Abstract
Amitraz is used as a pesticide in agricultural and veterinary medicine. It is primarily a central α2 adrenergic agonist and known to cause central nervous system depression, convulsions, respiratory depression, and bradycardia on severe intoxication. We report a case of a 3-year-old child who presented with accidental ingestion of amitraz solution with signs of severe poisoning. There is no specific antidote of amitraz poisoning in humans, however, animal experiments with α2 adrenergic antagonists such as yohimbine and atimepazole have been successful. The child was managed besides intensive management with enteral yohimbine, and he regained consciousness in 18 h and was successfully weaned off mechanical ventilation.
Key Words: Amitraz poisoning, poisoning, yohimbine
Introduction
Amitraz is used as a pesticide in agricultural and veterinary medicine.[1] It is primarily a central α2 adrenergic agonist and known to cause central nervous system (CNS) depression, convulsions, respiratory depression, and bradycardia on severe intoxication. We report a case of a 3-year-old child who presented with accidental ingestion of amitraz solution with signs of severe poisoning.
Case Report
A 3-year-old child, weighing 12 kg, was admitted with an alleged history of consumption of around 10 ml of 12.5% solution of amitraz 1 h before the presentation. He was dull on presentation and responding to tactile stimuli, with a pulse rate of 59/min and a systolic blood pressure (BP) of 60 mmHg. He was given 0.6 mg intravenous atropine, and his heart rate increased to 134/min and BP to 82/44 mmHg. His clothes were changed, and he was shifted to Intensive Care Unit (ICU). He was obtunded, and bilateral pupils were pinpoint, but other systemic examination revealed no significant findings. An arterial blood gas revealed acute respiratory acidosis (pH 7.24, pCO2 65, pO2 105) and he was immediately intubated and started on assisted ventilation. His hemodynamics, oxygen saturation were closely monitored and maintained in normal limits. His laboratory investigations were normal. He was started on yohimbine 2 mg [Figure 1], 8th hourly through nasogastric tube. He regained full consciousness after 18 h and was weaned off ventilator and was extubated in next 2 h. Yohimbine was continued for 48 h, and he was shifted out of ICU on day 3 and discharged next day.
Figure 1.
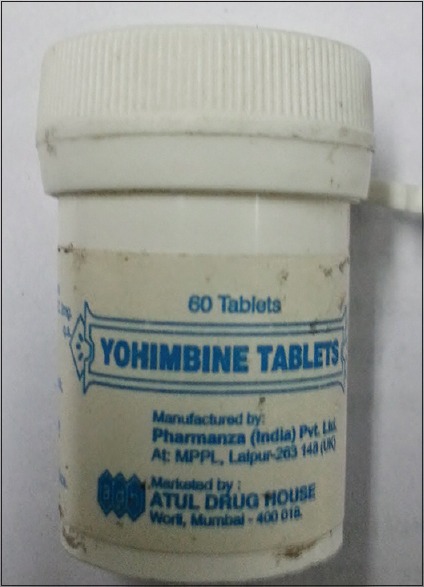
Yohimbine vial used
Discussion
Amitraz is a α2 adrenergic agonist and is used as a pesticide and insect repellent.[1] There are a few human cases of its intoxication, with minimal toxic dose reported as 3.57 mg/kg and around 0.3–1.25 g of 12.5% formulation.[2,3,4,5,6] The clinical features are related to α-adrenergic stimulation and include vomiting, miosis, hyperglycemia, CNS depression, convulsions, respiratory depression, hypothermia, and bradycardia.[1,5] The differential diagnosis of amitraz intoxication includes overdose with opioids, organophosphates, and centrally acting α2 adrenergic agonist drugs like clonidine and sedative-hypnotics such as barbiturates, benzodiazepines, phenothiazines, and tricyclic antidepressants.[1] Coma, the absence of light reflex, and respiratory depression are signs of severe amitraz poisoning.[5] In our patient, there was loss of consciousness, respiratory depression, bradycardia, and miosis which suggested significant intoxication.
The treatment of amitraz intoxication is mainly supportive and symptomatic.[1] Gastric lavage is not recommended unless the dose is massive, because of the presence of petroleum distillate in amitraz formulations.[1] The use of atropine to treat bradycardia is controversial as atropine is mainly effective for the bradycardia that occurs from vagal stimulation and atrioventricular blocks.[1,2,4,6] However, atropine has been found to resolve miosis and bradycardia caused by α2 adrenergic agonist action of amitraz poisoning in a few studies.[1,5] In our patient, bradycardia responded to atropine. After yohimbine was started, no further episodes of bradycardia were seen in the child.
