Abstract
Older adults are highly vulnerable to the detriment of extreme weather. The rapid non-linear increase in heat-related morbidity is difficult to quantify, hindering the attribution of direct effects of exposure on severe health outcomes. We examine the effects of ambient temperatures on heat-related hospitalizations (HH) among the elderly in presence of strong seasonality and by assessing the effects caused by the first and subsequent seasonal heatwaves. We empirically derived the thresholds for a heatwave episode in Boston MSA based on 16 years of daily observations. We compared the health risks of heatwaves using the proposed and four alternative definitions. 701 cases of HH in older residents of Boston area were examined using harmonic regression models, designed to capture the non-linear effects of ambient temperatures and heatwave episodes when the night-time temperature is above 65.5 °F for 3 consecutive nights. The overall relative risk of HH associated with a heatwave episode was 6.9 [95%CI:4.8–9.8]. The relative risk of HH associated with the first heatwave increases up to 13.3 [95%CI:7.4–24.0]. The risk declined to 3.7 [95%CI:2.4–5.8] for the subsequent heatwave. Four other commonly used heatwave definitions confirmed these findings. Public health actions have to target the first heatwave to maximize the impact of preventive measures.
Heat waves threaten health, especially of those who are less capable to cope and adapt to the thermal extremes1,2. The recent WHO report and the 2016 US Global Change Research Program on Human Health emphasized the importance of this issue3,4. The major heat wave in Europe in the summer of 2003 caused 15,000 deaths in France alone5,6,7,8,9 and has prompted several investigations of the relationship between human health and maximum daily ambient temperature10,11,12. It has been reported that elderly, defined as people who are 65 years or older, suffer disproportionally more than younger population during heat waves due to lower efficiency of their thermoregulatory mechanisms, potential side effects of medications, and limited mobility13,14,15,16,17,18. Furthermore, high perspiration threshold combined with increased blood viscosity, elevated cholesterol level, and diminished ability to detect changes in body temperature may further contribute to severe heat-related health conditions in older adults. The older adult population in the USA is increasing in both size and proportion19, underpinning the need of targeted preventive actions20.
While the body of research on adverse health effects of extreme weather is rapidly growing, some methodological issues of assessing such effects have yet to be addressed. One of the major ongoing issues is the definition of a heatwave. The WHO report3 lists at least fifteen different exposure metrics used to categorize heat exposure. The Report on the Impacts of Climate Change on Human Health in the United States also notes the lack of commonly accepted methodology in defining extreme hot weather: “Extremes can be defined by average, minimum, or maximum daily temperatures, by nighttime temperatures, or by daytime temperatures. However, there is no standard method for defining a heat wave or cold wave. There are dramatic differences in the observed relationships between temperature, death, and illness across different regions and seasons; these relationships vary based on average temperatures in those locations and the timing of the heat or cold event”4. Recent studies provide extensive and detailed overviews and comparisons of various indicators of extreme heat events21,22,23,24. It is apparent that the most promising and realistic measures consider both duration and intensity of exposure21,22,23,24, so the heatwave indicators mark when the value of a specific measure exceeds an absolute or relative threshold for a selected environmental condition lasting for some period of time, usually from 1 to 5 days. Examples of such definitions include situations when a heat wave is defined as “environmental condition when the daily maximum temperature of more than five consecutive days exceeds the average maximum temperature by 5 °C (9 °F)”25, or “when minimum daily temperature exceeds 95th percentile for 2 consecutive nights”21.
The heatwave threshold is typically determined using absolute values of used measures (physiology-based threshold), as well as relative values (location-based threshold), such as 81st to 99th percentiles26. Physiology-based thresholds are linked to comfort-related ergonomic conditions with potentially less narrow range than location-based thresholds, which vary dramatically and thus reduce comparability of research findings. Yet, the concordance between physiology-based and location-based thresholds is rarely established.
The decision for selecting physiology-based or location-based thresholds in specific context is not clear, yet a solution can be found in better understanding the non-linear relationship between ambient temperature and health conditions. Heat-related morbidity and temperature typically shows a J-shaped relationship with shapes varying by location, climate features, and affected populations16,27,28,29,30,31,32. The lower part of the “J” shape indicate a thermal “comfort” zone, in which heat-related morbidity are less likely to occur. Above the comfort zone, the associated increase in mortality with a unit of exposure increase accelerates. A better characterization of such non-linear relationships should advance the detection of meaningful thresholds and the formulation of location-specific physiologically relevant definition of heatwave episodes.
Ability to quantify and differentiate the effect of individual heat waves with respect to their time of appearance represents another important issue. If the early heat waves pose elevated threat to public, more emphasis could be made on protective measures at the onset of warm season33,34,35. A disproportional effect of the early season’s hot weather on mortality has been noted33,34. A study in North Italian province of Veneto has demonstrated that morbidity equally peaked at the first and the last heat waves of the season35. Thus, if such a phenomenon holds uniformly especially in vulnerable population, effective communication, and mitigation strategies can be better tailored.
While the heat-related mortality has been widely discussed, less attention has been paid to morbidity due to the limited access to reliable data, complexity of reporting, and multifaceted response to the heat. The benefits of using Medicare claim data for large scale investigations of the vulnerable older populations due to its universal, near-exhaustive coverage of Medicare beneficiaries aged 65 and above are well demonstrated36,37. Using this large national data repository comprising of approximately 220 million individual records, we examined the effects of maximum daily ambient temperature on hospitalizations caused by heat exposure among adults residing in the Boston Metropolitan Statistical Area (MSA) between January 1st 1991 and December 31st 2006, inclusive. These urban communities of Massachusetts are characterized by temperate climate, relatively high living standards, close proximity and easy access to points of medical care. We hypothesized that: (1) the magnitude and duration of ambient temperature exposure directly contributes to the occurrence and severity of HHs in a non-linear fashion with an accelerating effect when ambient day and night temperatures exceeded specific thresholds; (2) the first heatwave of each year is associated with more cases of HHs when compared to the subsequent heatwaves in the same year; and (3) the disproportional effect of the first wave will be present after adjusting for the seasonal nature of exposure the HHs has well-pronounced temporal features, which can be described by harmonic oscillations and specific calendar effects. We empirically defined location-specific thresholds and describe non-linear associations between daily ambient temperature and hospitalization rates due to exposure to environmental heat based on International Classification of Diseases (ICD-9-CM). We determined the effect caused by the first and subsequent heatwaves by estimating the relative risks in presence of well-pronounced seasonal variations of the selected health outcomes. We then compared the proposed data-driven definition with four commonly used definitions of a heatwave episode in terms of assessing the detrimental effects on heat-related hospitalizations.
