Abstract
Background:
The patient-ventilator asynchrony is almost observed in all modes of ventilation, and this asynchrony affects lung mechanics adversely resulting in deleterious outcome. Innovations and advances in ventilator technology have been trying to overcome this problem by designing newer modes of ventilation. Pressure support ventilation (PSV) is a commonly used flow-cycled mode where a constant pressure is delivered by ventilator. Proportional assist ventilation (PAV) is a new dynamic inspiratory pressure assistance and is supposed to be better than PSV for synchrony and tolerance, but reports are still controversial. Moreover, most of these studies are conducted in chronic obstructive pulmonary disease patients with respiratory failure; the results of these studies may not be applicable to surgical patients. Thus, we proposed to do compare these two modes in surgical Intensive Care Unit (ICU) patients as a randomized crossover study.
Aims:
Comparison of patient-ventilator asynchrony between PSV and PAV plus (PAV+) in surgical patients while weaning.
Subjects and Methods:
After approval by the Hospital Ethics Committee, we enrolled twenty patients from surgical ICU of tertiary care institute. The patients were ventilated with pressure support mode (PSV) and PAV+ for 12 h as a crossover from one mode to another after 6 h while weaning.
Results:
Average age and weight of patients were 41.80 ± 15.20 years (mean ± standard deviation [SD]) and 66.50 ± 12.47 (mean ± SD) kg, respectively. Comparing the asynchronies between the two modes, the mean number of total asynchronous recorded breaths in PSV was 7.05 ± 0.83 and 4.35 ± 5.62, respectively, during sleep and awake state, while the same were 6.75 ± 112.24 and 10.85 ± 11.33 in PAV+.
Conclusion:
Both PSV and PAV+ modes of ventilation performed similarly for patient-ventilator synchrony in surgical patients. In surgical patients with acute respiratory failure, dynamic inspiratory pressure assistance modalities are not superior to PSV with respect to cardiorespiratory function.
Key Words: Patient-ventilator dyssynchrony, pressure support ventilation, proportional assist ventilation
Introduction
The patient-ventilator asynchrony is the mismatching between patient's neural inspiratory drive and breath delivery by the ventilator. Alterations in respiratory drive, timing, respiratory muscle pressure, and respiratory system mechanics influence the interaction between the patient and the ventilator.[1] It is well known that patient-ventilator asynchrony affects adversely on lung mechanics, gas exchange, ventilator-induced lung injury, and ventilator-free days in Intensive Care Unit (ICU). Pressure support ventilation (PSV) is a commonly used flow-cycled mode for weaning in ICU. In PSV, the ventilator applies constant preset pressure for every detected patient's inspiratory effort.[2] Proportional assist ventilation (PAV) was developed as a mode to enhance ventilator responsiveness to patient's breathing effort. Like PSV, PAV uses a sensitive inspiratory set trigger in the form of negative pressure or flow, but unlike PSV that uses a clinician preset inspiratory pressure, PAV provides dynamic pressure in proportion to the patient's spontaneous breathing effort as determined by instantaneous feedback from an in-line pneumotachometer. In addition, cycling from inspiration to expiration is not dependent on a predetermined reduction in inspiratory flow. Rather PAV, when properly adjusted, terminates delivery of inspiratory assistance with cessation of inspiratory effort.[2,3] PAV plus (PAV+ in Puritan Bennett 840 ventilator range) is a commercially available implementation of PAV which automatically amplifies the patient's own spontaneous effort to breathe by increasing airway pressure during inspiration proportionally to a set amplification factor.
Although some studies have shown that PAV+ improves synchrony between patient and ventilator as compared to PSV, some other studies have challenged the superiority of PAV+.[4,5,6] Thus, to work on this controversy, so we studied these two modes as a crossover study.
