 60 cm2 and 80 cm, respectively, in Japanese school-age children11, 16). Although it is important to accurately evaluate overweight (adiposity), it is more important to predict whether metabolic complications exist.
Thivel et al. have devised a new index using waist circumference named BAI-waist circumference (BAIw), which is similar to BAI8). The formula is as follows: BAIw = waist circumference/height1.5–18. Unfortunately, they8) reported that BAIw underestimated total body adiposity, and the correlation with adiposity measured by DEXA was weaker than BAI and BAIp.
Conclusion
We investigated whether hip/heightP is useful for the evaluation of obesity in children. Hip/height and BAIp (hip/height0.8) are better markers for overweight (adiposity) in obese children than BAI (hip/height1.5). Hip/height appears to be better than BAIp. However, hip/height, BAIp, and BAI are not useful to predict metabolic complications. Waist is considered to be the best index for obese children overall at this time because waist significantly reflects the metabolic complications.
Acknowledgements
This work was supported in part by a Grant-in-Aid for Scientific Research (C) from Japan Society for the Promotion of Science.
Conflicts of Interest
We have no conflicts of interest to declare.
References
- 1). World Health Organization: Facts about overweight and obesity. Obesity and overweight. http://www.who.int/mediacentre/factsheets/fs311/en/
- 2). Chung A, Backholer K, Wong E, Palermo C, Keating C, Peeters A: Trends in child and adolescent obesity prevalence in economically advanced countries according to socioeconomic position: a systematic review. Obes Rev. 2015; 10.1111/obr.12360 [DOI] [PubMed] [Google Scholar]
- 3). Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, Xiang AH, Watanabe RM: A better index of body adiposity. Obesity (Silver Spring). 2011; 19: 1083-1089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4). Schulze MB, Stefan N: The body adiposity index and the sexual dimorphism in body fat. Obesity (Silver Spring). 2011; 19: 1729. [DOI] [PubMed] [Google Scholar]
- 5). Marques-Vidal P, Waeber G, Vollenweider P: Another (better) index of adiposity. Obesity (Silver Spring). 2012; 20: 1137-1138 [DOI] [PubMed] [Google Scholar]
- 6). Snijder MB, Nicolaou M, van Valkengoed IG, Brewster LM, Stronks K: Newly proposed body adiposity index (bai) by Bergman et al. is not strongly related to cardiovascular health risk. Obesity (Silver Spring). 2012; 20: 1138-1139 [DOI] [PubMed] [Google Scholar]
- 7). de Lima JG, Nóbrega LH, de Souza AB: Body adiposity index indicates only total adiposity, not risk. Obesity (Silver Spring). 2012; 20: 1140. [DOI] [PubMed] [Google Scholar]
- 8). Thivel D, O'Malley G, Pereira B, Duché P, Aucouturier J: Comparison of total body and abdominal adiposity indexes to dual x-ray absorptiometry scan in obese adolescents. Am J Hum Biol. 2015; 27: 334-338 [DOI] [PubMed] [Google Scholar]
- 9). El Aarbaoui T, Samouda H, Zitouni D, di Pompeo C, de Beaufort C, Trincaretto F, Mormentyn A, Hubert H, Lemdani M, Guinhouya BC: Does the body adiposity index (BAI) apply to paediatric populations? Ann Hum Biol. 2013; 40: 451-458 [DOI] [PubMed] [Google Scholar]
- 10). Dobashi K: Evaluation of Obesity in School-Age Children. J Atheroscler Thromb. 2016; 23: 32-38 [DOI] [PubMed] [Google Scholar]
- 11). Asayama K, Dobashi K, Hayashibe H, Kodera K, Uchida N, Nakane T, Araki T, Nakazawa S: Threshold values of visceral fat measures and their anthropometric alternatives for metabolic derangement in Japanese obese boys. Int J Obes Relat Metab Disord, 2002; 26: 208-213 [DOI] [PubMed] [Google Scholar]
- 12). Asayama K, Hayashibe H, Dobashi K, Uchida N, Nakane T, Kodera K, Shirahata A: Increased serum cholesteryl ester transfer protein in obese children. Obes Res. 2002; 10: 439-446 [DOI] [PubMed] [Google Scholar]
- 13). Brozek J, Grande J, Anderson T, Keys A: Densitomet ric analysis of body composition: revision of some quantitative assumptions. Ann N Y Acad Sci. 1963; 110: 113-140 [DOI] [PubMed] [Google Scholar]
- 14). Nagamine S, Suzuki S: Anthropometry and body composition of Japanese young men and women. Hum Biol. 1964; 36: 8-15 [PubMed] [Google Scholar]
- 15). Tokunaga K, Matsuzawa Y, Ishikawa K, Tarui S: A novel technique for the determination of body fat by computed tomography. Int J Obes Relat Metab Disord. 1983; 7: 437-445 [PubMed] [Google Scholar]
- 16). Asayama K, Ozeki T, Sugihara S, Ito K, Okada T, Tamai H, Takaya R, Hanaki K, Murata M: Criteria for medical intervention in obese children: a new definition of ‘obesity disease’ in Japanese children. Pediatr Int, 2003; 45: 642-646 [DOI] [PubMed] [Google Scholar]
- 17). Okada T, Murata M, Yamauchi K, Harada K: New criteria of normal serum lipid levels in Japanese children: the nationwide study. Pediatr Int. 2002; 44: 596-601 [DOI] [PubMed] [Google Scholar]
- 18). Zhao D, Zhang Y: Body mass index (BMI) predicts percent body fat better than body adiposity index (BAI) in school children. Anthropol Anz. 2015; 72: 257-262 [DOI] [PubMed] [Google Scholar]
- 19). Yu Y, Wang L, Liu H, Zhang S, Walker SO, Bartell T, Wang X: Body mass index and waist circumference rather than body adiposity index are better surrogates for body adiposity in a Chinese population. Nutr Clin Pract. 2015; 30: 274-282 [DOI] [PubMed] [Google Scholar]
- 20). Dong B, Wang Z, Wang HJ, Ma J: Associations between adiposity indicators and elevated blood pressure among Chinese children and adolescents. J Hum Hypertens. 2015; 29: 236-240 [DOI] [PubMed] [Google Scholar]
- 21). Ellis KJ, Shypailo RJ, Wong WW, Abrams SA: Bone mineral mass in overweight and obese children: diminished or enhanced? Acta Diabetol. 2003; 40: S274-S277 [DOI] [PubMed] [Google Scholar]
- 22). Matsuzawa Y, Funahashi T, Nakamura T: The concept of metabolic syndrome: contribution of visceral fat accumulation and its molecular mechanism. J Atheroscler Thromb. 2011; 18: 629-639 [DOI] [PubMed] [Google Scholar]