Methods
Hospitalization records
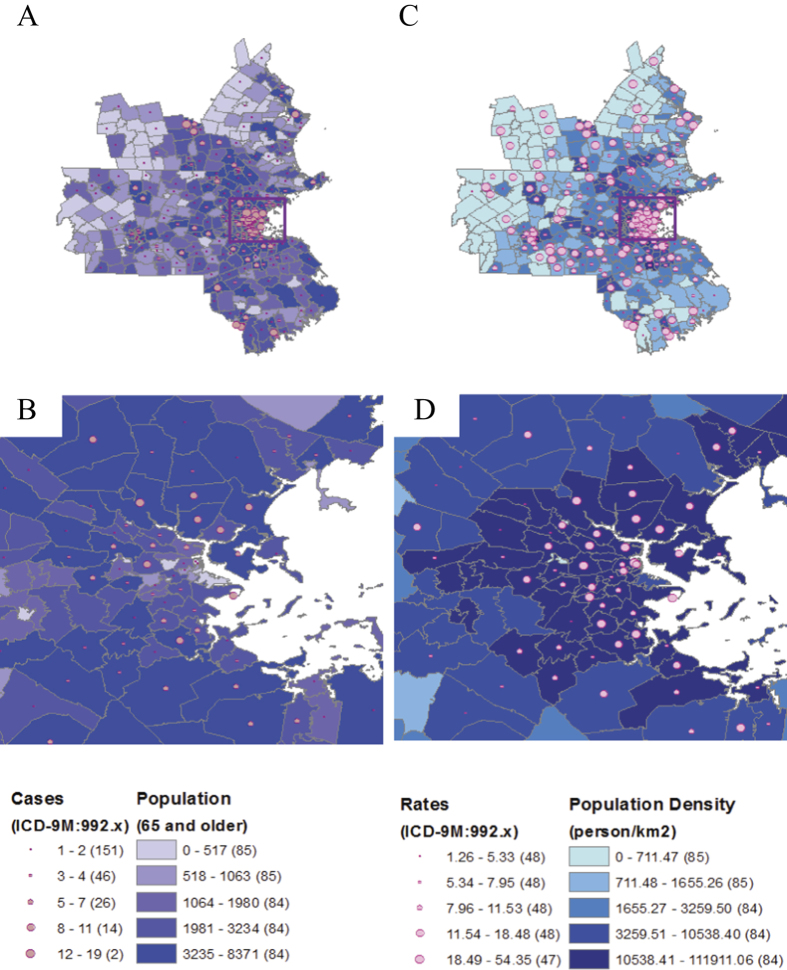
Daily hospitalization records from January 1st 1991 to December 31st 2006 were obtained from the CMS database. Each record contains age, ZIP code of residence, date of admission, and up to 10 diagnostic codes based on International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM). 1123 hospitalization records with ICD-9-CM 992.0–992.9 in any of 10 diagnostic fields were abstracted. This ICD category covers a broad range of health conditions, which in the opinion of a treating physician are most likely caused by environmental exposures to heat. While other ICD categories are associated with exposure to hot weather, we purposefully selected this ICD codes to minimize potential misclassification. For 701 records selected for the analysis, the heat-related diagnosis was listed as primary or secondary cause; 83% of cases were coded as heat stroke or heat exhaustion (Table 1). Using reported ZIP codes of residence we selected all ZIP codes that belongs to Boston-Cambridge-Quincy Metropolitan Statistical Area (Boston MSA) (United States Census Bureau 2014). According to the US Office of Management and Budget, MSA is defined as “a region that has at least one urbanized area of 5,000 or more population, plus adjacent territory that has a high degree of social and economic integration with the core as measured by community ties.” In 2010, Boston MSA was the 10th most populated MSA in the US with the total area of 4,674 mi2 and the total population of 4,552,402; consisted of 74.9% non-Hispanic White population, 9% Hispanic and Latino population, 7.4% non-Hispanic Black population, 7.1% Asians and 1.6% of other races and ethnicities; 10% of MSA population was 65 years old and older (United States Census Bureau 2014). Using linear interpolation of Census 1990, 2000, and 2010 data we estimated older adult population in the study area, calculated the annual hospitalization rates per 1 million people aged 65 and older. We created the MSA maps by matching ZIP codes of the Census basemaps with the list of ZIP codes within Boston MSA and mapped the hospitalizations with ArcGIS 10.2. http://www.esri.com/software/arcgis/arcgis-for-desktop (see Fig. 1).
Table 1. Distribution of cases based on diagnostic code ICD-9-CM.
| ICD-9-CM code | Description | Cases (%) |
|---|---|---|
| 992.0 | Heat stroke and sunstroke | 115 (16.4) |
| 992.1 | Heat syncope | 49 (7.0) |
| 992.2 | Heat cramps | 6 (0.9) |
| 992.3 | Heat exhaustion, anhydrotic | 40 (5.7) |
| 992.4 | Heat exhaustion due to salt depletion | 9 (1.3) |
| 992.5 | Heat exhaustion, unspecified | 465 (66.3) |
| 992.6 | Heat fatigue, transient | 2 (0.3) |
| 992.7 | Heat edema | 0 (0) |
| 992.8 | Other specified heat effects | 7 (1.0) |
| 992.9 | Unspecified effects of heat and light | 8 (1.1) |
Figure 1.
The distributions of heat-related hospitalizations (HH), population of older adults aged 65 and over, or elderly (Panels (A) and (B), respectively), hospitalization rates (per 1 M people) and elderly population density (Panels (C) and (D), respectively), within the Boston MSA (Panels (A) and (C), respectively), and its the most urbanized part (Panels (B) and (D), respectively) observed in 1991–2006. Maps were created with ArcGIS 10.2. http://www.esri.com/software/arcgis/arcgis-for-desktop.
Ambient temperature data
Daily temperature records of the Boston MSA were obtained from the National Oceanic and Atmospheric Administration–Global Summary of the Day (NOAA-GSOD) (Unites States National Oceanic and Atmospheric Administration 2014) for the study period. The dataset includes maximum and minimum daily temperature from 83 meteorological stations situated within the borders of Boston MSA and up to 120 miles buffer zone. The daily temperature data were interpolated for each ZIP code (average number of stations per ZIP code: 54.4 ± 4.7, distance between nearest station and ZIP code centroid: 7.75 ± 3.84 miles) using an inverse distance weighting (IDW) method, which allows for multivariate interpolation by assigning the values to unknown locations calculated with a weighted average of the values available at the known points38.
Non-linear fit and empirical definition of a heatwave episode
To capture the effect of a heatwave on non-linear exponential increase in hospitalization counts we derived an empirical definition of a heatwave episode assuming that the magnitude and duration of ambient temperature exposure directly contributes to the occurrence and severity of heat-related hospitalizations (HHs) in a non-linear fashion with an accelerating effect when ambient day and night temperatures exceeded specific thresholds.
To estimate thresholds, the maximum (day-time) and minimum (night-time) temperature values were transformed and parameterized as follow:
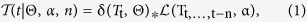 |
where δ(Tt, Θ) is a Dirac delta function with a threshold parameter Θ, and  is a scaled lag-distributed ambient temperature for n periods with exponential decay parameter α.
is a scaled lag-distributed ambient temperature for n periods with exponential decay parameter α.
Dirac delta function δ(Tt, Θ) in Eq. (1) is defined as:
 |
where Tt is the daily temperature value for a t-day and Θis a temperature threshold value.
Scaled lag-distributed temperature  in Eq. (1) is defined as weighted sum of temperature measures for n days prior to date t, linearly scaled to the [0..1] interval:
in Eq. (1) is defined as weighted sum of temperature measures for n days prior to date t, linearly scaled to the [0..1] interval:
 |
where α is the exponential decay parameter and n is the number of included temporal lags. Due to the exponential nature of weights α in Eq. (3), the effective number of lags n, i.e. the number of days with sufficiently large weight capable to substantially influence the outcome, is determined as:
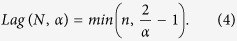 |
By setting parameter n sufficiently large, the exponential decay parameter α effectively determines the number of lags included in the model. For example, with the number of lags n = 10, and decay parameter α = 0.5, the contribution of lag 0 is slightly above 50%, the contribution of lag 4 is about 6%, and the contribution of lag 10 is less than 0.1%.
To fit the non-linear association between daily ambient temperature and HH the Negative-Binomial Generalized Linear Model (NB-GLM) has been applied:
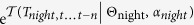
 |
where Ht is the daily hospitalization counts for the study period; 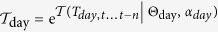 ,
, 
 and Yt is an indicator variable absorbing inter-year variability. We selected the vector of parameters:
and Yt is an indicator variable absorbing inter-year variability. We selected the vector of parameters:
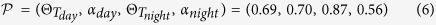 |
by maximizing goodness of fit of the NB-GLM Eq. (5)) based on Akaike Information Criterion (AIC). The optimized data-driven parameters Θ and α from Eq. (6) represent temperature threshold and effective duration or a number of days with temperature above this threshold that maximizes the non-linear effect of the scaled lag-distributed ambient temperature on the health outcome. As such, the parameter vector  can be used to determine heatwave episodes. The length of the effective day time lag is
can be used to determine heatwave episodes. The length of the effective day time lag is 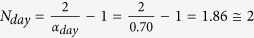 , and the effective night-time temperature lag is
, and the effective night-time temperature lag is 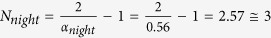 . Thus, we proposed a definition of heatwave for our study area as an environmental condition when daytime temperature is above 69.5 °F (20.8 °C) for the current and previous day and night-time temperature is above 65.5 °F (18.6 °C) for the current and two previous nights. The span between two consecutive heatwave episodes should be no less than 2 days. A binary variable indicating a day when such condition is met, or a heatwave day, was created for each day during the study period.
. Thus, we proposed a definition of heatwave for our study area as an environmental condition when daytime temperature is above 69.5 °F (20.8 °C) for the current and previous day and night-time temperature is above 65.5 °F (18.6 °C) for the current and two previous nights. The span between two consecutive heatwave episodes should be no less than 2 days. A binary variable indicating a day when such condition is met, or a heatwave day, was created for each day during the study period.