Subjects and Methods
After approval by the Hospital Ethics Committee, the study was carried out in twenty surgical ICU patients of tertiary care institute. The written informed consent was obtained from patients' attendants. Patients with head injury, history of stroke/cerebrovascular accidents, having chronic obstructive pulmonary diseases (COPDs), and myopathies were excluded from the study to minimize bias. The patients were ventilated with pressure support mode (PSV) and PAV+ for 12 h as a crossover from one mode to another after 6 h. Order of ventilation modes was selected randomly once the patient started triggering all ventilator breaths on assist-control (A/C) ventilation. All patients were given analgesia and sedation using fentanyl 0.5 μg/kg/h by body weight through intravenous infusion and were sedated using midazolam infusion keeping sedation score of 3–5 on Ramsay scale at the start of the study. Ventilator settings depending on the mode and patient characteristics were chosen. Triggering was adjusted during sedation period to minimize ineffective breaths and auto triggering. Thereafter, 2 h before second recordings at 0400 h, midazolam infusion was stopped to awaken the patient. Recording was done at 0600 h, and ventilator mode was then changed to second study mode and sedation was stepped up to Ramsay scale 3 again. Recordings were done at 0700 and 1200 h again with and without sedation, respectively. Puritan Bennett 840 was used for the entire study. Pressure support in PSV was set to achieve a tidal volume of 6 ml/kg approximately. PSV cycling-off criterion was set at 20% of the peak flow. PSV rise time was set at 0 s. PAV+ was set to adjust work of breathing between 0.3 and 0.7 J/L. The ventilator settings other than FiO2 and positive end-expiratory pressure were kept constant. In case of difficulty and failure to ventilate, patients were excluded from analysis. Average spirometric data were noted over ten consecutive breaths. The asynchrony was recorded visually on 10 min recordings of flow and airway pressure. In addition, ventilator graphics were recorded on video for 10 min for 0100, 0600, 0700, and 1200 h. These recorded videos were later analyzed to see the types of patient-ventilator asynchrony as described in Table 2. In addition to the above data, change in patient's hemodynamic data, spirometric data, and arterial blood gas was also recorded and analyzed.
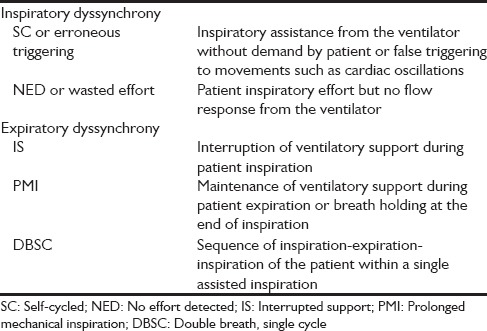
Table 2.
Types of patient-ventilator asynchrony
Results
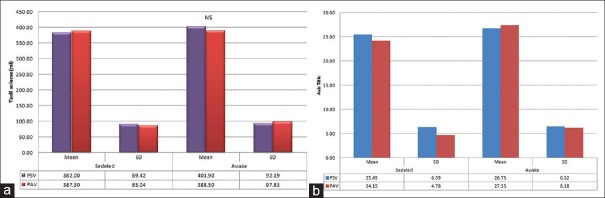
There was no dropout case during the entire study period because of failure to ventilate with either mode. Patient demographic, characteristics, and respiratory parameters are shown in tables and figures [Table 1, and Figure 1a, b]. Average age of patients was 41.80 ± 15.20 (mean ± standard deviation [SD]) years. Nearly 75% of patients were male. The weight of patients ranged between 40 and 90 kg with a mean of 66.50 ± 12.47(mean ± SD) kg.
Table 1.
Patient characteristics (n=20), crossover study
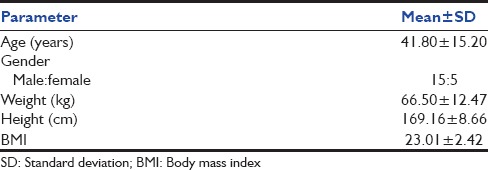
Figure 1.
(a) Similar tidal volume among two modes in different states. (b) Similar respiratory rates among two modes in different states
The mean number of cycles studied in PSV was 254.50 ± 63.86 (mean ± SD) in sedated and 267.50 ± 65.20 (mean ± SD) in awake state and the difference was found to be statistically insignificant (P = 0.528). The same for PAV+ was 241.50 ± 47.82 (mean ± SD) in sedated and 273.50 ± 61.84 (mean ± SD) in awake state and difference again insignificant (P = 0.075). Furthermore, the difference between cycles of two modes was found to be statistically insignificant in sedated (P = 0.471) and awake states (P = 0.767) [Tables 3 and 4].