Amitraz and its active metabolite are known to cause hyperglycemia by inhibiting insulin and stimulating glucagon secretion. However, we did not find hyperglycemia in our case.[7] Although there is a lack of sufficient human literature on specific antidote of amitraz poisoning, a few experimental studies in animals have evaluated the use of α2 adrenergic antagonists such as yohimbine and atimepazole, successfully.[8,9] Their use in humans is recommended only for severe cases.[1,10] In our case, the child had all clinical features of severe intoxication. We used the oral formulation of yohimbine at a dose of 0.12 mg/kg (2 mg) 8th hourly through nasogastric tube. This is only case, in our knowledge, about use of yohimbine as an antidote in severe amitraz poisoning. There were no side effects. The resolution time for CNS depression was reported up to 48 h in the previous reports.[1,2,5] In our case, the child regained consciousness in 18 h and could be weaned off ventilator in 20 h of intoxication. The use of yohimbine in this child helped in faster neurological recovery, prevented bradycardia, and provided hemodynamic stability. We recommend further human studies to evaluate the use of yohimbine as an antidote to amitraz poisoning.
Conclusion
Amitraz is an uncommon source of poisoning, but it can be fatal. Timely intensive care supportive management can improve survival in most patients, but antidotes like yohimbine can be used in severe poisoning. However, more human studies are required to establish the efficacy and safety of yohimbine in amitraz poisoning.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Yilmaz HL, Yildizdas DR. Amitraz poisoning, an emerging problem: Epidemiology, clinical features, management, and preventive strategies. Arch Dis Child. 2003;88:130–4. doi: 10.1136/adc.88.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aydin K, Per H, Kurtoglu S, Poyrazoglu MH, Narin N, Aslan D. Amitraz poisoning in children. Eur J Pediatr. 2002;161:349–50. doi: 10.1007/s00431-002-0945-5. [DOI] [PubMed] [Google Scholar]
- 3.Doganay Z, Aygun D, Altintop L, Guven H, Bildik F. Basic toxicological approach has been effective in two poisoned patients with amitraz ingestion: Case reports. Hum Exp Toxicol. 2002;21:55–7. doi: 10.1191/0960327102ht204cr. [DOI] [PubMed] [Google Scholar]
- 4.Aydin K, Kurtoglu S, Poyrazoglu MH, Uzüm K, Ustünbas HB, Hallaç IK. Amitraz poisoning in children: Clinical and laboratory findings of eight cases. Hum Exp Toxicol. 1997;16:680–2. doi: 10.1177/096032719701601109. [DOI] [PubMed] [Google Scholar]
- 5.Eizadi-Mood N, Sabzghabaee AM, Gheshlaghi F, Yaraghi A. Amitraz poisoning treatment: Still supportive? Iran J Pharm Res. 2011;10:155–8. [PMC free article] [PubMed] [Google Scholar]
- 6.Kleinman ME, Chameides L, Schexnayder SM, Samson RA, Hazinski MF, Atkins DL, et al. Part 14: Pediatric advanced life support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S876–908. doi: 10.1161/CIRCULATIONAHA.110.971101. [DOI] [PubMed] [Google Scholar]
- 7.Abu-Basha EA, Yibchok-Anun S, Hopper DL, Hsu WH. Effects of the pesticide amitraz and its metabolite BTS 27271 on insulin and glucagon secretion from the perfused rat pancreas: Involvement of alpha2D-adrenergic receptors. Metabolism. 1999;48:1461–9. doi: 10.1016/s0026-0495(99)90160-9. [DOI] [PubMed] [Google Scholar]
- 8.Andrade SF, Sakate M. The comparative efficacy of yohimbine and atipamezole to treat amitraz intoxication in dogs. Vet Hum Toxicol. 2003;45:124–7. [PubMed] [Google Scholar]
- 9.Andrade SF, Sakate M, Laposy CB, Sangiorgio F. Yohimbine and atipamezole on the treatment of experimentally induced amitraz intoxication in cats. Int J Appl Vet Med. 2006;4:200–8. [Google Scholar]
- 10.Young FM, Menadue MF, Lavranos TC. Effects of the insecticide amitraz, an alpha2-adrenergic receptor agonist, on human luteinized granulosa cells. Hum Reprod. 2005;20:3018–25. doi: 10.1093/humrep/dei194. [DOI] [PubMed] [Google Scholar]