Alternative definitions of a heatwave episode
In addition to the definition of a heatwave proposed above we have examined four alternative heatwave definitions:
Definition A: daily maximum temperature over 95% threshold for 3+ consecutive days3;
Definition B: daily maximum temperature over 95% threshold (computed over summer months between May 1 and September 30) for 3+ consecutive days21,26;
Definition C: maximum daily temperature above 80.6 °F (27 °C) for 6+ consecutive days3,39,40;
Definition D: humidex above 104 °F (40 °C) for 2+ consecutive days41,42.
Definitions A–C are based on the simple threshold of one parameter (maximum daily ambient temperature), while Definition D is a function of maximum daily temperature and humidity. The first two definitions use relative measures, while the last two use absolute thresholds. We then created binary variables indicating day when relevant conditions are met for each day during the study period to further use in the analysis.
Estimation of seasonal peaks for heat-related hospitalizations and ambient temperature
The heat related hospitalizations are highly seasonal phenomenon where of the 701 cases of heat-related admissions, 621 (89%) occurred in summer. The harmonic regression has the ability to naturally adjust for periodic seasonal oscillations by using data for the entire study period. A harmonic component properly accounts for transitional periods of spring and autumn and accommodates periods with high level of outcomes (i.e. during the hot season) and with low level of outcome (i.e. during the cold season)43,44.
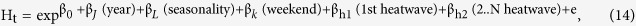
First, we fit a NB-GLM to HH counts, denoted as Model 1:
 |
where Ht is the daily HH counts for a t-day; βL is the vector of coefficients for a seasonal pattern based on one harmonic term with the period ω = 1/365.25 and Seasonality is a short hand for βssin(2πωt) + βccos(2πωt).
Similarly, daily maximum and minimum temperature values were fitted as Gaussian OLS, as Model 1 modification of:
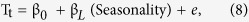 |
where Tt is the daily maximum or minimum temperature value for a t-day; βL is the vector of coefficients for a seasonal pattern based on one harmonic term with the period ω = 1/365.25 and Seasonality ~βssin(2πωt) + βccos(2πωt).
Based on models’ βL values related to seasonal harmonics, the average peak timing of HH and its 95th confidence interval (CI) were estimated using δ–method43,44. Peak timing of a periodic process of the form 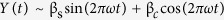 was determined as:
was determined as:
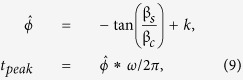 |
where constant k depends on the join sign of estimated coefficients βs and βc: k = 0 when both βs and βc are positive, k = 2π when βs > 0 and βc < 0, and k = π otherwise.
The 95th confidence interval (CI) of the peak timing was determined as:
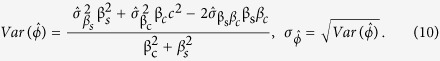 |
From the Model 1 we determined the peak timing of HH and compared it with the peak timing of the ambient temperature.
Individual effects of consecutive heat waves
In order to test the stated hypotheses we built statistical models sequentially. First, we built a model considering temporal features in HH time series, such as seasonality, annual and weekly cycles, and the effects of local social calendars (Model 2). Then, we incorporated the heatwave indicator based on the proposed and alternative definitions to test if heatwave days have higher HH than non-heatwave days (Model 3). Finally, we used separate indicators for the first heatwave episode and consecutive episodes during the same season (Model 4). This model allowed us to test the hypothesis that first heatwave have disproportionally large effect on vulnerable population relative to the consecutive heatwaves the same season. These steps are described in details below.
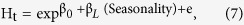
Temporal features in the daily time series of HH counts were examined using NB-GLM for count data, denoted as Model 2:
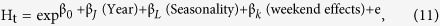 |
where Ht is the daily HH counts; βJ is the vector of coefficients for the effect of a calendar year based on a set of indicator variables with 1991 set as a reference year (the βJ term accounts for the inter-year changes in population at risk, as well as potential changes in reporting policies and practices during the 16 year study); βL is the vector of coefficients for a seasonal pattern based on a harmonic regression with the period ω = 1/365.25 and two harmonics:
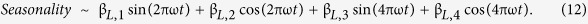 |
Model 2 also includes variables to account for the effects of weekdays: βk is the vector of coefficients for an indicator variable considering weekends combined with major federal holidays (Saturday, Sunday and major holidays, including New Year’s Day (January 1st), Labor Day (June 19th), Independence Day (July 4th), Veterans Day (Nov 11th), and Christmas Day (December 25th); weekdays, Monday to Friday, were set as a reference category).
To assess the effect of heatwave episodes we added an indicator variable to Model 2, as in Model 3:
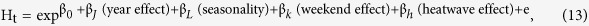 |
where βh is the coefficient indicating the effects of the heat waves in the season relative to the rest of the days; the remaining coefficients are the same as in Eq. (11).
We then further separated the effect of the first heatwave in the season from the effects of the following up heat waves on HH in Model 4:
 |
where βh1 is the coefficient indicating the effects of the first heatwave in the season relative to the rest of the days, and βh2 is the coefficient indicating the effects of the second and all subsequent heat waves in the season relative to the all other days. The relative risk of HH associated with a heatwave episode along with its 95th CI were estimated as: 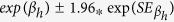 for βh1 and βh2, respectively. Model 4 was also applied to estimate individual effects of the first and consecutive heatwaves on HH using four alternative definitions as described above.
for βh1 and βh2, respectively. Model 4 was also applied to estimate individual effects of the first and consecutive heatwaves on HH using four alternative definitions as described above.
We examined the individual contribution of the effects of the year, seasonality, effects of weekdays and the effects of heatwaves on variability explained by Models 2, 3 and 4 based on the relationship between total and residual deviance and the AIC score.
Results
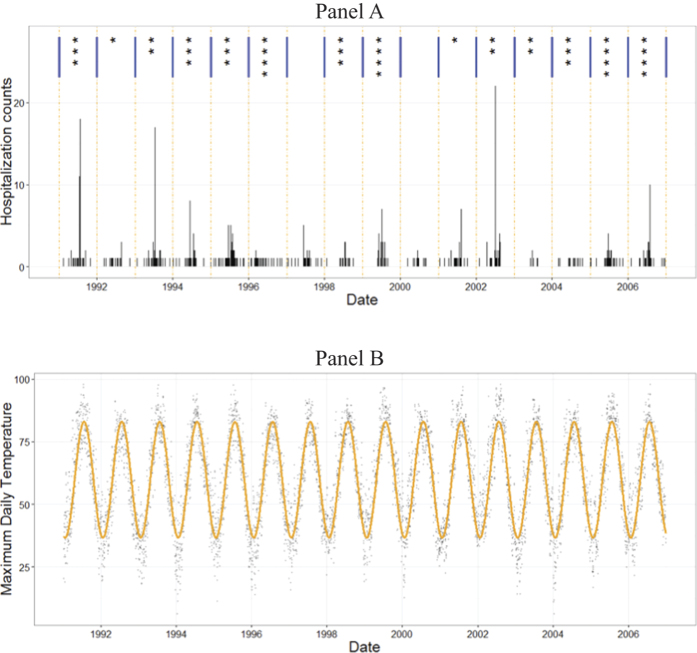
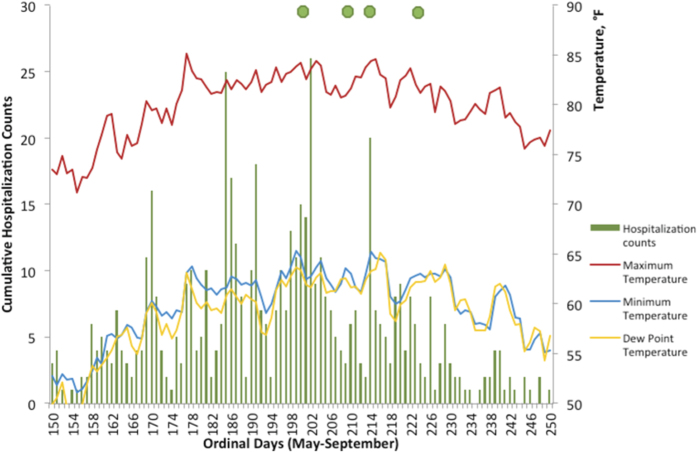
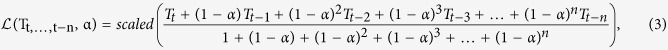
During the 16-year study period there were 701 hospitalizations due to heat in the Boston-Cambridge-Quincy, MA-NH MSA. Figure 1 illustrates the spatial patterns of the abstracted records. Elevated rates of heat-related hospitalization tend to concentrate in urban areas with greater population density. The time series of daily counts of HH reflects sharp spikes with up to 20-fold increase during summer months (Fig. 2). As estimated from Model 1, HH peaked on July 13th with a median peak date at 194th (IQR: 170th; 210th) Julian calendar day. As estimated from regression model, ambient maximum and minimum temperature peaked on July 24th (205th; IQR: 183rd; 213th) and on August 1st with a median of 213th (IQR: 205th; 243rd) Julian calendar day, respectively. Therefore, heat-related hospitalizations are expected to peak on average 11 days earlier than the expected peak in temperature.