Table 3.
Total asynchronous breaths including and excluding prolonged mechanical inspiration (n=20)
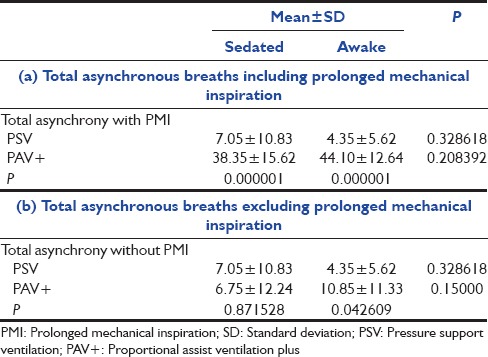
Table 4.
Distribution of patient-ventilator asynchronies among two modes (n=20)
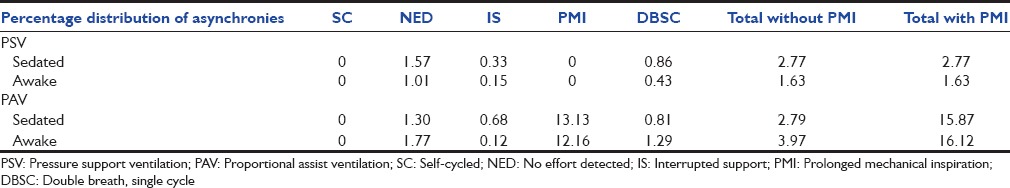
Comparing the asynchronies between the two modes [Table 3], the mean number of total asynchronous cycles in sedated and awake states in PSV was 7.05 ± 10.83 (mean ± SD) and 4.35 ± 5.62 (mean ± SD), respectively, and in PAV+ was 38.35 ± 15.62 (mean ± SD) and 44.10 ± 12.64 (mean ± SD), respectively. We also calculated the percentage distribution of asynchronies in both the modes and in both states. Patients during PAV+ mode had variable inspiratory hold for a short period unlike prolonged mechanical inspiration (PMI) extending into expiratory phase. To minimize interpretation and conclusion bias, we calculated asynchrony frequency with and without PMI. The number of PMI asynchronies in PSV was nil in both awake and sedated states. In PAV+, the mean number of PMI asynchronies in sedated and awake states was 31.70 ± 7.91 (mean ± SD) and 33.25 ± 7.99 (mean ± SD), respectively, and this difference was found to be statistically insignificant (P = 0.541). The results showed that the difference between the total asynchronies in sedated and awake states was statistically insignificant in both modes during intragroup comparison (P = 0.329 for PSV and P = 0.208 for PAV+). However, for intergroup comparison, the difference between the two modes was found to be highly significant in both sedated and awake states if we considered inspiratory hold in PAV+ as PMI (P = 0.000001 for both states). The second type of asynchrony observed was no effort detected (NED). The mean number of patients with NED asynchronies in sedated and awake states in PSV was 4.00 ± 7.46 (mean ± SD) and 2.70 ± 4.26 (mean ± SD), respectively, and in PAV+ is 3.15 ± 6.18 (mean ± SD) and 4.15 ± 4.85 (mean ± SD), respectively. On intragroup comparison, the difference between the number of NED asynchrony was insignificant in PSV (P = 0.503) and in PAV+ (P = 0.596). The intergroup difference between PSV and PAV+ was also found to be insignificant in sedated and awake states (P = 0.709 for sedated and P = 0.321 for awake). The third type of asynchrony was interrupted support (IS), and as shown in the table in awake state, there were 3.15 ± 5.22 (mean ± SD) cases of IS in PAV+ as compared to 1.65 ± 3.01 (mean ± SD) in PSV, and this difference was statistically significant (P = 0.026). The double-breath, single cycle (DBSC) type of asynchrony was also uncommon, and the difference was statistically insignificant during both intra- and intergroup comparison (P = 0.868 for sedated and 0.114 for awake). The self-cycled type of asynchrony was not observed during the entire study period in either mode. The total asynchronies were 2.77% in PSV sedated, 1.63% in PSV awake, 15.87% in PAV+ sedated, and 16.12% PAV+ awake. If we exclude PMI type of asynchrony, the percentage is same in PSV mode, but in PAV+, it is 2.79% in sedated and 3.97% in awake state. Respiratory and hemodynamic parameters were comparable in both modes [Table 5]. There was an interesting observation that changeover between modes resulted in swings in hemodynamics and respiratory mechanics indicating that patients were either uncomfortable to change or got disturbed due to change [Figures 2 and 3].