Figure 2.
Annual number of heat waves episodes (top row, Panel A) and daily counts of heat-related hospitalizations (bottom row, Panel B) and daily maximum temperature: actual and fitted with Model B (°F; Panel C) in Boston MSA, 1991–2006.
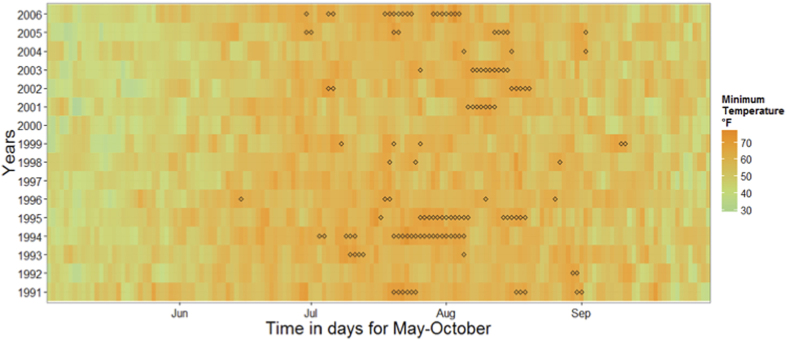
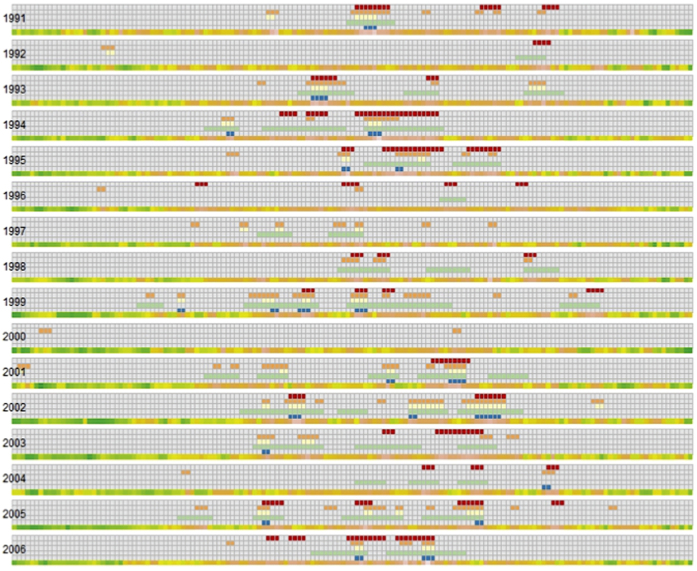
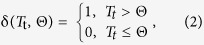
Based on the proposed definition of heatwave in Boston MSA, we identified 44 heat waves comprised of totally 111 days during the study period (Table 2). Timing for the individual heatwave days along with the heat map of daily night temperature are presented in Fig. 3. Descriptive statistics of heatwave occurrence, duration, the start of the first and last episodes and heat-related hospitalizations (HH) during the heatwave episodes are shown in Table 3. The number of heatwaves and days associated with heatwaves varied for alternative definitions, yet they uniformly agreed on low counts of HH for relatively cold summers of 1992, 1996, 2000, and 2004 (Fig. 4). As expected, Definitions A and D appeared to be the most and least conservative estimates for Boston MSA, respectively.
Table 2. Heatwaves for Boston MSA, 1991–2006: total number of HH cases and days associated with heatwave definitions with Julian calendar days for the first and last heatwaves.
| All* | 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Proposed Definition | |||||||||||||||||
| Number of HW | 44 | 3 | 1 | 2 | 3 | 5 | 4 | 0 | 3 | 4 | 0 | 2 | 2 | 2 | 3 | 4 | 6 |
| Maximum length | 4.64 | 6 | 2 | 4 | 17 | 6 | 2 | 1 | 2 | 3 | 5 | 9 | 1 | 4 | 3 | ||
| Total days | 111 | 11 | 2 | 5 | 22 | 13 | 5 | 3 | 5 | 4 | 7 | 10 | 3 | 10 | 11 | ||
| Date of the first HW | 195 | 198 | 241 | 188 | 181 | 195 | 165 | 197 | 186 | 215 | 183 | 204 | 216 | 177 | 178 | ||
| Date of the last HW | 231 | 241 | 242 | 214 | 214 | 228 | 237 | 236 | 251 | 221 | 229 | 224 | 244 | 242 | 213 | ||
| HH counts** | 207 | 46 | 0 | 35 | 18 | 17 | 0 | 4 | 7 | 11 | 39 | 3 | 1 | 8 | 18 | ||
| HH per HW day | 1.96 | 4.18 | 0 | 7 | 0.82 | 1.31 | 0 | 1.33 | 1.4 | 2.75 | 5.57 | 0.3 | 0.33 | 0.8 | 1.64 | ||
| HH per non-HW day | 0.18 | 0.16 | 0.14 | 0.23 | 0.25 | 0.31 | 0.07 | 0.17 | 0.11 | 0.29 | 0.09 | 0.22 | 0.23 | 0.05 | 0.08 | 0.21 | 0.25 |
| Definition A | |||||||||||||||||
| Number of HW | 81 | 7 | 1 | 5 | 4 | 6 | 2 | 7 | 3 | 10 | 2 | 8 | 7 | 4 | 2 | 9 | 4 |
| Maximum length | 3.75 | 5 | 2 | 5 | 4 | 4 | 1 | 2 | 3 | 5 | 2 | 4 | 9 | 4 | 2 | 6 | 2 |
| Total days | 165 | 12 | 2 | 11 | 8 | 11 | 2 | 8 | 6 | 21 | 3 | 15 | 25 | 11 | 3 | 20 | 7 |
| Date of the first HW | 162 | 179 | 143 | 177 | 169 | 170 | 142 | 162 | 196 | 152 | 129 | 123 | 178 | 177 | 161 | 163 | 170 |
| Date of the last HW | 226 | 240 | 144 | 240 | 207 | 229 | 200 | 229 | 237 | 247 | 222 | 222 | 253 | 234 | 243 | 256 | 215 |
| HH counts | 314 | 43 | 2 | 39 | 23 | 30 | 1 | 4 | 10 | 31 | 2 | 27 | 58 | 5 | 2 | 14 | 23 |
| HH per HW day | 1.74 | 3.58 | 1 | 3.55 | 2.88 | 2.73 | 0.5 | 0.5 | 1.67 | 1.48 | 0.67 | 1.8 | 2.32 | 0.45 | 0.67 | 0.7 | 3.29 |
| HH per non-HW day | 0.14 | 0.19 | 0.13 | 0.21 | 0.19 | 0.21 | 0.06 | 0.15 | 0.08 | 0.14 | 0.08 | 0.12 | 0.11 | 0.04 | 0.07 | 0.18 | 0.21 |
| Definition B | |||||||||||||||||
| Number of HW | 34 | 2 | 1 | 2 | 2 | 2 | 0 | 3 | 0 | 4 | 0 | 4 | 6 | 2 | 0 | 4 | 2 |
| Maximum length | 2.75 | 4 | 1 | 3 | 2 | 1 | 1 | 3 | 3 | 8 | 2 | 3 | 2 | ||||
| Total days | 66 | 5 | 1 | 6 | 4 | 2 | 3 | 7 | 6 | 18 | 4 | 7 | 3 | ||||
| Date of the first HW | 172 | 179 | 144 | 189 | 169 | 196 | 173 | 159 | 123 | 178 | 177 | 177 | 199 | ||||
| Date of the last HW | 209 | 202 | 144 | 240 | 203 | 213 | 199 | 200 | 222 | 253 | 188 | 226 | 215 | ||||
| HH counts | 211 | 35 | 1 | 28 | 20 | 6 | 2 | 15 | 20 | 53 | 5 | 8 | 18 | ||||
| HH per HW day | 3.18 | 7 | 1 | 4.67 | 5 | 3 | 0.67 | 2.14 | 3.33 | 2.94 | 1.25 | 1.14 | 6 | ||||
| HH per non-HW day | 0.17 | 0.23 | 0.13 | 0.28 | 0.2 | 0.36 | 0.07 | 0.16 | 0.14 | 0.24 | 0.09 | 0.16 | 0.14 | 0.03 | 0.09 | 0.2 | 0.24 |
| Definition C | |||||||||||||||||
| Number of HW | 46 | 1 | 2 | 3 | 3 | 2 | 1 | 2 | 3 | 5 | 1 | 5 | 4 | 3 | 3 | 4 | 4 |
| Maximum length | 7.69 | 6 | 2 | 8 | 14 | 10 | 1 | 3 | 7 | 20 | 4 | 6 | 14 | 11 | 2 | 9 | 6 |
| Total days | 237 | 6 | 3 | 15 | 30 | 16 | 1 | 6 | 15 | 31 | 4 | 17 | 30 | 25 | 6 | 23 | 9 |
| Date of the first HW | 186 | 201 | 195 | 190 | 169 | 205 | 223 | 181 | 199 | 154 | 178 | 169 | 177 | 180 | 204 | 163 | 193 |
| Date of the last HW | 226 | 206 | 241 | 244 | 217 | 230 | 223 | 199 | 243 | 252 | 181 | 236 | 235 | 229 | 228 | 226 | 222 |
| HH counts | 290 | 43 | 1 | 39 | 26 | 20 | 0 | 4 | 9 | 17 | 1 | 24 | 62 | 4 | 3 | 15 | 22 |
| HH per HW day | 1.35 | 7.17 | 0.33 | 2.6 | 0.87 | 1.25 | 0 | 0.67 | 0.6 | 0.55 | 0.25 | 1.41 | 2.07 | 0.16 | 0.5 | 0.65 | 2.44 |
| HH per non-HW day | 0.15 | 0.18 | 0.14 | 0.22 | 0.2 | 0.3 | 0.07 | 0.15 | 0.09 | 0.27 | 0.09 | 0.14 | 0.08 | 0.05 | 0.07 | 0.17 | 0.22 |
| Definition D | |||||||||||||||||
| Number of HW | 9 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 2 | 0 | 1 | 2 | 0 | 0 | 0 | 1 |
| Maximum length | 1.71 | 1 | 2 | 1 | 1 | 2 | 4 | 1 | |||||||||
| Total days | 14 | 1 | 2 | 1 | 2 | 2 | 5 | 1 | |||||||||
| Date of the first HW | 200 | 202 | 190 | 203 | 187 | 221 | 185 | 215 | |||||||||
| Date of the last HW | 209 | 202 | 191 | 203 | 200 | 222 | 230 | 215 | |||||||||
| HH counts | 97 | 18 | 24 | 2 | 9 | 9 | 30 | 5 | |||||||||
| HH per HW day | 7.43 | 18 | 12 | 2 | 4.5 | 4.5 | 6 | 5 | |||||||||
| HH per non-HW day | 0.22 | 0.34 | 0.14 | 0.3 | 0.32 | 0.4 | 0.07 | 0.17 | 0.14 | 0.27 | 0.09 | 0.23 | 0.29 | 0.07 | 0.09 | 0.25 | 0.32 |