Table 5.
Comparison of ventilator mode impact on lung compliance and resistance among two modes n=20
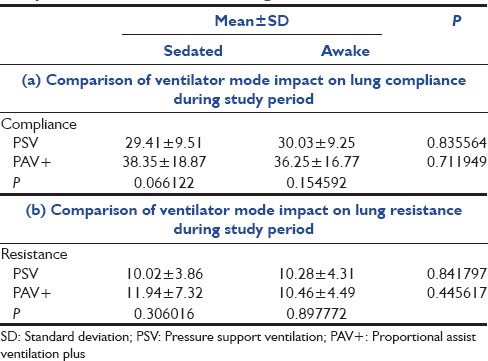
Figure 2.
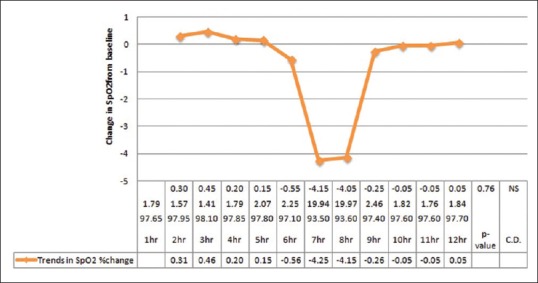
Trends in SpO2 change during study period
Figure 3.
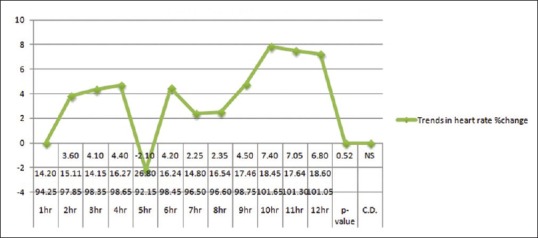
Trends in heart rate during study period
Discussion
The patient-ventilator asynchrony has been an issue concern and is observed in almost all spontaneous modes of ventilation. This asynchrony not only results in patient discomfort but also leads to heterogeneous ventilation distribution and atelectasis. Patients with high level of asynchrony require a longer duration of mechanical ventilation (MV), higher incidence of tracheostomy, weaning failure, longer ICU, and hospital stay with additional economic burden.[7,8,9,10] To improve upon this patient-ventilator interaction, various new modes of ventilation are designed and tested.
In our crossover study of PSV and PAV+ modes, in PAV+ mode, we found no flow near the end of inspiration in some patients, i.e., end-inspiratory hold/PMI. However, inspiratory hold did not have apparent detrimental effect on gas exchange in our study. Costa et al. observed this finding in PSV also.[11] Authors found that during PSV trials, the mechanical inspiratory time Ti (flow) was significantly longer than patient inspiratory time Ti (pat) as compared to PAV+ (P < 0.05). PAV+ significantly reduced delay (P < 0.001). If we include this as asynchrony, then PSV had lesser asynchronous breaths as compared to PAV+ (P = 0.000001). However, if we exclude this asynchrony from analysis, both modes performed clinically in a similar fashion. More patient-ventilator asynchronies were observed in PAV+ than PSV while patients were awake (P = 0.043). During inspiratory cycle, two asynchronies (self-cycling and no effort) were comparable and statistically insignificant in both the modes. During expiratory phase, the IS type of asynchronies was noted more frequently in PAV+ as compared to PSV during awake state. DBSC type of asynchrony was also comparable in both modes. Compliance, resistance, tidal volume, and hemodynamics were comparable without statistical significance. The changes in PCO2 and PO2 were statistically insignificant in all the comparisons. The comparison of the mean SaO2 values, PaO2 /FiO2 ratio, and Δ(A-a) O2 difference was all statistically insignificant. Thus, it means there is no superiority or inferiority of any mode for pulmonary mechanics and gas exchange. Hart et al. had similar finding while comparing these two modes in patient with chest deformity and muscle disease having chronic respiratory failure. However, they found greater unloading in PSV than in PAV, associated with greater benefit too.[12] Although some authors in short-term studies found some physiological and symptomatic improvements in patients with chronic respiratory failure due to COPD and cystic fibrosis with PAV mode, most of the studies at large have failed to prove superiority of either mode.[8] Our observations were similar to those reported by Kondili et al. and Porta et al.[5,6] Bosma et al. found fewer patient-ventilator asynchronies and better quality of sleep with PAV.[7] Dirk Varelmann et al. compared randomly PSV and PAV as a crossover study on 12 patients and did not observe a significant difference in hemodynamics and blood gas parameters.[4] In 2011, Hosking et al. compared A/C, PSV, and PAV modes for weaning and found high asynchrony index in 27% of cases in the high PSV group and in 6% in the low PSV group with no cases in the PAV group at its different levels of assist.