aThe maximum length, date of the first and last heatwave, heat-related hospitalizations (HH) per heatwave (HW) and non-HW days across all years are shown as averages; Number of HW episodes, total number of days associated with HW and total HH counts across all years are shown as sum of all events.
bHH counts are estimated over the summer period of 151 days from May to September.
Figure 3.
Calendar map of night temperature with “◊” marking days of a heatwave in Boston MSA, 1991–2006 (May through October) based on the proposed definition.
Table 3. Descriptive statistics of heatwave episodes occurrence for Boston MSA, 1991–2006: total duration and average timing; heat-related hospitalizations (HH); average daytime (Max T) and night time (Min T) temperature values during the heatwave episodes and relative risks with CI95% of HH associated with heatwave episodes estimated from Model 3.
| Heatwave sequence | Number seasons | Number of days | Mean (SD) Ordinal Day | Number of HH | HH per day | Max Temp °F Mean (SD) | Min Temp °F Mean (SD) | HW episode RR (CI95%) |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 27 | 196.7 (17.6) | 124 | 4.59 | 87.4 (6.1) | 68.8 (2.5) | 15.3 (9.2–25.5) |
| 2 | 4 | 39 | 213.7 (14.0) | 42 | 1.08 | 87.3 (4.7) | 69.1 (2.1) | 3.8 (2.1–6.7) |
| 3 | 4 | 33 | 214.3 (13.0) | 30 | 0.91 | 87.2 (4.6) | 68.9 (2.1) | 2.7 (1.5–5) |
| 4+ | 5 | 12 | 226.6 (17.2) | 11 | 0.92 | 84.0 (5.3) | 68.6 (2.3) | 7.1 (2.7–18.9) |
Figure 4. Comparison of the proposed definition with four alternative definitions.
Each row represents days from May 1st to Sep 30th; Days assigned to be a HW by a selected definition are marked by color (Proposed Definition–red; Definition A–orange; Definition B–yellow, Definition C–green; Definition D–blue). The last line represents maximum daily temperature for a given day for each year with the spectrum from green (~30 °F) to orange (~90 °F).
Over the study period, there were 111 days marked as heatwave days based on the proposed data-driven definition. While they represent only 1.9% out of 5844 days of observations, during those days 207 cases of heat-related hospitalizations were recorded, accounting for 30% of all 701 cases or 33% of 621 cases occurred during the summer-time period. During the first heatwave of the season, that occurred on average on 196.7 ± 17.6 Julian calendar day, almost two weeks before the average peak in minimum temperature, the daily number of hospitalizations were almost 5 times higher as compared to rates at the second and subsequent heatwaves (Table 3). The average daily maximum and minimum temperature during heatwave episodes lasted for 3.2 days had exceeded 86 °F and 68 °F, respectively. For the first heatwave of the season the average number of hospitalization were 4.59 per day for the total of 27 days. For the subsequent heatwaves the mean number of hospitalizations per day were 0.99 per day for the total of 84 days.
The effects of heatwaves on HH were estimated using the results of Models 3 and 4, presented in Table 4. After adjusting for seasonality and weekday effects, the relative risk of HH associated with a heatwave episode was 6.89 [95%CI: 4.84–9.8] (Model 3). The relative risk of HH associated with the first heatwave in a summer season was the highest for first episode: 13.33 [95%CI: 7.4–24] (Model 4). The risk declined to 3.74 [95%CI: 2.43–5.76] for the subsequent heatwave episodes. For the four additional definitions, the relative risks associated with the first heatwave and the subsequent heatwaves are presented in Table 4. The first heatwave has consistently higher relative risks than subsequent heatwaves for all alternative definitions. The measures for the quality of fit for different model specifications and heatwave definitions are presented in Table 5.
Table 4. The results of the sequentially built Negative-Binomial Generalized Linear Models (NB-GLM) with harmonic terms for heat-related hospitalizations (HH) for heatwave episodes in Boston MSA, 1991–2006 based on the proposed definition and four alternative definitions of a heatwave episode.
| Model 2 |
Model 3 |
Model 4 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | Std. Error | p-value | Estimate | Std. Error | p-value | Estimate | Std. Error | p-value | |
| Proposed Definition | |||||||||
| Intercepta | −2.46 | 0.20 | <0.001 | −2.76 | 0.20 | <0.001 | −2.88 | 0.20 | <0.001 |
| COS (1st)b | −1.58 | 0.11 | <0.001 | −1.38 | 0.10 | <0.001 | −1.38 | 0.10 | <0.001 |
| SIN (1st) | 0.07 | 0.12 | 0.52 | 0.14 | 0.11 | 0.21 | 0.13 | 0.11 | 0.25 |
| COS (2nd) | 0.69 | 0.09 | <0.001 | 0.59 | 0.09 | <0.001 | 0.56 | 0.09 | <0.001 |
| SIN (2nd) | 0.46 | 0.10 | <0.001 | 0.21 | 0.10 | 0.03 | 0.23 | 0.09 | 0.02 |
| WEEKEND-HDAYc | −0.23 | 0.12 | 0.06 | −0.26 | 0.12 | 0.03 | −0.29 | 0.12 | 0.01 |
| HW Episode | 1.93 | 0.18 | <0.001 | ||||||
| 1st HW | 2.59 | 0.30 | <0.001 | ||||||
| Later HW | 1.32 | 0.22 | <0.001 | ||||||
| Definition A | |||||||||
| HW Episode | 2.26 | 0.14 | <0.001 | ||||||
| 1st HW | 2.48 | 0.28 | <0.001 | ||||||
| Later HW | 2.20 | 0.15 | <0.001 | ||||||
| Definition B | |||||||||
| HW Episode | 2.52 | 0.19 | <0.001 | ||||||
| 1st HW | 2.63 | 0.34 | <0.001 | ||||||
| Later HW | 2.46 | 0.22 | <0.001 | ||||||
| Definition C | |||||||||
| HW Episode | 1.70 | 0.15 | <0.001 | ||||||
| 1st HW | 2.20 | 0.20 | <0.001 | ||||||
| Later HW | 1.21 | 0.19 | <0.001 | ||||||
| Definition D | |||||||||
| HW Episode | 2.84 | 0.44 | <0.001 | ||||||
| 1st HW | 3.01 | 0.53 | <0.001 | ||||||
| Later HW | 2.21 | 0.77 | <0.001 | ||||||
aAll models are adjusted for the year effects as described in Method section (data not shown).
bThe sin and cos terms for the first and second harmonics of seasonal components, respectively.
cA term for weekend and holiday effects (WEEKEND-HDAY).
Table 5. Quality of fit measures for different model specifications and heatwave definitions.
| Model | AIC* | Null Deviance (DF = 5833) | Residual Deviance (DF) | −(Log-Likelihood) |
|---|---|---|---|---|
| Model 2 | 3343 | 2659.3 | 1580.6 (5813) | 3299 |
| Model 3 | 3221 | 2772.9 | 1622.1 (5812) | 3175 |
| Model 4 | ||||
| Proposed Definition | 3204 | 2772.9 | 1616.3 (5809) | 3152 |
| Definition A | 3100 | 2956.2 | 1620.0 (5811) | 3052 |
| Definition B | 3167 | 2838.5 | 1625.1 (5811) | 3119 |
| Definition C | 3211 | 2668.1 | 1573.4 (5811) | 3163 |
| Definition D | 3275 | 2532.9 | 1557.2 (5811) | 3226 |
*AIC–Akaike Information Criterion; DF–degrees of freedom.
Discussion
The impact of heat on human health has received significant public attention. The most recent National Climate Assessment (United States National Climate Assessment (USNCA) Program 2014) and WHO report on heatwaves and health3 emphasizes the need for broad public health actions, especially in the areas of preparedness and prevention, which can do much to protect vulnerable population from the detrimental impacts of extreme weather45. The heat related mortality has been extensively studied in relation to various death related causes and adaptation scenarios in the context of the current climate and projected climate changes46,47,48,49,50. The heat related morbidity, on the other hand, has been less examined yet the cost associated with hospitalizations is quite substantial. The analysis demonstrates that a heatwave episode results in almost 7-fold increase in heat-related hospitalizations over 16-year period among the older adults in Boston MSA, a composite of urban and semi-urban communities with mild temperate climate, relatively high living standards, and easy access to medical care.
In this study we utilized medical claims, maintained by the US Centers of Medicare and Medicaid Services. The significant potential of this data repository for conducting a broad range of investigations in environmental epidemiology at the local and nationwide has been widely demonstrated. In our research, we explored CMS data to describe the effects of drinking water contamination on vulnerable population51, examined the emerging trends52,53, seasonal patterns54,55,56, and nationwide spatio-temporal synchronization in hospitalizations due to infectious agents56. This data source also allowed us to estimate immediate direct medical expenses associated with hospitalizations directly related to environmental heat exposure. Total charges associated with 41,927 cases of heat-related hospitalizations, reported over 16 years resulted in $438,845,346 nationwide, or ~$27 million annually. In Boston MSA, HHs contributed $5,714,391 of medical charges, which is almost equivalent to the annual state budget allocated to the Supportive Senior Housing of $5.5 million for 2015 (Massachusetts Budget and Policy Center (MassBudget) 2013). The overall impact of heat waves on health is not limited to the heat related morbidity14,57,58. Thus, the observed increase of heat related hospitalizations based on the selected ICD codes is very likely to underestimate the impact of heat waves on health and provides very conservative estimate of the effect and associated costs. As we limited the study to only hospitalizations directly related to environmental heat exposure with well-defined symptoms codes as primary causes, the presented results are likely to be least affected by changes in somewhat complex hospitalization coding rules58.
The pattern of hospitalization due to heat varied quite significantly across geographic regions59,60,61,62,63 and the reasons for such difference are not yet clear. This study demonstrates that one of the reasons might be a different response to heatwaves and its dependence on the timing of heatwaves. While the days defined as heatwave represent only 2% out of 5,844 days under observations, one third of heat-related hospitalizations occurred during one week of the summer-time period annually. The relative risk of heat strokes associated with the first heatwave of a season is 5-fold higher than the risks of the subsequent waves. With the average maximum daily temperature of 87.3 °F and average minimum night temperature of 69.3 °F observed during heatwaves, a sudden increase in daily hospitalization up to 10–15 cases are plausible14,57,58. These findings suggest that the prevention programs should focus their effort on the first heat wave of the season to maximize the public health impact.
We also argue that in the temperate climate of Boston special attention should be paid to daily minimum temperature in setting up public health communication. Our data-derived empirical definition of a heatwave episode includes both minimum and maximum temperature. A day is defined as heatwave if the night-time temperatures is above 65.5 °F (or above 86.5th percentile) for 3 consecutive nights. At this threshold the maximum daily temperature is likely to be about 87.3 °F, or at its 86.5th percentile. Minimum daily air temperature is often used as a proxy variable to estimate average daily near-surface humidity, especially in non-arid climates64. The relative near-surface humidity in temperate climate with relative humidity above 50% can be approximated by the conversion formula
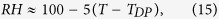 |
where RH is relative humidity, T is an ambient temperature, and TDP is a dew point temperature65. From the Eq. (15) follows that the higher dew point temperature indicate higher relative humidity. In Boston MSA, the night-time temperature follows very closely the dew point temperature during summer months (correlation coefficient of 0.86, p < 0.001). The average timing of heatwave episodes tends to cluster when dew points are high late July and August (Fig. 5). Therefore, our empirical definition more likely selects days with high humidity and temperature above 85th percentile, emphasizing that humid nights with high minimum daily temperature are likely to provide little relieve from daily heat.
Figure 5. Average daily minimum, maximum, and dew point temperature values (solid lines), average timing of first, second, third and forth heatwave episodes (shown with green dots), and cumulative heat-related hospitalization counts (needle plot) during summer months in Boston MSA, in 1991–2006 (May through September).
This study offers a number of methodological innovations for investigating the effects of thermal extremes on human health. In order to define a locally-specific definition of a heatwave episode, we designed an approach that allows incorporating the steep exponential increase in health outcome as daily temperature within a widely accepted linear regression framework and simultaneously select the thresholds for daytime and nighttime temperatures accounting for lag-distributed effects. The use of a threshold assumes that there is a comfort zone, exceeding which human thermoregulation fails to respond properly and adverse health outcomes might occur. We argue that an “ideal” threshold should be both person- and location- specific. A person with underlying health conditions, known to contribute to individual vulnerability16,23,66 might have a temperature threshold lower than that of a healthy individual. Temperature thresholds should be also location-specific and may depend on cultural, social and economic adaptation67,68. A better understanding of individual-based and community-based thresholds will help to reliably predict an ability to withstand the extreme weather effects and to implement location-specific early warning systems. Furthermore, affordable measures for regular hydration and cooling can be and should be introduced in a timely manner.
The proposed concept of the lag-distributed effect of exposure, initially introduced by Naumova and MacNeill in ref. 55 has been further developed and adapted in this research. The proposed approach accounts for overall duration of exposure by estimating an effective duration using distributed lag model for both minimum and maximum temperature in one model. Diurnal variations between daytime and nighttime convey valuable information on the likelihood of adverse health effects by indicating the potential for heat relief at night after exposure to heat through the day. The smaller difference between minimum and maximum temperatures demonstrates a longer duration of heat exposure and higher relative humidity. This approach allows us to improve the estimation of relative risk by proper depiction of a complex non-linear nature of relationship between temperature and health outcomes and reducing underestimation. In the proposed model each component controls for a biological mechanism or behavioral pattern. The year-related component explicitly controls the temporal changes during multi-year study, including demographic changes and potential adaptation measures due to changes in the coding rules for the medical diagnoses in Medicare claim data58. The seasonality-related terms account for sharp intra-year changes in hospitalizations due to environmental exposure to heat, markedly different during warm and cold seasons. The short-term intra-week periodic changes were controlled to recognize the fact that hospital admissions might be influenced by social calendars, so admissions during weekends and holidays are generally lower than during the workdays in the middle of the week. Finally, the two terms of primary interest measure the effect of the first seasonal heatwave and subsequent heatwaves and test the hypotheses that the impact of the first seasonal heat wave differs from the consecutive heatwaves.