[13] In studies by Elganady and Xirouchaki et al., authors found high asynchrony index with PSV as compared to PAV.[14,15] They observed mainly ineffective triggering and cyclic dyssynchrony with high asynchrony index in PSV. Elganady et al. found higher weaning success rate (90%) and fewer ventilator days with PAV in COPD patients as compared to PSV 66.7%. The variation in results might be due to different patient characteristics, sedation, diurnal orientation, and trigger setting, etc.
Recently, Aguirre-Bermeo et al. and Teixeira et al. in prospective studies found no difference among two modes for tolerance, extubation failure, duration of MV, ICU and hospital stays, and clinical outcomes during weaning from MV.[16,17] Most of the studies on different modes of ventilation conducted for synchrony comparison, have reported similar outcome with PSV and PAV, but with PAV having better tolerance. However, these studies are from COPD patients. Comparing MV modes are difficult as patient characteristics, level of support, pain, sedation, circadian rhythm, coexisting disease, etc., all affect the demand and patient comfort.
There were few limitations in our study as we did not study the esophageal pressures and transpulmonary pressures to detect the ineffective breaths. Another limitation is that we did not study ventilator support at different levels of support. High and low support can alter asynchrony index. Another limitation was that we did not maintain and record the circadian rhythm of the patients.
From the observations made during our study and literature, we conclude that both PSV and PAV+ modes perform overall similarly for patient-ventilator interactions in awake and sedated states. Variable end inspiratory hold was observed in PAV+ mode without detrimental concerns on gas exchange. Patients had a higher compliance and PO2 /FiO2 ratio values in PAV+ mode although these values did not gain statistical significance. There was an interesting observation that changeover between modes resulted in swings in hemodynamics and respiratory mechanics indicating that patient tunes to ventilator deliveries overtime.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Grasso S, Puntillo F, Mascia L, Ancona G, Fiore T, Bruno F, et al. Compensation for increase in respiratory workload during mechanical ventilation. Pressure-support versus proportional-assist ventilation. Am J Respir Crit Care Med. 2000;161(3 Pt 1):819–26. doi: 10.1164/ajrccm.161.3.9902065. [DOI] [PubMed] [Google Scholar]
- 2.Sassoon CS, Foster GT. Patient-ventilator asynchrony. Curr Opin Crit Care. 2001;7:28–33. doi: 10.1097/00075198-200102000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Gay PC, Hess DR, Hill NS. Noninvasive proportional assist ventilation for acute respiratory insufficiency comparison with pressure support ventilation. Am J Respir Crit Care Med. 2001;164:1606–11. doi: 10.1164/ajrccm.164.9.2011119. [DOI] [PubMed] [Google Scholar]
- 4.Varelmann D, Wrigge H, Zinserling J, Muders T, Hering R, Putensen C. Proportional assist versus pressure support ventilation in patients with acute respiratory failure: Cardiorespiratory responses to artificially increased ventilatory demand. Crit Care Med. 2005;33:1968–75. doi: 10.1097/01.ccm.0000178191.52685.9b. [DOI] [PubMed] [Google Scholar]