As we compared the proposed region-specific data-driven definition of heatwave with four other heatwave definitions, we observed the expected overlap of 69 out of 111 days, with many remaining non-overlapping days differ by a day or two which indicates a good agreement with existing definition as well as certain amount of a site specific localization. The proposed data-driven definition is an improvement over existing schemes as it allows dynamic definition adjusted for local climatic variations and levels of social adaptation. It replaces universal rigid rules with tailored region-specific guidelines that can be adjusted based on underlying latent regional properties, including climate change. This flexibility is important in the context of regional adaptation. The next step is to explore how data-driven location-specific definitions vary across climatic zones and to determine a set of rules for selecting definitions with high predictive ability for specific health conditions and subpopulations.
We strongly advocate for better timing and targeting public health announcements, increasing the awareness of detrimental health effects of heat exposure in older adults and for the need of systematic improvement of living conditions, infrastructure and medical support for most vulnerable population to ensure their wellbeing and reduce the cost of health care. The disproportionally strong impact of the first heatwave highlights the importance of surveillance and early warning systems. The systematic seasonal pattern in heat-related hospitalizations calls for better planning hospital workload in the summer months. It also supports the assertion of the high return of investing in improving early warning notifications of vulnerable population and the urban infrastructure. Computationally intensive mathematical and statistical modeling applied to routinely and timely collected national data should provide strong basis for reliable near-term forecasting and real-time assessment of effectiveness of intervention strategies.
Additional Information
How to cite this article: Liss, A. et al. Heat-Related Hospitalizations in Older Adults: An Amplified Effect of the First Seasonal Heatwave. Sci. Rep. 7, 39581; doi: 10.1038/srep39581 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Acknowledgments
This study was in part supported by the National Institute of Environmental Health Sciences through the project “Gastroenteritis and Extreme Weather Events in Elderly–GEWEL” (NIEHS-R01ES013171). The hospitalization records were provided by the Center for Medicare and Medicaid Services (CMS). RW and AL thank the School of Engineering, Tufts University for travel support to present preliminary results at scientific conferences. This project was supported by a grant from the Intelligence Community Postdoctoral Research Fellowship Program. All statements of fact, opinion, or analysis expressed are those of the author and do not reflect the official positions or views of the Intelligence Community or any other US Government agency. Nothing in the contents should be construed as asserting or implying US Government authentication of information or Intelligence Community endorsement of the authors’ views.
Footnotes
Author Contributions A.L. and E.N.N. designed the study; R.W. and K.C. conducted preliminary analysis; E.N.N. secured data acquisition and oversaw data abstraction; A.L. and E.N.N. analyzed the data and drafted the manuscript with input from R.W. and K.C. All authors have reviewed and approved the manuscript.
References
- Hajat S. & Kosatky T. Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health 64, 753–760, doi: 10.1136/jech.2009.087999 (2010). [DOI] [PubMed] [Google Scholar]
- Kovats R. S. & Hajat S. Heat stress and public health: a critical review. Annual review of public health 29, 41–55, doi: 10.1146/annurev.publhealth.29.020907.090843 (2008). [DOI] [PubMed] [Google Scholar]
- World Meteorological Organization & World Health Organization. Heatwaves and health: guidance on warning-system development 114 (2015).
- Crimmins A. et al. Eds. 312 pp (US Global Change Research Program, Washington, DC, 2016).
- Vanhems P., Gambotti L. & Fabry J. Excess rate of in-hospital death in Lyons, France, during the August 2003 heat wave. The New England journal of medicine 349, 2077–2078, doi: 10.1056/nejm200311203492120 (2003). [DOI] [PubMed] [Google Scholar]
- Gremy I., Lefranc A. & Pepin P. Impact of the August 2003 heat wave: sanitary consequences in Ile-de-France. Revue d’epidemiologie et de sante publique 52, 93–98 (2004). [DOI] [PubMed] [Google Scholar]
- Fouillet A. et al. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health 80, 16–24, doi: 10.1007/s00420-006-0089-4 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecomte D. & de Penanster D. People living in Paris, dead during the August 2003 heatwave, and examined in Medicolegal Institute. Bulletin de l’Academie nationale de medecine 188, 459–469; discussion 469–470 (2004). [PubMed] [Google Scholar]
- Dhainaut J. F., Claessens Y. E., Ginsburg C. & Riou B. Unprecedented heat-related deaths during the 2003 heat wave in Paris: consequences on emergency departments. Critical care (London, England) 8, 1–2, doi: 10.1186/cc2404 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonardi G. S. et al. Syndromic surveillance use to detect the early effects of heat-waves: an analysis of NHS direct data in England. Soz Praventivmed 51, 194–201 (2006). [DOI] [PubMed] [Google Scholar]
- Villamil Cajoto I. et al. Health impact of 2003 heat wave at Hospital de Riveira (A Coruna). Anales de medicina interna (Madrid, Spain: 1984) 22, 15–20 (2005). [DOI] [PubMed] [Google Scholar]
- Claessens Y. E. et al. How emergency departments might alert for prehospital heat-related excess mortality? Critical care (London, England) 10, R156, doi: 10.1186/cc5092 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis F. P., Prince H. P., Lovatt G. & Whittington R. M. Mortality and morbidity in Birmingham during the 1976 heatwave. The Quarterly journal of medicine 49, 1–8 (1980). [PubMed] [Google Scholar]
- Basu R. & Samet J. M. Relation between Elevated Ambient Temperature and Mortality: A Review of the Epidemiologic Evidence. Epidemiologic Reviews 24, 190–202, doi: 10.1093/epirev/mxf007 (2002). [DOI] [PubMed] [Google Scholar]
- Gamble J. L. et al. Climate change and older Americans: State of the science. Environ Health Perspect 121, 15–22, doi: 10.1289/ehp.1205223 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stafoggia M. et al. Vulnerability to heat-related mortality: a multicity, population-based, case-crossover analysis. Epidemiology 17, 315–323, doi: 10.1097/01.ede.0000208477.36665.34 (2006). [DOI] [PubMed] [Google Scholar]
- Vandentorren S. et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. The European Journal of Public Health 16, 583–591 (2006). [DOI] [PubMed] [Google Scholar]
- Semenza J. C., McCullough J. E., Flanders W. D., McGeehin M. A. & Lumpkin J. R. Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med 16, 269–277 (1999). [DOI] [PubMed] [Google Scholar]
- Wiener J. M. & Tilly J. Population ageing in the United States of America: implications for public programmes. Int J Epidemiol 31, 776–781, doi: 10.1093/ije/31.4.776 (2002). [DOI] [PubMed] [Google Scholar]
- White-Newsome J. L. et al. Survey of county-level heat preparedness and response to the 2011 summer heat in 30 US States. Environ Health Perspect 122, 573–579, doi: 10.1289/ehp.1306693 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson G. B. & Bell M. L. Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 US communities. Environ Health Perspect 119, 210–218, doi: 10.1289/ehp.1002313 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oudin Åström D., Bertil F. & Joacim R. Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas 69, 99–105, doi: 10.1016/j.maturitas.2011.03.008 (2011). [DOI] [PubMed] [Google Scholar]
- D’Ippoliti D. et al. The impact of heat waves on mortality in 9 European cities: results from the EuroHEAT project. Environ Health 9, 37, doi: 10.1186/1476-069X-9-37 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong S., Ren C. & Becker N. Excess deaths during the 2004 heatwave in Brisbane, Australia. Int J Biometeorol 54, 393–400, doi: 10.1007/s00484-009-0290-8 (2010). [DOI] [PubMed] [Google Scholar]
- Frich P. et al. Observed coherent changes in climatic extremes during the second half of the twentieth century. Climate Research 19, 193–212, doi: 10.3354/cr019193 (2002). [DOI] [Google Scholar]