- 5.Kondili E, Xirouchaki N, Vaporidi K, Klimathianaki M, Georgopoulos D. Short-term cardiorespiratory effects of proportional assist and pressure-support ventilation in patients with acute lung injury/acute respiratory distress syndrome. Anesthesiology. 2006;105:703–8. doi: 10.1097/00000542-200610000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Porta R, Appendini L, Vitacca M, Bianchi L, Donner CF, Poggi R, et al. Mask proportional assist vs. pressure support ventilation in patients in clinically stable condition with chronic ventilatory failure. Chest. 2002;122:479–88. doi: 10.1378/chest.122.2.479. [DOI] [PubMed] [Google Scholar]
- 7.Bosma K, Ferreyra G, Ambrogio C, Pasero D, Mirabella L, Braghiroli A, et al. Patient-ventilator interaction and sleep in mechanically ventilated patients: Pressure support versus proportional assist ventilation. Crit Care Med. 2007;35:1048–54. doi: 10.1097/01.CCM.0000260055.64235.7C. [DOI] [PubMed] [Google Scholar]
- 8.Thille AW, Rodriguez P, Cabello B, Lellouche F, Brochard L. Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006;32:1515–22. doi: 10.1007/s00134-006-0301-8. [DOI] [PubMed] [Google Scholar]
- 9.Chao DC, Scheinhorn DJ, Stearn-Hassenpflug M. Patient-ventilator trigger asynchrony in prolonged mechanical ventilation. Chest. 1997;112:1592–9. doi: 10.1378/chest.112.6.1592. [DOI] [PubMed] [Google Scholar]
- 10.de Wit M, Miller KB, Green DA, Ostman HE, Gennings C, Epstein SK. Ineffective triggering predicts increased duration of mechanical ventilation. Crit Care Med. 2009;37:2740–5. doi: 10.1097/ccm.0b013e3181a98a05. [DOI] [PubMed] [Google Scholar]
- 11.Costa R, Spinazzola G, Cipriani F, Ferrone G, Festa O, Arcangeli A, et al. A physiologic comparison of proportional assist ventilation with load-adjustable gain factors (PAV+) versus pressure support ventilation (PSV) Intensive Care Med. 2011;37:1494–500. doi: 10.1007/s00134-011-2297-y. [DOI] [PubMed] [Google Scholar]
- 12.Hart N, Hunt A, Polkey MI, Fauroux B, Lofaso F, Simonds AK. Comparison of proportional assist ventilation and pressure support ventilation in chronic respiratory failure due to neuromuscular and chest wall deformity. Thorax. 2002;57:979–81. doi: 10.1136/thorax.57.11.979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hosking B, Nikoo M, Bosma KJ. The incidence of patient-ventilator asynchrony during weaning from mechanical ventilation: A comparison of proportional assist ventilation, (PAV) to pressure support (PS) Am J Respir Crit Care Med. 2011;183:A3197. [Google Scholar]
- 14.Elganady AA, Beshey BN, Abdelaziz AA. Proportional assist ventilation versus pressure support ventilation in the weaning of patients with acute exacerbation of chronic obstructive pulmonary disease. Egypt J Chest Dis Tuberc. 2014;63:643–50. [Google Scholar]
- 15.Xirouchaki N, Kondili E, Vaporidi K, Xirouchakis G, Klimathianaki M, Gavriilidis G, et al. Proportional assist ventilation with load-adjustable gain factors in critically ill patients: Comparison with pressure support. Intensive Care Med. 2008;34:2026–34. doi: 10.1007/s00134-008-1209-2. [DOI] [PubMed] [Google Scholar]
- 16.Aguirre-Bermeo H, Bottiroli M, Italiano S, Roche-Campo F, Santos JA, Alonso M, et al. Pressure support ventilation and proportional assist ventilation during weaning from mechanical ventilation. Med Intensiva. 2014;38:363–70. doi: 10.1016/j.medin.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Teixeira SN, Osaku EF, Costa CR, Toccolini BF, Costa NL, Cândia MF, et al. Comparison of proportional assist ventilation plus, t-tube ventilation, and pressure support ventilation as spontaneous breathing trials for extubation: A randomized study. Respir Care. 2015;60:1527–35. doi: 10.4187/respcare.03915. [DOI] [PubMed] [Google Scholar]