- Smith T. T., Zaitchik B. F. & Gohlke J. M. Heat waves in the United States: Definitions, patterns and trends. Climatic Change 118, 811–825, doi: 10.1007/s10584-012-0659-2 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baccini M. et al. Heat effects on mortality in 15 European cities. Epidemiology 19, 711–719, doi: 10.1097/EDE.0b013e318176bfcd (2008). [DOI] [PubMed] [Google Scholar]
- Ballester-Díez F., Corella-Piquer D., Pérei-Hoyos S., Hervás-Hernandorena A. & Merino-Egea C. Seasonal variation of mortality rates within the city of Valencia, Spain. Variacion estacional de la mortalidad en la ciudad de Valencia, Espana 39, 95–101 (1997). [PubMed] [Google Scholar]
- Curriero F. C. et al. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol 155, 80–87 (2002). [DOI] [PubMed] [Google Scholar]
- Kovats R. S., Hajat S. & Wilkinson P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occup Environ Med 61, 893–898, doi: 10.1136/oem.2003.012047 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S. et al. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology 20, 738–746, doi: 10.1097/EDE.0b013e3181ad5522 (2009). [DOI] [PubMed] [Google Scholar]
- Michelozzi P. et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. American journal of respiratory and critical care medicine 179, 383–389, doi: 10.1164/rccm.200802-217OC (2009). [DOI] [PubMed] [Google Scholar]
- Chestnut L. G., Breffle W. S., Smith J. B. & Kalkstein L. S. Analysis of differences in hot-weather-related mortality across 44 US metropolitan areas. environmental science & policy 1, 59–70 (1998). [Google Scholar]
- Kalkstein L. S. Health and climate change. Direct impacts in cities. Lancet 342, 1397–1399 (1993). [DOI] [PubMed] [Google Scholar]
- Mastrangelo G. et al. Pattern and determinants of hospitalization during heat waves: an ecologic study. BMC Public Health 7, 200, doi: 10.1186/1471-2458-7-200 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. & Naumova E. In Intelligence and Security Informatics: Biosurveillance Vol. 4506 Lecture Notes in Computer Science (eds Daniel Zeng et al.) Ch. 5, 47–58 (Springer Berlin Heidelberg, 2007). [Google Scholar]
- Hess J. J., Saha S. & Luber G. Summertime Acute Heat Illness in US Emergency Departments from 2006 through 2010: Analysis of a Nationally Representative Sample. Environ Health Perspect 34, doi: 10.1289/ehp.1306796 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu G. Y. & Wong D. W. An adaptive inverse-distance weighting spatial interpolation technique. Computers & Geosciences 34, 1044–1055, doi: 10.1016/j.cageo.2007.07.010 (2008). [DOI] [Google Scholar]
- WHO (World Health Organization). Improving Public Health Responses to Extreme Weather/Heat-Waves—EuroHEAT: Technical Summary. 70 pp (WHO Regional Office for Europe, Copenhagen Ø, Denmark, 2009). [Google Scholar]
- Matthies F. & Menne B. Prevention and management of health hazards related to heatwaves. Int J Circumpolar Health 68, 8–22 (2009). [DOI] [PubMed] [Google Scholar]
- Smoyer-Tomic K. E., Kuhn R. & Hudson A. Heat Wave Hazards: An Overview of Heat Wave Impacts in Canada. Natural Hazards 28, 465–486, doi: 10.1023/a:1022946528157. [DOI] [Google Scholar]
- Barnett A. G., Tong S. & Clements A. C. A. What measure of temperature is the best predictor of mortality? Environ Res 110, 604–611, doi: 10.1016/j.envres.2010.05.006 (2010). [DOI] [PubMed] [Google Scholar]
- Naumova E. & MacNeill I. In Advances in Statistical Methods for the Health Sciences Statistics for Industry and Technology (eds Jean-Louis Auget N. Balakrishnan, Mounir Mesbah & Geert Molenberghs) 437–450 (Birkhäuser Boston, 2007). [Google Scholar]
- Naumova E. N. et al. Seasonality in six enterically transmitted diseases and ambient temperature. Epidemiol Infect 135, 281–292, doi: 10.1017/S0950268806006698 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajat S., O’Connor M. & Kosatsky T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet (London, England) 375, 856 (2010). [DOI] [PubMed] [Google Scholar]
- Barnett A. G. Temperature and cardiovascular deaths in the US elderly: Changes over time. Epidemiology 18, 369–372 (2007). [DOI] [PubMed] [Google Scholar]
- Barreca A., Clay K., Deschenes O., Greenstone M. & Shapiro J. S. Vol. w18692 (National Bureau of Economic Research, Inc, NBER Working Papers: 18692, 2013).
- Bobb J. F., Peng R. D., Bell M. L. & Dominici F. Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect 122, 811–816, doi: 10.1289/ehp.1307392 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A. et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. The Lancet 386, 369–375, doi: 10.1016/S0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson H. et al. The impact of the 2003 heat wave on daily mortality in England and Wales and the use of rapid weekly mortality estimates. Euro Surveill 10, 168–171 (2005). [PubMed] [Google Scholar]
- Naumova E. N., Egorov A. I., Morris R. D. & Griffiths J. K. The elderly and waterborne Cryptosporidium infection: gastroenteritis hospitalizations before and during the 1993 Milwaukee outbreak. Emerg Infect Dis 9, 418–425 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagai J. & Naumova E. Clostridium difficile-associated disease in the elderly, United States. Emerg Infect Dis 15, 343–344 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mor S. M., DeMaria A. Jr., Griffiths J. K. & Naumova E. N. Cryptosporidiosis in the elderly population of the United States. Clin Infect Dis 48, 698–705, doi: 10.1086/597033 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chui K. K., Jagai J. S., Griffiths J. K. & Naumova E. N. Hospitalization of the elderly in the United States for nonspecific gastrointestinal diseases: a search for etiological clues. Am J Public Health 101, 2082–2086, doi: 10.2105/AJPH.2010.300096 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naumova E. N. & MacNeill I. B. Time-distributed effects of exposure and infectious outbreaks. Environmetrics. 20, 235–248 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenger J. B. & Naumova E. N. Seasonal synchronization of influenza in the United States older adult population. PLoS One 5, e10187, doi: 10.1371/journal.pone.0010187 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health 8, 40, doi: 10.1186/1476-069X-8-40 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilbourne E. M. The spectrum of illness during heat waves. Am J Prev Med 16, 359–360 (1999). [DOI] [PubMed] [Google Scholar]
- Sheridan S. C. & Lin S. Assessing variability in the impacts of heat on health outcomes in New York City over time, season, and heat-wave duration. Ecohealth 11, 512–525, doi: 10.1007/s10393-014-0970-7 (2014). [DOI] [PubMed] [Google Scholar]
- Knowlton K. et al. Projecting Heat-Related Mortality Impacts Under a Changing Climate in the New York City Region. Am J Public Health 97, 2028–2034, doi: 10.2105/AJPH.2006.102947 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson L. A. et al. The impact of heat on mortality and morbidity in the Greater Metropolitan Sydney Region: a case crossover analysis. Environ Health 12, 98, doi: 10.1186/1476-069x-12-98 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye X. et al. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect 120, 19–28, doi: 10.1289/ehp.1003198 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaneckova P. & Bambrick H. Cause-specific hospital admissions on hot days in Sydney, Australia. PLoS One 8, e55459, doi: 10.1371/journal.pone.0055459 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimball J. S., Running S. W. & Nemani R. An improved method for estimating surface humidity from daily minimum temperature. Agricultural and Forest Meteorology 85, 87–98, doi: 10.1016/S0168-1923(96)02366-0 (1997). [DOI] [Google Scholar]
- Lawrence M. G. The Relationship between Relative Humidity and the Dewpoint Temperature in Moist Air: A Simple Conversion and Applications. Bulletin of the American Meteorological Society 86, 225–233, doi: 10.1175/BAMS-86-2-225 (2005). [DOI] [Google Scholar]
- Mastrangelo G. et al. Contrasting patterns of hospital admissions and mortality during heat waves: are deaths from circulatory disease a real excess or an artifact? Med Hypotheses 66, 1025–1028, doi: 10.1016/j.mehy.2005.09.053 (2006). [DOI] [PubMed] [Google Scholar]
- Bell M. L. et al. Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol 37, 796–804, doi: 10.1093/ije/dyn094 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill M. S., Hajat S., Zanobetti A., Ramirez-Aguilar M. & Schwartz J. Impact of control for air pollution and respiratory epidemics on the estimated associations of temperature and daily mortality. Int J Biometeorol 50, 121–129 (2005). [DOI] [PubMed] [Google Scholar]